Abstract
Association between chronic lymphocytic leukemia and other malignancies has been known for a long time. This epidemiological phenomenon is explained by immunosuppression caused by disease itself or by the applied therapy. Merkel cell carcinoma is a rare malignant tumor of the skin of neuroendocrine origin diagnosed almost exclusively in immunocompromised host. We presented an unique case of coexisting infiltration of chronic lymphocytic leukemia cells within primary cutaneous Merkel cell carcinoma and metastatic lymph node in young HIV-negative female patient.
Keywords: Merkel cell carcinoma, Chronic lymphocytic leukemia, Secondary malignancy
Introduction
Association between chronic lymphocytic leukemia (CLL/SLL) and other malignancies has been known for a long time. This epidemiological phenomenon is explained by immunosuppression caused by disease itself or by the applied therapy [1]. Merkel cell carcinoma (MCC) is a rare malignant tumor of the skin of neuroendocrine origin. It usually appears as a solitary, red lump commonly on head and neck and rarely on the extremities. The development of MCC is 11 times more often in HIV-positive patients and five times in patients who underwent solid organ transplantation [2]. MCC has also been reported in patients affected with CLL. Six cases of concomitant MCC have been reported in the group of 4,164 patients with CLL [3]. Infiltration of the same lymph node with two different tumors is relatively rare and thus presents a problem in differential diagnosis.
Case Report
A 45 years old female came to our Institute complaining of a reddish lump of 3 cm in diameter on her right upper arm. She had no other symptoms. According to disease history, she was affected with asymptomatic leukocytosis 3 years ago 20 × 109/L, but without any further diagnostics from her general practitioner at that point of time. Around the same time, she was diagnosed with non functional node in thyroid gland. Familiar history for malignant diseases was negative. At presentation bilateral neck and axillary lymph nodes of around 3 cm were found during the physical examination. The blood tests showed leukocytosis of 84.3 × 109/L with lymphocytosis 77.9 %, hemoglobin level of 157 g/L, platelets 199 × 109/L, elevation of LDH for 1.2 times; other blood test results were within the normal ranges. The results of chest, abdominal and pelvic CT indicated the presence of lymphadenomegaly of 1–3 cm in the neck, axillas, and mediastinum and abdominal lymph node conglomerate of 12 cm in diameter. Patient was HIV-negative. In addition, the resection of upper arm tumor and the biopsy of the right neck lymph nodes were done. Histopathological diagnosis of lymph nodes was CLL/SLL, with immunohistochemical TdT−, CD20++, CD10−, CD5+, CD23++, CD43+, CD38∓, bcl-2+, Cyclin D1−, and Ki 67 5 %. Immunohistochemical analysis of the upper arm lesion showed NSE+, chromogranin A+, EMA−, LCA−, S-100−, CD34−, cytokeratin 7−, cytokeratin 20−, TTF− within the infiltration of CD23, CD5 and CD20 positive CLL cells. This profile established the diagnosis of merkel cell carcinoma within the co-infiltration of CLL/SLL cells (Fig. 1a, b). Bone marrow histopathology showed same morphological and immunohistochemical pattern as CLL/SLL involved lymph node.
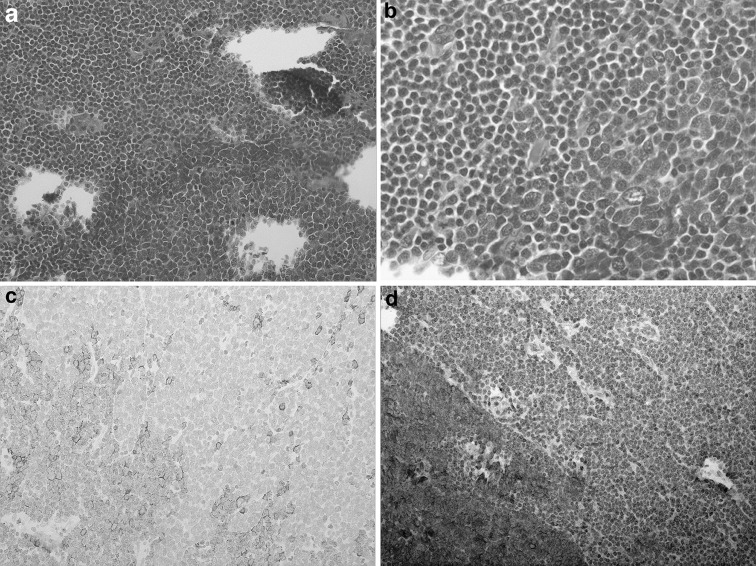
Fig. 1.
a MCC infiltrate in the skin and CLL within the MCC infiltrate (HE 100×), b MCC infiltrate in the skin and CLL within the MCC infiltrate (HE 400×)
The treatment of the patient with CLL/SLL was started with CHOP protocol. After eight cycles of the protocol therapies, partial response was achieved. Treatment was continued with four cycles of FC protocol which resulted in disease complete remission.
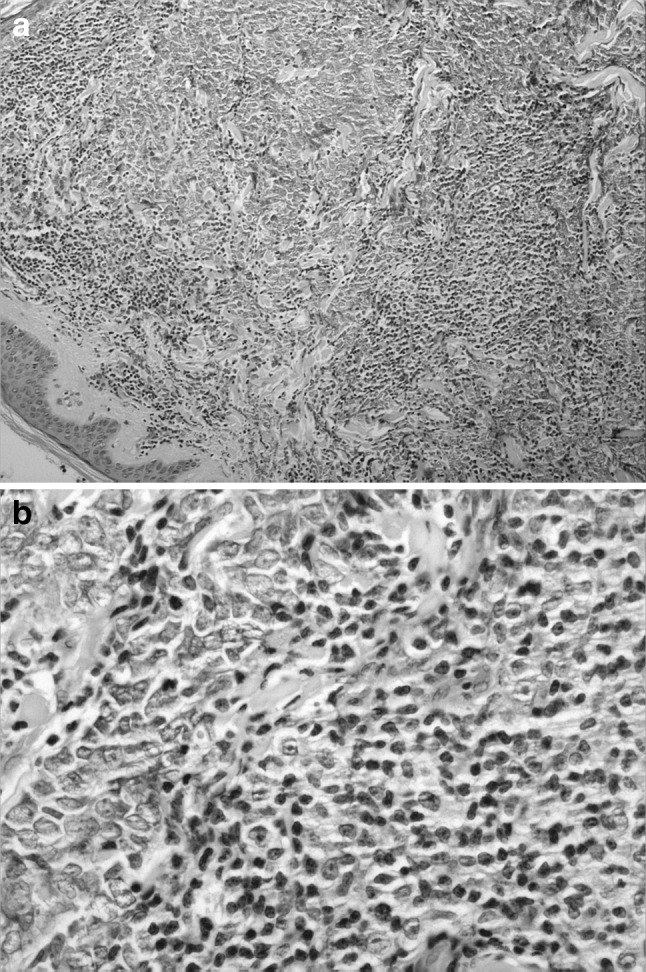
Six months later, bilateral enlarged lymph nodes in the neck and in the right axilla reappeared but with normal blood count: hemoglobin level 141 g/L, leucocytes 7.3 × 109/L with 28 % of lymphocytes and platelets 234 × 109/L. Biopsy of axillary lymph node was performed and the results indicated the infiltration of SLL and Merkel cell carcinoma in the same lymph node (Fig. 2a–d). Immunohistochemical analysis resulted in NSE and Chromogranin positivity of MCC cells and also CD20, CD79alpha, CD5 and CD23 positivity of CLL cells.
Fig. 2.
a HE 100× lymph node upper left CLL, lower right MCC, b HE 400× lymph node upper left CLL, lower right MCC, c Lymph node 200× CD20+ lower left CLL, upper right CD20− MCC, d Lymph node 200× chromogranin A+ lower left MCC, chromogranin A− upper right CLL
We initiated the treatment with the combination of etoposide and cisplatin for MCC and rituximab. A week after treatment initiation fast progression of neck lymph nodes was observed and patient died 1 month later.
Discussion
Merkel cell carcinoma is a rare neoplasm of the skin and most often appears in immunocompromised patients. Consequently, the MCC incidence is higher among HIV-positive individuals, patients who undergo solid organ transplantation, and patients affected with CLL [2, 3]. Recent discovery that MC polyomavirus infection has a role in MCC development gave more support to the statement that MCC is the disease of immunocompromised host [4].
Chronic lymphocytic leukemia causes aberrant immune response and it is associated with frequent infections and appearance of secondary malignancies [1], and occasionally with MCC. Koljonen et al. in the group of 4,164 patients with CLL and 172 patients with MCC found 6 patients had both malignancies [3].
MCC and CLL are diseases that usually affect people of older age and rarely occur in individuals under 50 years of age [2]. In case of our patient diagnosis was established when she was 45 years old. Although there are many publications that report coexistence of CLL and MCC [3, 5–11] the case of our patient was unique due to two reasons. The first was that CLL infiltrate coexisted within the primary skin tumor (MCC). As far as we know, there is only one such case reported in the literature so far, where authors presented a case of 66 years old male with purple tumor of the scalp. A biopsy showed MCC as well as dense aggregates of small lymphocytes within and surrounding the MCC. Immunohistochemistry showed characteristic dot-like cytoplasmic positivity for cytokeratin 20 in the MCC; the lymphocytic infiltrate was positive for CD5, CD20 and CD23, diagnostic of CLL [5]. The infiltrate described in our patient was chromogranin A and NSE positive, within which there was infiltrate of positive cells CD23, CD20, CD5 that morphologically and immunohistochemically corresponded to CLL found in biopsied lymph node and bone marrow. The second reason was that in case of our patient the infiltrate of both malignancies was detected in the same axillar lymph node subsequent to the rebiopsy. There is only one case of concomitant CLL and MCC infiltrate within the same lymph node reported by Pandey et al. 11 years ago. Apart from 82 years old male patient with MCC where unexpected SLL infiltration within lymph node was seen. The second case within the same publication was patient breast cancer with SLL and breast cancer infiltration in lymph nodes after axillary dissection, and third one was the patient with squamous cell carcinoma and unexpected co-infiltration of SLL cells and squamous cell carcinoma cells within 18 lymph nodes after neck dissection [12]. A similar case was detected in mesenteric lymph node of a patient with CLL and colorectal carcinoma [13].
Physicians should be aware of the association of CLL with another malignancy. One of the examples is MCC which is result of Merkel Cell Polyoma virus infection in immunocompromised host, like in patients with CLL. Beacause of elevated risk, patients with CLL should be screened often for secondary malignancy during the course of the disease.
Conflict of interest
None.
Refernces
- 1.Manusow D. Weinerman BH Subsequent neoplasia in chronic lymphocytic leukemia. JAMA. 1975;232:267–269. doi: 10.1001/jama.1975.03250030023012. [DOI] [PubMed] [Google Scholar]
- 2.The Rockville Merkel Cell Group Merkel Cell carcinoma Recent progress and current priorities on etiology pathogenesis, and clinical management. J Clin Oncol. 2009;27:4021–4026. doi: 10.1200/JCO.2009.22.6605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koljonen V, Kukko H, Pukkala E, et al. Chronic lymphocytic leukaemia patients have a high risk of Merkel-cell polyomavirus DNA-positive Merkel-cell carcinoma. Br J Cancer. 2009;101(8):1444–1447. doi: 10.1038/sj.bjc.6605306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feng H, Shuda M, Chang Y, et al. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319:1096–1100. doi: 10.1126/science.1152586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Craig PJ, Calonje JE, Harries M, et al. Incidental chronic lymphocytic leukaemia in a biopsy of Merkel cell carcinoma. J Cutan Pathol. 2009;36(6):706–710. doi: 10.1111/j.1600-0560.2008.01115.x. [DOI] [PubMed] [Google Scholar]
- 6.Cervigón I, Gargallo AB, Bahillo C, et al. Merkel cell carcinoma in a patient with chronic lymphocytic leukemia. Actas Dermosifiliogr. 2006;97(4):264–266. doi: 10.1016/S0001-7310(06)73396-8. [DOI] [PubMed] [Google Scholar]
- 7.Quaglino D, Di Leonardo G, Lalli G, et al. Association between chronic lymphocytic leukaemia and secondary tumours: unusual occurrence of a neuroendocrine (Merkell cell) carcinoma. Eur Rev Med Pharmacol Sci. 1997;1(1–3):11–16. [PubMed] [Google Scholar]
- 8.Ziprin P, Smith S, Salerno G, et al. Two cases of merkel cell tumour arising in patients with chronic lymphocytic leukaemia. Br J Dermatol. 2000;142(3):525–528. doi: 10.1046/j.1365-2133.2000.03370.x. [DOI] [PubMed] [Google Scholar]
- 9.Vlad R, oodlock TW. Merkel cell carcinoma after chronic lymphocytic leukemia: case report and literature review. Am J Clin Oncol. 2003;26(6):531–534. doi: 10.1097/01.coc.0000037108.86294.5E. [DOI] [PubMed] [Google Scholar]
- 10.Robak E, Biernat W, Krykowski E, et al. Merkel cell carcinoma in a patient with B-cell chronic lymphocytic leukemia treated with cladribine and rituximab. Leuk Lymphoma. 2005;46(6):909–914. doi: 10.1080/10428190500057759. [DOI] [PubMed] [Google Scholar]
- 11.Papageorgiou KI, Kaniorou-Larai MG. A case report of Merkel cell carcinoma on chronic lymphocytic leukemia: differential diagnosis of coexisting lymphadenopathy and indications for early aggressive treatment. BMC Cancer. 2005;19(5):106. doi: 10.1186/1471-2407-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandey U, Naraynan M, Karnik U, et al. Carcinoma metastasis to unexpected synchronous lymphoproliferative disorder: report of three cases and review of literature. J Clin Pathol. 2003;56(12):970–971. doi: 10.1136/jcp.56.12.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silvestris N, Zito FA, Fiore MG, et al. Synchronous presentation of B-cell chronic lymphocytic leukemia/small-cell lymphoma and colon adenocarcinoma within the same mesenteric lymph nodes and a single liver metastasis. J Clin Oncol. 2011;29(1):e11–e13. doi: 10.1200/JCO.2010.31.1001. [DOI] [PubMed] [Google Scholar]