Abstract
Hypertriglyceridemia in children can be familial or acquired. Acquired forms of hypertriglyceridemia in children may be associated with several other diseases obesity, diabetes mellitus, uremia/dialysis, hypothyroidism, nephrotic syndrome, drugs etc. Hypertriglyceridemia with β-thalassemia major is an association of unknown pathogenesis which is rarely described in the literature but is important to recognize, for the prevention of complications and proper management of thalassemic children.
Keywords: Thalassemia, Hypertriglyceridemia, HPLC
Introduction
Hypertriglyceridemias are traditionally defined as conditions in which the concentration of triglyceride carrying lipoproteins in plasma exceeds the normal limits (>150 mg/dl). Hypertriglyceridemia may be familial or acquired and reflect increased hepatic synthesis or decreased catabolism [1]. We report a rare association of β-thalassaemia major and hypertriglyceridemia in four cases.
Materials and Methods
All four cases were referred to hematology clinic, MAMC for chronic anemia and hepatosplenomegaly. The age ranged from 11 months to 2 years (average 1.5 years) with male: female ratio of 1:3. Complete hemogram with red cell indices (MCV:MCH ratio), peripheral smear and reticulocyte count were carried out in all the cases. This was followed by high performance liquid chromatography (HPLC) Variant II β thal short programme. Incidentally it was noticed that plasma turned diffusely milky on standing (Fig. 1) so serum lipid profile was obtained.
Fig. 1.
Blood sample showing milky white colour of plasma in a patient of Thalassemia major indicating high lipid content
Results
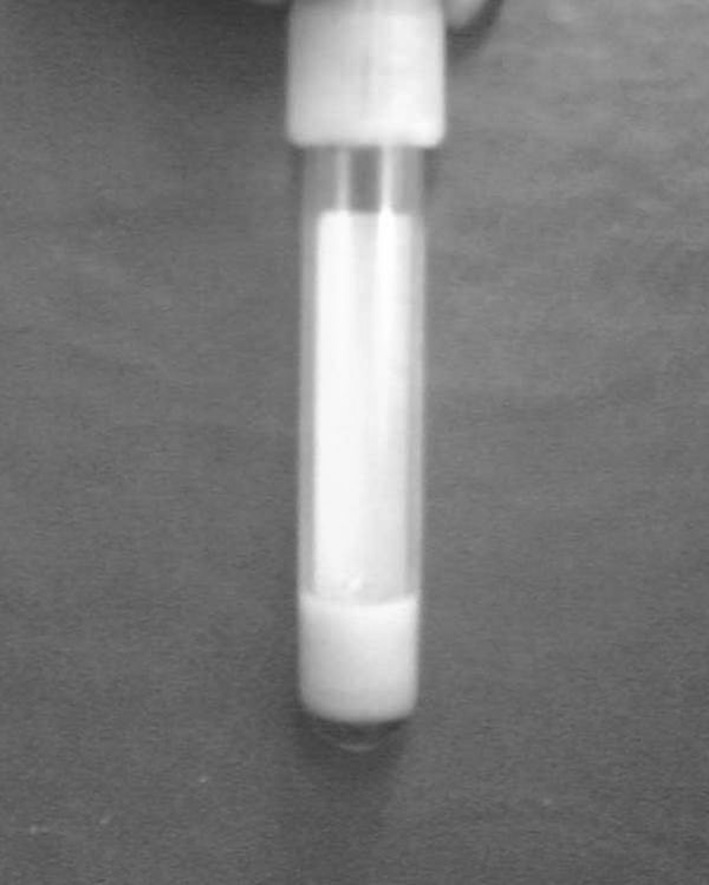
On HPLC all four cases were diagnosed as thalassemia major (Fig. 2a–d). Family studies were carried out which showed both the parents to be thalassemia trait in all four cases. Serum LDL-C, HDL-C and total cholesterol were within normal limits while the triglycerides were found to be markedly raised in all four cases. The values ranged from 800 to 1,400 mg/dl (average 1,050 mg/dl; N = 46–236 mg/dl). Suspecting hyperlipidemia, children were re-examined for xanthomas, corneal arcus or tonsillar hypertrophy which was absent in all of them. Other causes of secondary hypertriglyceridemia, including hypothyroidism and diabetes mellitus, were ruled out with appropriate testing. Neither the mother nor father had laboratory evidence of hyperlipidemia in any of the cases. Results are tabulated in Table 1.
Fig. 2.
HPLC chromatograms in cases of Thalassemia major showing HbF a) 31% b) 94.9% c) 97.6% and d) 112%
Table 1.
Clinical details, hematological parameters and Triglyceride levels in all the four cases
| Parameter | C/C | Age/sex | Hb | MCV/MCH | HbF (%) | HbA (%) | HbA2 (%) | TG levels (mg/dl) |
|---|---|---|---|---|---|---|---|---|
| Patient1 | Chronic anemia Hepatosplenomegaly Poor growth |
11 month/F | 5.9 | 66.9 fL 26.2 pg |
31 | 60.7 | 3.2 | 800 |
| Patient 2 | Pallor Jaundice Hepatosplenomegaly |
2 year/F | 4.2 | 56.7 fL 18.3 pg |
94.9 | 12.2 | – | 1,100 |
| Patient 3 | Severe anemia Failure to thrive |
1.5 year/M | 1.6 | 79.7 fL 19.0 pg |
97.6 | 5.6 | 4.5 | 900 |
| Patient 4 | Anemia Poor growth Splenomegaly |
1.8 year/F | 5.5 | 63 fL 21.4 pg |
112.6 | 6.6 | 3.3 | 1,400 |
Discussion
In β-Thalassemia major, level of HbF is variable depending upon the presence of β0 or β+ mutation. In β0 thalassemia major, almost all the hemoglobin is comprised of HbF and there is no detectable HbA while in β+ thalassemia major, level of HbF varies from 30 to 90 % but in both the instances patient usually presents within first year of life with failure to thrive, poor feeding, intermittent bouts of infection and general malaise, pallor and splenomegaly similar to our first case who presented with pallor, hepatosplenomegaly and poor growth at 11 months of age with microcytic hypochromic indices and marked degree of anisoipoikilocytoisis on peripheral blood smear while HbF levels on HPLC were only 31 %.
There are five groups of Primary lipid disorders according to Frederickson Classification of Dyslipidemias-Type I, IIA,IIB,III,IV,V. The most common dyslipidemias associated with markedly elevated triglyceride levels are are types I, III, IV and V. Type I, type III and V are rare in pediatric patients. Our patients had markedly elevated levels of triglycerides (mean 1,050 mg/dl), while rest of the lipid profile (Total cholesterol, HDL-C, and LDL-C) was normal. Possibility of primary hypertriglyceridemia was ruled out by the presence of absolutely normal lipid profile in parents of all the four children and absence of associated findings of primary hyperlipidemias like tendon and tuberous xanthomas.
A variety of diseases have been linked to secondary hypertriglyceridemia, including infection, renal insufficiency, and diabetic ketoacidosis which were ruled out proper history and clinical examinations along with relevant investigations.
Hypertriglyceridemia may accompany acute, massive hemolysis [2]. The association of thalassemia major with hypertriglyceridemia termed as Hypertriglyceridemia-thalassemia syndrome has been described by some authors in India [3, 4, 5]. Most of these children had presented in the age group of 4 months to 2.5 years. In our study the patients’ age ranged from 11 months to 2 years (average 1.5 years). Though pathogenesis of such association has remained unclear but when present might put the thalassemic children at high risk for developing atherosclerosis and acute pancreatitis at a very early age which can further increase morbidity and mortality in such cases.
Conclusion
We propose that all children suffering from thalassemia major or other conditions associated with massive hemolysis should be screened for abnormal lipid profile especially triglyceride levels, and this entity must be considered in thalassemics as its early detection and appropriate management could help prevent risk of atherosclerosis, myocardial infarction and acute pancreatitis in such children.
References
- 1.Gomber S, Kela K, Rahiman CLA (1996) Hypertriglyceridemia-thalassemia syndrome. Ann Trop Med 16(4):359–360 [DOI] [PubMed]
- 2.Druml W, Grimm G, Laggner AN, Schneeweiss B, Lenz K. Hyperlipidemia in acute hemolysis. Klin Wochenschr. 1991;69:462–492. doi: 10.1007/BF01666827. [DOI] [PubMed] [Google Scholar]
- 3.Rao AV, Bai KI, Ramanujiah D. Hypertriglyceridaemia in thalassaemia major. J Indian Med Assoc. 1972;59:15–17. [PubMed] [Google Scholar]
- 4.Indira BK, Das NS, Subrahmanyam MV, Rama Rao AV. Thalassemia major with hypertriglyceridemia. Indian Pediatr. 1975;12:929–931. [PubMed] [Google Scholar]
- 5.Seervai MH, Merchant SM, Babar ST. Thalassemia major with idiopathic hypertriglyceridemia (type I) Indian Pediatr. 1976;13:623–628. [PubMed] [Google Scholar]