Abstract
Cation exchange high performance liquid chromatography (CE- HPLC) is an excellent tool for the diagnosis of various hemoglobin (Hb) disorders. HbD-Punjab is an uncommon structural Hb variant seen in North-India. Rarely, a compound heterozygous state for HbD-Punjab with high HbA2 has been described. We describe an index case whose CE-HPLC showed a compound heterozygous state for Hb-Punjab/HbD-Iran which was confirmed by family study, acid and alkaline electrophoresis and beta gene sequencing. This case highlights the role of alkaline and acid electrophoresis to resolve common peaks that elute with HbA2 on CE-HPLC. To the best of our knowledge, this compound heterozygous state of HbD-Punjab with HbD-Iran has not been reported earlier.
Keywords: HbD-Punjab, HbD-Iran, Novel hemoglobinopathy, Hemoglobin variant, Compound heterozygous
Introduction
Inherited disorders of blood including haemoglobinopathies and thalassemia are one of the major public health problems in the whole world. Haemoglobinopathies may be due to deletion, insertion or substitution in the amino acid sequence in either alpha or beta globin chains leading to the formation of structurally defective hemoglobin (Hb). The first hemoglobinopathy, HbS, discovered by Pauling et al. [1], is the most clinically significant hemoglobinopathy. The number of clinically significant variants is relatively low, usually stated as less than 10, compared to the total number of haemoglobinopathies [2].
Here we describe a novel compound heterozygous hemoglobinopathy HbD-Punjab/HbD-Iran that to the best of our knowledge has not been reported in the literature so far.
Case Study
A three and a half year old female was referred to our hospital with the complaints of weakness and easy fatigability since 6 months for which the possibility of a hemoglobinopathy was suggested outside. An earlier complete blood count (CBC) showed mild anemia with Hb of 10.8 g/dl with microcytic hypochromic red cell indices. Her serum iron was low (14.0 μg/dl, reference range 50–160) with normal ferritin levels (26.22 ng/ml, reference range 24–336). She was treated for iron deficiency anemia followed by symptomatic improvement and normalization of the iron and ferritin levels. At our center, on examination there was no pallor, icterus or hepatosplenomegaly and rest of the systemic examination was also unremarkable. She was a resident of Roorkee, India with an ancestral origin from Pakistan. CBC was done which showed a Hb of 12.1 g/dl. However her red cell indices were microcytic hypochromic with MCV-60.7 fl, MCH-20.3 pg, MCHC-33.4 g/dl, red cell count-5.98 million/μl and RDW-23.4 %. Her total leucocyte count and platelet count were within normal limits.
HPLC and Electrophoresis Analysis
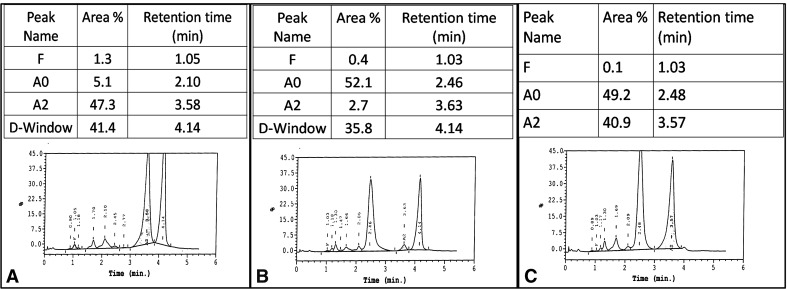
High performance liquid chromatography (HPLC) was done in view of the microcytic hypochromic red cell indices with erythrocytosis. It was performed on the Bio Rad Variant II using beta thalassemia short program. It showed two abnormal Hb peaks, one within the D-window with a retention time (RT) of 4.14 min comprising 41.4 % of the total Hb and the other peak within HbA2 window with a RT of 3.58 min comprising 47.3 % of the total Hb (Fig. 1a). As per Bio Rad Library of Abnormal Hemoglobin version 3 the abnormal Hb in D window is possibly HbD-Punjab and the peak within the HbA2 RT window is most likely due to HbD-Iran or HbE, which elute closest at that position. However HbD-Iran was considered to be a better possibility in view of RT of 3.58 min and the amount of this abnormal Hb to be >40 %. The case was further analyzed on alkaline and acid electrophoresis using SAS-1 alkaline Hb-12 and SAS-1 acid Hb-12 (Helena) respectively.
Fig. 1.
HPLC chromatograms using Bio Rad Variant II beta thalassemia column for the index case (a), mother (b) and father (c)
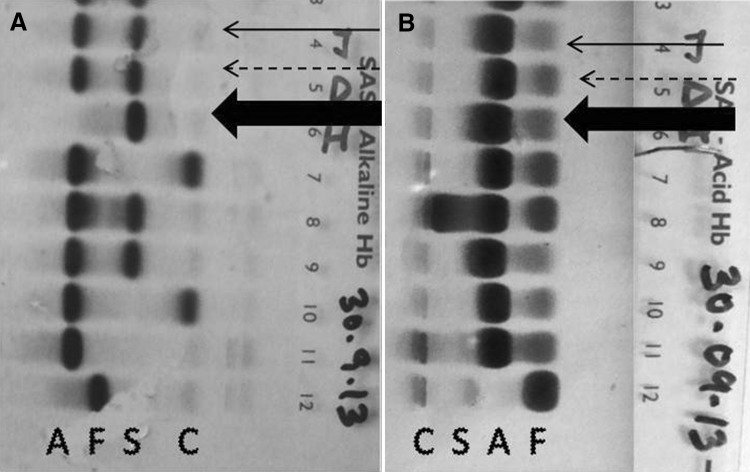
Alkaline electrophoresis of the child showed one major band at S/D/G position with no band at HbA position or at C/E/O position, thereby, further confirming the variant Hb to be HbD and not HbE. The acid electrophoresis showed a single major band at HbA position (Fig. 2). Based on the Hb electrophoresis alone the case could be misdiagnosed as homozygous HbD-Punjab/homozygous HbD-Iran, while actually the child was a compound heterozygote for two abnormal hemoglobins which moved at HbD position. The HPLC together with the electrophoresis helped us to recognize this compound heterozygous state as HbD-Punjab/HbD-Iran.
Fig. 2.
Electrophoresis at alkaline pH (A) and acid pH (B) showing the index case (marked with thick solid arrow), father (dashed arrow) and mother (solid arrow). Lanes 7, 8, 9, 10 were from patients with AE, AS, AD and AE respectively. Lane 11 and 12 are normal adult and cord blood samples respectively
Family studies on the parents including HPLC and electrophoresis at alkaline and acid pH were advised for further characterization.
Father’s CBC was normal and HPLC showed prominent peaks of HbA (49.2 %) with abnormal Hb within HbA2-window (40.9 %) with RT of 3.57 min, likely a heterozygote for HbA/HbD-Iran (Fig. 1b). Alkaline electrophoresis of the father showed two major bands, one at HbA and the other at S/D/G position with no band at C/E/O position further confirming the possibility of heterozygous HbA/HbD. The acid electrophoresis showed one major band corresponding to HbA position (Fig. 2).
Mother’s CBC was also normal and HPLC showed a major peak of HbA (52.1 %) and another peak of an abnormal Hb within the D-window (35.8 %) with RT of 4.14 min, possibly HbD-Punjab. Hence the mother was a possible heterozygote for HbA/HbD-Punjab (Fig. 1c). Alkaline electrophoresis of the mother showed two major bands, one at HbA and the other at S/D/G position with no band seen at C/E/O position. The acid electrophoresis showed one major band corresponding to HbA position (Fig. 2).
Together with the HPLC findings and Hb electrophoresis the father was confirmed to be a heterozygote for HbA/HbD-Iran and the mother to be HbA/HbD-Punjab. The parental HPLCs confirmed the possibility of the child inheriting HbD-Punjab from her mother and HbD-Iran for her father.
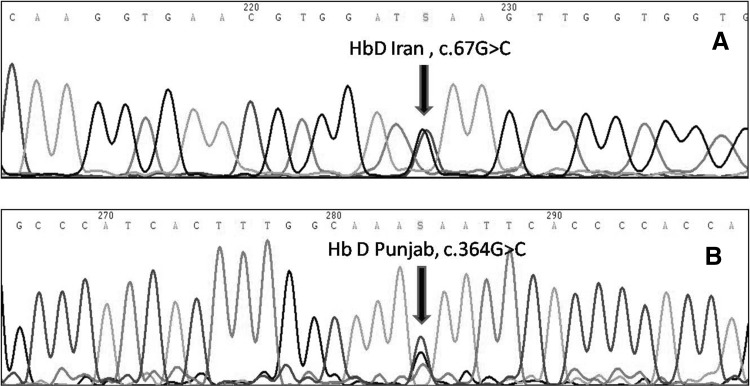
Hence the two techniques, HPLC and electrophoresis contributed in proper recognition of Hb variants. For confirmation of this novel co-inheritance, capillary sequencing (ABI, version 3500) of beta globin gene of the child was done, that confirmed the compound heterozygous state for HbD-Punjab (HBB:c.364G > C) and HbD-Iran (HBB:c.22G > C) (Fig. 3).
Fig. 3.
β-globin gene sequencing of the index case showing mutation for HbD-Punjab and HbD-Iran
Discussion
HbD-Punjab and HbD-Iran are structural Hb variants with point mutation seen at the beta globin chain in both but at different positions. HbD Punjab or Los Angeles [beta 121 (GH4) Glu → Gln] differs structurally from normal HbA as glutamic acid is replaced by glutamine at 121 position on beta chain. HbD-Iran occurs due to replacement of glutamic acid by glutamine at beta 22 (helical residue B4) [3]. To the best of our knowledge co-inheritance of these two Hb variants has not been described. HbD-Punjab has been reported in North-west regions. In the largest series of HbD-Punjab described from North India, the prevalence of HbD-Punjab was ~0.55 % of the total HbHPLCs performed [4]. Prevalence of HbD-Iran in India is not known.
The identification of a Hb variant by HPLC in our laboratory is based on a comparison of its RT, its amount as the percentage of the total Hb and peak characteristics with the Bio-Rad Library of Variants along with the ethnic origin of case. The HPLC performed on the index case showed two major peaks which were identified as HbD-Iran (α2ββ D-Iran) (3.58 min) and HbD-Punjab (α2ββ D-Punjab) (4.14 min).
Thus, the two techniques of HPLC and Hb electrophoresis must be used together for proper recognition of Hb variants. Alkaline and acid electrophoresis of the child alone could have been misdiagnosed as homozygous D-Punjab/HbD-Iran. The centers which still use the electrophoresis as the primary mode to detect abnormal Hb can easily miss the variant described on electrophoresis alone if HPLC had not been done. This is clinically relevant as HbD-Punjab in combination with HbS gives rise to a sickling disorder [5] while a case of HbD-Iran and HbS co-inheritance is a benign sickle cell syndrome [6]. A spousal HbHPLC for this patient should be considered at the relevant time-point and genetic counseling may be required.
The importance of alkaline and acid electrophoresis over and above HPLC underlies the fact that they help us to clearly differentiate HbE from HbD which are the close differential diagnoses seen with a high HbA2 value. The common hemoglobins that elute in A2-window on HPLC include HbE, HbLepore and HbD-Iran among others. HbE is a thalassemic hemoglobinopathy with HbE of ≤30 % in heterozygous state [7] and a RT of ~3.69 min [8]. HbLepore is usually ~15 % in heterozygous state [9] and elutes at RT of ~3.37 min [8]. An uncommon variant observed is HbD-Iran which has a RT of ~3.49 min and an amount of >40 %. While considering the characteristic of a Hb variant, the RT cannot be considered alone as there may be mild variations with different instruments and even on the same instrument over a period of time [8].
The pattern of hemoglobinopathy was further confirmed by beta globin gene sequencing in the index case. However, doing sequencing in every case is not practical as HPLC and alkaline and acid electrophoresis together are sufficient for correct characterization of many abnormal hemoglobins.
The patient’s indices were microcytic hypochromic even though her anemia had responded to iron replacement. This may be accounted for by a co-inheritance of alpha thalassemia or by the compound heterozygosity for HbD-Punjab and HbD-Iran. HbD-Punjab in a heterozygous state has normal RBC indices but in the homozygous state, the indices are thalassemic [5]. Similarly in the present case, the HbD-Punjab/HbD-Iran combination could result in microcytic indices. However, we have not evaluated her for alpha thalassemia and therefore cannot exclude it as a cause of microcytosis.
Conclusion
This to the best of our knowledge is the first case report of a compound heterozygous state for HbD-Punjab/D-Iran from our geographic region. HPLC studies, electrophoresis at alkaline and acid pH and gene sequencing of the beta globin gene were consistent with this interpretation.
Declaration of Interest
The authors report no conflicts of interest
References
- 1.Pauling L, Itano HA, Singer SJ, Wells K. Sickle cell anemia: a molecular disease. Science. 1949;110:543–548. doi: 10.1126/science.110.2865.543. [DOI] [PubMed] [Google Scholar]
- 2.Higgins T, Sachnabl K, Savoy M, Rowe P, Flamini M, Bananda S. A novel double heterozygous, HbD Punjab/HbQ India, hemoglobinopathy. Clin Biochem. 2012;45:264–266. doi: 10.1016/j.clinbiochem.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Sachdev R, Dam AR, Tyagi G. Detection of Hb variants and haemoglobinopathies in Indian population using HPLC: report of 2,600 cases. Indian J Pathol Microbiol. 2010;53:57–62. doi: 10.4103/0377-4929.59185. [DOI] [PubMed] [Google Scholar]
- 4.Srinivas U, Pati HP, Saxena R. Hemoglobin D-Punjab syndromes in India: a single center experience on cation-exchange high performance liquid chromatography. Hematology. 2010;15:178–181. doi: 10.1179/102453309X12583347113735. [DOI] [PubMed] [Google Scholar]
- 5.Bain BJ. Hemoglobinopathy diagnosis. Massachusetts: Blackwell Publishing; 2006. [Google Scholar]
- 6.Serjeant B, Myerscough E, Serjeant GR, Higgs DR, Moo-Penn WF. Sickle cell-Hemoglobin D-Iran: a benign sickle cell syndrome. Hemoglobin. 1982;6:57–59. doi: 10.3109/03630268208996934. [DOI] [PubMed] [Google Scholar]
- 7.Higgs DR, Thein SL, Wood WG. Human haemoglobin. In: Weatherall DJ, Clegg JB, editors. The thalassaemia syndromes. 4. Oxford: Blackwell Science Ltd; 2001. pp. 65–120. [Google Scholar]
- 8.Joutovsky A, Hadzi-Nesic J, MiNardi MA. HPLC retention time as a diagnostic tool for hemoglobin variants and hemoglobinopathies: a study of 60,000 samples in a clinical diagnostic laboratory. Clin Chem. 2004;50:1736–1747. doi: 10.1373/clinchem.2004.034991. [DOI] [PubMed] [Google Scholar]
- 9.Gibbons R, Higgs DR, Olivieri NF, Wood WG. Clinical features of the thalassaemias. In: Weatherall DJ, Clegg JB, editors. The thalassaemia syndromes. 4. Oxford: Blackwell Science Ltd; 2001. pp. 357–392. [Google Scholar]