Abstract
OBJECTIVE:
There is no consensus regarding the most appropriate methods (i.e., the side-by-side versus the stent-in-stent technique) for placing bilateral stents for malignant hilar biliary obstructions. We aimed to perform a quantitative review of the published data regarding the clinical efficacy of the side-by-side and stent-in-stent bilateral drainage techniques for hilar biliary obstructions.
METHODS:
A comprehensive search of several databases was conducted and a fixed-effects or random-effects model was used to pool the data from all of the study end-points.
RESULTS:
Four clinical trials were identified. A comparison of the side-by-side and stent-in-stent groups revealed no significant differences with respect to the rates of successful placement, successful drainage, early complications, late complications and stent occlusions. There were also no significant inter-group differences in stent patency and patient survival and no publication bias was observed.
CONCLUSIONS:
The performance of the side-by-side technique appears to be similar to that of the stent-in-stent technique for bilateral drainage in patients with malignant hilar biliary obstructions.
Keywords: Malignant Hilar Obstruction, Biliary Stent, Side-by-Side, Stent-in-Stent
INTRODUCTION
Malignant hilar biliary obstruction, which can be caused by a heterogeneous group of tumors, often has an extremely poor prognosis. Endoscopic biliary stenting is now a well-established palliative treatment modality. The current evidence indicates that the performance of metallic stents is superior to that of plastic stents for hilar tumor palliation with respect to stent patency, repeat drainage rate and patient survival (1,2). Endoscopic biliary drainage of malignant hilar strictures is often more challenging and complex than the management of distal malignant biliary obstructions. However, whether it is more appropriate to perform unilateral versus bilateral stent placements in patients with malignant hilar strictures is a topic of current debate (1). Many studies have suggested that bilateral drainage affords significantly better cumulative stent patency and is associated with a reduced potential of developing cholangitis when compared with unilateral drainage (3). Furthermore, a recent study suggested that draining more than 50% of the liver volume, which frequently requires bilateral stent placements, appears to be an important predictor of drainage effectiveness in malignant hilar strictures (4). In current clinical practice, there are two methods of placing bilateral stents: the side-by-side (SBS) and the stent-in-stent (SIS) techniques (5). The SBS deployment technique results in the simultaneous insertion of two parallel metallic stents to drain the bile ducts of both hepatic lobes (6). In the SIS deployment technique, after placing the first metallic stent across the hilar stricture, a second stent is inserted into the undrained contra-lateral hepatic duct through the mesh of the first stent (7). To date, no consensus has been reached regarding the preferred method, but several comparative studies on this topic have been published recently (8-11). In the current study, we aimed to perform a quantitative review of the published data regarding the clinical efficacy of the SBS and SIS techniques for achieving bilateral drainage for hilar biliary obstructions.
MATERIALS AND METHODS
We searched the Medline (via Pubmed) and Embase databases for all trials that were published between January 1985 and August 2013 comparing bilateral stenting methods in the treatment of malignant hilar biliary obstructions.
Two individuals independently performed the search, then reviewed and extracted the relevant data from each study according to a pre-specified protocol. The following data were extracted and pooled wherever possible: successful insertion, successful drainage, early complications, late complications, rate of stent occlusions during the follow up, stent patency and patient survival. Early complications were defined as those that occurred within 30 days of stent insertion and late complications were defined as those occurring more than 30 days after stent insertion (8,9).
The quality of the randomized and nonrandomized studies was assessed using the Newcastle–Ottawa Scale (12). Study quality was evaluated by examining three items: patient selection, the comparability of the two study groups and the outcome assessments. Studies achieving five or more stars were considered to be of the highest quality.
The hazard ratios (HRs) and 95% confidence intervals (CIs) for stent patency were extracted from papers and/or presentations (13). The weighted mean differences (WMDs) and 95% CIs were calculated for all continuous outcomes, whereas odds ratios (ORs) and 95% CIs were calculated for all dichotomous data. For each outcome, a fixed-effects or random-effects model was used to pool the data according to the results of a statistical heterogeneity test. Heterogeneity between studies was evaluated using χ2 and I2 tests. Publication bias was assessed visually using a funnel plot and it was assessed statistically by means of regression asymmetry tests (i.e., Egger's test (14)) and rank correlation tests (i.e., Begg's test (15)). To minimize type 1 error and reduce the likelihood of false positive results, all analyses were performed using the intention-to-treat method. Two-tailed p-values less than 0.05 were considered to be statistically significant for all analyses.
RESULTS
Study characteristics
The clinical characteristics of the patients in the selected trials are shown in Table 1. A total of four trials were included in the current study (8-11). There were 158 patients included in the meta-analysis and successful bilateral drainage was recorded in 146 (92.4%) of these patients. Out of this study sample, 79 patients received stent placements using the SBS method and 67 received stent placements using the SIS technique. A short follow up of 97 days was performed in the study by Law et al. (9), but most other studies followed patients for the remainder of their lives.
Table 1.
-Characteristics of the included studies.
| Study | N | Gender Male/female | Etiology (cancer) Biliary/gallbladder/others | Bismuth type I/II/III/IV | Study Quality (Star Rating) |
| Law et al. (9) | 24 | 19/5 | 14/4/6 | 0/11/3/10 | ☆☆☆☆ |
| Naitoh et al. (8) | 52 | 25/27 | 18/24/10 | 6/14/9/23 | ☆☆☆☆☆ |
| Kim et al. (11) | 41 | 28/13 | 24/4/13 | 2/11/15/13 | ☆☆☆☆☆☆ |
| Koh et al. (10) | 41 | 41/0 | 26/9/6 | 0/3/26/12 | ☆☆☆☆ |
SBS vs. SIS
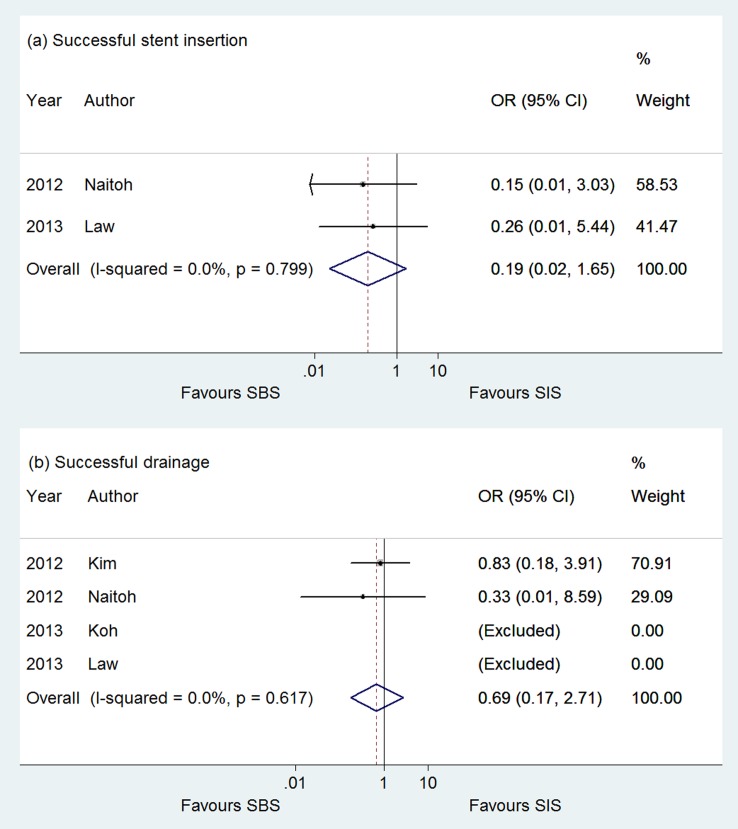
As shown in Figure 1, no significant differences in the successful stent insertion rates were observed between the SBS and SIS groups (OR 0.195; 95% CI, 0.023, 1.652; p = 0.799; 2 studies (8,9); I2 = 0%) (Figure 1a). The two groups did not differ significantly in their rates of successful drainage (OR 0.688; 95% CI, 0.175, 2.71; p = 0.617; 4 studies (8-11); I2 = 0%) (Figure 1b).
Figure 1.
A comparison of the successful stent insertion rate (a) and the successful drainage rate (b) between the SBS and SIS groups.
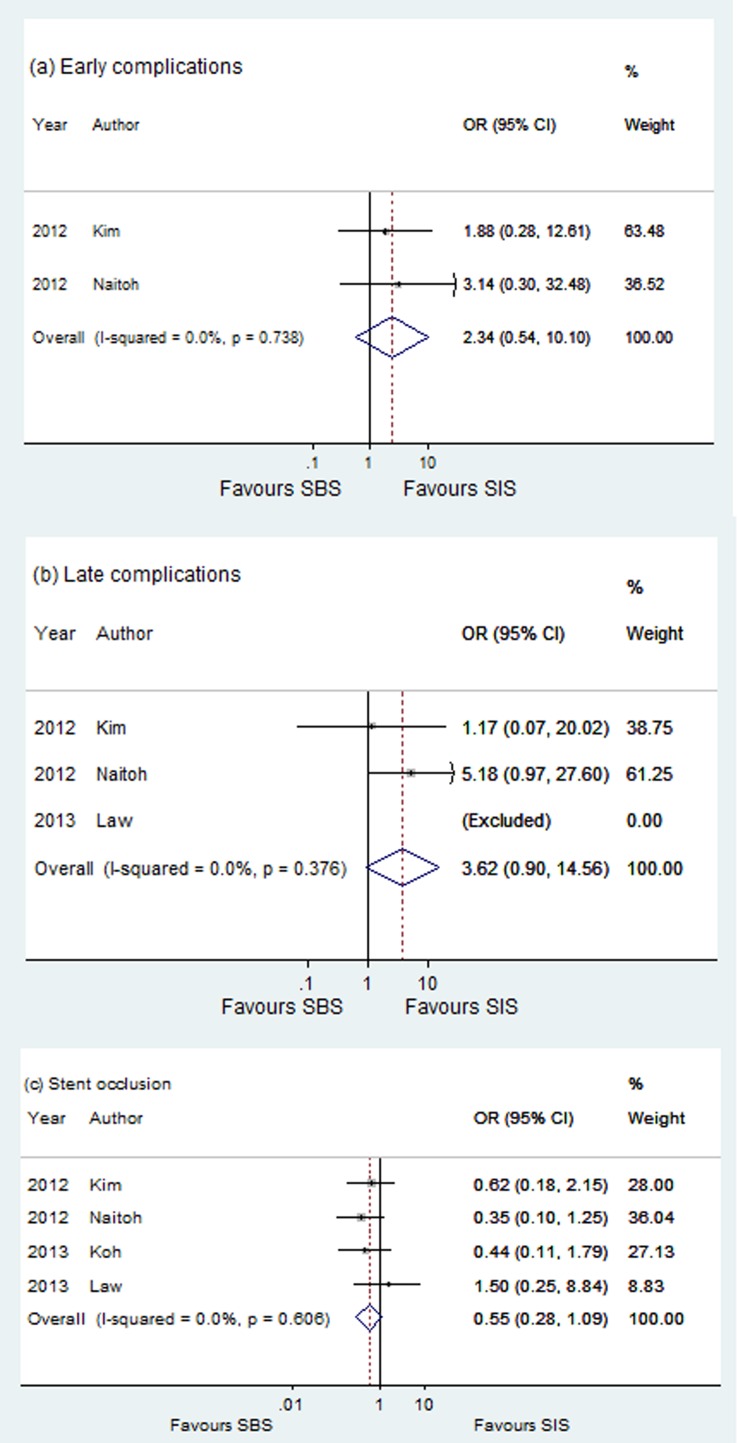
A comparison of the SBS and SIS groups revealed no significant differences with respect to early complications (OR 2.34; 95% CI, 0.54, 10.11; p = 0.738; 2 studies (8,11); I2 = 0%) or late complications (OR 3.62; 95% CI, 0.90, 14.56; p = 0.744; 3 studies (8,9,11); I2 = 0%) (Figures 2a and 2b). During the follow-up period, the stent occlusion rates observed in the SBS and SIS groups were not significantly different (OR 0.554; 95% CI, 0.281, 1.091; p = 0.606; 4 studies (8-11); I2 = 0%) (Figure 2c).
Figure 2.
A comparison of the early complications (a), late complications (b) and stent occlusions (c) between the SBS and SIS groups.
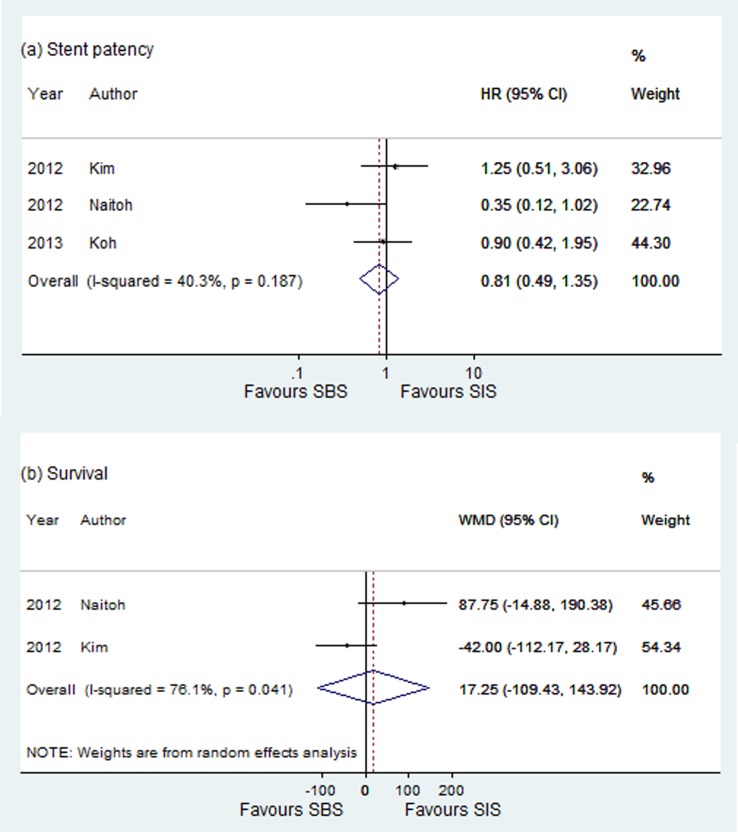
The pooled estimates of the cumulative patency of the stent did not reach statistical significance (HR = 0.811; 95% CI: 0.486, 1.353; p = 0.187; 3 studies (8,10,11); I2 = 40.3%) (Figure 3a). As to overall patient survival, the SBS method was not associated with a statistically significant survival benefit when compared with SIS (WMD = 17.25; 95% CI: -109.426, 143.921; p = 0.790; 2 studies (8,11); I2 = 56.9%) (Figure 3b).
Figure 3.
A comparison of stent patency (a) and patient survival (b) between the SBS and SIS groups.
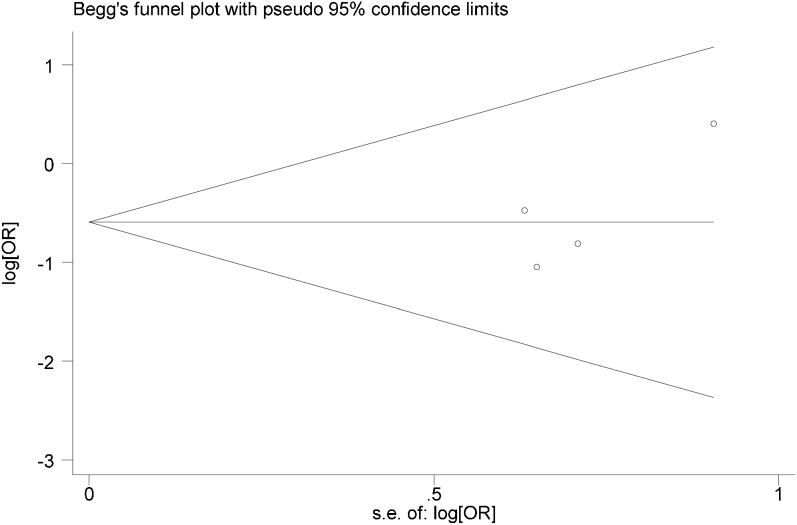
Publication bias
An analysis of publication bias was performed for all study endpoints. Neither Egger's nor Begg's tests provided evidence of publication bias. Figure 4 shows the funnel plot depicting the publication bias analysis of stent occlusion (Egger's test, p = 0.216; Begg's test, p = 0.734).
Figure 4.
Begg's funnel plot for publication bias.
DISCUSSION
Although bilateral stent drainage for malignant hilar biliary obstructions is performed in many academic centers, the deployment of bilateral metal stents can be technically challenging, even for experienced surgeons. The SIS deployment technique is made challenging by the requirement to dilate the wire mesh for the introduction of a second stent and for re-intervention through the mesh at the time of occlusion (16). SBS procedures are limited by difficulties in passing the stricture, guiding the stent through the available delivery shafts and the non-dilated common bile duct. Because of the different limitations of these techniques, Kim et al. (11) recommended that the selection of bilateral stenting methods should be based on the features of each patient, such as the bile duct diameter and the length of the stenotic segments in the hilar region. Law et al. (9) also reported that both techniques are viable and safe but that success using either technique could be dependent on the operator and on proper treatment selection. Our data revealed no significant differences between the SBS and SIS groups with respect to the rates of successful placement or successful drainage. In addition, no heterogeneity was observed. These results are in accordance with the results of several previous comparative studies (8-11).
Cholecystitis, cholangitis, tumor in-growth and tumor over-growth are common complications of bilateral stenting. The stent mesh in the hilar region is often larger for SIS deployments than for SBS deployments, a feature that more easily allows for tumor in-growth. However, SBS deployments often increase the diameter of the bile duct by the parallel stents, thus causing portal vein occlusions (11). The present study revealed no significant differences between these groups with respect to the rate of early complications, late complications or stent occlusions during the follow-up period. In addition, no heterogeneity was observed.
The median stent patency observed in the SIS and SBS procedures ranged from 61 (10) to 155 days (8). The median survival time of patients treated with the SIS and SBS procedures ranged between 38 (10) and 198 days (8). As expected, we also found no significant group differences in stent patency or patient survival. However, it should be emphasized that these findings exhibited marked heterogeneity and should be interpreted with caution. The heterogeneity of our results may result, at least in part, from the fact that different individual trials included different percentages of cholangiocarcinoma. Therefore, in the future, it will be interesting and necessary to analyze stent and patient survival for SIS versus SBS procedures in patients stratified on the basis of the etiology of their hilar biliary strictures.
Although we observed no evidence of publication bias, our meta-analysis has several limitations. For example, the small number of studies that were included and the relatively small number of patients prevented a more robust assessment of heterogeneity and publication bias. In addition, we included one study (11) in which a percutaneous approach to stent placement was used exclusively. Saleem et al. (17) noted that although insertion complications differ when stents are placed percutaneously compared with those placed endoscopically, the method of stent placement does not affect the subsequent stent outcome. Moreover, patients with various disease etiologies were included; hence, this analysis does not differentiate the performance of the SBS versus SIS techniques according to the causes of hilar biliary strictures, thus limiting the generalizability of these results. Finally, although we performed an extensive literature and abstract review to minimize bias in the results, all of the studies examined were observational in design; thus, the assignment of patients to the various interventions is subject to selection bias. In addition, low-quality studies can lead to a distortion of summary effect estimates.
In conclusion, the performance of the SBS technique appears to be similar to that of the SIS method for bilateral drainage in patients with malignant hilar biliary obstructions. Further prospective control trials with larger sample sizes are warranted to confirm our conclusions.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Hong W, Sun X, Zhu Q. Endoscopic stenting for malignant hilar biliary obstruction: should it be metal or plastic and unilateral or bilateral. Eur J Gastroenterol Hepatol. 2013;25(9):1105–12. doi: 10.1097/MEG.0b013e328360b9ec. [DOI] [PubMed] [Google Scholar]
- 2.Hong WD, Chen XW, Wu WZ, Zhu QH, Chen XR. Metal versus plastic stents for malignant biliary obstruction: An update meta-analysis. Clin Res Hepatol Gastroenterol. 2013;37(5):496–500. doi: 10.1016/j.clinre.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Kim DU, Kang DH, Kim GH, Song GA, Kim CW, Kim S, et al. Bilateral biliary drainage for malignant hilar obstruction using the ‘stent-in-stent' method with a Y-stent: efficacy and complications. Eur J Gastroenterol Hepatol. 2013;25(1):99–106. doi: 10.1097/MEG.0b013e3283590a2a. [DOI] [PubMed] [Google Scholar]
- 4.Vienne A, Hobeika E, Gouya H, Lapidus N, Fritsch J, Choury AD, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010;72(4):728–35. doi: 10.1016/j.gie.2010.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Dumonceau JM, Heresbach D, Deviere J, Costamagna G, Beilenhoff U, Riphaus A. Biliary stents: models and methods for endoscopic stenting. Endoscopy. 2011;43(7):617–26. doi: 10.1055/s-0030-1256315. [DOI] [PubMed] [Google Scholar]
- 6.Saleem A, Baron TH, Gostout CJ. Large-diameter therapeutic channel duodenoscope to facilitate simultaneous deployment of side-by-side self-expandable metal stents in hilar cholangiocarcinoma. Gastrointest Endosc. 2010;72(3):628–31. doi: 10.1016/j.gie.2010.04.035. [DOI] [PubMed] [Google Scholar]
- 7.Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc. 2010;71(1):195–9. doi: 10.1016/j.gie.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Naitoh I, Hayashi K, Nakazawa T, Okumura F, Miyabe K, Shimizu S, et al. Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci. 2012;57(12):3279–85. doi: 10.1007/s10620-012-2270-9. [DOI] [PubMed] [Google Scholar]
- 9.Law R, Baron TH. Bilateral metal stents for hilar biliary obstruction using a 6Fr delivery system: outcomes following bilateral and side-by-side stent deployment. Dig Dis Sci. 2013;58(9):2667–72. doi: 10.1007/s10620-013-2671-4. [DOI] [PubMed] [Google Scholar]
- 10.Koh E, Jin GY, Hwang SB, Choi EJ, Song JS, Han YM, et al. A Comparison of Y-Type and T-Type Metallic Bilateral Biliary Stents in Patients with Malignant Hilar Biliary Obstruction. J Korean Soc Radiol. 2013;68:297–303. [Google Scholar]
- 11.Kim KM, Lee KH, Chung YH, Shin JU, Lee JK, Lee KT, et al. A comparison of bilateral stenting methods for malignant hilar biliary obstruction. Hepatogastroenterology. 2012;59(114):341–6. doi: 10.5754/hge11533. [DOI] [PubMed] [Google Scholar]
- 12.Wells G, Shea B, O′Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2012 http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 13.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–34. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 14.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 16.Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010;72(3):632–6. doi: 10.1016/j.gie.2010.04.037. [DOI] [PubMed] [Google Scholar]
- 17.Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011;74(2):321–327. e1–3. doi: 10.1016/j.gie.2011.03.1249. [DOI] [PubMed] [Google Scholar]