Abstract
Based on data from the National Medical Care Utilization and Expenditure Survey, the 10 percent of the noninstitutionalized U.S. population that incurred the highest medical care charges was responsible for 75 percent of all incurred charges. Health status was the strongest predictor of high-cost use, followed by economic factors. Persons 65 years of age or over incurred far higher costs than younger persons and had higher out-of-pocket costs, absolutely and as a percentage of income, although they were more likely to be insured.
Introduction
It is well known that a small minority of the U.S. population accounts for a majority of national health care expenditures. Relatively little is known about these people, however. Are high-cost users of medical care more likely to be wealthy or poor? What kinds of health insurance do they have? How much of their medical care expenses must they pay out of pocket? Are their health care needs greater than those of other persons, or do other factors determine their high use of medical care? The answers to these questions can yield insights into several areas of public concern, including the aggregate consumption of health care resources, access to care, and the financial burden experienced by individuals who incur high costs.
The extensive use of health care resources by a small segment of the population has been documented for individuals and families, using several different criteria of high cost in a variety of populations, including Medicare beneficiaries, Federal employees, and the U.S. population as a whole. The estimates of high-cost use in these populations are remarkably similar. Birnbaum (1978a, 1978b) reported that the 1.2 percent of the total U.S. population with the highest medical charges incurred 20 percent of the total charges in 1977, including charges for nursing home care. In a Congressional Budget Office (1982) report on Federal employees covered by Blue Cross and Blue Shield, it was shown that the 1 percent of families with the highest medical charges accounted for 22 percent of total expenditures in 1978.
In other studies, the concentration of Medicare expenditures among the aged Medicare population has been described. Riley et al. (1986) reported that the top 1 percent of aged Medicare beneficiaries accounted for 21 percent of expenditures in 1975 and 20 percent in 1982. Gornick, Beebe, and Prihoda (1983) found that 14 percent of aged Medicare beneficiaries accounted for 84 percent of Medicare reimbursements nationally in 1980, and McCall and Wai (1983) reported that 19 percent of aged Medicare beneficiaries in Colorado incurred 88 percent of Medicare-allowed charges in 1978. Thus, it appears that the distribution of expenditures is similarly skewed for persons under 65 years of age, persons 65 years or over, and the population as a whole. Moreover, the distribution of expenditures remained stable from the mid-1970's to the early 1980's.
The purpose of this article is to identify the characteristics of the small segment of the noninstitutionalized population that incurs high medical care costs in order to improve our understanding of factors that contribute to high costs. Clearly, the most appropriate reason for using medical resources is the need for medical care (i.e., health status). Other factors that have been shown to be related to the use of services include factors that enable people to obtain care, such as insurance coverage and income; predisposing personal characteristics, such as age and sex; the cost of care; and the supply of medical resources (Andersen, 1968; Aday, Andersen, and Fleming, 1980; Newhouse et al., 1981; Newhouse, 1978; Rice, 1983).
Thus, we hypothesize a model in which the probability of incurring high costs is a function of health status; personal financial resources, including income and insurance coverage; other personal characteristics; and community characteristics, such as the local cost of living, cost of medical care, and supply of inpatient and ambulatory medical care resources. To identify the unique contribution of each of these factors, we have conducted a three-step analysis.
First, we have described the distribution of medical expenses in the population; second, we have selected a criterion by which to classify high-cost persons; and third, we have regressed the variable indicating high-cost use on these potential explanatory factors. In addition, we have explored the relationship between high total costs and high out-of-pocket expenditures.
Methods
The data used in this study pertain to the civilian noninstitutionalized population of the United States and were collected in 1980 through the National Medical Care Utilization and Expenditure Survey, or NMCUES (Bonham, 1983). Household respondents reported extensive information about charges incurred for health care, payments made by all sources, and personal characteristics, including health status, income, and insurance coverage. The NMCUES sample comprised 15,189 persons under age 65 and 1,934 persons 65 years or over. The unit of analysis for this article is the individual. The analysis includes charges for all services except ambulatory dentistry and nursing home care.
Household interview data have several advantages over insurance claims data, which were used for most of the studies mentioned in the introduction. NMCUES data include information about health and socioeconomic status that is not usually available from claims and billing data. NMCUES also includes data on charges for all types of health care and payments by all sources; these are unavailable from hospital billing records alone or from insurance claims, which rarely cover all types of services.
NMCUES information on charges and expenditures is more subjective than data from claims and billing information systems. Household respondents are sometimes unaware of the full charge or payment for services, necessitating imputations for missing data. Furthermore, NMCUES data do not include information on the institutionalized population, which was found to account for 43 percent of all catastrophic health care costs according to Birnbaum's (1978a) definition. Nevertheless, NMCUES provides unusually comprehensive data on expenditures and personal characteristics of the 95 percent of the U.S. population who were not living in institutions in 1980.
Data on community characteristics in 1980 were obtained for each individual from the Area Resource File (Bureau of Health Professions, 1983). The cost of living was represented by the median gross rent for the county of residence. The supply of inpatient resources was measured by the number of short-stay hospital beds per 1,000 persons in the county of residence and all contiguous counties. The supply of physicians was represented by the number of doctors of medicine and osteopathy per 100,000 persons in the county of residence and contiguous counties.
The cost of medical care in the community was represented by the 75th percentile of prevailing charges to Medicare for a routine followup office visit by a general practitioner in the county of residence. These data were obtained from the Medicare Directory of Prevailing Charges, 1980 (Health Care Financing Administration, 1980).
The parameters of the model were estimated using logistic regression. Logistic regression is an appropriate statistical method for analyzing the relationship between the proportion of persons who incur high costs (a dichotomous dependent variable) and explanatory variables because it is not based on the assumptions that the relationship is linear and the error terms are homoscedastic and because predicted proportions lie within the valid 0-1 range of probabilities.
Important correlates of high-cost use were identified from among a set of hypothesized correlates using an ordinary stepwise logistic regression procedure (Harrell, 1983). The reduced models were then fit using a weighted logistic regression procedure that adjusted for the effects of unequal probabilities of selection and the complex sample design of NMCUES (Shah et al., 1984).
The analysis was conducted separately for persons under 65 years of age and persons 65 years or over because separate policy questions often arise for the two groups. They differ substantially with respect to insurance coverage and utilization. Almost everyone 65 years of age or over has Medicare as primary insurance; persons under 65 may be uninsured or may have private insurance or Medicaid as their primary coverage. Moreover, persons 65 years or over use more health care services, on average, than younger persons do (Garfinkel, Wheeless, and Corder, 1985).
As with all sample surveys, NMCUES estimates are subject to sampling error. The relative standard errors of the estimates presented in this article are available from the authors.
Distribution of charges
In Table 1, the distribution of total charges for medical care is compared with the corresponding population percentile for the total noninstitutionalized population, persons under 65 years of age, and persons 65 years or over. The 1 percent of the total population with the highest charges (i.e., persons above the 99th percentile of the charge distribution) incurred at least $8,744 per person in total charges and accounted for 29 percent of all charges incurred by the population. Among persons under age 65, the most expensive 1 percent incurred charges of at least $6,833 and were responsible for 28 percent of total charges. The top 1 percent of persons 65 years of age or over incurred at least $16,701 in charges, more than twice as much as persons under 65 years, and accounted for 21 percent of the charges incurred by this age group. The slightly more even distribution of charges among the older group suggests that a greater percentage of older persons experienced substantial medical expenses.
Table 1. Charges for personal medical services and percent of charges, by age and population percentile: United States, 1980.
| Population percentile (highest percent)1 | All ages | Under 65 years | 65 years or over | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Charges incurred2 | Percent of charges | Charges incurred2 | Percent of charges | Charges incurred2 | Percent of charges | |
| 1 | $8,744 | 29 | $6,833 | 28 | $16,701 | 21 |
| 10 | 1,258 | 75 | 1,012 | 73 | 4,001 | 68 |
| 15 | 655 | 82 | 543 | 81 | 2,595 | 79 |
| 25 | 316 | 90 | 269 | 89 | 866 | 89 |
| 30 | 244 | 92 | 212 | 91 | 636 | 91 |
| 50 | 104 | 98 | 92 | 97 | 286 | 97 |
Population percentiles are specified in descending order. For example, the second row of the table indicates the percent of charges incurred by the 10 percent of the population incurring the highest charges or, alternatively, persons above the 90th percentile of the distribution of persons.
Charges incurred by the person at the indicated population percentile.
NOTES: All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980. Persons who did not incur any charges are included in the distribution.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
The charges for persons age 65 years or over were consistently higher than charges for persons under age 65 at each point in the distribution. For example, the minimum amount incurred by the most costly 10 percent of the older population, $4,001, was four times the minimum amount incurred by the most costly 10 percent of the younger group, $1,012. The median charge incurred by persons age 65 or over, $286, was three times the median charge of persons under age 65, $92.
High-cost criteria
Definition of high cost
For the purpose of this study, the high-cost population was defined as that group of persons who accounted for a disproportionately large share of all medical charges.
Among persons under age 65, the 15 percent of the population between the 75th ($269) and 90th ($1,012) percentiles accounted for 15 percent of all charges and, thus, is defined empirically as the normative cost group. The 10 percent of the population above the 90th percentile ($1,012) was responsible for 73 percent of all charges and, thus, represents the group that incurred a disproportionately large share of all charges. These persons have been defined as the high-cost group under age 65. Persons below the 75th percentile of the population are included in both the low-cost and no-cost groups. Those who incurred some charges (56 percent of the population under age 65) were defined as the low-cost group because they incurred a disproportionately small percentage of all charges. The remaining 19 percent of persons under age 65 did not incur any charges for medical care in 1980.
Using the same criteria for persons 65 years of age or over, the 15 percent of the population between the 70th ($636) and 85th ($2,595) percentiles was defined as the medium, or normative, cost group because they incurred charges in proportion to their percentage of the population. The 15 percent of the population above the 85th percentile was defined as the high-cost group. This group accounted for 79 percent of all charges. The low-cost group comprised 60 percent of the population, and 10 percent of the population incurred no charges. The distributions of both age groups among the four cost classifications are compared in Table 2.
Table 2. Percent distributions of persons and of total charges for personal medical services, by age and cost level: United States, 1980.
| Cost level | Under 65 years | 65 years or over | ||
|---|---|---|---|---|
|
|
|
|||
| Persons | Total charges | Persons | Total charges | |
|
| ||||
| Percent distribution | ||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 |
| High | 10.0 | 73.3 | 15.0 | 78.7 |
| Medium | 15.0 | 15.6 | 15.0 | 12.7 |
| Low | 55.9 | 11.1 | 59.7 | 8.6 |
| None | 19.1 | 0.0 | 10.2 | 0.0 |
NOTES: All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980. Persons who did not incur any charges are included in the distribution.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Utilization and cost
The intensive use of medical resources can be defined in terms of both cost and utilization. Although we have chosen to focus on cost in this article, a brief discussion of the relationship between cost and utilization is worthwhile because it tells us more about whom we have defined as a high-cost user.
The use of inpatient hospital services is strongly associated with incurring high costs. Among persons under age 65, 73 percent of those with one hospital stay and 93 percent of those with two hospital stays were classified as high-cost users, compared with less than 2 percent of those without a hospital stay. Among persons under 65 years who were classified as high-cost users, 84 percent had at least one hospital stay. Sixteen percent of high-cost users under age 65 had no hospital stay and, thus, incurred high charges from other medical services.
Among persons age 65 or over, only 51 percent of persons with one hospital stay, but 95 percent of persons with two stays, were classified as high-cost users. Of the persons age 65 or over who were classified as high-cost users, 97 percent had at least one hospital stay. These persons were divided about evenly between those with one stay and those with two stays or more.
Having at least one hospital stay is highly associated with incurring high costs in both age groups. However, only one-quarter of the younger group with one hospital stay were not considered high-cost users, but one-half of the persons age 65 or over with one hospital stay were below the cutoff. This is a further example of the more even distribution of expenses in the older age group. Incurring the charges associated with a hospital stay was less likely to place persons age 65 or over at the extreme end of the charge distribution because hospital stays are far more common in this age group.
Multivariable model of high-cost use
Introduction
In the preceding sections, we described the distribution of health care charges in the noninstitutionalized U.S. population and presented a classification scheme for high-cost use. In this section, we describe characteristics of the population that are associated with high-cost use. The multivariable model discussed later enables us to identify the characteristics that are most highly associated with high-cost use while controlling for the effects of other characteristics. The univariate distributions of persons in each cost group by several personal and health characteristics are available for both age groups from the authors.
Children have been excluded from the model because their high-cost experience is most likely to be associated with hospital stays for birth. We are mainly interested in high costs associated with illness. Furthermore, the marriage, employment, and functional limitations variables are undefined for children under age 17. Thus, the model of factors associated with high costs was estimated separately for persons 17-64 years of age and persons age 65 or over.
Variables
The model describes the relationship between high costs, defined as being in the high-cost group (the dependent variable), and characteristics of individuals and the communities in which they live (the independent variables). The characteristics of individuals include their demographic characteristics, economic resources, and health status. The characteristics of their communities include the cost of medical care, the cost of other goods and services, and the supply of medical care resources.
The independent variables in this model include age, race, sex, marital status, education, and whether the respondent lived alone (to represent demographic characteristics); family income, poverty level, employment status, and insurance coverage (to represent economic characteristics); and perceived health status, number of chronic conditions, number of restricted-activity days, score on a functional limitations scale, and whether the respondent died during the survey (to represent health status). The model also includes an indication of whether the individual had a usual source of medical care. Information on financial assets, an important measure of personal economic resources, would have improved the model from a theoretical perspective but is unavailable from NMCUES.
Community characteristics include U.S. census region, type of community in which the respondent lived (e.g., central city of standard metropolitan statistical area), cost of medical care, cost of other goods and services (a measure of the cost of living in general), and number of hospital beds per 1,000 persons and number of physicians per 100,000 persons (to account for the effect of resource availability).
These variables are shown in Table 3 for persons age 17-64 and persons 65 years of age or over. An unweighted model using the full set of independent variables was first estimated for each age group using the stepwise logistic regression procedure in Statistical Analysis System (SAS) (Harrell, 1983).1 Variables significant at the 0.15 level were included in a reduced weighted model for each age group using the RTILOGIT procedure for weighted logistic regressions of complex sample survey data (Shah et al., 1984). The weighted model was then reestimated using only those variables significant at the 0.15 level. Although it is usual to choose 0.05 as the criterion for significance, we have chosen to indicate variables that were close to being significant by using 0.15 as the criterion for inclusion in the final model. The discussion of results is based on variables that were significant at the 0.05 level.
Table 3. Weighted descriptive means and proportions for the variables in the high-cost regression models, by age: United States, 1980.
| Variable | 17-64 years | 65 years or over |
|---|---|---|
| Dependent variable | ||
| High-cost user | 0.12 | 0.15 |
| Independent variables | ||
| Age as of July 1, 1980 (years) | 37 | 73 |
| Race: White | 0.87 | 0.90 |
| Sex: Male | 0.48 | 0.41 |
| Marital status: | ||
| Married | 0.62 | 0.53 |
| Widowed, separated, or divorced | 0.13 | 0.41 |
| Never married | 0.24 | 0.06 |
| Education of head of family (years) | 12 | 10 |
| Living alone | 0.13 | 0.33 |
| Annualized family income (1980) | $27,378 | $14,644 |
| Poverty level (percent)1 | 353 | 264 |
| Employment status: | ||
| Full time | 0.49 | 0.07 |
| Part time | 0.31 | 0.12 |
| Unemployed— | ||
| In labor force | 0.03 | 0.02 |
| Retired | 0.04 | 0.77 |
| Other | 0.13 | 0.02 |
| Covered by Medicare | 0.03 | 0.98 |
| Covered by Medicaid | 0.07 | 0.17 |
| Covered by private health insurance | 0.83 | 0.71 |
| Covered by other public plans or programs | 0.08 | 0.05 |
| Not insured | 0.08 | 0.01 |
| Perceived health status: | ||
| Excellent | 0.49 | 0.26 |
| Good | 0.38 | 0.37 |
| Fair | 0.09 | 0.25 |
| Poor | 0.04 | 0.12 |
| Number of chronic conditions | 1.54 | 3.24 |
| Number of restricted-activity days | 13.32 | 30.41 |
| Functional limitations score2 | 1.43 | 3.11 |
| Died during survey period | 0.002 | 0.02 |
| Census region: | ||
| Northeast | 0.22 | 0.20 |
| North Central | 0.27 | 0.24 |
| South | 0.31 | 0.34 |
| West | 0.20 | 0.22 |
| Type of community: | ||
| SMSA central city | 0.29 | 0.31 |
| SMSA remainder | 0.41 | 0.34 |
| Not SMSA—urban | 0.13 | 0.17 |
| Not SMSA—rural | 0.18 | 0.18 |
| Medicare prevailing charge (cost of medical care) | $33 | $33 |
| 1980 median gross rent (cost of other goods and services) | $236 | $231 |
| Hospital beds per 1,000 population | 4.63 | 4.65 |
| Number of physicians3 per 100,000 population | 164 | 161 |
Ratio of family income, adjusted for age and sex of the family head and family size, to 1980 national nonfarm poverty level income.
An 8-point scale (0-7) indicating ability to perform tasks related to work, recreation, household chores, and transportation. Increasing score reflects greater limitations.
Medical doctors and doctors of osteopathy.
NOTES: SMSA is standard metropolitan statistical area. All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Results
Persons age 17-64 years
In Table 4, we present the results of the reduced weighted logistic regression model for persons 17-64 years of age. Significant effects were found for individual demographic, economic, and health characteristics and characteristics of the community. The importance of each variable in explaining high-cost use, controlling for all other variables in the model, is indicated by the magnitude of the partial correlation coefficient, R (Harrell, 1983).
Table 4. Results of reduced-model logistic regression procedure for persons 17-64 years of age: United States, 1980.
| Independent variable | Logistic regression coefficient | Standard error | Level of significance | Partial correlation coefficient (R) |
|---|---|---|---|---|
| Intercept | –2.9973 | 0.2943 | < 0.0001 | — |
| Health status | ||||
| Number of restricted-activity days | 0.0246 | 0.0012 | < 0.0001 | 0.233 |
| Number of chronic conditions | 0.2024 | 0.0190 | < 0.0001 | 0.121 |
| Died during survey period1 | 2.0552 | 0.5330 | 0.0001 | 0.041 |
| Perceived health status2: | ||||
| Good | 0.1471 | 0.0748 | 0.1064 | 0.016 |
| Fair | 0.3954 | 0.1121 | 0.0011 | 0.037 |
| Functional limitations score3 | 0.0684 | 0.0300 | 0.0754 | 0.020 |
| Economic characteristics | ||||
| Employment2: | ||||
| Employed part time | 0.6370 | 0.0837 | < 0.0001 | 0.085 |
| Unemployed— | 0.7369 | 0.1949 | 0.0022 | 0.040 |
| In labor force | ||||
| Retired | 0.4391 | 0.1849 | 0.0366 | 0.022 |
| Other | 0.5740 | 0.1155 | 0.0001 | 0.054 |
| Covered by Medicaid1 | 0.3423 | 0.1290 | 0.0272 | 0.026 |
| Not insured1 | –1.1253 | 0.1935 | < 0.0001 | –0.064 |
| Poverty level4 | 0.0006 | 0.0001 | 0.0025 | 0.034 |
| Demographic characteristics | ||||
| Age | –0.0228 | 0.0033 | < 0.0001 | –0.076 |
| Marital status2: | ||||
| Widowed, separated, or divorced | –0.3620 | 0.1193 | 0.0116 | –0.030 |
| Never married | –0.5704 | 0.1109 | < 0.0001 | –0.056 |
| Male1 | –0.3716 | 0.0773 | < 0.0001 | –0.052 |
| Living alone1 | 0.2550 | 0.1249 | 0.0794 | 0.017 |
| Education of head of family | 0.0224 | 0.0134 | 0.1310 | 0.010 |
| Community characteristics | ||||
| North Central census region2 | 0.1258 | 0.0772 | 0.1172 | 0.009 |
| SMSA5 central city2 | 0.2535 | 0.0799 | 0.0156 | 0.032 |
| 1980 median gross rent | 0.0025 | 0.0011 | 0.0359 | 0.020 |
| Number of physicians6 per 100,000 population | –0.0027 | 0.0008 | 0.0115 | –0.034 |
Dichotomous variables for which the reference level is the opposite of the specified level.
Omitted levels for multilevel categorical variables are poor health status, employed full time, married, West Region, and rural community outside standard metropolitan statistical area.
An 8-point scale (0-7) indicating ability to perform tasks related to work, recreation, household chores, and transportation. Increasing score reflects greater limitations.
Ratio of family income, adjusted for age and sex of the family head and family size, to 1980 national nonfarm poverty level income.
Standard metropolitan statistical area.
Medical doctors and doctors of osteopathy.
NOTES: The proportion of log-likelihood explained by the model (R2) is 0.222. The overall model level of significance is <0.0001. n (unweighted) is 10,309. The dependent variable is high-cost indicator. All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Health status
The probability of high-cost use should increase as health status declines. Poorer health is represented in the model by more restricted-activity days, chronic conditions, and functional limitations. Thus, positive relationships between high-cost use and these variables were expected.
As expected, high costs were associated with more restricted-activity days and chronic conditions. These measures of health status were considerably more important than any other variable for persons age 17-64. The other measures of health that were significant at the 0.05 level, died during the survey and fair health, both made weak to moderate contributions to the explanation of high costs. Persons who died during the survey were more likely to incur high costs than those who survived. Persons who reported fair health were more likely to incur high costs than persons in excellent health. The predominance of health status is desirable because it indicates that consumption of health care resources was primarily influenced by medical need rather than by personal preference, availability, or economic factors (Andersen, 1968).
Economic characteristics
Increased ability to pay for medical care has been associated with a greater probability of incurring high costs. Thus, increasing family income, increasing ratio of family income to the national poverty level, and the presence of insurance coverage were expected to be positively associated with high costs.
Full-time employment was expected to be negatively related to high costs because persons who use medical resources intensively may be less able to hold a full-time job. The negative association between full-time employment and high costs could be offset to some extent by the positive effects of better insurance coverage and higher income that generally accompany full-time employment. Because the effects of the three potentially confounding factors—income, insurance coverage, and several aspects of health status—are estimated separately in the model, we did not expect to find a statistical association between employment and high costs.
The expected effects were found for measures of insurance and income. Persons age 17-64 who were not insured were less likely to incur high costs than those who were insured, and Medicaid eligibles were more likely to incur high costs than persons without Medicaid. The probability of incurring high costs increased as the ratio of family income to the poverty level increased.
Employment status was significant, despite the fact that insurance coverage, income, and several health status measures were controlled. Persons who were employed part time and those who were unemployed for any reason were more likely to be high cost than persons employed full time. This negative association between full-time employment and the probability of incurring high costs suggests that persons who are ill may be less likely than others to hold a full-time job and that the health status variables included in the model may not have measured the aspect of health that is related to employment status.
Demographic characteristics
Age, sex, race, marital status, education, and family size (one person or more than one in family) were included in the initial model as control variables. The probability of high-cost use was expected to increase with age because increasing age is often accompanied by decreasing health status. However, to the extent that the effects of health status are accounted for by the health measures included in the model, the independent effect of age should diminish.
Age was found to be a relatively important predictor of high-cost use after controlling for health status, but the relationship was negative. This unexpected result might be attributable to the inclusion in the population 17-64 years of pregnant women, who incurred high costs associated with childbirth. Thus, some high-cost users might be younger women who reported good health. This result suggests that costs associated with childbirth should be treated separately; however, we were unable to identify them for this article.
It was expected that females would be more likely than males to incur high costs in the age group 17-64 years because of charges for childbirth. Race should have had no influence on the probability of incurring high costs after controlling for health status, insurance coverage, and income. Both of these hypotheses were found to be true.
Persons who are married generally report better health status than those who have never married or who are widowed, separated, or divorced. They are also more likely to avoid hospital stays because someone is home to care for them. Thus, married persons should be less likely to incur high costs. Alternatively, married individuals may be wealthier and better insured than unmarried persons and therefore more likely to incur high costs. Either relationship should attenuate after controlling for health status, income, and insurance coverage.
Unexpectedly, persons who were never married or formerly married were less likely to incur high costs than persons who were married. Because higher income and better insurance coverage are the most obvious explanations for this result, its persistence after controlling for income and insurance coverage is also unexpected. Some other characteristic associated with marriage—maybe childbirth and related costs— appears to be responsible for this relationship.
Community characteristics
The probability of high-cost use should be influenced by community characteristics because we have used a single high-cost criterion nationwide. Thus, persons who reside in higher cost communities should be more likely to meet the high-cost criterion that we have established for individuals. It is valuable to include measures of community cost level in the model, both to determine if they have an influence on high-cost use and to control for the effect of community characteristics when assessing the impact of personal characteristics. The community characteristics of interest include the region of the country, type of community of residence (i.e., the degree to which the community of residence is urban or rural based on definitions of the U.S. Bureau of the Census), the local cost of medical care, the local cost of living in general, and the availability of health care resources.
We found that persons living in central city communities within standard metropolitan statistical areas (SMSA's) were more likely to incur high costs than persons living elsewhere in SMSA's or outside SMSA's. There were no significant differences among the four major census regions of the United States. The probability of incurring high costs increased with the general cost of living (i.e., median gross rent) in the community. However, it was not sensitive to the cost of medical care (i.e., the Medicare prevailing office visit charge). The probability of incurring high costs decreased as the physician-to-population ratio increased, but the ratio of hospital beds to the population had no effect.
Persons age 65 or over
The reduced model for persons 65 years of age or over is presented in Table 5. High-cost use in this age group was mainly influenced by health status and economic resources. Community characteristics and demographic characteristics, with the exception of sex, had no effect on the probability of high-cost use.
Table 5. Results of reduced-model logistic regression procedure for persons 65 years of age or over: United States, 1980.
| Independent variable | Logistic regression coefficient | Standard error | Level of significance | Partial correlation coefficient (R) |
|---|---|---|---|---|
| Intercept | –5.1783 | 0.3196 | <0.0001 | — |
| Health status | ||||
| Number of chronic conditions | 0.2695 | 0.0285 | <0.0001 | 0.231 |
| Number of restricted-activity days | 0.0098 | 0.0011 | <0.0001 | 0.209 |
| Functional limitations score1 | 0.1202 | 0.0370 | 0.0046 | 0.072 |
| Died during survey period2 | 2.3511 | 0.4160 | <0.0001 | 0.135 |
| Economic characteristics | ||||
| Annual family income in 1980 | <0.0001 | <0.0001 | 0.0097 | 0.048 |
| Covered by private plan2 | 0.8706 | 0.2003 | 0.0001 | 0.102 |
| Covered by Medicaid2 | 0.6657 | 0.2015 | 0.0016 | 0.074 |
| Demographic characteristics | ||||
| Male2 | 0.6701 | 0.1685 | 0.0002 | 0.092 |
| Never married3 | 0.3221 | 0.1706 | 0.0712 | 0.031 |
An 8-point scale (0-7) indicating ability to perform tasks related to work, recreation, household chores, and transportation. Increasing score reflects greater limitations.
Dichotomous variables for which the reference level is the opposite of the specified level.
Omitted level for marital status is married.
NOTES: The proportion of log-likelihood explained by the model (R2) is 0.251. The overall model level of significance is <0.0001. n (unweighted) is 1,934. The dependent variable is high-cost indicator. All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Health status
The probability of high-cost use among persons 65 years of age or over increased with increases in the number of chronic conditions, the number of restricted-activity days, and the functional limitations score, all of which indicate decreasing health status. Persons who died during the survey period were more likely to incur high costs than those who did not die. By all four measures of health status, high costs were associated with poor health, which was the expected result. Chronic conditions and restricted-activity days were most strongly associated with high-cost use. This result is similar to the result observed for persons age 17-64 years.
Economic and demographic characteristics
Among persons 65 years of age or over, private insurance and Medicaid coverage as supplements to Medicare were positively associated with the probability of incurring high costs, as was annual family income. Persons who were better able to pay for care because they had higher incomes or insurance coverage were more likely to incur high costs. Both insurance variables made greater contributions to the explanation of high-cost use than income. Males were more likely to incur high costs than females.
Out-of-pocket expenditures
Up to this point, we have discussed high-cost use in terms of total charges incurred for health care rather than in terms of out-of-pocket expenditures. Out-of-pocket expenditures were not considered separately because our main objective is to study persons who consume large amounts of resources. Insurance coverage would obscure this information if out-of-pocket expenditures were used to define the high-cost group because insurance reduces the impact of high charges. Nevertheless, the extent to which out-of-pocket expenditures reach high levels is an important measure of the impact of high medical care costs on the individual.
When discussing total charges, the criterion for determining high costs was based on the distribution of charges in the population because we wished to identify persons who consumed a disproportionate share of resources. In the following discussion of out-of-pocket expenditures, the criteria for determining expenditure levels are actual dollars spent, absolutely and as a percentage of income. Dollars spent are a more realistic and understandable concept when speaking of individual burden.
Population distribution
As shown in Table 6, about 4.1 percent of the population under 65 years of age spent $500 or more out of pocket for personal medical care services, and 1.5 percent spent $1,000 or more. About 12 percent of persons 65 years of age or over spent at least $500 in out-of-pocket expenditures, and 5 percent spent at least $1,000. Thus, the percentages of older persons who exceeded both the $500 and $1,000 thresholds were about three times as high as the percentages of younger persons.
Table 6. Cumulative percent distribution of persons at or above specific amounts of out-of-pocket expenditures for personal medical services, by age: United States, 1980.
| Amount of out-of-pocket expenditure | Under 65 years | 65 years or over |
|---|---|---|
|
| ||
| Cumulative percent distribution | ||
| $0 | 100.0 | 100.0 |
| $100 | 29.3 | 56.0 |
| $200 | 14.2 | 36.7 |
| $300 | 8.5 | 24.7 |
| $400 | 5.7 | 17.1 |
| $500 | 4.1 | 12.4 |
| $1,000 | 1.5 | 5.0 |
| $3,000 | 0.2 | 0.4 |
| $5,000 | 0.1 | 0.1 |
NOTES: All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980. Persons who did not incur any out-of-pocket expenditures are included in the distribution.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Out-of-pocket expenditures and income
The burden imposed by out-of-pocket expenditures obviously varies by the resources available. To understand the impact of high out-of-pocket expenditures, it is useful to determine the variation in the percentage of persons who incur high out-of-pocket expenditures by income and the distribution of the population by out-of-pocket expenditures as a percentage of family income.
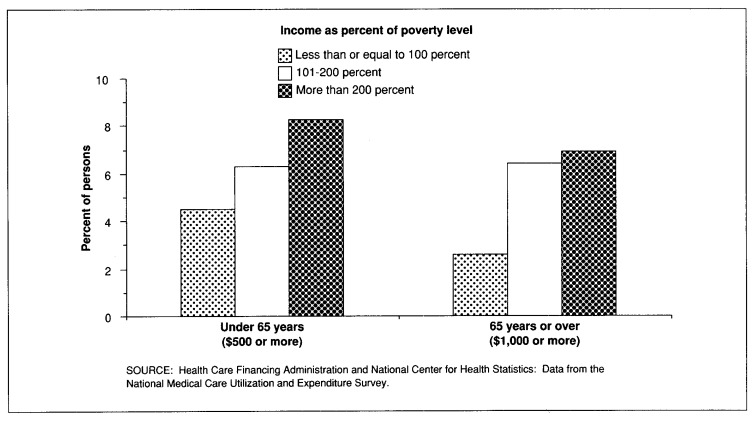
In Figure 1, we display the percentage of persons under age 65 and age 65 or over who met or exceeded an arbitrarily chosen level of out-of-pocket expenditures ($500 for persons under 65 and $1,000 for persons 65 or over) by poverty level. Poverty level represents the ratio of annual family income, adjusted for the age and sex of the head of household and the number of persons in the family, to national nonfarm poverty level income. As demonstrated in the figure, the percentage of persons with high out-of-pocket expenditures increased with adjusted family income, although the differences were not great. The relatively low prevalence of high out-of-pocket expenditures among the poorest persons reflects Medicaid coverage and free care.
Figure 1. Percent of persons under 65 years of age meeting or exceeding $500 in out-of-pocket expenditures for personal medical services and percent of persons 65 years of age or over meeting or exceeding $1,000 in such expenditures, by annual family income as a percent of poverty level: United States, 1980.
In Table 7, the effect of third-party payments on the burden of medical care charges is demonstrated by comparing the distributions of persons by the percentage of income spent out of pocket for medical care and by the percentage of income accounted for by total charges, excluding insurance premiums. Income is defined as the combined annualized income of the family of which the person was a member at the beginning of 1980. Income from wages, salaries, rents, pensions, and help from relatives was included; assets were excluded. The percentage of family income that is spent out of pocket is obviously less, on average, than the percentage of family income accounted for by the total charge. The difference is attributable to health insurance and a small amount of unpaid debt (Garfinkel, Wheeless, and Corder, 1985).2
Table 7. Percent distribution of population, by percentage of family income accounted for by total charges and out-of-pocket expenditures for personal medical services and age: United States, 1980.
| Percentage of family income accounted for by personal medical services | Total charges | Out-of-pocket expenditures | ||
|---|---|---|---|---|
|
|
|
|||
| Under 65 years | 65 years or over | Under 65 years | 65 years or over | |
|
| ||||
| Percent distribution | ||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 |
| None | 19.0 | 10.2 | 28.4 | 14.7 |
| 1 percent | 49.2 | 20.6 | 56.4 | 34.4 |
| 2-5 percent | 19.6 | 31.3 | 12.1 | 34.6 |
| More than 5 percent | 11.8 | 37.6 | 2.8 | 16.0 |
NOTES: All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
Among persons under age 65, 19 percent had no charges, but 28 percent had no out-of-pocket expenditures. Thus, 9 percent of this group (28 percent less 19 percent) had their obligation for care completely paid by insurance or public programs or did not pay the bill. About one-half of the population under age 65 (49 percent) had total charges equal to 1 percent of family income, and about one-half (56 percent) also had out-of-pocket expenditures equal to 1 percent of income. However, the two groups are not necessarily composed of the same persons.
About 11.8 percent of the population under 65 years had total charges in excess of 5 percent of family income, compared with 2.8 percent of this population who incurred out-of-pocket expenditures constituting more than 5 percent of income. Thus, insurance coverage appears to have reduced the number of persons at risk for this high level of cost by about three-fourths.
A similar pattern was observed for persons 65 years or over. Although 37.6 percent of this age group incurred total charges in excess of 5 percent of family income, only 16 percent actually spent more than 5 percent of their income for health care. Thus, insurance coverage reduced by about one-half the proportion of the high-cost population age 65 or over actually incurring out-of-pocket expenditures at that high level.
Percent of total charges
The extent to which high-cost users of health care are at risk for high out-of-pocket expenditures is directly addressed in Table 8, in which we compare the percentage of the charges of the high-cost group that were paid out of pocket with the percentage for the other cost groups in both age groups. Among persons under 65 years, 25 percent of all incurred charges were paid out of pocket. High-cost users were personally responsible for only 16 percent of their charges, the lowest percentage of any cost group. Nevertheless, the per capita out-of-pocket payment by high-cost users, $581, was more than four times the per capita out-of-pocket payment for the population as a whole, $125.
Table 8. Total per capita charges for personal medical services and out-of-pocket per capita expenditures and percent of charges, by cost level and age: United States, 1980.
| Age and type of statistic | Total1 | Cost level | ||
|---|---|---|---|---|
|
| ||||
| High | Medium | Low | ||
| Under 65 years | ||||
| Total per capita charge | $491 | $3,598 | $512 | $97 |
| Out-of-pocket per capita: | ||||
| Expenditure | $125 | $581 | $218 | $60 |
| Percent of charge | 25 | 16 | 43 | 62 |
| 65 years or over | ||||
| Total per capita charge | $1,606 | $8,431 | $1,345 | $231 |
| Out-of-pocket per capita: | ||||
| Expenditure | $282 | $921 | $391 | $143 |
| Percent of charge | 18 | 11 | 29 | 62 |
Includes 19 percent of persons under 65 years and 10 percent of persons 65 years or over who had no charges for personal medical services.
NOTES: All medical services except dentistry and nursing home care are included. The population is the civilian noninstitutionalized population of the United States in 1980. Persons who had no charges are included in the denominator for determining the per capita charges and expenditures.
SOURCE: Health Care Financing Administration and National Center for Health Statistics: Data from the National Medical Care Utilization and Expenditure Survey.
The proportion of total incurred charges that were paid out of pocket by persons under age 65 increased substantially as the level of total charges decreased. Although high-cost users paid 16 percent of their charges out of pocket, low-cost individuals paid 62 percent. The same pattern was observed for persons 65 years or over. High-cost persons paid 11 percent of charges out of pocket, compared with 62 percent for low-cost individuals.3
The fact that high-cost persons were personally responsible for a smaller proportion of their total bill most likely reflects the maximum limit and deductible provisions of some medical insurance plans. The maximum limit (or catastrophic cap) provision lowers the proportion of total charges high-cost persons pay out of pocket by fixing out-of-pocket expenditures at a maximum amount, such as $500 or $1,000, although the total charge continues to increase. The deductible makes low-cost users personally responsible for a high proportion of small total charges. Furthermore, high-cost users are more likely to have used inpatient hospital services, for which insurance coverage tends to be more complete.
Discussion
High-cost users are a small part of the population who consume an extremely large share of medical care resources. We found that the pattern for high-cost users was similar for persons under age 65 and persons age 65 or over. However, high costs were a more significant problem for older persons as a group.
Persons 65 years or over were more likely than persons under 65 to be included in the high-cost category, reflecting the higher likelihood of intensive service use among older persons.
The dollar amounts incurred by persons age 65 or over were greater than those incurred by persons under age 65 throughout the distribution and were four times higher at the 90th percentile.
The percentages of persons 65 or over who exceeded $500 and $1,000 in out-of-pocket expenditures were three times greater than the percentages of younger persons, despite the facts that almost everyone 65 years or over was covered by Medicare and about three-fourths of them had a public or private supplement (Garfinkel, Bonito, and McLeroy, 1987).
The percentage of persons who spent more than 5 percent of their family income on medical care was almost six times greater for persons 65 years or over than for the younger age group.
The average per capita out-of-pocket expenditure, excluding insurance premiums, of persons 65 years or over was more than twice that of persons under age 65.
High-cost users age 65 or over clearly consume far more resources than high-cost users under age 65, and they devote more of their income to paying for care (exclusive of insurance premiums).
Out-of-pocket expenditures as a percentage of total charges were lowest for the high-cost group and highest for the low-cost group. This reflects the use of deductibles, coinsurance, and out-of-pocket maximums in most health insurance plans. High-cost users are far more likely to exceed their maximums (i.e., the out-of-pocket cap), at which point further out-of-pocket expenditures for covered services cease, although total charges continue to accrue. Conversely, some low-cost users will still be accruing charges against their deductible, in which case all expenditures for their care will be out of pocket.
High-cost use was more strongly associated with poor health status than with any other factor, as it should be. However, in both age groups, persons who were insured and persons with higher income were more likely to incur high costs than uninsured and lower income persons even after controlling for the effects of health. Thus, ability to pay appears to influence the use of intensive medical care. The availability of resources, hospital beds in particular, had no effect on high-cost use, even though almost everyone who incurred high costs had a hospital stay.
The pattern of high costs for persons age 65 or over suggests that they were unequally exposed to the financial burden of medical care in 1980. There is no absolute measure of what constitutes an excessive burden of medical care costs. However, the level of total incurred charges and out-of-pocket expenditures experienced by persons age 65 or over, both compared with younger persons and relative to their family income, suggests that gaps in insurance coverage existed in 1980 despite the widespread availability of Medicare and supplemental insurance.4
Future research
The usefulness of sample survey data for studying high-cost utilization is limited by the relative imprecision of estimates for small domains. The percentage of persons who incur extremely high costs is small. Nevertheless, survey data are valuable for this purpose because they include comprehensive information on expenditures, sources of payment, and personal covariates that is unavailable from secondary insurance claims and discharge files, the main alternative sources of data. In future research, attempts should be made to combine both types of data so that users with extremely high costs can be studied with precision.
Future efforts should also be designed to combine data on the noninstitutionalized population with data for persons in long-term care institutions. In combining data from several sources for the 1970's, Birnbaum (1978a, 1978b) clearly indicated the importance of including both populations and both types of costs in the definition of high-cost use. The National Medical Expenditure Survey, which is being conducted in 1987 and 1988, includes both kinds of information.
Health insurance premiums, which represent a prepayment for medical care in most cases, are a component of out-of-pocket expenditures that was not included in this article because the data were not available. Because the extent to which people are insured and the out-of-pocket expense for that coverage are important aspects of measuring the burden of expenditures and the value of insurance, these topics should be specifically addressed in future data collection efforts.
The effect of reduced inpatient admission rates and length of stay beginning in 1983 on the similarity of the distribution of charges observed in several studies prior to 1983 should be determined.
Finally, high-cost use affects people over time. In this study, we used cross-sectional data for 1 year to examine high-cost use. McCall and Wai (1983) observed considerable stability in total charges over time, which suggests that the percentage of persons incurring high costs in a single year may be an adequate estimate of the burden of high costs. Nevertheless, the number of persons who experience high costs over several years may be substantially greater than can be determined from the percentages reported on the basis of 1 year. Multiple-year studies would provide a more realistic estimate of the number of persons incurring high costs and the ways in which public policy might ease that burden.
Acknowledgments
The authors thank Tim Gabel for his extensive computer work and thank Lisa LaVange and Sara Wheeless for advice about statistical methods and the structure of the data set. We also wish to thank Deborah Freund, Marian Gornick, Judith Kasper, James Lubitz, John Paul, and Herbert Silverman for comments on earlier drafts. Any errors and opinions expressed in the paper are solely the responsibility of the authors.
Footnotes
Reprint requests: Steven A. Garfinkel, Research Triangle Institute, P.O. Box 12194, Research Triangle Park, North Carolina 27709.
The sampling weights were not used in the first-stage reduction of the initial model because they increased the cost of the analysis substantially. The weights were used in subsequent estimations so that the results would reflect the noninstitutionalized U.S. population. Multicollinearity was avoided by comparing correlation coefficients and using the stepwise procedure.
Insurance premiums paid by individuals, which are not included in these data, are also out-of-pocket costs, offsetting to some extent the difference between total charges and out-of-pocket expenditures.
All charges for nursing home services are excluded. Gibson and Waldo (1982) reported that, in 1980, out-of-pocket expenditures for nursing home services made up 43 percent of nursing home charges, and out-of-pocket expenditures for all personal health service charges, including nursing home charges but excluding dental charges, made up 30 percent.
Additional data on out-of-pocket expenditures for health insurance premiums, which were unavailable in NMCUES, might alter the comparison between the younger and older age groups, although it is not certain in which direction.
References
- Aday L, Andersen R, Fleming G. Health Care in the US: Equitable for Whom? Beverly Hills, Calif.: Sage Publications; 1980. [Google Scholar]
- Andersen R. Research Series. No. 25. Chicago: Center for Health Administration Studies, University of Chicago; 1968. A behavioral model of families' use of health services. [Google Scholar]
- Birnbaum H. The Cost of Catastrophic Illness. Lexington, Mass.: Lexington Books; 1978a. [Google Scholar]
- Birnbaum H. NCHSR Research Summary Series. National Center for Health Services Research; 1978b. A national profile of catastrophic illness. DHEW Pub. No. (PHS) 78-3201. [Google Scholar]
- Bonham GS. National Medical Care Utilization and Expenditure Survey. Washington: U.S. Government Printing Office; Mar. 1983. Procedures and questionnaires of the National Medical Care Utilization and Expenditure Survey. (A). Methodological Report No. 1. DHHS Pub. No. 83-20001. National Center for Health Statistics Public Health Service, and Health Care Financing Administration. [Google Scholar]
- Bureau of Professions, Health Services and Resources Administration. Data from the Area Resource File. Rockville, Md.: Feb. 1983. [Google Scholar]
- Congressional Budget, Office U.S. Congress. Catastrophic Medical Expenses: Patterns in the Non-Elderly, Non-Poor Population. Washington: Dec. 1982. [Google Scholar]
- Garfinkel SA, Bonito AJ, McLeroy KR. Health Care Financing Review. No. 1. Vol. 9. Washington: U.S. Government Printing Office; Fall. 1987. Socioeconomic factors and Medicare supplemental health insurance. HCFA Pub. No. 03240. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Garfinkel SA, Wheeless SC, Corder LS. Health Status and Utilization and Expenditures for Health Services of the Civilian, Noninstitutionalized population of the United States in 1980. Research Triangle Park, N.C.: Research Triangle Institute; Sept. 1985. Contract No 500-81-0047. Prepared for Health Care Financing Administration. [Google Scholar]
- Gibson RM, Waldo DR. Health Care Financing Review. No. 1. Vol. 4. Washington: U.S. Government Printing Office; Sept. 1982. National health expenditures, 1981. HCFA Pub. No. 03146. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Gornick M, Beebe J, Prihoda R. Health Care Financing Review. No. 1. Vol. 5. Washington: U.S. Government Printing Office; Fall. 1983. Options for change under Medicare: Impact of a cap on catastrophic illness expense. HCFA Pub. No. 03154. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Harrell FE., Jr . SUGI Supplemental Library User's Guide. 1983. Cary, N.C.: SAS Institute; 1983. The logist procedure. [Google Scholar]
- Health Care Financing Administration. Medicare Directory of Prevailing Charges, 1980. Baltimore, Md.: Jul, 1980. HCFA 1-008. Mimeographed document. [Google Scholar]
- McCall N, Wai HS. An analysis of the use of Medicare services by the continuously enrolled aged. Medical Care. 1983 Jun;21(6):567–585. doi: 10.1097/00005650-198306000-00001. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. The Economics of Medical Care. Reading, Mass.: Addison-Wesley Publishing Co.; 1978. [Google Scholar]
- Newhouse JP, Manning WG, Morris CN, et al. Some interim results from a controlled trial of cost sharing in health insurance. New England Journal of Medicine. 1981 Dec.305(25):1501–1507. doi: 10.1056/NEJM198112173052504. [DOI] [PubMed] [Google Scholar]
- Rice T. The impact of changing Medicare reimbursement rates on physician-induced demand. Medical Care. 1983 Aug.21(8):803–815. doi: 10.1097/00005650-198308000-00004. [DOI] [PubMed] [Google Scholar]
- Riley G, Lubitz J, Prihoda R, Stevenson MA. Health Care Financing Review. No. 3. Vol. 7. Washington: U.S. Government Printing Office; Spring. 1986. Changes in distribution of Medicare expenditures among aged enrollees, 1969-82. HCFA Pub. No. 03222. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Shah BV, Folsom RE, Harrell FE, Dillard CN. Survey Data Analysis Software for Logistic Regression. Research Triangle Park, N.C.: Research Triangle Institute; Nov. 1984. [Google Scholar]