Abstract
Background
Cabergoline is typically effective for treating prolactinomas; however, some patients display cabergoline resistance, and the early characteristics of these patients remain unclear. We analyzed early indicators predicting long-term response to cabergoline.
Methods
We retrospectively reviewed the cases of 44 patients with macroprolactinomas who received cabergoline as first-line treatment; the patients were followed for a median of 16 months. The influence of various clinical parameters on outcomes was evaluated.
Results
Forty patients (90.9%) were treated medically and displayed tumor volume reduction (TVR) of 74.7%, a prolactin normalization (NP) rate of 81.8%, and a complete response (CR; TVR >50% with NP, without surgery) rate of 70.5%. Most patients (93.1%) with TVR ≥25% and NP at 3 months eventually achieved CR, whereas only 50% of patients with TVR ≥25% without NP and no patients with TVR <25% achieved CR. TVR at 3 months was strongly correlated with final TVR (R=0.785). Patients with large macroadenomas exhibited a low NP rate at 3 months, but eventually achieved TVR and NP rates similar to those of patients with smaller tumors. Surgery independently reduced the final dose of cabergoline (β=-1.181 mg/week), and two of four patients who underwent surgery were able to discontinue cabergoline.
Conclusion
Determining cabergoline response using TVR and NP 3 months after treatment is useful for predicting later outcomes. However, further cabergoline administration should be considered for patients with TVR >25% at 3 months without NP, particularly those with huge prolactinomas, because a delayed response may be achieved. As surgery can reduce the cabergoline dose necessary for successful disease control, it should be considered for cabergoline-resistant patients.
Keywords: Cabergoline, Dopamine, Prolactinoma, Hyperprolactinemia
INTRODUCTION
Prolactinomas are the most frequent functioning pituitary adenomas, comprising approximately 40% of pituitary tumors [1,2]. Their prevalence in the general adult population has been reported to range from 100 to 625 cases per million people [3,4]. Prolactinomas cause symptoms via two mechanisms, hormonal effects via hyperprolactinemia and mass effects via tumor expansion [1,5]. Hyperprolactinemia causes sexual and gonadal dysfunction, such as decreased libido, amenorrhea, erectile disorder, and infertility, as well as galactorrhea. Mass effects in patients with macroadenomas include bilateral hemianopsia, headache, hypopituitarism, and cranial neuropathy.
Dopamine agonists (DAs) are well-established first-line treatments for prolactinomas that can induce tumor shrinkage and normalization of prolactin (PRL) levels (NP) [1,5]. These agonists include bromocriptine, pergolide, cabergoline (CAB), and quinagolide, but only bromocriptine and CAB are currently available in Korea. Bromocriptine, which was introduced clinically in the 1980s, is a traditional drug for the treatment of prolactinomas [1,6]. However, CAB, which was introduced more recently, is used more commonly than bromocriptine. CAB is a selective agonist of the D2 receptor, which is related to the resolution of hyperprolactinemia, contrary to bromocriptine, which has partial affinity for the D1 receptor and affinity for the D2 receptor [6]. This agent has superior tolerability and convenience for patients, as well as higher rates of tumor shrinkage and control of hyperprolactinemia compared with bromocriptine [7,8]. It has also been shown to be effective in patients with bromocriptine-intolerant or bromocriptine-resistant prolactinomas [9,10].
However, a considerable proportion of patients display resistance to CAB. CAB treatment was reported to induce NP and successful tumor reduction in 61% to 92% and 55% to 100% of patients with prolactinomas, respectively [1]. Molitch [11] defined pharmacologic resistance in prolactinoma as a failure to achieve NP and/or to decrease tumor size by ≥50%, and described the rate of CAB resistance as 10% to 15% in terms of PRL levels and tumor size. The treatment of patients with CAB resistance remains challenging, although a few articles have suggested that surgical debulking or high-dose CAB therapy can be helpful for patients with resistance to DAs [12,13,14,15]. In addition, it is unclear how these patients can be identified early in the course of treatment.
A few years ago, we reported the long-term outcomes of patients with invasive prolactinomas who were treated with bromocriptine [16]. We documented that patients who achieved a tumor volume reduction (TVR) of at least 25% with NP at 3 months had a high probability of achieving a long-term complete response (CR), defined as a TVR of at least 50% with sustained NP. However, patients who were treated with CAB as a first-line therapy could not be included because CAB was a newly introduced and expensive drug in Korea at that time.
In this study, we describe the results of CAB administration as a first-line treatment for 44 patients with macroprolactinomas who were followed for a median of 16 months. To identify early predictors of long-term response to CAB, we analyzed the influence of initial clinical parameters and early response to CAB on later outcomes. We also evaluated which treatment factors could affect the patient outcomes.
METHODS
Patients
We conducted a 6-year retrospective study of patients with macroprolactinomas who were treated with CAB as a primary drug at Severance Hospital, Seoul, Korea between 2008 and 2013. Macroprolactinoma was defined as (1) a PRL level of at least 150 ng/mL and (2) a maximal diameter of at least 1 cm on baseline magnetic resonance imaging (MRI) scans of the sellar area. To evaluate the relationship between early and late parameters, the following additional inclusion criteria were applied: (1) a full dataset of pituitary hormone assays (including PRL) and sella MRI at baseline, (2) follow-up PRL assay and MRI after 3 months of CAB treatment, and (3) total follow-up duration of at least 12 months.
Treatment and response assessment
In all cases, oral CAB was started at a low dose (1 to 1.5 mg/wk), and the dosage was gradually increased to 1.5 to 4 mg/wk within 2 to 4 weeks. The increased dose was maintained for 3 months after treatment initiation to ensure a sufficient period of exposure to CAB. Evaluations of response occurred after 3 months, and the dose of CAB and interval of follow-up were continuously adjusted in consideration of response, tolerance, and other clinical indicators. For patients with good response and tolerance, reduction of CAB dose was carefully attempted with a relatively long interval of follow-up. For patients with poor response, a higher dose of CAB and a short interval of follow-up were employed. Because the follow-up intervals and treatment durations of the patients varied, three representative time points of response assessment were retrospectively defined as follows: early assessment, when the first sella MRI and PRL assay were performed after 3 months of CAB treatment; late assessment, when the first sella MRI and PRL assay were performed 12 to 24 months after treatment; and last assessment, when the last sella MRI and PRL assay were performed. Tumor volume was calculated according to Di Chiro and Nelson's formula: volume=height×length×width×π/6 [17]. The degree of response was assessed using TVR and NP. When evaluating the relationship between early response and later outcomes, we used group criteria according to the early response to CAB, as suggested in our previous article [16]: group 1, TVR ≥25% with NP; group 2, TVR ≥25% without NP; group 3, TVR <25% with NP; and group 4, TVR <25% without NP [16]. A successful response at the late or last assessment was defined as follows: volume response, TVR ≥50% without surgery; PRL response, NP without surgery; and CR, volume response with PRL response.
PRL assays
Serum PRL levels were measured via chemiluminescence immunoassay using commercial kits (Beckman Coulter, Brea, CA, USA). The within-run and total coefficients of variation for PRL concentrations were 3.66% and 3.77%, respectively. PRL levels <15 ng/mL for males and <25 ng/mL for females were regarded as normal. If serum PRL levels were normal or mildly elevated, PRL was measured again in diluted serum samples to exclude the hook effect, which can cause falsely low results [18,19].
Statistical analysis
Data were presented as the median (interquartile range) or the mean±SD. The relationship between early response and late or last response was analyzed using the Pearson correlation coefficient and multiple linear regression tests. The Student t test, Kruskal-Wallis test, Mann-Whitney U test, and Fisher exac t test were used to compare multiple groups. The relationship between tumor volume or PRL levels at baseline and TVR, PRL levels, or the maintained dose of CAB after treatment was analyzed using the Spearman correlation coefficient. Statistical analyses were performed using SPSS version 20 (IBM Co., Armonk, NY, USA). Values of P<0.05 were considered statistically significant.
RESULTS
Baseline characteristics and overall treatment outcomes
Of 66 patients with macroprolactinomas who were treated with CAB as a primary drug during the study period, 47 patients were followed for at least 1 year from the initial administration of CAB to the end of the data collection. One patient was lost to follow-up before 12 months, and two female patients who became pregnant less than 12 months into CAB treatment were also excluded because CAB had to be discontinued irrespective of tumor size and PRL level. Finally, in total, 44 patients, including 28 males (63.6%), were included in the study (Tables 1, 2). The mean age of the patients was 36.8 years, and the median follow-up duration was 16 months (interquartile range, 15 to 25.5). Eleven patients (25%) had visual field defects, and 28 patients (61.4%) complained of sexual dysfunction including impotence, oligomenorrhea/amenorrhea, and/or infertility. The patients also complained of headache and dizziness (n=12, 27.3%), ocular movement abnormalities (n=2, 4.5%), and galactorrhea (n=6, 13.6%). The median PRL level and median tumor volume were 796.7 ng/dL (range, 202.5 to 2,431.3) and 3.71 cm3 (range, 1.60 to 11.51), respectively. Tumor invasion of the cavernous sinus was noted in 20 patients (45.5%). Most patients (n=40, 90.9%) displayed sex hormone deficiency, defined as a testosterone level below the lower limit of the normal population for males, oligomenorrhea/amenorrhea in premenopausal females, and an inappropriately low gonadotropin level in postmenopausal females. Five patients (11.4%) displayed growth hormone (GH) deficiency, defined as a lower serum insulin-like growth factor 1 (IGF-1) level than the age- and sex-specific lower limit of the normal population, whereas secondary hypothyroidism and adrenal insufficiency were found in one patient and zero patients, respectively. Compared with female patients, male patients were older (41.5 years vs. 28.5 years, P<0.001), less likely to complain of sexual dysfunction (46.4% vs. 87.5%, P=0.010), and more likely to have a visual field defect (39.3% vs. 0%, P=0.003), and they displayed higher tumor volume (10.64 cm3 vs. 0.87 cm3, P<0.001) and PRL level (923.3 ng/mL vs.428.5 ng/mL, P=0.023).
Table 1.
Summary of 44 Patients with Macroprolactinomas

Values are expressed as mean±SD, number (%), or median (interquartile range).
GH, growth hormone.
aThe Student t test was used for parametric and nonparametric analyses, respectively; bThe Fisher exact test was used for categorical data analyses; cThe Mann-Whitney U test was used for parametric and nonparametric analyses, respectively; dPatients who underwent surgery before the final assessment were excluded.
Table 2.
Forty-Four Patients with Macroprolactinomas
Tx, treatment; TVR, tumor volume reduction; CAB, cabergoline; M, male; F, female.
aSurgery was performed before measuring other variables; bResidual tumor was not distinguished from postoperative changes on last magnetic resonance imaging.
At the last assessment, a volume response, PRL response, and CR were achieved by 35 (79.5%), 36 (81.8%), and 31 patients (70.5%), respectively (Table 1). Two patients who exhibited transient mild PRL elevation (patients no. 18 and 24, who had PRL levels of 52.3 and 33.6 ng/mL, respectively) showed very poor drug compliance at the last assessment, but were regarded as having achieved a PRL response. Four patients (9.1%) underwent surgery in their treatment courses, and the median TVR of the patients who did not undergo surgery was 74.7% (range, 61.7 to 85.4).
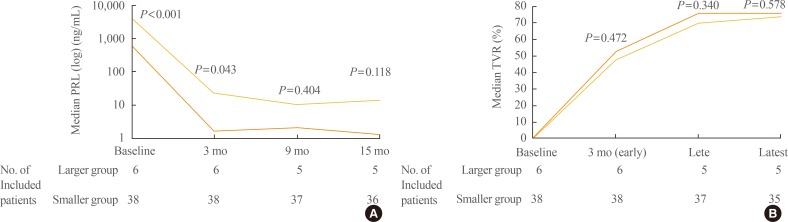
Influence of baseline tumor burden on outcomes
Neither the baseline tumor volume nor PRL level were directly correlated with TVR or PRL level at the early, late, and last assessments (Spearman correlation coefficients, all P>0.05). However, six patients with large tumors (larger group), whose baseline tumor volume exceeded 18 cm3 and whose PRL level exceeded 2,000 ng/mL, displayed higher PRL levels than patients with smaller tumors (smaller group) 3 months after treatment (22.9 ng/mL vs. 1.6 ng/mL, P=0.043) (Fig. 1A). Interestingly, these differences in PRL levels between groups lost their statistical significance at 9 months (Fig. 1A), and the TVR of patients who did and did not undergo surgery did not vary between the groups during the entire treatment course (Fig. 1B).
Fig. 1.
Changes in prolactin (PRL) levels and tumor volume reduction (TVR) in two groups according to baseline tumor volume. Black lines indicate patients with larger tumors (larger group); gray lines, patients with smaller tumors (smaller group). The cutoff between the two groups was a baseline tumor volume of 18 cm3. Each P value between the groups was calculated at each time point with the Mann-Whitney U test. At each time point, the patients who underwent surgery before the assessment were excluded. (A) Changes in median PRL levels. (B) Changes in median TVR.
Relationships between early response and late or last response
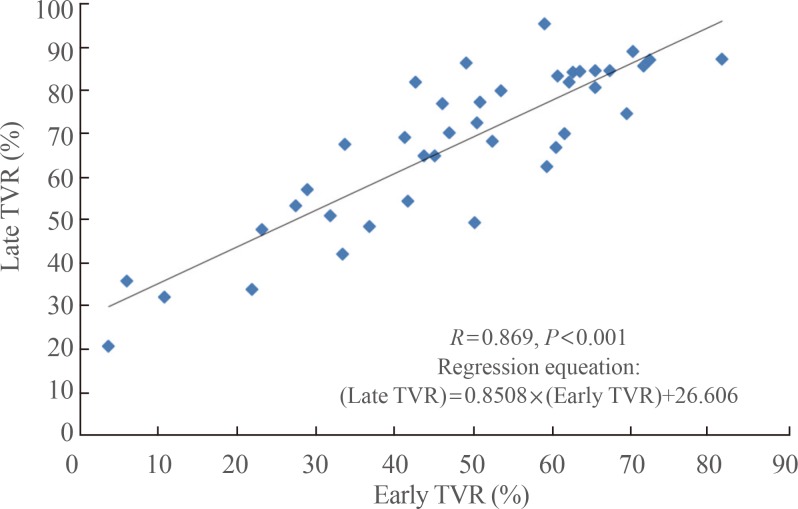
To assess the influence of early response on late or last response, we primarily categorized patients into four groups according to their early responses to CAB. Of the total 44 patients, 29 patients were included in group 1 (TVR ≥25% with NP), eight in group 2 (TVR ≥25% without NP), five in group 3 (TVR <25% with NP), and two in group 4 (TVR <25% without NP) (Fig. 2A). Most patients in group 1 (93.1%) achieved a CR as expected, but two patients (6.9%) did not achieve TVR ≥50% until the last assessment. Four of eight patients (50%) in group 2 eventually achieved a CR, whereas no patients in groups 3 and 4 achieved a CR. The proportion of CRs significantly differed between the groups (group 1 vs. 2 vs. 3 vs. 4; 93.1% vs. 50% vs. 0% vs. 0%; P<0.001). The last maintenance dose of CAB differed according to the last responses (CR vs. volume response without NP vs. PRL response without TVR ≥50% vs. surgery; 1.5 mg/wk (range, 1.0 to 2.0) vs. 4.5 mg/wk (range, 2.75 to 4.5) vs. 2.0 mg/wk (range, 1.0 to 2.0) vs. 0.5 mg/wk (range, 0.0 to 0.7); overall P=0.006), but no differences were observed between the four groups according to early responses (P=0.109).
Fig. 2.
Fate of 44 patients with macroprolactinomas according to early response. (A) Overall progress of patients according to categorization by early response. (B) Prolactin (PRL) levels of the patients in group 2. Black line indicates patients who eventually achieved normalization of prolactin level (NP; delayed response subgroup); gray line, patients who did not achieve NP (sustained resistance subgroup). TVR, tumor volume reduction. aP<0.05 between the subgroups, the P value was calculated with the Mann-Whitney U test.
We conducted further analysis of change in PRL levels to identify the distinguishing characteristics of the patients in group 2 that eventually achieved a CR (Fig. 2B). Of the four patients who achieved NP, three patients displayed normal PRL levels at 6 to 9 months (patients no. 32, 33, and 37). The remaining patient, who had a giant prolactinoma (patient no. 31; maximum tumor diameter 4.8 cm, tumor volume 20.4 cm3, and PRL level 8,759 ng/mL at baseline), maintained a slightly supranormal range PRL until 15 months (18.6 ng/mL at 9 months and 19.5 ng/mL at 15 months), but exhibited NP at 21 months. Median PRL levels did not differ between the patients who achieved NP (delayed response subgroup, n=4) and those who did not achieve NP (sustained resistance subgroup, n=4) until 3 months (1,947.4 ng/mL vs. 813.5 ng/mL, P=0.886 at baseline; 55.3 ng/mL vs. 115.3 ng/mL, P=0.686). However, a meaningful difference in median PRL levels between the two subgroups could also be observed after 9 months of CAB treatment (median PRL level: 13.0 ng/mL vs. 117.9 ng/mL, P=0.029). Median TVR did not vary between the subgroups (59.1% vs. 65.3%, P=0.486 at 3 months; 81.9% vs. 74.7%, P=0.200 at 15 months).
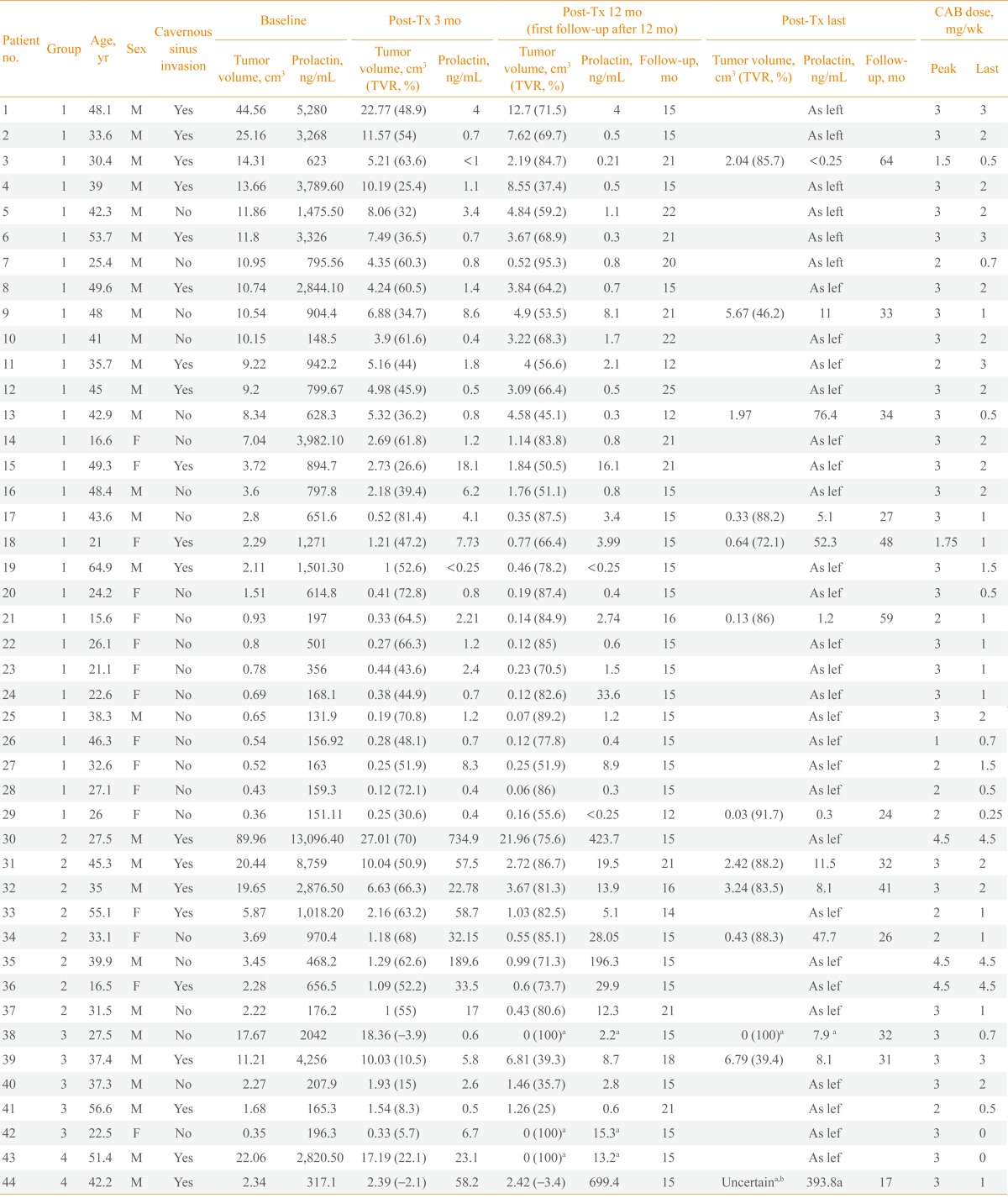
We also attempted to determine whether the absolute value of early TVR itself is predictive of response or whether only a certain cutoff such as 25% is meaningful. Pearson correlation analysis demonstrated that late TVR had a very strong correlation with early TVR (R=0.869, P<0.001) according to the following regression equation: late TVR=0.851×early TVR+26.606 (Fig. 3). Last TVR also displayed a correlation with early TVR, although the strength of the correlation was slightly lower (R=0.785, P<0.001). Multiple regression analysis was subsequently performed using sex, natural logarithm of the CAB maintenance duration between early and late assessment (Ln [weeks]), and cumulative dose of CAB between early and late assessments (mg) as independent variables. In this analysis, a greater TVR at the early assessment and a longer CAB maintenance duration were independent predictors for greater TVR at the late assessment (β=0.849, P<0.001; and β for Ln [weeks], 16.978, P=0.016, respectively), whereas sex and cumulative dose of CAB were not predictive (P=0.074 and P=0.613, respectively).
Fig. 3.
Correlation between late tumor volume reduction (TVR) and early TVR. The Pearson correlation analysis was used for statistical analysis.
Influence of surgery on the final maintenance dose of CAB
Because the patients who underwent surgery maintained the lowest dose of CAB (Fig. 2A), we sought to confirm whether surgery could independently reduce CAB dose. Thus, we performed multiple linear regression analysis with four independent variables as follows: undergoing surgery, baseline PRL level (mg/mL), 1/baseline volume (1/cm3), and natural logarithm of the treatment duration (Ln [months]). Baseline volume was transformed reciprocally to ensure the linearity of the model. Analysis confirmed that undergoing surgery (β=-1.181, P=0.013), a lower baseline PRL level (β=0.161, P=0.008), a smaller baseline volume (β for 1/baseline volume=-0.448, P=0.026), and a longer treatment duration (β for Ln [months]=-0.882, P=0.010) were independent predictors for a lower dose of CAB at the last assessment.
Summary of patients who underwent surgery
Four patients underwent transsphenoidal surgery (Table 3; patient nos. 38, 42, 43, and 44). The first patient (patient no. 38) underwent surgery after 3 months of CAB treatment because of acute hemorrhage in the tumor accompanied by severe headache. Immunohistochemical analysis for all pituitary hormones including PRL was negative, but the PRL result was regarded to be false-negative due to destruction of tumor cells following acute hemorrhage, as a nonfunctioning pituitary adenoma could not explain the patient's extremely high baseline PRL level (2,042 ng/mL). His headache resolved completely after surgery, although he developed panhypopituitarism. His CAB dose was reduced from 3 to 0.7 mg/wk, and his serum PRL levels were within the reference range. The second patient (patient no. 43) underwent surgery at 5 months because of a progressive visual field defect and diplopia. Immunohistochemical analysis of the excised tumor revealed PRL immunoreactivity. His symptoms were dramatically improved after surgery, although panhypopituitarism developed. The patient was able to discontinue CAB with sustained NP, and MRI revealed no residual tumor. The third patient (patient no. 42) underwent elective surgery after 12 months of CAB treatment owing to CAB resistance. Her early TVR was only 5.7%, and her preoperative PRL level was 168.6 ng/mL. Immunohistochemical analysis demonstrated PRL reactivity. She was able to discontinue CAB with sustained NP and no evidence of a residual tumor. The fourth patient (patient no. 44) also underwent elective surgery after 16 months of CAB treatment due to CAB resistance. His tumor size had increased by 2.1% despite 3 months of CAB treatment, and it continued to grow after 12 additional months of treatment without NP. Immunohistochemical staining revealed immunoreactivity for PRL. Postoperative MRI could not confirm whether there was residual tumor or only postoperative changes. PRL levels were not normalized despite surgery; however, CAB dose was markedly decreased (from 3 to 1 mg/wk) with a partial reduction in serum PRL level (from 699.4 to 393.8 ng/mL).
Table 3.
Summary of Patients Who Underwent Surgery
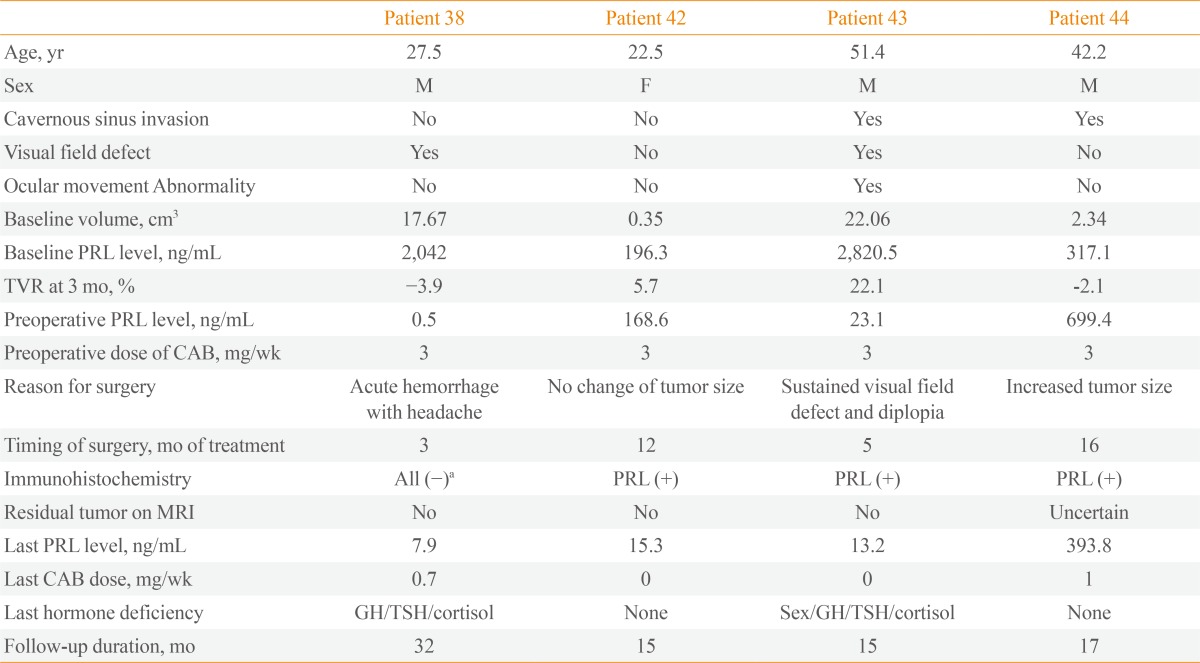
M, male; F, female; PRL, prolactin; TVR, tumor volume reduction; CAB, cabergoline; MRI, magnetic resonance imaging; GH, growth hormone; TSH, thyroid-stimulating hormone.
aThis was regarded as a false-negative result owing to acute hemorrhage.
Overall, none of the patients achieved TVR ≥25% at 3 months, including those with (patient no. 38 and 42) and those without (patient no. 43 and 44) NP. CAB dose was decreased after surgery, and two patients were able to discontinue CAB without evidence of residual tumor or PRL elevation.
Changes in the pituitary hormone levels and haracteristics of patients who did not exhibit testosterone level recovery
Among the patients who did not undergo surgery, CAB treatment improved baseline abnormalities of other pituitary hormones in most. All subnormal IGF-1 levels (patient no. 6, 8, 9, 13, and 24) and secondary hypothyroidism (patient no. 34) were gradually restored. All premenopausal women with oligomenorrhea/amenorrhea demonstrated improvement of symptoms following reduction of PRL levels, and the subnormal gonadotropin level of one postmenopausal woman was also improved. However, six male patients with NP and two male patients without NP displayed subnormal serum testosterone levels at the last assessment.
To elucidate the early characteristics of patients who could not achieve normalization of testosterone levels despite NP, we compared various clinical parameters of these patients (subnormal group, n=6) with those of male patients with normal testosterone levels and NP at the last assessment (normal group, n=16). Three patients who underwent surgery and one patient who received exogenous testosterone replacement before the first visit to our institution were excluded from this analysis to minimize confounding factors. The subnormal group had lower baseline IGF-1 (median 112.0 ng/mL vs. 212.1 ng/mL, P=0.013) and testosterone levels (median 57.9 ng/dL vs. 159.4 ng/dL, P=0.010) than the normal group. Patients in the subnormal group tended to be older (48.4 years vs. 39.8 years, P=0.052), and this group had a higher proportion of patients with age-specific subnormal IGF-1 levels (50% vs. 6.3%, P=0.046). Baseline tumor volume, PRL levels, proportion of patients with symptoms related to volume effects, and responses to CAB in terms of TVR and residual volume did not differ between the groups.
DISCUSSION
We described the clinical outcomes of 44 patients with macroprolactinomas who were treated with CAB, and this is the first report on CAB treatment in Korea with a relatively large sample size. Only one previous article on the efficacy of CAB in Korea has been published [20]. This study concluded that CAB could be used effectively even for invasive giant prolactinoma; however, its sample size was relatively small (n=10), and patients treated with other modalities such as transsphenoidal approach during their treatment courses were excluded. In our study, the CR rate (TVR ≥50% with NP) of CAB treatment at the last assessment was 70.5% (total 31/44; group 1, n=27; group 2, n=4). This rate was not superior to the CR rate of bromocriptine treatment (CR rate, 69.4%) that we reported previously, but this appears to have resulted from the shorter follow-up duration (15 months vs. 44 months) [16]. Previous reports of the treatment results of CAB varied widely according to different inclusion criteria, cutoff of "responsiveness," and treatment duration [1,19,21]. In a retrospective study of 455 patients with hyperprolactinemia, TVR ≥50% was noted in 31% of 190 evaluable patients and NP was achieved in 77% of 181 patients with macroprolactinomas after a median of 28 months of CAB treatment [22]. In another retrospective study of 56 de novo patients with macroprolactinoma, significant tumor reduction (defined as a ≥30% reduction of the maximal tumor diameter) was achieved in 89.1% of patients, and NP was achieved in 82.1% of patients [7]. In a prospective study of 26 drug-naive patients with macroprolactinomas, NP was achieved in 80.7% of patients after 6 months of treatment, the mean volume was reduced by 67.5% after 1 year, and the mean TVR was 92.1% after 3 years of CAB treatment [23]. Our outcomes regarding TVR and NP were in line with the findings of these previous reports.
In our study, we primarily focused on discovering early indicators that could reliably predict long-term response to CAB. Early identification of CAB-resistant patients is valuable considering the following facts. First, recent large studies of patients with CAB-resistant prolactinomas demonstrated that pharmacological resistance to CAB is associated with more aggressive disease, the potential risk of malignant evolution, and genetic predisposition to pituitary adenomas [15]. Second, there are concerns about the safety of long-term high-dose CAB treatment in patients with resistant prolactinomas. CAB was found to increase the frequency of valvular heart disease in a dose-dependent manner in studies of patients with Parkinson disease [24,25,26,27]. Although many studies indicated that a lower dose of CAB used in treatment for hyperprolactinemia or prolactinoma was not related to valvular dysfunction [28], some studies reported an increased risk of tricuspid valve dysfunction in patients with prolactinomas who were treated with long-term, high-dose CAB regimens [29,30]. Finally, long-term treatment with DAs may cause peritumoral fibrosis, which makes removal of the entire tumor difficult, although it is unclear whether this phenomenon also occurs as a result of CAB treatment [31,32].
In our study, we determined that grouping patients after 3 months of CAB treatment using TVR ≥25% and NP criteria was a potentially reliable approach. Groups with TVR ≥25% with NP, TVR ≥25% without NP, and TVR <25% at 3 months after CAB treatment could be regarded as having early responsiveness, early partial resistance, and early resistance respectively, considering the different long-term CR rates of 93.1%, 50%, and 0%, respectively. We reconfirmed that TVR=25% at 3 months might be a reliable cutoff because TVR at 3 months was very strongly correlated (R>0.8) with TVR at 15 months, and the estimated regression equation revealed that a cutoff resistance of TVR=50% at 15 months [11] corresponded to TVR=25% at 3 months. These results are in line with our previous reports demonstrating that TVR ≥25% and NP after 3 months of bromocriptine treatment are useful predictors of responsiveness to DAs [16].
In addition, patients with early partial resistance should be reassessed after several months to confirm whether they achieved a delayed response. Among patients with TVR ≥25% without NP at 3 months, the PRL levels of patients who achieved a CR were lower than those of patients who did not achieve a CR after 9 months. This is similar to the results observed for bromocriptine treatment, in which three of five patients with TVR ≥25% without NP at 3 months achieved NP at 5 to 9 months [16]. Moreover, patients with giant prolactinomas might require a longer treatment duration to achieve NP than patients with smaller tumors even if the giant tumors exhibit sufficient responsiveness to CAB. The patients with the largest tumors and very high PRL levels displayed higher PRL levels at 3 months than other patients, but, after 9 months of treatment, they achieved similar TVR rates and PRL levels as patients with smaller tumors. Similarly, in a study of 10 male patients with invasive giant prolactinomas (tumor diameter >4 cm with PRL levels >1,000 ng/mL), none achieved PRL levels <15 ng/mL at 3 months, although six patients (60%) exhibited PRL levels <15 ng/mL at the final assessment with continuous CAB treatment [20].
The most effective treatment modality for patients with resistance to standard-dose CAB remains unclear. In this situation, high doses of CAB, transsphenoidal surgery, and occasionally radiotherapy can be applied, and temozolomide therapy can be used for patients with malignant prolactinomas [8,19,21]. Recently, Vroonen et al. [15] reviewed the outcomes of 92 patients with resistance to CAB, defined as a failure to achieve NP on a CAB dose of 2.0 mg/wk. Of the 17 patients treated with high-dose CAB regimens (≥3.5 mg/wk) without surgery, only five patients (26.3%) achieved NP. Surgery demonstrated significant usefulness for controlling PRL levels and reducing CAB dose, whereas radiotherapy did not have a significant benefit. Based on these results, the authors suggested that surgery could improve the outcomes of patients with CAB resistance [15].
In our study, surgery demonstrated its usefulness for disease control and reducing CAB dose. Three of the four patients who underwent surgical interventions achieved complete tumor resolution on MRI with NP even though they had TVR <25% and/or no NP at 3 months. Two patients were able to discontinue CAB early, and multiple regression analysis of all the 44 patients also revealed that surgery could reduce CAB dose independently. Conversely, a higher cumulative dose of CAB did not alter TVR upon correction for treatment duration. CAB inhibits PRL production in a dose-dependent manner [1], and resistance to DAs is occasionally overcome by high-dose CAB treatment [13,14]. Therefore, guidelines suggest escalating the CAB dose in patients with resistance [8,19]. This difference between our results and the results of previous reports may be due to the relatively narrow range of our CAB dose. A CAB dose exceeding 3 mg/wk is rarely necessary for prolactinomas [1,8,19], but doses as high as 11 mg/wk may be required to overcome pharmacological resistance [13,14]. In our study, the median peak CAB dose was 3 mg/wk with an interquartile range of only 1 mg, and this dose may be insufficient to reverse the resistance of some patients. However, it should be noted that a markedly increased CAB dose might be associated with cardiac valve disease, as discussed previously.
Another interesting finding was that baseline IGF-1 level was associated with final restoration of sex hormones. Unlike other pituitary hormones, suppression of sex hormones can be a result of hyperprolactinemia-induced hypogonadism and compression of the gonadotropic cells by tumors [21]. However, CAB treatment results in rapid normalization or marked reduction of PRL levels in most patients, and, thus, persistent subnormal sex hormone levels would primarily result from volume effects rather than hyperprolactinemia. In our study, six of the eight nonsurgically-treated male patients with hypogonadism at the last assessment displayed NP; thus, these patients were regarded as having hypogonadism induced by compression. In terms of pituitary hormone deficits induced by tumors, GH deficiency is the second most common deficit after hypogonadism [33,34,35,36]. In our study, six patients with persistent hypogonadism despite NP had lower IGF-1 levels at diagnosis than other male patients, whereas their baseline tumor volume or residual volume after treatment was not larger. These findings suggest that a low IGF-1 level at diagnosis might be a useful indicator for predicting persistent hypogonadism induced by volume effects, which might not be directly proportional to tumor size itself.
This study has some limitations. First, this study is a retrospective, single-center study, and fully standardized protocols were not available for adjusting CAB dose or follow-up interval. For collection of further precise data, a prospective study with a preset protocol is warranted. Second, the prevalence of adrenal insufficiency could have been underestimated, because stimulation tests were not routinely performed. However, the basal pituitary hormone test is used as an important screening test in clinical fields, and gonadal function and thyroid function can be interpreted from the basal hormone test and symptoms/signs. Thus, the descriptive data of the basal hormone test may be a useful indicator. Third, 16 months of follow-up might be relatively short to represent long-term response. Further cumulative data collection on CAB treatment would provide us with additional information.
In conclusion, CAB treatment was very effective in two-thirds of patients with macroprolactinomas. Assessing response using TVR and NP after 3 months of treatment is a useful approach for predicting long-term response and resistance to CAB. When patients achieve TVR ≥25% without NP at 3 months, the assessment of resistance should be delayed for several months to rule out a delayed response, especially in patients with large tumors. Surgical treatment can help reduce CAB dose and contribute to successful disease control, and should be considered in CAB-resistant patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gillam MP, Molitch ME, Lombardi G, Colao A. Advances in the treatment of prolactinomas. Endocr Rev. 2006;27:485–534. doi: 10.1210/er.2005-9998. [DOI] [PubMed] [Google Scholar]
- 2.Colao A. Pituitary tumours: the prolactinoma. Best Pract Res Clin Endocrinol Metab. 2009;23:575–596. doi: 10.1016/j.beem.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Colao A, Lombardi G. Growth-hormone and prolactin excess. Lancet. 1998;352:1455–1461. doi: 10.1016/S0140-6736(98)03356-X. [DOI] [PubMed] [Google Scholar]
- 4.Daly AF, Rixhon M, Adam C, Dempegioti A, Tichomirowa MA, Beckers A. High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J Clin Endocrinol Metab. 2006;91:4769–4775. doi: 10.1210/jc.2006-1668. [DOI] [PubMed] [Google Scholar]
- 5.Oh MC, Kunwar S, Blevins L, Aghi MK. Medical versus surgical management of prolactinomas. Neurosurg Clin N Am. 2012;23:669–678. doi: 10.1016/j.nec.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Colao A, Savastano S. Medical treatment of prolactinomas. Nat Rev Endocrinol. 2011;7:267–278. doi: 10.1038/nrendo.2011.37. [DOI] [PubMed] [Google Scholar]
- 7.Di Sarno A, Landi ML, Cappabianca P, Di Salle F, Rossi FW, Pivonello R, Di Somma C, Faggiano A, Lombardi G, Colao A. Resistance to cabergoline as compared with bromocriptine in hyperprolactinemia: prevalence, clinical definition, and therapeutic strategy. J Clin Endocrinol Metab. 2001;86:5256–5261. doi: 10.1210/jcem.86.11.8054. [DOI] [PubMed] [Google Scholar]
- 8.Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, Brue T, Cappabianca P, Colao A, Fahlbusch R, Fideleff H, Hadani M, Kelly P, Kleinberg D, Laws E, Marek J, Scanlon M, Sobrinho LG, Wass JA, Giustina A. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf) 2006;65:265–273. doi: 10.1111/j.1365-2265.2006.02562.x. [DOI] [PubMed] [Google Scholar]
- 9.Delgrange E, Maiter D, Donckier J. Effects of the dopamine agonist cabergoline in patients with prolactinoma intolerant or resistant to bromocriptine. Eur J Endocrinol. 1996;134:454–456. doi: 10.1530/eje.0.1340454. [DOI] [PubMed] [Google Scholar]
- 10.Colao A, Di Sarno A, Sarnacchiaro F, Ferone D, Di Renzo G, Merola B, Annunziato L, Lombardi G. Prolactinomas resistant to standard dopamine agonists respond to chronic cabergoline treatment. J Clin Endocrinol Metab. 1997;82:876–883. doi: 10.1210/jcem.82.3.3822. [DOI] [PubMed] [Google Scholar]
- 11.Molitch ME. Pharmacologic resistance in prolactinoma patients. Pituitary. 2005;8:43–52. doi: 10.1007/s11102-005-5085-2. [DOI] [PubMed] [Google Scholar]
- 12.Primeau V, Raftopoulos C, Maiter D. Outcomes of transsphenoidal surgery in prolactinomas: improvement of hormonal control in dopamine agonist-resistant patients. Eur J Endocrinol. 2012;166:779–786. doi: 10.1530/EJE-11-1000. [DOI] [PubMed] [Google Scholar]
- 13.Ono M, Miki N, Kawamata T, Makino R, Amano K, Seki T, Kubo O, Hori T, Takano K. Prospective study of high-dose cabergoline treatment of prolactinomas in 150 patients. J Clin Endocrinol Metab. 2008;93:4721–4727. doi: 10.1210/jc.2007-2758. [DOI] [PubMed] [Google Scholar]
- 14.Ono M, Miki N, Amano K, Kawamata T, Seki T, Makino R, Takano K, Izumi S, Okada Y, Hori T. Individualized high-dose cabergoline therapy for hyperprolactinemic infertility in women with micro- and macroprolactinomas. J Clin Endocrinol Metab. 2010;95:2672–2679. doi: 10.1210/jc.2009-2605. [DOI] [PubMed] [Google Scholar]
- 15.Vroonen L, Jaffrain-Rea ML, Petrossians P, Tamagno G, Chanson P, Vilar L, Borson-Chazot F, Naves LA, Brue T, Gatta B, Delemer B, Ciccarelli E, Beck-Peccoz P, Caron P, Daly AF, Beckers A. Prolactinomas resistant to standard doses of cabergoline: a multicenter study of 92 patients. Eur J Endocrinol. 2012;167:651–662. doi: 10.1530/EJE-12-0236. [DOI] [PubMed] [Google Scholar]
- 16.Yang MS, Hong JW, Lee SK, Lee EJ, Kim SH. Clinical management and outcome of 36 invasive prolactinomas treated with dopamine agonist. J Neurooncol. 2011;104:195–204. doi: 10.1007/s11060-010-0459-3. [DOI] [PubMed] [Google Scholar]
- 17.Di Chiro G, Nelson KB. The volume of the sella turcica. Am J Roentgenol Radium Ther Nucl Med. 1962;87:989–1008. [PubMed] [Google Scholar]
- 18.Frieze TW, Mong DP, Koops MK. "Hook effect" in prolactinomas: case report and review of literature. Endocr Pract. 2002;8:296–303. doi: 10.4158/EP.8.4.296. [DOI] [PubMed] [Google Scholar]
- 19.Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, Wass JA Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:273–288. doi: 10.1210/jc.2010-1692. [DOI] [PubMed] [Google Scholar]
- 20.Cho EH, Lee SA, Chung JY, Koh EH, Cho YH, Kim JH, Kim CJ, Kim MS. Efficacy and safety of cabergoline as first line treatment for invasive giant prolactinoma. J Korean Med Sci. 2009;24:874–878. doi: 10.3346/jkms.2009.24.5.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iglesias P, Diez JJ. Macroprolactinoma: a diagnostic and therapeutic update. QJM. 2013;106:495–504. doi: 10.1093/qjmed/hcs240. [DOI] [PubMed] [Google Scholar]
- 22.Verhelst J, Abs R, Maiter D, van den Bruel A, Vandeweghe M, Velkeniers B, Mockel J, Lamberigts G, Petrossians P, Coremans P, Mahler C, Stevenaert A, Verlooy J, Raftopoulos C, Beckers A. Cabergoline in the treatment of hyperprolactinemia: a study in 455 patients. J Clin Endocrinol Metab. 1999;84:2518–2522. doi: 10.1210/jcem.84.7.5810. [DOI] [PubMed] [Google Scholar]
- 23.Colao A, Di Sarno A, Landi ML, Scavuzzo F, Cappabianca P, Pivonello R, Volpe R, Di Salle F, Cirillo S, Annunziato L, Lombardi G. Macroprolactinoma shrinkage during cabergoline treatment is greater in naive patients than in patients pretreated with other dopamine agonists: a prospective study in 110 patients. J Clin Endocrinol Metab. 2000;85:2247–2252. doi: 10.1210/jcem.85.6.6657. [DOI] [PubMed] [Google Scholar]
- 24.Schade R, Andersohn F, Suissa S, Haverkamp W, Garbe E. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med. 2007;356:29–38. doi: 10.1056/NEJMoa062222. [DOI] [PubMed] [Google Scholar]
- 25.Zanettini R, Antonini A, Gatto G, Gentile R, Tesei S, Pezzoli G. Valvular heart disease and the use of dopamine agonists for Parkinson's disease. N Engl J Med. 2007;356:39–46. doi: 10.1056/NEJMoa054830. [DOI] [PubMed] [Google Scholar]
- 26.Corvol JC, Anzouan-Kacou JB, Fauveau E, Bonnet AM, Lebrun-Vignes B, Girault C, Agid Y, Lechat P, Isnard R, Lacomblez L. Heart valve regurgitation, pergolide use, and parkinson disease: an observational study and meta-analysis. Arch Neurol. 2007;64:1721–1726. doi: 10.1001/archneur.64.12.1721. [DOI] [PubMed] [Google Scholar]
- 27.Antonini A, Poewe W. Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson's disease. Lancet Neurol. 2007;6:826–829. doi: 10.1016/S1474-4422(07)70218-1. [DOI] [PubMed] [Google Scholar]
- 28.Valassi E, Klibanski A, Biller BM. Clinical review: potential cardiac valve effects of dopamine agonists in hyperprolactinemia. J Clin Endocrinol Metab. 2010;95:1025–1033. doi: 10.1210/jc.2009-2095. [DOI] [PubMed] [Google Scholar]
- 29.Colao A, Galderisi M, Di Sarno A, Pardo M, Gaccione M, D'Andrea M, Guerra E, Pivonello R, Lerro G, Lombardi G. Increased prevalence of tricuspid regurgitation in patients with prolactinomas chronically treated with cabergoline. J Clin Endocrinol Metab. 2008;93:3777–3784. doi: 10.1210/jc.2007-1403. [DOI] [PubMed] [Google Scholar]
- 30.Wakil A, Rigby AS, Clark AL, Kallvikbacka-Bennett A, Atkin SL. Low dose cabergoline for hyperprolactinaemia is not associated with clinically significant valvular heart disease. Eur J Endocrinol. 2008;159:R11–R14. doi: 10.1530/EJE-08-0365. [DOI] [PubMed] [Google Scholar]
- 31.Saeki N, Nakamura M, Sunami K, Yamaura A. Surgical indication after bromocriptine therapy on giant prolactinomas: effects and limitations of the medical treatment. Endocr J. 1998;45:529–537. doi: 10.1507/endocrj.45.529. [DOI] [PubMed] [Google Scholar]
- 32.Menucci M, Quinones-Hinojosa A, Burger P, Salvatori R. Effect of dopaminergic drug treatment on surgical findings in prolactinomas. Pituitary. 2011;14:68–74. doi: 10.1007/s11102-010-0261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Regal M, Paramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol (Oxf) 2001;55:735–740. doi: 10.1046/j.1365-2265.2001.01406.x. [DOI] [PubMed] [Google Scholar]
- 34.Dekkers OM, Hammer S, de Keizer RJ, Roelfsema F, Schutte PJ, Smit JW, Romijn JA, Pereira AM. The natural course of non-functioning pituitary macroadenomas. Eur J Endocrinol. 2007;156:217–224. doi: 10.1530/eje.1.02334. [DOI] [PubMed] [Google Scholar]
- 35.Karavitaki N, Collison K, Halliday J, Byrne JV, Price P, Cudlip S, Wass JA. What is the natural history of nonoperated nonfunctioning pituitary adenomas? Clin Endocrinol (Oxf) 2007;67:938–943. doi: 10.1111/j.1365-2265.2007.02990.x. [DOI] [PubMed] [Google Scholar]
- 36.Iglesias P, Bernal C, Villabona C, Castro JC, Arrieta F, Diez JJ. Prolactinomas in men: a multicentre and retrospective analysis of treatment outcome. Clin Endocrinol (Oxf) 2012;77:281–287. doi: 10.1111/j.1365-2265.2012.04351.x. [DOI] [PubMed] [Google Scholar]