Abstract
Alzheimer's disease is closely associated with disorders of neurogenesis in the brain, and growing evidence supports the involvement of immunological mechanisms in the development of the disease. However, at present, the role of T cells in neuronal regeneration in the brain is unknown. We injected amyloid-beta 1–42 peptide into the hippocampus of six BALB/c wild-type mice and six BALB/c-nude mice with T-cell immunodeficiency to establish an animal model of Alzheimer's disease. A further six mice of each genotype were injected with same volume of normal saline. Immunohistochemistry revealed that the number of regenerated neural progenitor cells in the hippocampus of BALB/c wild-type mice was significantly higher than that in BALB/c-nude mice. Quantitative fluorescence PCR assay showed that the expression levels of peripheral T cell-associated cytokines (interleukin-2, interferon-γ) and hippocampal microglia-related cytokines (interleukin-1β, tumor necrosis factor-α) correlated with the number of regenerated neural progenitor cells in the hippocampus. These results indicate that T cells promote hippocampal neurogenesis in Alzheimer's disease and T-cell immunodeficiency restricts neuronal regeneration in the hippocampus. The mechanism underlying the promotion of neuronal regeneration by T cells is mediated by an increased expression of peripheral T cells and central microglial cytokines in Alzheimer's disease mice. Our findings provide an experimental basis for understanding the role of T cells in Alzheimer's disease.
Keywords: nerve regeneration, neurodegeneration, Alzheimer's disease, beta-amyloid 1–42 peptide, neuronal precursors, mice, microglia, interleukin-2, interferon-gamma, interleukin-1β, tumor necrosis factor-α, microtubule associated protein, NSFC grant, neural regeneration
Introduction
Alzheimer's disease (AD), a degenerative disease of the central nervous system, is characterized pathologically by extracellular senile plaques, intracellular neurofibrillary tangles, and a reduction in the number of neurons in the cerebral cortex and hippocampus. The clinical manifestations for AD include loss of memory, and cognitive and behavioral disorders (Finder, 2010). AD is the most common type of dementia, but its etiology and pathogenesis remain unclear. At present, AD is considered a complex pathological process involving several factors. The amyloid cascade hypothesis, or amyloid-beta (Aβ) toxicity hypothesis, has dominated research for decades, and postulates that the deposition of Aβ peptide in the brain is a central event in AD (Honjo et al., 2012). Although AD is not recognized as a classic immune response-mediated disease, growing evidence highlights the immunological mechanisms closely involved in the occurrence and development of AD (Schroeter et al., 2008; Tabira, 2010). According to the immune hypothesis of AD pathogenesis, when immune dysfunction occurs, Aβ metabolism is disrupted. Subsequently, inflammatory and neurotoxic cascade reactions occur, leading to synaptic damage, and neuronal degeneration and death in the brain, ultimately inducing AD (Chopra et al., 2011).
As the mechanism underlying neuronal death in AD has been investigated, researchers have begun to focus on the opposite aspect, newborn neurons, in AD pathogenesis (Donovan et al., 2006; Zhang et al., 2007; Yu et al., 2009; Biscaro et al., 2012). The precursor cells in the subventricular zone of the brain have the ability to regenerate (Alvare-Buylla et al., 2004). In adults, neurogenesis provides a specific mechanism for plasticity of the nervous system (Lazarov et al., 2010). AD pathology studies have revealed that damage to the regions where adult neural cells form (subventricular zone and subgranular zone) leads to a dysfunction in neuronal regeneration; if the dead neurons cannot be replaced by new neurons in time, memory and cognitive disorders will inevitably occur (Demars et al., 2010). AD pathogenesis is closely associated with disorders of neuronal regeneration in the brain, and the effect of immunological mechanisms on neuronal regeneration has become a focus of current AD research. Patients with AD have a significantly higher number of T cells in the brain than healthy people. Immune cells cross the blood-brain barrier and enter the brain, participating in its physiological and pathological functions (Togo et al., 2002; Cao et al., 2009; Monsonego et al., 2013). Additionally, immune cells are shown to maintain nerve cell regeneration function (Ziv et al., 2008). Central-specific T cells play an important role in the maintenance of adult learning and memory capacity, and a deficiency of T cells leads to severe impairments in spatial learning and memory in adult rats (Ziv et al., 2006). We hypothesize that, in AD pathology, T cells are involved in the maintenance of nervous system plasticity, which is also related to neuron regeneration. To our knowledge, no studies have examined the correlation between T cells and neuronal regeneration in the brain. Therefore, the aim of the present study was to investigate the role of T cells in hippocampal neurogenesis in AD pathogenesis, and the underlying molecular mechanisms, in an effort to reveal the contribution of T cells in neuronal regeneration, using immunohistochemistry and quantitative PCR techniques.
Materials and Methods
Animals
Twelve BALB/c wild-type (WT) mice and 12 BALB/c-nude mice, all specific pathogen free, with T lymphocyte deficiency were provided by Guangdong Medical Laboratory Animal Center, China (license No. SCXK (Yue) 2008-0002). The mice were all male, aged 8 weeks, weighing 20–28 g, and housed for 1 week prior to experimentation. Experimental procedures were in accordance with the Guidelines of the Use of Experimental Animals, issued by the Ministry of Science in China.
Animal grouping
The mice were randomly divided into an experimental group and a control group (n = 6 per group). In experimental group I (WT + Aβ) and experimental group II (nude + Aβ), oligomeric state Aβ1–42 was injected bilaterally into the hippocampal CA1 region, to establish a model of AD. In control group I (WT + NS) and control group II (nude + NS), mice received equivalent volumes of normal saline instead of Aβ1–42.
On day 7 after modeling, peripheral blood samples collected from the mice were harvested for quantitative PCR detection of interleukin-2 (IL-2) and interferon-γ (IFN-γ) expression. The mouse brain was divided symmetrically along the midline. The left hemisphere was used for immunohistochemistry of hippocampal neuronal regeneration, and the right for quantitative PCR assay of interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) expression in hippocampal tissue.
Establishment of AD models using hippocampal injection of Aβ1–42
To prepare oligomeric state Aβ1–42, freeze-dried Aβ1–42 powder (500 μg; AnaSpec, San Jose, CA, USA) was dissolved in 100 μL of 1% NH4OH solution for a stock solution at a concentration of 500 μg/100 μL, which was then aliquoted (50 μg/10 μL) and stored at −20°C. At the time of experimentation, an aliquot was thawed and 15 μL normal saline was added to prepare the working solution (2 μg/μL, 50 μg/25 μL), which was incubated at 37°C for 24 hours. This allowed aggregation of Aβ1–42 to toxic oligomeric Aβ (Dahlgren et al., 2002).
Mice were anesthetized by intraperitoneal injection of 0.4% sodium pentobarbital at a dose of 0.2 mL/10 g body weight. The heads were fixed onto a stereotaxic frame, and then the skull was drilled to create a hole at 2.3 mm posterior to bregma and 1.8 mm lateral to the midline, to 1.0 mm depth. A 25 μL microsyringe was inserted 2.0 mm into the brain, and 2 μL Aβ1–42 working solution (experimental groups I and II) or saline (control groups I and II) was slowly (0.4 μL/minute) injected bilaterally into the hippocampal CA1 via micropipette (KDS Model 310 Plus, KD Scientific Holliston, MA, USA). The needles were maintained in place for 5 minutes and then slowly withdrawn to prevent leakage. The skin was sutured and disinfected with alcohol, followed by intramuscular injections of sodium penicillin (40,000 units) for 3 consecutive days. For the remainder of the experiment, mice were housed in specific-pathogen-free cages.
Harvesting the specimens
The brain tissue was harvested 7 days after injection. In brief, mice were anesthetized with 0.4% sodium pentobarbital via intraperitoneal injection, and 1 mL cardiac blood was collected and placed into a tube containing the anticoagulant EDTA. The sample was stored at −20°C for gene expression analysis. After the blood sample was collected, the mice were quickly decapitated, and the brain was removed and cut in two along the middle. The left hemisphere was fixed in 4% paraformaldehyde and embedded in paraffin for the detection of hippocampal neuronal regeneration. The right hippocampus was removed and preserved in pre-cooling preservation tubes, then frozen in liquid nitrogen and stored at −80°C for the detection of microglial cytokine expression.
Immunohistochemistry of doublecortin (DCX) expression in hippocampal neurons
The brain sections were dewaxed and hydrated through an alcohol series and rinsed three times with double-distilled water (ddH2O). Antigen retrieval was performed in 0.01 mol/L citrate buffer (pH 6.0) for 20 minutes using a microwave before the sections were cooled to room temperature, rinsed three times with ddH2O, incubated with 3% H2O2 at room temperature for 15 minutes, and rinsed with 0.01 mol/L PBS three times for 5 minutes each time. The sections were then blocked with 10% bovine serum albumin in a humid chamber at 37°C for 30 minutes, incubated with rabbit anti-DCX polyclonal antibody (1:100, Santa Cruz Biotechnology) at 4°C overnight, rinsed with PBS three times for 5 minutes each time, incubated with biotin-labeled donkey anti-rabbit IgG (Boster Biological Engineering Co., Ltd,, Wuhan, Hubei Province, China) at 37°C for 30 minutes, and rinsed as before with PBS. The sections were then incubated with HRP-conjugated streptavidin working solution at 37°C for 30 minutes, rinsed as before with PBS, developed with DAB for 2–3 minutes and counterstained with hematoxylin for 1–2 minutes, before being dehydrated, cleared with xylene, and mounted with neutral gum. Specimens were observed and photographed under a BX51 microscope (Olympus, Tokyo, Japan). The mean integrated absorbance of positive products for DCX immunostaining was measured using Image-Pro Plus 6.0 software (Media Cybernetics, Rockville, MD, USA) and used for statistical analysis.
Fluorescence quantitative PCR detection of mRNA expression in peripheral blood and hippocampus of mice
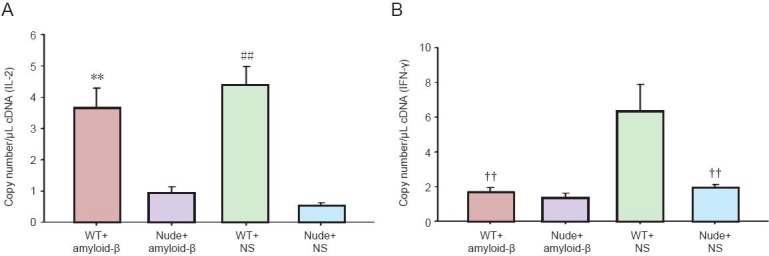
Specific primers in the coding region were designed using Primer Express v2.0 software (Applied Biosystems, Foster, CA, USA) according to the target gene mRNA sequences in GenBank. The primers were synthesized using the ABI 3900 High-Throughput DNA synthesizer (Applied Biosystems).
Primer sequences and product sizes are as follows:
The total RNA in whole blood and brain tissue was extracted with TRIzol, and then reverse-transcribed from an RNA template (4 μL) at 37°C for 1 hour and at 95°C for 3 minutes using the ABI 9700 PCR system (Applied Biosciences). For the quantitative PCR reactions, a positive standard and its gradient were prepared using a standard curve, and the samples and standards were subjected to the reaction system. Reaction conditions were 40 cycles of 93°C for 3 minutes, 93°C for 30 seconds, and 55°C for 45 seconds. Automated analysis was carried out on the results. Total RNA concentration was calculated according to the following formula: A = B1/B2, where A is the statistical value, B1 is the number of copies of the target gene per μL cDNA, and B2 is the number of copies of the reference gene per μL cDNA.
Statistical analysis
Data were analyzed using SPSS 16.0 statistical software (SPSS, Chicago, IL, USA) and expressed as mean ± SD. Groups were compared using one-way analysis of variance followed by the least significant difference tests. Statistical significance was set at P < 0.05.
Results
Neuronal regeneration in the hippocampus of AD mice
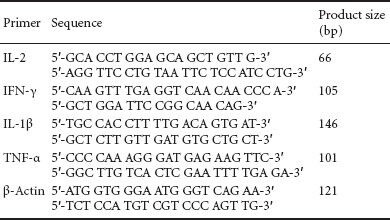
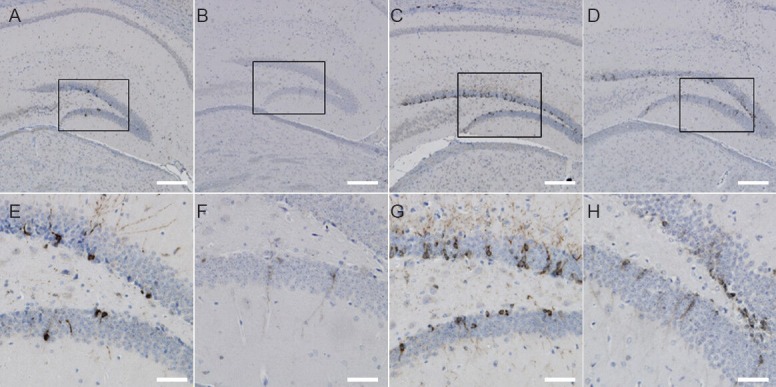
The mice were injected with Aβ1–42 peptide or normal saline for 7 days, and neuronal regeneration in the hippocampus was examined using DCX immunohistochemistry (Figure 1). Under a high magnification microscope, DCX-immunopositive cells were stained brown or yellow, with unilateral radial filament-like projections. The results revealed significant differences in DCX expression between the groups (F = 460.707, P < 0.01). In the WT groups (Figure 1A, C), the number of positive cells was significantly higher than that in the nude groups (Figure 1B, D). DCX expression was the highest in the WT + NS group, then in the WT + Aβ group, nude + NS group, and the lowest in the nude + Aβ group. Statistical analysis showed that the WT groups had a significantly higher number of DCX-positive cells than the nude groups (P < 0.01), and that nude + Aβ mice had a higher expression of DCS than nude + NS mice (P < 0.01; Figure 2). The findings confirm that injection of Aβ1–42 peptide inhibits the regeneration of hippocampal neurons. Furthermore, they indicate that T cells promote hippocampal neuron regeneration, and that such regeneration does not notably occur without T cells.
Figure 1.
Immunolabeling for doublecortin-positive (newborn) neurons in the hippocampal dentate gyrus 7 days after hippocampal injection of Aβ1–42 or saline.
The number of doublecortin-positive cells in the dentate gyrus of wide-type mice (A, C, E, G) was significantly higher than that in nude mice (B, D, F, H). Expression was greatest in control group I (wide-type + saline; C, G), followed by experimental group I (wide-type + Aβ; A, E), control group II (nude + saline; D, H), and minimal in experimental group II (nude + Aβ; B, F). (E, F, G, H) Enlarged view (× 40; scale bars: 200 μm) of the boxed areas in A, B, C, D (× 10; scale bars: 50 μm), respectively.
Figure 2.
Quantitative analysis of doublecortin (DCX) expression in hippocampal dentate gyrus neurons 7 days after modeling.
Y-axis represents the integrated absorbance (IA) value of doublecortin-positive cells. Data are expressed as mean ± SD (n = 6) and compared using one-way analysis of variance and the least significant difference test. **P < 0.01, vs. nude + Aβ group; ##P < 0.01, vs. nude + NS group. NS: Normal saline; WT: wide-type.
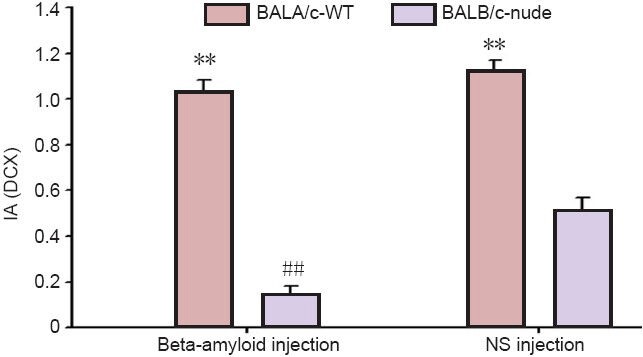
IL-2 and IFN-γ expression in peripheral blood of AD mice
To explore the correlation between hippocampal neuronal regeneration and T cell-associated cytokine expression in AD mice, we measured the expression of cytokines in peripheral blood using quantitative PCR 7 days after modeling. A significant difference in IL-2 gene expression was found (F = 120.109, P < 0.01). IL-2 expression in the WT mice was significantly higher than that in nude mice (P < 0.01; Figure 3A). The results of IL-2 expression were consistent with those of DCX expression in each group, suggesting that IL-2 expression might be related to neuronal regeneration. Significant differences in IFN-γ expression were also found among the groups (F = 55.663, P < 0.01). IFN-γ expression was greatest in the WT + NS group, and significantly lower in the WT + Aβ and nude + NS groups (P < 0.01; Figure 3B). These results indicate that intrahippocampal injection of Aβ1-42 inhibited the expression of IFN-γ in BALB/c-WT mice, and that the BALB/c-nude genotype was associated with lower expression of IFN-γ.
Figure 3.
Quantitative fluorescence PCR for interleukin-2 (IL-2) and interferon-γ (IFN-γ) gene expression in peripheral blood of mice 7 days after modeling.
**P < 0.01, vs. nude + amyloid-β group; ##P < 0.01, vs. nude + NS group; ††P < 0.01, vs. WT + NS group (one-way analysis of variance and the least significant difference test). Data are expressed as mean ± SD (n = 6). WT: Wide-type; NS: normal saline.
IL1-β and TNF-α gene expression in the hippocampus of AD mice
To further explore the possible mechanism of T cells on neuronal regeneration in AD mouse models, we used quantitative PCR to measure the expression of microglial cytokines in the hippocampus 7 days after modeling (Figure 4). Significant differences in IL-1β gene expression were found among the groups (F = 1217.713, P < 0.01). Expression levels of IL-1β and TNF-α in wild-type mice were higher than those in nude mice (P < 0.01). The highest level of IL-1β and TNF-α expression was found in the WT + Aβ group, suggesting that hippocampal injection of Aβ peptides may produce some toxicity, and that WT mice with normal immune function react more severely to Aβ peptide (and produced more cytokines) than nude mice with T-cell immunodeficiency, which respond weakly to Aβ peptide, producing fewer reactive cytokines.
Figure 4.
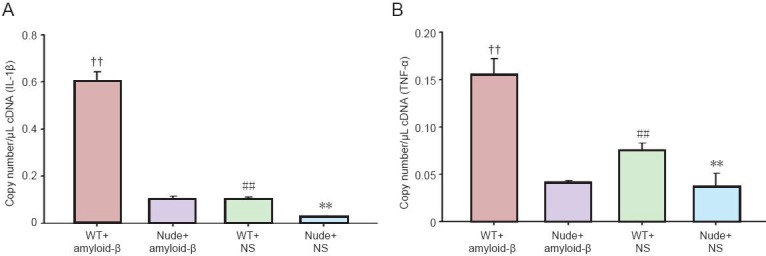
Interleukin-1β (IL-1β; A) and tumor necrosis factor-α (TNF-α; B) gene expression in the hippocampus of mice 7 days after modeling.
**P < 0.01, vs. nude + amyloid-β group; ##P < 0.01, vs. nude + NS group; ††P < 0.01, vs. all other groups (one-way analysis of variance and the least significant difference test). Data are expressed as mean ± SD (n = 6). WT: Wide-type; NS: normal saline.
Discussion
AD is caused by synaptic loss and neuronal death, which result from Aβ deposition-mediated chronic inflammation (Ferretti et al., 2012; Rubio-Perez et al., 2012). In the brain of patients with AD, Aβ deposition not only causes inflammation, but also allows specific T cells to cross the microvascular endothelial cells of the blood-brain barrier and enter the brain parenchyma, thus exacerbating inflammatory responses (Man et al., 2007; Li et al., 2009; Fisher et al., 2011). Neuronal regeneration, in particular its induction and maintenance, is attracting increasing attention in studies of AD pathogenesis.
DCX is a microtubule-associated protein, which is specifically expressed in neuronal precursors and is involved in the migration of immature neurons and neurite growth (Rao et al., 2004). DCX is transiently expressed for 2–3 weeks in the cytoplasm and projections of newly formed neuronal precursors, after which it begins to decline; it is not expressed in mature neurons (Brown et al., 2003). This characteristic allows the use of DCX as a specific marker of neuronal precursors. The present results indicate that T cells promote nerve cell regeneration in the subgranular zone of the hippocampus in WT mice, and a lack of T cells may impair regeneration. In addition, injection of Aβ1–42 inhibits the production of hippocampal nerve cells, depending on the neurotoxicity of Aβ1–42. Previous studies compared neuronal regeneration in WT BALB/c/Ola mice and BALB/c-nude mice with a deficiency of T cells but normal B cells. The evidence suggests that T-cells can not only promote proliferation of neural precursors in the dentate gyrus, but also affect the differentiation of precursor cells (Ziv et al., 2006). Immune deficiency in cells is considered to be the main cause of conflicting results. In the present study, we compared neuronal regeneration in normal BALB/c-WT mice and T-cell-deficient BALB/c-nude mice; our results highlight the contribution of T cells to neuronal regeneration in the hippocampus of AD mice, consistent with previous findings. Thus, hippocampal neuronal regeneration is presumably mediated by the activation of microglial cells. The mechanisms underlying T cell promotion of hippocampal neuronal regeneration also depend on microglial cell-secreted cytokines (Monsonego et al., 2003; Pellicanò et al., 2010; Swardfager et al., 2010).
IL-2 is a T-cell growth factor, mainly produced by activated T-cells. It plays a crucial role in maintaining the growth of T-cell subsets and promoting the proliferation of activated B cells. In the present study, we used PCR to show that the secretion of IL-2 from T cells (IL-2 expression) was positively correlated with the regeneration of hippocampal neurons. IL-2 is an important pro-inflammatory cytokine, and its expression correlates closely with the degree of inflammation and neuronal loss in AD and other degenerative diseases (Meola et al., 2013). The quantity of CD4+ T-cells is significantly increased in the peripheral blood of AD patients, consistent with upregulated expression of IL-2, IL-6 and other inflammatory cytokines in peripheral blood, all of which are secreted by T cells (Becher et al., 2006; Wolf et al., 2009). Interestingly, IL-2 expression correlates with neuronal regeneration, indicating that the inflammatory and neuroprotective effects exist simultaneously in AD, and peripheral IL-2 gene expression can reflect the activation state of T-cells.
IFN-γ is generated by a variety of immune cells including T-cells, the crucial immune regulators in vivo. IFN-γ can increase the expression of MHC-II molecules on the macrophage surface and promote phagocytosis. In AD model mice, IFN-γ produced by Aβ-specific T cells activates microglia to stimulate inflammation and aggravate abnormal Aβ protein deposition (Browne et al., 2013). Another study showed that Aβ-specific T-cells induce immune cells to clear Aβ protein deposition in the brain through the secretion of IFN-γ (Fisher et al., 2010). Hippocampal injection of Aβ1–42 downregulates the expression of IFN-γ and inhibits neuronal regeneration (Zheng et al., 2013). The major adaptive immune cytokine, IFN-γ, not only promotes regeneration of hippocampal neurons and improves spatial learning and memory capacity in adult WT mice, but also plays a crucial role in the regulation of brain inflammation, repair of damaged neurons, and maintenance of normal nervous system function (Baron et al., 2008; Mastrangelo et al., 2009). The present study shows that hippocampal injection of Aβ1–42 peptide inhibits the expression of peripheral blood IFN-γ, and the expression level in BALB/c-nude mice is lower than that in WT mice. Changes in IFN-γ expression reflect the complexity of immunoregulation.
There may be cross-talk between brain-infiltrated T-cells and microglia, activating brain microglia. Microglia secretes various cytokines, which affect the function of nerve cells and other glial cells. In the process of AD pathology, activated microglia may release a series of proinflammatory cytokines, primarily IL-1β, TNF-α, IFN-γ and IL-6. Among these, IL-1β exerts important and diverse biological roles (Farfara et al., 2008; Graber et al., 2009), including its action as an acute inflammatory cytokine in the brain, its expression sharply increasing within a few hours of injury; its autocrine effects on microglia, promoting microglial proliferation and increasing its own secretion as well as that of TNF-α and IL-6; its enhancement of APP-α lyase activity and promotion of its metabolism, reducing Aβ deposition; and at moderate levels it can promote the growth of cultured neurons, but at high levels IL-1β is neurotoxic (Tachida et al., 2008; Moore et al., 2009; Matousek et al., 2012; Song et al., 2013). The present study demonstrated that BALB/c-WT mice have a strong response to Aβ peptide, showing high IL-1β expression, whereas BALB/c-nude mice react weakly to Aβ peptide, with little IL-1β expression. IL-1β expression levels correlated with neuron regeneration throughout the four groups.
TNF-α is an important inflammatory factor that can kill tumor cells or cytokines that induce tumor tissue necrosis. It is mainly produced by activated microglia (Montgomery et al., 2012). The biological activity of TNF-α is diverse, and includes direct killing of cells, as well as immune regulation and the promotion of cell proliferation and differentiation (McCoy et al., 2008; Alvarez et al., 2011). Studies have shown that the loss of neurons in AD is mainly due to the activation of microglial cells by oligomerized Aβ protein, altering the cell cycle via the TNF-α and c-Jun kinase signaling pathways, affecting normal neuronal differentiation and ultimately leading to apoptosis (Bhaskar et al., 2014). The present results suggest that TNF-α expression correlates positively with neuronal regeneration in each group.
As AD progresses, the Aβ-activated microglia produce inflammatory cytokines (such as IL-1α, IL-1β and TNF-α), inducing neuronal death and memory impairment (Fang et al., 2010). Neurotrophic factors (including NGF, BDNF and GDNF) are also produced, to maintain neuronal regeneration and learning and memory functions (Scharfman et al., 2005; Ji et al., 2011; Lilja et al., 2013). Changes in the balance of inflammatory cytokines and neurotrophic factors will accelerate or delay the AD process. Here, we have examined the regeneration of hippocampal neurons and the expression of pro-inflammatory cytokines (IL-2, IFN-γ, IL-1β, TNF-α) in AD mice at 7 days, and found a positive correlation, that is, significant neuronal regeneration and high expression levels of cytokines are found in the same group. The present results suggest that both nerve inflammation and neuroprotective effects might be concomitant in the AD pathological state, and they may maintain a dynamic balance under normal immune function; when an immune imbalance or defect occurs, neuroprotective effects are decreased, affecting nerve regeneration. Our experimental results showed that neuronal regeneration in BALB/c-WT mice was notably better than in T-cell-deficient BALB/c-nude mice. The contribution of T cells to neuronal regeneration in AD mice is closely related to immune status, microglial activation, and the secretion of cytokines.
Footnotes
Funding: This study was supported by the National Natural Science Foundation of China, No. 30840073; the Medical Science Foundation of Guangdong Province, No. A2012298.
Conflicts of interest: None declared.
Copyedited by Murphy S, Norman C, Wang J, Yang Y, Li CH, Song LP, Zhao M
References
- 1.Alvare-Buylla A, Lim DA. For the long run: maintaining germinal niches in the adult brain. Neuron. 2004;41:683–686. doi: 10.1016/s0896-6273(04)00111-4. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez S, Blanco A, Fresno M, Muñoz-Fernández MÁ. TNF-α contributes to caspase-3 independent apoptosis in neuroblastoma cells: role of NFAT. PLoS One. 2011;6:e16100. doi: 10.1371/journal.pone.0016100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron R, Nemirovsky A, Harpaz I, Cohen H, Owens T, Monsonego A. IFN-gamma enhances neurogenesis in wild-type mice and in a mouse model of Alzheimer's disease. FASEB J. 2008;22:2843–2852. doi: 10.1096/fj.08-105866. [DOI] [PubMed] [Google Scholar]
- 4.Becher B, Bechmann I, Greter M. Antigen presentation in autoimmunity and CNS inflammation: how T lymphocytes recognize the brain. J Mol Med. 2006;84:532–543. doi: 10.1007/s00109-006-0065-1. [DOI] [PubMed] [Google Scholar]
- 5.Bhaskar K, Maphis N, Xu G, Varvel NH, Kokiko-Cochran ON, Weick JP, Staugaitis SM, Cardona A, Ransohoff RM, Herrup K, Lamb BT. Microglial derived tumor necrosis factor-α drives Alzheimer's disease-related neuronal cell cycle events. Neurobiol Dis. 2014;62:273–285. doi: 10.1016/j.nbd.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biscaro B, Lindvall O, Tesco G, Ekdahl CT, Nitsch RM. Inhibition of microglial activation protects hippocampal neurogenesis and improves cognitive deficits in a transgenic mouse model for Alzheimer's disease. Neurodegener Dis. 2012;9:187–198. doi: 10.1159/000330363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown JP, Couillard-Despres S, Cooper-Kuhn CM, Winkler J, Aigner L, Kuhn HG. Transient expression of doublecortin during adult neurogenesis. J Comp Neurol. 2003;467:1–10. doi: 10.1002/cne.10874. [DOI] [PubMed] [Google Scholar]
- 8.Browne TC, McQuillan K, McManus RM, O’Reilly JA, Mills KH, Lynch MA. IFN-γ Production by amyloid β-specific Th1 cells promotes microglial activation and increases plaque burden in a mouse model of Alzheimer's disease. J Immunol. 2013;190:2241–2251. doi: 10.4049/jimmunol.1200947. [DOI] [PubMed] [Google Scholar]
- 9.Cao C, Arendash GW, Dickson A, Mamcarz MB, Lin X, Ethell DW. Abeta-specific Th2 cells provide cognitive and pathological benefits to Alzheimer's mice without infiltrating the CNS. Neurobiol Dis. 2009;34:63–70. doi: 10.1016/j.nbd.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chopra K, Misra S, Kuhad A. Neurobiological aspects of Alzheimer's disease. Expert Opin Ther Targets. 2011;15:535–555. doi: 10.1517/14728222.2011.557363. [DOI] [PubMed] [Google Scholar]
- 11.Dahlgren KN, Manelli AM, Stine WB, Jr, Baker LK, Krafft GA, LaDu MJ. Oligomeric and fibrillar species of amyloid-beta peptides differentially affect neuronal viability. J Biol Chem. 2002;277:32046–32053. doi: 10.1074/jbc.M201750200. [DOI] [PubMed] [Google Scholar]
- 12.Demars M, Hu YS, Gadadhar A, Lazarov O. Impaired neurogenesis is an early event in the etiology of familial Alzheimer's disease in transgenic mice. J Neurosci Res. 2010;88:2103–2107. doi: 10.1002/jnr.22387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donovan MH, Yazdani U, Norris RD, Games D, German DC, Eisch AJ. Decreased adult hippocampal neurogenesis in the PDAPP mouse model of Alzheimer's disease. J Comp Neurol. 2006;495:70–83. doi: 10.1002/cne.20840. [DOI] [PubMed] [Google Scholar]
- 14.Fang F, Lue LF, Yan S, Xu H, Luddy JS, Chen D, Walker DG, Stern DM, Yan S, Schmidt AM, Chen JX, Yan SS. RAGE-dependent signaling in microglia contributes to neuroinflammation, Abeta accumulation, and impaired learning/memory in a mouse model of Alzheimer's disease. FASEB J. 2010;24:1043–1055. doi: 10.1096/fj.09-139634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farfara D, Lifshitz V, Frenkel D. Neuroprotective and neurotoxic properties of glial cells in the pathogenesis of Alzheimer's disease. J Cell Mol Med. 2008;12:762–780. doi: 10.1111/j.1582-4934.2008.00314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferretti MT, Bruno MA, Ducatenzeiler A, Klein WL, Cuello AC. Intracellular Aβ-oligomers and early inflammation in a model of Alzheimer's disease. Neurobiol Aging. 2012;33:1329–1342. doi: 10.1016/j.neurobiolaging.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Finder VH. Alzheimer's disease: a general introduction and pathomechanism. J Alzheimers Dis. 2010;22:5–19. doi: 10.3233/JAD-2010-100975. [DOI] [PubMed] [Google Scholar]
- 18.Fisher Y, Nemirovsky A, Baron R, Monsonego A. T cells specifically targeted to amyloid plaques enhance plaque clearance in a mouse model of Alzheimer's disease. PLoS One. 2010;5:e10830. doi: 10.1371/journal.pone.0010830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher Y, Nemirovsky A, Baron R, Monsonego A. Dendritic cells regulate amyloid-β-specific T-cell entry into the brain: the role of perivascular amyloid-β. J Alzheimers Dis. 2011;27:99–111. doi: 10.3233/JAD-2011-102034. [DOI] [PubMed] [Google Scholar]
- 20.Graber JJ, Dhib-Jalbut S. Protective autoimmunity in the nervous system. Pharmacol Ther. 2009;121:147–159. doi: 10.1016/j.pharmthera.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Honjo K, Black SE, Verhoeff NP. Alzheimer's disease, cerebrovascular disease and the β-amyloid cascade. Can J Neurol Sci. 2012;39:712–728. doi: 10.1017/s0317167100015547. [DOI] [PubMed] [Google Scholar]
- 22.Ji C, Song C, Zuo P. The mechanism of memory impairment induced by Aβ chronic administration involves imbalance between cytokines and neurotrophins in the rat hippocampus. Curr Alzheimer Res. 2011;8:410–420. doi: 10.2174/156720511795745366. [DOI] [PubMed] [Google Scholar]
- 23.Lazarov O, Marr RA. Neurogenesis and Alzheimer's disease: at the crossroads. Exp Neurol. 2010;223:267–281. doi: 10.1016/j.expneurol.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li M, Shang SD, Zhao WD, Tian L, Li B, Fang WG, Zhu L, Man SM, Chen YH. Amyloid β interaction with receptor for advanced glycation end products up-regulates brain endothelial CCR5 expression and promotes T cells crossing the blood-brain barrier. J Immunol. 2009;182:5778–5788. doi: 10.4049/jimmunol.0803013. [DOI] [PubMed] [Google Scholar]
- 25.Lilja AM, Röjdner J, Mustafiz T, Thomé CM, Storelli E, Gonzalez D, Unger-Lithner C, Greig NH, Nordberg A, Marutle A. Age-dependent neuroplasticity mechanisms in Alzheimer Tg2576 mice following modulation of brain amyloid-β levels. PLoS One. 2013;8:e58752. doi: 10.1371/journal.pone.0058752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Man SM, Ma YR, Shang DS, Zhao WD, Li B, Guo DW, Fang WG, Zhu L, Chen YH. Peripheral T cells overexpress MIP-1α to enhance its transendothelial migration in Alzheimer's disease. Neurobiol Aging. 2007;28:485–496. doi: 10.1016/j.neurobiolaging.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 27.Mastrangelo MA, Sudol KL, Narrow WC, Bowers WJ. Interferon-gamma differentially affects Alzheimer's disease pathologies and induces neurogenesis in triple transgenic-AD mice. Am J Pathol. 2009;175:2076–2088. doi: 10.2353/ajpath.2009.090059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matousek SB, Ghosh S, Shaftel SS, Kyrkanides S, Olschowka JA, O’Banion MK. Chronic IL-1β-mediated neuroinflammation mitigates amyloid pathology in a mouse model of Alzheimer's disease without inducing overt neurodegeneration. J Neuroimmune Pharmacol. 2012;7:156–164. doi: 10.1007/s11481-011-9331-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCoy MK, Tansey MG. TNF signaling inhibition in the CNS: implications for normal brain function and neurodegenerative disease. J Neuroinflammation. 2008;5:45. doi: 10.1186/1742-2094-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meola D, Huang Z, Ha GK, Petitto JM. Loss of neuronal phenotype and neurodegeneration: effects of T lymphocytes and brain interleukin-2. J Alzheimers Dis Parkinsonism Suppl. 2013;10:3. doi: 10.4172/2161-0460.s10-003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monsonego A, Imitola J, Zota V, Oida T, Weiner HL. Microglia-mediated nitric oxide cytotoxicity of T cells following amyloid beta-peptide presentation to Th1 cells. J Immunol. 2003;171:2216–2224. doi: 10.4049/jimmunol.171.5.2216. [DOI] [PubMed] [Google Scholar]
- 32.Monsonego A, Nemirovsky A, Harpaz I. CD4 T cells in immunity and immunotherapy of Alzheimer's disease. Immunology. 2013;139:438–446. doi: 10.1111/imm.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montgomery SL, Bowers WJ. Tumor necrosis factor-alpha and the roles it plays in homeostatic and degenerative processes within the central nervous system. J Neuroimmune Pharmacol. 2012;7:42–59. doi: 10.1007/s11481-011-9287-2. [DOI] [PubMed] [Google Scholar]
- 34.Moore AH, Wu M, Shaftel SS, Graham KA, O’Banion MK. Sustained expression of interleukin-1beta in mouse hippocampus impairs spatial memory. Neuroscience. 2009;164:1484–1495. doi: 10.1016/j.neuroscience.2009.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pellicanò M, Bulati M, Buffa S, Barbagallo M, Di Prima A, Misiano G, Picone P, Di Carlo M, Nuzzo D, Candore G, Vasto S, Lio D, Caruso C, Colonna-Romano G. Systemic immune responses in Alzheimer's disease: in vitro mononuclear cell activation and cytokine production. J Alzheimers Dis. 2010;21:181–192. doi: 10.3233/JAD-2010-091714. [DOI] [PubMed] [Google Scholar]
- 36.Rao MS, Shetty AK. Efficacy of doublecortin as a marker to analyse the absolute number and dendritic growth of newly generated neurons in the adult dentate gyrus. Eur J Neurosci. 2004;19:234–246. doi: 10.1111/j.0953-816x.2003.03123.x. [DOI] [PubMed] [Google Scholar]
- 37.Rubio-Perez JM, Morillas-Ruiz JM. A review: inflammatory process in Alzheimer's disease role of cytokines. Scientific World Journal 2012. 2012:756357. doi: 10.1100/2012/756357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scharfman H, Goodman J, Macleod A, Phani S, Antonelli C, Croll S. Increased neurogenesis and the ectopic granule cells after intrahippocampal BDNF infusion in adult rats. Exp Neurol. 2005;192:348–356. doi: 10.1016/j.expneurol.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 39.Schroeter S, Khan K, Barbour R, Doan M, Chen M, Guido T, Gill D, Basi G, Schenk D, Seubert P, Games D. Immunotherapy reduces vascular amyloid-beta in PDAPP mice. J Neurosci. 2008;28:6787–6793. doi: 10.1523/JNEUROSCI.2377-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song C, Zhang Y, Dong Y. Acute and subacute IL-1β administrations differentially modulate neuroimmune and neurotrophic systems: possible implications for neuroprotection and neurodegeneration. J Neuroinflammation. 2013;10:59. doi: 10.1186/1742-2094-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N. A meta-analysis of cytokines in Alzheimer's disease. Biol Psychiatry. 2010;68:930–941. doi: 10.1016/j.biopsych.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 42.Tabira T. Immunization therapy for Alzheimer disease: a comprehensive review of active immunization strategies. Tohoku J Exp Med. 2010;220:95–106. doi: 10.1620/tjem.220.95. [DOI] [PubMed] [Google Scholar]
- 43.Tachida Y, Nakagawa K, Saito T, Saido TC, Honda T, Saito Y, Murayama S, Endo T, Sakaguchi G, Kato A, Kitazume S, Hashimoto Y. Interleukin-1 beta up-regulates TACE to enhance alpha-cleavage of APP in neurons: resulting decrease in Abeta production. J Neurochem. 2008;104:1387–1393. doi: 10.1111/j.1471-4159.2007.05127.x. [DOI] [PubMed] [Google Scholar]
- 44.Togo T, Akiyama H, Iseki E, Kondo H, Ikeda K, Kato M, Oda T, Tsuchiya K, Kosaka K. Occurrence of T cells in the brain of Alzheimer's disease and other neurological diseases. J Neuroimmunol. 2002;124:83–92. doi: 10.1016/s0165-5728(01)00496-9. [DOI] [PubMed] [Google Scholar]
- 45.Wolf SA, Steiner B, Akpinarli A, Kammertoens T, Nassenstein C, Braun A, Blankenstein T, Kempermann G. CD4-positive T lymphocytes provide a neuroimmunological link in the control of adult hippocampal neurogenesis. J Immunol. 2009;182:3979–3984. doi: 10.4049/jimmunol.0801218. [DOI] [PubMed] [Google Scholar]
- 46.Yu Y, He J, Zhang Y, Luo H, Zhu S, Yang Y, Zhao T, Wu J, Huang Y, Kong J, Tan Q, Li XM. Increased hippocampal neurogenesis in the progressive stage of Alzheimer's disease phenotype in an APP/PS1 double transgenic mouse model. Hippocampus. 2009;19:1247–1253. doi: 10.1002/hipo.20587. [DOI] [PubMed] [Google Scholar]
- 47.Zhang C, McNeil E, Dressler L, Siman R. Long-lasting impairment in hippocampal neurogenesis associated with amyloid deposition in a knock-in mouse model of familial Alzheimer's disease. Exp Neurol. 2007;204:77–87. doi: 10.1016/j.expneurol.2006.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng M, Liu J, Ruan Z, Tian S, Ma Y, Zhu J, Li G. Intrahippocampal injection of Aβ1-42 inhibits neurogenesis and down-regulates IFN-γ and NF-κB expression in hippocampus of adult mouse brain. Amyloid. 2013;20:13–20. doi: 10.3109/13506129.2012.755122. [DOI] [PubMed] [Google Scholar]
- 49.Ziv Y, Ron N, Butovsky O, Landa G, Sudai E, Greenberg N, Cohen H, Kipnis J, Schwartz M. Immune cells contribute to the maintenance of neurogenesis and spatial learening abilities in adulthood. Nat Neurosci. 2006;9:268–275. doi: 10.1038/nn1629. [DOI] [PubMed] [Google Scholar]
- 50.Ziv Y, Schwartz M. Orchestrating brain-cell renewal: the role of immune cells in adult neurogenesis in health and disease. Trends Mol Med. 2008;14:471–478. doi: 10.1016/j.molmed.2008.09.004. [DOI] [PubMed] [Google Scholar]


