Abstract
Background:
Psychiatric illnesses are an important group of co-morbidities that can occur among patients with non-communicable diseases (NCDs). Both these chronic conditions have an important implication in terms of quality of life, general well-being and cost of treatment and general longevity of the patient. The objectives of our study were to assess the burden of psychiatric co-morbidities among patients with select NCDs and to identify the determinants associated with them.
Methods:
A cross-sectional study was conducted at the outpatient departments (OPDs) of Government District Hospital, Mangalore. The study was conducted among patients with select NCDs viz. diabetes mellitus, hypertension, ischemic heart diseases and their combinations attending OPDs of Government District Hospital, Mangalore. Participants were interviewed using Patient Health Questionnaire-Somatic, Anxiety and Depressive Symptoms. Data analysis was performed using SPSS version 11.0 (SPSS Inc., 233 South Wacker Drive, 11th floor, Chicago, IL 60606-6412). Bivariate and logistic regression analyses were performed to test the association between different variables.
Results:
Among the 282 study participants, psychiatric illnesses observed were somatization (n = 99, 35.1%), anxiety (n = 54, 19.1%) and depression (n = 82, 29.1%). Bivariate analysis showed significant negative association (P <0.05) between psychiatric illness and factors such as education, marital status, age <60 years, duration of illness of <10 years. However, on multivariate analysis only marital status (odds ratio [OR]: 0.500, confidence interval [CI]: 0.321-0.777, P = 0.002) and duration of illness (OR: 0.651, CI: 0.439-0.967, P = 0.032) were found to be significantly associated negatively with depression and anxiety.
Keywords: Mental health, non-communicable diseases, psychiatric illnesses, South India
INTRODUCTION
Non-communicable diseases (NCDs) are a group of conditions/diseases, which are non-infectious and non-transmissible among people. The common NCDs include diabetes, hypertension (HTN), ischemic heart diseases (IHDs), cancers, osteoporosis and chronic kidney diseases. NCDs are fast replacing communicable diseases as the major cause of death and disability world-wide. NCDs were responsible for 36 million (63%) deaths among a total of 57 million deaths world-wide in the year 2008.[1] Like many other developing countries in the world, India too is experiencing an epidemiological transition resulting in increased burden of NCDs due to industrialization, socio-economic development, urbanization, changing age-structure, changing life-styles. In India, NCDs are estimated to account for 53% of all deaths and 44% of disability-adjusted life-years lost in 2005.[2] Apart from being responsible for the increasing number of deaths, these groups of diseases are also associated with various types of co-morbidities due to their chronic nature. These co-morbidities include diseases such as diabetic micro-vascular pathology resulting in peripheral neuropathies, gastrointestinal abnormalities, renal abnormalities, retinal abnormalities etc.
Psychiatric illnesses are another important group of co-morbidities that can occur among patients with NCDs. The co-existence of psychiatric disorders with various NCDs is an important phenomenon, as both tend to be chronic in nature and have important implications in terms of quality of life, general well-being and cost of treatment and general longevity of the patient. Available evidence suggests increasing prevalence of psychiatric co-morbidities among NCD patients.[3,4,5,6,7,8] The current study was carried out to assess the burden of psychiatric co-morbidities among patients with select NCDs and to identify the determinants associated with them.
METHODS
This cross-sectional study was conducted at Government Wenlock Hospital, Mangalore which is an associate hospital of Kasturba Medical College under public private partnership. It is a tertiary care hospital located in the urban area of Mangalore city. The hospital caters to around 500-700 patients every day and provides general out-patient, specialist and super-specialty services. The study was carried out during February and March 2012. A sample of 282 participants was calculated considering a power of 80%, confidence level of 95%, absolute precision of 6% and considering prevalence of psychiatric disorders among patients with various NCDs to be 30%[9] and a non-response rate of 20%. Convenient sampling method was used for recruiting the participants into the study.
The study group participants were recruited from patients visiting the hospital with physician diagnosed NCDs viz. Diabetes mellitus (DM) type-II, HTN and IHDs either alone or in combination with each other and disease duration of more than 1 year. Socio-demographic and clinical information was collected from the participants using Patient Health Questionnaire-Somatic, Anxiety and Depressive Symptoms (PHQ-SADS).[10] The PHQ-SADS contains 3 parts viz. PHQ-15 to assess somatic functions, Generalized anxiety disorder-7 to assess anxiety and PHQ-9 to assess depression. The PHQ-SADS questionnaire is a validated questionnaire, which is found to be useful in screening of patients for psychiatric illnesses world-wide.[11,12,13,14,15] In view of ethical rules, patients screened and found positive on the PHQ were referred to Psychiatric Outpatient Departments of the Government Wenlock Hospital, Mangalore for further evaluation. Ethical clearance to conduct the study was obtained from the Institutional Ethics Committee of Kasturba Medical College, Mangalore. A written informed consent was obtained from the study participants prior to inclusion in the study. All the information collected from the participants was kept confidential.
Statistical analysis
The information collected from the participants was analyzed using SPSS (Statistical Package for Social Sciences) version 11.0 computer software (SPSS, Inc., Chicago, IL, USA). The data was analyzed in terms of descriptive statistics as well as bivariate analysis (Chi-square test). We undertook both unadjusted and adjusted logistic regression to assess the association between socio-demographic variables (age, sex, marital status, literacy, place of residence etc.), clinical variables (type of NCD and duration of illness) and psychiatric disorders. The fit of the logistic model was assessed with the Hosmer and Lemeshow goodness-of-fit test; P <0.05 was considered evidence of a statistically significant difference between predictive and outcome variables. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) are reported.
RESULTS
A total of 282 patients with various NCDs participated in our study. Among them, 159 participants (56.4%) were males and 123 (43.6%) were females. The mean age of study participants was 53.2 ± 7.2 years. Majority of the study participants (n = 240, 85.1%) were non-smokers and did not consume alcohol. The socio-demographic characteristics of the study participants are presented in Table 1. Type 2 DM constituted of 44.7% (n = 126) NCDs, followed by HTN 16.3% (n = 46) and IHD 2.5% (n = 7). DM and HTN were co-morbid in 30.5% (n = 86) of the study participants followed by HTN and IHD (n = 7, 2.5%) and DM and IHD (n = 5, 1.8%). All three were co-morbid in 5 cases (1.8%) [Table 2].
Table 1.
Profile of study participants (n=282)
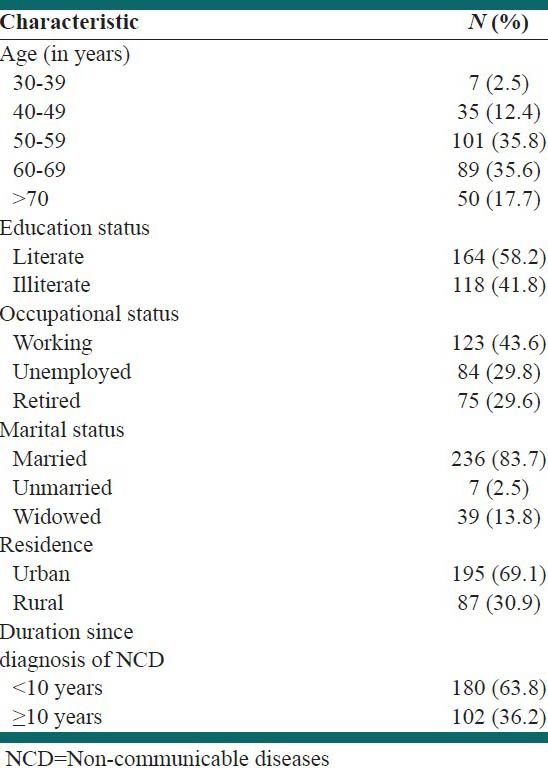
Table 2.
Prevalence of somatization, anxiety and depression among different NCDs
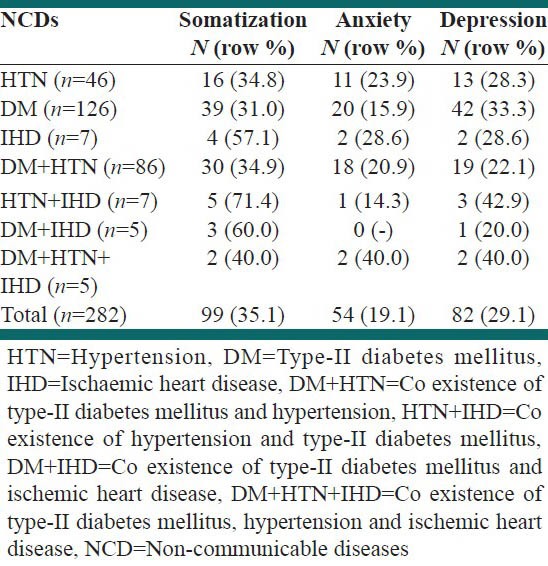
Among the various NCDs the overall proportion of symptoms of somatization, anxiety and depression were found to be 35.1% (n = 99), 19.1% (n = 54) and 29.1% (n = 82) respectively [Table 2]. Among patients with symptoms of anxiety disorders (n = 54), 88.9% (n = 48) of them had mild and 11.1% (n = 6) showed moderate anxiety symptoms. None of the participants had symptoms of severe anxiety disorders. Among patients with depressive symptoms (n = 82), 87.8% (n = 72) had mild, 11.0% (n = 9) had moderate and 1.2% (n = 1) had moderately severe symptoms of depression. The proportion of symptoms of somatization, anxiety and depression across various NCDs is shown in Table 2. A higher proportion of patients with HTN and IHD showed evidence of symptoms of somatization and depression, whereas symptoms of anxiety were proportionately higher among patients suffering from DM, HTN and IHD.
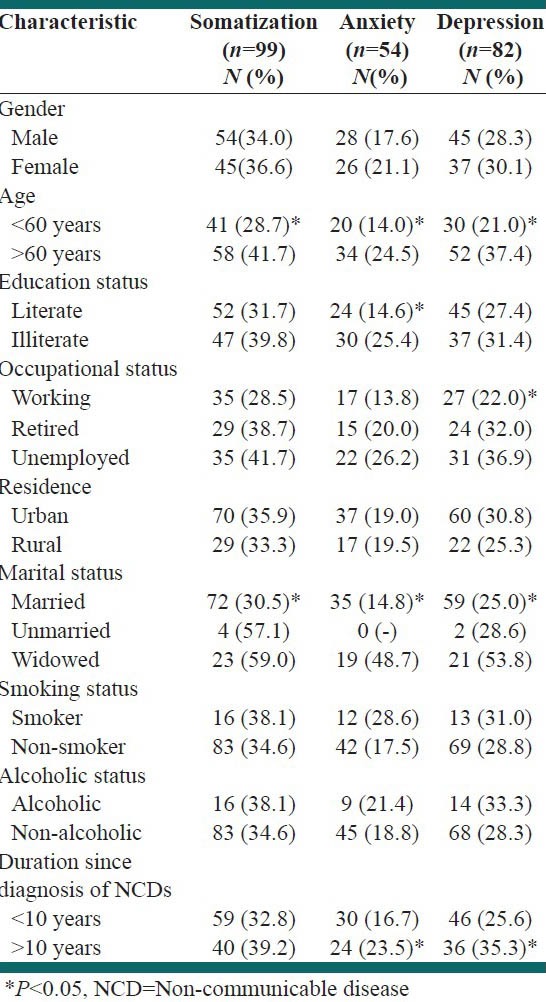
The symptoms of somatization and depression were found to be proportionately higher among female subjects, patients aged more than 60 years, illiterates, unemployed and retired participants, urban residents, unmarried and widowed subjects, smokers, alcoholics and those with duration of NCDs more than 10 years. However, statistically significant prevalence of somatization symptoms was observed among patients more than 60 years of age and unmarried/widowed patients. Similarly, statistically significant prevalence of depression symptoms was observed among patients who were more than 60 years, unemployed, unmarried/widowed and with more than 10 years duration of NCDs. Anxiety symptoms were found to be higher among females, patients aged more than 60 years, illiterates, unemployed and retired persons, rural residents, widowed subjects, smokers, alcoholics and those with NCD duration of more than 10 years. Statistically significant prevalence of anxiety symptoms were observed among patients more than 60 years of age, illiterate patients, unmarried/widowed patients and those with NCD duration of more than 10 years [Table 3].
Table 3.
Prevalence (%) of somatization, anxiety and depression across various socio-demographic subgroups
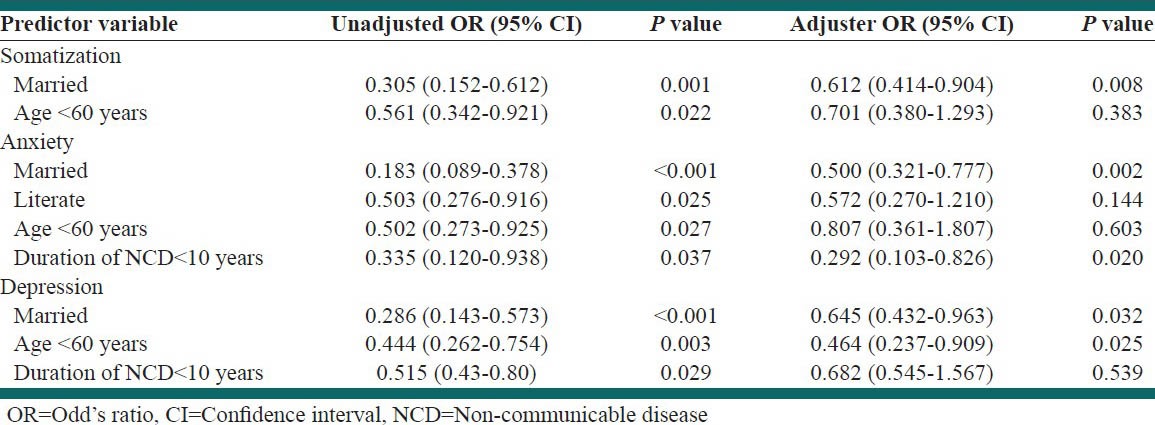
Binary logistic regression revealed significant negative association between somatization symptoms and variables like marriage (OR: 0.305 CI: 0.152-0.612, P = 0.001) and age <60 years (OR: 0.561 CI: 0.342-0.921, P = 0.022). However, after adjusting for variables such as age, sex, literacy status, duration of NCD etc., marriage was the only significant factor (OR: 0.612 CI: 0.414-0.904, P = 0.008) found to be negatively associated with symptoms of somatization. Socio-demographic variables like literacy (OR: 0.503, CI: 0.276-0.916, P = 0.025), marriage (OR: 0.183, CI: 0.089-0.378, P = 0.001), duration of illness (NCD) <10 years (OR: 0.335 CI: 0.120-0.938, P = 0.037) and age <60 years (OR: 0.502, CI: 0.273-0.925, P = 0.027) were found to be negatively associated with symptoms of anxiety disorders on binary logistic regression analysis. However, after adjusting for other socio-demographic variables only marriage (OR: 0.500, CI: 0.321-0.777, P = 0.002) and duration of illness (OR: 0.292, 0.103-0.826, P = 0.002) were found to be significantly associated with symptoms of anxiety disorders. Symptoms of depression were found to be negatively associated with variables like marriage (OR: 0.286, CI: 0.143-0.573, P <0.001), duration of illness <10 years (OR: 0.444 CI: 0.262-0.754, P = 0.003) and age <60 years (OR: 0.515 CI: 0.430-0.800, P = 0.029) upon binary logistic analysis. However, after adjusting for age, sex, literacy and duration of illness, marriage (OR: 0.645, CI: 0.432-0.963, P = 0.032) and age <60 years (OR: 0.464 CI: 0.237-0.909, P = 0.025) were only significantly associated with symptoms of depression [Table 4].
Table 4.
Factors associated with psychiatric co-morbidities among the study participants
DISCUSSION
In the present study, more than half of the study participants (53.3%) were aged more than 60 years. As per the existing national statistics, individuals aged above 60 years constitute 7.5% of the total population.[16] A proportionately higher number of older patients in our study can be attributed to the fact that NCDs are commonly age related diseases and in the majority of the cases the diagnosis tends to be delayed due to late manifestations and detection of the diseases. The majority of study participants were diagnosed with type-II DM followed by combined DM and HTN. Our observations are in accordance with the existing prevalence of various NCDs in India, where type-II DM tops the chart with prevalence of >20%.[17]
The prevalence of somatization symptoms were found to be 35.1% among the study participants which was found to be consistent with the available evidence where the prevalence of somatization was found to be ranging from 3.7% to 52% respectively.[18,19,20] The prevalence of somatization symptoms was associated significantly with age <60 years and marriage on bivariate analysis. However, after adjusting for other variables, marriage was the only variable with which somatization was found to be significantly associated. This may be due to the observation that psychological distress as a result of chronic illness and prolonged medication tends to be low among people who are married and are <60 years of age. Whether this is explained by age or by better marital life is only hypothetical and needs detailed study. However, a cautionary note is to be exercised when drawing conclusions from this finding as several old age related diseases such as osteoporosis, osteoarthritis and post-menopausal syndrome might mimic symptoms of somatization and this study did not collect any information regarding these illnesses nor exclude them specifically.
The prevalence of anxiety symptoms was found to be 19.1% among our study participants. The prevalence was found to be higher among females, persons aged more than 60 years, illiterates, unemployed and retired persons, rural residents, widowed subjects, smokers, alcoholics and those with illness duration of more than 10 years. Among these factors, only marriage and duration of illness <10 years were found to be significantly associated with anxiety after multivariate analysis. Our findings are similar to those observed in studies conducted elsewhere.[6,7,8,21,22,23] The relationship between anxiety and development of NCDs is yet to be understood completely and conflicting evidences regarding the causative pathway between anxiety and HTN still needs to be evaluated. Our study identifies two factors viz. marriage and duration of NCD <10 years to be protective against anxiety among patients with NCDs.
The prevalence of depressive symptoms was found to be 29.1% among the study participants. The prevalence observed in our study is higher when compared with the studies conducted in India and abroad.[4,5,22,24,25,26,27] However, our observations in general are consistent with the prevalence of depression reported by World Health Organization[28] for developing countries like India (10-44%). The factors which were found to be associated with depression were marriage and age <60 years, which were found to be protective against the development of depression.
To summarize, marriage or companionship and short durations of untreated illness have a lower risk of developing psychiatric co-morbidities among patients with NCDs. Since India is currently implementing the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke which is a large scale program for the prevention and control of NCDs, we believe that this program should include mental health as one of its components. Apart from providing treatment to the existing ailments, there is also a need for development of support systems in the community and provide psychiatric counseling to patients diagnosed with NCDs in order to combat the increasing burden of mental health illness and to promote healthy ageing. Future research in this area needs to be conducted to address the mental health needs of patients diagnosed with NCDs.
The strength of the present study is that it reports the prevalence of multiple psychiatric disorders among a fairly adequate sample of patients diagnosed with NCDs using a valid screening tool. The limitations of our study are primarily due to the study settings, which may limit the generalizability of the findings. Furthermore, our study did not include any information in relation to common old age diseases such as osteoporosis, osteoarthritis etc., which mimic symptoms of somatization, which might have led to a higher prevalence of somatization in our study. The other limitation may be a relatively smaller sample size of NCDs like IHDs and other combinations of NCDs that could have influenced the study findings.
ACKNOWLEDGMENT
The authors are grateful to the study participants’ who voluntarily participated in the study. The authors would also like to thank Dr. Sahoo Saddichha, Clinical Fellow, Department of Psychiatry, University of British Columbia, Vancouver, British Columbia, Canada, who's critical inputs were vital in formation of this manuscript. We wish to acknowledge Manipal University for encouraging research and its publication in international journals of repute.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Burden: Mortality, morbidity and risk factors. Global Status Report on Non-communicable Diseases. 2010. [Last accessed on 2012 Oct 01]. Available from: http://www.who.int/nmh/publications/ncd_report_chapter 1.pdf .
- 2.World Health Organization. Mortality and Burden of Disease Estimates for WHO Member States in. 2004. [Last accessed on 2012 Oct 12]. Available from: http://www.who int/entity/healthinfo/global_burden_disease/gbddeathdalycountryestimates2004xls 2009 .
- 3.Asghar S, Hussain A, Ali SM, Khan AK, Magnusson A. Prevalence of depression and diabetes: A population-based study from rural Bangladesh. Diabet Med. 2007;24:872–7. doi: 10.1111/j.1464-5491.2007.02136.x. [DOI] [PubMed] [Google Scholar]
- 4.Guruprasad KG, Niranjan MR, Ashwin S. A study of association of depressive symptoms among the type 2 diabetic outpatients presenting to a tertiary care hospital. Indian J Psychol Med. 2012;34:30–3. doi: 10.4103/0253-7176.96153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poongothai S, Anjana RM, Pradeepa R, Ganesan A, Umapathy N, Mohan V. Prevalence of depression in relation to glucose intolerance in urban south Indians: The Chennai Urban Rural Epidemiology Study (CURES-76) Diabetes Technol Ther. 2010;12:989–94. doi: 10.1089/dia.2010.0081. [DOI] [PubMed] [Google Scholar]
- 6.Gois C, Dias VV, Raposo JF, do Carmo I, Barbosa A. Vulnerability to stress, anxiety and depressive symptoms and metabolic control in type 2 diabetes. BMC Res Notes. 2012;5:271. doi: 10.1186/1756-0500-5-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Saffar NM, Saeed DA. Generalized anxiety disorder in type 2 diabetes mellitus in Suleimaniya city. Tikrit Medical Journal. 2009;15:78–85. [Google Scholar]
- 8.Grimsrud A, Stein DJ, Seedat S, Williams D, Myer L. The association between hypertension and depression and anxiety disorders: Results from a nationally-representative sample of South African adults. PLoS One. 2009;4:e5552. doi: 10.1371/journal.pone.0005552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coelho FM, Pinheiro RT, Horta BL, Magalhães PV, Garcias CM, Silva CV. Common mental disorders and chronic non-communicable diseases in adults: A population-based study. Cad Saude Publica. 2009;25:59–67. doi: 10.1590/s0102-311x2009000100006. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer RL, Williams JB, Kroenke K. Patient Health Questionnaire (PHQ-SADS) [Last accessed on 2012 Jan 28]. Available from: http://www.phqscreeners.com/pdfs/05_PHQ-SADS/English.pdf .
- 11.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Reliability and validity of a modified PHQ-9 item inventory (PHQ-12) as a screening instrument for assessing depression in Asian Indians (CURES-65) J Assoc Physicians India. 2009;57:147–52. [PubMed] [Google Scholar]
- 12.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: The PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–21. [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Census of India. Office of the Registrar General of India. [Last accessed on 2012 Oct 15]. Available from: http://www.censusindia.gov.in/Census_Data_2001/India_at_glance/broad.aspx .
- 17.Anjana RM, Ali MK, Pradeepa R, Deepa M, Datta M, Unnikrishnan R, et al. The need for obtaining accurate nationwide estimates of diabetes prevalence in India-Rationale for a national study on diabetes. Indian J Med Res. 2011;133:369–80. [PMC free article] [PubMed] [Google Scholar]
- 18.Oshodi YO, Adeyemi JD, Oke DA, Seedat S. Psychiatric morbidity in hypertensives attending a cardiology outpatient clinic in West Africa. Niger J Clin Pract. 2012;15:84–8. doi: 10.4103/1119-3077.94105. [DOI] [PubMed] [Google Scholar]
- 19.Kruse J, Schmitz N, Thefeld W. German National Health Interview and Examination Survey. On the association between diabetes and mental disorders in a community sample: Results from the German National Health Interview and Examination Survey. Diabetes Care. 2003;26:1841–6. doi: 10.2337/diacare.26.6.1841. [DOI] [PubMed] [Google Scholar]
- 20.Bener A, Ghuloum S, Al-Mulla AA, Al-Marri S, Hashim MS, Elbagi IE. Prevalence of somatisation and psychologisation among patients visiting primary health care centres in the State of Qatar. Libyan J Med. 2010 Jun 16;5:01–08. doi: 10.3402/ljm.v5i0.5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hermanns N, Kulzer B, Krichbaum M, Kubiak T, Haak T. Affective and anxiety disorders in a German sample of diabetic patients: Prevalence, comorbidity and risk factors. Diabet Med. 2005;22:293–300. doi: 10.1111/j.1464-5491.2005.01414.x. [DOI] [PubMed] [Google Scholar]
- 22.Chaudhry R, Mishra P, Mishra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: A hospital-based study. Ind Psychiatry J. 2010;19:47–9. doi: 10.4103/0972-6748.77637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roupa Z, Koulouri A, Sotiropoulou P, Makrinika E, Marneras X, Lahana I, et al. Anxiety and depression in patients with type 2 diabetes mellitus, depending on sex and body mass index. Health Sci J. 2009;3:32–40. [Google Scholar]
- 24.Lin CH, Lee YY, Liu CC, Chen HF, Ko MC, Li CY. Urbanization and prevalence of depression in diabetes. Public Health. 2012;126:104–11. doi: 10.1016/j.puhe.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 25.Jimenez-Garcýa R, Martinez Huedo MA, Hernandez-Barrera V, Lopez de Andres A, Martinez D, Jimenez-Trujillo I, et al. Psychological distress and mental disorders among Spanish diabetic adults: A case-control study. Prim Care Diabetes. 2012;6:149–56. doi: 10.1016/j.pcd.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Coclami T, Cross M. Psychiatric co-morbidity with type 1 and type 2 diabetes mellitus. East Mediterr Health J. 2011;17:777–83. doi: 10.26719/2011.17.10.777. [DOI] [PubMed] [Google Scholar]
- 27.Jurisić-Erzen D, Benko K, Ljubić S, Jerković R. The prevalence of depression and anxiety in seafarers type 2 diabetic patients. Coll Antropol. 2011;35:1067–70. [PubMed] [Google Scholar]
- 28.Ruiz P, editor. Washington, DC: American Psychiatric Press; 2000. Ethnicity and Psychpharmacology. (Review of Psychiatry Series, Vol. 19, No. 4; Oldham JO, Riba MB, series editors) [Google Scholar]


