Abstract
Health care spending has grown almost twice as fast as has the gross national product since 1965. Various parties in the health care financing arena have been affected to different degrees by this rising health care spending. As discussed in this article, households, businesses, and government all have had to devote increasing shares of their resources to financing health care. Although businesses have been increasingly burdened, either directly or through higher insurance premiums and Medicare taxes, that burden is less than is popularly believed.
Introduction
Since 1965, health care spending has grown almost twice as has fast as has the gross national product (GNP)—a broad-based measure of society's ability to pay for that care. Although the sheer size of the GNP could continue to support health expenditures well into the future (even considering the current differential rates of growth), it is important to understand that various parties in the health care financing arena have been affected to different degrees by the rising bite of health care spending. The purposes of this article are to disaggregate health care financing among four major payers—business, households (individuals), Federal Government, and State and local governments; to show how these shares have changed over time; and to examine the burden of health care spending, comparing health expenditures for each payer with related financial measures of income and expenditure.
This type of analysis is spawned by headlines of skyrocketing business health care costs. In these headlines, increases in business health care premiums of 20-30 percent are cited for 1988 and 1989 (Donahue, 1988; Hamilton, 1989; Kramon, 1988). In fact, however, there is little solid information on a national aggregate basis on the cost to business of health care. Often, the data quoted reflect the experience of individual or selected groups of firms and are not typical of the Nation as a whole. Aggregate data from the Bureau of Labor Statistics' Employer Cost Index for the year ending September 1988 indicate increases in employer health insurance premiums (excluding those paid on behalf of retirees) well below the range of 20 to 30 percent often cited in the media; on the other hand, those premiums are shown to be growing substantially faster than wages and salaries are (Bureau of Labor Statistics, 1988).
Even if the media reports cannot be generalized to the economy as a whole, however, they indicate a recurrent concern with the cost of care, particularly among small businesses (Dennis, 1985; Garland and Gleckman, 1989; ICF Incorporated, 1987; Lewin/ICF, 1988). The rising proportion of retirees and proposed changes in accounting practices that could require business to account currently for future retiree health care benefits will further increase the concerns of business (Dopkeen, 1987; Loomis, 1988; Rappaport and Kalman, 1987). In that sense, a measure of the cost of health to businesses is definitely useful.
To construct such a measure requires a new disaggregation of the existing estimates of national health expenditures. The current accounting framework (Letsch, Levit, and Waldo, 1988) was designed to track government-sponsored programs and other financing mechanisms over time. To the extent that business or households pay dedicated funds into government programs, the current framework overstates the role of government; to the extent that employers share in the cost of employees' health insurance premiums, the current framework does not delineate the role of business employers in paying for health care.
We divided payers of health care into four classes (businesses, households (individuals), Federal Government, and State and local governments) in recognition of the general homogeneity of function and motivation within the various parties. Businesses, for example, pay for health care for their workers to attract and keep that work force. Households seek to minimize the risk imposed by the cost of health care through either work-place benefits or individual private insurance. Governments act to redistribute risk from one generation to another (through Medicare), from one income class to another (through Medicaid and State and local general assistance and hospital subsidies), or from one risk class to another (through, for example, maternal and child health programs).
Although we speak of four types of payers, one should keep in mind that individuals ultimately finance all health care, regardless of which sector nominally pays for care (Musgrave and Musgrave, 1973; Pauly, 1988). Although employer-sponsored health care is paid primarily by the business sector, the ultimate burden is transferred to individuals. In the long run, business pays for health care by raising prices to consumers, paying lower real wages and salaries to employees than would otherwise be the case, or decreasing dividends to owners. Government programs are financed through income taxes, payroll taxes, or debt (which, in turn, is paid through taxes).
As is always the case when aggregate statistics are used, this analysis must be viewed with an eye to certain limitations. First, the quality of estimates of individual components varies.
In some cases, concrete figures are not available and estimates are developed using the best available information. For example, estimates of the employer share of private health insurance are prepared by the U.S. Department of Commerce, using total premium information from the national health accounts and employer share ratios from the U.S. Chamber of Commerce Employee Benefits Survey (Chamber of Commerce of the United States, 1986). The survey of employers is weighted toward medium and large firms, those employers more likely to finance health care benefits. Therefore, we expect the employer share derived from these data to be higher than the share that would be calculated if we had more accurate data. Despite these limitations, the Chamber of Commerce survey remains one of the best surveys available for estimating the employer share of premiums.
In other cases, estimates from two separate sources are combined, although they may not be strictly comparable. For example, there is some inherent incompatibility between the employer share of private health insurance (PHI) and PHI premiums. Commerce Department estimates of employer share, prepared by the Bureau of Economic Analysis (BEA), are based on the national health accounts estimate of total private health insurance premiums. However, BEA's revision policy permits only 2 prior years of revisions when new annual estimates are introduced, with more extensive revisions incorporated every 5-10 years. The latest national health account revisions to PHI have not been incorporated into the BEA estimates, leading to incomparability between the employer share of PHI (produced by BEA) and total PHI premiums (recorded in the national health accounts). Both these series are used in the payer classification estimates presented in this article.
Finally, the basic national health expenditure data for as far back as 1960 are themselves undergoing a comprehensive reestimation, which may alter some of the patterns presented in this article. We expect to introduce these revisions during calendar year 1989. Preliminary indications are that PHI will be revised upward, with accompanying downward revisions in out-of-pocket spending. These changes will affect the level of business and individual health care spending.
A second caveat related to this framework deals with creating a classification structure for a specific policy-relevant purpose. No one classification system is dictated by economic theory. For example, we could have done away with the government payers entirely by allocating expenditures from general revenue back to taxpaying businesses and households (Musgrave and Musgrave, 1973). However, we feel that the taxonomy we have used is the most useful taxonomy for gaining a clearer understanding of health care financing. For example, the pressures created by government budget deficits would not be seen in a model in which the government sector was not explicitly shown. In each of the sectors we show, health care costs have risen as a proportion of income or receipts, causing a reallocation of spending within that sector. If the reallocation is severe enough, pressure for redistribution among sectors is likely to occur (Kowalczyk, Freeland, and Levit, 1988).
In the work described here, we examined a subset of national health expenditures, those for health services and supplies (HSS). This subtotal, which excludes research and construction, comprises spending for the delivery of health care goods and services and the attendant costs of administering that delivery. The consequence of using HSS rather than total national health expenditures is that the aggregate ratios of health spending to GNP are lower than those to which the reader may have become accustomed.
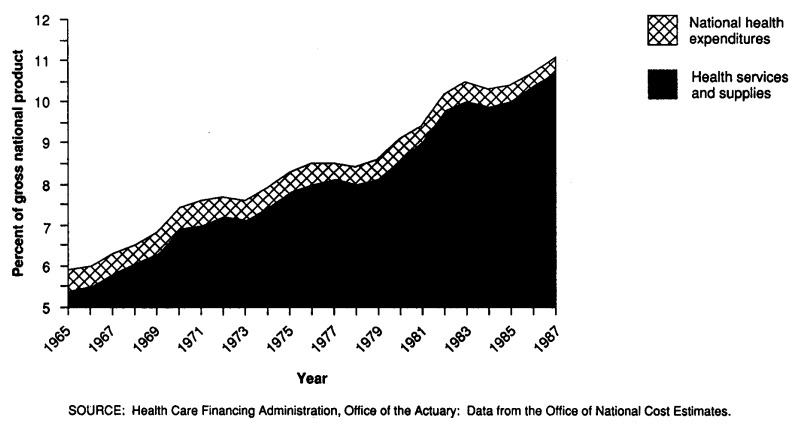
With few exceptions, the annual growth of HSS has been faster than that of the GNP, so that HSS as a percent of the GNP almost doubled from 1965 to 1987 (Table 1 and Figure 1). The exceptions to this rule are notable in themselves. The Economic Stabilization Period of 1973-74 and the effective implementation of Medicare's prospective payment system (PPS) in 1984 affected the growth of health care spending, and the general economic recoveries of 1978 and 1984 created surges in the GNP, the denominator of the ratio.
Table 1. National health expenditures, national expenditures for health services and supplies, and percent of gross national product: United States, calendar years 1965-87.
| Year | National health expenditures | Health services and supplies | ||
|---|---|---|---|---|
|
|
|
|||
| Amount in millions | Percent of gross National product | Amount in millions | Percent of gross national product | |
| 1965 | $41,929 | 5.9 | $38,417 | 5.4 |
| 1966 | 46,267 | 6.0 | 42,579 | 5.5 |
| 1967 | 51,456 | 6.3 | 47,622 | 5.8 |
| 1968 | 58,219 | 6.5 | 54,093 | 6.1 |
| 1969 | 65,633 | 6.8 | 60,795 | 6.3 |
| 1970 | 74,995 | 7.4 | 69,595 | 6.9 |
| 1971 | 83,484 | 7.6 | 77,363 | 7.0 |
| 1972 | 93,968 | 7.7 | 87,375 | 7.2 |
| 1973 | 103,382 | 7.6 | 96,544 | 7.1 |
| 1974 | 116,113 | 7.9 | 108,645 | 7.4 |
| 1975 | 132,680 | 8.3 | 124,279 | 7.8 |
| 1976 | 150,760 | 8.5 | 141,741 | 8.0 |
| 1977 | 169,855 | 8.5 | 160,687 | 8.1 |
| 1978 | 189,657 | 8.4 | 179,895 | 8.0 |
| 1979 | 214,659 | 8.6 | 204,229 | 8.1 |
| 1980 | 248,110 | 9.1 | 236,172 | 8.6 |
| 1981 | 286,975 | 9.4 | 273,801 | 9.0 |
| 1982 | 323,635 | 10.2 | 309,354 | 9.8 |
| 1983 | 357,185 | 10.5 | 341,797 | 10.0 |
| 1984 | 388,453 | 10.3 | 372,698 | 9.9 |
| 1985 | 419,015 | 10.4 | 403,415 | 10.0 |
| 1986 | 455,673 | 10.7 | 439,310 | 10.4 |
| 1987 | 500,346 | 11.1 | 483,244 | 10.7 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Figure 1. National health expenditures and health services and supplies as a percent of the gross national product: United States, calendar years 1965-87.
Disaggregating health expenditures among payers
When disaggregating HSS among payers, we followed principles different from those used to construct the more familiar source-of-funds (i.e., program) presentation. In the new construct by payer, the business sector includes the employer share of private health insurance premiums, the employer share of Medicare and other health-related employment taxes, and direct health care operations of private employers. The household (individual) sector includes private health insurance and Medicare premiums, Medicare hospital insurance payroll taxes paid by individuals, copayments, deductibles, and other nonreimbursable out-of-pocket payments. The two government sectors—Federal, and State and local—consist of expenditures from general revenue, including activities of governments as employers. Finally, we used a philanthropy payer to account for funds routed through charitable organizations, whether from business or individuals. The national health accounts include a small amount of money donated to providers of care by organized charity for direct operation. This amount is transferred intact to the philanthropic sector. However, in the analysis that follows, the role of this sector is not discussed, because the sum reflects private and corporate giving and can be viewed as nonhealth spending by those donors. The omission is not serious, as philanthropy as defined here accounts for about 1 percent of total spending.
Table 2 is a guide to our new payer classification. In the table, we show the steps taken to convert from the familiar national health accounts source-of-funds classification (or program classification) to the payer classification. We discuss the specific payer categories in the next sections.
Table 2. Payer classification of health services and supplies compared with national health accounts program classification: United States.
| Program classification | Payer classification | ||||
|---|---|---|---|---|---|
|
| |||||
| Private | Public | ||||
|
|
|
||||
| Business | Household (individual) | Philanthropy | Federal Government | State and local governments | |
| Private financing | |||||
| Direct patient payments | + | ||||
| Private health insurance premiums | + | ||||
| Employer share | + | − | |||
| Federal Government employers | − | + | |||
| State-local government employers | − | + | |||
| Industrial health services | + | ||||
| Philanthropy | + | ||||
| Public financing | |||||
| Federal Government programs | + | ||||
| Medicare: | |||||
| Employer Medicare taxes1 | + | − | |||
| Federal Government employers | − | + | |||
| State-local government employers | − | + | |||
| Employee Medicare taxes1 | + | − | |||
| Self-employed Medicare taxes1 | +½ | +½ | − | ||
| HI and SMI premiums paid by individuals | + | − | |||
| State and local government programs | + | ||||
| Employer taxes for non-Federal workers' compensation and temporary disability insurance | + | − | |||
Medicare hospital insurance portion of Federal Employment Compensation Act (FICA) taxes, which are paid by employers and employees. One-half of self-employed Medicare taxes are added to the household sector and the other half to the business sector because the self-employed are treated as employer and employee combined.
NOTE: A plus sign indicates that the program item is added to the payer sum; a minus sign indicates that it is deducted.
SOURCE: Health Care Financing Administration, Office of the Actuary: Classification developed by the Office of National Cost Estimates.
Business
Health expenditures allocated to the business sector are of three kinds: private health insurance premiums, public payroll taxes, and direct health operations. An estimate of employer contributions for private health insurance, based on data from the Commerce Department's national income and product accounts (NIPA), forms the basis of the first kind of expenditure; from the figure is deducted an NIPA estimate of health insurance premiums paid by governments in their role as employer. Public payroll taxes paid by businesses include the employer share of Medicare hospital insurance taxes (part of Federal Income Compensation Act, or FICA, taxes), currently 1.45 percent of wages below $48,000. The amount also includes one-half of the Medicare hospital insurance (HI) tax payments of self-employed persons, who must pay both the employer and employee share of the tax. (The figures for Medicare HI trust fund employer and self-employed contributions are estimated by the Social Security Administration and represent liability incurred.) Other payroll taxes support the medical portion of State-mandated workers' compensation and temporary disability insurance programs. These estimates represent medical benefits paid plus administrative costs and the net cost of insurance for these two programs, as estimated in the national health accounts. Finally, the category of spending called “industrial health services” in the national health accounts, which comprises business spending for onsite clinics and other health services, is allocated to the business share of HSS.
Households
Like businesses, households make three kinds of payments for health care: health insurance premiums, payroll taxes, and direct expenditures for services. The national health accounts estimate of total private health insurance premiums, less all employer payments discussed previously, is allocated to households. Aggregate enrollee premiums for Medicare HI and supplementary medical insurance (SMI), excluding SMI premium payments by the Medicaid program on behalf of eligible recipients (buy-ins), are allocated to the household sector as well. (For simplicity, the relatively insignificant amount of employer payments for SMI premiums is classified as a household expenditure.) Employee payroll taxes for Medicare HI, plus one-half of such taxes for the self-employed (who pay both the employer and employee share), are also included. Finally, all funds classified as direct patient payments in the national health accounts—typically expenditures for coinsurance, deductibles, and uninsured services (including nonpatient revenue of hospitals and nursing homes)—are added to the household payer account.
Federal Government
All of the steps needed to re-aggregate Federal program expenditures along payer lines already have been described in connection with the business and household sectors. The Federal payer allocation begins with estimates of Federal spending contained in the published national health accounts (Levit and Freeland, 1988). This amount is reduced by transfer of employee Medicare HI tax payments to the household sector and by transfer of employer Medicare HI tax payments (except for those paid by the Federal Government on its employees' wages) to the business sector. In addition, enrollee Medicare premium payments, most of which are for SMI, are transferred to the household sector. All other Federal programs except the Federal workers' compensation program are supported with general revenue, and these expenditures are left in the Federal payer sector. Finally, an NIPA estimate of Government premium payments for Federal Employee Health Benefits (the Federal Government system of health insurance for its employees) is transferred from the business sector to this sector.
State and local governments
As with the Federal Government, the State and local government allocation begins with the national health accounts estimate of State and local funding for HSS, which already excludes funds obtained from the Federal Government through block grants, Federal matching funds, and other grants in aid. An NIPA estimate of State and local governments' employer share of private health insurance premiums is transferred to this account from the business sector, as is an estimate of Medicare HI tax payments by State and local government employers. Workers' compensation and temporary disability insurance medical benefit payments, administrative costs, and net cost of insurance are transferred out, accruing to the business sector.
Health spending levels in 1987
In 1987, individuals paid for 42 percent of all HSS, more than $200 billion of the Nation's $483 billion health bill (Tables 3 and 4). Most of that amount, $123 billion, was in the form of out-of-pocket expenditures. Of the remainder, $43 billion were spent on private health insurance premiums and $35 billion on Medicare payroll taxes and premiums.
Table 3. Expenditures for health services and supplies, by type of payer: United States, selected calendar years 1965-87.
| Type of payer | 1965 | 1967 | 1970 | 1975 | 1980 | 1981 | 1982 | 1983 | 1984 | 1985 | 1986 | 1987 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Amount in billions | ||||||||||||
| Total | $38.4 | $47.6 | $69.6 | $124.3 | $236.2 | $273.8 | $309.4 | $341.8 | $372.7 | $403.4 | $439.3 | $483.2 |
| Private | 29.9 | 35.0 | 50.6 | 84.7 | 160.4 | 189.6 | 211.6 | 234.4 | 257.5 | 278.2 | 308.5 | 338.5 |
| Private business | 6.7 | 9.2 | 15.3 | 30.7 | 68.1 | 80.0 | 90.7 | 99.5 | 108.1 | 114.4 | 125.0 | 134.6 |
| Private employer share of private health insurance premiums | 5.4 | 6.2 | 11.2 | 22.4 | 51.1 | 58.5 | 68.0 | 75.0 | 81.4 | 84.7 | 90.7 | 96.8 |
| Private employer contribution to Medicare hospital insurance trust fund1 | — | 1.4 | 2.1 | 5.0 | 10.5 | 14.3 | 15.0 | 15.9 | 18.1 | 20.0 | 23.1 | 24.5 |
| Workers' compensation and temporary disability insurance medical benefits and administration | 0.8 | 1.0 | 1.4 | 2.4 | 5.1 | 5.6 | 6.0 | 6.7 | 6.7 | 7.5 | 8.8 | 10.6 |
| Industrial inplant health services | 0.4 | 0.5 | 0.6 | 0.9 | 1.4 | 1.6 | 1.7 | 1.8 | 2.0 | 2.2 | 2.4 | 2.6 |
| Household (individual) | 22.6 | 25.4 | 34.6 | 53.2 | 90.7 | 107.6 | 118.7 | 132.3 | 146.8 | 160.8 | 180.4 | 200.6 |
| Employee share of private health insurance premiums and individual policy premiums | 4.1 | 4.2 | 4.8 | 7.7 | 13.0 | 15.6 | 18.4 | 20.6 | 25.0 | 28.3 | 35.2 | 42.5 |
| Employee and self-employment contributions and voluntary premiums paid to Medicare hospital insurance trust fund1 | — | 1.6 | 2.4 | 5.7 | 11.9 | 16.3 | 17.2 | 19.1 | 21.4 | 23.7 | 27.4 | 29.1 |
| Premiums paid by individuals to Medicare supplementary medical insurance trust fund | — | 0.6 | 1.0 | 1.7 | 2.7 | 3.1 | 3.6 | 3.8 | 4.7 | 5.1 | 5.2 | 6.1 |
| Out-of-pocket health spending by individuals2 | 18.5 | 19.0 | 26.5 | 38.1 | 63.0 | 72.6 | 79.6 | 88.7 | 95.7 | 103.7 | 112.6 | 123.0 |
| Philanthropy | 0.5 | 0.5 | 0.7 | 0.9 | 1.6 | 2.0 | 2.2 | 2.6 | 2.5 | 3.0 | 3.0 | 3.3 |
| Public | 8.5 | 12.6 | 19.0 | 39.6 | 75.8 | 84.2 | 97.7 | 107.4 | 115.2 | 125.2 | 130.8 | 144.7 |
| Federal Government | 4.2 | 6.7 | 10.3 | 21.9 | 41.7 | 45.2 | 53.1 | 59.7 | 63.4 | 69.2 | 70.6 | 78.5 |
| Federal spending for health services and supplies by program | 4.0 | 10.1 | 15.7 | 33.8 | 65.8 | 77.9 | 87.6 | 96.9 | 105.4 | 115.9 | 125.0 | 136.3 |
| Less Medicare hospital trust fund contributions and premiums paid by private business, individuals, and State and local government | — | 3.1 | 4.7 | 11.3 | 23.6 | 32.2 | 34.0 | 36.9 | 41.5 | 46.0 | 53.2 | 56.6 |
| Less Medicare supplementary medical insurance premiums from individuals | — | 0.6 | 1.0 | 1.7 | 2.7 | 3.1 | 3.6 | 3.8 | 4.7 | 5.1 | 5.2 | 6.1 |
| Plus Federal employer contributions to private health insurance | 0.2 | 0.2 | 0.3 | 1.2 | 2.2 | 2.6 | 3.1 | 3.6 | 4.1 | 4.3 | 4.0 | 4.8 |
| State and local government | 4.4 | 5.9 | 8.6 | 17.6 | 34.1 | 39.0 | 44.7 | 47.7 | 51.8 | 56.1 | 60.2 | 66.2 |
| State and local health services and supplies by program | 5.0 | 6.4 | 9.2 | 17.5 | 31.7 | 35.3 | 39.5 | 42.1 | 45.1 | 49.5 | 53.7 | 60.2 |
| Plus State and local employer contributions to private health insurance | 0.3 | 0.4 | 0.6 | 1.9 | 6.2 | 7.6 | 9.3 | 10.5 | 11.3 | 11.9 | 12.5 | 13.6 |
| Plus State and local employer contributions to Medicare hospital insurance trust fund | — | 0.1 | 0.2 | 0.7 | 1.2 | 1.7 | 1.8 | 1.9 | 2.0 | 2.2 | 2.7 | 2.9 |
| Less workers' compensation and temporary disability insurance | 0.8 | 1.0 | 1.4 | 2.4 | 5.1 | 5.6 | 6.0 | 6.7 | 6.7 | 7.5 | 8.8 | 10.6 |
Includes one-half of self-employment contribution to Medicare hospital insurance trust fund.
Includes nonpatient revenues for hospitals and nursing homes.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 4. Percent distribution of expenditures for health services and supplies, by type of payer: United States, selected calendar years 1965-87.
| Type of payer | 1965 | 1967 | 1970 | 1975 | 1980 | 1981 | 1982 | 1983 | 1984 | 1985 | 1986 | 1987 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Percent distribution | ||||||||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private | 77.7 | 73.6 | 72.8 | 68.2 | 67.9 | 69.3 | 68.4 | 68.6 | 69.1 | 69.0 | 70.2 | 70.1 |
| Private business | 17.5 | 19.3 | 22.0 | 24.7 | 28.8 | 29.2 | 29.3 | 29.1 | 29.0 | 28.4 | 28.5 | 27.9 |
| Household (individual) | 58.9 | 53.2 | 49.7 | 42.8 | 38.4 | 39.3 | 38.4 | 38.7 | 39.4 | 39.9 | 41.1 | 41.5 |
| Philanthrophy | 1.4 | 1.1 | 1.0 | 0.7 | 0.7 | 0.7 | 0.7 | 0.8 | 0.7 | 0.7 | 0.7 | 0.7 |
| Public | 22.3 | 26.4 | 27.2 | 31.8 | 32.1 | 30.7 | 31.6 | 31.4 | 30.9 | 31.0 | 29.8 | 29.9 |
| Federal Government | 10.8 | 14.0 | 14.8 | 17.6 | 17.7 | 16.5 | 17.2 | 17.5 | 17.0 | 17.1 | 16.1 | 16.2 |
| State and local government | 11.4 | 12.4 | 12.4 | 14.2 | 14.4 | 14.2 | 14.4 | 14.0 | 13.9 | 13.9 | 13.7 | 13.7 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Business contributed $135 billion in health care spending, 28 percent of HSS. Again, the bulk of spending was for insurance, $97 billion going for the purchase of PHI for employees and another $25 billion to the Medicare HI trust fund as employer-paid premiums. Additional business health expenses for workers' compensation and temporary disability insurance medical benefits amounted to $11 billion in 1987, and onsite health operations cost businesses about $3 billion.
Federal Government outlays for HSS under the new classification scheme amounted to $79 billion in 1987, 16 percent of the total. This amount is significantly less than the 28 percent of HSS designated as Federal under the traditional program classification scheme because of the treatment of the Medicare program. In the payer classification scheme used in this article, payroll taxes and premiums are allocated to the sectors in which they originated. Thus, of total Medicare outlays of $83 billion, $27 billion were transferred to non-Federal employers (businesses and State and local governments) and another $35 billion were transferred to the household account. Only $21 billion—general revenue contributions, Federal employer payments, and trust fund interest income less any change in trust fund balances—remained in the Federal sector.
In contrast to the Federal sector, the State and local government share of HSS in 1987 is slightly higher under the payer classification scheme than under the traditional source-of-funds scheme: 14 percent, compared with 12 percent. The additional money classified here comes in the form of employer payroll taxes and private health insurance premiums. In all, State and local governments funded $66 billion in HSS in 1987.
Trends in health spending
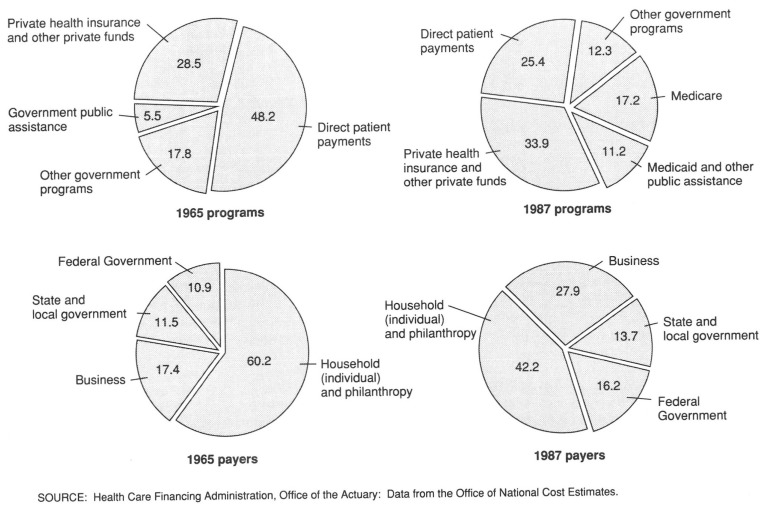
When the traditional disaggregation of HSS by program is used, resources appear to have shifted from private funding to government programs during the last two decades (Figure 2). However, when HSS are disaggregated by payer, it becomes clear that the split between public and private payers has changed much less. Private spending financed 78 percent of HSS in 1965; that share dropped to 73 percent of HSS in 1967, reflecting the introduction of Medicare and its 50-percent subsidy of SMI with general revenue. Governments' share of spending increased as general revenue accounted for a rising portion of SMI (currently 75 percent) and the Medicaid program became a major payer for long-term care. The private share continued to fall, reaching 68 percent in 1980. By 1987, the private spending share had risen again, to 70 percent of HSS.
Figure 2. Percent distribution of expenditures for health services and supplies, by national health accounts program and type of payer: United States, calendar years 1965 and 1987.
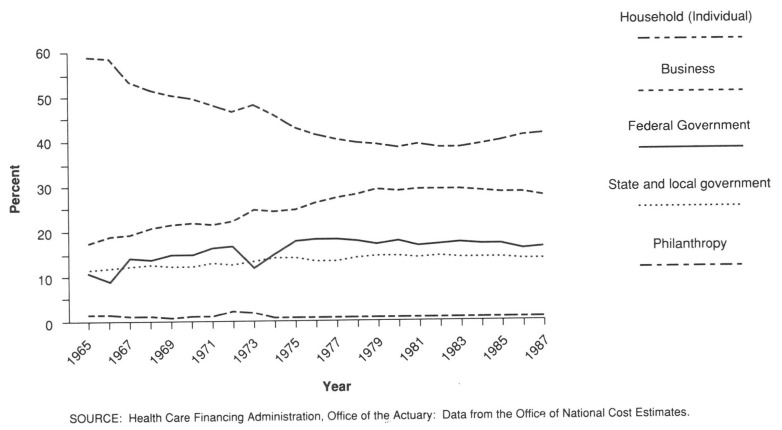
Although the aggregate private share of HSS was fairly constant over time, the split within that share between businesses and households (individuals) has changed dramatically (Figure 3). In 1965, individuals paid for 59 percent of all HSS; by 1980, that share had dropped to 38 percent. The household share began to rise after 1982, reaching 42 percent in 1987, as both businesses and the Federal Government attempted to minimize increases in their health care costs.
Figure 3. Percent of expenditures for health services and supplies, by payer: United States, calendar years 1965-87.
Changes in the trend in the business share of HSS offset more than one-half of the changes in the household share. The decades of the 1960's and 1970's were characterized by increasing depth and breadth of employer-sponsored (and largely employer-paid) health insurance, a trend reflected in the growth of the business share of HSS from 18 percent in 1965 to 29 percent by 1980. Early in the 1980's, the watchword became retrenchment, with increased copayments and deductibles and employees paying for a larger proportion of insurance premiums (Hay Management Consultants, 1988; Hewitt Associates, 1988; Wyatt Company, 1988). Meanwhile, there was a move to managed care (use of preferred provider organizations and health maintenance organizations, required second opinions, preadmission reviews, etc.) and increased reliance on self-funded insurance (in contrast to traditional insurance purchased from Blue Cross, Blue Shield, or a commercial carrier). These types of actions lowered employers' share of the Nation's HSS bill, partly by shifting costs to the household sector and partly by reducing the price and use of health care goods and services and administrative services (Gabel et al., 1988; McDonnell et al., 1987; Short, 1988).
The combined government share of HSS grew from 22 percent in 1965 to 30 percent in 1987. Most of that change occurred in the Federal sector, and most of the Federal change was attributable to growth of the Medicare program. In 1965, just prior to the introduction of Medicare, the Federal share of HSS was 11 percent; by 1967, it had climbed to 14 percent. By 1975, after the inclusion of portions of the disabled population in Medicare, the aggregate Federal share had become 18 percent. Since 1982, that share has fallen to 16 percent as a result of the effective implementation of cost and utilization containment measures such as PPS. In contrast to the Medicare program, Medicaid has played a fairly small role in changing the size of the Federal share, in part because it replaced other federally funded medical care programs for the poor and in part because program spending is limited by State budget constraints.
The State and local share of HSS has grown relatively little over the last two decades, rising from 11.4 percent in 1965 to a high of 14.4 percent in 1982 and then falling to 13.7 percent by 1987. The most significant change in this sector was the adoption of Medicaid, effective in 1966. Explicit attempts to limit the growth of Medicaid expenditures have restrained the growth of the program, with an attendant effect on the overall State and local government share of HSS.
Burden of health care spending
Although the trend in the various payers' share of HSS is interesting in its own right, it is far more instructive from the standpoint of understanding the pressures for financial reform to see how the burden of health care spending has changed over time: That is, how has health spending changed relative to the ability to finance that spending?
No single indicator of burden is preeminent from a theoretical standpoint. Although the concept of income is fairly straightforward at the individual firm or household level, the process of aggregation to national levels introduces several accounting and philosophical issues. Depending on the use or purpose of the analysis, plausible arguments can be made to use post-tax income, pretax income, savings, or any of a host of other measures of resources available to payers. For the business sector, we have constructed several indicators of burden, using not only different measures of resources available but also some measures of other labor costs and of profits. The underlying trends are similar among most of these various indicators, but the timing and intensity of changes vary.
In addition to the difficulties in finding the right indicator of the burden of health care spending, difficulties arise in comparing the level of that indicator across payers. A superficial solution to equitable financing might be simply a matter of equalizing the indicator of burden among payers through mandated benefits, taxation, and so on, and of maintaining the equality of the indicators over time. In fact, however, society appears to place value on limiting the growth of the direct burden to individuals. As we will show shortly, societal preference seems to be to shift the burden of health care costs from individuals, whose aggregate burden has changed little over time, to businesses and government, whose burdens have grown three to four times over the last 22 years. The result of the shift is to distribute the cost of health care differently from the way that use of health care is distributed.
Even if there were agreement on the proper formulation of aggregate burden, we would need to recognize that any aggregate measure, by its nature, does not reflect the different pressures for health care financing reform felt by various groups within each of the four sectors. For example, an individual firm or industry may press for lower health insurance premiums, not because it feels that those premiums are inherently too high, but because the price of the steel it uses has just gone up. Unable to affect the price of steel, the firm looks for costs over which it does have some control, and labor-related costs are prime among those. In this case, an aggregate indicator of burden may fail to signal the pressure for reform. Despite these shortcomings, however, aggregate indicators can convey significant and policy-relevant information and are an important first step.
Business
According to most of the measures used in this article, business health spending at least doubled from 1965 to 1987, and in some cases it rose sixfold (Table 5).
Table 5. Expenditures for health services and supplies as a percent of business income, expense, or profit: United States, selected calendar years 1965-87.
| Year | Business health spending as a share of | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Total business receipts1 | Gross private domestic product2 | Labor compensation | Corporate profits4 | ||||
|
|
|
||||||
| Total compensation3 | Wages and salaries3 | Fringe benefits3 | Before taxes | After taxes | |||
|
| |||||||
| Percent | |||||||
| 1965 | 0.5 | 1.1 | 2.1 | 2.3 | 23.1 | 8.7 | 14.4 |
| 1967 | 0.6 | 1.3 | 2.4 | 2.7 | 25.1 | 11.4 | 19.3 |
| 1970 | 0.7 | 1.8 | 3.2 | 3.5 | 29.8 | 20.2 | 36.8 |
| 1975 | 0.8 | 2.2 | 4.1 | 4.8 | 30.4 | 22.8 | 36.6 |
| 1980 | 1.0 | 2.9 | 5.2 | 6.1 | 33.3 | 28.7 | 44.7 |
| 1981 | 1.0 | 3.0 | 5.5 | 6.5 | 35.2 | 35.3 | 55.0 |
| 1982 | 1.2 | 3.3 | 6.0 | 7.1 | 37.3 | 53.5 | 85.1 |
| 1983 | 1.3 | 3.4 | 6.2 | 7.4 | 38.3 | 47.9 | 76.3 |
| 1984 | 1.2 | 3.3 | 6.1 | 7.2 | 38.0 | 45.1 | 74.0 |
| 1985 | 1.2 | 3.3 | 6.0 | 7.1 | 38.7 | 51.0 | 89.5 |
| 1986 | (5) | 3.4 | 6.2 | 7.4 | 40.2 | 52.9 | 96.3 |
| 1987 | (5) | 3.4 | 6.2 | 7.4 | 41.3 | 48.6 | 94.2 |
Business receipts for sole proprietorships and total receipts of partnerships and corporations based on Internal Revenue Service data.
Reflects health costs embedded in the unduplicated value of intermediate and final goods; based on data from the U.S. Department of Commerce national income and product accounts.
For employees in private industry.
Based on data from the U.S. Department of Commerce national income and product accounts.
Data not available.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
First, we compare the trend of health spending with that of aggregate business income. We have used two measures of income: business receipts and value added. In 1965, the ratio of health spending to business receipts was one-half of 1 percent. By the 1980's, the share had almost tripled, to 1.2 percent, indicating that business health spending had escalated substantially faster than output had during the period. A similar trend is evidenced by the ratio of health spending and private gross domestic product (GDP), an aggregate measure of businesses' value added at each stage of production.
The trends in these two ratios are similar, but the ratios themselves are not. Use of value added rather than business receipts reflects the ratio to account for the value of health spending embedded in purchases made by individual firms as well as their direct health expenditures. For example, a manufacturer of final products pays health insurance premiums for its workers; this spending is direct. It also purchases intermediate products, and part of the cost of those products is attributable to health benefits paid to workers in the intermediate industries. That latter cost is not seen by the final product manufacturer as health care spending, but, in fact, it is, and should be so represented at an aggregate level. The ratio of health spending and private GDP is at least double that of health spending and business receipts.
Next, we examine health spending as a share of labor costs. That spending constituted 2.1 percent of total labor compensation in 1965 and had tripled, to 6.2 percent, by 1987. Over the same period of time, fringe benefits grew more rapidly than wages and salaries did, reflecting their substitution for money wages, accelerated in part by the tax benefits of health insurance and other fringe benefits (Feldstein, 1988; Rhine, 1987). Health spending almost doubled as a proportion of fringe benefits, reaching 41 percent in 1987, and equaled 7 percent of 1987 wages and salaries.
Finally, we compare business health care costs with the bottom line: profits. The ratio of health spending to pretax corporate profits rose from 9 percent in 1965 to a high of 53 percent in 1982 and has remained near 50 percent since that time. Compared with after-tax profits, the ratio is even higher, climbing fairly steadily from 14 percent in 1965 to 94 percent in 1987. Business health care costs may not be eroding corporate profits any more than any other factor input of production; however, the fact that health care spending is almost the same size as after-tax profit helps to explain the high level of business interest in reducing health care costs.
The stabilization of health care spending relative to other labor costs and to measures of income after the early 1980's reflects several factors. There is anecdotal evidence that employers are shifting health care costs to employees through increased employee cost sharing of premiums, reduced coverage of employee dependents, and larger deductibles and coinsurance; some employers are even dropping employee group coverage (Chollet, 1988; Congressional Research Service, 1988; Hay Management Consultants, 1988; Hewitt Associates, 1988). On the other hand, we mentioned earlier that the current national estimates of aggregate employer health insurance premium payments may be low; if such is the case, revised data will result in a ratio that continues to rise through the late 1970's into the 1980's.
Households
Based on our estimates, individual health care spending as a proportion of personal income remained roughly unchanged from 1965 to 1980, about 4 percent (Table 6). During the 1980's, however, that share rose slowly but steadily, reaching 5.5 percent by 1987. This may result from increased deductibles and cost sharing or from changes in the composition of the uninsured population and the use of services not covered by insurance.
Table 6. Expenditures for health services and supplies as a percent of household (individual) income: United States, selected years 1965-87.
| Year | Individual health spending as a share of adjusted personal income1 | Health spending as a share of income after taxes2 | |
|---|---|---|---|
|
| |||
| All ages | Reference person 65 years of age or over3 | ||
|
| |||
| Percent | |||
| 1965 | 4.1 | — | — |
| 1967 | 4.0 | — | — |
| 1970 | 4.2 | — | — |
| 1972-73 | — | 4.9 | 7.8 |
| 1975 | 4.1 | — | — |
| 1980 | 4.1 | — | — |
| 1981 | 4.4 | — | — |
| 1982 | 4.6 | — | — |
| 1983 | 4.8 | — | — |
| 1984 | 4.8 | 4.6 | 10.4 |
| 1985 | 5.0 | 4.5 | 10.2 |
| 1986 | 5.2 | 4.6 | 11.3 |
| 1987 | 5.5 | — | — |
Personal income adjusted to include personal Medicare contributions and to exclude certain transfer payments (medical benefits for Medicare, Medicaid, workers' compensation, and temporary disability insurance).
Calculated from the Consumer Expenditure Interview Survey of the Bureau of Labor Statistics. In this survey, the institutionalized population, including nursing home residents, were excluded, so spending for nursing home care covers only a small portion of total days of care.
Consumer expenditure data are tabulated by age of reference person. These households may include some individuals under 65 years of age. Similarly, individuals 65 years or over who reside in households where the reference person is under 65 years of age are excluded.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
However, data from another source do not substantiate this trend. According to data from the Labor Department's Consumer Expenditure Survey, which covers the noninstitutionalized population, the share of income consumed by health care costs has changed little since 1973. The exact cause of this disparity is not certain; we expect to address it during our revisions of the national health accounts.
Data from the Consumer Expenditure Survey highlight an important point: Aggregate measures can obscure distributional issues within a payer class. The share of income consumed by health care spending for families with an elderly head of household is 11 percent, compared with a ratio of 4 percent for families in general, and has risen over the last 15 years.
Government
Like businesses, the Federal Government experienced a tripling of the demands of health care on its income—general tax revenue—from 1965 to 1982 (Table 7). After 1982, favorable economic conditions spurred growth of tax revenues to keep pace with rising SMI outlays.
Table 7. Expenditures for health services and supplies as a share of Federal and State and local government receipts: United States, selected calendar years 1965-87.
| Year | Federal Government health spending as a share of total Federal receipts1 | State and local government health spending as a share of total State and local receipts2 |
|---|---|---|
|
| ||
| Percent | ||
| 1965 | 4.2 | 7.4 |
| 1967 | 5.9 | 8.3 |
| 1970 | 7.2 | 8.5 |
| 1975 | 11.3 | 10.5 |
| 1980 | 11.4 | 12.5 |
| 1981 | 10.7 | 12.8 |
| 1982 | 13.2 | 13.5 |
| 1983 | 14.7 | 13.1 |
| 1984 | 14.4 | 12.7 |
| 1985 | 14.5 | 12.8 |
| 1986 | 14.2 | 12.8 |
| 1987 | 13.9 | 13.1 |
Excludes contributions to social insurance because these come directly from businesses and individuals. These funds are for dedicated purposes and are not part of the general revenue pool of funds from which health spending can be financed. Based on data from the U.S. Department of Commerce national income and product accounts.
Excludes contributions to social insurance, as explained in footnote 1, and Federal grants in aid, such as Federal Medicaid grants to States. Based on data from the U.S. Department of Commerce national income and product accounts.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
The share of State and local receipts devoted to health care financing, primarily Medicaid spending and funding of hospitals, almost doubled from 1965 to 1982. As with the Federal Government, the outlay share stabilized after 1982, primarily because of the slowing of growth rates of Medicaid and hospital funding and the general health of the economy.
Conclusion
The measures we have developed in this article can serve as a useful way to describe changes in the health care financing system during the last 20 years. We have shown that expenditure share shifted from households to the business and government sectors during the 1960's and 1970's, with a reverse shift during the 1980's. (It is important to remember, however, that households eventually bear the burden of health care through higher taxes, higher prices, or lower wages and dividends.) We have also shown that the burden of health care grew over time, particularly for businesses and governments, precipitating efforts to reform the financing mechanisms in place.
What cannot be shown through aggregate measures are the distributional facets of the health care financing issue. For example, the overall proportion of household income spent for health obscures the fact that some families experience much greater burdens and others experience much smaller burdens. Similarly, small firms may be forced to pay more for an equivalent employee health benefits package than large firms do.
All health care costs eventually are borne by individuals. From a policy standpoint, a health care financing scheme must balance fairness to those individuals in their various roles as consumer, employee, and business owner. Is health care access equitable based on need? Is health care financing equitable based on ability to pay? Are real employee wages and salaries reduced so much that other basic needs cannot be met? Are businesses so burdened with the cost of health care that they can no longer compete in the national and international marketplace, resulting in a loss of jobs, reduced output, and unemployment? The framework developed here cannot be used to resolve these issues, but it can provide a clearer understanding of the aggregate burden of health care financing among payers.
Footnotes
Reprint requests: Carol Pearson, L-1, 1705 Equitable Building, 6325 Security Boulevard, Baltimore, Maryland 21207.
References
- Bureau of Labor Statistics. News—Employment Cost Index—September 1988. U.S. Department of Labor; Washington: Oct. 1988. USDL Pub. No. 88-527. [Google Scholar]
- Chamber of Commerce of the United States. Employee Benefits, 1985. Washington, D.C.: 1986. [Google Scholar]
- Chollet D. Uninsured in the United States: The Nonelderly Population Without Health Insurance, 1986. Washington, D.C.: Employee Benefit Research Institute; Oct. 1988. [Google Scholar]
- Congressional Research Service. Health Insurance and the Uninsured: Background Data and Analysis. Washington: Library of Congress; May, 1988. CRS Report No. 88-537EPW. [Google Scholar]
- Dennis WJ. Small Business Employee Benefits. Washington, D.C.: National Federation of Independent Business Research and Education Foundation; Dec. 1985. [Google Scholar]
- Donahue R. ′89 corporate health plan rates expected to soar 22 percent. National Underwriter. 1988 Nov.47:1. [Google Scholar]
- Dopkeen JC. Postretirement health benefits. Health Services Research. 1987 Feb.21(6):795–848. [PMC free article] [PubMed] [Google Scholar]
- Feldstein PJ. Health Economics. New York: John Wiley & Sons, Inc.; 1988. [Google Scholar]
- Gabel J, Jajich-Toth C, de Lissovoy G, et al. The changing world of group health insurance. Health Affairs. 1988 Summer;7(3):48–65. doi: 10.1377/hlthaff.7.3.48. [DOI] [PubMed] [Google Scholar]
- Garland SB, Gleckman H. Health insurance: A tax-reform footnote trips up small business. Business Week. 1989 Jan.:45. [Google Scholar]
- Hamilton J. The prognosis on health care: Critical—and getting worse. Business Week. 1989 Jan.:82. [Google Scholar]
- Hay Management Consultants. Hay/Huggins Benefit Report: 1988—Prevalence of Practice. Philadelphia: Hay Group, Inc.; Dec. 1988. [Google Scholar]
- Hewitt Associates. Salaried Employee Benefits Provided by Major US Employers in 1982-1987. Lincolnshire, Ill.: Jun, 1988. [Google Scholar]
- ICF Incorporated. Health Care Coverage and Costs in Small and Large Businesses. Washington, D.C.: Office of Advocacy, U.S. Small Business Administration; Apr. 1987. [Google Scholar]
- Kowalczyk G, Freeland M, Levit K. Health Care Financing Review. No. 2. Vol. 10. Washington: U.S. Government Printing Office; Winter. 1988. Using marginal analysis to evaluate health spending trends. HCFA Pub. No. 03276. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Kramon G. Insurance rates for health care increase sharply: January 1 jump stuns many. The New York Times. 1988 Jan.:A-1. [Google Scholar]
- Letsch S, Levit K, Waldo D. Health Care Financing Review. No. 2. Vol. 10. Washington: U.S. Government Printing Office; Winter. 1988. National health expenditures, 1987. HCFA Pub. No. 03276. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Levit K, Freeland M. National medical care spending. Health Affairs. 1988 Winter;7(5):124–136. doi: 10.1377/hlthaff.7.5.124. [DOI] [PubMed] [Google Scholar]
- Lewin/ICF. Increases in Health Insurance Coverage Among Small Firms, 1986-1988. Washington, D.C.: National Association for the Self-Employed; Jun 7, 1988. [Google Scholar]
- Loomis CJ. Will “FASBEE” pinch your bottom line? Fortune. 1988 Dec.:93–108. [Google Scholar]
- McDonnell P, Guttenberg A, Greenberg L, Arnett RH. Health Care Financing Review. No. 2. Vol. 8. Washington: U.S. Government Printing Office; Winter. 1986. Self-insured health plans. HCFA Pub. No. 03226. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Musgrave RA, Musgrave PB. Public Finance in Theory and Practice. New York: McGraw-Hill Book Company; 1973. [Google Scholar]
- Pauly MV. Health Care Issues and American Economic Growth: Innovations in Financing Health Care. Paper presented at the 1988 Karl Eller Center Business/Academic Dialogue on Health Care Issues and American Economic Growth; Tucson, Ariz.. Dec. 2-3, 1988. [Google Scholar]
- Rappaport AM, Kalman RW. The future of employer-sponsored retiree medical plans. Inquiry. 1987 Spring;24:26–35. [PubMed] [Google Scholar]
- Rhine SW. The determinants of fringe benefits: Additional evidence. Journal of Risk and Insurance. 1987 Dec.LIV(4):790–799. [Google Scholar]
- Short P. Trends in employee health insurance benefits. Health Affairs. 1988 Summer;7(3):186–196. doi: 10.1377/hlthaff.7.3.186. [DOI] [PubMed] [Google Scholar]
- Wyatt Company. Group Benefits Survey Summary Highlights: A Survey of Health and Welfare Plans Covering Salaried Employees of US Employers. Washington, D.C.: 1988. [Google Scholar]