Abstract
Although many studies indicate that people in low quality relationships are less healthy, precisely how relationships influence health remains unclear. We focus on one physiological pathway that may provide clues to understanding the link between relationships and health: the hypothalamic-pituitary-adrenal (HPA) axis. Evidence indicates that attachment processes in adult romantic relationships are associated with HPA responses to stress (assessed via cortisol levels). Specifically, attachment insecurity predicts different cortisol patterns than does attachment security, especially when the stressor potentially threatens the relationship. Thus, attachment may get under the skin through biological responses to attachment-relevant stressors, but further work is needed to pinpoint the complete physiological and behavioral pathways through which attachment may influence health and disease outcomes.
Keywords: relationships, adult attachment, cortisol, affect, health
Many studies have established that social isolation, few social network ties, and having unsupportive close relationships are risk factors for poor emotional and physical health comparable to established risk factors such as smoking (Holt-Lunstad, Smith, & Layton, 2010; House, Landis, & Umberson, 1988). What features of relationships potentially influence emotional and physical health? Is it the mere presence or absence of close bonds with others, the objectively positive or negative qualities of those bonds, or people’s perceptions of and expectations about them that matter? Recent work on the physiological correlates of attachment processes in adult romantic relationships has begun to provide some answers regarding the latter. Through past relationship experiences, people develop distinct lenses through which they interpret events in their current romantic relationships. These different lenses, or attachment styles, are inextricably connected to people’s affective responses to relationship stressors, including physiological reactions to stressors, and their ability to regulate distress.
Most evidence connecting attachment styles to affective reactions comes from studies examining people’s self-reported, consciously accessible affective experiences, but affective reactions occur at multiple levels, including at a less consciously accessible physiological level. Links between attachment and physiological indicators of affective reactions are important to consider because they are distinct from self-reports of distress (Dickerson & Kemeny, 2004; Powers, Pietromonaco, Gunlicks, & Sayer, 2006), and because they offer likely pathways through which attachment-related processes may influence later health and disease outcomes.
In this article, we focus on how attachment styles are connected to physiological stress responses that reflect activation in the HPA axis, which is a major stress response system in humans modulating the release of cortisol. Although other physiological systems (e.g., the sympathetic adrenal medullary axis) are implicated in stress responses (e.g., cardiovascular activity), we focus specifically on HPA responses because a large literature has identified HPA responses as a mechanism through which psychological stress may influence a wide range of mental and physical health outcomes (Dickerson & Kemeny, 2004; Miller, Chen, & Zhou, 2007). This article reviews research suggesting that HPA responses may offer a pathway through which attachment in adult relationships shapes health and disease outcomes. We first provide a brief overview of attachment theory in connection to affect regulation and then discuss evidence demonstrating that attachment styles predict different patterns of cortisol stress responses, especially in attachment-relevant contexts.
Adult Attachment Theory
According to attachment theory, people develop working models of their close relationships that are initially based on experiences with caregivers in childhood but are open to revision based on experiences in later relationships (e.g., with romantic partners) (Bowlby, 1973; Hazan & Shaver, 1987; Mikulincer & Shaver, 2007). These working models consist of sets of expectations, beliefs, and goals about whether a relationship partner will be responsive and whether the self is worthy of love, and they guide people’s reactions in their close relationships (see Mikulincer & Shaver, 2007 and Pietromonaco & Beck, in press).
Working models serve a primary function of the attachment system: to help individuals regulate distress in the face of an actual or perceived threat. The affective response to relationship threat and the particular behavioral and cognitive strategies people use to regulate distress depend on their prior experiences with relationship partners (Mikulincer & Shaver, 2007). Secure individuals trust that partners will be responsive, and they are comfortable with both receiving and giving support to partners; they can apply a variety of constructive strategies to regulate distress, including relying on their partner when needed. Insecure individuals with an anxious attachment style expect that their partner will not be sufficiently responsive, and therefore show a pattern of hyperactivation that calls attention to their distress. Anxious attachment is associated with heightened distress and more intense emotions (e.g., Davis, Shaver, & Vernon, 2003; Hazan & Shaver, 1987; Pietromonaco & Barrett, 1997; Pietromonaco & Carnelley, 1994), and more symptoms of depression (Carnelley, Pietromonaco, & Jaffe, 1994; Simpson, Rholes, Campbell, Tran, & Wilson, 2003). Insecure adults with an avoidant attachment style show a pattern of deactivation, which is marked by avoiding closeness and a preference for self-reliance (see Mikulincer & Shaver, 2007 and Pietromonaco & Beck, in press). Avoidant individuals evidence blunted emotions (Pietromonaco & Barrett, 1997) and suppress their feelings (Fraley & Shaver, 1997). Attachment avoidance, however, is associated with distress and depression under chronic conditions that may tax cognitive resources and interfere with employing self-protective interpersonal distancing strategies to regulate distress (Berant, Mikulincer, & Shaver, 2008; Carnelley et al., 1994; Simpson et al., 2003; see Pietromonaco & Beck, in press).
Attachment and HPA Activation
While research focusing on how attachment relates to the conscious experience and regulation of affect has provided an important first step in understanding links between attachment and health, revealing the physiological components of such experiences is arguably a necessary second step toward fully understanding these links. Thus, we focus next on research examining whether individual differences in adult attachment are related to responses within the HPA axis. When activated by a stressor, the HPA axis initiates a cascade of hormones that trigger the secretion of cortisol from the adrenal cortex into the bloodstream. The release of cortisol influences the metabolic, immune, and nervous systems, which play an important role in health and disease. Cortisol has been flagged as a primary mechanism through which psychological stress may influence health, and disruptions in HPA functioning have been linked to deleterious health outcomes (Miller et al., 2007).
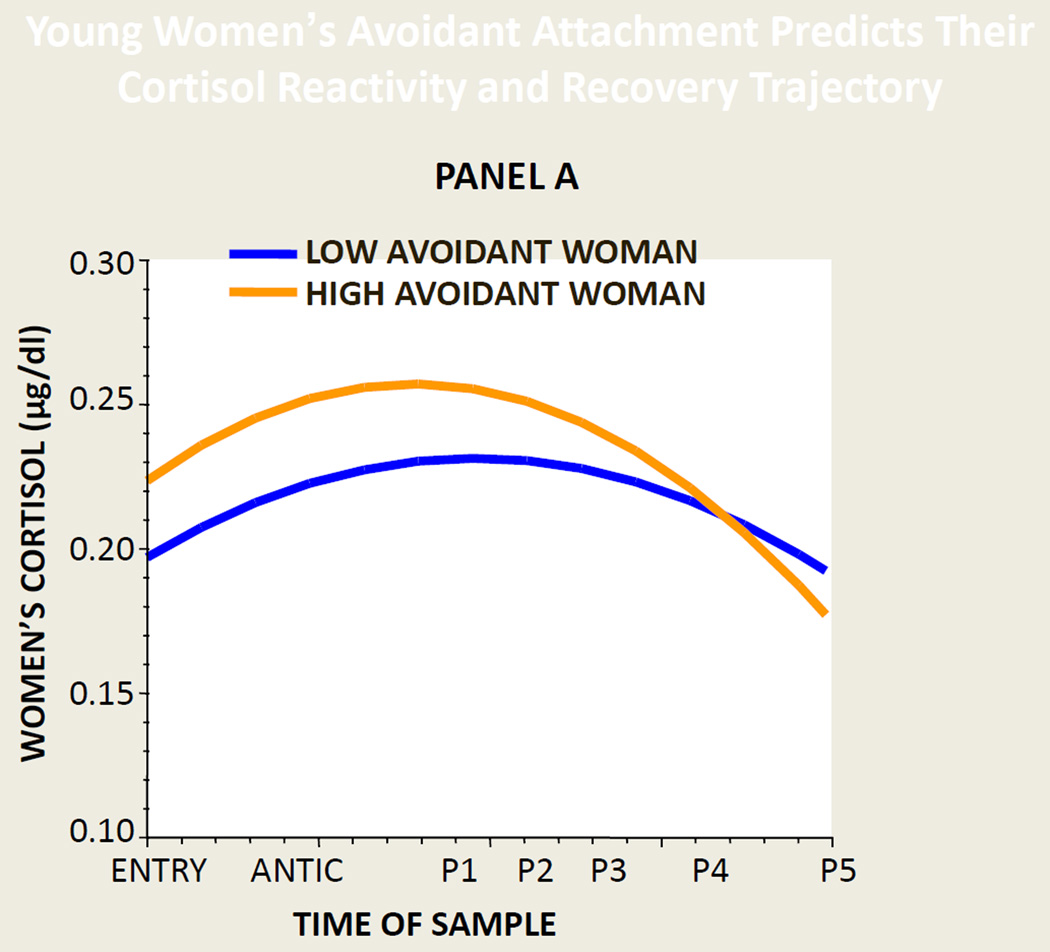
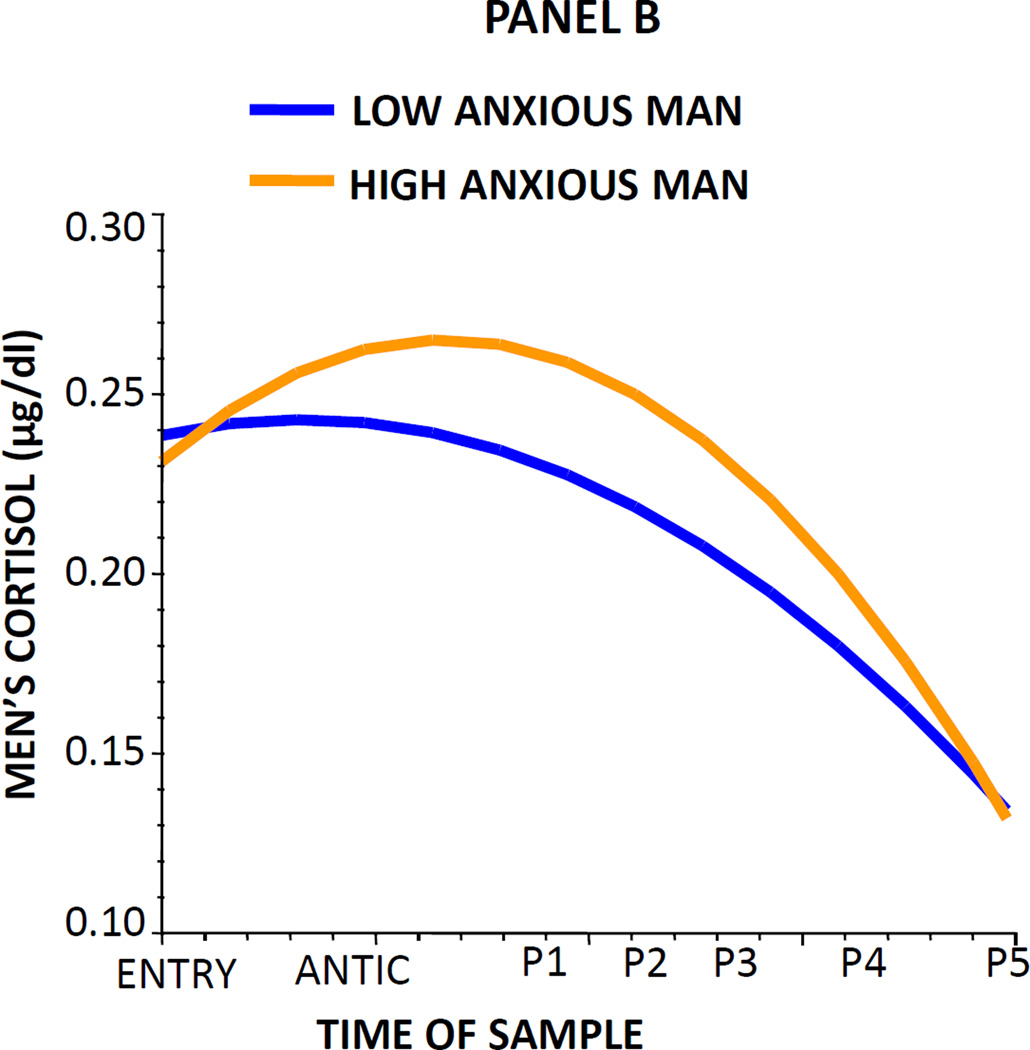
Building on research linking psychological stress and cortisol, relationship researchers have begun to examine cortisol responses as a pathway linking relationship processes to later health outcomes (see Pietromonaco, Uchino, & Dunkel Schetter, in press). A growing literature suggests that how partners perceive and provide support to each other predicts their cortisol responses (Gunlicks-Stoessel & Powers, 2009; Laurent & Powers, 2006). Because adults’ attachment-related anxiety and avoidance within intimate relationships are closely tied to their perceptions of support and provision of support (see Pietromonaco & Beck, in press), researchers have hypothesized that couple members’ levels of attachment anxiety and avoidance could directly contribute to each partner’s cortisol responses to interpersonal stress. Some evidence supports this hypothesis and also suggests that these links differ for women and men. In one study, 124 young dating couples discussed an unresolved conflict in their relationship and provided saliva samples reflecting their cortisol levels before, during, and after the discussion (Powers et al., 2006). Figure 1 (Panel A) indicates that women high (vs. low) in attachment avoidance showed higher cortisol levels when entering the lab and during the discussion, but they recovered rapidly when the discussion ended, a pattern that may reward and perpetuate avoidant coping behavior. Men high (vs. low) in attachment anxiety showed greater cortisol reactivity in anticipating the discussion and recovered more slowly afterwards (Figure 1, Panel B). Furthermore, men evidenced lower cortisol reactivity and quicker recovery when their female partner was more securely attached (and presumably more responsive). These different patterns for men and women may result from different gender role norms for the conflict task (see Powers et al., 2006). Women typically guide discussions of relationship problems, a role that may be difficult for avoidant women who prefer to disengage from conflict. Men, however, are expected to take a less active role, which may produce tension in anxiously attached men who want to share their concerns. We note that one study replicated our findings for anxious men, but not for avoidant women (Brooks, Robles, & Dunkel Schetter, 2011). This study differed from ours in sample size (30 couples) and other ways (e.g., fewer cortisol samples) that may explain these variations. Overall, we expect that contextual features of the stressor task determine when attachment and gender interact but further work is needed to specify when such differences arise.
Figure 1.
Cortisol reactivity and recovery trajectories of two prototypical women with avoidant attachment scores at the 25th and 75th percentile (Panel A) and two prototypical men with anxious attachment scores at the 25th and 75th percentile (Panel B). Time points reflect cortisol levels before entering the lab (entry), when anticipating the conflict discussion (antic), during the discussion (P1), and during the recovery period at approximately 5 (P2), 15 (P3), 30 (P4), and 45 (P5) minutes after the end of the discussion.
Source: Adapted from Powers, S. I., Pietromonaco, P. R., Gunlicks, M., & Sayer, A. Dating couples’ attachment styles and patterns of cortisol reactivity and recovery in response to a relationship conflict. Journal of Personality and Social Psychology, 90, pp. 621–622. 2006, American Psychological Association. Adapted with permission.
Research using other paradigms reveals similar associations between attachment styles and cortisol responses to relationship-related stressors. In one study, participants believed their partner would be interviewed by an attractive opposite-sex experimenter about the intimate details of the partner’s past and current romantic relationships and that they and their partner would later watch a video of the interview (Dewitte, De Houwer, Goubert, & Buysse, 2010). In this situation, greater cortisol reactivity was observed for men who were more anxiously attached and for women who were higher in both attachment anxiety and avoidance (i.e., reflecting “fearful-avoidance,” or a desire for closeness while fearing rejection). In work examining married individuals’ daily cortisol levels before, during, and after a 4–7 day travel-related separation from their spouse, attachment anxiety predicted higher cortisol during the separation, supporting the idea that separation is particularly threatening for those who are preoccupied with closeness (Diamond, Hicks, & Otter-Henderson, 2008).
Overall, attachment patterns have been consistently linked to cortisol responses in situations that provoke an attachment threat, such as a conflict discussion within a close relationship. The picture is less clear for studies examining stressful contexts that are not specifically attachment-related. For example, two studies using a psychosocial challenge task did not find a link between attachment and cortisol patterns (Ditzen et al., 2008; Smeets, 2010); however, another study found that anxious attachment predicted greater cortisol reactivity to a task involving uncontrollable noise (Quirin, Pruessner, & Kuhl, 2008). Additional work is needed to understand links between attachment and cortisol in attachment-relevant contexts, other interpersonal contexts (e.g., tasks involving strangers), and in non-interpersonal contexts.
Most research has focused on cortisol reactivity to a specific stressor (e.g., conflict, separation), but naturally-occurring daily cortisol patterns are of interest because a flatter pattern of cortisol at awakening and over the day can co-occur with adverse health outcomes such as depression (Hsiao et al., 2010). This flatter pattern contrasts with more normative daily cortisol patterns in which people experience a marked rise in cortisol about 30 minutes after waking up followed by a gradual decline in cortisol over the day. Some work indicates that more anxiously attached individuals show a blunted cortisol response after awakening (Hicks & Diamond, 2011; Quirin et al., 2008), suggesting dysregulated HPA activation. Recent work, however, found that anxious attachment predicted higher cortisol levels over 2 days following a marital problem discussion, but patterns did not vary by time of day (Jaremka et al., in press). These few studies of attachment style and diurnal cortisol differ considerably in methodology, and thus more work is required to clarify this link (Hicks & Diamond, 2011).
Conclusions and Future Directions
Attachment styles shape not only people’s perceptions of distress but also their cortisol stress responses, which have been connected in separate work to health and disease outcomes. The findings reviewed here indicate that attachment insecurity is associated with different cortisol response patterns than attachment security. These differential responses may be especially likely to emerge in contexts that are relevant to attachment such as interpersonal conflict or separation.
Research also suggests that another aspect of the situational context—the partner’s attachment characteristics—needs to be considered in evaluating biological stress responses. Emerging evidence suggests that one relationship partner’s attachment style may influence the other’s physiological stress reactions (e.g., Laurent & Powers, 2007; Powers et al., 2006). Indeed, new findings from a study of 218 newlywed couples indicate that the interplay between spouses’ attachment styles predicts their cortisol patterns (Beck, Pietromonaco, DeBuse, Powers, & Sayer, 2012). Couples including an anxiously attached wife and an avoidant husband showed a sharp increase in cortisol followed by a rapid decline in anticipation of a conflict discussion, and this pattern was distinct from those observed for other attachment pairings (e.g., an anxious wife with a non-avoidant husband). Although the mechanisms underlying such partner effects remain to be determined, they may follow from different expectations based on recurring interaction patterns in the relationship. For example, anxious wife-avoidant husband couples evidence difficulty constructively engaging during the conflict discussion, which may explain their physiological disengagement even before the interaction begins (Beck et al., 2012). Given the potential for partners to influence each other’s physiological responses and downstream health outcomes (see Pietromonaco et al., in press), examining the interplay between partners’ attachment styles and the mechanisms through which partners influence each other represents an important avenue for future research.
Research also is needed to understand the complete physiological and behavioral pathways through which attachment is linked to differential health outcomes. For example, avoidantly attached married individuals showed an increased inflammatory response (IL-6) after a conflict interaction with their spouse but not after a support interaction (Gouin et al., 2009). Other work indicates that both attachment anxiety and daily levels of cortisol are associated with lower cellular immunity (Jaremka et al., in press). Immune responses may precede HPA axis responses (Sapolsky, Romero, & Munck, 2000), and inflammation is prognostic of a host of negative health consequences (Kiecolt-Glaser, Gouin, & Hantsoo, 2010). Conversely, cortisol can inhibit immune responses (Sapolsky et al., 2000), which may increase susceptibility to infectious disease. Supportive romantic relationships also promote health-enhancing behaviors (e.g., exercise, nutrition), while unsupportive relationships hinder such behaviors (Kiecolt-Glaser et al., 2010), and attachment dynamics likely play a key role in determining whether individuals perceive their relationships as supportive or not.
Another critical question is whether attachment patterns in childhood, which are related to children’s cortisol reactivity (e.g., Gunnar, Brodersen, Nachmias, Buss, & Rigatuso, 1996), predict cortisol responses in adulthood. Furthermore, cortisol patterns show some stability over the course of development (e.g., from childhood to adolescence, Shirtcliff et al., 2012), and it would be important to know whether such individual differences in cortisol patterns are related to attachment in childhood, adulthood, or both. Answering questions such as these will illuminate the role of attachment patterns and associated relationship processes across the life span in contributing to health outcomes.
The findings reviewed here suggest that patterns of HPA activation and related biological responses may provide a key pathway connecting attachment-related processes to health and disease outcomes. Understanding the role of attachment processes in health outcomes may suggest ways in which health care systems might more effectively use close relationship networks in treatment and prevention efforts, or potentially underscore the importance of supportive family policies for improved health outcomes. However, no studies have yet determined whether biological responses to relationship-related stressors lead to detrimental health outcomes over time. Research examining this question will enhance our understanding of how attachment-related relationship processes get “under the skin.”
Acknowledgments
Preparation of this article was supported by a grant (R01 CA133908) from the National Cancer Institute to Paula Pietromonaco and Sally Powers and a graduate research fellowship (S121000000211) from the National Science Foundation to Casey DeBuse. Some of the research described here was supported by a grant (R01 MH60228-01A1) from the National Institute of Mental Health to Sally Powers.
Footnotes
Recommended Readings
Diamond, L. M., & Fagundes, C. P. (2010). Psychobiological research on attachment. Journal of Social and Personal Relationships, 27(2), 218–225. doi:10.1177/0265407509360906. An overview and analysis of connections between adult attachment and a broader range of psychophysiological responses than covered in this article.
Miller, G. E., Chen, E., & Zhou, E. S. (2007). See reference list. A comprehensive review and analysis of the link between chronic stress and hypothalamic-pituitary-adrenal axis functioning.
Pietromonaco, P. R., & Beck, L. A. (in press). See reference list. This chapter provides an accessible review of theory and research on attachment processes in adult romantic relationships.
Pietromonaco, P. R., Uchino, B., & Dunkel Schetter, C. (in press). See reference list. This article discusses the significance of attachment processes for research in several health domains (e.g., health behavior, pain, chronic disease) and its implications for health-related interventions.
Powers, S. I., Pietromonaco, P. R., Gunlicks, M., & Sayer, A. (2006). See reference list. The first empirical study to demonstrate links between adult attachment insecurity and dating partners’ cortisol patterns in reaction to a conflict negotiation task.
References
- Beck LA, Pietromonaco PR, DeBuse CJ, Powers SI, Sayer AG. Spouses’ attachment pairings predict neuroendocrine, behavioral and psychological responses to marital conflict. Amherst: University of Massachusetts; 2012. Unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berant E, Mikulincer M, Shaver PR. Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: A 7-year study of children with congenital heart disease. Journal of Personality. 2008;76(1):31–65. doi: 10.1111/j.1467-6494.2007.00479.x. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 2. Separation: Anxiety and anger. New York: Basic Books; 1973. [Google Scholar]
- Brooks KP, Robles TF, Schetter CD. Adult attachment and cortisol responses to discussions with a romantic partner. Personal Relationships. 2011;18(2):302–320. [Google Scholar]
- Carnelley KB, Pietromonaco PR, Jaffe K. Depression, working models of others, and relationship functioning. Journal of Personality and Social Psychology. 1994;66(1):127–140. doi: 10.1037//0022-3514.66.1.127. [DOI] [PubMed] [Google Scholar]
- Davis D, Shaver PR, Vernon ML. Physical, emotional, and behavioral reactions to breaking up: The roles of gender, age, emotional involvement, and attachment style. Personality and Social Psychology Bulletin. 2003;29(7):871–884. doi: 10.1177/0146167203029007006. [DOI] [PubMed] [Google Scholar]
- Dewitte M, De Houwer J, Goubert L, Buysse A. A multi-modal approach to the study of attachment-related distress. Biological Psychology. 2010;85(1):149–162. doi: 10.1016/j.biopsycho.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Diamond LM, Hicks AM, Otter-Henderson KD. Every time you go away: Changes in affect, behavior, and physiology associated with travel-related separations from romantic partners. Journal of Personality and Social Psychology. 2008;95(2):385–403. doi: 10.1037/0022-3514.95.2.385. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Ditzen B, Schmidt S, Strauss B, Nater UM, Ehlert U, Heinrichs M. Adult attachment and social support interact to reduce psychological but not cortisol responses to stress. Journal of Psychosomatic Research. 2008;64(5):479–486. doi: 10.1016/j.jpsychores.2007.11.011. [DOI] [PubMed] [Google Scholar]
- Fraley RC, Shaver PR. Adult attachment and the suppression of unwanted thoughts. Journal of Personality and Social Psychology. 1997;73:1080–1091. doi: 10.1037//0022-3514.73.5.1080. [DOI] [PubMed] [Google Scholar]
- Gouin J, Glaser R, Loving TJ, Malarkey WB, Stowell J, Houts C, Kiecolt-Glaser JK. Attachment avoidance predicts inflammatory responses to marital conflict. Brain, Behavior, and Immunity. 2009;23(7):898–904. doi: 10.1016/j.bbi.2008.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunlicks-Stoessel ML, Powers SI. Romantic partners’ coping strategies and patterns of cortisol reactivity and recovery in response to relationship conflict. Journal of Social & Clinical Psychology. 2009;28(5):630–649. doi: 10.1521/jscp.2009.28.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazan C, Shaver P. Romantic love conceptualized as an attachment process. Journal of Personality and Social Psychology. 1987;52(3):511–524. doi: 10.1037//0022-3514.52.3.511. [DOI] [PubMed] [Google Scholar]
- Hicks AM, Diamond LM. Don’t go to bed angry: Attachment, conflict, and affective and physiological reactivity. Personal Relationships. 2011;18(2):266–284. [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7(7):1–20. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hsiao F-H, Yang T-T, Ho RTH, Jow G-M, Ng S-M, Chan CLW, Lai Y-M, et al. The self-perceived symptom distress and health-related conditions associated with morning to evening diurnal cortisol patterns in outpatients with major depressive disorder. Psychoneuroendocrinology. 2010;35(4):503–515. doi: 10.1016/j.psyneuen.2009.08.019. [DOI] [PubMed] [Google Scholar]
- Jaremka L, Glaser R, Loving T, Malarkey W, Stowell J, Kiecolt-Glaser J. Attachment anxiety is linked to alterations in cortisol production and cellular immunity. Psychological Science. doi: 10.1177/0956797612452571. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin J, Hantsoo L. Close relationships, inflammation, and health. Neuroscience & Biobehavioral Reviews. 2010;35(1):33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent HK, Powers SI. Social-cognitive predictors of hypothalamic-pituitary-adrenal reactivity to interpersonal conflict in emerging adult couples. Journal of Social and Personal Relationships. 2006;23(5):703–720. [Google Scholar]
- Laurent H, Powers S. Emotion regulation in emerging adult couples: Temperament, attachment, and HPA response to conflict. Biological Psychology. 2007;76(1–2):61–71. doi: 10.1016/j.biopsycho.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. New York, NY US: Guilford Press; 2007. [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic- pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133(1):25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Pietromonaco PR, Barrett LF. Working models of attachment and daily social interactions. Journal of Personality and Social Psychology. 1997;73(6):1409–1423. doi: 10.1037//0022-3514.73.6.1409. [DOI] [PubMed] [Google Scholar]
- Pietromonaco PR, Beck LA. Attachment processes in adult romantic relationships. In: Simpson JA, Dovidio J, editors. Handbook of interpersonal relations and group processes. Washington, DC: American Psychological Association; (in press). To appear in. [Google Scholar]
- Pietromonaco PR, Carnelley KB. Gender and working models of attachment: Consequences for perceptions of self and romantic relationships. Personal Relationships. 1994;1(1):63–82. [Google Scholar]
- Pietromonaco PR, Uchino B, Dunkel Schetter C. Close relationship processes and health: Implications of attachment theory for health and disease. Health Psychology. doi: 10.1037/a0029349. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers SI, Pietromonaco PR, Gunlicks M, Sayer A. Dating couples’ attachment styles and patterns of cortisol reactivity and recovery in response to a relationship conflict. Journal of Personality and Social Psychology. 2006;90(4):613–628. doi: 10.1037/0022-3514.90.4.613. [DOI] [PubMed] [Google Scholar]
- Quirin M, Pruessner JC, Kuhl J. HPA system regulation and adult attachment anxiety: Individual differences in reactive and awakening cortisol. Psychoneuroendocrinology. 2008;33(5):581–590. doi: 10.1016/j.psyneuen.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Allison AL, Armstrong JM, Slattery MJ, Kalin NH, Essex MJ. Longitudinal stability and developmental properties of salivary cortisol levels and circadian rhythms from childhood to adolescence. Developmental Psychobiology. 2012;54(5):493–502. doi: 10.1002/dev.20607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson JA, Rholes WS, Campbell L, Tran S, Wilson CL. Adult attachment, the transition to parenthood, and depressive symptoms. Journal of Personality and Social Psychology. 2003;84(6):1172–1187. doi: 10.1037/0022-3514.84.6.1172. [DOI] [PubMed] [Google Scholar]
- Smeets T. Autonomic and hypothalamic–pituitary–adrenal stress resilience: Impact of cardiac vagal tone. Biological Psychology. 2010;84(2):290–295. doi: 10.1016/j.biopsycho.2010.02.015. [DOI] [PubMed] [Google Scholar]