Abstract
Background: Recent regulatory and clinical concerns have brought into sharp focus antipsychotic drug-induced QTc interval prolongation, torsades de pointes, and sudden cardiac death. Several new generation (atypical) antipsychotic drugs have either been withdrawn from clinical use or delayed in reaching the marketplace due to these concerns. Because torsades de pointes is rarely found, QTc interval prolongation serves as a surrogate marker for this potentially life-threatening arrhythmia. Current methods of calculating this electrocardiographic parameter have limitations. The primary care physician is a key member of the team managing a patient who requires administration of antipsychotic drugs. This article focuses on new generation antipsychotic drugs and principles useful to both the primary care physician and the psychiatrist.
Method: PubMed was searched in September 2002 using the terms antipsychotic drug and QT interval. References were examined from review articles describing antipsychotic drugs and the QT interval. The author's files gathered over the past 20 years on the QT interval were also reviewed.
Results: Nine cases were available in which drug-induced QTc interval prolongation was associated with new generation antipsychotic drug administration. Eight cases were taken from the literature, and the author added one additional report. The newer agents involved were risperidone, quetiapine, and ziprasidone. In at least 8 cases, there was evidence of other risk factors associated with QTc interval prolongation. In one case frequently referenced in the literature, the authors misunderstood their own data showing that QTc interval prolongation did not relate to delayed ventricular repolarization. In another instance, 2 authors reported on the same patient, with important information missing from both articles. No evidence of torsades de pointes appeared in any of the 9 cases.
Conclusions: No evidence is currently available in the literature implicating new generation antipsychotic drugs in the production of torsades de pointes. However, the absence of such evidence does not prove that newer antipsychotic drugs do not cause torsades de pointes. Among patients free of risk factors for QTc interval prolongation and torsades de pointes, current literature does not dictate any specific consultative or laboratory intervention before administering new generation antipsychotic drugs. When risk factors are present, evaluation and intervention specific to those risk factors should dictate the clinician's course of action. More specific guidelines for monitoring the QT interval and risk of torsades de pointes await improved methods of measuring the QTc interval relevant to each patient.
Integrated medical care for patients with chronic mental illness requires a close working relationship between the psychiatrist and the primary care physician. In no area of medicine is this more important than when considering the subject of cardiovascular disease.
In both private-sector and public-sector psychiatry, whether inpatient or outpatient focused, psychiatric care may be physically, organizationally, or geographically separated from medical care. Cardiovascular disease and its complications may be life threatening. Thus, developing a set of definitions and criteria agreed upon by both the mental health provider and the medical care provider is essential to providing good care for the psychiatric patient vulnerable to the complications of cardiovascular disease.
Antipsychotic drug-induced or drug-associated QT interval prolongation remains an area of intense interest for both primary care providers and psychiatrists. Recent articles on this topic have appeared in journals of various disciplines.1–28 These articles largely focus on the potential for older antipsychotic drugs to cause QT interval prolongation and torsades de pointes. Because at least some newer antipsychotic drugs may cause QT interval prolongation, we must consider the possibility that these agents may also cause torsades de pointes.
This article looks at the issue of newer antipsychotic drugs and their potential to lengthen the electrocardiographic QT interval, leaving the patient vulnerable to the cardiac arrhythmia torsades de pointes. Specifically, information available in the literature is reviewed and an additional case report of a patient who developed QT interval prolongation while receiving risperidone is reported.
CARDIAC ELECTROPHYSIOLOGY
Before the case reports are reviewed and comment provided, cardiac electrophysiology relevant to the care of patients receiving drugs that may prolong the QT interval is discussed. Both normal and drug-induced changes in the electrocardiogram (ECG) and cardiac action potential are reviewed.
Electrocardiographic QT Interval
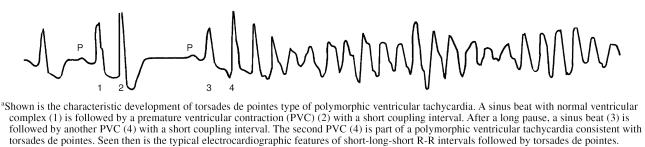
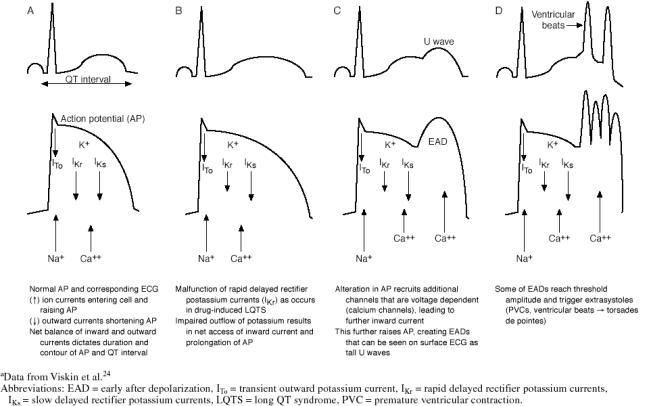
The electrical forces generated within the heart by the various myocardial cells contribute to the surface ECG (Figure 1). Heart rate inversely relates to the QT interval. Various group-derived formulae are used to correct the QT interval (QTc) for heart rate. The “c” in “QTc” stands for “correction.” This correction is intended to remove heart rate as a confounding variable. The Bazett formula29 (QTc = QT divided by the square root of the R-R interval) is the most popular method for correcting (normalizing) the QT interval to a heart rate of 60 beats/min. We may compare patients with one another or compare the same patient at different times (different QT intervals) by normalizing the QT interval (QTc). The Bazett formula is a less useful estimate of QTc interval at higher heart rates.
Figure 1.
Electrocardiographic (ECG) QT Intervala
For men below the age of 55 years, the normal range for the QTc interval is 350 to 430 ms. For women, the comparable value is 350 to 450 ms.18 Concern arises when the QTc interval is between 450 and 500 ms. When the QTc interval is greater than 500 ms, the patient is at an increased risk of developing torsades de pointes.4
Zareba et al.30 reported that the risk of cardiac events before age 40 years in family members with congenital long QT syndrome (LQTS) not taking β-blockers was influenced by the QTc interval. The odds ratio was 2.18 in family members with a QTc interval > 440 ms to 460 ms, 3.93 with a QTc interval > 460 ms to 500 ms, and 9.66 with a QTc interval > 500 ms.
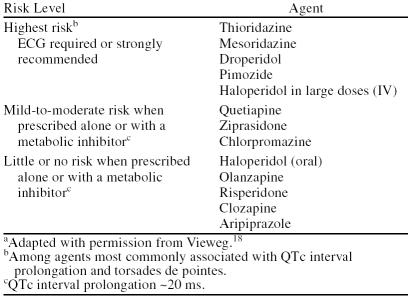
Cardiac Action Potential
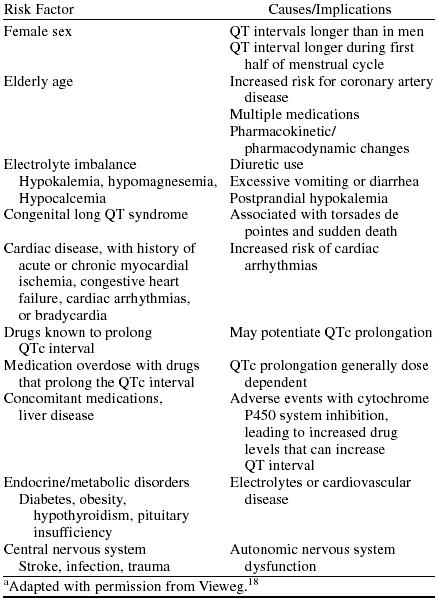
Figure 2 shows the action potential of a single ventricular muscle cell. Depicted are sodium, calcium, and potassium ionic movements during ventricular muscle cell action potential. Ions are distributed unevenly between the interstitium and interior of the myocyte because impermeable, negatively charged proteins inside the myocyte and cell membrane selectively limit ionic movement between the cell and interstitium.31 Ion channels are made up of specialized proteins and are selective for certain ions. Factors including membrane potential, neurohormones, ATP supply, and drugs may modify ion channel activity.
Figure 2.
Cardiac Action Potentiala
A net inward flux of Na+ and then Ca++ account for cell depolarization. Repolarization derives from a net outward flux of K+.
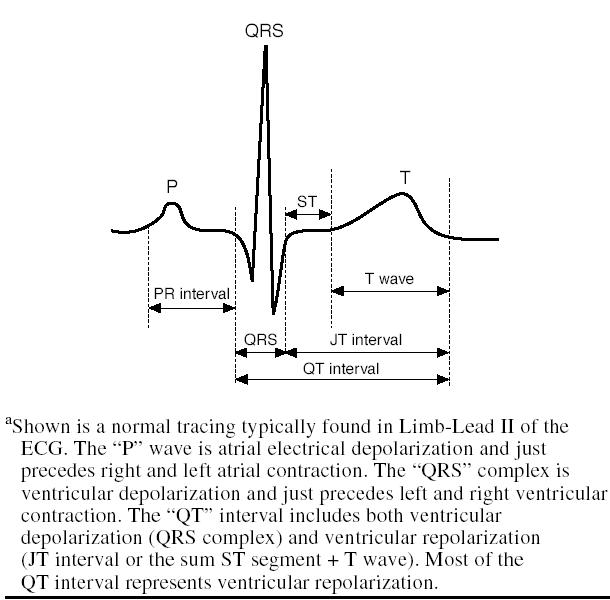
ECG, Action Potential, and Torsades de Pointes
QT interval prolongation occurs when drugs or conditions enhance inward depolarizing Na+ or Ca++ currents or decrease outward K+ currents.32 Figure 3 shows sequential changes in the ECG and the action potential leading to torsades de pointes.
Figure 3.
ECG, Action Potential, and Torsades de Pointesa
Antipsychotic drugs, particularly thioridazine of the phenothiazine family, primarily block the rapid component of the delayed rectifier K+ channel (IKr) (Figure 3), yielding inhomogeneous lengthening of the myocyte action potential, QTc interval prolongation, early after depolarizations (EADs), and torsades de pointes.33
The quinidine-like (ion blocking) properties of tricyclic antidepressants (TCAs) act primarily on sodium influx during phase 0 (sodium “fast” channel). In overdose, TCAs may induce widening of the QRS complex.34 TCAs may secondarily affect calcium influx (calcium “slow” channel) and potassium efflux during phase 3—thereby lengthening the JT interval component of the QT interval. Thus, TCAs may cause QT interval prolongation both by widening the QRS complex and delaying repolarization (lengthening the JT interval).
The secondary effects of TCAs and the primary effects of thioridazine-like drugs may act together to lengthen the QT interval and stimulate torsades de pointes. Because the JT interval is the major component of the QT interval, drugs impacting on the JT interval are more likely to significantly lengthen the QT interval than are drugs widening the QRS complex alone.
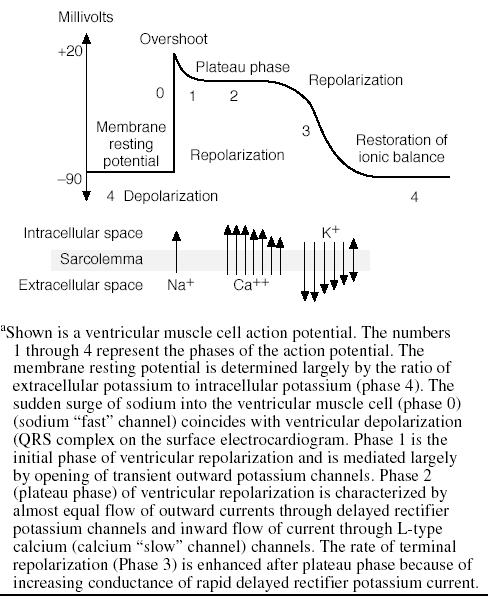
Torsades de Pointes
Figure 4 shows the typical ECG features of polymorphic ventricular tachycardia of the torsades de pointes type. Tachycardia is present because the ventricular beats appear close together. The arrhythmia is presumed to be ventricular in origin because the ventricular complexes are wide. The ventricular complexes vary in configuration; that is, the shape (morphology) varies from beat to beat consistent with polymorphic ventricular tachycardia of the torsades de pointes type.
Figure 4.
Torsades de Pointesa
The ever changing morphology of the QRS complex in torsades de pointes is due to an ever changing focus within ventricular tissue causing each beat; that is, the beats are multifocal in origin. The more common form of ventricular tachycardia is unifocal, with all QRS complexes looking the same—quite different from the polymorphic ventricular tachycardia appearing in torsades de pointes.
The relationship between QT interval or QTc and torsades de pointes is such that either measurement commonly exceeds 500 ms among subjects developing torsades de pointes.4 The most common QT interval or QTc is 600 to 649 ms among patients with torsades de pointes.4
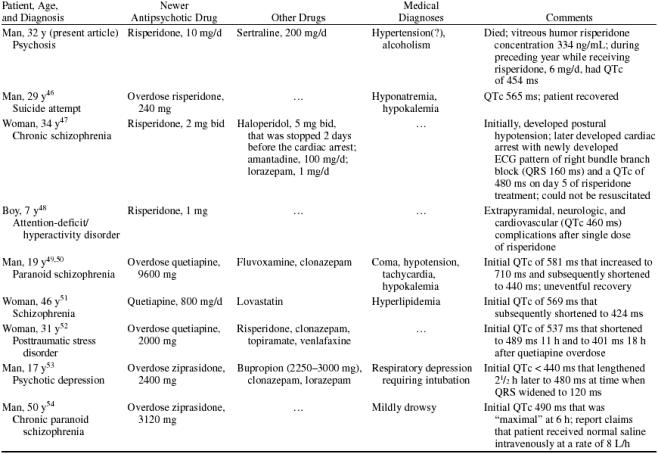
RISK FACTORS FOR QT INTERVAL PROLONGATION (Table 1)
Table 1.
Risk Factors Contributing to QTc Interval Prolongationaa
Circadian Variation
The QTc interval varies throughout the 24-hour cycle, with nighttime values about 20 ms longer than daytime measurements. Changes in sympathetic and parasympathetic (autonomic) tone determine these differences.35,36 In 20 normal subjects, circadian QTc interval variation was 76 ± 19 ms (range, 35–108 ms).36 Cardiovascular disease may widen this variation.
Sex
At birth, QTc interval measurements are the same for male and female infants.37 At puberty, the male QTc interval shortens by about 20 ms. This androgen-driven difference remains until ages 50 to 55 years when, coincident with a decline in male testosterone levels, sex differences in QTc measurements narrow. We would expect about 45% of cases of torsades de pointes to occur in women based on the usual cardiovascular risk factors; however, about 70% of cases are found in women.37
Menstrual Cycle
Rodriguez et al.38 studied men and women between ages 21 and 40 years to see if phases of the menstrual cycle altered QTc interval measurements among women compared with men. They gave subjects intravenous low-dose ibutilide (an antiarrhythmic agent known to prolong the QT interval). The authors studied men once and women 3 times coincident with the 3 phases of the menstrual cycle during the month.
QTc interval measurements increased the most during the first half of the menstrual cycle compared with those during the second half of the menstrual cycle and with those of men. If quinidine-like drugs are not given, QTc interval measurements are stable throughout the menstrual cycle.38
Age and Cardiovascular Disease
Elderly men and women tend to have longer QTc interval measurements than their nonelderly counterparts even when both groups are free of cardiovascular disease.39 Age-matched subjects with cardiovascular disease tend to have longer QTc interval measurements than do those free of cardiovascular disease.
Electrolytes
Electrolyte disturbances, particularly hypokalemia and hypomagnesemia, may contribute to or even cause QT interval prolongation.40–42 Hypokalemia, by decreasing intracellular concentration of potassium, prolongs the cardiac action potential and may cause EADs, leading to torsades de pointes. Various factors may contribute to electrolyte disturbances, including diuretics and excessive vomiting and diarrhea. Postprandial states may lower serum potassium levels. Intensive exercise and agitation may be associated with hypokalemia.
Pharmacodynamic/Pharmacokinetic Factors
Drugs may alter phase 3 (Figure 2) potassium flow (pharmacodynamic factor) and disrupt the synchrony of action of individual cardiac cells during the latter part of repolarization.32 This may induce EADs and torsades de pointes.
Five percent to 10% of European Americans are “poor metabolizers” (pharmacokinetic factor).43 The cytochrome P450 (CYP) isoenzyme 2D6 is most commonly involved. The Pfizer 054 study44 assessed the potential for metabolic inhibitors such as paroxetine to induce QTc interval prolongation by increasing antipsychotic drug levels. The metabolic pathways inhibited in the Pfizer 054 study were 2D6 (paroxetine) for thioridazine, risperidone, and haloperidol; 3A4 (ketoconazole) for ziprasidone, quetiapine, and haloperidol; and 1A2 (fluvoxamine) for olanzapine. Aripiprazole is metabolized by both 2D6 and 3A4 pathways.
Congenital Long QT Syndrome (LQTS)
Congenital LQTS occurs in approximately 1 in 5000 births and accounts for about 3000 to 4000 deaths/year in the United States (mostly children and young adults).45 Nine percent of pediatric patients with LQTS present with sudden cardiac death. More than 71% of such patients will die within 15 years if not treated. Clinicians should take a careful personal and family history of syncope and sudden death when considering treatment with drugs that may prolong the QT interval and leave the patient vulnerable to torsades de pointes.
METHOD
PubMed was searched using the terms antipsychotic drug and QT interval. References were examined from review articles describing antipsychotic drugs and the QT interval. The author's files on the QT interval gathered over the past 20 years were also reviewed for articles about antipsychotic drugs and the QT interval.
RESULTS (Table 2)
Table 2.
Case Reports of QTc Interval Prolongation in Patients Taking New Generation Antipsychotic Drugs
Regulatory concern and recent reports have associated a number of older (typical) antipsychotic drugs with QTc interval prolongation, torsades de pointes, and sudden death.1,8,9,17,18 Little information is available with regard to newer (atypical) antipsychotic drugs (clozapine, risperidone, olanzapine, quetiapine, ziprasidone, and aripiprazole) and these cardiac problems. In addition to the author's case report of risperidone administration and QT interval prolongation, 8 articles were found reporting an association between newer antipsychotic drugs and QT interval prolongation. Three cases from the literature included treatment with risperidone,46–48 3 with quetiapine,49–52 and 2 with ziprasidone.53,54
Risperidone Case Report
Four years before his death in the early summer of 1997 at age 32 years, a then 28-year-old black man was found to suffer from psychosis with features of a religious conversion in which he had been forgiven for his sins. The patient underwent a brief trial of haloperidol with some improvement. Several months earlier, the patient had entered an alcohol rehabilitation program.
In early 1995, the patient was taking haloperidol and nortriptyline. He complained of isolation, memory impairment, reduced energy, and hypersomnia. Haloperidol was stopped, and the patient was started on risperidone, reaching a dose of 6 mg/day. Nortriptyline was stopped, and he was started on sertraline, 50 mg/day. Sertraline was increased over the next several months to 150 mg/day and 6 months later to 200 mg/day. The patient also received benzodiazepines for sleep.
In mid-1996, an ECG showed a QTc interval of 405 ms and minor T wave flattening and inversion. Several months later, an ECG showed a QTc interval of 454 ms and minor T wave flattening. Later that year, the patient sought care in an emergency department (ED) for nausea, vomiting, and abdominal pain. Clinicians were concerned about alcohol abuse. Risperidone was increased to 8 mg/day.
In early 1997, the dose of risperidone was increased to 10 mg/day. The patient continued to take sertraline, 200 mg/day. Three weeks before his death, an endoscopy showed mild esophagitis and nonspecific gastritis.
The patient was found dead at home. Because of an error, the autopsy was performed after the patient was embalmed. Necropsy findings included normal coronary arteries, left ventricular hypertrophy, and moderate hepatosplenomegaly. Risperidone concentration in the vitreous humor was 334 ng/mL. Review of the clinical records revealed no history of presyncope, syncope, or torsades de pointes.
Commentary.
In this case, QTc interval prolongation of 454 ms (above the normal range of 350 to 430 ms for nonelderly men) appeared when the patient was taking risperidone, 6 mg/day. Subsequently, risperidone was increased to 8 mg/day and then 10 mg/day while the patient continued to take sertraline (a drug that may interfere with CYP2D6 pathways used by risperidone). Complicating the clinical picture was a history of alcohol abuse and autopsy findings of hepatosplenomegaly. Liver disease may have slowed the metabolism of risperidone. The vitreous humor concentration of risperidone was 334 ng/mL, which is more than 30 times therapeutic levels of this drug.55 Left ventricular hypertrophy was found at autopsy and may, in and of itself, account for the patient's death. Thus, we are left with many more questions than answers relating drug to death (or QTc interval prolongation) in this patient.
Cases From the Literature
Risperidone literature: Case 1.
During the premarketing studies of risperidone, a case report appeared in which a 29-year-old man presented to the ED 45 hours after taking 240 mg of risperidone as a suicide gesture.46 The patient was alert and well oriented, and vital signs were normal. An initial ECG showed a QTc interval of 565 ms that returned to a near-normal value (444 ms) in 12 hours. Complicating factors included hyponatremia and hypokalemia. No cardiac arrhythmias were reported, and the patient recovered uneventfully.
1. Commentary. In this case described by Brown et al.,46 QTc interval prolongation appeared in the setting of risperidone overdose and hypokalemia. Hypokalemia was corrected, and the QTc interval returned to a near-normal value within 12 hours. Hypokalemia in and of itself may be associated with QTc interval prolongation of this magnitude. We are left with much uncertainty in linking risperidone to QTc interval prolongation in this case.
Risperidone literature: Case 2.
A 34-year-old white woman received risperidone to treat an exacerbation of chronic schizophrenia.47 She developed cardiac arrest on hospital day 5 of drug treatment (risperidone, 2 mg b.i.d.). An ECG associated with pulseless electrical activity showed QRS interval duration of 160 ms and QTc interval of 480 ms. Resuscitative efforts were not successful. No evidence of torsades de pointes was found.
1. Commentary. The article by Ravin and Levenson47 is referenced frequently in the literature linking risperidone to a fatal cardiac event via the finding of QTc interval prolongation. Apparently unappreciated in this report by the authors was the finding that the QRS duration was prolonged to 160 ms as a part of a newly found right bundle branch block (RBBB) configuration. One may assume that the QRS duration was normal (probably about 80 ms) before the conduction abnormality appeared. Therefore, most, if not all, of the measured QT interval prolongation was due to QRS complex widening rather than JT interval prolongation. The JT interval measures ventricular repolarization whereas QRS duration measures ventricular depolarization.18 Vulnerability to torsades de pointes derives from delay of ventricular repolarization and EADs, setting in motion polymorphic ventricular tachycardia. Formulae to calculate the QTc interval derive from patients free of cardiac conduction disturbances of the RBBB type. Thus, the patient did not have lengthening of ventricular repolarization as suggested in this article. Ravin and Levenson47 also referenced another report56 of risperidone overdose and claimed that the QTc interval (400 ms) was prolonged when it was well within the normal range.
Risperidone literature: Case 3.
A 7-year-old boy received risperidone, 1 mg, to treat attention-deficit/hyperactivity disorder.48 During the next 24 hours, his parents noted confusion, psychomotor retardation, tongue stiffness, and drooling. The boy then received a second dose of risperidone. He deteriorated further and was taken to the ED. The patient appeared tired and was making guttural sounds. Blood pressure measurements showed significant orthostasis. His extremities were hypotonic, and he made occasional spontaneous movements. An ECG showed a QTc interval of 460 ms. Several doses of diphenhydramine were given. Within a few hours, his abnormal symptoms and signs resolved. He was observed in the intensive care unit overnight, and the QTc interval returned to normal the next day.
1. Commentary. Risperidone-induced QTc interval prolongation occurred in a 7-year-old boy without other risk factors after he received a 1-mg dose of risperidone on sequential days.48 It is possible that genetic testing of the patient and family might lead to a diagnosis of congenital LQTS. Because of the paucity of experience with risperidone in young children, youth itself may constitute a risk factor for drug-induced QTc interval prolongation.
Quetiapine literature: Case 1.
QTc interval prolongation occurred in a 19-year-old white man with paranoid schizophrenia who ingested 48 200-mg tablets of quetiapine (9600 mg).49,50 The heart rate in the ED (22 hours after ingestion) was 138 beats/min and serum potassium concentration was slightly depressed at 3.3 mmol/L. The initial QTc interval was 581 ms and subsequently increased to 710 ms (33 hours after ingestion) before returning to near normal (440 ms) 49 hours after overdose. Quetiapine overdose was complicated by the patient also receiving fluvoxamine, a potent blocker of the CYP3A4 isoenzyme that metabolizes quetiapine. No evidence of torsades de pointes was found, and the patient returned home taking quetiapine after 5 days of hospitalization.
1. Commentary. The report of the 19-year-old man who took 9600 mg of quetiapine in a suicide attempt is interesting for several reasons.49,50 The same report appears twice in the literature by different authors submitting to different journals with each article emphasizing different aspects of this case. Dramatic and impressive QTc interval prolongation occurred with an initial value of 581 ms that increased to 710 ms. Initially, mild hypokalemia was present along with a rapid heart rate. Before the overdose, fluvoxamine had been provided to the patient. This drug may inhibit the metabolism of quetiapine.
Quetiapine is the new generation antipsychotic drug most likely to induce tachycardia, probably by a nonanticholinergic mechanism. The formula (Bazett)29 most commonly used to calculate QTc interval from the measured QT interval is least accurate at higher heart rates—that is, it is most likely to overestimate the actual QTc interval. This observation is unlikely to account for the QTc interval of 710 ms despite the rapid heart rate. Although the patient's clinical course was difficult, he made a complete recovery.
Quetiapine literature: Case 2.
Coadministration of quetiapine and lovastatin was associated with QTc interval prolongation in a 46-year-old woman with schizophrenia initially receiving quetiapine, 800 mg/day, and sertraline, 100 mg/day.51 A screening lipid profile revealed mildly elevated cholesterol and triglycerides. The patient was given lovastatin, 10 mg/day. An ECG obtained 2 months later showed a QTc interval of 569 ms. A day later, after reducing lovastatin to 5 mg/day, the QTc interval was 424 ms. Several months later, clinicians switched from lovastatin to niacin because of recurrent hyperlipidemia. During the entire clinical course, torsades de pointes was not found. Because lovastatin is also metabolized by the CYP3A4 isoenzyme, this agent was implicated in the finding of QTc interval prolongation.
Representatives of the manufacturer of quetiapine responded to this case report.57 They argued that any relationship between quetiapine administration and QTc interval prolongation was speculative because (1) QTc interval measurement methodology was not given, (2) the QT correction formula was not described, (3) QTc interval normalization within 24 hours suggested a spurious reading, (4) sertraline administration may be associated with QTc interval prolongation, and (5) the Pfizer 054 study showed little propensity for quetiapine-induced QTc interval prolongation to occur when this drug was coadministered with the powerful CYP3A4 inhibitor, ketoconazole.
The authors' reply pointed out the limitations of using single case reports to define causality.58 They discussed the limitations of the Bazett QT correction formula used by them. Also, they pointed out that quetiapine was the only atypical antipsychotic drug in the Pfizer 054 study associated with QTc interval prolongation when coadministered with a metabolic inhibitor.
1. Commentary. To explain QTc interval prolongation in their case, Furst et al.51 postulated that lovastatin inhibited the metabolism of quetiapine, thereby increasing the plasma concentration of the newer antipsychotic drug to cardiotoxic levels. The authors offer no information about the patient's heart rate, and recovery was uneventful.
Quetiapine literature: Case 3.
Overdose with 2000 mg of quetiapine led to an ED presentation of a 31-year-old white woman receiving treatment for long-standing post-traumatic stress disorder.52 The patient's maintenance medications included quetiapine, 100 mg at night, risperidone, 1 mg in the morning and 2 mg in the evening, clonazepam, 0.5 mg twice a day, topiramate, 50 mg in the morning and 200 mg in the evening, and venlafaxine extended release, 225 mg/day.
Initially, the patient was drowsy. Physical and laboratory examinations were largely unremarkable except for QTc interval prolongation of 537 ms at a heart rate of 95 beats/min. The patient received activated charcoal by mouth and fluids intravenously. All medications were stopped. About 11 hours after her overdose, the QTc interval measurement was 489 ms. Seven hours later, it had shortened to 401 ms. Recovery was uneventful. Specifically, there was no evidence of torsades de pointes. Plasma concentrations of quetiapine were consistent with the original overdose of the drug. The authors hypothesized that the combination of quetiapine and risperidone led to QTc interval prolongation in this patient.
1. Commentary. Beelen et al.52 hypothesized that the combination of an overdose of 2000 mg of quetiapine and a maintenance dose of risperidone, 1 mg in the morning and 2 mg in the evening, accounted for QTc interval prolongation in their case. Decreases in plasma levels of quetiapine and risperidone coincided with QTc interval normalization and subsequent recovery.
Ziprasidone literature: Case 1.
Overdose with ziprasidone and bupropion in a 17-year-old male adolescent with psychotic depression led to an ED evaluation.53 One hour after ingesting 120 20-mg tablets of ziprasidone; between 15 and 20 tablets of bupropion sustained release, 150 mg; 15 tablets of clonazepam, 0.5 mg; and 4 tablets of lorazepam, 0.5 mg, the patient was drowsy but responsive to verbal commands. Subsequently, he became stuporous and underwent elective intubation.
The first ECG was normal, with the QTc interval less than 440 ms. The QRS complex widened to 200 ms (presumably from an initial measurement of approximately 80 ms) 2½ hours later. Lidocaine was given intravenously, and the QRS complex was 120 ms and the QTc interval was 480 ms. Subsequent ECGs showed the QTc interval to range between 420 ms and 480 ms with final stabilization at about 440 ms 40 hours after overdose. Electrolytes remained normal, and torsades de pointes did not appear.
The authors referenced a case report by Shrier et al.59 in which a 16-year-old female adolescent ingested 1500 mg of bupropion followed by generalized seizures. Four hours after overdose, an ECG showed a QRS complex of 100 ms and a QTc interval of 600 ms. No torsades de pointes developed.
Based, in part, on the case by Shrier et al,59 Biswas et al.53 pointed out the cardiotoxicity of the combination of ziprasidone and bupropion in overdose. The authors stated that this overdose combination may require several days of careful cardiac monitoring and meticulous management.
1. Commentary. In the 17-year-old patient described by Biswas et al.,53 the initial QTc interval was “less than 440 ms.” How much less, we were not told. Given that the initial QRS complex was described as normal, we may assume it was about 80 ms. Later, the QRS complex widened to 200 ms and then shortened to 120 ms. Thus, the major cardiotoxic effect of the overdose combination of ziprasidone and bupropion related more to slowing of ventricular depolarization than slowing of ventricular repolarization. Slowing of ventricular depolarization by about 40 ms probably accounted for most, if not all, of the QTc interval prolongation of 480 ms. It is slowing of ventricular repolarization that provokes EADs and subsequent torsades de pointes.
Ziprasidone literature: Case 2.
A 50-year-old man with chronic paranoid schizophrenia presented to an ED 4½ hours after overdosing with 3120 mg of ziprasidone.54 An ECG showed a QTc interval of 490 ms that was judged consistent with minimal prolongation. Laboratory testing, including electrolyte measurement, was normal. It is not clear whether the patient started receiving normal saline intravenously at a rate of 8 L/hour before or after the initial ECG. The patient did not develop torsades de pointes.
1. Commentary. Burton and colleagues' notation54 that the patient was administered normal saline at a rate of 8 L/hour is probably a typographical error. Given that the Pfizer 054 study44 showed that ziprasidone was capable of provoking QTc interval prolongation in therapeutic doses, a QTc interval measurement of 490 ms is not surprising when the patient takes more than 3000 mg of ziprasidone at one time. Although Table 1 does not specifically list overdose of drugs associated with QT interval prolongation as a risk factor, it does state that QT interval prolongation is generally dose-dependent. The absence of torsades de pointes in this setting argues for the relative safety of ziprasidone.
DISCUSSION
No cases of drug-induced torsades de pointes have appeared in the literature with the new generation antipsychotic drugs. Because torsades de pointes is such a rare arrhythmia, QTc interval prolongation (surrogate marker) best identifies persons at risk for torsades de pointes.
Tracking Drugs Associated With QTc Interval Prolongation and Torsades de Pointes
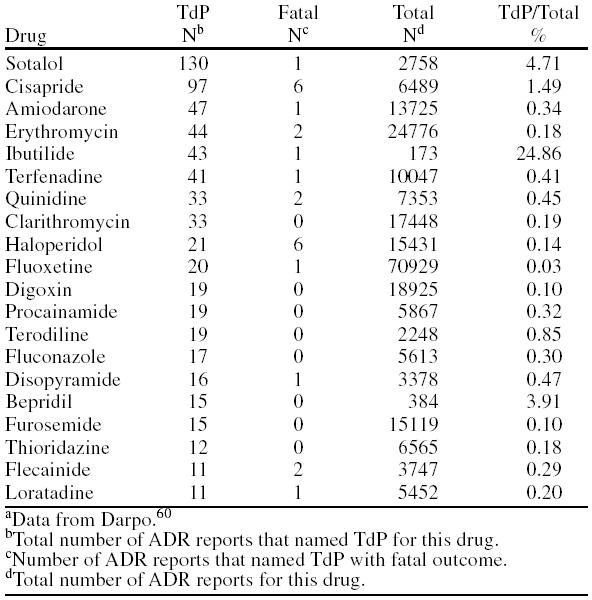
Darpo60 (Table 3) listed the 20 drugs most commonly associated with torsades de pointes according to adverse drug reactions as reported to the World Health Organization between 1983 and 1999. Haloperidol and thioridazine appeared in this list.
Table 3.
Twenty Drugs Most Commonly Associated With Torsades de Pointes (TdP) According to Adverse Drug Reactions (ADR) Reported to World Health Organization, 1983–1999a
The Web site Arizona Cert (http://www.torsades.org) is maintained by Raymond L. Woosley, M.D., Ph.D., and lists drugs that prolong the QT interval and/or induce torsades de pointes. Case reports are an important source of information on the institutionally maintained Web site, and Dr. Woosley is a recognized authority in this area.
For risperidone, quetiapine, and ziprasidone, the Web site states “QT prolongation is mentioned in the FDA-approved labeling as a known action of the drug.”61 No statement is made regarding any of these 3 drugs causing torsades de pointes. Olanzapine is not listed on this Web site as a drug that causes QTc interval prolongation or torsades de pointes. No case reports of QTc interval prolongation associated with olanzapine administration appear in the literature.
Pfizer 054 Study
QT interval changes were investigated for the new generation antipsychotic drugs risperidone, quetiapine, ziprasidone, and olanzapine along with thioridazine and haloperidol in the Pfizer 054 study.44 Thioridazine and ziprasidone were associated with the greatest degree of drug-induced QTc interval prolongation. Haloperidol and olanzapine were associated with the least degree of drug-induced QTc interval prolongation. All 6 drugs induced QTc interval prolongation. Only quetiapine and haloperidol were associated with drug-induced QTc interval prolongation exacerbated by a metabolic inhibitor. Discussed earlier was the observation that quetiapine is the novel antipsychotic drug most commonly associated with increased heart rate, and the Bazett correction formula tends to be less accurate at higher heart rates.
What Have We Learned About QTc Interval Prolongation and New Generation Antipsychotic Drugs?
The 9 case reports reviewed in this article generate many more questions than answers. They document that newer antipsychotic drugs may cause QT interval prolongation. They do not say whether such agents may also cause torsades de pointes. They do not even semiquantitate the risk for torsades de pointes when prescribing such drugs. And, they do not provide agreed upon guidelines for cardiologic evaluation when considering prescribing new generation antipsychotic drugs. These case reports are at least consistent with the Pfizer 054 study findings that risperidone, quetiapine, and ziprasidone may induce QTc interval prolongation.44 At least 8 of the 9 case reports were associated with risk factors for QT interval prolongation and leave uncertain whether, in the absence of risk factors, risperidone, quetiapine, or ziprasidone alone might disrupt the repolarization process sufficient to cause torsades de pointes. In particular, when risk factors are suspected or present, consultation and laboratory studies are indicated. Table 4 describes the relative risk of QTc interval prolongation with common antipsychotic drugs.
Table 4.
Relative Risk of QTc Interval Prolongation With Common Antipsychotic Drugsa
What Lies Ahead?
Current group-derived formulae to correct QT interval measurements to a heart rate of 60 beats per/min (QTc) are unsatisfactory.62 Finding the signal of drug-induced change amid the noise of random variation (regression to the mean) awaits new technology. Changes of less than 20 to 30 ms in serial QTc interval measurements probably do not reach thresholds of clinical significance.
Individual QTc interval measurements optimized for each subject by drug-free QT/R-R regression modeling offers the best hope for establishing baseline data with which drug-induced changes may be compared.62 However, this is an expensive and time consuming process. Multiple ECGs at different heart rates for each person for whom the clinician is considering prescribing a drug associated with QTc interval prolongation will be required. For pharmaceutical companies planning premarketing drug trials, such a practice will add greatly to the cost of bringing new drugs to the marketplace.
CONCLUSION
No new generation antipsychotic drug has been associated with torsades de pointes. All of them have been associated with QTc interval prolongation. In order of comparison data, QTc interval prolongation is greatest with ziprasidone and least with olanzapine. This does not necessarily mean that ziprasidone is any more likely than olanzapine to induce torsades de pointes.
The clinician is largely left with the advice to follow the package insert in prescribing new generation antipsychotic drugs. More precise guidelines await refined measures to correct or normalize the QT interval for individual patients.
Drug names: amantadine (Symmetrel and others), amiodarone (Pacerone, Cordarone, and others), aripiprazole (Abilify), bepridil (Vascor), bupropion (Wellbutrin and others), chlorpromazine (Thorazine, Sonazine, and others), clarithromycin (Biaxin), clonazepam (Klonopin and others), clozapine (Clozaril and others), digoxin (Lanoxin and others), diphenhydramine (Benadryl and others), disopyramide (Norpace and others), droperidol (Inapsine and others), erythromycin (Eryc, PCE, and others), flecainide (Tambocor and others), fluconazole (Diflucan), fluoxetine (Prozac and others), furosemide (Lasix and others), haloperidol (Haldol and others), ibutilide (Corvert), ketoconazole (Nizoral, Ketozole, and others), lidocaine (Xylocaine and others), lorazepam (Ativan and others), lovastatin (Altocor, Mevacor, and others), mesoridazine (Serentil), nortriptyline (Aventyl, Pamelor, and others), olanzapine (Zyprexa), paroxetine (Paxil and others), pimozide (Orap), procainamide (Pronestyl, Procanbid, and others), quetiapine (Seroquel), risperidone (Risperdal), sertraline (Zoloft), sotalol (Betapace, Sorine, and others), topiramate (Topamax), venlafaxine (Effexor), ziprasidone (Geodon).
Footnotes
The author reports no financial affiliation or other relationship relevant to the subject matter of this article.
REFERENCES
- Vieweg WVR, Nicholson CS. Torsade de pointes ventricular tachycardia, QT interval, and psychotropic drugs. Med Update Psychiatrists. 1997;2:48–54. [Google Scholar]
- Reilly JG, Ayis SA, and Ferrier IN. et al. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet. 2000 355:1048–1052. [DOI] [PubMed] [Google Scholar]
- Welch R. Antipsychotic agents and QT changes. J Psych Neurosci. 2000;25:154–160. [PMC free article] [PubMed] [Google Scholar]
- Bednar MM, Harrigan EP, and Anziano RJ. et al. The QT interval. Prog Cardiovas Dis. 2001 43:1–45. [DOI] [PubMed] [Google Scholar]
- DePonti F, Poluzzi E, Montanaro N. Organizing evidence on QT prolongation and occurrence of torsade de pointes with non-antiarrhythmic drugs: a call for consensus. Eur J Clin Pharmacol. 2001;57:185–209. doi: 10.1007/s002280100290. [DOI] [PubMed] [Google Scholar]
- Fayek M, Kingsbury SJ, and Zada J. et al. Cardiac effects of antipsychotic medications. Psychiatr Serv. 2001 52:607–609. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Patel J. Sudden cardiac death and antipsychotic drugs: do we know enough? Arch Gen Psychiatry. 2001;58:1168–1171. doi: 10.1001/archpsyc.58.12.1168. [DOI] [PubMed] [Google Scholar]
- Glassman AH, Bigger JT Jr. Antipsychotic drugs: prolonged QTc interval, Torsade de pointes, and sudden death. Am J Psychiatry. 2001;158:1774–1782. doi: 10.1176/appi.ajp.158.11.1774. [DOI] [PubMed] [Google Scholar]
- Ray WA, Meredith S, and Thapa PB. et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001 58:1161–1167. [DOI] [PubMed] [Google Scholar]
- Reilly JG, Ayis SA, and Ferrier IN. et al. Thioridazine and sudden unexplained death in psychiatric in-patients. Br J Psychiatry. 2002 180:515–522. [DOI] [PubMed] [Google Scholar]
- Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsade de pointes, and sudden death. Drugs. 2002;62:1649–1671. doi: 10.2165/00003495-200262110-00006. [DOI] [PubMed] [Google Scholar]
- Reilly JG, Thomas SHL, Ferrier IN. Recent studies on ECG changes, antipsychotic use, and sudden death in psychiatric patients. Psychiatr Bull R Coll Psychiatr. 2002;26:110–112. [Google Scholar]
- Hennessy S, Bilker WB, and Knauss JS. et al. Cardiac arrest and ventricular arrhythmia in patients taking antipsychotic drugs: cohort study using administrative data. BMJ. 2002 325:1070–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herxheimer A, Healy D. Arrhythmias and sudden death in patients taking antipsychotic drugs. BMJ. 2002;325:1253–1254. doi: 10.1136/bmj.325.7375.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodnick PJ, Jerry J, Parra F. Psychotropic drugs and the ECG: focus on the QTc interval. Expert Opin Pharmacother. 2001;3:479–498. doi: 10.1517/14656566.3.5.479. [DOI] [PubMed] [Google Scholar]
- DePonti F, Poluzzi E, and Cavalli A. et al. Safety of non-antiarrhythmic drugs that prolong the QT interval or induce torsade de pointes. An overview. Drug Saf. 2002 25:263–286. [DOI] [PubMed] [Google Scholar]
- Vieweg WVR. Mechanisms and risks of electrocardiographic QT interval prolongation when using antipsychotic drugs. J Clin Psychiatry. 2002 63suppl 9. 18–24. [PubMed] [Google Scholar]
- Vieweg WVR. Strategies to prevent fatal arrhythmias in patients taking antipsychotics. Current Psychiatry. 2002;1:10–21. [Google Scholar]
- Al-Khatib SM, LaPointe NMA, and Kramer JM. et al. What clinicians should know about the QT interval. JAMA. 2003 289:2120–2127. [DOI] [PubMed] [Google Scholar]
- Roe CM, Odell KW, Henderson RR. Concomitant use of antipsychotics and drugs that may prolong the QT interval. J Clin Psychopharmacol. 2003;23:197–200. doi: 10.1097/00004714-200304000-00013. [DOI] [PubMed] [Google Scholar]
- Curtis LH, Ostbye T, and Sendersky V. et al. Prescription of QT-prolonging drugs to a cohort of about 5 million outpatients. Am J Med. 2003 114:135–141. [DOI] [PubMed] [Google Scholar]
- Elming H, Sonne J, Lublin HKF. The importance of the QT interval: a review of the literature. Acta Psychiatr Scand. 2003;107:96–101. doi: 10.1034/j.1600-0447.2003.00061.x. [DOI] [PubMed] [Google Scholar]
- Taylor DM. Antipsychotics and QT prolongation. Acta Psychiatr Scand. 2003;107:85–95. doi: 10.1034/j.1600-0447.2003.02078.x. [DOI] [PubMed] [Google Scholar]
- Viskin S, Justo D, and Halkin A. et al. Long QT syndrome caused by noncardiac drugs. Prog Cardiovasc Dis. 2003 45:415–427. [DOI] [PubMed] [Google Scholar]
- Vieweg WVR, McDaniel NL. Drug-induced QT interval prolongation and torsade de pointes in children and adolescents, pt 1. Child and Adolescent Psychopharmacology News. 2003;8(1):1–7. [Google Scholar]
- Vieweg WVR, McDaniel NL. Drug-induced QT interval prolongation and torsade de pointes in children and adolescents, pt 2. Child and Adolescent Psychopharmacology News. 2003;8(2):1–5. [Google Scholar]
- Vieweg WVR, McDaniel NL. Drug-induced QT interval prolongation and torsade de pointes in children and adolescents, pt 3. Child and Adolescent Psychopharmacology News. 2003;8(3):1–4. [Google Scholar]
- Vieweg WVR, McDaniel NL. Drug-induced QT interval prolongation and torsade de pointes in children and adolescents, pt 4. Child and Adolescent Psychopharmacology News. 2003;8(4):1–4. [Google Scholar]
- Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–370. [Google Scholar]
- Zareba W, Moss AJ, and Le Cessie S. et al. Risk of cardiac events in family members of patients with long QT syndrome. J Am Coll Cardiol. 1995 26:1685–1691. [DOI] [PubMed] [Google Scholar]
- Fu EY, Clemo HF, Ellenbogen KA. Acquired QT prolongation: mechanisms and implications. Cardiol Rev. 1998;6:319–324. doi: 10.1097/00045415-199811000-00007. [DOI] [PubMed] [Google Scholar]
- Tan HL, Hou CJ, and Lauer MR. et al. Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med. 1995 122:701–714. [DOI] [PubMed] [Google Scholar]
- Yap YG, Camm J. Risk of torsade de pointes with non-cardiac drugs. BMJ. 2000;320:1158–1159. doi: 10.1136/bmj.320.7243.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehnert MT, Lovejoy FH Jr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313:474–479. doi: 10.1056/NEJM198508223130804. [DOI] [PubMed] [Google Scholar]
- Browne K, Prystowsky E, and Heger JJ. et al. Prolongation of the QT interval in man during sleep. Am J Cardiol. 1983 52:55–59. [DOI] [PubMed] [Google Scholar]
- Morganroth J, Brozovich FV, and McDonald JT. et al. Variability of the QT measurement in healthy men, with implications for selection of an abnormal QT value to predict drug toxicity and proarrhythmia. Am J Cardiol. 1991 67:774–776. [DOI] [PubMed] [Google Scholar]
- Woosley R, Sketch MH. Gender and Drug-Induced Torsade de Pointes. ACCEL 30, No. 2. Bethesda, Md: American College of Cardiology. 1998 [Google Scholar]
- Rodriguez I, Kilborn MJ, and Liu XK. et al. Drug-induced QT prolongation in women during the menstrual cycle. JAMA. 2001 285:1322–1326. [DOI] [PubMed] [Google Scholar]
- Khan SP, Dahlvani S, and Vieweg WVR. et al. Electrocardiographic QT interval in a geropsychiatric inpatient population: a preliminary study. Med Psychiatr. 1998 1:71–74. [Google Scholar]
- Compton SJ, Lux RL, and Ramsey MR. et al. Genetically defined therapy of inherited long-QT syndrome: correction of abnormal repolarization by potassium. Circulation. 1996 94:1018–1022. [DOI] [PubMed] [Google Scholar]
- Hatta K, Takahashi T, and Nakamura H. et al. Hypokalemia and agitation in acute psychotic patients. Psychiatry Res. 1999 86:85–88. [DOI] [PubMed] [Google Scholar]
- Hatta K, Takahashi T, and Nakamura H. et al. Prolonged QT interval in acute psychotic patients. Psychiatry Res. 2000 94:279–285. [DOI] [PubMed] [Google Scholar]
- Niewinski P, Orzechowska-Juzwenko K, Hurkack M. CYP2D6 extensive, intermediate, and poor phenotypes and genotypes in a Polish population. Eur J Clin Pharmacol. 2002;58:533–535. doi: 10.1007/s00228-002-0505-y. [DOI] [PubMed] [Google Scholar]
- US Food and Drug Administration Advisory Committee. Zeldox Capsules (ziprasidone): Summary of Efficacy and Safety and Overall Benefit Risk Relationship. Bethesda, Md: US Food and Drug Administration. 19July2000 [Google Scholar]
- Vincent GM. Long QT syndrome. Cardiol Clin. 1999;18:309–325. doi: 10.1016/s0733-8651(05)70143-0. [DOI] [PubMed] [Google Scholar]
- Brown K, Levy H, and Brenner C. et al. Overdose of risperidone. Ann Emerg Med. 1993 22:1908–1910. [DOI] [PubMed] [Google Scholar]
- Ravin DS, Levenson JW. Fatal cardiac event following initiation of risperidone therapy. Ann Pharmacother. 1997;31:867–870. doi: 10.1177/106002809703100712. [DOI] [PubMed] [Google Scholar]
- Gesell LB, Stephen M. Toxicity following a single dose of risperidone for pediatric attention deficit hyperactivity disorder (ADHD) J Toxicol Clin Toxicol. 1997;35:549. [Google Scholar]
- Gajwani P, Pozuelo L, Tesar GE. QT interval prolongation associated with quetiapine (Seroquel) overdose. Psychosomatics. 2000;41:63–65. doi: 10.1016/S0033-3182(00)71175-3. [DOI] [PubMed] [Google Scholar]
- Hustey F. Acute quetiapine poisoning. J Emerg Med. 1999;17:995–997. doi: 10.1016/s0736-4679(99)00128-6. [DOI] [PubMed] [Google Scholar]
- Furst BA, Champion KM, and Pierre JM. et al. Possible association of QTc interval prolongation with co-administration of quetiapine and lovastatin. Biol Psychiatry. 2002 51:264–265. [DOI] [PubMed] [Google Scholar]
- Beelen AP, Yeo K-TJ, Lewis LD. Asymptomatic QTc prolongation associated with quetiapine fumarate overdose in a patient being treated with risperidone. Hum Exp Toxicol. 2001;20:215–219. doi: 10.1191/096032701678766778. [DOI] [PubMed] [Google Scholar]
- Biswas AK, Zabrocki LA, and Mayes KL. et al. Cardiotoxicity associated with intentional ziprasidone and bupropion overdose. J Toxicol Clin Toxicol. 2003 41:79–82. [DOI] [PubMed] [Google Scholar]
- Burton S, Heslop K, and Harrison K. et al. Ziprasidone overdose. Am J Psychiatry. 2000 157:835. [DOI] [PubMed] [Google Scholar]
- Heykants J, Huang M-L, and Mannens G. et al. The pharmacokinetics of risperidone in humans: a summary. J Clin Psychiatry. 1994 55(suppl). 13–17. [PubMed] [Google Scholar]
- Lo Vecchio F, Hamilton RJ, Hoffman RJ. Risperidone overdose. Am J Emerg Med. 1996;14:95–96. doi: 10.1016/s0735-6757(96)90026-1. [DOI] [PubMed] [Google Scholar]
- Geller W, Smith M, and Winter H. et al. In response to Furst et al, “Possible association of QTc interval prolongation with co-administration of quetiapine and lovastatin” [letter]. Biol Psychiatry. 2002 52:914. [DOI] [PubMed] [Google Scholar]
- Pierre JM, Wirshing DA, Wirshing WC. Reply [letter] Biol Psychiatry. 2002;52:914–915. [Google Scholar]
- Shrier M, Diaz JE, Tsarouhas N. Cardiotoxicity associated with bupropion overdose. Ann Emerg Med. 2000;35:100. doi: 10.1016/s0196-0644(00)70119-3. [DOI] [PubMed] [Google Scholar]
- Darpo B. Spectrum of drugs prolonging QT interval and the incidence of torsade de pointes. Eur Heart J Suppl. 2001 3suppl K. K70–K80. [Google Scholar]
- The University of Arizona Health Sciences Center. Arizona CERT. QT Drug Lists. Available at: http://www.torsades.org/medical-pros/drug-lists/browse-drug-list.cfm. Accessed Aug 21, 2003. [Google Scholar]
- Malik M. Problems of heart rate correction in assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol. 2001;12:411–420. doi: 10.1046/j.1540-8167.2001.00411.x. [DOI] [PubMed] [Google Scholar]