Abstract
Medicaid coverage of children is analyzed in this article, using data from uniform Medicaid files (Tape-to-Tape) for California, Georgia, Michigan, and New York. Results show that Medicaid is a different program to children of different enrollment groups and ages. For children receiving cash assistance through either Aid to Families with Dependent Children or Supplemental Security Income, Medicaid represents a source of ongoing health coverage. However, for children in families not receiving cash assistance, coverage is more episodic and disproportionately related to acute care and hospitalization. Across all child enrollment groups, infants had higher than expected utilization and expenditures.
Introduction
About one-half of Medicaid recipients nationwide are children, making them the largest single coverage group. In fiscal year 1985, the Health Care Financing Administration (HCFA) reported that more than 10 million children were Medicaid recipients. However, relatively little research has focused on children in the Medicaid program, in part because they account for such a small part of Medicaid dollars. Medicaid expenditures for children in 1985 were about $5 billion, constituting only 13 percent of the overall budget. Child Medicaid expenditures, in real terms, have also declined over the last few years, unlike Medicaid expenditures for the aged and disabled (Rymer and Burwell, 1987).
Nevertheless, Medicaid coverage of children has emerged as a policy concern. While the number of children in poverty has increased, the number of children receiving Medicaid services has remained relatively static. In 1980, the ratio of child Medicaid recipients to children in poverty was 897 per 1,000, but coverage had eroded to 737 per 1,000 by 1983. Both Congress and the States have been concerned about this trend. Recent Federal Medicaid amendments mandated coverage for some groups of children and provided States with greater flexibility in their coverage of other optional groups of children. Many States have responded to this increased flexibility in Medicaid policy by significantly expanding their coverage of children.
Only limited data in aggregate form have been available for cross-State analysis of Medicaid children. Presented in this article is a summary of findings from a study in which person-based Medicaid data for a year were analyzed for each of four States to develop detailed enrollment, utilization, and expenditure information on Medicaid children. The analysis focused on various subsets of Medicaid children, using enrollment group, age group, and institutional status as key variables. Data were for California and Michigan (1983) and Georgia and New York (1982). These States accounted for about 36 percent of both Medicaid recipients and expenditures nationwide in 1985. Study results cover the Medicaid experience of close to 4 million children with expenditures of $1.7 billion during the study period.
Coverage of children by Medicaid
In addition to certain groups for which coverage is mandated, States have numerous options with regard to their Medicaid coverage of children. Medicaid encompasses three broad enrollment groups for children—children covered by Aid to Families with Dependent Children (AFDC), disabled children, and other children. Within each overall group, States can elect to cover numerous subgroups. For this study, nine subgroups were selected, as shown in Figure 1. These subgroups cover the most important State options for children. An overview of these subgroups follows.
Figure 1. Medicaid child enrollment groups.
AFDC children
AFDC children are by far the largest child Medicaid enrollment group. According to HCFA data, about 9.2 millon AFDC children were Medicaid recipients during 1985, accounting for 46 percent of Medicaid recipients nationwide. For study purposes, AFDC children were subdivided into four subgroups.
AFDC cash—regular
The majority of Medicaid children in each State qualify as a result of their receipt of cash assistance through the AFDC program. The AFDC cash assistance program is mandatory in every State. Generally, the regular AFDC cash program extends eligibility to children under age 17 (or 18 at State option) in single-parent families.
AFDC cash—unemployed parent
States have the option to extend AFDC cash assistance to two-parent families in which the principal wage earner is unemployed or underemployed. In 1984, 26 States provided AFDC—unemployed parent (AFDC-U) coverage under Medicaid. Three of the four study States extended AFDC-U coverage during the study period: California, Michigan, and New York.
AFDC cash—Title IV-E
States must also “deem” AFDC cash assistance for purposes of Medicaid to children covered by Title IV-E of the Social Security Act. Generally, Title IV-E children are foster care or adoptive children who would be eligible for AFDC cash assistance if they were still living with their natural parents. Foster care children are children who are the legal responsibility of the State child welfare agency. They may have been voluntarily placed by their parents under State responsibility, or the State may have removed the children from their homes. Most foster care children are placed with the State child welfare agency because there are problems with their parent(s)' (or caretaker's) conduct or condition. Foster care children include those suffering from neglect, exploitation, or abuse by their families, as well as children whose parents are physically or mentally unable to care for them.
AFDC noncash
This group includes children under age 19 who meet the categorical requirements but not the financial requirements of the AFDC program. It includes both those who are categorically needy but not receiving cash assistance and those who are medically needy. All States are required to include in their Medicaid coverage some groups of AFDC families that are not eligible for cash benefits. Mandatory noncash AFDC coverage for States includes families eligible for less than $10 a month in AFDC benefits (which are therefore denied cash), families that lose AFDC because of employment, and other smaller groups. States also have several optional groups for noncash AFDC coverage. The most significant optional coverage by AFDC involves extending benefits to families that do not meet the financial requirements of AFDC but are medically needy; that is, families that lack the resources to pay their medical bills but satisfy special income and resource limits set under the State Medicaid plan. Among the study States, only Georgia did not extend coverage to medically needy children for the study period. Medically needy and categorically needy noncash children were combined into one group for the study.
Disabled children
With the implementation of the Supplemental Security Income (SSI) program in 1974, a new group of beneficiaries was added to Medicaid—disabled (and blind) children in low-income families. Prior to SSI, disabled children generally qualified for Medicaid only if their families were eligible through the AFDC provisions. With SSI, children became eligible for assistance in their own right if they were substantially disabled and if their families satisfied certain financial requirements. Adult disability requirements are largely based on whether a person is capable of work. For children, disability assessment primarily focuses on the impact of a child's handicap on his or her normal daily activities. Generally, in setting the financial eligibility requirements for disabled children, the SSI program assumes that some of the parents' income is available to meet the needs of the child.
A survey sponsored by the Social Security Administration in 1979 produced the following profile of noninstitutionalized disabled SSI cash children:
“Approximately 85% of SSI disabled children lived at home with their families, while about 15% lived in foster care or other (non-institutional) protective settings. The average age was around 12 years. They were more likely to be male (58%). They had a greater proportion of minorities than the general or low-income population. The average household size was 5 persons (including the SSI child). In just over half the households (57%) the mother was the only parent present. The majority of children (53%) were reported by their caretakers to be multiply handicapped. The data on the main disabling conditions showed mental retardation to be the most frequently occurring main disability (27% of the cases). Fifteen percent indicated that “other diseases of the nervous system” were the main handicap. This grouping covers several conditions including epilepsy, brain disease, other paralysis, meningitis, muscular dystrophy and multiple sclerosis. Another 15% reported “other mental condition” to be the main handicap. Included in this classification are psychosis, schizophrenia, neurosis, personality disorders, alcoholism, drug problems, speech defects, hearing defects and hyperactivity. Congenital anomalies, such as spina bifida, Down's syndrome, and hydrocephalus, were reported as the main problems by 11 % of the cases” (Rymer et al., 1980).
With the routine Medicaid data reported to HCFA (Annual Form 2082), it is not possible to determine the number of disabled child recipients nationwide or expenditures for them. Data from the Social Security Administration indicate that children make up about 14 percent of the overall disabled (and blind) SSI cash assistance population. In December 1984, 345,764 children under age 22 were enrolled in the SSI program.
For purposes of the study, disabled children were divided into three subgroups:
Disabled cash (noninstitutionalized)
This group includes blind and disabled children under 21 years of age receiving cash assistance through the SSI program. Coverage of SSI disabled children by Medicaid is not mandatory. In 1984, seven States restricted SSI and Medicaid coverage for disabled children; however, all four study States provided full Medicaid coverage to disabled SSI cash children. Institutionalized children were not included in the disabled cash group.
Disabled noncash (noninstitutionalized)
This group of children, as with AFDC, includes both those who are categorically needy but not receiving cash assistance and those who are medically needy. Unlike AFDC coverage, most State coverage of noncash disabled children is optional. States have the option to include in their noncash disabled coverage the disabled who are eligible for but not receiving SSI. As with AFDC, States also have the option to extend their Medicaid coverage to include the disabled who are medically needy. The medically needy are disabled children whose families lack the resources to pay their medical bills but satisfy special income and resource limits set under the State Medicaid plan. Among the study States, only Georgia did not extend coverage to the medically needy. Institutionalized children were not included in the disabled noncash group.
Disabled institutionalized
Children who were institutionalized in a long-term care facility at some point during the study period are the third disabled group. The institutionalized were defined as a separate group because their Medicaid utilization and expenditure patterns are so different from those of the noninstitutionalized. States with medically needy programs automatically extend coverage to the disabled in institutions if their income is less than the cost of their medical care. In determining eligibility, parental income is not generally considered to be available for institutionalized children. Thus, disabled children who are institutionalized may come from families not considered to be low income. If a State does not have a medically needy program, it can elect either of two optional coverage groups for the institutionalized: the disabled who would be eligible for cash assistance except that they are in an institution and the institutionalized disabled who qualify under a special income eligibility level. Georgia did not have a medically needy program during the study period; however, it extended Medicaid eligibility to the disabled who would be eligible for cash assistance except for their institutional status.
Other children
In addition to AFDC and disabled children, States have the option of covering other groups of children under Medicaid. These children are not eligible for cash assistance. Adjusted HCFA data for 1985 indicate that about 741,000 “other” child recipients were covered under Medicaid, accounting for about 4 percent of Medicaid recipients nationwide (Rymer and Burwell, 1987). Other children covered under Medicaid mainly consist of two subgroups:
Ribicoff children
Generally, Ribicoff children are those in low-income two-parent families that do not meet the AFDC categorical requirements. Thus, by extending Medicaid to Ribicoff children, a State opens up Medicaid eligibility to all low-income children whose families satisfy the AFDC or medically needy financial requirements. The name Ribicoff is used because Senator Ribicoff was responsible for the Medicaid legislation establishing this optional coverage group. In 1986, 32 States extended Ribicoff coverage to all low-income children under age 18-21 years. (The exact age cutoff varies by State.) Beginning in 1984, all States were required to phase in Ribicoff coverage of children under age 5. Of the study States, California, Michigan, and New York had Ribicoff coverage for children under age 21; Georgia had no Ribicoff coverage for the study period.
Child welfare children
States have the option to extend Medicaid coverage to all foster care and adoptive children not covered under the Title IV-E provisions. These are foster care or adoptive children who were not eligible for AFDC cash assistance prior to placement with the State. All States include foster care and adoptive children in their optional Medicaid coverage. The child welfare group encompasses both foster care and adoptive children.
Financial eligibility criteria for children
Just as States vary in the groups of children they elect to include under Medicaid, they also vary in the financial criteria used to determine eligibility. In 1985, cash payment standards for a four-person AFDC family ranged from $144 monthly in Mississippi to $800 in Alaska. The four study States also showed a broad range in their AFDC financial criteria during the study period (Table 1).
Table 1. Monthly payment standards for Aid to Families with Dependent Children (AFDC) and Supplemental Security Income (SSI): California, Georgia, Michigan, and New York, 1982 and 1983.
| State | AFDC standard for 4-person family | SSI standard for disabled person living independently | ||
|---|---|---|---|---|
|
|
|
|||
| 1982 | 1983 | 1982 | 1983 | |
|
| ||||
| Monthly payment standard | ||||
| California | $601 | $625 | $439 | $451 |
| Georgia | 229 | 238 | 1265 | 1284 |
| Michigan | 492 | 492 | 289 | 318 |
| New York | 515 | 515 | 328 | 348 |
Federal SSI minimum payment level.
SOURCES: Social Security Administration, Office of Family Assistance: Characteristics of State Plans for AFDC. SSA Pub. No. 80-21235. Washington, D.C. 1983 and 1984; Social Security Administration, Office of Policy: Selected Characteristics of State Supplementation Programs as of January 1982. SSA Pub. No. 13-11975. Washington. U.S. Government Printing Office, Mar. 1983; State Medicaid officials: Personal communication, data for 1983.
The SSI program is Federal and has a nationwide minimum payment standard. As a result, less variation is seen among States in the financial criteria used for determining the eligibility of disabled cash children. However, States have the option of supplementing the SSI Federal minimum. In 1986, 28 States supplemented the basic SSI payment of $336 to individuals living independently. For the study period, California, Michigan, and New York supplemented the Federal minimum, but Georgia did not. The monthly SSI payment standards for the study States are shown in Table 1.
Federal regulations require that States set their medically needy income standards no higher than 133 percent of the AFDC level. In 1984, medically needy levels for a family of four varied from $205 in Tennessee to $801 in California. The income levels for medically needy coverage used by the relevant study States during the study period are shown in Table 2.
Table 2. Monthly medically needy income levels for Medicaid coverage: California, Michigan, and New York, 1982 and 1983.
| State | Medically needy level for 4-person family | |
|---|---|---|
|
| ||
| 1982 | 1983 | |
|
| ||
| Monthly income level | ||
| California | $801 | $834 |
| Michigan | 492 | 492 |
| New York | 458 | 525 |
SOURCE: State Medicaid officials: Personal communication, data for 1982 and 1983.
Thus, California had the most generous financial eligibility criteria, followed by New York and Michigan. As mentioned earlier, these three States also covered all of the key optional coverage groups for children. Georgia's financial requirements were considerably more restrictive, and Georgia also did not cover medically needy children or Ribicoff children during the study period. As a result, the Georgia program was generally much less comprehensive with regard to the coverage of low-income children under Medicaid than those of the other States.
Data and methods
The data for this study were developed from a multi-State Medicaid data base developed by the Office of Research and Demonstrations at HCFA. This data base, commonly referred to as Tape-to-Tape, contains person-level data collected through the Medicaid Management Information System (MMIS) in several States. For this study, Tape-to-Tape data for the States of California, Georgia, Michigan, and New York were used. The number of Medicaid children enrolled and the total Medicaid expenditures for children included in the study data are shown in Table 3.
Table 3. Medicaid child enrollees and expenditures for children: Georgia and New York, 1982; California and Michigan, 1983.
| State | Number of enrollees | Expenditures in thousands |
|---|---|---|
| Total | 3,751,850 | $1,752,341 |
| California | 1,664,538 | 720,751 |
| Georgia | 228,621 | 92,520 |
| Michigan | 665,303 | 269,940 |
| New York | 1,193,388 | 669,130 |
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
The Tape-to-Tape data base contains complete enrollment, service utilization, and expenditure data from each State's MMIS for all study children for the covered years. An important aspect of the Tape-to-Tape data base is that the Medicaid data for each State have been recoded into a uniform format, making comparisons across States possible for research projects. The Tape-to-Tape data base also allows the use of the person-year method of counting enrollment, a more precise method than most other Medicaid data sets allow. With the person-year method, the variation in enrollment time of individual enrollees is adjusted by counting all enrollees fractionally according to the portion of the study year for which they were actually enrolled. Thus, a person who was enrolled for 6 months contributed .5 person-year to the pool of enrollment experience. The person-year method is used throughout this article because it adjusts for differences in the rate of turnover across child enrollment groups. When utilization and expenditure rates are presented, they are computed on the basis of person-years of enrollment.
Three important limitations of the Tape-to-Tape data are relevant to this study. First, Tape-to-Tape data do not include screening visits and expenditures for the early and periodic screening, diagnosis, and treatment (EPSDT) program. Because the EPSDT program is the major source of preventive services for Medicaid children, this omission is significant. Only non-EPSDT preventive care utilization and expenditures were reported in study data. Thus, any comparison of study data with data on the general population of children should be made cautiously.
A second limitation of the data involves differences across study States in the reporting of utilization and expenditures for infants. In three States (California, Georgia, and Michigan), hospitals generally assign all charges for normal childbirth to the mother. However, in New York, hospitals routinely assign nursery-related charges to the newborn infant instead. Thus, infants in New York have birth-related expenditures, but infants in the other study States do not.
Another difference relates to how quickly following birth infants are assigned their own Medicaid identification numbers and thus are linked directly to health care service charges. In New York, infants are often assigned Medicaid identification numbers before birth (when the pregnant mother is a Medicaid recipient) so that charges can be made to the infant immediately following birth. In Georgia, infants are assigned Medicaid identification numbers very soon following birth. As a result, any services to a newborn infant after discharge from the hospital are assigned directly to the infant's Medicaid number. However, in California it can take 1-2 months for a Medicaid identification number to be assigned to a newborn infant. Thus, any utilization of Medicaid services immediately following birth is not entered on the infant's Medicaid file but the mother's file instead. Also, in Michigan during the study period, charges to infants could be made to the mother's Medicaid file. The effect of these inconsistencies is that study data on infant utilization and expenditures are understated for California and Michigan.
A third limitation is that New York does not include all Medicaid service claims in its MMIS. Of relevance to this study, a substantial portion of enrollment and expenditure data for disabled children receiving services in intermediate care facilities for the mentally retarded (ICF's/MR) is not included in the study data. It is estimated that only about one-third of expenditures for ICF/MR services for disabled children were included in New York's MMIS in 1982 and therefore are included in the study data. Beyond the $56 million in Medicaid expenditures for ICF/MR services to disabled children reported in the study data, an additional $104 million were spent on ICF/MR services to disabled children by New York during 1982. However, the study data on institutionalized children available for New York are believed to be representative with regard to overall utilization and expenditure patterns for this group of children.
Findings
Because of the differences in the optional enrollment groups elected by study States, the composition of their populations of Medicaid children during the study period was quite different, as shown in Table 4. California, Michigan, and New York included both the medically needy and Ribicoff children in their coverage groups, so their AFDC noncash and “other children” groups accounted for a larger proportion of child enrollment. However, in all study States, Medicaid child enrollment was dominated by the regular AFDC cash assistance group.
Table 4. Percent distribution of Medicaid child enrollees and expenditures, by enrollment group: Georgia and New York, 1982; California and Michigan, 1983.
| Enrollment group | California | Georgia1 | Michigan | New York | California | Georgia1 | Michigan | New York |
|---|---|---|---|---|---|---|---|---|
| Percent distribution of enrollees | Percent distribution of expenditures | |||||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| AFDC | 83 | 94 | 83 | 85 | 58 | 64 | 59 | 63 |
| AFDC cash | 67 | 92 | 77 | 74 | 46 | 63 | 56 | 55 |
| AFDC cash—regular | 51 | 91 | — | 69 | 34 | 62 | — | 51 |
| AFDC cash—unemployed parent | 15 | — | — | 4 | 10 | — | — | 2 |
| AFDC cash—Title IV-E | 1 | 0.7 | — | 1 | 1 | 1 | — | 2 |
| AFDC noncash | 16 | 2 | 6 | 11 | 12 | 1 | 4 | 8 |
| Disabled | 2 | 5 | 1 | 4 | 21 | 35 | 14 | 24 |
| Disabled cash (noninstitutionalized) | 2 | 5 | 1 | 3 | 8 | 18 | 4 | 7 |
| Disabled noncash (noninstitutionalized) | (2) | — | (2) | 0.5 | 1 | 0.2 | 0.2 | 3 |
| Disabled institutionalized | (2) | 0.3 | 0.1 | 30.3 | 12 | 17 | 10 | 314 |
| Other | 15 | 1 | 15 | 12 | 21 | 2 | 27 | 13 |
| Ribicoff | 13 | — | — | 9 | 18 | — | — | 7 |
| Child welfare | 2 | 1 | — | 3 | 3 | 2 | — | 6 |
| Percent | ||||||||
| Children as a percent of Medicaid total | 48 | 45 | 55 | 51 | 21 | 15 | 20 | 16 |
ln 1982, Georgia did not have a medically needy program, nor did it extend Medicaid coverage to the AFDC—unemployed parent or Ribicoff groups. Because Georgia had only 41 children in the disabled noncash noninstitutionalized group, data on this group are not presented in subsequent tables.
Less than 0.1 percent.
Study data for disabled children receiving intermediate care facility for the mentally retarded services in New York are incomplete. Thus, the percent of overall child enrollment and expenditures attributable to disabled instutionalized children is understated.
NOTES: AFDC is Aid to Families with Dependent Children. AFDC-U is AFDC—unemployed parent. The Michigan reporting system does not distinguish among AFDC groups. Instead, all AFDC cash assistance children are reported as AFDC cash—regular. Similarly, child welfare enrollees are not distinguishable from Ribicoff enrollees in the Michigan data.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
The distribution of expenditures for the different groups of Medicaid children during the study period are also shown in Table 4. The expenditure patterns look very different from the enrollment patterns. Several coverage groups accounted for a much greater proportion of expenditures than enrollment. In particular, the disabled children groups were responsible for 14-35 percent of Medicaid expenditures for children among the study States, even though they constituted no more than 5 percent of any State's Medicaid enrollment of children.
AFDC cash children
As shown in Table 4, AFDC cash children made up the vast majority of child Medicaid enrollees in each State. They constituted 92 percent of child enrollment in Georgia. However, in California, Michigan, and New York, which also extended Medicaid to many optional noncash children's groups, they constituted only 67-77 percent of child enrollment.
Table 5 is a summary of study data for AFDC cash assistance children across the study States. Study data on utilization and expenditures are presented by three summary classes of service: inpatient hospital care (including acute hospitals but excluding psychiatric and chronic care hospitals); long-term care (including psychiatric hospitals, chronic hospitals, skilled nursing facilities, and intermediate care facilities); and physician/ambulatory care. Physician/ambulatory care includes all service visits attributed to physicians, other medical providers (optometrists, chiropractors, etc.), hospital outpatient departments/emergency rooms, and clinics. This category includes physician visits to hospitalized children. A fourth grouping, “other,” is included in the expenditure data. It covers all services not included in the other three categories, including laboratory and X-ray services, home health care, prescription drugs, dental care, ambulances, and durable medical equipment.
Table 5. Selected data for Medicaid child enrollees in Aid to Families with Dependent Children (AFDC) cash group: Georgia and New York, 1982; California and Michigan, 1983.
| Item | AFDC cash | |||
|---|---|---|---|---|
|
| ||||
| California | Georgia | Michigan | New York | |
| Mean length of enrollment in months for study year | 9.4 | 9.7 | 9.7 | 9.4 |
| Percent male enrollees | 51 | 50 | 51 | 52 |
| Age: | ||||
| Under 1 year | 12 | 11 | 10 | 10 |
| 1-4 years | 30 | 28 | 27 | 25 |
| 5-9 years | 26 | 26 | 27 | 26 |
| 10-14 years | 21 | 22 | 24 | 24 |
| 15-18 years | 11 | 12 | 12 | 16 |
| Percent using any Medicaid service | 83 | 76 | 86 | 88 |
| Percent using inpatient hospital services | 4 | 8 | 6 | 9 |
| Hospital days per user | 7 | 6 | 7 | 8 |
| Percent using physician/ambulatory care | 66 | 64 | 76 | 83 |
| Physician ambulatory care visits per user | 6 | 5 | 6 | 8 |
| Percent using dental services | 31 | 31 | 34 | 32 |
| Dental visits per user | — | 2 | 2 | 2 |
| Percent using prescription drugs | 59 | 51 | 61 | 57 |
| Prescriptions per user | 5 | 5 | 5 | 5 |
| Percent using long-term care | (1) | 0 | (1) | (1) |
| Annual expenditure per enrollee: | ||||
| All services | $373 | $345 | $362 | 2$533 |
| Inpatient hospital | 173 | 169 | 152 | 236 |
| Physician/ambulatory | 91 | 59 | 74 | 202 |
| Long-term care | 1 | 0 | 17 | 10 |
| Other | 108 | 117 | 119 | 74 |
| Per diem rate | — | — | — | 211 |
Less than 1 percent.
New York officials have estimated that $33.1 million were spent during fiscal year 1982 on per diem coverage for Title IV-E and child welfare children, an average of $1,034 per person-year of enrollment. These per diem expenditures have been factored into the total expenditure per enrollee.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
Many areas of similarity for AFDC cash children are revealed. Across all States, AFDC cash children were enrolled in Medicaid for an average of more than 9 months during the study year. They were evenly distributed by sex, and more than one-third were under 5 years of age. Thus, AFDC cash children were much younger than the general population of children.
At least three-fourths of AFDC child enrollees in each State were Medicaid recipients, i.e., they used at least one Medicaid service during the year. About two-thirds of AFDC cash children used at least one physician/ambulatory service during the year, with an average of 5-8 visits per user across the study States. The States were not as consistent with regard to hospitalization rates. California had the lowest hospital user rate, 4 percent of AFDC child enrollees, compared with a high of 9 percent for New York AFDC child enrollees. The average number of days per hospital user ranged from 6 to 8 days across States. About one-third of AFDC cash children received dental services during the year. Slightly more than one-half of AFDC cash children received at least one prescription drug during the year. There was only negligible use of long-term care (less than 1 percent of enrollees) by the AFDC cash group among study States.
Annual expenditures per AFDC cash enrollee ranged from $345 to $373 for three study States but were $533 for New York. From 42 percent to 49 percent of expenditures were for inpatient hospital services.
Two subgroups of AFDC cash children were analyzed as well. The first, AFDC—unemployed parent children, were analyzed in two States, California and New York. AFDC-U children comprised 15 percent of overall child Medicaid enrollment in California but only 4 percent in New York (Table 4). Between the two States, there were no consistent patterns of difference between AFDC-U children and regular AFDC cash children, with one exception. AFDC-U children were found to be somewhat younger than regular AFDC cash children. Close to one-half of AFDC-U children were under age 5, compared with about one-third of AFDC cash children.
A second subgroup of AFDC cash children, Title IV-E children, comprised up to 1 percent of overall child Medicaid enrollment among the three States for which data were available. Title IV-E children are foster care children who would be eligible for AFDC cash assistance if they were still living with their natural parents. Title IV-E children were found to have several differences from regular AFDC cash children. As shown in Table 6, Title IV-E children were much older than children in the regular AFDC cash program. More than one-half of Title IV-E children were 10 years of age or over. Although the proportion of Title IV-E children who were inpatient hospital users during the year was not consistently greater than the proportion of other AFDC cash children in all three States, Title IV-E children had about 50 percent more hospital days per user than regular AFDC cash children. Title IV-E children in California and Georgia were as likely or more likely to have used physician/ambulatory services than AFDC cash children during the year, and they averaged considerably more visits per user. They also had a much higher dental service user rate for the two States in which these data were available. Not surprisingly, then, per-enrollee expenditures for Title IV-E children were considerably greater than expenditures for AFDC cash children. Annual per-enrollee expenditures for Title IV-E children were $538 in Georgia, $693 in California, and $1,682 in New York.
Table 6. Selected data for Medicaid child enrollees in Aid to Families with Dependent Children (AFDC) cash—Title IV-E group: Georgia and New York, 1982; California, 1983.
| Item | AFDC cash—Title IV-E | ||
|---|---|---|---|
|
| |||
| California | Georgia | New York | |
| Mean length of enrollment in months for study year | 9.5 | 10.5 | 8.5 |
| Percent male enrollees | 53 | 53 | 55 |
| Age: | |||
| Under 1 year | 5 | 4 | 7 |
| 1-4 years | 22 | 19 | 16 |
| 5-9 years | 22 | 23 | 18 |
| 10-14 years | 27 | 34 | 30 |
| 15-18 years | 24 | 20 | 30 |
| Percent using any Medicaid service | 86 | 89 | — |
| Percent using inpatient hospital services | 6 | 9 | 8 |
| Hospital days per user | 10 | 9 | 12 |
| Percent using physician/ambulatory care | 66 | 70 | 170 |
| Physician/ambulatory care visits per user | 10 | 7 | 111 |
| Percent using dental services | 42 | 51 | 130 |
| Dental vists per user | — | 2 | 13 |
| Percent using prescription drugs | 54 | 50 | 138 |
| Prescriptions per user | 4 | 5 | 15 |
| Percent using long-term care | (2) | 0 | (2) |
| Annual expenditure per enrollee: | |||
| All services | $693 | $538 | 3$1,682 |
| Inpatient hospital | 331 | 232 | 308 |
| Physician/ambulatory | 157 | 96 | 228 |
| Long-term care | 26 | 1 | 40 |
| Other | 179 | 209 | 72 |
| Per diem rate | — | — | 31,034 |
Routine medical care for many Title IV-E and child welfare children in New York is covered under a per diem rate paid to the voluntary child care agencies responsible for their supervision. This per diem does not cover inpatient hospital care or referred ambulatory care. These utilization data are only for services that were outside the Medicaid per diem and were a direct claim on the Medicaid Management Information System.
Less than 1 percent.
New York officials have estimated that $33.1 million were spent during fiscal year 1982 on per diem coverage for Title IV-E and child welfare children, an average of $1,034 per person-year of enrollment. These per diem expenditures have been factored into the total expenditure per enrollee.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
AFDC noncash children
A decision to extend medically needy coverage has a significant impact on the size of a State's AFDC noncash group. AFDC noncash children in Georgia, which did not have a medically needy program, made up only 2 percent of the State's total population of child Medicaid enrollees, compared with 6 percent in Michigan, 11 percent in New York, and 16 percent in California (Table 4).
In Table 7, study results for AFDC noncash children are presented. For the three States with medically needy coverage, AFDC noncash children were different from AFDC cash children in several respects. They averaged about 6 months of enrollment for the study year, significantly less than the 9-month average for cash children. Noncash children were as likely or more likely than AFDC cash children to have been hospital users in each study State, and they stayed longer once hospitalized. The greater number of hospital days per user ranged from 4 to 6 days among the States. As a result, annual expenditures per enrollee for AFDC noncash children ranged from an average of $475 to $807 across the three States, 31 percent to 72 percent greater than the expenditures for AFDC cash children.
Table 7. Selected data for Medicaid child enrollees in Aid to Families with Dependent Children (AFDC) noncash group: Georgia and New York, 1982; California and Michigan, 1983.
| Item | AFDC noncash | |||
|---|---|---|---|---|
|
| ||||
| California | Georgia | Michigan | New York | |
| Mean length of enrollment in months for study year | 6.3 | 5.6 | 6.2 | 6.0 |
| Percent male enrollees | 51 | 51 | 51 | 50 |
| Age: | ||||
| Under 1 year | 14 | 10 | 14 | 17 |
| 1-4 years | 21 | 26 | 23 | 19 |
| 5-9 years | 22 | 26 | 24 | 20 |
| 10-14 years | 22 | 25 | 23 | 22 |
| 15-18 years | 21 | 13 | 16 | 22 |
| Percent using any Medicaid service | 70 | 70 | 77 | 71 |
| Percent using inpatient hospital services | 5 | 5 | 6 | 13 |
| Hospital days per user | 12 | 7 | 11 | 14 |
| Percent using physician/ambulatory care | 53 | 55 | 66 | 60 |
| Physician/ambulatory care visits per user | 7 | 5 | 7 | 8 |
| Percent using dental services | 28 | 30 | 28 | 24 |
| Dental visits per user | — | 3 | 3 | 3 |
| Percent using prescription drugs | 42 | 44 | 50 | 37 |
| Prescriptions per user | 4 | 6 | 5 | 5 |
| Percent using long-term care | (1) | 0 | (1) | (1) |
| Annual expenditure per enrollee: | ||||
| All services | $642 | $316 | $475 | $807 |
| Inpatient hospital | 413 | 144 | 251 | 560 |
| Physician/ambulatory | 97 | 53 | 76 | 153 |
| Long-term care | 3 | 0 | 19 | 29 |
| Other | 129 | 119 | 129 | 65 |
Less than 1 percent.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
However, study results suggest that the utilization and expenditure patterns of noncash children may not be so different from those of AFDC cash children unless a State has a medically needy program. In Georgia, the one study State without medically needy coverage, AFDC noncash children were very similar to the cash group in both utilization and expenditure averages per enrollee. Analysis of additional States without medically needy coverage would be needed to determine if this pattern persisted.
Disabled cash children (noninstitutionalized)
Disabled cash children (who were not institutionalized) comprised from 1 percent to 5 percent of child Medicaid enrollment across the study States (Table 4). This group accounted for the vast majority of disabled child enrollees, with relatively few disabled children falling into the noncash group or institutionalized group.
Disabled cash children (noninstitutionalized) were very different from AFDC children, as shown in Table 8. Disabled cash children generally averaged about 10 months of enrollment for the study year. There were more males than females (57-59 percent male across the study States). The majority of children were older, with more than two-thirds of the children in each State being 10 years of age or over. As with AFDC children, there was significant variation among the States in hospital utilization. The hospital user rate ranged from 12 percent to 21 percent, with 13-20 days of care per user for the year. The physician/ambulatory care user rate was close to 75 percent for all four States; however, the average number of visits per user ranged from 8 to 17 for the study year. Dental care user rates were reported to be 26-36 percent, similar to rates for the AFDC groups. Prescription drug user rates ranged from 49 percent to 67 percent, with an average of 9 to 14 prescriptions per user annually.
Table 8. Selected data for Medicaid child enrollees in disabled cash and disabled noncash (noninstitutionalized) group: Georgia and New York, 1982; California and Michigan, 1983.
| Item | California | Georgia1 | Michigan | New York | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| Disabled cash | Disabled noncash | Disabled cash | Disabled cash | Disabled noncash | Disabled cash | Disabled noncash | |
| Mean length of enrollment in months for study year | 10.7 | 7.6 | 10.8 | 10.3 | 8.2 | 9.4 | 5.6 |
| Percent male enrollees | 57 | 57 | 57 | 57 | 59 | 59 | 58 |
| Age: | |||||||
| Under 1 year | (2) | 5 | 2 | (2) | 3 | 3 | 13 |
| 1-4 years | 10 | 12 | 11 | 9 | 7 | 9 | 8 |
| 5-9 years | 18 | 18 | 19 | 16 | 9 | 17 | 8 |
| 10-14 years | 22 | 16 | 23 | 19 | 5 | 26 | 16 |
| 15-18 years | 26 | 24 | 27 | 27 | 25 | 27 | 30 |
| 19-20 years | 24 | 25 | 19 | 29 | 51 | 18 | 25 |
| Percent using any Medicaid service | 89 | 76 | 85 | 86 | 90 | 81 | 72 |
| Percent using inpatient hospital services | 14 | 23 | 21 | 12 | 18 | 15 | 31 |
| Hospital days per user | 13 | 70 | 13 | 14 | 31 | 20 | 93 |
| Percent using physician/ambulatory care | 74 | 62 | 73 | 77 | 77 | 75 | 49 |
| Physician/ambulatory care visits per user | 13 | 31 | 10 | 8 | 16 | 17 | 32 |
| Percent using dental services | 36 | 22 | 27 | 32 | 26 | 26 | 14 |
| Dental visits per user | — | — | 2 | 2 | 2 | 2 | 3 |
| Percent using prescription drugs | 65 | 47 | 67 | 66 | 70 | 49 | 28 |
| Prescriptions per user | 10 | 10 | 12 | 14 | 17 | 9 | 11 |
| Percent using long-term care | — | — | — | — | — | — | — |
| Annual expenditure per enrollee: | |||||||
| All services | $2,314 | $13,362 | $1,694 | $1,347 | $4,120 | $1,956 | $9,715 |
| Inpatient hospital | 1,190 | 11,399 | 1,085 | 786 | 3,120 | 1,050 | 8,969 |
| Physician/ambulatory | 285 | 791 | 129 | 99 | 188 | 603 | 460 |
| Long-term care | — | — | — | — | — | — | — |
| Other | 839 | 1,172 | 480 | 462 | 812 | 303 | 286 |
Because Georgia had only 41 children in the disabled noncash—noninstitutionalized group in 1982, data for this group are not presented.
Less than 1 percent.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
The annual Medicaid expenditure per disabled cash child ranged from $1,347 to $2,314. It should be remembered in reviewing these expenditures that disabled children, unlike many adults in the Medicaid disabled population, are not eligible for Medicare.
Disabled noncash children (noninstitutionalized)
Disabled noncash children comprised less than 1 percent of overall Medicaid enrollment of children among the three States with medically needy coverage (Table 4). Compared with disabled cash children, disabled noncash children had considerably shorter lengths of enrollment (Table 8). Disabled noncash children were enrolled for 6 to 8 months of the study year, compared with the 10-month average for disabled cash children. Disabled noncash children were much more likely to be hospitalized, with a hospital user rate of 18-31 percent. The number of days per hospital user ranged from 31 to 93 days, 2-5 times the rate for disabled cash children. The physician/ambulatory care user rate ranged from 49 percent to 77 percent across States, with the number of visits per user ranging from 16 to 32. The annual cost per enrollee was 3-6 times greater than for disabled cash children, with annual expenditures per enrollee ranging from $4,120 to $13,362 across the study States.
Disabled institutionalized children
Disabled institutionalized children made up considerably less than 1 percent of overall child Medicaid enrollment in each study State (Table 4). They comprised 6-11 percent of the overall group of disabled children. As shown in Table 9, most institutionalized children were enrolled for the entire year. Like disabled cash and noncash children, almost 60 percent of the institutionalized group was male. More than one-half of the disabled institutionalized children in each State were 15 years of age or over. The average number of long-term care days per institutionalized child ranged from 245 to 335. Thus, children in this group were institutionalized for most of the year. A majority of the institutional care days (55-81 percent) were in ICF/MR facilities (data not shown in this table). About 17 percent of the institutionalized disabled children were hospitalized during the year, with the number of days per hospital user varying from 14 to 37. Different physician/ambulatory care user rates for institutionalized children were seen among the States, but this comparison is complicated because some States “bundle” physicians' and other services into their institutional care package.
Table 9. Selected data for Medicaid child enrollees in disabled institutionalized group: Georgia and New York, 1982; California and Michigan, 1983.
| Item | Institutionalized disabled children | |||
|---|---|---|---|---|
|
| ||||
| California | Georgia | Michigan | New York | |
| Mean length of enrollment in months for study year | 11.4 | 11.7 | 11.8 | 8.5 |
| Percent male enrollees | 58 | 61 | 58 | 58 |
| Age: | ||||
| Under 1 year | 1 | 1 | (1) | 1 |
| 1-4 years | 5 | 3 | 3 | 7 |
| 5-9 years | 10 | 11 | 10 | 10 |
| 10-14 years | 20 | 27 | 21 | 21 |
| 15-18 years | 35 | 36 | 35 | 36 |
| 19-20 years | 29 | 22 | 31 | 25 |
| Percent using any Medicaid service | 100 | 100 | 100 | 100 |
| Percent using inpatient hospital services | 16 | 17 | 16 | 17 |
| Hospital days per user | 19 | 14 | 15 | 37 |
| Percent using physician/ambulatory care | 65 | 39 | 76 | 53 |
| Physician/ambulatory care visits per user | 25 | 7 | 17 | 20 |
| Percent using dental services | 30 | 5 | 27 | 14 |
| Dental visits per user | — | 1 | 2 | 2 |
| Percent using prescription drugs | 54 | 27 | 64 | 23 |
| Prescriptions per user | 23 | 26 | 28 | 13 |
| Percent using long-term care | 100 | 100 | 100 | 100 |
| Long-term care days per user | 302 | 335 | 300 | 245 |
| Annual expenditure per enrollee: | ||||
| All services | $27,882 | $25,053 | $29,967 | $36,388 |
| Inpatient hospital | 1,758 | 686 | 896 | 2,047 |
| Physician/ambulatory | 458 | 55 | 212 | 593 |
| Long-term care | 24,761 | 24,068 | 28,205 | 33,406 |
| Other | 905 | 244 | 654 | 342 |
Less than 1 percent.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
Annual expenditures per enrollee for institutionalized children ranged from $25,053 to $36,388. Long-term care costs accounted for 89-96 percent of these expenditures. Although disabled institutionalized children comprised considerably less than 1 percent of child enrollment in each State, they accounted for 10-17 percent of overall Medicaid expenditures for children, according to study data. If New York data for ICF/MR expenditures had been complete, its disabled institutionalized group would have been shown to account for 26 percent of overall child expenditures.
Ribicoff children
Three study States provided full Ribicoff coverage during the study period (all but Georgia). In California and New York, Ribicoff children comprised 9-13 percent of child Medicaid enrollment (Table 4). The Michigan MMIS system did not separately identify Ribicoff children. However, because Ribicoff children were estimated to constitute the vast majority of its “other” group, this group was used for comparisons with Ribicoff children in California and New York. Michigan's other group comprised 15 percent of overall enrollment.
Generally, because of their greater utilization and expenditures, Ribicoff children were more like AFDC noncash children than AFDC cash children. As shown in Table 10, their average length of enrollment for the study year was 6-8 months. From 11 percent to 12 percent of Ribicoff children were hospitalized during the study year, with an average of 9-12 days per hospital user. From 58 percent to 73 percent of Ribicoff children were users of physician/ambulatory services, with an average of 7-10 visits per user. Total annual expenditures per enrollee ranged from $716 to $1,237. These expenditure levels were greater than the levels for AFDC cash children in the study States. The main difference between Ribicoff children and both groups of AFDC children is that Ribicoff children had an older age distribution. More than one-third of Ribicoff enrollees in each State were 15 years of age or over, and in one State, 65 percent of Ribicoff children were age 15 or over.
Table 10. Selected data for Medicaid child enrollees in Ribicoff group: New York, 1982; California and Michigan, 1983.
| Item | Ribicoff children | ||
|---|---|---|---|
|
| |||
| California | Michigan1 | New York | |
| Mean length of enrollment in months for study year | 5.8 | 8.0 | 6.9 |
| Percent male enrollees | 48 | 51 | 50 |
| Age: | |||
| Under 1 year | 18 | 7 | 12 |
| 1-4 years | 22 | 10 | 19 |
| 5-9 years | 14 | 8 | 16 |
| 10-14 years | 10 | 9 | 14 |
| 15-18 years | 14 | 26 | 19 |
| 19-20 years | 22 | 39 | 19 |
| Percent using any Medicaid service | 73 | 83 | 81 |
| Percent using inpatient hospital services | 11 | 12 | 12 |
| Hospital days per user | 12 | 9 | 11 |
| Percent using physician/ambulatory care | 58 | 73 | 73 |
| Physician/ambulatory care visits per user | 10 | 7 | 10 |
| Percent using dental services | 26 | 33 | 28 |
| Dental visits per user | — | 3 | 3 |
| Percent using prescription drugs | 46 | 60 | 50 |
| Prescriptions per user | 5 | 7 | 6 |
| Percent using long-term care | (2) | 2 | (2) |
| Annual expenditure per enrollee: | |||
| All services | $1,237 | $1,078 | $716 |
| Inpatient hospital | 821 | 410 | 377 |
| Physician/ambulatory | 175 | 99 | 205 |
| Long-term care | 29 | 341 | 30 |
| Other | 212 | 228 | 104 |
Michigan data include both Ribicoff and child welfare children; however, Michigan officials estimated that the vast majority of the children reported in this group qualified under the Ribicoff provisions. Thus, the combined Michigan data are used for comparison with data on Ribicoff children in California and New York.
Less than 1 percent.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
Child welfare children
Generally speaking, child welfare children are foster care or adoptive children who were not eligible for AFDC cash assistance prior to placement with the State. Thus, they come from two-parent families or families with higher income or resources than the families of foster care children who qualify under the Title IV-E AFDC cash provisions. Data were available for this group in only three of the study States.
Child welfare children comprised 1-3 percent of all child Medicaid enrollees among the study States (Table 4). As shown in Table 11, child welfare children in New York were almost identical to Title IV-E children in terms of expenditures per enrollee. This is not surprising because New York used a capitated per diem approach to covering many Medicaid services for both Title IV-E and child welfare children. However, in the other two States (California and Georgia), the child welfare group had much higher utilization and expenditures per enrollee than Title IV-E children had. The expenditures per enrollee were 45 percent greater for child welfare children in both States. Child welfare children in Georgia had greater inpatient hospital utilization than Title IV-E children had. In California, the hospital user rates for the two groups were almost identical, but child welfare children showed greater use of physician/ambulatory care and long-term care services.
Table 11. Selected data for Medicaid child enrollees in child welfare group: Georgia and New York, 1982; California, 1983.
| Item | Child welfare children | ||
|---|---|---|---|
|
| |||
| California | Georgia | New York | |
| Mean length of enrollment in months for study year | 7.8 | 8.7 | 9.3 |
| Percent male enrollees | 55 | 51 | 56 |
| Age: | |||
| Under 1 year | 6 | 11 | 5 |
| 1-4 years | 12 | 24 | 15 |
| 5-9 years | 16 | 21 | 17 |
| 10-14 years | 28 | 25 | 27 |
| 15-18 years | 37 | 18 | 30 |
| 19-20 years | 1 | — | 5 |
| Percent using any Medicaid service | 82 | 88 | — |
| Percent using inpatient hospital services | 6 | 11 | 8 |
| Hospital days per user | 11 | 12 | 11 |
| Percent using physician/ambulatory care | 67 | 71 | 135 |
| Physician/ambulatory care visits per user | 14 | 8 | 16 |
| Percent using dental services | 39 | 48 | 13 |
| Dental visits per user | — | 2 | 12 |
| Percent using prescription drugs | 50 | 55 | 12 |
| Prescriptions per user | 5 | 6 | 14 |
| Percent long-term care users | 1 | 0 | 1 |
| Annual expenditure per enrollee: | |||
| All services | $1,005 | $780 | 2$1,642 |
| Inpatient hospital | 338 | 428 | 345 |
| Physician/ambulatory | 272 | 108 | 110 |
| Long-term care | 59 | 0 | 142 |
| Other | 336 | 244 | 11 |
| Per diem rate | — | — | 21,034 |
Routine medical care for many Title IV-E and child welfare children in New York is covered under a per diem rate paid to the voluntary child care agencies responsible for their supervision. This per diem does not cover inpatient hospital care or referred ambulatory care. These utilization data are only for services that were outside the Medicaid per diem and were a direct claim on the Medicaid Management Information System.
New York officials have estimated that $33.1 million were spent during fiscal year 1982 on per diem coverage for Title IV-E and child welfare children, an average of $1,034 per person-year of enrollment. These per diem expenditures have been factored into the total expenditure per enrollee.
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
Analysis by age group
In most previous research on Medicaid children, differences in enrollment, utilization, and cost have not been analyzed by the age of children. However, it is well documented that differences in health care utilization occur by age for the general population of children (Thompson, Bornstein, and Connelly, 1980). Study data were compiled using the following age groupings: under 1 year, 1-4 years, 5-9 years, 10-14 years, 15-18 years, and 19-20 years. The detailed enrollment groups were collapsed into three overall enrollment groups—AFDC children, disabled children, and other children—for the age-related analyses.
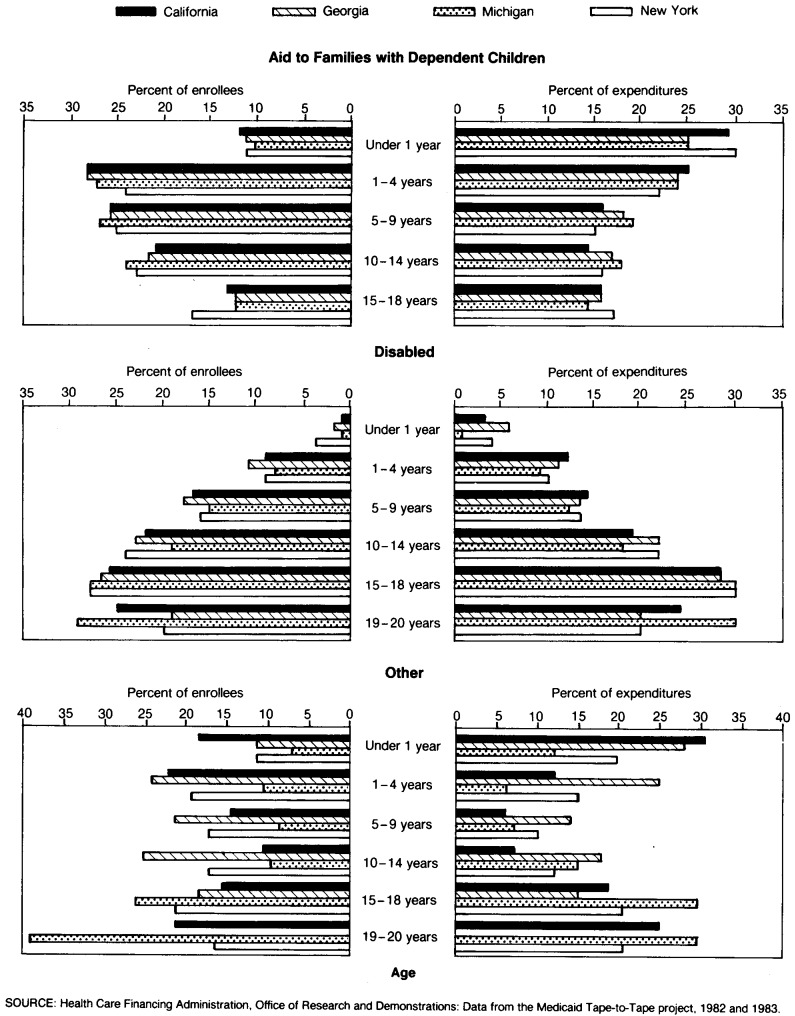
As shown on the left side of Figure 2, AFDC child enrollees across States were skewed to the very young, whereas the majority of disabled children were older. The age distribution of the other children group was not consistent across the study States, except that States with Ribicoff coverage had a higher proportion of older teenage children than is found in the general population of children.
Figure 2. Distribution of Medicaid child enrollees and expenditures, by age and enrollment group: Georgia and New York, 1982; California and Michigan, 1983.
Utilization data for AFDC children by age group are presented in Table 12. For AFDC children, the highest physician/ambulatory care user rates were for infants. From 72 percent to 91 percent of AFDC infants across the study States had at least one ambulatory visit during the study year, and the average number of visits per infant user ranged from 9 in Georgia to 13 in New York. AFDC children in the age group 1-4 years were also very likely to have received physician/ambulatory services during the year, but the number of visits per user was considerably less, ranging from 5 to 8 across States. The user rates for children in the older age groups were lower than those of younger children in all States.
Table 12. Selected utilization data for Medicaid child enrollees in Aid to Families with Dependent Children group, by age: Georgia and New York, 1982; California and Michigan, 1983.
| Utilization measure | Total | Under 1 year | 1-4 years | 5-9 years | 10-14 years | 15-18 years |
|---|---|---|---|---|---|---|
| Percent using physician/ambulatory care | ||||||
| California | 64 | 72 | 70 | 62 | 58 | 60 |
| Georgia | 64 | 83 | 72 | 58 | 57 | 61 |
| Michigan | 76 | 91 | 84 | 73 | 68 | 70 |
| New York | 81 | 84 | 87 | 80 | 77 | 77 |
| Number of physician/ambulatory care visits per user | ||||||
| California | 6 | 12 | 7 | 5 | 5 | 6 |
| Georgia | 5 | 9 | 5 | 4 | 4 | 5 |
| Michigan | 6 | 12 | 6 | 4 | 4 | 5 |
| New York | 8 | 13 | 8 | 7 | 7 | 7 |
| Percent using inpatient hospital services | ||||||
| California | 4 | 12 | 4 | 2 | 3 | 7 |
| Georgia | 8 | 21 | 8 | 5 | 5 | 11 |
| Michigan | 6 | 17 | 8 | 4 | 3 | 7 |
| New York | 9 | 46 | 8 | 4 | 4 | 11 |
| Number of hospital days per user | ||||||
| California | 7 | 12 | 6 | 5 | 6 | 6 |
| Georgia | 7 | 12 | 5 | 5 | 5 | 5 |
| Michigan | 7 | 13 | 5 | 5 | 5 | 6 |
| New York | 9 | 13 | 7 | 6 | 7 | 7 |
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
There was a somewhat U-shaped pattern to AFDC hospitalization by age group, with the likelihood of hospitalization being greater for the very young and older teenage children. Infants who were hospitalized averaged 12-13 days of care; for all other age groups, the average number of days per user averaged 5-7 days.
Utilization data for disabled children, shown in Table 13, include both hospital and long-term care services. Long-term care utilization data, rather than physician/ambulatory utilization, are shown for the disabled because a significant portion of expenditures for disabled children were for this service area. For disabled children, hospital utilization generally declined with age, with infants showing the highest user rates. Although not shown here, physician/ambulatory care use followed the same pattern. However, the utilization rate for long-term care showed an opposite pattern. Generally, the likelihood of using long-term care services increased with age for disabled children.
Table 13. Selected utilization data for Medicaid child enrollees in disabled group, by age: Georgia and New York, 1982; California and Michigan, 1983.
| Utilization measure | Total | Under 1 year | 1-4 years | 5-9 years | 10-14 years | 15-18 years | 19-20 years |
|---|---|---|---|---|---|---|---|
| Percent using inpatient hospital services | |||||||
| California | 14 | 46 | 30 | 17 | 12 | 10 | 12 |
| Georgia | 20 | 45 | 38 | 23 | 18 | 15 | 17 |
| Michigan | 13 | 51 | 31 | 19 | 12 | 8 | 9 |
| New York | 16 | 34 | 28 | 18 | 13 | 14 | 16 |
| Number of hospital days per user | |||||||
| California | 16 | 58 | 17 | 12 | 13 | 16 | 17 |
| Georgia | 13 | 41 | 13 | 9 | 11 | 13 | 15 |
| Michigan | 14 | 27 | 20 | 11 | 10 | 14 | 16 |
| New York | 30 | 83 | 27 | 23 | 28 | 30 | 36 |
| Percent using long-term care | |||||||
| California | 10 | 17 | 6 | 6 | 9 | 14 | 12 |
| Georgia | 6 | 3 | 1 | 4 | 7 | 8 | 7 |
| Michigan | 11 | 3 | 5 | 7 | 11 | 14 | 11 |
| New York | 9 | 4 | 8 | 6 | 7 | 11 | 11 |
| Number of long-term care days per user | |||||||
| California | 302 | 294 | 287 | 307 | 317 | 312 | 282 |
| Georgia | 335 | 352 | 315 | 305 | 331 | 343 | 347 |
| Michigan | 300 | 278 | 325 | 292 | 317 | 299 | 291 |
| New York | 245 | 270 | 303 | 277 | 247 | 239 | 218 |
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
As with the AFDC and disabled groups, infants in the other child group generally had the highest utilization rates for both physician/ambulatory and hospital services, as shown in Table 14. From 63 percent to 87 percent of infants received physician/ambulatory services during the year, with an average of 12-17 visits per user. From 22 percent to 39 percent of infants in the other child group had at least one hospitalization for the study year, with an average of 14-22 days per user.
Table 14. Selected utilization data for Medicaid child enrollees in other groups1, by age: Georgia and New York, 1982; California and Michigan, 1983.
| Utilization measure | Total | Under 1 year | 1-4 years | 5-9 years | 10-14 years | 15-18 years | 19-20 years |
|---|---|---|---|---|---|---|---|
| Percent using physician/ambulatory care | |||||||
| California | 60 | 63 | 63 | 55 | 56 | 61 | 61 |
| Georgia | 71 | 76 | 79 | 69 | 64 | 69 | — |
| Michigan | 73 | 87 | 83 | 72 | 71 | 73 | 70 |
| New York | 62 | 73 | 71 | 63 | 54 | 55 | 67 |
| Number of physician/ambulatory care visits per person | |||||||
| California | 11 | 17 | 10 | 8 | 9 | 12 | 11 |
| Georgia | 10 | 12 | 7 | 8 | 13 | 13 | 12 |
| Michigan | 7 | 15 | 7 | 5 | 6 | 7 | 7 |
| New York | 10 | 14 | 10 | 8 | 7 | 9 | 12 |
| Percent using inpatient hospital services | |||||||
| California | 10 | 22 | 5 | 3 | 3 | 12 | 19 |
| Georgia | 11 | 35 | 11 | 10 | 7 | 9 | — |
| Michigan | 12 | 24 | 10 | 4 | 4 | 13 | 14 |
| New York | 11 | 39 | 7 | 4 | 4 | 11 | 17 |
| Number of hospital days per user | |||||||
| California | 11 | 16 | 9 | 9 | 11 | 9 | 10 |
| Georgia | 12 | 22 | 9 | 3 | 15 | 7 | — |
| Michigan | 9 | 19 | 9 | 8 | 7 | 7 | 7 |
| New York | 11 | 14 | 9 | 10 | 11 | 10 | 11 |
Ribicoff children and child welfare children (all foster care and adoptive children not covered under the Title IV-E provisions).
NOTE: Data were calculated using person-years.
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the Medicaid Tape-to-Tape project, 1982 and 1983.
Like AFDC children, other children had a somewhat U-shaped pattern for hospitalization by age group, with the likelihood of hospitalization greater for the very young and the older teenage children. Physician/ambulatory utilization did not show a consistent pattern across States by age group.
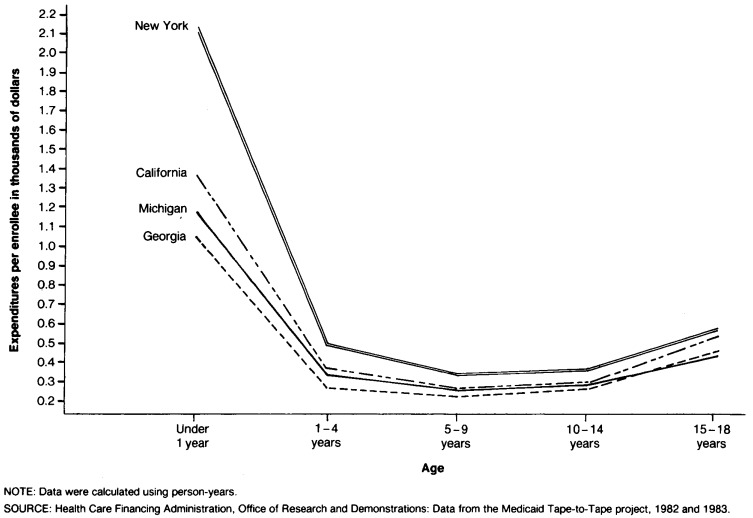
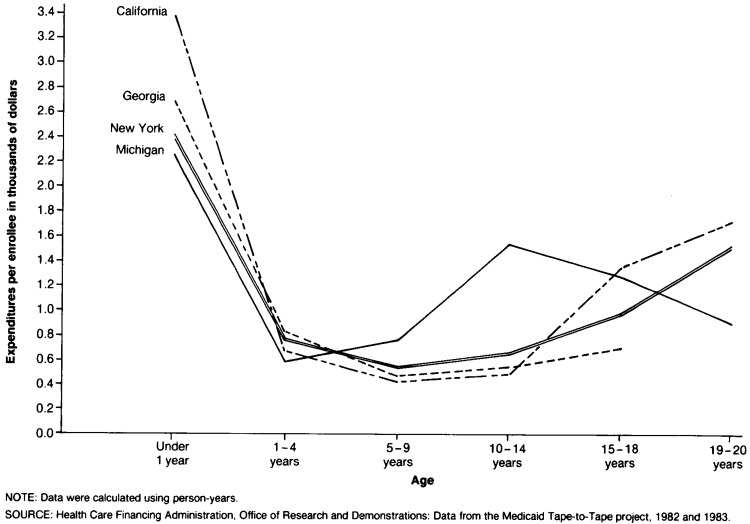
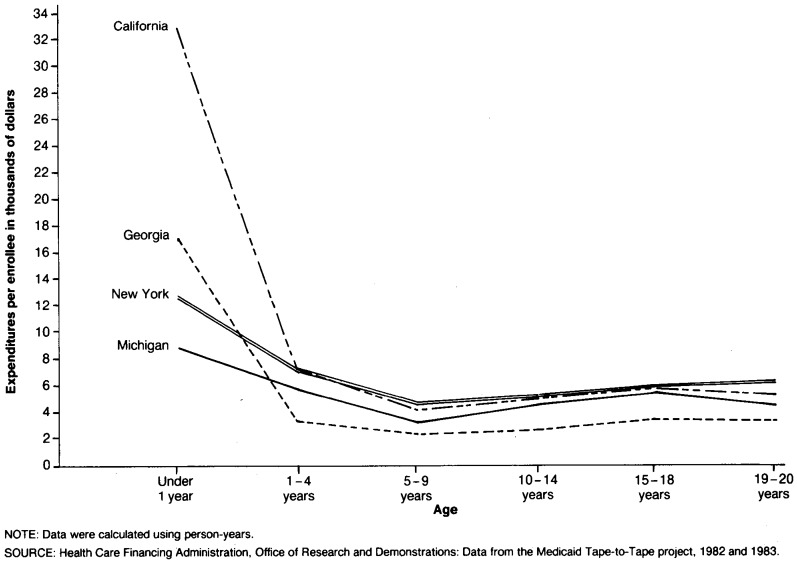
Given these utilization patterns, it is not surprising to find that Medicaid children had very different expenditure patterns by age. Certainly the most dramatic result is that infants had by far the highest per capita expenditures. Expenditure patterns by age across each of the three major enrollment groups of children are shown in Figures 3-5.
Figure 3. Average annual Medicaid expenditure per child enrolled in Aid to Families with Dependent Children group, by age: Georgia and New York, 1982; California and Michigan, 1983.
Figure 5. Average annual Medicaid expenditure per child enrolled in “other” group, by age: Georgia and New York, 1982; California and Michigan, 1983.
Annual Medicaid expenditures per AFDC infant ranged from $1,040 in Georgia to $2,133 in New York. AFDC children in the age group 5-9 years were the least expensive, ranging from $228 in Georgia to $339 in New York. Expenditures rose again for older AFDC children. For example, annual expenditures per enrollee for AFDC children aged 15-18 years were $437 in Michigan, $455 in Georgia, $510 in California, and $579 in New York.
As expected, the expenditures for disabled infants were substantial. The average annual expenditure for disabled infants ranged from $8,442 in Michigan to $32,165 in California. Like AFDC children, disabled children in the age group 5-9 years were the least expensive, with expenditures ranging from $2,235 annually in Georgia to $4,428 in New York. Expenditures for disabled children in the older age groups rose in a pattern similar to that seen for AFDC children. However, the main reason expenses increased for older disabled children was their higher utilization of long-term care services, not hospital and physician/ambulatory care services.
Infants also had the highest average expenditures in the other Medicaid children group across all study States, ranging from $2,250 in Michigan to $3,348 in California. Although the pattern was not entirely consistent by State, expenditures for other children were generally lowest for children in the groups 1-4 years and 5-9 years. Expenditures rose for older children. The unusually high expenditure average shown for the age groups 10-14 years and 15-18 years among other children in Michigan resulted because 3-4 percent of children in these age groups were institutionalized during the year, compared with user rates for long-term care of 1 percent or less for children in all the other age groups.
Among AFDC children, infants accounted for 25-30 percent of Medicaid expenditures across States, even though they constituted only 10-12 percent of enrollment (Figure 2). Across all study States, about one-half of AFDC child Medicaid dollars were spent on children under age 5.
A very different pattern is seen with disabled children. Most disabled children were older, and 48-60 percent of Medicaid expenditures for disabled children went to groups aged 15 and over. Although disabled infants were very expensive, on average, they did not comprise a large proportion of disabled child enrollees across the study States.
Infants in the other children group also accounted for a disproportionate share of expenditures. However, in the States with Ribicoff coverage, most Medicaid dollars for other children went to the older age groups. In Michigan, 60 percent of expenditures were for children age 15 and over; in New York and California, 42-44 percent of expenditures were for this age group. In Georgia, where the other children program was limited to child welfare children, the expenditure pattern looked more like that for the AFDC program. About 28 percent of expenditures were for infants, and 53 percent of expenditures were for children under age 5.
Conclusions
In spite of the diversity in State Medicaid programs and the differences in health care practice regionally, study results showed several consistent patterns in Medicaid use and expenditures for children. Generally, expenditures per enrollee were lowest for AFDC cash children. As expected, disabled children were considerably more expensive, with the disabled institutionalized being the most expensive children's group relative to enrollment size.
Children covered by Title IV-E and child welfare were found to have considerably higher utilization and expenditures, on average, than regular AFDC cash children. The finding is not unexpected because many of these children come from situations of abuse, neglect, or exploitation. An additional factor may be that they are more likely to use medical services as a result of supervision from their foster parents. It appears that, in the two States with detailed data, child welfare children had greater utilization and expense than Title IV-E children had. It is not obvious why such a difference occurred, but further investigation is warranted. It may be that many Title IV-E children were previously eligible for Medicaid under the regular AFDC program and thus had ongoing access to health care services. Child welfare children—especially those from two-parent low-income families—may be less likely to have had prior health coverage.
Ribicoff and AFDC noncash children (in the States with medically needy coverage) also had greater utilization and expenditures than AFDC cash children had, especially for inpatient hospital services. State officials confirmed that many poor families not receiving AFDC cash benefits apply for Medicaid only when a family member becomes seriously ill. Often, hospitals encourage Medicaid application for a noncash poor family when it is clear that, otherwise, the hospital services will have to be written off as uncompensated care. An information problem is also reported: Many low-income families are not aware that they (or their children, for the Ribicoff group) could be eligible for Medicaid without receiving AFDC. Many providers, especially physicians, are also poorly informed about Medicaid's eligibility criteria for noncash poor families. A final factor is that, because of the financial criteria used to determine eligibility (especially the medically needy criteria), families are unlikely to satisfy the requirements without a major medical expense, e.g., a hospitalization or extensive use of ambulatory care by a family member.
In any event, the AFDC noncash and Ribicoff groups do not cover many poor children with routine medical needs. Instead, this coverage seems to be focused on children with acute service needs. It does not seem reasonable to conclude that low-income children not receiving AFDC cash, on average, have a significantly different health status from that of AFDC cash children. Instead, the higher utilization and expenditures are likely to be triggered by the tendency to enroll children after, or concurrent with, illness.
A related finding is that children in the AFDC noncash and Ribicoff groups have shorter average lengths of enrollment during the study year than AFDC cash children have. After the acute service need is met by Medicaid, it seems likely that many of these children return to a situation of poor health care coverage or none at all.
These results provide some guidance to States in estimating the cost of extending coverage to some of these optional groups. States should expect that children enrolled in optional groups will have higher short-term service needs than AFDC cash children. However, these groups are not very large. AFDC cash children still make up the vast majority of enrollees in States that cover all the optional child groups. Also, as noted earlier, children in the AFDC noncash and Ribicoff groups are enrolled for a much shorter period of time. Previous researchers have noted a tendency by States to overestimate the number of children who would potentially be eligible in these optional groups (Fox, 1986). Although the low participation rates and shorter lengths of enrollment have been favorable for States with regard to the pressure on Medicaid budgets, concern continues about the number of low-income children who are reported to be without any health care coverage. States that want to improve their coverage of low-income children with more routine preventive health care should consider aggressive public education campaigns about Medicaid eligibility requirements. The provider community, in particular, should be targeted for education efforts.
The 1986 Omnibus Budget Reconciliation Act (OBRA) offers States, for the first time, the option of extending Medicaid eligibility to all children, regardless of family structure, up to the Federal poverty level. This could reduce many barriers to participation. However, this coverage is phased in, with 1-year increments. Initially, only infants are eligible, and coverage will eventually extend only to children through age 5. Nevertheless, how States will respond to the opportunity to expand coverage for children will be of interest. This new option could be instrumental in allowing State Medicaid programs to reach many low-income children with routine service needs.
Another conclusion from the study results is that the age of children being covered has an important effect on utilization and expenditures. Across all child enrollment groups in each study State, infants had disproportionately high expenditures. This pattern occurred even though study data in some States significantly understate infant utilization and expenditures.
One would expect infants to have higher health care utilization than other children and therefore to account for a disproportionately high portion of Medicaid expenditures. For example, the hospital discharge rate for children under age 1 (excluding newborns) in the general population is much higher than that for other children (McCarthy and Kozak, 1985). Because infants with low birth weight and other health problems are disproportionately found in the low-income population, this higher utilization is not unexpected.
These results suggest that the legislation in recent years, which has been phasing in Medicaid coverage for younger Ribicoff children, will probably extend coverage to the most expensive children first. A similar pattern may occur with the 1986 OBRA legislation, mentioned earlier, which allows States the option to begin phasing in infants whose family income is up to the poverty level.
Study data did not include information on the Medicaid experience of the infants' mothers. However, many of the mothers may not have had adequate prenatal care. Such a finding would support the conclusions of the Southern Regional Task Force on Infant Mortality (1985) that it would be cost effective for the Medicaid program to provide greater coverage to low-income pregnant women.
Some other age-related results should also be noted. Most AFDC expenditures are for younger children. Across all study States, about one-half of AFDC Medicaid dollars were spent on children under age 5, whereas this group accounted for one-third or more of AFDC enrollment. A different pattern is seen with disabled children. Most disabled children were older, and from 48 percent to 60 percent of expenditures for disabled children were for those aged 15 or over. Some analysts have suggested that it is difficult for younger disabled children to satisfy disability requirements. Only when children enter school and move into adulthood do functional disabilities become manifestly evident.
The age-related patterns for the other children's group are more puzzling. In the three study States with Ribicoff coverage, most Medicaid expenditures for the other children's group were for older children. In one State, 65 percent of Ribicoff enrollees were 15 years of age or over, and 60 percent of Ribicoff expenditures were for these children. In the other two States, slightly more than one-third of Ribicoff enrollment and 38-42 percent of Ribicoff expenditures were in this age group. Clearly, the Ribicoff program is reaching a much older age group than the AFDC program is. Other study data, not shown here, suggest that many teenagers are receiving pregnancy-related services through the Ribicoff group. Apparently, pregnant teenagers are enrolled in Medicaid as Ribicoff children if they are in families that do not meet AFDC categorical requirements (e.g., two-parent families). Also, verification of pregnancy is not required for a child under age 21 to qualify under the Ribicoff provisions. These age-related results lend support to the hypothesis that Ribicoff coverage is not reaching younger low-income children in two-parent poor families whose needs are more routine. Instead, the coverage is focusing more on teenagers with acute health care problems.
Another age-related result of interest is that many younger children did not use any services at all during the year. For example, in the age group 1-4 years, 13-30 percent of AFDC children and 17-38 percent of other children across the study States did not receive any physician/ambulatory services during the study period. Every child under age 5 should have at least one ambulatory medical encounter annually for preventive services, and children up to age 2 years should be seen at more frequent intervals (American Academy of Pediatrics, 1981). Dental user rates were similarly low: Only about one-third of AFDC and other children received any dental services during the year. Because the study data did not include EPSDT screening services, it is not possible to know if some of these younger children were completely unserved during the year. Nevertheless, this study result deserves further investigation.
A final age-related pattern is that of increased institutionalization for disabled children as they age. As disabled children grow older, they may be placed in institutional settings because they are too difficult for their families to manage. Institutionalization may also be the only way these children can qualify for Medicaid because of SSI rules regarding parental income. Given the high expenditures associated with institutionalized children and the fact that many of these children may be institutionalized permanently, the availability of Medicaid community-based long-term care services for disabled children should be carefully reviewed.
This study represents an important step in increasing the understanding of how the Medicaid program serves low-income children. Study results confirm that Medicaid is a different program to children in different enrollment groups and ages. For children who receive cash assistance through either AFDC or SSI, Medicaid represents a source of ongoing health coverage. However, for children whose families are not receiving cash assistance, coverage is more episodic and disproportionately related to acute care and hospitalization. Although many noncash low-income children with acute health care needs are served by Medicaid, the program does not appear to be serving noncash low-income children who require routine ongoing health care services.
Figure 4. Average annual Medicaid expenditure per child enrolled in disabled group, by age: Georgia and New York, 1982; California and Michigan, 1983.
Acknowledgments
The authors would like to thank Linda Graver of SysteMetrics/McGraw-Hill, Inc., who prepared the data files for this analysis. She managed the large data sets with great efficiency and much-appreciated equanimity. The study State liaisons for the Tape-to-Tape project include John Keith (California), Albert Skellie (Georgia), Keith Pier (Michigan), and Thomas Fanning (New York). These individuals coordinated review of the study results for their States and were the source of many insights and helpful comments. The Tape-to-Tape project officers are David Baugh and Penelope Pine of HCFA's Office of Research and Demonstrations. They have managed the development of the Tape-to-Tape data base over several years now, and were enthusiastic from the beginning about using Tape-to-Tape to support research on children. Sara Rosenbaum of the Children's Defense Fund was extremely helpful as an outside reviewer of the study results. We also appreciate the review comments of Kathleen Adams, Brian Burwell, and Embry Howell of SysteMetrics/McGraw-Hill, Inc. Finally, we thank Kipp Gabriel of SysteMetrics/McGraw-Hill, Inc. for her assistance in preparing this article for publication. The authors retain sole responsiblity for any errors or omissions.
This project was supported by Contract No. 500-84-0037 from the Health Care Financing Administration.
Footnotes
Reprint requests: Marilyn Rymer, SysteMetrics/McGraw-Hill Inc., 24 Hartwell Avenue, Lexington, Massachusetts 01890.
References
- American Academy of Pediatrics. Guidelines for Health Supervision of Children and Youth. Elk Grove Village, Ill.: Committee on Practice and Ambulatory Medicine; 1981. [Google Scholar]
- Fox H. Memorandum to Directors of Maternal and Child Health Service and Crippled Children's Services. Washington, D.C.: Feb. 1985. The Medically Needy Option for Expanding Medicaid Eligibility. [Google Scholar]
- McCarthy E, Kozak LJ. Advance Data from Vital and Health Statistics. No. 109. National Center for Health Statistics, Public Health Service; Hyattsville, Md.: May 23, 1985. Hospital use by children: United States, 1983. DHHS Pub. No. (PHS) 85-1250. [DOI] [PubMed] [Google Scholar]
- Rymer M, Burwell B. Medicaid Program Evaluation. Lexington, Mass.: SysteMetrics/McGraw-Hill, Inc.; 1987. Medicaid Eligibility: Analysis of Trends and Special Population Groups. Working Paper 5.6. [Google Scholar]
- Rymer M, Reither M, Goldman R, VandeVanter M. Survey of Blind and Disabled Children Receiving SSI Benefits. Social Security Administration; Washington: 1980. SSA Pub. No. 13-11728. [Google Scholar]
- Southern Regional Task Force on Infant Mortality. Final Report: For the Children of Tomorrow. Nov. 1985. [PubMed] [Google Scholar]
- Thompson HC, Bornstein S, Connelly JP. Demographic and Socioeconomic Fact Book on Child Health Care: A Survey of Trends in the United States. American Academy of Pediatrics; 1980. [Google Scholar]