Introduction
The Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 (Public Law 97-248) provided new incentives for health maintenance organizations (HMO's) to enroll Medicare beneficiaries on an at-risk basis.1 TEFRA provisions encouraging HMO participation in Medicare on an at-risk basis sought to further the goals of promoting competition and cost effectiveness, and providing greater beneficiary choice in health care and greater autonomy to providers.
The TEFRA provisions represented a major change from the way HMO's were paid under the 1972 Amendments to the Social Security Act (Public Law 92-603). Under TEFRA, HMO's are paid a prospectively determined amount for risk enrollees. They receive 95 percent of the adjusted average per capita cost (AAPCC), which is defined as the actuarially estimated per capita amount that would be payable if Medicare services for HMO members were furnished in the local fee-for-service market. HMO's must use any difference between 95 percent of the AAPCC and their adjusted community rate (ACR) to provide additional benefits or to lower premiums. The ACR is defined as the premium the HMO would have charged Medicare enrollees for the Medicare benefit package. TEFRA also provides for cost contracts with HMO's in which case HMO's are paid for reasonable costs up to 100 percent of the AAPCC.
Under the 1972 Amendments to the Social Security Act, payments under both cost and risk contracts were subject to retrospective adjustments. This is contrary to the way HMO's are paid in the private sector where they receive a fixed premium and can appropriately budget and plan. Only four plans signed risk contracts under the provisions of the 1972 amendments.
This article describes the trends in TEFRA HMO enrollment. It compares patterns of Medicare and total HMO enrollment by State, by HMO, by type of HMO, and by profit status. Data on extra benefits offered beyond those covered by Medicare are also presented.
There are four classes of Medicare HMO enrollees. These are:
Risk enrollees under the TEFRA provisions.
Cost enrollees under the TEFRA provisions.
Risk enrollees under the 1972 Amendments to the Social Security Act.
Enrollees in HMO demonstration projects.
Trends
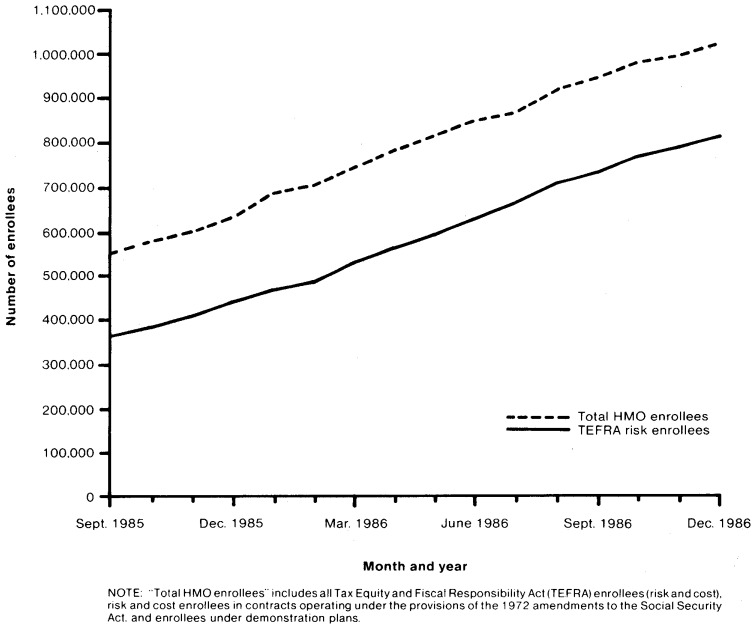
In September 1985, there were 552,096 total Medicare HMO enrollees (Figure 1). Growth continued each month and by December 1986 there were 1,025,466 enrollees, representing a 4.2 percent compound rate of growth per month. As shown in Figure 1, TEFRA provisions encouraged growth in Medicare HMO enrollment. Regulations to implement the TEFRA HMO provisions were issued in January 1985, and the first contract under these provisions was signed in April 1985. By September 1985, there were 395,374 TEFRA HMO enrollees, of which 92.2 percent were enrolled under TEFRA risk contracts and 7.8 percent under TEFRA cost. Total TEFRA enrollees reached 916,995 by December 1986.
Figure 1. Medicare health maintenance organization (HMO): September 1985-December 1986.
This growth in TEFRA enrollees averaged 5.8 percent monthly while enrollment in old risk plans showed a much slower rate of growth, less than 1 percent per month. Enrollment in demonstration projects more than doubled, rising from 12,387 in September 1985 to 30,404 in December 1986.
Enrollment by State
Data by State on HMO enrollment in the total population (maintained by InterStudy) are compared with data on HMO enrollment of Medicare beneficiaries (Table 1). In 1986, 23.7 million persons2 or nearly 10 percent of the total U.S. population was enrolled in an HMO. Five States accounted for nearly one-half of those enrollees: California, 6.5 million or 27.3 percent; New York, 1.7 million or 7.1 percent; Michigan, 1.2 million or 5.0 percent; Minnesota, 1.0 million or 4.4 percent; and Illinois, 1.1 million or 4.8 percent. HMO enrollment in both California and Minnesota represented nearly one-fourth of those States' total populations. Other States that had a high percent enrolled in HMO's were Wisconsin (19.4 percent), Hawaii (18.4 percent), and Massachusetts (16.6 percent).
Table 1. Population, total health maintenance organization (HMO) enrollees, Medicare enrollees, and HMO Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk Medicare enrollees, by State.
| State | National | Medicare | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Population in thousands July 1986 | HMO enrollees in thousands June 1986 | HMO enrollees as percent of population | Medicare enrollees in thousands January 1986 | HMO TEFRA risk enrollees December 1986 | TEFRA risk enrollees as percent of Medicare enrollees | TEFRA risk contracts December 1986 | |
| United States | 241,077 | 23,664 | 9.8 | 29,421 | 813,712 | 2.8 | 149 |
| Alabama | 4,053 | 70 | 1.7 | 510 | 0 | 0.0 | 0 |
| Alaska | 534 | 0 | 0.0 | 17 | 0 | 0.0 | 0 |
| Arizona | 3,317 | 444 | 13.4 | 398 | 11,420 | 2.9 | 1 |
| Arkansas | 2,372 | 16 | 0.7 | 354 | 0 | 0.0 | 0 |
| California | 26,981 | 6,465 | 24.0 | 2,805 | 164,296 | 5.9 | 14 |
| Colorado | 3,267 | 413 | 12.6 | 294 | 11,396 | 3.9 | 5 |
| Connecticut | 3,189 | 316 | 9.9 | 424 | 2,422 | 0.6 | 1 |
| Delaware | 633 | 54 | 8.5 | 75 | 0 | 0.0 | 0 |
| District of Columbia | 626 | 308 | 49.2 | 68 | 0 | 0.0 | 0 |
| Florida | 11,675 | 859 | 7.4 | 1,949 | 175,192 | 9.0 | 11 |
| Georgia | 6,104 | 247 | 4.0 | 629 | 0 | 0.0 | 1 |
| Hawaii | 1,062 | 195 | 18.4 | 97 | 17,653 | 18.2 | 3 |
| Idaho | 1,003 | 0 | 0.0 | 115 | 0 | 0.0 | 0 |
| Illinois | 11,553 | 1,124 | 9.7 | 1,392 | 53,525 | 3.8 | 7 |
| Indiana | 5,504 | 308 | 5.6 | 683 | 9,906 | 1.5 | 2 |
| Iowa | 2,851 | 163 | 5.7 | 428 | 2,600 | 0.6 | 1 |
| Kansas | 2,461 | 152 | 6.2 | 335 | 13,371 | 4.0 | 12 |
| Kentucky | 3,728 | 110 | 3.0 | 474 | 0 | 0.0 | 0 |
| Louisiana | 4,501 | 113 | 2.5 | 452 | 0 | 0.0 | 0 |
| Maine | 1,174 | 2 | 0.2 | 166 | 0 | 0.0 | 0 |
| Maryland | 4,463 | 361 | 8.1 | 458 | 2,681 | 0.6 | 3 |
| Massachusetts | 5,832 | 966 | 16.6 | 789 | 51,509 | 6.5 | 15 |
| Michigan | 9,145 | 1,187 | 13.0 | 1,105 | 38,550 | 3.5 | 12 |
| Minnesota | 4,214 | 1,047 | 24.8 | 537 | 137,390 | 25.6 | 11 |
| Mississippi | 2,625 | 0 | 0.0 | 326 | 0 | 0.0 | 0 |
| Missouri | 5,066 | 394 | 7.8 | 715 | 139 | 0.0 | 1 |
| Montana | 819 | 0 | 0.0 | 103 | 0 | 0.0 | 0 |
| Nebraska | 1,598 | 47 | 2.9 | 222 | 3,244 | 1.5 | 1 |
| Nevada | 963 | 96 | 10.0 | 98 | 14,970 | 15.3 | 3 |
| New Hampshire | 1,027 | 92 | 9.0 | 122 | 0 | 0.0 | 0 |
| New Jersey | 7,620 | 580 | 7.6 | 996 | 14,246 | 1.4 | 5 |
| New Mexico | 1,479 | 125 | 8.5 | 144 | 12,605 | 8.8 | 4 |
| New York | 17,772 | 1,686 | 9.5 | 2,314 | 16,681 | 0.7 | 7 |
| North Carolina | 6,331 | 265 | 4.2 | 754 | 337 | 0.0 | 1 |
| North Dakota | 679 | 28 | 4.1 | 90 | 0 | 0.0 | 0 |
| Ohio | 10,752 | 988 | 9.2 | 1,365 | 3,312 | 0.2 | 5 |
| Oklahoma | 3,305 | 124 | 3.8 | 403 | 4,285 | 1.1 | 3 |
| Oregon | 2,698 | 428 | 15.9 | 365 | 21,221 | 5.8 | 2 |
| Pennsylvania | 11,889 | 752 | 6.3 | 1,769 | 21,296 | 1.2 | 4 |
| Rhode Island | 975 | 154 | 15.8 | 144 | 2,506 | 1.7 | 1 |
| South Carolina | 3,378 | 190 | 5.6 | 366 | 938 | 0.3 | 1 |
| South Dakota | 708 | 1 | 0.1 | 101 | 0 | 0.0 | 0 |
| Tennessee | 4,803 | 148 | 3.1 | 608 | 2,361 | 0.4 | 1 |
| Texas | 16,685 | 789 | 4.7 | 1,544 | 1,900 | 0.1 | 6 |
| Utah | 1,665 | 215 | 12.9 | 131 | 1 | 0.0 | 2 |
| Vermont | 541 | 0 | 0.0 | 68 | 0 | 0.0 | 0 |
| Virginia | 5,787 | 214 | 3.7 | 609 | 0 | 0.0 | 0 |
| Washington | 4,463 | 408 | 9.1 | 521 | 0 | 0.0 | 0 |
| West Virginia | 1,919 | 41 | 2.1 | 279 | 0 | 0.0 | 0 |
| Wisconsin | 4,785 | 927 | 19.4 | 652 | 1,759 | 0.3 | 3 |
| Wyoming | 507 | 1 | 0.2 | 44 | 0 | 0.0 | 0 |
InterStudy: 1986 June Update. A mid-year report on HMO growth.
Health Care Financing Administration, Bureau of Data Management and Strategy: Aged and disabled with Part A and Part B, Data from the Medicare Statistical System.
Health Care Financing Administration: Data from the Office of Prepaid Health Care.
NOTES: In both the data on total HMO enrollment from InterStudy and the Medicare data, HMO enrollment is assigned to States according to location of plan. Thus, the high percent of HMO enrollment in the District of Columbia represents an artifact of the data. Several HMO's having main offices in the District of Columbia have members living in the neighboring States of Maryland and Virginia.
Of the 29 million aged and disabled Medicare enrollees, 3.5 percent are enrolled in HMO's, with most, 2.8 percent, under TEFRA risk contracts. (The number of contracts is larger than the number of plans because a plan may have several contracts, for example, one for each service area within a State. Plans are used synonymously with contracts in this article.) Concentrations (50,000 or more) of TEFRA risk enrollees were heavy in five States: Florida, 175,192 or 9.0 percent of its Medicare population enrolled under TEFRA risk contracts; California, 164,296 or 5.9 percent of its Medicare population; Minnesota, 137,390 or 25.6 percent; Massachusetts, 51,509 or 6.5 percent; and Illinois, 53,525 or 3.8 percent of its Medicare population. These States accounted for 71.5 percent of the TEFRA risk enrollees in December 1986.
The five States with the highest percents of Medicare enrollees covered by TEFRA risk plans were Minnesota (25.6), Hawaii (18.2), Nevada (15.3), Florida (9.0), and New Mexico (8.8). Minnesota and Hawaii, as noted earlier, also had high HMO penetration in the total population. Medicare TEFRA risk enrollment in California (5.9 percent of the Medicare population) had not yet reached the level of HMO penetration in that State (24.0 percent). In four States (Florida, Minnesota, New Mexico, and Nevada) the HMO penetration in the Medicare population was greater than the HMO penetration in the general population.
Largest plans
Of the 813,712 TEFRA risk HMO enrollees in December 1986, 72.6 percent were covered by the 30 plans with the most Medicare enrollees that comprised the top quintile (i.e., the top 20th percentile) of the 149 plans (Table 2). The second quintile covered another 16.7 percent of enrollees, and the third quintile covered 7.3 percent, leaving the remaining 3.4 percent of enrollees distributed among 59 plans that had small numbers of Medicare enrollees.
Table 2. Percent of Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk Medicare enrollment, by quintile of health maintenance organization (HMO) plans: December 1986.
| Quintile of HMO plans | Cumulative plans | Percent | Cumulative percent |
|---|---|---|---|
| 1st | 30 | 72.6 | 72.6 |
| 2nd | 60 | 16.7 | 89.3 |
| 3rd | 90 | 7.3 | 96.6 |
| 4th | 120 | 3.1 | 99.7 |
| 5th | 149 | 0.3 | 100.0 |
NOTE: The total number of plans was 149 with 813,712 enrollees.
SOURCE: Health Care Financing Administration, Office of Prepaid Health Care.
In June 1986, there was a national total of 595 HMO's that had 23.7 million enrollees. As shown in Table 3, the 20 largest HMO's accounted for 9.3 million enrollees or 39.2 percent of total HMO enrollment. Five of these HMO's were in California and accounted for 5.0 million enrollees. As of December 1986, only 11 of the largest 20 HMO's had enrolled some Medicare persons under a TEFRA risk contract. Medicare enrollment in one HMO, International Medical Centers of Miami, represented 74.8 percent of its total enrollment.
Table 3. Number of enrollees and percent distribution in the 20 largest health maintenance organizations (HMO's) and the percent of Medicare Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk enrollees and rank: June 1986.
| Name of HMO | Total number of HMO enrollees June 19861 | Percent distribution | Percent Medicare TEFRA risk enrollees June 1986 | Rank among Medicare TEFRA risk December 19862 | |
|---|---|---|---|---|---|
| Total | 323,663,626 | 100.0 | 2.7 | — | |
| Top 20 | 9,263,310 | 39.2 | (4) | — | |
| 1. | Kaiser Foundation Health Plan—Oakland | 1,997,207 | 8.4 | (4) | (4) |
| 2. | Kaiser Foundation Health Plan—Pasadena | 1,841,806 | 7.8 | (4) | (4) |
| 3. | Health Insurance Plan—Greater New York | 902,934 | 3.8 | (4) | (4) |
| 4. | Health Net—Van Nuys, California | 443,860 | 1.9 | (4) | (4) |
| 5. | HMO of Pennsylvania—Blue Bell | 412,012 | 1.7 | 3.2 | 8 |
| 6. | CIGNA Healthplans of California—Glendale | 395,386 | 1.7 | (4) | (4) |
| 7. | Physicians Health Plan of Minnesota | 330,758 | 1.4 | 9.3 | 4 |
| 8. | Group Health Corporation of Puget Sound | 325,289 | 1.4 | (4) | (4) |
| 9. | Maxicare—South California | 298,182 | 1.3 | 3.2 | 22 |
| 10. | Kaiser Foundation Health Plan of Northwest Oregon | 289,197 | 1.2 | 5.0 | 9 |
| 11. | Medcenters Health Plan—St. Louis Park—Minnesota | 238,033 | 1.0 | 5.9 | 10 |
| 12. | HMO Illinois—Chicago | 226,045 | 1.0 | 1.6 | (4) |
| 13. | HMO of New Jersey—Paramus | 219,884 | 0.9 | 2.4 | 18 |
| 14. | Harvard Community Health Plan | 218,534 | 0.9 | 1.6 | 51 |
| 15. | Group Health—Minnesota/St. Paul | 209,198 | 0.9 | 3.4 | 20 |
| 16. | CIGNA Health Plan of Arizona | 201,724 | 0.8 | (4) | (4) |
| 17. | Health Alliance Plan of Michigan | 189,302 | 0.8 | (4) | (4) |
| 18. | Compcare Health Services Insurance Corporation—Wisconsin | 181,500 | 0.8 | (4) | (4) |
| 19. | International Medical Centers—Miami | 180,360 | 0.8 | 74.8 | 1 |
| 20. | Kaiser Foundation Health Plan of Colorado—Denver | 162,099 | 0.7 | 0.6 | 30 |
| All others | 14,400,316 | 60.8 | — | — | |
InterStudy: 1986 June Update. A mid-year report on HMO growth.
Health Care Financing Administration: Data from the Office of Prepaid Health Care.
Includes 49,361 persons enrolled in 3 plans on Guam.
No TEFRA risk enrollees.
The 20 largest TEFRA risk HMO's as of December 1986 are shown in Table 4. These 20 HMO's had 517,268 or 63.6 percent of the total enrollees. International Medical Centers of Florida had the largest number of enrollees, 129,499 or 15.9 percent, and Family Health Plan, Inc. of California followed with 48,420 or 6.0 percent. Five of the top 20 plans are in California: Family Health Plan, Inc., Pacificare, United Health Plan, Bay Pacific, and Inland Health Plan.
Table 4. Number of Medicare Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk health maintenance organization (HMO) enrollees and percent distribution, in the 20 HMO's that had the most Medicare enrollees: December 1986.
| Name of HMO | HMO Medicare enrollees | ||
|---|---|---|---|
|
| |||
| Number | Percent | ||
| Total, TEFRA risk | 813,712 | 100.0 | |
| Top 20 TEFRA risk | 517,268 | 63.6 | |
| 1. | International Medical Centers—Florida | 129,499 | 15.9 |
| 2. | Family Health Plan, Inc.—California | 48,420 | 6.0 |
| 3. | PacifiCare Inc., California | 45,779 | 5.6 |
| 4. | Physicians Health Plan of Minnesota | 45,384 | 5.6 |
| 5. | SHARE Health Plan Minnesota | 42,082 | 5.2 |
| 6. | Comprehensive American Care-Florida | 18,218 | 2.2 |
| 7. | SHARE Illinois | 17,502 | 2.2 |
| 8. | HMO—Pennsylvania | 16,735 | 2.1 |
| 9. | Kaiser—Northwest Oregon | 15,747 | 1.9 |
| 10. | Medcenters Health Plan—Minnesota | 15,672 | 1.9 |
| 11. | United Health Plan (Watts—California) | 15,003 | 1.8 |
| 12. | Blue Care—Michigan | 14,943 | 1.8 |
| 13. | Hawaii Medical Service Association-Hawaii | 14,897 | 1.8 |
| 14. | Fallon Community Health Plan—Massachusetts | 12,559 | 1.5 |
| 15. | Bay Pacific—California | 11,880 | 1.5 |
| 16. | Inland Health Plan—California | 11,487 | 1.4 |
| 17. | Family Health Plan—Arizona | 11,420 | 1.4 |
| 18. | HMO—New Jersey | 11,085 | 1.4 |
| 19. | Health Plan of Nevada | 10,549 | 1.3 |
| 20. | Group Health Inc.—Minnesota | 8,407 | 1.0 |
SOURCE: Health Care Financing Administration: Data from the Office of Prepaid Health Care.
HMO characteristics
Multi-State networks of HMO's linked by common ownership or management have contributed greatly to the rapid growth in HMO enrollment (InterStudy, 1986). The five largest TEFRA risk multi-State or chain operations are shown in Table 5. These 5 multi-State organizations operated under 20 different contracts and accounted for 30.7 percent of TEFRA risk enrollees in December 1986. All except U.S. Health Care Systems of Pennsylvania are headquartered in California. United Health Plan had the largest number of enrollees in TEFRA risk contracts in four States that had a total combined enrollment of 65,428 or 8.0 percent of TEFRA risk enrollees; Family Health Plan, Inc. ranked second in TEFRA risk contracts in three States that had a total combined enrollment of 65,319.
Table 5. Number of plans and number and percent of Medicare enrollees in the 5 health maintenance organization (HMO) chains that had the most Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk enrollees: December 1986.
| HMO chain and participating States | Number of plans | Number of enrollees | Percent of enrollees |
|---|---|---|---|
| Total, TEFRA risk | 149 | 813,712 | 100.0 |
| Risk, top 5 chains | 20 | 250,215 | 30.7 |
| United Health Plan | |||
| (Minnesota, Illinois, Iowa, Nebraska) | 4 | 65,428 | 8.0 |
| Family Health Plan, Inc. | |||
| (New Mexico, Arizona, California) | 3 | 65,319 | 8.0 |
| PacifiCare, Inc. | |||
| (California, Oregon) | 2 | 51,253 | 6.3 |
| Maxicare | |||
| (Pennsylvania, Florida, Illinois, Michigan, Indiana, California) | 8 | 35,809 | 4.4 |
| U.S. Health Care Systems of Pennsylvania | |||
| (New Jersey, Pennsylvania, Illinois) | 3 | 32,406 | 4.0 |
NOTE: All plans are headquartered in California except U.S. Health Care Systems of Pennsylvania.
SOURCE: Health Care Financing Administration: Data from the Office of Prepaid Health Care.
HMO's may use one or more organizational models to deliver services to the enrollees. The four current types of HMO models and the number of enrollees in each type are shown in Table 6. The majority of all HMO's operate under the independent practice association (IPA) arrangement—58.0 percent of total HMO's and 56.4 percent of Medicare TEFRA risk plans. Under an IPA arrangement, an HMO contracts directly with physicians in solo or group practice. This type of model allows the enrollee whose physician signs with an HMO to keep this physician as his/her personal doctor in the HMO, perhaps contributing to their growing popularity.
Table 6. Number and percent of total health maintenance organization (HMO) and Medicare Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk plans and enrollees, by type of model.
| Type of model | Plans | Enrollees | ||
|---|---|---|---|---|
|
|
|
|||
| Number | Percent | Number | Percent | |
| Total HMO's1 | 595 | 100.0 | 23,663,626 | 100.0 |
| IPA | 345 | 58.0 | 8,454,157 | 35.7 |
| Group | 86 | 14.5 | 7,118,377 | 30.1 |
| Staff | 71 | 11.9 | 3,135,830 | 13.3 |
| Network | 93 | 15.6 | 4,955,262 | 20.9 |
| Medicare TEFRA risk2 | 149 | 100.0 | 813,712 | 100.0 |
| IPA | 84 | 56.4 | 344,022 | 42.3 |
| Group | 33 | 22.1 | 224,165 | 27.5 |
| Staff | 24 | 16.1 | 108,360 | 13.3 |
| Network | 8 | 5.4 | 137,165 | 16.9 |
As of June 1986, InterStudy: 1986 June Update. A mid-year report on HMO growth.
As of December 1986. Health Care Financing Administration: Data from the Office of Prepaid Health Care.
Total enrollment in HMO's with IPA arrangements grew from 1.6 million or 15 percent of total HMO enrollment in June 1981 to 8.5 million or 36 percent in June 1986. Medicare enrollment under TEFRA risk IPA models from September 1985 through December 1986 grew from 65,631 or 18.0 percent of total TEFRA risk to 344,022 or 42.3 percent. More Medicare HMO enrollees are in IPA's than in any other model.
Network models (i.e., those HMO's that contract predominately with two or more independent practices) ranked second among HMO's nationwide in June 1986 and accounted for 15.6 percent of HMO's and 20.9 percent of enrollees. In contrast, network models under TEFRA risk plans in December 1986 accounted for only 5.4 percent of plans and 16.9 percent of enrollees.
Group models (HMO's that contract predominately with one independent group practice) ranked third among HMO's nationwide and accounted for 14.5 percent of all HMO's. Although the group models were fewer in number than network models, they accounted for a larger proportion, 30.1 percent, of enrollees. In comparison, group models under TEFRA risk plans in December 1986 accounted for 22.1 percent of plans and 27.5 percent of enrollees.
Nationwide in June 1986, HMO's operating under staff models (those that deliver health services through a physician group that is controlled by the HMO) accounted for 11.9 percent of HMO's and 13.3 percent of enrollees. In December 1986, the proportion of staff models and enrollees under TEFRA risk plans were not very different from the nationwide figures mentioned, 16.1 percent of plans and 13.3 percent of enrollees.
According to a national HMO census from InterStudy (1986), the number of for-profit HMO's surpassed the number of nonprofit plans for the first time during the latter half of 1985. In June 1986, 58.5 percent of the HMO's reporting profit status were for-profit plans and accounted for 38.2 percent of enrollees; 39.8 percent were nonprofit with 61.5 percent of enrollees (Table 7).
Table 7. Number and percent distribution of total health maintenance organization (HMO) and Medicare Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk plans and enrollees, by profit status.
| Profit status | Number of plans | Percent | Number of enrollees | Percent |
|---|---|---|---|---|
| All HMO's, June 19861 | 2595 | 100.0 | 23,663,626 | 100.0 |
| For-profit | 348 | 58.5 | 9,037,890 | 38.2 |
| Nonprofit | 237 | 39.8 | 14,552,955 | 61.5 |
| Medicare TEFRA risk—October 19863 | 149 | 100.0 | 813,712 | 100.0 |
| For-profit | 63 | 42.3 | 383,882 | 47.2 |
| Nonprofit | 86 | 57.7 | 429,830 | 52.8 |
InterStudy. 1986 June Update. A mid-year report on HMO growth.
Health Care Financing Administration: Data from the Office of Prepaid Health Care.
Includes 10 plans not reporting profit status.
The proportion of for-profit plans under TEFRA risk contracts was less than that for all HMO's (42.3 percent versus 58.5 percent). The proportion of enrollees in for-profit plans, however, was considerably greater than that for all HMO's (47.2 percent versus 38.2 percent).
Benefits above Medicare
All TEFRA risk HMO's cover Medicare deductibles and coinsurance. All TEFRA risk HMO's offered Medicare beneficiaries one or more benefits in addition to the services covered by Medicare, such as additional hospital days, preventive care, prescription drugs, and routine eye examination or eyeglasses. Some services require a copayment amount. For example, some HMO's may require a copayment for each drug prescription. In December 1986, 120 or 80.5 percent of the 149 TEFRA risk plans offered coverage of hospital days in addition to those covered by Medicare; 123 or 82.6 percent covered some preventive care such as routine physicals; 105 or 70.5 percent offered coverage for prescription drugs; and 103 or 69.1 percent offered some eye care coverage such as routine eye examination and eyeglasses (Table 8).
Table 8. Number and percent of Medicare Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 risk health maintenance organizations (HMO's) providing benefits in addition to Medicare, and number and percent of enrollees, by type of benefit: December 1986.
| Type of benefit | Plans | Enrollees | ||
|---|---|---|---|---|
|
|
|
|||
| Number | Percent | Number | Percent | |
| Total | 149 | 100.0 | 813,712 | 100.0 |
| Extended hospital days | 120 | 80.5 | 630,447 | 77.5 |
| Extended SNF1 days | 56 | 37.6 | 249,675 | 30.7 |
| Preventive care | 123 | 82.6 | 695,864 | 85.5 |
| Drugs | 105 | 70.5 | 689,560 | 84.7 |
| Eye care | 103 | 69.1 | 596,099 | 73.3 |
| Ear care | 55 | 36.9 | 337,120 | 41.4 |
| Dental care | 23 | 15.4 | 310,386 | 38.1 |
| Extended mental health | 52 | 34.9 | 137,192 | 16.9 |
| Miscellaneous | 54 | 36.2 | 421,448 | 51.8 |
SNF is for skilled nursing facility.
SOURCE: Health Care Financing Administration: Data from the Office of Prepaid Health Care.
Most TEFRA risk enrollees, 77.5 percent, were enrolled in HMO's that offered extended hospital days, 85.5 percent were in ones that offered preventive care, and 84.7 percent were in ones that offered a prescription drug benefit. Also, most enrollees, 73.3 percent, were enrolled in HMO's that offered some type of eye care.
In December 1986, the basic premium charge under TEFRA risk HMO's ranged from no charge to $50.76 per month. Twenty-one HMO's or 14 percent had no premium charge for their basic plan and most of these offered extended hospital days and/or preventive care and eye care. Of the 21 plans that had no basic premium charge, 15 had a copayment charge on at least one type of service and 6 did not have a copayment charge. Sixteen HMO's or 11 percent had basic premiums of $40.00 or more. All but one of these HMO's offered extended hospital days, 8 offered extended skilled nursing facility days, and 14 offered preventive care. Eleven of these plans required a copayment on at least one type of service, and five did not.
Future study
In view of the steady growth in Medicare HMO enrollment and the strong interest in HMO's as an alternative delivery system for Medicare beneficiaries, it will be increasingly important to analyze patterns of Medicare enrollment in HMO's. An indepth analysis of trends in HMO enrollment is now in progress. That study will examine enrollment by demographic variables such as age, sex, and race; length of enrollment, geographic area, and type of plan; and several other variables.
Acknowledgments
The authors wish to thank Lois Landolina and Cathy Carter of the Office of Prepaid Health Care for their assistance in making available much of the data presented in this article. A special thanks to Marian Gornick for her valuable suggestions provided during the preparation of this article.
Footnotes
Reprint requests: Alma McMillan, Health Care Financing Administration, 2-C-16 Oak Meadows Building, 6325 Security Boulevard, Baltimore, Maryland 21207.
TEFRA defines two types of organizations that can qualify for risk contracts, HMO's, and competitive medical plans (CMP's). HMO's are organizations meeting the HMO requirements of section 1310 of the Social Security Act; CMP's are capitated plans that meet the less extensive requirements in TEFRA. Both are referred to as HMO's in this article. Of the 149 TEFRA risk contracts in December 1986, 17 were with CMP's.
In both the data on total HMO enrollment from InterStudy and the Medicare data, HMO enrollment is assigned to States according to location of the plan. Thus, the high percent of HMO enrollment in the District of Columbia represents an artifact of the data. Several HMO's having main offices in the District of Columbia have members living in the neighboring States of Maryland and Virginia.
References
- InterStudy. 1986 June Update. Excelsior, Minn.: 1986. A mid-year report on HMO growth. [Google Scholar]
- InterStudy. National HMO Census 1985, Annual Report on the Growth of HMO's. Excelsior, Minn.: 1986. [Google Scholar]
- Trieger S, Galblum TW, Riley G. HMO's: Issues and Alternatives for Medicare and Medicaid. Washington. U.S.: Government Printing Office; Apr, 1981. HCFA Pub. No. 03107. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [Google Scholar]