Abstract
The diagnosis, Posttraumatic Stress Disorder, was introduced in 1980 amidst debate about the psychiatric toll of the Vietnam War. There is controversy, however, about its central assumption that potentially traumatic stressors are more important than personal vulnerability in causing the disorder. We tested this assumption with data from a rigorously diagnosed male subsample (n = 260) from the National Vietnam Veterans Readjustment Study. Combat exposure, pre-war vulnerability, and involvement in harming civilians or prisoners were examined, with only combat exposure proving necessary for disorder onset. While none of the three factors proved sufficient, estimated onset reached 97% for veterans high on all three, with harm to civilians or prisoners showing the largest independent contribution. Severity of combat exposure proved more important than pre-war vulnerability in onset; pre-war vulnerability at least as important in long-term persistence. Implications for the primacy of the stressor assumption, further research, and policy are discussed.
The diagnosis, Posttraumatic Stress Disorder (PTSD), was introduced in the 1980 Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-III) (American Psychiatric Association, 1980) amid debate about the psychiatric toll of the Vietnam War (e.g., Friedman, Keane, & Resick, 2007). The new diagnosis described a novel syndrome of intrusive, avoidance/numbing, and arousal symptoms as the distinctive psychopathology following exposure to traumatic stressors. PTSD is unusual among psychiatric diagnoses in that it requires a putative main cause, “Criterion A” stressor exposure, among its indicators. In DSM-III-R (American Psychiatric Association, 1987) which was used to make the diagnoses in the present research, the description of Criterion A emphasizes events that threaten the life or physical integrity of the individual or someone close to him or her, and also includes witnessing death or serious injury to others.
The role of Criterion A stressors is spelled out in the current DSM-IV as follows:
The severity, duration, and proximity of an individual’s exposure to the traumatic event are the most important factors affecting the likelihood of developing this disorder. There is some evidence that social supports, family history, childhood experiences, personality variables, and preexisting mental disorders may influence the development of Posttraumatic Stress Disorder. This disorder can develop in individuals without any predisposing conditions, particularly if the stressor is especially extreme (American Psychiatric Association, 1994, pp. 426–427, italics added).
Stressor exposure in DSM-III through IV was assumed, in and of itself, to be capable of producing underlying disturbance that resulted in persistent symptoms. As Friedman (2005) put it, “Armed with this diagnosis…, we have begun to appreciate the profound and sometimes irreversible changes produced by overwhelming stress. These include fundamental alterations in perception, cognition, behavior, emotional reactivity, brain function, personal identity, world view, and spiritual beliefs” (Friedman, 2005). The implication is that the Criterion A stressor exposure itself can produce the underlying disorder that is manifested by symptoms that are far from transient.
This formulation of the role of the stressors differs from that of the DSM-I diagnosis of its forerunner that followed World War II, which was called “Gross Stress Reaction,” and was grouped under a broader heading of “Transient Personality Disorder” (American Psychiatric Association, 1952, page 40). This 1952 formulation was carried over to to DSM-II (American Psychiatric Association, 1968) and emphasized “reactions [that] differ from those of neurosis and psychosis chiefly with respect to clinical history, reversibility of the reaction” (American Psychiatric Association, 1952, page 40). The reactions were thought to be transient in persons with “good adaptive capacity;” if they persisted after the stressful exposure lessened, this was evidence of “a more severe underlying disturbance (American Psychiatric Association, 1952, p. 48). The implication is that symptom responses to traumatic events will usually be transient unless the exposed individuals had prior vulnerabilities such as a previous history of serious psychiatric disorders.
The assumption that Criterion A stressors are the primary causes of the disorder has become a center of controversy. There are arguments over whether Criterion A should be broadened or narrowed or done away with altogether (Brewin, Lanius, Novac, Snyder, & Galea, 2009; Maier, 2007; McNally, 2003; Weathers & Keane, 2007). Some critics have argued that predisposing personal vulnerability factors contribute more to the development of the disorder than does exposure to traumatic events (e.g., Breslau, 2002; Yehuda and McFarlane, 1995). War-zone stressors in Vietnam, whose U.S. veterans’ re-adjustment problems gave rise to the diagnosis, are included in this generalization by Yehuda and McFarlane (1995). They cite data on the prevalence of PTSD from the most important psychiatric investigation of U.S Vietnam veterans, the National Vietnam Veterans Readjustment Study (NVVRS). However, their critique does not adequately consider the fact that there are often marked individual differences in “severity, duration, and proximity of an individual’s exposure to the traumatic event” (American Psychiatric Association, 1994, p. 426) and corresponding dose-response differences in rates of the disorder (Dohrenwend, 1998).
The novel symptom criteria for the diagnosis of PTSD in DSM III through IV, like the stressor Criterion A, have also been grouped into alphabetically designated types: Criterion B (intrusive symptoms), Criterion C (avoidance/numbing symptoms) and Criterion D (symptoms of arousal). We refer to the required co-occurrence and duration (at least one month) of B, C, and D as the PTSD symptom syndrome, abbreviated here as PSS. Fortunately, the clinical examinations for the diagnosis of PTSD in a subsample of veterans from the NVVRS were conducted so that all PTSD symptoms were rated for all veterans regardless of whether the clinician judged that the veteran had experienced a Criterion A stressor in Vietnam. It is possible, therefore, to assess the presence or absence of PSS independently of the presence of Criterion A stressors that are needed for the full PTSD diagnosis. Our purpose is to use measures of PSS, personal vulnerability and combat stressors obtained from the NVVRS (Kulka et al., 1990), or constructed by us from the NVVRS interview data and military records, to investigate the primacy of the stressor assumption. In doing so, we will take into account involvement in harm to civilians and prisoners in a type of war that was new for this generation of Americans. It has been described as a “war amongst the people” (Smith, 2007), in which it was often hard to distinguish civilians from enemy combatants, and as a “war without fronts” (Thayer, 1985), where the body count of presumed enemy dead became a substitute for the taking of territory as an indicator of military success (Nelson, 2008; Turse, 2008).
We will ask and seek answers to three main questions:
Were Criterion A combat stressors, i.e. exposures that meet Criterion A specifications (e.g., life threatening combat experiences) necessary for the onset of war-related PTSD symptom syndrome (PSS) defined as meeting Criteria B through D? Alternatively, was it possible for a veteran to experience PSS onset based on his general experience in Vietnam without having experienced one or more Criterion A combat stressors?
Are there specific types or severities of Criterion A combat stressors that were sufficient for the onset of war-related PSS?
What were the effects of pre-Vietnam vulnerability factors and harming civilians or prisoners during service in Vietnam on the onset and adverse course of war-related PSS?
This last question is the most complex and bears directly on the relative importance of exposure and personal vulnerability in the development of PTSD. To assess the claim that vulnerability factors contribute more than Criterion A exposure in the war-zone to the development of the disorder, we must first define in operational terms what it might mean to “contribute more.” We will address the question in three ways. First, exposure will contribute more if its effect on war-related PSS with vulnerability controlled is greater than the effect of vulnerability with exposure controlled. Second, exposure will contribute more if the effect of vulnerability diminishes or disappears at very high levels of exposure—levels “that would evoke significant symptoms of distress in almost anyone” (DSM-III, p. 236). In other words, we would expect a negative interaction between combat exposure and vulnerability. Finally, if as suggested by previous research (e.g., Laufer, Gallops & Frey-Wouters, 1984), personal involvement in harm to civilians or prisoners is found to be strongly related to PTSD, we can investigate whether such harm showed a stronger association with combat exposure than with vulnerability. If so, this would be another indication of the greater importance of exposure compared with vulnerability in the development of the disorder.
Method
Data Sources and Participants
The National Vietnam Veterans Readjustment Study (NVVRS) was conducted 11 to 12 years after the war by the Research Triangle Institute (RTI) in response to a Congressional mandate to investigate PTSD and other psychological problems in U.S. Vietnam veterans (Kulka et al., 1990). Our focus is on veterans subsampled from the 1,200 member NVVRS sample of males who served in the Vietnam theater of operations (Theater veterans) during the period of the war from 1965 to 1975. The tours were typically for one year.
The subsample consisted of 260 Theater veterans who came from 28 Standard Metropolitan Regions (SMRs), including the 15 largest. Unlike other veterans in the full sample, the veterans in the subsample received diagnostic examinations by experienced, doctoral level clinicians using the Structured Clinical Interview for DSM-III-R Diagnoses (SCID) (Spitzer, Williams, & Gibbon, 1987). As with the full sample, the completion rate was well over 80%. Suitably weighted, the demographic distribution of subsample veterans is very similar to that in the full 1,200 member sample, except that it does not include veterans from rural areas (Dohrenwend et al, 2007).
Five veterans from minority backgrounds other than Black and Hispanic are removed as too few to analyze. Relevant data on PTSD status or information about sampling weights was missing for three more, and they are also omitted.
Only four of the remaining subsample veterans had first onsets of PTSD that occurred prior to their service in Vietnam. These are too few to provide a basis for evaluating whether pre-war PTSD increased vulnerability to war-related PTSD, and these four veterans are, therefore, also omitted from the analyses. The subsample for the analyses consequently consists of the remaining 248 male veterans of the Vietnam War who did or did not have first onsets of PTSD that were war-related. As in the larger sample, Blacks and Hispanics were oversampled. Reflecting this oversampling of these two minorities, the racial/ethnic composition of the now 248-member subsample is 70 Black, 84 Hispanic, and 94 majority white veterans.
War-related first onsets of PTSD and their adverse course as “current” PTSD
To investigate questions about the primacy of the stressor in symptom onset as well as adverse course, it is necessary to be able to distinguish between the two. Onset requires establishing the presence of the PTSD symptom syndrome (PSS) for at least a month; adverse course requires the assessment of the persistence or recurrence of the syndrome over much longer periods of time after onset. Fortunately, the detailed diagnostic histories that were obtained from the intensively studied subsample of veterans in the NVVRS make it possible to differentiate between onset of war-related PTSD and, broadly, its subsequent course.
The SCID interviews were conducted by 28 doctoral level clinicians 11 to 12 years after the end of the war in 1975. They made the diagnoses according to then current DSM-III-R criteria. The diagnostic examinations were tape-recorded, and staff psychiatrists and psychologists on the RTI study team reviewed every interview to check the adequacy of the data elicited on PTSD. The clinicians also conducted an independent reliability check of the diagnoses of current and lifetime PTSD on a subsample of 30 of the taped clinical interviews. These checks found the quality of the data on PTSD to be excellent and inter-rater reliability for the diagnoses of current and lifetime PTSD as measured by kappa to be .87 and .94, respectively (Weiss et al., 1992, p. 371).
The basic distinction called for in the SCID module for each PTSD symptom was between “lifetime” (i.e., whether it occurred or not during the veteran’s lifetime) and, if lifetime, whether the symptom was current (present at any time during the past six months). The clinician then ascertained whether the symptoms recorded occurred together for at least a month in sufficient numbers and types to meet criteria for current (syndrome present for one month or more of the last six months) or lifetime but not current (syndrome not present in the last six months, but present in criteria-meeting combination for at least one month before then) (Schlenger, 1987).
We used additional information to establish whether a PTSD diagnosis was war-related. For each criterion stressor identified, the clinicians asked about whether it occurred prior to, during, and/or following military service. For respondents who met lifetime criteria for PTSD, the clinicians also asked about the date of initial onset of PTSD and diagrammed the course of the disorder on a chart divided into the pre-event, event, and post-event periods in the veterans’ lives. If there were subsequent traumatic events, these and the course of PTSD symptoms that coincided with them were also diagrammed. For the present research, all of this information was used to establish whether the first onset of PTSD for the subsample respondents was related to their service in Vietnam, and to determine for whom in this group war-related PTSD was current and for whom it had remitted. Only four veterans in the subsample had first onsets of PTSD that occurred prior to their service in Vietnam. As noted above, these are omitted from the present investigation.
As noted earlier, all veterans in this subsample were asked about PTSD symptoms related to Vietnam regardless of whether the clinician believed that Criterion A was met. When the clinician judged that none of the Vietnam-related stressors reported qualified for Criterion A according to DSM-III-R, the clinician nevertheless asked about each PTSD symptom with reference to the veteran’s experience in Vietnam in general (Schlenger, 1987). This convention makes it possible to determine the presence or absence of a war-related symptom syndrome (PSS) consisting of the requisite numbers of intrusive, avoidance/numbing, and arousal symptoms (Criteria B, C and D), whether or not the clinician judged that the respondent had experienced a Criterion A exposure while in Vietnam. This information enabled us to test whether Criterion A stressors were necessary for the occurrence of the symptom syndrome (PSS).
Combat Exposure
For use in much of our previous research with the NVVRS, we constructed a measure of probable severity of combat exposure based on military records and historical accounts that are independent of the veterans’ recall of their war-zone experiences (Dohrenwend et al., 2004; 2006; 2008). This military-historical measure (MHM) shows a strong dose-response relationship with PTSD (Dohrenwend et al., 2006). While free of recall bias and indicating a general context of probable exposure, the MHM does not provide information about the veteran’s personal war zone experiences. For example, the MHM does not describe his involvement in injuring or killing enemy combatants, whether he was wounded, or his possible experiences with harm to prisoners or civilians, any of which may have contributed to the development of PTSD symptoms (e.g., Grossman, 1995; Laufer, Brett, & Gallops, 1985; McNair, 2002; Maguen et al., 2009; Yager, Laufer & Gallops, 1984). It makes sense, therefore, to use measures carefully constructed on the basis of self reports in combination with the MHM to develop comprehensive measures of stressful war-zone experiences. The following is an account of the record-based measures including the MHM and the self-report measures of combat exposure.
Record-based measures of combat exposure and construction of the MHM
Data extracted in the NVVRS from personnel files (“201 files”) for the purpose of designing and drawing the NVVRS sample (Kulka et al., 1988; 1990) facilitated construction of a new measure of probable severity of exposure from recently available records and historical accounts (e.g., Coffelt, Arnold, & Argabright, 2002). Foremost among these is the MHM mentioned above, which has been described in detail elsewhere (Dohrenwend et al., 2004; Dohrenwend et al., 2006; Dohrenwend et al., 2007). In brief summary, the composite military historical measure (MHM) consists of four categories ranging from probable very high to probable low severity of exposure. Veterans in the high and very high categories typically had high exposure military occupational specialties (MOSs), served in large military units with high casualty rates measured by killed in action (KIA), and served at times of high American KIA rates; men in the very high category were further distinguished by having served in smaller units (e.g., companies) that suffered 10 or more KIAs during their tour in Vietnam. By contrast, veterans in the low exposure category typically had low exposure MOSs, served in large units (e.g., divisions) with low KIA rates, served at times of low KIA rates, and were in small units with no KIAs during their Vietnam service. The remaining veterans in the moderate exposure category differed from those in the low exposure category mainly in that most served in Vietnam when KIA rates were moderate or high rather than low.
In addition to the MHM, the military record provides another piece of information that serves as an indicator of direct personal exposure—namely, whether the veteran received a Purple Heart for being wounded.
Self-report measures of combat exposure
The main NVVRS interview was called the National Survey of the Vietnam Generation (NSVG). The NSVG included items on traditional combat with the enemy and also items on whether the veteran witnessed or participated in harm to prisoners and civilians (Kulka et al. (1988, Appendix C). We have used NSVG items to develop four measures of combat exposure: 1) a scale of life threatening experiences, 2) whether the respondent witnessed the death of a close friend in his unit, 3) whether he killed enemy personnel, and 4) whether he experienced betrayal involving life threat (usually in the form of friendly fire).
Scale of life threatening experiences
This is a scale of intensity of exposure to life-threatening combat with the enemy based on the veteran’s reports of frequency of involvement in 11 types of war-zone situations: 1) Received incoming fire from enemy artillery, rockets and/or mortars. 2) Received sniper fire and/or sapper attacks. 3) Unit (patrol) engaged the Vietcong, guerrilla or unidentified troops in a firefight. 4) Received small arms fire from the enemy. 5) Unit (patrol) encountered anti-personnel weapons such as land mines, booby traps. 6) Unit (patrol) engaged the North Vietnamese Army or other organized forces in a firefight. 7) Unit (patrol) was ambushed. 8) Had to do particularly dangerous tasks (e.g., walk point, check out bunkers or tunnels). 9) Vehicle, aircraft or boat in which you were traveling was disabled by enemy fire. 10) Cut off/separated from your unit in hostile territory. 11) Experienced hand-to-hand combat. Respondents were asked how often they had each of the 11 experiences described—very often, often, sometimes, rarely or never. They were given concrete definitions of these terms, ranging from “weekly or more” to “experience did not occur.”
Following the questions about these 11 situations, the respondents were asked a general question: “In your opinion, how often were you in danger of being killed or wounded in (or around) Vietnam? Would you say Very Often (more than 50 times), Often (13–50 times), Sometimes (3–12 times), Rarely (1–2 times), or Never. We examined the relation of each of the 11 combat situations above to the general life threat item. Our aim was to dichotomize the items in order to lessen the potential for bias from extreme reporting but to do it in a way that maximized each item’s relation to the general question of overall life threat. Usually this resulted in dichotomizing the variable to indicate whether the respondent ever had the experience. The 11 dichotomized items were then summed to create the Count of Life Threatening Experiences, which exhibited properties of a Guttman (1950) scale with reproducibility of .93 and an internal consistency reliability of .88.
Witnessed death of a close friend in unit
The veteran’s response of more than “never” to the question, “How often did you see a close friend from your unit(s) killed or die?
Killed enemy
The veteran’s report about how often he knew that he had personally killed enemy combatants, indicated by a response other than “never” to the following query:
“In the Vietnam arena, enemy personnel were often killed or wounded without any one American soldier being able to say definitely that he fired the shot that did it or was otherwise personally responsible for the casualty. But occasionally a soldier did know that he was personally responsible for the death of an enemy. How often (if ever) were you in a combat situation where you were sure that you personally had killed enemy personnel?”
Betrayal involving life threat (friendly fire)
This was rated by research staff members as having occurred (or not) from open-ended responses to various questions; it usually involved “friendly fire” incidents.
Harm to civilians or prisoners
The questions used to identify involvement in harming civilians or prisoners followed a general introductory statement that was read to each veteran:
“In combat situations in (or around) Vietnam, Vietnamese prisoners or civilians were often injured because they were suspected of being enemy sympathizers, or to obtain information, or to avenge the deaths of American soldiers, or for other reasons.”
This was followed by questions about the veteran’s direct or indirect involvement in harming prisoners and in harming civilians. For example, he was asked first whether he was ever in a situation in which a Vietnamese prisoner was injured or killed for any reason and, if so, did you “only see this happen, or were you directly involved?” and, if directly involved, were you “personally responsible?” A similar series of questions was asked in a self-administered questionnaire about situations involving civilians and prisoners that inquired into the extent to which the veteran was involved in “terrorizing, wounding, or killing civilians” and the extent to which he was involved in “torturing, wounding, or killing hostages or prisoners of war.” To define “extent,” he was asked to choose among the following alternatives: Not at all, knew/heard about it, saw it, unit participated, I participated, I was responsible. Admission of direct personal involvement (I participated or I was responsible) to the set of questions about harming prisoners or the set about harming civilians was taken to indicate the soldier had harmed prisoners and/or civilians, respectively.
Pre-Vietnam Vulnerability factors
There is now a considerable body of literature on vulnerability factors that are strongly associated with PTSD. This literature has been extensively reviewed (Brewin, Andrews, & Valentine, 2000; Dalgleish, 2004; Fontana, & Rosenheck, 1994; Halligan & Yehuda, 2000; King, King, Foy, & Gudanowske, 1996; Macklin et al., 1998; Ozer, Best Lipsy, & Weiss, 2003; and Schnurr, P.P., Lunney, & Sengupta, 2004). For the present study, we only consider vulnerability factors that occurred prior to or were present at the start of the Vietnam service thus ensuring a time order to the relationship between vulnerability and exposure.
In total, 15 possible indicators of pre-Vietnam vulnerability were extracted from the NVVRS based on veterans’ self reports, military records, or both (Hunt et al., 1994; Kulka et al., 1990, p. 80). The self-report measures either were provided in the public use tapes (Hunt et al., 1994) or could be readily constructed from raw survey data provided by RTI. The measures from the military record were based on data from the military records (“201 files”) that Kulka et al. (1990) extracted in relation to drawing the sample. Of the 15 vulnerability indicators, nine differentiated veterans with onsets of war-related PTSD and/or current war-related PTSD from other veterans with relative risks of 1.5 or more, or at least the .10 level of statistical significance and were subsequently used to create a total vulnerability load score. These indicators are (1) reporting one or more family members having been arrested during the respondent’s childhood (self-report); (2) one or more family members with alcohol or drug abuse problems during the respondent’s childhood (self-report); (3) childhood physical abuse involving being spanked or hit so hard by a parent or parent surrogate that the respondent “had marks or bruises, had to stay in bed, or see a doctor more often than “hardly ever” (self-report); (4) childhood conduct disorder (see below); (5) one or more other psychiatric disorders with pre-Vietnam onsets (see below); (6) low pre-Vietnam educational level (not beyond high school graduation) (military record); (7) average (category III) or worse on the Armed Forces Qualifications Test (AFQT) (military record); (8) arriving in Vietnam younger than age 25 (military record); and (9) having none of the following previous military experiences: no prior exposure to enemy fire in the Korean War or other conflicts prior to Vietnam, no prior attainment of rank of sergeant or equivalent, and no prior military service at all (military record).
Measurement of childhood conduct disorder and psychiatric disorders with pre-Vietnam onsets
Five of our colleagues, three psychiatrists and two doctoral level clinical psychologists, blind to the original diagnoses, reviewed a random selection of 52 tapes of the SCID interviews. We confirmed the good reliability of the PTSD diagnoses found by Weiss et al. (1992). In addition, our checks on diagnoses for psychiatric disorders other than PTSD showed that inter-rater reliabilities for most were satisfactory. For example, all but two of the kappas based on the weighted results for the current or lifetime presence of major depression, panic disorder, generalized anxiety disorder (current only), alcohol abuse or dependence, polysubstance abuse or dependence, and antisocial personality (lifetime only) were over .80. The exceptions were .68 for current panic disorder and .56 for lifetime polysubstance abuse or dependence. Because the clinicians probed for the dates of initial onsets of symptoms, it was possible to estimate whether the initial onsets of these disorders occurred prior to, during or after service in Vietnam. Initial onsets prior to Vietnam, including those of childhood conduct disorder, are considered possible vulnerability factors. As noted earlier, only four subsample veterans had first onsets of PTSD prior to their service in Vietnam, and these veterans are eliminated from our investigation as too few to analyze.
Other variables
Several other variables were needed for the analysis. One of these was racial/ethnic background (majority white, Black or Hispanic), which is included in all regression analyses as a control variable. Another consisted of psychiatric disorders other than PTSD with onsets during or after service in Vietnam that might be war-related and co-morbid with or alternatives to PTSD. Two additional items were included to provide a context for personal involvement in harm to civilians and prisoners. These were NSVG questions that asked how often the veteran “had trouble identifying who the enemy was” and “Were you ever in a situation in Vietnam where women, children, or old people were either injured or killed by American or South Vietnamese (ARVN) soldiers?”
Data Analysis Plan
All analyses incorporated sampling weights and strata so that estimates are representative of the entire population of Vietnam veterans from the 28 SMRs. To address the question of necessity of Criterion A stressor for PSS, the count (and proportion) of veterans with PSS who did not have Criterion A stressors, as identified by clinical diagnosticians, was examined. Qualitative assessment of military records, news reports and historical accounts was conducted to verify the clinicians’ judgments about the presence or absence of Criterion A stressors for those with PSS.
To address the question of sufficiency of combat exposures, we first examined veterans with a clinician-identified Criterion A stressor and calculated the proportion who met criteria for PSS as well as for other psychiatric disorders. Second, we elaborated rates and relative risks of PSS onset and current PSS across all of the record-based and self-reported combat exposure measures described above. Third, we developed a single composite measure of the severity of combat exposure that combined the six specific combat exposure measures. Given the moderate to large correlations among the six combat exposure measures (i.e., MHM, purple heart, count of life threatening experiences, witnessed death of a close friend in unit, betrayal involving life threat, killed enemy), a factor analytic method for ordered categorical items (Joreskog and Moustaki, 2001; Wirth and Edwards, 2007) was used to create a single score. This method combined the measures in such a way that the composite had the highest overall correlation with all of the original combat exposure measures. The resulting Combat Exposure Severity Scale (often abbreviated here as Combat Exposure) for each individual was calculated based on the posterior predicted value from an ordered categorical item factor analysis fit using maximum likelihood in Mplus 6.1 (Muthen and Muthen 2010). Finally, we examined rates of PSS onset and current PSS among veterans grouped by percentiles of the Combat Exposure Severity Scale and performed logistic regression on the scale treated as continuous and standardized to test for dose-response relationships.
To address the role of vulnerability, we first examined the relative risk of PSS onset and current PSS with each of the separate vulnerability factors. Then we created a single measure of Vulnerability Load (often abbreviated here as Vulnerability) which was constructed as a simple count of the number of vulnerability factors present (possible score 0–9). We used this simple sum score rather than a factor analytic approach because, unlike the combat exposure stressors, most of the nine vulnerability factors were not substantially correlated with each other. Finally we examined rates of PSS onset and current PSS among veterans grouped by percentiles of the Vulnerability Load measure and performed logistic regression on the scale treated as continuous and standardized to test for dose-response relationships.
To address the question of harm to civilians or prisoners, we used items from the NSVG to construct a dichotomous variable, Harm to Civilians or Prisoners (often abbreviated here as Harm), to indicate whether respondents reported having personally participated in such harm.
To assess the independent contributions of combat exposure and vulnerability, as well as harm to civilians or prisoners, to PSS onset and current PSS, we used a series of logistic regressions. We standardized both the Combat Exposure Severity Scale and the Vulnerability Load measure to have mean zero and variance 1 so that the magnitude of the associated odds ratios could be compared directly. The skew and kurtosis for the Combat Exposure Severity Scale were −0.5 and 1.6, and for the Vulnerability Load measure were −0.1 and 1.8 respectively, within ranges satisfying typical rules of thumb for normality assumptions thus justifying direct comparison in standard-deviation units (Kline, 2010). Racial/ethnic background was included as a control variable in all models. For each outcome separately (i.e. PSS onset, current PSS), Model 1 was a logistic regression on Combat Exposure and Vulnerability, both of which are continuous measures. Model 2 additionally included Harm. Odds ratios for each predictor and associated 95% confidence intervals were obtained from the fitted models.
Next, we considered tests for two-way interactions between Combat Exposure, Vulnerability and the Harm indicator on the additive risk scale (Rothman, Greenland, & Lash, (2008)). The test for interaction was conducted on the additive (risk difference) scale rather than the multiplicative (odds ratio) scale because the additive scale more closely represents synergy from a causal framework perspective (Rothman, Greenland, & Lash, 2008;Schwartz, 2006). Furthermore, because of the expected broad range from low to high risk for PSS onset and Current PSS associated with the wide range of exposure and vulnerability, interpretation of the interaction is facilitated by examining risk directly (and risk differences) rather than focusing entirely on odds ratios which can be more difficult to interpret when overall risk is not low. For tests of interactions on the additive scale, a logistic regression model was fit with cross product terms included between the variables of interest. Then, using a back transformation to the probability scale, an interaction risk difference contrast (Rothman, Greenland, & Lash, (2008); Greenland, 2004) was formed. This interaction risk difference contrast was associated with a one standard deviation increase from zero in each predictor while holding the other predictor in the interaction at zero and the other control variables at their marginal means. Tests for the significance of the interaction risk difference contrast were obtained using PROC NLMIXED in SAS; code is available from the authors.
After assessing interactions between the predictor variables, we then considered a more flexible Model 3, which allowed for the possibility of a breakpoint along the continuum of exposure at which point the odds ratio of PSS onset (or current PSS) could increase or decrease. The optimal breakpoint was empirically chosen to minimize the Akaike information criterion (AIC) obtained from a logistic regression of the outcome on a piecewise linear indicator for Combat Exposure (two slopes, one corresponding to continuous changes in Combat Exposure before the breakpoint and one after), continuous Vulnerability, racial/ethnic background, and Harm. An exhaustive search along the Combat Exposure continuum was conducted to identify the optimal breakpoint. The AIC for Model 3 was then compared to the AIC for Models 1, 2 and the interaction models described above to identify the best fitting model for PSS onset and current PSS. Finally, plots of predicted probabilities (i.e., estimated rates) from the best fitting models are presented to facilitate interpretation of results. Both exposure and vulnerability are continuous predictors in the models, but in plotting estimated rates of PSS we present values of Vulnerability Load fixed at 2, 4, and 6 corresponding to low (5th–22nd percentile), moderate (46th–80th percentile) and high (90th–97th percentile) values across the distribution of vulnerability. All regression analyses were performed in SAS 9.2.
Results
Criterion A Combat Stressors as Necessary
Most symptoms of PTSD – e.g., flashbacks, nightmares, other intrusive thoughts, and avoidance of reminders – include memories of the exposure to stressful events in their definitions. The exposures are, in this sense of inclusion in symptom memory, always necessary for the diagnosis. Whether these exposures qualify as Criterion A stressors, however, remains an issue. We can, therefore, still ask whether the exposures that meet specifications as to type (e.g., life threatening combat) and severity (e.g., long duration, frequent occurrence) are necessary for the symptom syndrome (PSS) to develop.
Every PTSD symptom, as noted earlier, was evaluated for all subsample veterans regardless of whether the veterans reported experiences that the clinicians considered evidence of exposure to Criterion A stressors. This convention offers the opportunity to investigate whether Criterion A stressors were necessary for the occurrence of war-related PSS.
Only two veterans were classified as meeting the symptom criteria (PSS) for first onsets of war-related PTSD but not the clinician rated (CR) exposure criterion. Suitably weighted, these two veterans represent much less than one percent (0.15%) of the population of veterans from the 28 SMRs. While in the clinicians’ judgment neither provided evidence during the examination of exposure to Criterion A combat stressors, there was ample evidence of such exposure in their NSVG interviews and military records. For example, both veterans were infantrymen according to their military records and their own self-reports. One of the veterans was scored in the second of the two most severe categories on the record-based MHM and reported that he was often (13–50 times) in danger of being killed or wounded. The other veteran was scored on the MHM in the intermediate category of moderately severe probable exposure and reported having been in danger of being killed or wounded “sometimes” (3–12 times).
We checked the plausibility of the clinicians’ positive Criterion A ratings for veterans they diagnosed as meeting both the PSS and Criterion A requirements. Weighted back to the population from which the subsample was drawn, only 1.8% of these veterans diagnosed with war-related PTSD had a CR Criterion A stressor that we could not corroborate as plausible with external sources, especially military records (Dohrenwend et al., 2006; 2007). It seems, then, that at most 2% of the veterans had onsets of PSS in the absence of one or more Criterion A stressors.
Criterion A Combat Stressors as Sufficient
The results on the question of sufficiency are more complicated. Suitably weighted, only 31.6% of the veterans judged by the clinicians to have experienced Criterion A stressors had full PSS onsets. However, PTSD is often co-morbid with other psychiatric disorders (e.g. Kessler, Sonnega, Bromet, & Nelson, 1995) and this is the case here.
Over three quarters (78.3%) of the veterans with PTSD also had onsets of other Axis I disorders during or after their service in Vietnam. More important for our purposes, almost half (49.5%) of the veterans who did not develop war-related PSS following CR Criterion A stressors developed one or more other Axis 1 disorders with alcoholism being the most prevalent at 32.1%. Thus, a total of 81.1% (i.e. 31.6% + 49.5%) of veterans with Criterion A stressors developed either PSS or some other psychiatric disorder. It may be that some of these other disorders are consequences of Criterion A exposure, however, some of the other disorders could have developed long after the war ended and are probably not war-related. Consistent with this possibility, a substantial 27.6% of the veterans who did not experience a CR Criterion A stressor did develop disorders other than PTSD with 19.5% being alcoholism, during or after their post-war service. If we consider them a control group and subtract their 27.6% rate of other disorders as clearly non-war-related from the 81.1%, we then have a substantial but far from sufficient rate of 53.3% with war-related PSS or other psychiatric disorders, especially alcoholism, in the absence of PSS, for the veterans who experienced CR Criterion A stressors.
Our findings thus far are based on the clinicians’ judgments about the presence or absence of Criterion A stressors. However, these either/or clinical judgments do not differentiate among stressors of varying types and severities of experiences in the war-zone. Would any of these different types and severities of combat experiences be sufficient for the onset of war-related PSS?
As Table 1 shows, all six combat exposure measures described earlier are strongly related to both PSS onset and current PSS. For example, 72.1% of the veterans reporting the the highest number of Life Threatening Experiences had onsets of PSS compared with only 7.5% in the lowest group. However, none of these measures, even at its most extreme exposure end, was close to being sufficient (i.e., risk was always much less than 100%). We therefore examined the possibility that a composite measure would have a greater impact than any one of the six alone.
Table 1.
Distribution of war zone experiences and their associations with risk of war-related PTSD symptom syndrome (PSS) onset and current PSS
| %(n)a | War-related PSS Onset | Current PSS | |||||
|---|---|---|---|---|---|---|---|
| risk | RR | 95% CI of RR | risk | RR | 95% CI of RR | ||
|
|
|
||||||
| Whole Sample | 100%(248) | 21.7% | 10.9% | ||||
| COMBAT EXPOSURE | |||||||
| Based on the Military Record | |||||||
| Military Historical Measure | |||||||
| lowest severity | 26.1% (38) | 10.3% | ref | 0.3% | ref | ||
| moderate severity | 63.1% (152) | 23.4% | 2.28 | (0.62–8.39) | 12.3% | 39.61 | (8.47–99)b |
| high severity | 7.8% (37) | 40.1% | 3.91 | (0.92–16.58) | 27.0% | 87.16 | (16.90–99)b |
| very high severity | 3.0% (21) | 38.7% | 3.77* | (0.88–16.14) | 33.6% | 108.22* | (21.4–99)b |
| Purple Heart | |||||||
| No | 90.9% (212) | 19.8% | ref | 9.1% | ref | ||
| Yes | 9.1% (33) | 45.9% | 2.32 | (1.24–4.32) | 31.7% | 3.47 | (1.57–7.69) |
| Reported by Veterans | |||||||
| Count of Life Threatening Experiences | |||||||
| 0–2 | 29.4% (44) | 7.5% | ref | 0.4% | ref | ||
| 3–6 | 24.5% (62) | 20.9% | 2.78 | (0.64–12.00) | 8.5% | 19.27 | (3.44–99) |
| 7–9 | 34.9% (89) | 19.2% | 2.54 | (0.60–10.68) | 7.6% | 17.17 | (3.33–88.6) |
| 10–11 | 11.2% (50) | 72.1% | 9.55 | (2.49–36.63) | 56.3% | 127.97 | (29.0–99)b |
| Witnessed death of a close friend in unit | |||||||
| No | 67.9% (125) | 12.7% | ref | 4.3% | ref | ||
| Yes | 32.1% (119) | 41.7% | 3.28 | (1.68–6.41) | 25.3% | 5.94 | (2.52–13.99) |
| Betrayal involving life threat (friendly fire) | |||||||
| No | 90.3% (224) | 19.4% | ref | 8.2% | ref | ||
| Yes | 9.7% (22) | 46.7% | 2.40 | (1.23–4.71) | 38.2% | 4.65 | (2.12–10.21) |
| Killed enemy | |||||||
| No | 66.4% (126) | 15.1% | ref | 4.6% | ref | ||
| Yes | 33.6% (106) | 34.9% | 2.31 | (1.20–4.45) | 23.7% | 5.17 | (2.21–12.10) |
Trend test for increasing risk by increasing severity of Military Historical Measure score is significant, p=.016 for PSS Onset, p<.0001 for Current PSS.
All percents are weighted to represent population estimates. N’s are raw sample sizes. Total n does not always total 248 due to missing values on exposure or harm variables.
CI value of 99 represents extreme upper limit estimate due to small risk in reference group
The individual combat exposure measures are substantially correlated with each other, with 21 of the 36 correlations .50 or higher--for example, .59 between the record-based MHM and the self-report item on knowledge of personally killing enemy soldiers; .55 between having a record of receiving a Purple Heart for wounds and a self-report of having witnessed the death of a friend in his unit. Given these moderate to large correlations, factor analysis for ordered categorical variables was used as described in the Data Analysis Plan to construct a single continuous Combat Exposure Severity Scale from the six individual combat exposure measures. For comparison, a simple sum score of the six combat exposure measures was also constructed. The simple sum score was highly correlated with the Combat Exposure Severity Scale but the weighted scale was preferred due to its ability to capture additional variability in severity due to different types of combat exposures.
Table 2 (left side) shows a clear dose-response relationship between the combat exposure severity scale and the risk of both PSS onset and current PSS with the overall odds ratios for trend being statistically significant. In the most severe exposure group on this scale (above the 99th percentile), the onset rate is 88.5%, which is nearer to sufficiency than exhibited by any of the individual combat exposure measures. It is still, however, considerably less than 100%.
Table 2.
Relationship of Combat Exposure Severity Scale and Total vulnerability with PSS onset and current PSS.
| Percentilec of predictor | Predictor is Combat Exposure Severityb | Predictor is Total Vulnerability Count | ||||
|---|---|---|---|---|---|---|
| na | %with PSS onset | %with Current PSS | n | %with PSS onset | %with Current PSS | |
| below 10th | 15 | 0.0% | 0.0% | 10 | 4.3% | 0.0% |
| below 25th | 42 | 7.4% | 0.2% | 38 | 7.4% | 0.5% |
| below 50th | 95 | 12.8% | 3.0% | 84 | 10.1% | 3.8% |
| above 50th | 153 | 31.0% | 19.2% | 164 | 31.6% | 17.1% |
| above 75th | 97 | 46.9% | 30.5% | 85 | 53.8% | 35.0% |
| above 90th | 42 | 69.9% | 55.4% | 45 | 67.0% | 49.6% |
| above 99th | 4 | 88.5% | 27.4% | 6 | 89.4% | 75.4% |
| Odds ratio for trend (95% CI)d | 2.78 (1.67–4.64) | 5.64 (2.53–12.57) | 2.85 (1.89–4.31) | 3.56 (2.28–5.57) | ||
n’s are raw unweighted sample sizes within each weighted percentile group for combat exposure severity or total vulnerability. Weighted sample percents within each percentile category differ slightly from nominal (e.g. below 25th percentile for combat exposure severity has 28.6% of sample) due to ties at percentile cutpoints.
Scale created from factor analysis using the 6 combat exposure variables as indicators
Categories are not mutually exclusive (e.g. veterans above 90th percentile on combat exposure severity are a subset of those above 75th percentile).
Odds ratios corresponding to a 1 standard deviation increase in combat exposure or standardized total vulnerability.
Effects of Vulnerability and Harming
Like the combat exposure measures, the individual vulnerability measures were positively associated with increased risk of PSS onset and adverse course represented by current PSS (data not shown). The two pre-war vulnerability factors with the highest statistically significant risk of PSS onset (approximately 39%) were childhood experience of physical abuse and childhood conduct disorder. Almost as high were one or more other pre-Vietnam psychiatric disorders 34.3% and having one or more family members with an arrest record 38.4%. Age was also a substantial factor; men who entered Vietnam at an age under 25 were nearly 7 times as likely (25.8%) to have PSS onset compared to men 25 or older (3.7% PSS onset).
With few exceptions, such as a correlation of .47 between pre-Vietnam educational level and AFQT score, the nine vulnerability factors are not highly inter-correlated. By contrast with the individual exposure measures, only one of the 36 correlations is .50 or higher (.93 between pre-Vietnam age and previous military experience); 18 of the correlations are below .20. Given these generally low correlations, our Vulnerability Load measure is a simple count of the nine vulnerability factors.
Table 2 (right side) shows that like the Combat Exposure Severity Scale, Vulnerability Load has a strong dose-response relationship with PSS onset and current PSS. The combat exposure severity and the vulnerability load measures are only moderately correlated (r=.28, p<.001) with each other.
Both personal involvement in harm to prisoners and personal involvement in harm to civilians are also strongly related to PSS, with an onset rate of 76.1% among men reporting harming prisoners and 53.9% for harming civilians. To increase statistical power, the two measures were combined into a single dichotomous indicator of Harm to Civilians or Prisoners (Harm). An estimated 13.3% of soldiers reported personal involvement in inflicting harm on prisoners or civilians. We will refer to these men as “Harmers.” Almost two thirds of the Harmers (63.2%) had onsets compared with only 15.3% of the non-Harmers. The rate of current PSS was 39.9% among the Harmers compared with only 6.2% among the non-Harmers.
Table 3 presents the results of regression analyses assessing the independent contributions of combat exposure, vulnerability, and harm to PSS. The Combat Exposure Severity Scale and the Vulnerability Load measure are both standardized, so the odds ratios represent the effects of an increase of one standard deviation in either scale. Model 1 in Table 3 shows that the contributions of the two factors to the onset of PSS were both substantial and about equal. Model 2, with Harm added to the equation, shows that the independent contributions of Combat Exposure and Vulnerability were still substantial, and that there was also a large independent contribution of Harm as represented by an odds ratio of 4.78. To produce an equivalent odds ratio to that of being a Harmer compared to a non-Harmer, a soldier’s Combat Exposure would have to increase by 2.6 standard deviations (ln(4.78)/ln(1.83)) which can occur in several ways including going from less than 2 Life Threatening experiences up to 7 or more or his Vulnerability Load would have to increase by 1.9 standard deviations equivalent to adding approximately 3 more vulnerability factors. For current PSS, all effects, especially that of Vulnerability Load, are again substantial, but Harm does not show a significant independent effect.
Table 3.
Adjusted odds ratios of PSS onset and current PSS for increases in Severity of Combat Exposure, Vulnerability Load and Harm to Civilians or Prisoners.
| PSS Onset | Current PSS | |||
|---|---|---|---|---|
| Model 1a OR (95% CI) |
Model 2b OR (95% CI) |
Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
|
| Combat Exposure Severity Scale | 2.29 (1.35–3.88) | 1.83 (1.10–3.03) | 4.41 (2.10–9.25) | 3.47 (1.55–7.77) |
|
| ||||
| Total Vulnerability Load | 2.33 (1.51–3.58) | 2.31 (1.49–3.60) | 2.67 (1.70–4.19) | 2.60 (1.65–4.10) |
|
| ||||
| Harmed civilians or prisoners | - | 4.78 (1.84–12.45) | - | 2.70 (0.78–9.37)NS |
Model 1 simultaneously includes standardized Combat Exposure Severity Scale and standardized Total Vulnerability load as continuous predictors and also includes racial/ethnic group.
Model 2 adds to Model 1 by including an indicator of whether the soldier reported harming civilians or prisoners.
We investigated interactions among the three variables. Only the additive interaction between Combat Exposure and Vulnerability as predictors of current PSS was statistically significant. The interaction contrast (i.e. difference in risk differences) was 9.3% (s.e. = 1.6%, p<.0001) indicating a positive or super-additive synergistic effect between exposure and vulnerability on current PSS.
We also investigated an additional Model 3 to allow for the possibility of a breakpoint along the continuum of exposure at which point the odds ratio could increase or decrease. Model 3 showed superior fit for PSS onset compared to both Models 1 and 2 for PSS onset. For current PSS, Model 3 did not show superior fit to Model 1 or 2. The optimal breakpoint along the Combat Exposure continuum for predicting PSS onset was found using Model 3 to be 0.98 or approximately 1 standard deviation above the mean, corresponding to approximately the 75th percentile of the Combat Exposure scale in this sample. Model 3 finds for PSS onset that the odds ratio associated with changes in Combat Exposure in the range below 1 is not significant (OR=1.25, 95% CI = (0.72–2.18), but is dramatically large and statistically significant in the range above 1 (OR=13.00, 95% CI=1.34–125.0); the wide confidence interval is due in part to the limited sample size above the 75th percentile and also due to the large value of the odds ratio in this region). The odds ratio for Vulnerability Load in Model 3 for PSS onset is also significant (OR = 2.34, 95% CI = (1.47–3.72) and the odds ratio of harm remains significant (OR = 3.85 (1.44–10.28).
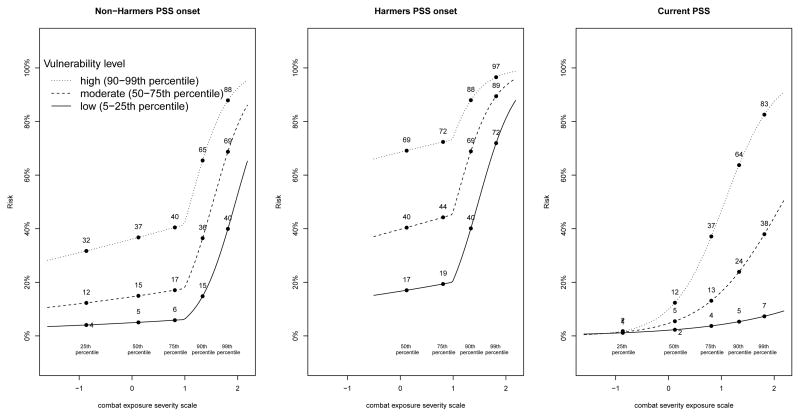
The left and middle panels of Figure 1 portray the regression estimated rates of PSS onset (from Model 3 in non-Harmers and Harmers as a function of Combat Exposure and Vulnerability Load). The right panel portrays the estimated rates of current PSS (from Model 1 with interaction) as functions of Combat Exposure and Vulnerability Load.
Figure 1. Estimated ratesa of PSS onset (left and middle by harmer status) and current PSS (right) as a function of both combat exposure severity and vulnerability loadb.
aEstimated rates are obtained from best fitting logistic regression models for PSS onset and current PSS. For PSS onset the best model was Model 3 including an indicator of harm and a change point in increased log odds risk at +1 standard deviation on the combat exposure severity scale (approximately the 75th percentile). For current PSS the best fitting model was Model 1 additionally including a cross-product between combat exposure severity and vulnerability. Estimated rates presented are for fixed values of vulnerability and exposure corresponding to low, moderate and high percentiles of each variable. To avoid extrapolation to combinations of predictors with no observations, no estimates are given for PSS onset among Harmers at low end of combat exposure severity scale.
As the left hand panel of Figure 1 shows, both Combat Exposure and Vulnerability contribute to PSS onset. However, the effect of Combat Exposure is most pronounced above the 75th percentile of severity for both non-Harmers and Harmers. Because there was no significant interaction between Vulnerability and Combat Exposure in predicting PSS onset, the effect of Vulnerability is specified as constant here in terms of odds ratio from one vulnerability value to the next. Comparing this constant effect with the effects of Combat Exposure below and above the breakpoint, we see that below the 75th percentile the impact of Vulnerability is higher (significant odds ratios of about 2) than the impact of Combat Exposure (odds ratio of about 1.3 and not significant), but that above the 75th percentile exposure matters much more (odds ratio of 13.0) than Vulnerability (with odds ratio remaining at about 2). Even at low levels of Vulnerability an estimated 40% of the non-Harmers and 72% of the Harmers who were highly exposed developed PSS.
It is striking that, as the central panel shows, the predicted rates of PSS onset are shifted markedly upward for Harmers compared to non-Harmers in the left panel even for those with low Vulnerability Load. Those veterans with both high Combat Exposure and high Vulnerability have a very high risk (88%) of developing PSS if they were not harmers and a nearly sufficient 97% risk if they were Harmers.
The positive additive interaction found between Combat Exposure and Vulnerability for current PSS is portrayed in the estimated rates plotted in the right hand side of Figure 1. The effect of Vulnerability on current PSS increases with Combat Exposure. For those with Combat Exposure below the 25th percentile, the estimated rate of current PSS is only around 1.0%, regardless of Vulnerability. By contrast, at the 99th percentile, the range is from an estimated current PSS rate of 7% for those with the lowest Vulnerability Load to 83% for those in the most vulnerable group.
Combat Exposure, Vulnerability, and Harming
Vulnerability was positively correlated only .20 with Harm by contrast with a positive correlation of .41 between Harm and Combat Exposure. The import of this difference can be seen in Table 3, which shows that adjusting for Harm reduces the effects of Combat Exposure on PSS onset and current PSS but does not substantially alter the effects of Vulnerability.
Correlations between Harm and the individual combat exposure measures were moderate to high (.28 to.66) with the scale of life threatening experiences, killing the enemy, and witnessing the death of a friend in the unit all having correlations greater than .50. Among the individual vulnerability factors, the highest correlation was .36 between physical abuse during childhood and Harm. There were small to moderate correlations (.20 to .27) of Harm with younger age, having no more than a high school education, and having had a family member arrested. The correlations were negligible between Harm and childhood conduct disorder (.03) and pre-war psychiatric disorder (−.03).
The record-based MHM with its reliance on type of military unit and MOS is the measure of exposure that most clearly differentiates among those veterans whose job was more or less likely to involve seeking combat with enemy forces. Fully half (50.4%) of the veterans in the high and very high severity categories of the MHM reported that they often or very often “had trouble identifying who the enemy was.” Only 15.2% in these high exposure categories said that they never had this problem, compared to 45.2% in the moderate and low MHM categories. Moreover, 66.4% of those in the two high exposure MHM categories, compared with 42.7% in the two lower exposure categories, answered “yes” to the question, “Were you ever in a situation in Vietnam where women, children, or old people were either injured or killed by American or South Vietnamese (ARVN) soldiers?” Against this background, it would be reasonable to expect the proportions of Harmers to be highest in the Very High and High probable exposure categories of the MHM, and this expectation is confirmed. The proportions of Harmers are: 33.9% in the Very High and 27.9% in the High, but only14.7% in the Moderate and 4.7% in the Low MHM exposure groups.
Discussion
The central assumption in DSM-III, III-R, and IV, that potentially traumatic stressors are more important than personal vulnerability in causing PTSD, is controversial. We tested this assumption with data from a rigorously diagnosed subsample of men from the National Vietnam Veterans Readjustment Study (NVVRS). Combat exposure, vulnerability, and personal involvement in harming civilians or prisoners were examined, with only combat exposure proving necessary for disorder onset. While none of the three factors proved sufficient, estimated PSS onset reached 97% for veterans high on all three, with harm to civilians or prisoners showing the largest independent contribution. Severity of combat exposure proved more important than vulnerability in onset; vulnerability was at least as important in long-term persistence. These results have conceptual implications for the primacy of the stressor assumption in the diagnosis of PTSD, and they raise questions that require further research. Moreover, they have policy implications that need consideration.
Even the most severe combat stressors that we measured were not sufficient to bring about the onset of PSS in almost all such exposed veterans. This may be because the types, severities and duration (tours typically lasting about a year) of exposure in the NVVRS sample of Vietnam veterans do not cover the entire variety, intensity and duration of stressful events that have been found in other research to approach near sufficiency for onset. For example, only two veterans in the subsample reported being prisoners of war (POWs), and neither described situations nearly as prolonged or severe as the experiences of U.S. POWs of the Japanese during World War II. As systematic research with a carefully selected and rigorously diagnosed sample found, the PTSD onset rate was 84% in these World War II surviving prisoners of the Japanese; 59% still met criteria 40 – 50 years after capture (Engdahl, Dikel, Eberly, & Blank1997).
There is, nevertheless, support for the primary role of combat exposure compared with vulnerability in our results for these factors in the onset of PSS. Most important is that, unlike vulnerability, Criterion A combat stressors were necessary for the occurrence of war-related PSS. We were able to investigate the necessity of Criterion A exposure because of the NVVRS procedure of asking about the symptoms of PTSD of all veterans in the diagnostic examinations regardless of whether or not the clinicians judged that the veteran satisfied Criterion A. In addition to necessary stressor exposure, an estimated 40% of the most severely exposed and least vulnerable men who did not personally harm civilians or prisoners had onsets of PSS (Figure 1). Consistent with the primacy assumption, this suggests that PSS can occur in individuals who show little personal vulnerability when stressor exposure is especially severe, as may have been the case for some veterans in our highest severity exposure category.
By contrast with its role in onset, pre-Vietnam personal vulnerability appears to be at least as important as combat exposure in the adverse course of the disorder represented by current PSS (present at the time of data collection 11–12 years after the war). Unlike onset PSS, and contrary to our prediction under the primacy assumption, we found a positive rather than negative interaction between vulnerability and combat exposure for current PSS; that is, the greater the severity of combat exposure, the greater (rather than lesser) the contribution of vulnerability load to highly chronic current PSS (Figure 1, right panel). For those with low severity of combat exposure (the 25th percentile), the estimated rate of current PSS is less than 5% regardless of vulnerability load. By contrast, vulnerability makes a huge difference for those with the highest level of combat exposure (99th percentile) ranging from an estimated rate of 7% for the least vulnerable to 83% for those in the most vulnerable group (Figure 1).
There are important questions about the generalizability of the present results. These questions involve both the nature and severity of the stressors and the nature of the PSS syndrome. The stressors of war-time combat in Vietnam involved threat to one’s life and physical integrity. The present results may generalize to other wars such as those in Iraq and Afghanistan. Much research on U.S war-fighters in Iraq and Afghanistan has been done, but it has tended to rely on self-report symptom checklists rather than clinical diagnostic examinations (e.g., Hogue, Castro, Messer, McGurk, Cotting, & Koffman, 2004). As far as we know, no studies using comparable methodology with veterans of the Iraq and Afghanistan wars have yet been published. Possibly the results we obtained will generalize to prolonged exposure to life-threatening situations such as human-made and natural disasters. Again, however, we know of no studies using comparable measures to those reported here.
While our results may generalize to situations that involve life threat or threat to physical integrity in civilian life, such as child abuse, rape, and domestic violence, we would not expect the results to generalize to stressful situations and events in civilian life that do not involve threat to life or physical integrity. It is puzzling, therefore, that putative PTSD symptoms and syndrome have been found in at least 12 studies to be associated with stressful events such as breaking up with a boy friend, divorce and unemployment (Dohrenwend, 2010). These events pose threats to personal and social goals but typically do not threaten life or physical integrity. Even the broadened Criterion A of DSM-IV, which goes well beyond direct threat to life or physical integrity to learning about such threats to others, does not include such events.
Some investigators have argued that these findings with more usual events support an argument for further broadening Criterions A or even doing away with it altogether as a requirement for the diagnosis, a logical conclusion of wide broadening (Brewin et al., 2009; Maier, 2007). By contrast, Weathers and Keane (2007) suggest the PTSD-like symptoms associated with more usual stressors of everyday life may not be “real” PTSD symptoms and argue for a relatively narrow definition of Criterion A.
Most of the research on PTSD involving non-Criterion A events has been done using self-report symptom checklists. It is possible that these checklists measure nonspecific psychological distress rather than PSS as evaluated by clinicians (Arbisi, Kaler, Kehle-Forbes, Erbes, Polusny, & Thuras, 2012). There is a need for research that includes rigorous diagnostic examinations for PTSD and other disorders by experienced clinicians of samples from the general population of persons who have experienced non-Criterion A stressful events, such as divorce and unemployment, as well as narrowly defined Criterion A events that threaten life or physical integrity, such as abuse in childhood, domestic violence and rape, in addition to combat.
This research could be designed to investigate still other ways in which the PSS syndromes associated with non-Criterion A stressors and with Criterion A stressors may differ. For example, an individual need not experience all of the qualifying symptoms in each of the BCD clusters to receive a diagnosis of PTSD. It is possible, therefore, for two individuals to meet the BCD syndrome criteria with quite different B, C, and D symptoms. It may be that there are different subtypes of BCD symptom syndromes associated with Criterion A and non-Criterion A stressors.
It would be valuable as well to include biological measures in such research; some of the relevant data could be obtained, for example, by collecting genetic samples (e.g., saliva or blood) or through brain imaging. It is possible that the syndrome may be associated with non-Criterion A events assessed by self-report symptom checklist or by clinical diagnoses, and that it is the underlying biology that differs for syndromes following Criterion A and non-Criterion A stressors.
In addition to evaluation of PTSD symptoms and syndromes, diagnostic examinations for other comorbid disorders should be conducted. We found that alcoholism was by far the most frequently comorbid disorder with war-related PTSD. It is possible that different disorders may be more likely to be comorbid with PTSD syndromes associated with other types of stressful situations and events.
Future research designed to investigate these various possibilities could have substantial impact on the diagnosis of PTSD. Moreover, it would increase our knowledge of the roles of adversity and stress more generally in various types of psychopathology including, but not limited to, war-related PTSD.
The full psychological impact of the Vietnam war on U.S. forces cannot be understood without considering the role of the involvement of a substantial minority of the veterans (an estimated 13%) in personally harming civilians or prisoners. We found that such involvement showed a large independent contribution to PSS onset.. It is important to learn more about the harmers – who they were and why they inflicted harm. There are some clues in the present results.
We found that involvement in harm to civilians or prisoners was less correlated with the veteran’s vulnerability load (.20) than with his severity of combat exposure(.41) There were no correlations with childhood conduct disorder or with the pre-war presence of other disorders such as major depression and alcoholism. None of the background and vulnerability factors was as important in predicting who was a harmer as experiencing more severe combat stressors.
The nature of combat for U.S. forces in Vietnam probably had an important part in producing the association of harm to civilians and prisoners with severity of combat exposure. We found that fully half of the veterans in the high and very high severity of exposure categories of our record-based MHM reported that they often or very often “had trouble identifying who the enemy was.” Moreover, two thirds of those in the two high exposure MHM categories responded affirmatively to the question, “Were you ever in a situation in Vietnam where women, children, or old people were either injured or killed by American or South Vietnamese (ARVN) soldiers?” And over a quarter (27% in the High and 33% in the Very High MHM exposure groups) reported personally harming civilians or prisoners.
For some veterans, especially among those exposed to severe combat, this war among the people, with its emphasis on the body count, may have been a moral quagmire, one in which they behaved differently than they would have in previous wars -- those between states with clearly identifiable enemy forces -- much less than in civilian life. Some studies of patient samples of Vietnam veterans have found that strong feelings of guilt have been associated with involvement in harm to civilians, and that such feelings are associated with PTSD (Beckham, Feldman, & Kirby, 2010;; Hendin, H. & Haas, A.P., 1991; Henning & Frueh, 1997; Marx et al., 2010). It is possible that guilt feelings heighten susceptibility to PSS in combat veterans (see also Filkins, 2012).
There are limitations to our research that need consideration in evaluating the firmness of the results. The measures of severity of combat exposure and vulnerability include retrospective self-reports. These cross-sectional data could be affected, therefore, by recall biases (e.g., Kihlstrom, Eich, Sandbrand, 2000). However, the measures of combat exposure and vulnerability load also include record-based measures that are clearly antecedent to war-related PTSD and unaffected by recall bias. Their inclusion increases our confidence in the construct validity of these measures.
The measures of harm to civilians and harm to prisoners are wholly based on retrospective reports by the veterans. Here, we think, the problem of recall bias is likely to be different than, for example, possible over-reporting of combat exposure by veterans suffering from PSS. The problem with the measure of harming civilians or prisoners, rather, may be of under-reporting self-incriminating behavior. If so, our rate of harm involvement may be an underestimate.
It is also a limitation that our Vulnerability Load measure does not include all of the relevant indicators of vulnerability. Most important, we do not have measures of the polymorphisms that may indicate genetic susceptibility to stressors (Koenen, Amstadrer, & Nugent, 2009); such genetic vulnerability might explain why 40% in our most severely exposed/least vulnerable category experienced onsets of PSS. We do, however, have diagnoses of pre-Vietnam major depression and other possibly stress-related disorders that are likely to be associated with such polymorphisms (e.g., Caspi et al., 2003), and they are included in the measurement of Vulnerability Load. Nevertheless, it would be valuable to obtain samples of blood or saliva to test directly for evidence of genetic vulnerability. It would be important as well to investigate how these vulnerability factors are related to the veterans’ lives after their service in Vietnam – for example, their experiences with stressful situations and events that might exacerbate their symptoms or precipitate a recurrence of the syndrome.
As we have shown, the present results raise important questions that require further research. Nevertheless, as they stand, the results provide a compelling test of the primacy of the stressor assumption as it applies to male U.S. Vietnam veterans whose adjustment problems were so influential in giving rise to the PTSD diagnosis. By doing so, the results have important conceptual implications for the diagnosis of war-related PTSD and the theoretical assumptions that underlie it. The finding that exposure is more important in PSS onset is consistent with the formulations in all the DSMs, going back to the 1952 DSM-I and the 1968 DSM-II. The finding that vulnerability factors are more important in long-term course, however, may be more consistent with the role of prior vulnerability set forth in DSM-I and DSM-II than in subsequent DSMs. As noted at the outset, in these earlier DSMs, the effects of stressor exposure are assumed to be transient unless there is prior vulnerability. In the controversy over whether to narrow or broaden the types of stressful experience included under Criterion A, our results support narrowing the definition. As we pointed out, it is only those veterans experiencing very severe combat exposure that PSS onset rates are sharply elevated regardless of vulnerability load (Figure 1). This suggests that it was the very severe stressors that are important for defining Criteriion A for war-related PTSD.
Our results have implications for policy that need attention. If, as we believe it must be, the goal is to reduce rates of highly chronic war-related PTSD, the positive interaction of severity of combat exposure and vulnerability with current PSS points to the need to keep the more vulnerable soldiers out of the most severe combat situations. While this may seem obvious, it was not the U.S. policy in Vietnam, where pre-war personal vulnerability showed a modest positive correlation (.28) with severity of exposure.
More research is needed on the involvement of U.S. forces in harm to civilians and prisoners that proved such a strong independent contributor to the onset of war-related PSS. It will be particularly important to learn more about the combat circumstances in which such harm occurred, why some soldiers became harmers while others did not, and the possible role of subsequent guilt as a factor in the development of PSS.
The human toll on harmers and harmed, and the moral and ethical problems involved underline the importance of this need for further research. It should be designed to inform preventive efforts by the armed forces and government of any country that is involved in a “war amongst the people.” Vietnam was such a war for U.S. forces. So, more recently, have been the conflicts in Iraq and Afghanistan.
Acknowledgments
We thank C. J. Douglass, R. Lewis-Fernandez, R. Neugebauer, P.E. Shrout, J.B. Turner, and N. Turse for valuable comments and suggestions. The research was supported by the National Institute of Mental Health (NIMH) grant R01-MH059309 (B.P.D) and grants from The Spunk Fund, Inc. (B.P.D.) and a Ruth L. Kirschstein National Research Service Award (NRSA) from the NIMH (B.G.A.).
Contributor Information
Bruce P. Dohrenwend, Columbia University Department of Psychiatry and Mailman School of Public Health and New York State Psychiatric Institute
Thomas J. Yager, Columbia University Mailman School of Public Health
Melanie M. Wall, Columbia University Department of Psychiatry and Mailman School of Public Health and New York State Psychiatric Institute
Ben G. Adams, Columbia University Mailman School of Public Health
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1952. (DSM-I) [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1968. Revised, (DSM-II) [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1980. (DSM-III) [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1987. Revised, (DSM-III-R) [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. (DSM-IV) [Google Scholar]
- Arbisi PA, Kaler ME, Kehle-Forbes SM, Erbes CR, Thuras P. The predictive validity of the PTSD Checklist in a nonclinical sample of combat-exposed National Guard troops. Psychological Assessment. 2012 doi: 10.1037/a0028014. published online. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: Relationship to combat exposure, symptom severity, guilt, and interpersonal violence. Journal of Traumatic Stress. 1988;11:777–785. doi: 10.1023/A:1024453618638. [DOI] [PubMed] [Google Scholar]
- Breslau N. Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Canadian Journal of Psychiatry. 2002;47:923–929. doi: 10.1177/070674370204701003. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Lanius RA, Novak A, Schnyder U, Galea Reformulating PTSD for DSM-V: Life after Criterion A. Journal of Traumatic Stress. 2009;22:366–273. doi: 10.1002/jts.20443. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Coffelt RD, Arnold RJ, Argabright D. An electronic database of combat area causalities. National Archives and Records Administration; Washington, DC: 2002. [Google Scholar]
- Dalgleish T. Cognitive approaches to posttraumatic stress disorder: The evolution of multirepresentional theorizing. Psychological Bulletin. 2004;130:228–260. doi: 10.1037/0033-2909.130.2.228. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. Overview of the evidence for the importance of adverse environmental conditions in causing psychiatric disorders. In: Dohrenwend BP, editor. Adversity, Stress, and Psychopathology. New York: Oxford University Press; 1998. pp. 523–538. [Google Scholar]
- Dohrenwend BP. The stressor criterion in posttraumatic stress disorder: Issues, evidence, and implications. In: Simpson HB, Neria Y, Lewis-Fernandez R, Schneier F, editors. Understanding Anxiety: Clinical and Research Perspectives from the Columbia University Department of Psychiatry. New York: Cambridge University Press; 2010. pp. 216–226. [Google Scholar]
- Dohrenwend BP, Neria Y, Turner BJ, Turse NA, Marshall R, Lewis-Fernandez R, et al. Positive tertiary appraisals and posttraumatic stress disorder in U.S. male veterans of the war in Vietnam: The roles of positive affirmation, positive reformulation, and defensive denial. Journal of Consulting and Clinical Psychology. 2004;72:417–433. doi: 10.1037/0022-006X.72.3.417. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006;313:979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. Continuing controversy over the psychological risks of Vietnam for U.S. veterans. Journal of Traumatic Stress. 2007;20:449–465. doi: 10.1002/jts.20327. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Lewis-Fernandez R, Yager TJ. War-related posttraumatic stress disorder in Black, Hispanic, and Majority White veterans: The roles of exposure and vulnerability. Journal of Traumatic Stress. 2008;21:133–141. doi: 10.1002/jts.20296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engdahl B, Dikel TN, Eberly R, Blank A. Posttraumatic stress disorder in a community group of former prisoners of war: A normative response to severe trauma. American Journal of Psychiatry. 1997;154:1576–1581. doi: 10.1176/ajp.154.11.1576. [DOI] [PubMed] [Google Scholar]
- Filkins D. Atonement: An Iraq veteran and the family he harmed. The New Yorker. 2012 October 29 and November 5;:92–103. [Google Scholar]
- Fontana A, Rosenheck R. Posttraumatic stress disorder among Vietnam theater veterans: A causal model of etiology in a community sample. Journal of Nervous and Mental Disease. 1994;182:677–684. doi: 10.1097/00005053-199412000-00001. [DOI] [PubMed] [Google Scholar]
- Friedman MJ. Veterans’ mental health in the wake of war. New England Joural of Medicine. 2005;352:1287–1290. doi: 10.1056/NEJMp058028. [DOI] [PubMed] [Google Scholar]
- Friedman MJ, Resick PA, Keane TM. PTSD twenty-five years of progress and challenges. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and Practice. New York, NY: Guilford Press; 2007. pp. 3–18. [Google Scholar]
- Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. American Journal of Epidemiology. 2004;160:301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- Grossman D. On killing: The psychological costs of learning to kill in war and society. Boston: Little, Brown and Company; 1995. [Google Scholar]
- Guttman L. The basis for scalogram analysis. In: Stouffer SA, et al., editors. Measurement and Prediction. Princeton, New Jersey: Princeton University Press; 1950. pp. 60–90. [Google Scholar]
- Halligan SL, Yehuda R. Risk factors for PTSD. PTSD Research Quarterly. 2000;11:1–8. [Google Scholar]
- Hendin H, Haas AP. Suicide and guilt as manifestations of PTSD in Vietnam combat veterans. American Journal of Psychiatry. 1991;148:586–591. doi: 10.1176/ajp.148.5.586. [DOI] [PubMed] [Google Scholar]
- Henning KR, Frueh BC. Combat guilt and its relationship to PTSD symptoms. Journal of Clinical Psychology. 1997;53:801–808. doi: 10.1002/(SICI)1097-4679(199712). [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer D, McGurk DI, Cotting DL, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hunt PN, Schlenger WE, Jordan BK, Fairbank JA, LaVange LM, Potter FJ. NVVRS Public Use Analysis File Documentation: Analysis Variables from the National Vietnam Veterans Readjustment Study. Research Triangle Institute, RTP; NC: 1994. [Google Scholar]
- Joreskog K, Moustaki I. Factor analysis for ordinal variables: A comparison of three approaches. Multivariate Behavioral Research. 2001;36:347–387. doi: 10.1207/S15327906347-387. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kihlstrom JF, Eich E, Sandbrand D, Tobias BA. Emotion and memory: Implications for self-report. In: Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman HS, Cain VS, editors. The science of self-report: Implications for research and practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 81–99. [Google Scholar]
- King DW, King LA, Foy DW, Gudanowske DM. Prewar factors in combat related posttraumatic stress disorder: Structural equation modeling with national sample of female and male Vietnam veterans. Journal of Consulting and Clinical Psychology. 1996;64:520–531. doi: 10.1037/0022-006X.64.3.520. [DOI] [PubMed] [Google Scholar]
- Kline R. Principles and Practice of Structural Equation Modeling, Third Edition, (Methodology in the social sciences) New York: Guilford Press; 2010. [Google Scholar]
- Koenen KC, Amstadrer AB, Nugent NR. Gene-environment interaction in posttraumatic stress disorder: An update. Journal of Traumatic Stress. 2009;22:416–426. doi: 10.1002/jts.20435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. National Vietnam Veterans Readjustment Study (NVVRS): Description, current status, and initial PTSD prevalence estimates. Washington, DC: Veterans Administration; 1988. [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War Generation. New York: Brunner/Mazel; 1990. [Google Scholar]
- Laufer RS, Gallops MS, Frey-Wouters E. War stress and trauma: The Vietnam veteran experience. Journal of Health and Social Behavior. 1984;25:68–72. doi: 10.2307/2136705. [DOI] [PubMed] [Google Scholar]
- Macklin ML, Metzger LJ, Litz BT, McNally RJ, Lasko NB, Orr SP, et al. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1998;66:323–326. doi: 10.1037/0022-006X.66.2.323. [DOI] [PubMed] [Google Scholar]
- Maguen S, et al. The impact of killing in war on mental health symptoms and related functioning. Journal of Traumatic Stress. 2009;22:435. doi: 10.1002/jts.20451. [DOI] [PubMed] [Google Scholar]
- Maier T. Weathers’ and Keane’s “The Criterion A problem revisited: Controversies and challenges in defining and measuring psychological trauma. Journal of Traumatic Stress. 2007;20:915–916. doi: 10.1002/jts.20294. [DOI] [PubMed] [Google Scholar]
- Marx BP, Foley KM, Feinstein BS, Wolf EJ, Kaloupek DG, Keane TM. Combat-related guilt mediates the relations between exposure to combat related abusive violence and psychiatric diagnoses. Depression and Anxiety. 2010;27:287–295. doi: 10.1002/da.20659. [DOI] [PubMed] [Google Scholar]
- McNair RM. Preparation-induced traumatic stress in combat veterans. Peace and Conflict: Journal of Peace Psychology. 2002;8:63–72. doi: 10.1207/S15327949PAC0801_6. [DOI] [Google Scholar]
- McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology. 2003;54:229–252. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthen and Muthen; 1998–2010. [Google Scholar]
- Nelson D. The War Behind Me. New York: Basic Books; 2008. [Google Scholar]
- O’Toole B, Catts SV, Outram S, Pierce KR, Cockburn J. The physical and mental health of Australian Vietnam veterans 3 decades after the war and its relation to military service, combat, and post-traumatic stress disorder. American Journal of Epidemiology. 2009;170:318–330. doi: 10.1093/aje/kwp146. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of post traumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash . Modern Epidemiology. 3. Philadelphia, Pennsylvania: Lippincot Williams & Wilkins; 2008. [Google Scholar]
- Schlenger WE. Supplemental user’s guide to structured clinical interview for DSM-III-R nonpatient revision (SCID–NP-V) Research Triangle Park, North Carolina: Research Triangle Institute; 1987. [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:85–95. doi: 10.1023/B:JOTS.0000022614.21794.f4. [DOI] [PubMed] [Google Scholar]
- Schwartz S. Modern epidemiologic approaches to interaction: Applications to the study of genetic Interactions. Appendix E. In: Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington D.C: The National Academies Press; 2006. pp. 310–337. [PubMed] [Google Scholar]
- Sellman WS. Project 100 000 testimony and report on the study of Vietnam war era low aptitude military recruits: Statement to the subcommittee on oversight and investigations House Committee on veterans’ affairs 2-28-90. 1990 http://members.aol.com/vetschoice/100-1.htm.
- Smith R. The Utility of Force. Knopf; NY: 2007. [Google Scholar]
- Spitzer R, Williams J, Gibbon M. Structured clinical interview for DSM-III-R. Version NP-V. New York State Psychiatric Institute, Biometrics Research Department; NY: 1987. [Google Scholar]
- Thayer T. War Without Fronts. Westview Press; Boulder, CO: 1985. [Google Scholar]
- Weathers FW, Keane TM. The Criterion A problem revisited: Controversies and challenges in defining and measuring psychological trauma. Journal of Traumatic Stress. 2007;20:107–121. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, et al. The prevalence of lifetime and partial post traumatic stress disorder in Vietnam veterans. Journal of Traumatic Stress. 1992;5:365–376. doi: 10.1002/jts.249005030. [DOI] [Google Scholar]
- Wirth RJ, Edwards MC. Item factor analysis: Current approaches and future directions. Psychological Methods. 2007;12(1):58–79. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yager T, Laufer R, Gallops M. Some problems associated with war experience in men of the Vietnam generation. Archive of General Psychiatry. 1984;41:327–333. doi: 10.1001/arcpsyc.1984.01790150017003. [DOI] [PubMed] [Google Scholar]
- Yehuda R, McFarlane AC. Conflict between current knowledge about posttraumatic stress disorder and its original conceptual basis. American Journal of Psychiatry. 1995;152:1705. doi: 10.1176/ajp.152.12.1705. [DOI] [PubMed] [Google Scholar]