Abstract
OBJECTIVE:
To describe the profile of physicians working at the Prehospital Emergency Medical System (SAMU) in Brazil and to evaluate their quality of life.
METHODS:
Both a semi-structured questionnaire with 57 questions and the SF-36 questionnaire were sent to research departments within SAMU in the Brazilian state capitals, the Federal District and inland towns in Brazil.
RESULTS:
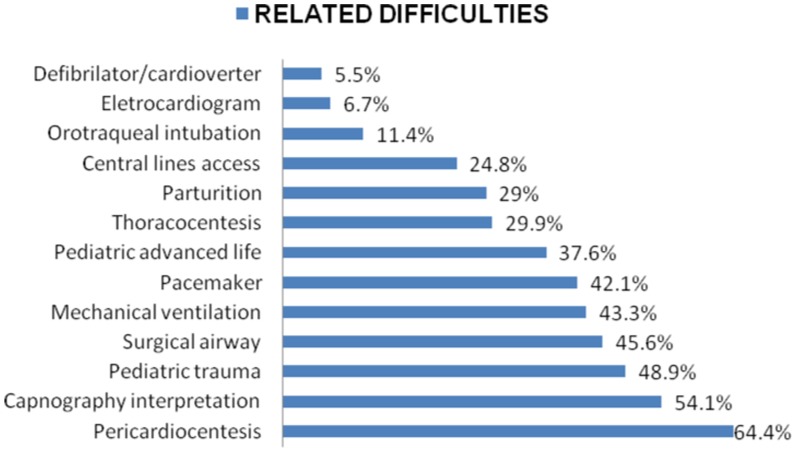
Of a total of 902 physicians, including 644 (71.4%) males, 533 (59.1%) were between 30 and 45 years of age and 562 (62.4%) worked in a state capital. Regarding education level, 45.1% had graduated less than five years before and only 43% were specialists recognized by the Brazilian Medical Association. Regarding training, 95% did not report any specific training for their work at SAMU. The main weaknesses identified were psychiatric care and surgical emergencies in 57.2 and 42.9% of cases, respectively; traumatic pediatric emergencies, 48.9%; and medical emergencies, 42.9%. As for procedure-related skills, the physicians reported difficulties in pediatric advanced support (62.4%), airway surgical access (45.6%), pericardiocentesis (64.4%) and thoracentesis (29.9%). Difficulties in using an artificial ventilator (43.3%) and in transcutaneous pacing (42.2%) were also reported. Higher percentages of young physicians, aged 25-30 years (26.7 vs 19.0%; p<0.01), worked exclusively in prehospital care (18.0 vs 7.7%; p<0.001), with workloads >48 h per week (12.8 vs 8.6%; p<0.001), and were non-specialists with the shortest length of service (<1 year) at SAMU (30.1 vs 18.2%; p<0.001) who were hired without having to pass public service exams* (i.e., for a temporary job) (61.8 vs 46.2%; p<0.001). Regarding quality of life, the pain domain yielded the worst result among physicians at SAMU.
CONCLUSIONS:
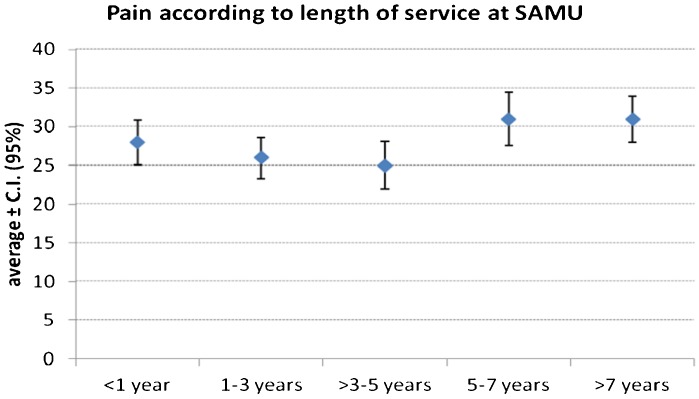
The doctors in this sample were young and within a few years of graduation, and they had no specific training in prehospital emergencies. Deficiencies were mostly found in pediatrics and psychiatry, with specific deficiencies in the handling of essential equipment and in the skills necessary to adequately attend to prehospital emergencies. A disrespectful labor scenario was also found; the evaluation of quality of life showed a notable presence of pain on the SF-36 among physicians at SAMU and especially among doctors who had worked for a longer length of time at SAMU.
Keywords: Emergency Medicine, Mobile Units, Role of Physician, Emergency Medical System
INTRODUCTION
Prehospital emergency care improves morbimortality as well as the social consequences of morbidity and mortality (1,2). Despite the different models of prehospital assistance in different countries, overall, the qualifications of the professionals involved are a major concern. In addition to improving care, these qualifications have an important impact on cost effectiveness (3,4).
The revision of the Brazilian National Policy for Urgent Care (PNAU) set standards for the organization of public services and defined its components, including the Prehospital Emergency Medical System (SAMU) (5). This service provides out-of-hospital acute medical care, transport to definitive care facilities and other medical transport to patients in Brazil who have illnesses and injuries that prevent the patients from transporting themselves.
At SAMU, physicians provide care in all medical specialties, interfacing with urgent care and still acting as health authorities within the system. The physicians thus establish a gateway for and early management of health care resources. The doctor has two roles within the service: to manage the ambulance service and to decide the patient's destination (6).
Therefore, given the importance of the physician within the service, a model of professional qualifications and continuing education, with indicators for the evaluation of its current state of efficiency, would be expected. Although very few studies have been conducted in this area, certain studies have indicated deficiencies in the technical training of professionals, in the efficient operation of the NEUs and in the current model of qualification of professionals (7-12).
This model, which is associated with precarious employment arrangements, generates high turnover within the service and the lack of clear qualification requirements for entry into the service may compromise the quality of care.
No centralized official data on the social, demographic and professional aspects of the quality of life of these providers are provided by the Ministry of Health or other competent entities. Currently, SAMU serves more than 137 million people in Brazil (13). Considering the essential role of SAMU's physicians and the lack of information on their features (qualifications for emergency situations, time since graduation, qualifications for and training in emergency procedures, workload, employment contract, current difficulties in performing tasks and aspects of quality of life), a study was undertaken to delineate the physicians' social, demographic, professional and quality-of-life profile.
MATERIALS AND METHODS
A 12-month cross-sectional study (August 2012 to August 2013) was conducted at the Centers for Teaching and Research (NEPs) at SAMU in 21 state capitals and in cities in the states of São Paulo, Paraná, Minas Gerais, Ceará and Maranhão. This study was approved by the Medical Ethics Committee of the Federal University of São Paulo - School of Medicine of the State of São Paulo (CEP No. 103.291). The work included elaboration of a social, demographic and professional profile and evaluation of the quality of life of the physicians working at the Mobile Emergency Care Service in Brazil. In the first phase, a commission was established to generate a semi-structured questionnaire to determine the profile. This commission was composed of the principal investigator, a physician who is a coordinator at SAMU, an interventionist physician and a regulatory physician with ten years of experience within the service and a graduate and post-graduate medical professor. The elaboration of the questionnaire, which contained 57 questions, was completed by the committee in June 2012. In the second phase, a pre-test was administered to SAMU's physicians to assess their understanding and acceptance of the questionnaire. We then excluded certain terms and possible ambiguities were corrected. In the third phase, all of SAMU's and the NEPs' medical coordinators from all state capitals and the Federal District were contacted. In the fourth phase, 2,400 questionnaires and consent forms, in separate sealed envelopes, were sent, divided among the 27 state capitals according to information on the average number of physicians in each local service. Additionally, over 1,000 questionnaires were sent to cities that had agreed to participate that were not capitals of the states of Ceará, Minas Gerais, São Paulo, Maranhão and Paraná. The coordinators then distributed the questionnaires and the FPIC forms to physicians; all physicians working at SAMU were included. Afterward, the coordinators returned the completed questionnaires by mail. Only questionnaires that were more than 80% complete and accompanied by a signed FPIC form were considered. We received 974 questionnaires and a total of 902 questionnaires were considered as acceptable for evaluation. In particular, we received valid questionnaires from all regions, from 21 state capitals, and from the Federal District. The translated and validated quality-of-life questionnaire SF-36, or the “Medical Outcomes Study 36-Item Short-Form Health Survey,” was also sent (14,15).
Analyses were performed using SPSS 10.0 software for Windows (SPSS, Chicago, IL). The numerical values are presented as the mean ± the SD of the mean, except when otherwise specified. Significance was set at p≤0.05. The data were analyzed using the chi-square test for categorical variables and Student's t-test for continuous variables. Additionally, for comparison among categories, analysis of variance (ANOVA) was used.
RESULTS
The demographic, social and labor characteristics of the profile are shown in Table 1.
Table 1.
Descriptive characteristics of the profile of the physicians who work at SAMU.
| N | % | |
| Male | 644 | 71.4 |
| 30-45 years of age | 533 | 59.1 |
| Live in a state capital | 562 | 62.4 |
| Workload of 24-48 h | 520 | 57.7 |
| Only work in prehospital care | 106 | 11.8 |
| Regulator or interventionist | 507 | 56.2 |
| Length of service at SAMU <3 years | 425 | 47.2 |
| Entered after passing a test | 502 | 55.7% |
| Monthly earning of 2-8,000 reais | 659 | 73% |
| ≤5 years since graduation | 496 | 45.01% |
| Specialist (Brazilian Medical Association) | 388 | 43% |
| Attended training courses at SAMU | 45 | 5% |
| Number of advanced procedures performed over 24 h | 8.76 | |
| Pleased at SAMU | 578 | 64.4% |
| No training in urgent care after graduation | 442 | 49.1% |
| Total | 902 | 100.0 |
The profile shows a predominance of males, which does not reflect the current trend of increased female participation in the profession (17). Regarding age, 54% of all physicians were less than 35 years old and a significant distribution of physicians under 30 was observed in inland towns (28.5 vs 20.6%; p<0.01).
Regarding the major skills necessary for prehospital procedures, difficulties were found in obtaining surgical access to airways and in performing thoracentesis, pericardiocentesis, deliveries and pediatric advanced support procedures (Figure 1).
Figure 1.
The major deficiencies in procedures and equipment handling in prehospital care.
The doctors were asked about their own capabilities in prehospital emergency care (Table 2).
Table 2.
General skills in emergency care.
| EMERGENCIES | N | YES | % | NO | % |
| Do you have any difficulties in PEDIATRICS assistance in prehospital care? | 902 | 387 | 42.1 | 515 | 57.9 |
| Do you have any difficulties in SURGICAL assistance in prehospital care? | 902 | 380 | 42.9 | 522 | 57.1 |
| Do you have any difficulties in PSYCHIATRIC assistance in prehospital care? | 902 | 516 | 57.2 | 386 | 42.8 |
| Do you have any difficulties in CARDIORESPIRATORY assistance in prehospital care? | 902 | 651 | 27.3 | 244 | 72.7 |
When the characteristics of the physicians from the capitals were compared with the characteristics of the physicians from inland towns, we found a significant difference in the time since graduation (>5 years: capital, 68.9% vs inland, 41.3%; p<0.001), in involvement in the specialties recognized by the Ministry of Education and Culture (MEC) (16) (capital, 46.2% vs inland, 38%; p<0.01) and in the percentage of physicians older than 35 years of age (capital, 47.3% vs inland, 45.3%; p<0.016). Regarding medical specialties, the majority were surgeons (69.0%), whereas clinical specialties accounted for 25.5% and all others accounted for 5.5%. Regarding training courses, 45.6% of physicians had attended courses that offered international certification and methodology. For example, 64.9% of physicians in the study attended a course on advanced cardiac life support (ACLS) and 57.8% completed a course on advanced trauma life support). Importantly, of the physicians who graduated more than 12 years ago, only 22.3% had attended training courses within the last three years.
For the labor profile, we observed that only 11.8% of physicians working at SAMU solely worked in prehospital care, with a higher percentage located inland (capital, 7.7% vs inland, 18.0%; p<0.001) and 88.2% worked in this field as a complementary activity in their professional life. The physicians who worked exclusively in prehospital care demonstrated a higher level of professional unpreparedness in their self-evaluations compared with those who did not work exclusively at SAMU (exclusive contract with SAMU, 21.1% vs non-exclusive, 2.8%; p<0.004). These physicians were also associated with a greater precarization of labor relations via contracts for emergencies (exclusive contract with SAMU, 25.5% vs non-exclusive, 18.6%; p<0.001) and with a lower incidence of specialists (exclusive contract with SAMU, 48% vs non-exclusive, 65%; p<0.001). The most common workload was 24-48 h per week, as reported by 57.7% of the physicians, whereas the shortest workloads (<24 h) were found among the physicians from the capitals (capital, 24.1% vs inland, 15.2%; p<0.001).
In the present study, 55.7% of physicians had passed a test to obtain their job; this finding may have been influenced by the data for capitals (capital, 61.8% vs inland, 46.2%; p<0.001). The remaining physicians worked under different regimens (e.g., Brazilian Consolidation labor laws, including CLT regulation, emergency contracts and autonomous worker systems). What is notable are the percentages of physicians who had passed a test to obtain work in Rio de Janeiro (97%) and in São Paulo (87%). Within the sample, the physicians who had passed an exam were more likely to be rooted in the service (for more than 3 years) that those who had not taken a public service exam (those who passed the exam and worked for >3 years, 68.4% vs others who worked for >3 years, 29.6%; p<0.001) and were also more likely to be specialists recognized by the Brazilian Medical Association. Among the physicians with medical emergency contracts, the majority were younger, or <30 years of age (44.2 vs 11.8% among those who passed the exam; p<0.001). Regarding the permanence of SAMU's physicians, we found that 51.4% of physicians had 3 or more years of activity in the service, with a significantly increased length of stay (>3 years) among the physicians from the capitals (capitals, 20.0% vs inland towns, 13.4%). This index was highly influenced by the data from the capital cities of São Paulo and Rio de Janeiro, where 54 and 48% of all physicians, respectively, had more than 5 years of experience at SAMU. In this population, there was a higher percentage of physicians who were specialists (specialists >3 years, 67.7% vs <3 years, 32.3%; p<0.001).
Among the physicians in the sample, 64.1% reported being satisfied with their work at SAMU and the majority of these physicians were from inland towns (capitals, 57.2% vs inland towns, 76.1%; p<0.001). Low pay was the main reason for dissatisfaction (63%) and other reasons were as follows: a lack of a career plan, 49.9%; poor working conditions, 24.7%; and an excessive workload while on service, 35.9%.
When only physicians with specialties were considered, a significant difference was observed in favor of medical specialists compared with those attending to surgical emergencies (76.3 vs 65.2%; p<0.001) for performing thoracentesis (76.4 vs 65.2%; p<0.001) and obtaining central venous access (78.9 vs 72.4%; p<0.02).
Regarding the equipment used, transcutaneous pacing was handled with difficulty by 36% of the physicians in the study. The main difficulty in handling equipment was related to artificial ventilators, as 43.3% indicated difficulties in mechanical ventilation.
In the areas of the quality-of-life scale, it was observed that, on average, the area with the highest score was functional capacity (87.5), whereas the area with the lowest score was the pain domain (27.8%). Particularly among physicians with more than 5 years of work at SAMU (1-3 years vs >7 years; p<0.009), a similar difference in social aspects was observed (3-5 years vs >7 years; p<0.018).
DISCUSSION
The physician working at SAMU must be able to attend to emergencies in internal medicine, psychiatry, surgery, trauma, pediatrics, obstetrics and gynecology. The Centers for Emergency Medical Education are organized as “interinstitutional spaces of education, training, qualification and continuing education of human resources for emergencies.” In the case of physicians, the policy estimates a workload of 120 h for their training. It was observed that a small number of physicians attended a training course specifically for their prehospital work at SAMU, with dual functions being very common in the service.
We found that 49.1% of physicians did not attend training for prehospital care or for trauma after their graduation, a phenomenon that has also been observed in other countries (17). This finding is inconsistent with the national syllabus guidelines for medical courses, which require training in the following: “clinical and surgical procedures indispensable for ambulatory care and early care of emergencies and urgencies in all phases of the life cycle” (18,19).
Many physicians in the sample took courses providing international certification, which confirms the National Policy for Urgent Care's observation of widespread proliferation of private companies that offer training courses that are distinct from the national reality of SUS.
Regarding training, although it is mentioned in the emergency policy, no specific medical training or program is being offered for continuing education in prehospital care in this system. Therefore, deficiencies in care, equipment handling and skills essential to practice are present.
Regarding the labor profile, a small number of physicians in the sample worked exclusively in prehospital care, and a large number of physicians had short lengths of service and poor employment arrangements. These findings suggest poor adherence and demonstrate the transitory nature of SAMU in the physicians' professional lives. However, physicians with longer lengths of service, most of whom had experienced stability at work, represented those who were most dissatisfied with SAMU. Regarding the practice of care at SAMU, the most prevalent cases were those in internal medicine, which are mainly cardiovascular in nature (20-27). In fact, in our sample, 27.3% of physicians mentioned difficulties in cardiovascular disease care.
Prehospital care for trauma patients may affect mortality (28-32). This concept is particularly relevant to children, for whom trauma is the major cause of morbidity and mortality in developed countries, accounting for 13.0% of all transportation of severely injured patients and for 10% of prehospital care (33). The physicians who work at SAMU also provide pediatric care and therefore need to master advanced support procedures. One study recommended intensive training for this type of care and reported frequent weaknesses in its implementation (34,35). In the present series, 51.1% of physicians were considered unprepared for pediatric trauma care, 34.9% reported difficulty in assessing pediatric symptomatology, and 62.4% were unprepared for advanced life support procedures. However, no difference was observed when we considered the responses of physicians with specialties recognized by the Brazilian Medical Association. Another skill required for working at SAMU is being able to handle the equipment used in prehospital care (36-39), the use of which is mandatory for advanced support service in ambulances. In particular, transcutaneous pacing was handled with difficulty by 36% of physicians in our study, whereas 94.5% did not have difficulties in handling a cardioverter-defibrillator. The most difficult equipment to handle was the artificial ventilator, as 43.3% of physicians indicated difficulties in introducing and maintaining mechanical ventilation. Additionally, we did not find references to specific training in the sampled physicians' answers to the questionnaire.
Regarding the mental health care provided by SAMU, one study (40) referred to SAMU as a body controller and a keeper of the social order, as its main strategy is physical restraint (41). The fact that the regulatory physician usually sends an ambulance for basic life support contributes to this inappropriate care. In such a situation, an unprepared professional can take inappropriate actions, based on prejudices related to the subject in psychological distress. In contrast, the presence of low-skilled, poorly prepared professionals with respect to mental health can lead to abuse of psychotropic drugs, which in turn can lead to toxicity, with serious consequences for the patient. A degree of negligence is also present regarding the proposal of the National Policy for Mental Health about the concept of beds for comprehensive care for mental health. Based on this proposal, generally, health institutions and the network of mental health have to jointly offer integral care to the patient in crisis, using the services available across the network through the mechanisms of reference and counter-reference to avoid psychiatric hospitalization (42-43). However, in the current study, 42.7% of physicians working at SAMU did not consider themselves to be prepared for mental health care or psychiatric emergencies.
Studies on the medical profession in Brazil have shown dissatisfaction and stress perception among physicians, who consider their medical activities tiring due to long hours and poor working conditions, double shifts, low pay, their specific professional responsibilities, their specific practice/specialty areas, change in the doctor-patient relationship, conflicts with the population, and a loss of autonomy within the profession (44-45). However, studies on the quality of life of physicians have primarily been conducted on those who are still being trained (46-49). In the current study, the SF-36 (50-51) was administered to physicians. The results for the quality-of-life scale showed that, on average, the area with the highest score was functional capacity (87.5%) and that the area with the lowest score was pain (27.8%). Higher pain scores more frequently were found among physicians with more than 5 years of work experience at SAMU compared with physicians with less than 5 years of work at SAMU (1-3 years vs >7 years; p<0.009) (Figure 2). A similar difference in social aspects was also observed (3-5 years vs >7 years; p<0.018). The few Brazilian studies on the prevalence of chronic pain were conducted in specific populations, such as the elderly and in the outpatient setting (52). One population-based study (53) on 2,550 adults found that chronic pain was present in 41% of the population. However, no studies have compared the prevalence of chronic pain in medical and non-medical populations in Brazil. In the present study, quality of life generally improved among physicians from inland towns in comparison with those from the state capitals, but no significant differences in quality of life were observed when general practitioners were compared with specialists.
Figure 2.
Graph showing the distribution of pain among physicians with different lengths of service at SAMU.
Limitations of the study
This study has limitations in its sampling design. First, it was not possible to produce a probability sample; rather, our sample was a convenience sample, which is a feature that limits our conclusions. Second, a related limitation was how difficult it was to access the managers who administered the questionnaire to obtain a profile of the physicians working at SAMU. Third, a degree of concern about the possible revelation of deficiencies not only among the participating physicians but also in the management and provision of services was observed. Thus, certain state capitals did not participate in the study and did not justify their absence, despite numerous attempts to contact them. A fourth limitation of this study is the construction of the tool for evaluation of the profile. In particular, several possible biases may have existed in the development of the semi-structured questionnaire. Therefore, we formed a commission to prepare both the questionnaire and a pre-test with a sample of physicians. However, intrinsic biases of the tool remain.
The profile of the doctors who work in the prehospital medical system in Brazil is as follows: predominantly male (71.4%), aged between 30 and 45 years (59.1%) and living in state capitals (62.4%). However, there is a great heterogeneity in the physicians' prehospital profile in Brazil. Many physicians have less than 5 years of work experience since graduation (45%), without any previous experience as undergraduates or previous training. Many also have precarious employment relationships and lack a medical specialty, particularly in the inland cities.
Deficiencies in training and care were also observed, showing the need for better arrangements to ensure quality in the system.
Moreover, after an evaluation of quality of life using the SF-36 questionnaire, the increased presence of pain in this profession was observed.
Footnotes
*In Brazil, to work as civil servant and achieve work stability, an individual has to pass an exam.
No potential conflict of interest was reported.
REFERENCES
- 1.World Health organization (WHO) Geneva: 2007. Prehospital trauma care system [internet] [cited Dec, 10; 2013]. Available: http://.Who.int/violence injury_prevention/publications/services/39162_oms_new.pdf. [Google Scholar]
- 2.Knowles E, Mason S, Colwell B. An initiative to provide emergency healthcare for older peaple in the comunity: the impact on carers. Emerg Med J. 2011;28(4):316–9. doi: 10.1136/emj.2009.084616. [DOI] [PubMed] [Google Scholar]
- 3.Snooks HA, Kingston MR, Anthony RE, et al. Wich extended paramedic skills are making an impact in emergency care and can be related to the UK paramedic system? A systematic review of the literature. Emerg Med J. 2013 doi: 10.1136/emermed-2012-202129. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruston AA, Tavabie AA. Na evaluation of a training placement in general practice for paramedic practioner students: improving patiente-centred care through greater interprofessional understeding and supporting the development autonomous practioners. Qual Prim Care. 2011;19(3):167–73. [PubMed] [Google Scholar]
- 5.Brasil. Ministério da saúde. Portaria n° 1864, de 29 de setembro de 2003b. Institui o Componente pré-hospitalar móvel da PNAU - o SAMU. Publicada no diário oficial da nação no dia 06 de outubro de 2003, seção 1, p.72-3, coluna 1 [Google Scholar]
- 6.Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Regulação Médica das Urgências. Brasília: Ministério da Saúde, 2006 (Serie A. Normas e Manuais Técnicos) :29. [Google Scholar]
- 7.O'Dwyer G, Matta IEA, Pepe VLE. Avaliação dos serviços hospitalares de emergência do estado do Rio de Janeiro. Ciência e Saúde Coletiva. 2008;13(5):1637–48. doi: 10.1590/s1413-81232008000500027. [DOI] [PubMed] [Google Scholar]
- 8.O'Dwyer G. Mattos RA. SAMU, a regulação no Estado do Rio de Janeiro e a integralidade segundo gestores de três níveis de governo. Physis Revista de Saúde Coletiva. 2012;22(1):141–60. [Google Scholar]
- 9.Chomatas M. Integração de saberes e práticas na organização do SAMU de Curitiba - PR. Divulg Saude Debate. 2005;2:90–5. [Google Scholar]
- 10.Assis SG, Deslandes SF, Minayo MCS. Vol. 2007. Rio de Janeiro: Fiocruz; Prevenção, monitoramento, capacitação e pesquisa. In: Minayo MCS, Deslandes SF, organizadores. Análise diagnóstica da Política Nacional de Saúde para redução de acidentes e violências; pp. 193–218. [Google Scholar]
- 11.Machado CV, Salvador FGF, O'Dwyer G. O Serviço de Atendimento Móvel de Urgência no Brasil: uma análise da política nacional. Revista de Saúde Pública São Paulo. 2011;45(3):519–28. doi: 10.1590/s0034-89102011005000022. [DOI] [PubMed] [Google Scholar]
- 12.Ciconet RM, Marques GQ, Lima MAD. Educação em serviço para profissionais de saúde do Serviço de Atendimento Móvel de Urgência (SAMU): relato de experiência de Porto Alegre - RS. Interface. 2008;12:659–66. [Google Scholar]
- 13.Rede nacional SAMU 192. Disponível em: http://www.portal.saude.gov.br >. Acesso em: 1 de agosto 2013. [Google Scholar]
- 14.Ciconelli RM. Tradução para língua portuguesa e validação do questionário genérico de avaliação da qualidade de vida SF-36 (Brasil SF-36) Rev Bras Reumato. 1999;39(3):143–50. [Google Scholar]
- 15.Ware JE, Kosinski M, Gandek B. Lincoln, RI: Quality Metric Incorporated; 2003. SF-36 Health Survey: Manual & Interpretation Guide. [Google Scholar]
- 16.Demografia médica no Brasil Volume 2 cenários e indicadores de distribuição. Perfil e distribuição dos médicos especialistas. Capítulo. 7:p 135. Disponível em: URL: http://www.cremesp.org.br/pdfs/DemografiaMedicaBrasilVol2.pdf. [Google Scholar]
- 17.Merlin MA, Moon J, Krimmel J, Liu J, Marques-Baptista A. Improving medical students' understanding of prehospital care through a fourth year emergency medicine clerkship. Emerg Med J. 2010;27(2):147–50. doi: 10.1136/emj.2008.066654. [DOI] [PubMed] [Google Scholar]
- 18.Brasil. Ministério da Educação. Conselho Nacional de Educação. Câmara de Educação Superior. Resolução n.4, CNE/ CES de 7/11/2001. Institui diretrizes curriculares nacionais do curso de graduação em medicina. Diário Oficial da União. Brasília, 9 nov. 2001;Seção 1, p.38. Disponível em: URL: http://portal.mec.gov.br/cne/arquivos/pedf/ CES04.pdf. [Google Scholar]
- 19.Almeida MJ, Pereira LA, Turini B, Nicoletto SCS, Campos JJB, Rezende LR, et al. Formação dos profissionais de saúde no Paraná e a implantação das diretrizes curriculares nacionais. [Paraná]; 2005. (Relatório final do projeto de pesquisa financiado pelo CNPq n.47.4029/2003-4). [Google Scholar]
- 20.Clemmensen P, Schoos MM, Lindholm MG, Ramussen LS, Steimetz J, Hesselfeldt R, et al. Pre-hospital diagnosis and transfer of patients with acute myocardial infarction - a decade long experience from one of Europe's largest STEMI networks. J Eletrocardiol. doi: 10.1016/j.jelectrocard.2013.07.004. [internet] 2013 Aug 9 [acesso em 2013 set 20]; Disponível em: http://www.jecgonline.com/article/S0022-0736(13)00355-5/fulltext. [DOI] [PubMed] [Google Scholar]
- 21.Morrison LJ, Rac VE, Bowen JM, Schwartz B, Ryan W, Zahn C, et al. Prehospital evaluation and economic analysis of different coronary syndrome treatment strategies–PREDICT–rationale, development and implementation. BMC Emerg Med [internet] 11(4) doi: 10.1186/1471-227X-11-4. 2011 Mar 29 [acesso em 2013 21] [aproximadamente 6 p.] Disponível em: http://www.biomedcentral.com/content/pdf/1471-227X-11-4.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu JR, Moser DK, Riegel B, McKinley S, Doering LV. Impact of prehospital delay in treatment seeking on in-hospital complications after acute myocardial infarction. J Cardiovasc Nurse. 2011;26(3):184–93. doi: 10.1097/JCN.0b013e3181efea66. [DOI] [PubMed] [Google Scholar]
- 23.Berguland A, Svensson L, Sjostrand C, Von Arbin M, Von Euler M, Wahlgren N, et al. Higher prehospital priority level of stroke improves thrombolysis frequency and time to stroke unit: the Hyper Acute STroke Alarm (HASTA) study. Stroke. 2012;43(10):2666–70. doi: 10.1161/STROKEAHA.112.652644. [DOI] [PubMed] [Google Scholar]
- 24.Evenson K, Foraker R, Morris D, Rosamond W. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke. 200;4(3):187–99. doi: 10.1111/j.1747-4949.2009.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kue R, Steck A. Prehospital diagnosis and management of patients with acute stroke. Emerg Med Clin North Am. 2012;30(3):617–35. doi: 10.1016/j.emc.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, et al. Prehospital Delay in Patients With Acute Coronary Syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103(5):598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 27.Levis JT, Koskovich M. Ability of First-Year Paramedic Students to Identify ST-Segment Elevation Myocardial Injury on 12-Lead Electrocardiogram: A Pilot Study. Prehosp Desaster Med. 2012;25(6):527–32. doi: 10.1017/s1049023x00008712. [DOI] [PubMed] [Google Scholar]
- 28.Tazarourte K, Caesareo E, Sapir D, Atchabahian A, Tourtier JP, Briole N, et al. Update on prehospital emergency care of severe trauma patients. Ann Fr Anesth Reanim. 2013;32(7):477–82. doi: 10.1016/j.annfar.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Hampton DA, Fabricant LJ, Differding J, Diggs B, Underwood S, Dela Crua D, et al. Prehospital intravenous fluid is associated with increased survival in trauma patients. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S9–15. doi: 10.1097/TA.0b013e318290cd52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bulger EM, Guffey D, Guyette FX, Macdonald RD, Brasel K, Kerby JD, et al. Impact of prehospital mode of transport after severe injury: A multicenter evaluation from the Resuscitation Outcomes Consortium. Trauma Acute Care Surg. 2013;72(3):567–803. doi: 10.1097/TA.0b013e31824baddf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butler DP, Anwar I, Willett K. Is it the H or the EMS in HEMS that has an impact on trauma patient mortality. A systematic review of the evidence. Emerg Med J. 2010;27(9):692–701. doi: 10.1136/emj.2009.087486. [DOI] [PubMed] [Google Scholar]
- 32.Shah M, Cushman J, Davis C, Bazarian J, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: An analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12(3):269–76. doi: 10.1080/10903120802100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LaRocco BG, Wang HE. Intraosseous infusion. Prehosp Emerg Care. 2003;7(2):280–5. doi: 10.1080/10903120390936950. [DOI] [PubMed] [Google Scholar]
- 34.Seid T, Ramaiah R, Grabinsky A. Pre-hospital care of pediatric patients with trauma. Int J Crit Illn Inj Sci. 2012;2(3):114–20. doi: 10.4103/2229-5151.100887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Möller JC, Ballnus S, Kohl M, Göpel W, Barthel M, Krüger U, et al. Evaluation of the performance of general physicians in pediatric emergencies: Obstructive airway diseases, seizures, and trauma. Pediatr Emerg Care. 2002;18(6):424–8. doi: 10.1097/00006565-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Macnab AJ, Susak L, Gagnon FA, Alred J, Sun C. The cost-benefit of pulse-oximeter use in the prehospital environment. Preohosp Disaster Med. 1999;14(4):245–50. [PubMed] [Google Scholar]
- 37.Hedges JR, Feero S, Shultz B, Easter R, Syverud SA, Dalsey WC. Prehospital transcutaneous cardiac pacing for symptomatic bradicardia. Pacing Clin Eletrophysiol. 1991;17(7):647–52. doi: 10.1111/j.1540-8159.1991.tb04068.x. [DOI] [PubMed] [Google Scholar]
- 38.Hatlestad D. The benefits of electricity: transcutaneus pacing in EMS. Emerg Med Serv. 2002;31(9):38–44. [PubMed] [Google Scholar]
- 39.Baurer K. Prehospital airway management: high tech meets trauma: an air medical perspective. Crit Care Nurs Q. 2012;35(3):281–91. doi: 10.1097/CNQ.0b013e3182542eb5. [DOI] [PubMed] [Google Scholar]
- 40.Bonfada D, Guimarães J. Serviço de atendimento móvel de urgências e as urgências psiquiátricas. Psicologia em estudo. 2012;17(2):227–36. [Google Scholar]
- 41.Venturini E. A qualidade do gesto louco na época da apropriação e da globalização. In P. Amarante (Org.), Arquivos de Saúde Mental e Atenção Psicossocial. 2003:157–184. Rio de Janeiro: Nau. [Google Scholar]
- 42.Portaria SNAS/MS INAMPS n° 224, de 29 de janeiro de. 1992 Brasil, Ministério da saúde. [Google Scholar]
- 43.Estabelece diretrizes e normas para o atendimento em saúde mental Diário Oficial da União 1994;30 jan [Google Scholar]
- 44.Brasil, Ministério da Saúde Saúde mental no SUS: acesso ao tratamento e mudança no modelo de atenção, relatório de gestão 2003-2006. :40. (2007). Brasília, DF: Autor. [Google Scholar]
- 45.Martins LAN. Saúde mental dos profissionais de Saúde. Rev Bras Trab. 2003;1(1):56–68. [Google Scholar]
- 46.Brasília (DF): Conselho Federal de Medicina. 2002 “O médico e o seu trabalho” - Aspectos metodológicos e resultados do Brasil. [Google Scholar]
- 47.Macedo PCM. São Paulo: Universidade Federal de São Paulo, Escola Paulista de Medicina; 2004. Avaliação da qualidade de vida em residentes de medicina da UNIFESP-EPM [tese] [Google Scholar]
- 48.Lourenção LG, Moscardini AC, Soler ZA. Saúde e qualidade de vida de médicos residentes. Rev Assoc Med Bras. 2010;56(1):81–91. doi: 10.1590/s0104-42302010000100021. [DOI] [PubMed] [Google Scholar]
- 49.Asaiag PE, Perotta B, Martins MA, Tempski P. Quality of life, daytime sleepiness, and burnout in medical residents. Rev Bras Educ Med. 2010;34(3):422–9. [Google Scholar]
- 50.Bolzam MEO. Estresse, coping, burnout, sintomas depressivos e hardinessem residentes médicos. [tese]. Santa Maria(RS): Centro de Ciências em Saúde, Universidade Federal de Santa Maria. 2012 [Google Scholar]
- 51.Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53(1):46–50. doi: 10.1136/jech.53.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ware JE, Sherbourne CD. The MOS 36 Item Short-Form Healt Survey (SF-36) I. Conceptual framework and item selection. Med Care. 1992 Jun. 30(6):473–83. [PubMed] [Google Scholar]
- 53.Sá K, Baptista AF, Matos MA, Lessa I. Prevalência de dor crônica e fatores associados na população de salvador, Bahia. Ver. Saúde Pública. 2009;43(4) doi: 10.1590/s0034-89102009005000032. [DOI] [PubMed] [Google Scholar]