Abstract
To study the use of health services before death for different causes, a 6-year file of Medicare use and cost data was linked to a file of death certificate information for persons dying at ages 65 years or over in 1979. Patterns of medical care use during the last years of life varied substantially by cause of death, reflecting the degree of chronicity of the disease that resulted in death and the nature of treatment. Persons dying of nephritis, chronic obstructive pulmonary disease, and diabetes mellitus incurred consistently high expenses for 6 years before death. Costs for cancer decedents were also high, especially in the last 2 years of life. Persons in their last 2 years of life have a considerable impact on Medicare expenses. An estimated 13 percent of annual Medicare expenses were attributable to persons who were within 2 years of death from heart disease and 10.7 percent to persons who were within 2 years of death from cancer.
Introduction
For the most common causes of death (i.e., heart disease, cancer, and stroke) the nature of the condition means that death is often preceded by years of illness and decline. Because of advances in the treatment of such chronic diseases, some people use a substantial amount of medical care for long periods of time before death. Consequently, medical care services received in the last year of life may often represent only a portion of the total care received during the course of a terminal illness. Services rendered to chronically ill patients in the last several years of life may have a considerable impact on health care expenditures.
In this study we examined Medicare use by cause of death for 6 years before death. We addressed the following questions regarding the patterns of care received in the last years of life:
At what time before death do beneficiaries begin to receive higher than average amounts of services?
How much and what kinds of services do they receive as they approach death and does the quantity of services differ by cause of death?
What causes of death have the greatest dollar impact on Medicare expenditures?
Most earlier studies of use of care by the dying have been limited to the last year or two of life. An exception was a study by Roos et al. (1987) that went back beyond the last year or two of life to examine the utilization experience for 4 years before death of 4,263 decedents who were covered in the Manitoba provincial health insurance system. Health care usage was above average for several years before death, with a shorter period of increased usage prior to death among the oldest decedents. The major increase in hospital usage occurred in the year before death, whereas there were large, regular increases in the number of nursing home days in each of the 4 years prior to death.
Previous studies of Medicare beneficiaries have found that expenses for persons in their last year of life are a large component of total Medicare expenditures. Decedents, who comprised approximately 6 percent of the Medicare population 67 years of age or over in 1978, accounted for 28 percent of Medicare reimbursements in their last 12 months of life (Lubitz and Prihoda, 1984). Among persons dying of the three major causes of death, those dying of malignant neoplasms have the highest per capita Medicare expenses in the last year of life—about twice the expenses of persons dying of heart disease and stroke (Riley et al., 1987). Because heart disease is by far the leading cause of death, however, more Medicare dollars are accounted for by heart disease decedents than by persons dying of any other cause, including cancer.
Methods
The study population consists of a 5-percent national probability sample of Medicare beneficiaries 65 years of age or over who died in 1979. Because it is estimated that at least 95 percent of the total population 65 years of age or over is covered by Medicare, Medicare data give a good picture of the aged in general.
Data on demographic characteristics such as age and sex and on use and cost of Medicare services come from the Continuous Medicare History Sample (CMHS). The CMHS is a longitudinal research file with data on a 5-percent sample of Medicare enrollees, with sample selection based on the last two digits of the beneficiary's Medicare number. New enrollees whose Medicare numbers place them in the sample are added to the file, and the records of enrollees who die are retained. The file contains demographic and entitlement information and information on the use of Medicare-covered services. Included is summary information on annual use of physician, hospital outpatient, and home health services and selected information on all inpatient hospital and skilled nursing facility (SNF) stays. Using this longitudinal file, we were able to track Medicare utilization and expenses retrospectively to 1974 for individuals who died in 1979. In 1979, there were approximately 1,300,000 aged enrollees in the file.
The use-and-cost data in the CMHS reflect only Medicare-covered services and Medicare payments for these services. Services of importance to the aged that are not covered by Medicare are nursing home care below the skilled level and outpatient prescription drugs. These services are mostly paid for by the Medicaid program or by the beneficiaries themselves. Medicare pays only 2 percent of nursing home costs for the aged population (Waldo et al., 1986). Scitovsky (1989), presenting expenditure data on 261 decedents who had been treated at the Palo Alto Medical Clinic, found that nursing home expenses constituted a substantial part of medical care costs in the last year of life, particularly for the very old and for those who were functionally impaired. Roos et al. (1987) also found that nursing home expenditures constituted a major portion of health care expenses for the oldest decedents in Manitoba and that nursing home use increased substantially in each of the 4 years before death for all age groups.
In order to obtain information on underlying cause of death for the decedents in the CMHS, Medicare data were linked to the National Death Index (NDI) and to the Mortality Statistics File, both maintained by the National Center for Health Statistics (NCHS). Cause of death was obtained for 58,382 individuals, or 92 percent of the aged decedents in our sample. Two percent of the nonmatches were attributable to one State that did not grant permission for the linkage of its death certificate records to Medicare files. Special permission had to be obtained from each State to link death certificate data in the NCHS files from that State to Medicare data. Because of the time and effort involved in obtaining permission from 50 States, the linkage was done only for 1979. That is why a linked file with more recent data is not available.
The cause of death for the 8 percent of Medicare decedents in the CMHS who did not match to NCHS data is not known. Consequently, estimates of total numbers of decedents and total program reimbursements by cause of death will be understated for individual causes to the extent that data related to the 8 percent of nonmatches should be distributed among the specific causes of death. Prorating Medicare expenses among the various causes of death was considered but rejected because the nonmatching population was atypical in several respects. Most of the nonmatches were women, and they tended to be older than the other decedents. Nonmatches also had lower average reimbursement and utilization rates than did all decedents combined. This suggests that the cause-of-death mix for nonmatches may be different from that of the other decedents.
All cost and utilization data are summarized by calendar year. For example, costs in the last calendar year of life reflect costs in 1979 for people who died in 1979. Use and costs were not summarized on an individual basis by 12-month periods before death (as in the 1984 Lubitz and Prihoda article) because the gain in the precision of the use-and-cost estimates would not be sufficient for most years of the study to justify the additional programming time and resources required. (However, aggregate costs are estimated for the last 12 and 24 months of life later in this article.) Consequently, decedents had, on average, only 6 months of Medicare exposure in 1979, their last calendar year of life, whereas comparison group members (defined later) averaged nearly 12 months. It is estimated that about 70 percent of costs in the last 12 months are captured when costs are computed in the last calendar year of life. Similarly, data on the years prior to the calendar year of death are organized by calendar year. For example, data for the year prior to the year of death represent costs in 1978 for people who died anytime in 1979.
Medicare beneficiaries dying before the age of 70 usually have less than 6 years of exposure in the Medicare files. They are excluded from table entries involving the years before they attained age 65. For example, persons dying at age 67 would contribute to the data on Medicare use or costs only in the last 3 calendar years of life.
One-percent samples of all aged persons entitled in each of the years 1974 through 1979 were selected from the CMHS to serve as comparison groups. This selection of annual cross-sectional samples of aged beneficiaries allowed a comparison of average reimbursements for 1979 decedents for various years before death to average Medicare expenses for each of those years. This was done by forming ratios of average cause-of-death-specific reimbursements to average reimbursements for all aged beneficiaries in a given year (including both survivors and decedents). These ratios will be referred to as “reimbursement ratios.” A reimbursement ratio above 1 indicates that per capita expenses for a given cause of death were above the Medicare average for a given year. Use of reimbursement ratios controls for the effect of inflation and provides a baseline for assessing the magnitude of decedents' per capita costs. It also facilitates comparisons among causes of death. For 1979, the reimbursement ratio implicitly compares decedents' costs in their last calendar year, which on the average includes only 6 months, with the per capita reimbursement of all Medicare enrollees in 1979, which for most enrollees includes 12 months of entitlement. Two-tailed t-tests were conducted to ascertain whether reimbursement ratios were statistically significantly different than 1 using methods described in the “Technical note.” All data in this article are national estimates, not sample counts.
Findings
Table 1 contains national estimates of the number of aged Medicare beneficiaries dying of specific causes in 1979. In 1979, an estimated 1.27 million Medicare beneficiaries 65 years of age or over died. This was 4.9 percent of all aged beneficiaries. Heart disease accounted for the most deaths (40.9 percent), followed by malignant neoplasms (18.0 percent) and cerebrovascular diseases (10.5 percent).
Table 1. Number and percent distribution of aged Medicare decedents, by cause of death: 1979.
| Survival status, cause of death, and ICD-9-CM code(s) | Number in thousands | Percent of decedents |
|---|---|---|
| All aged | 25,855 | — |
| Survivors | 24,580 | — |
| Decedents | 1,275 | 100.0 |
| Malignant neoplasms, including neoplasms of lymphatic and hematopoietic tissues (140-208) | 230 | 18.0 |
| Digestive organs and peritoneum (150-159) | 70 | 5.5 |
| Respiratory and intrathoracic organs (160-165) | 54 | 4.2 |
| Breast (174-175) | 15 | 1.2 |
| Diabetes mellitus (250) | 20 | 1.6 |
| Major cardiovascular diseases (390-448) | 699 | 54.9 |
| Diseases of heart (390-398, 402, 404-429) | 521 | 40.9 |
| Ischemic heart disease (410-414) | 395 | 31.0 |
| Acute myocardial infarction (410) | 200 | 15.7 |
| Old myocardial infarction and other forms of chronic ischemic heart disease (412,414) | 192 | 15.1 |
| Cerebrovascular diseases (430-438) | 134 | 10.5 |
| Cerebral thrombosis and unspecified occlusion of cerebral arteries (434.0,434.9) | 31 | 2.4 |
| Atherosclerosis (440) | 25 | 2.0 |
| Pneumonia (480-486) | 32 | 2.5 |
| Chronic obstructive pulmonary diseases and allied conditions (490-496) | 37 | 2.9 |
| Chronic liver disease and cirrhosis (571) | 8 | 0.6 |
| Nephritis, nephrotic syndrome, and nephrosis (580-589) | 11 | 0.9 |
| Accidents and adverse effects (E800-E949) | 21 | 1.6 |
| All other causes | 110 | 8.6 |
| Cause unknown (nonmatches) | 107 | 8.4 |
NOTE: Estimates are based on a national 5–percent sample of aged beneficiaries who died in 1979, and a 0.4–percent sample of all aged persons enrolled in Medicare on December 31, 1979. Sample counts are inflated to estimate totals. ICD-9-CM is International Classification of Diseases, 9th Revision, Clinical Modification, 1980.
SOURCE: For 1979 decedents: The Continuous Medicare History Sample (CMHS) of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics. For all other beneficiaries, data from the CMHS.
Reimbursement ratios
Decedents had expenses for all Medicare-covered services that were 4.31 times above the average in the last calendar year of life (Table 2).1 The reimbursement ratio for decedents was 2.60 in the first calendar year prior to the year of death, declining to 1.61 in the second calendar year prior to the year of death. This indicates that the heaviest use of services is generally during the last 2 calendar years of life. In the fifth calendar year prior to the year of death, the reimbursement ratio for all decedents was 1.02—not significantly different from average.
Table 2. Reimbursement ratios for aged Medicare decedents who died in 1979, by cause of death and calendar year prior to death: All covered services, 1974-79.
| Cause of death | Calendar year prior to death | Year of death 1979 | 6 years combined1 | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| 5th year 1974 | 4th year 1975 | 3rd year 1976 | 2nd year 1977 | 1st year 1978 | |||
| All decedents | 1.02 | 21.16 | 21.32 | 21.61 | 22.60 | 24.31 | 21.98 |
| Malignant neoplasms | 20.90 | 1.03 | 21.30 | 21.82 | 23.92 | 26.62 | 22.57 |
| Digestive organs | 0.86 | 0.91 | 21.23 | 21.84 | 23.79 | 26.63 | 22.56 |
| Respiratory organs | 20.83 | 0.95 | 1.11 | 21.36 | 23.59 | 26.57 | 22.34 |
| Breast | 1.09 | 1.21 | 21.75 | 22.48 | 24.30 | 26.04 | 22.70 |
| Diabetes mellitus | 21.62 | 21.67 | 21.84 | 22.27 | 23.13 | 24.66 | 22.47 |
| Major cardiovascular diseases | 1.04 | 21.17 | 21.30 | 21.50 | 22.16 | 23.38 | 21.73 |
| Diseases of heart | 1.03 | 21.20 | 21.33 | 21.52 | 22.19 | 23.26 | 21.72 |
| Ischemic heart disease | 1.04 | 21.19 | 21.34 | 21.53 | 22.15 | 23.11 | 21.69 |
| Acute myocardial infarction | 0.92 | 1.04 | 21.15 | 21.29 | 21.80 | 22.54 | 21.40 |
| Old acute myocardial infarction | 21.15 | 21.33 | 21.54 | 21.77 | 22.51 | 23.71 | 21.99 |
| Cerebrovascular disease | 1.05 | 1.08 | 21.24 | 21.43 | 22.07 | 23.68 | 21.76 |
| Cerebral thrombosis | 1.21 | 1.04 | 1.17 | 21.43 | 22.21 | 23.88 | 21.81 |
| Atherosclerosis | 0.99 | 1.07 | 1.07 | 21.51 | 22.00 | 23.21 | 21.66 |
| Pneumonia | 1.21 | 21.33 | 21.41 | 21.67 | 22.64 | 24.09 | 22.08 |
| Chronic obstructive pulmonary diseases | 21.33 | 21.55 | 21.87 | 22.47 | 23.83 | 25.76 | 22.75 |
| Chronic liver disease | 1.19 | 1.25 | 1.33 | 1.48 | 22.96 | 26.36 | 22.22 |
| Nephritis | 1.13 | 21.61 | 22.12 | 22.67 | 24.20 | 26.75 | 23.10 |
| Accidents | 0.77 | 0.95 | 1.01 | 1.06 | 21.51 | 24.16 | 21.56 |
| Other | 1.01 | 21.20 | 21.36 | 21.61 | 22.67 | 25.15 | 22.15 |
| Cause unknown (nonmatch) | 0.95 | 1.02 | 21.15 | 21.40 | 22.15 | 23.60 | 21.71 |
Beneficiaries dying before attaining 70 years of age have less than 6 years exposure under Medicare. Reimbursements for 6 years combined were computed in 1979 dollars.
Significantly different from 1 at the .0025 level.
NOTES: The reimbursement ratio is the ratio of average reimbursement per decedent in a particular cause-of-death group to average reimbursement per enrollee for all aged Medicare enrollees. Complete cause-of-death titles and codes from the International Classification of Diseases, 9th Revision, Clinical Modification, 1980, are given in Table 1.
SOURCE: The Continuous Medicare History Sample of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics.
There was considerable variation among the various causes with respect to patterns of expense over time. Among the major causes of death, malignant neoplasms exhibited the highest reimbursement ratios in the year of death (6.62) and the first calendar year prior to the year of death (3.92). Reimbursement ratios for cancer decedents decreased rapidly for preceding years, however, and the ratio in the fifth calendar year prior to the year of death was only 0.90. (Reimbursement ratios were below 1 for some causes in the fourth and fifth calendar years before the year of death. The reason is probably that, for 1979 decedents, the years before death include expenses of survivors only, by definition.) An exception to this pattern for cancer in general was breast cancer, which had a reimbursement ratio of 1.21 in the fourth calendar year prior to the year of death and 1.09 in the fifth year. Heart disease decedents had relatively low reimbursement ratios in the last 3 calendar years of life (3.26, 2.19, and 1.52). Beneficiaries dying of acute myocardial infarction (AMI) had the lowest ratio in the calendar year of death (2.54), which is consistent with the Roos et al. (1987) finding that many low users of services died of AMI. Persons dying of cerebrovascular diseases also had relatively low reimbursement ratios in the last 3 calendar years of life (3.68, 2.07, and 1.43).
Persons dying of diabetes mellitus, chronic obstructive pulmonary disease (COPD), pneumonia, chronic liver disease, and nephritis showed patterns of high use of services over a long period of time. Persons dying of diabetes mellitus exhibited a reimbursement ratio of 1.62 in the fifth year prior to the year of death; this ratio rose slowly with time to 4.66 in the last calendar year. Persons dying of COPD also exhibited a pattern of high chronic use over time, with a reimbursement ratio of 1.33 in the fifth year before the year of death, rising to 5.76 in the last calendar year.
The last column of Table 2 indicates which causes of death were most costly on a per capita basis during the entire 6-year period before death. The numbers in this column are the ratio of the average 6-year costs (inflation adjusted) for 1979 decedents to the average costs for the general Medicare population during the 1974-79 period. (Beneficiaries dying at ages under 71 years, who comprise approximately 22 percent of decedents, were included in the last column although they had less than 6 years of exposure under Medicare.) Nephritis and COPD decedents were most expensive with reimbursement ratios of 3.10 and 2.75, respectively, because of their consistently high use of services in the 6-year period. Persons dying of malignant neoplasms were also relatively costly (a reimbursement ratio of 2.57), primarily on the basis of their high expenses in the last 2 calendar years of life. Heart disease and cerebrovascular disease decedents incurred relatively low costs on a per capita basis over the 6 years with reimbursement ratios of 1.72 and 1.76, respectively.
Hospital and physician services
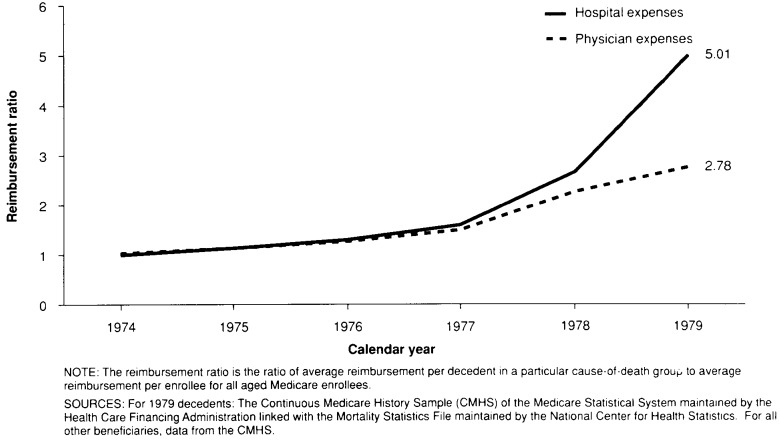
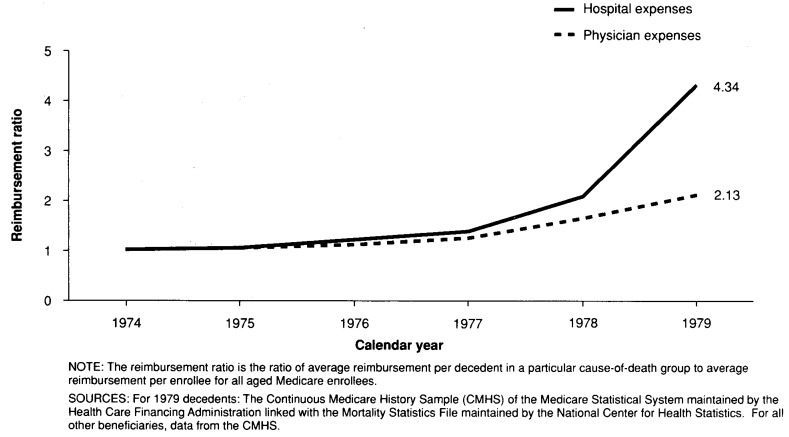
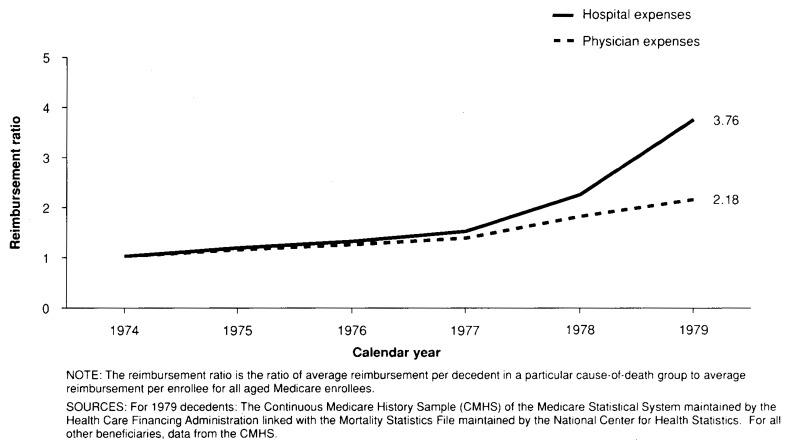
Patterns of inpatient hospital reimbursements differed markedly from patterns of physician reimbursements in the last 2 calendar years of life (Figures 1-4). Inpatient hospital and physician services are the two largest components of Medicare expense, accounting for 67 percent and 25 percent, respectively, of Medicare reimbursements in 1979.
Figure 1. Reimbursement, ratios for aged Medicare decedents who died in 1979, by hospital and physician expenses: All causes, 1974-79.
Figure 4. Reimbursement ratios for aged Medicare decedents who died in 1979, by hospital and physician expenses: Stroke, 1974-79.
Among all decedents, reimbursement ratios for inpatient hospital expenses (5.01) were much higher than for physician expenses (2.78) in the last calendar year of life (Figure 1). The reimbursement ratio for inpatient hospital services was also higher in the calendar year prior to the year of death, though by a lesser amount (2.66 versus 2.26). For earlier years, reimbursement ratios for inpatient hospital and physician services were similar. For the three major causes of death, reimbursement ratios for inpatient hospital services were higher than the ratios for physician services in each of the last 2 calendar years (Figures 2-4). Cancer decedents exhibited the largest difference in reimbursement ratios in the last calendar year (7.68 versus 4.28) and the smallest difference in the calendar year prior to the year of death (3.95 versus 3.72).
Figure 2. Reimbursement ratios for aged Medicare decedents who died in 1979, by hospital and physician expenses: Heart disease, 1974-79.
The costs attributed to cancer decedents were high largely because a very high percent of them were hospitalized in the last and next to last calendar years of life (Table 3). In the last calendar year of life, 86 percent of cancer decedents were hospitalized; and in the first calendar year before the year of death, 53 percent were hospitalized. On the other hand, the percents of persons hospitalized in the fourth and fifth calendar years before the year of death were relatively low for cancer decedents, very likely reflecting that many of the cancer patients who died in 1979 were not yet manifesting symptoms of their disease in 1974 and 1975. A total of 61 percent of heart disease decedents were hospitalized in the calendar year of death, and only 38 percent were hospitalized in the first calendar year prior to the year of death. The percent of stroke decedents hospitalized was very similar to the percent hospitalized for heart disease decedents, with the exception of the calendar year of death, when 72 percent of stroke victims entered the hospital.
Table 3. Percent hospitalized among aged Medicare beneficiaries who died in 1979, by year and selected major causes of death: 1974-79.
| Cause of death | Calendar year prior to death | Year of death 1979 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 5th year 1974 | 4th year 1975 | 3rd year 1976 | 2nd year 1977 | 1st year 1978 | ||
|
| ||||||
| Percent | ||||||
| All causes | 22 | 24 | 27 | 31 | 41 | 69 |
| Heart disease | 22 | 25 | 27 | 30 | 38 | 61 |
| Malignant neoplasms | 20 | 22 | 26 | 32 | 53 | 86 |
| Cerebrovascular disease | 24 | 25 | 27 | 30 | 37 | 72 |
NOTE: Complete cause-of-death titles and codes from the International Classification of Diseases, 9th Revision, Clinical Modification, 1980, are given in Table 1.
SOURCE: The Continuous Medicare History Sample of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics.
In the last 2 calendar years of life, 25.9 percent of all decedents were hospitalized with a principal diagnosis of heart disease, reflecting the high frequency of this condition among the elderly (Table 4). Among heart disease decedents, 39.9 percent were hospitalized for heart disease in their last 2 calendar years. More than 72 percent of cancer decedents were hospitalized with a principal diagnosis of cancer in their last 2 calendar years.
Table 4. Percent hospitalized for selected conditions in the last 2 calendar years of life among aged Medicare beneficiaries who died in 1979, by selected major causes of death: 1978-79.
| Cause of death | Percent hospitalized | Reason for hospitalization | ||
|---|---|---|---|---|
|
| ||||
| Heart disease | Cancer | Cerebrovascular disease | ||
|
| ||||
| Percent | ||||
| All causes | 78.8 | 25.9 | 16.4 | 11.6 |
| Heart disease | 73.0 | 39.9 | 3.6 | 8.8 |
| Cancer | 92.7 | 8.8 | 72.2 | 3.3 |
| Cerebrovascular disease | 81.2 | 17.2 | 2.8 | 44.5 |
NOTES: Reason for hospitalization is the principal diagnosis associated with the hospital stay. Complete cause-of-death titles and codes from the International Classification of Diseases, 9th Revision, Clinical Modification, 1980, are given in Table 1. Table includes persons at least 67 years of age at time of death in 1979.
SOURCE: The Continuous Medicare History Sample of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics.
Hospitalization for reasons different from the cause of death reflect a considerable rate of comorbidity among this population. For example, 17.2 percent of cerebrovascular disease decedents were hospitalized with a principal diagnosis of heart disease in their last 2 calendar years. Nearly 9 percent of cancer decedents were hospitalized for heart disease, and nearly 9 percent of heart disease decedents were hospitalized for cerebrovascular disease. Relatively few (less than 4 percent) of heart disease and cerebrovascular disease decedents were hospitalized for cancer in their last 2 calendar years, however.
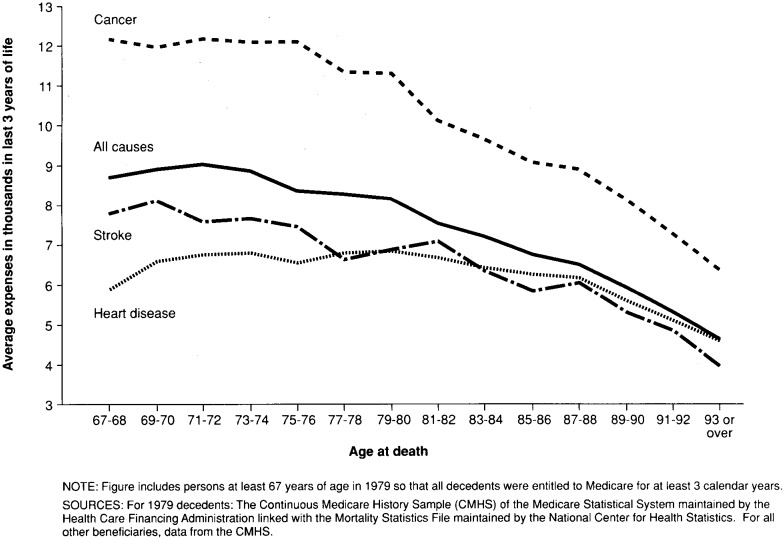
Age patterns
Medicare expenses in the last year of life have been found to decline with increasing age for most major causes of death (Riley et al., 1987). In particular, expenses for decedents 85 years of age or over were found to be substantially lower than those for decedents in other age groups for most causes of death. The impact of age on expenses among decedents is shown graphically in Figure 5. Inflation-adjusted Medicare expenses over the last 3 calendar years of life are plotted against age at death. In order to make sure all decedents in the figure would have 3 years of Medicare exposure, only persons dying at age 67 years or over were included. Among all causes, expenses are relatively level from ages 67 years to 74 years, after which they decline steadily. Among cancer decedents a similar pattern prevails, but the decline in expenses after age 76 is somewhat sharper. For heart disease decedents, expenses do not begin to decrease substantially until after age 88.
Figure 5. Average Medicare expenses in the last 3 calendar years of life for aged Medicare decedents who died in 1979, by age and cause of death: 1977-79.
Number of high-cost years
Over the 6 calendar years before death, many different patterns of utilization are possible for a given overall level of Medicare reimbursements. Some decedents may incur most expenses in a single calendar year; others may exhibit relatively stable or slowly rising levels of expenditure over time. In order to identify typical individual expenditure patterns, the number of high-cost years experienced by the decedent sample in the 6 years before death was examined. A high-cost year was defined as a calendar year in which the Medicare reimbursements incurred by a given individual were above the Medicare program average for all aged beneficiaries. Because Medicare costs are highly skewed, persons incurring an “average” amount of Medicare expenses were at the 81st percentile of expenses in 1982. In order to ensure 6 calendar years of Medicare exposure, only persons dying at age 70 or over were included in this particular analysis.
Although average expenses incurred by our sample of decedents tended to be higher than the Medicare average for several calendar years before death, most individuals had fewer than 3 years of higher than average expenses in the 6 calendar years before death (Table 5). Sixteen percent of the decedents had no years in which their Medicare expenses exceeded the Medicare average, and more than one-half had only one or two high-cost years. Fifteen percent had 4 or more high-cost years. Only 5 percent of cancer decedents had no high-cost years, compared with 20 percent of heart disease decedents and 14 percent of cerebrovascular disease decedents.
Table 5. Percent distribution of aged Medicare beneficiaries who died in 1979, by the number of high-cost years experienced in the last 6 calendar years of life for selected major causes of death: 1974-79.
| Cause of death | Number of high-cost years | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Total | 6 | 5 | 4 | 3 | 2 | 1 | 0 | |
|
| ||||||||
| Percent distribution | ||||||||
| All causes | 100 | 2 | 4 | 9 | 16 | 25 | 27 | 16 |
| Heart disease | 100 | 1 | 4 | 8 | 15 | 24 | 27 | 20 |
| Cancer | 100 | 1 | 5 | 10 | 22 | 30 | 26 | 5 |
| Cerebrovascular disease | 100 | 1 | 4 | 8 | 16 | 26 | 31 | 14 |
NOTES: Includes only decedents 70 years of age or over at time of death so that all decedents in the table were entitled to Medicare during at least 6 calendar years before death. Numbers may not add to total because of rounding. Complete cause-of-death titles and codes from the International Classification of Diseases, 9th Revision, Clinical Modification, 1980, are given in Table 1.
SOURCE: The Continuous Medicare History Sample of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics.
Program impact
The impact of the major causes of death on total Medicare expenditures for the aged is indicated in Table 6. The estimated percents of annual Medicare expenditures for the aged that are associated with care rendered in the last 12 months (column 1) and last 24 months (column 2) of life are shown by selected major causes in Table 6. The data in this table differ from those in other tables in that expenses for the last year of life reflect a full 12 months, not just expenses in the last calendar year of life. (See “Technical note” for details of the method of estimating expenses for the 12 months before death.)
Table 6. Estimated percents of annual Medicare costs for the aged attributable to care rendered in the last 12 months and last 24 months of life, by selected major causes of death: 1979.
| Cause of death | Last year of life | Last 2 years |
|---|---|---|
|
| ||
| Percent of Medicare expenses | ||
| All causes | 28.8 | 39.6 |
| Heart disease | 9.2 | 13.0 |
| Cancer | 8.0 | 10.7 |
| Cerebrovascular disease | 2.5 | 3.5 |
NOTES: See the “Technical note” for techniques used to estimate costs in this table. Complete cause-of-death titles and codes from the International Classification of Diseases, 9th Revision, Clinical Modification, 1980, are given in Table 1.
SOURCE: The Continuous Medicare History Sample of the Medicare Statistical System maintained by the Health Care Financing Administration linked with the Mortality Statistics File maintained by the National Center for Health Statistics.
Nearly 29 percent of Medicare expenses went for care rendered to persons in their last 12 months of life.2 (Five percent of aged beneficiaries are in their last year of life at any given time, and about 10 percent are in their last 2 years at any time.) It is estimated that 39.6 percent of annual Medicare expenses was for care of persons who were in their last 24 months of life. Persons dying of heart disease had the greatest impact on expenditures, with 9.2 percent of medical costs going for care of heart disease decedents in their last 12 months. When expenses for heart disease decedents who were in months 13-24 before death were added, the figure increased to 13.0 percent of annual Medicare costs. The frequency of heart disease as a cause of death (41 percent of all decedents) accounts for its high impact. Expenditures for the care of cancer patients in their last 12 months of life comprised 8.0 percent of Medicare expenses. When expenses for cancer decedents who were in months 13-24 before death were added, the figure increased to 10.7 percent.
Summary and discussion
The impact of illnesses ending in death on use of health services often extends to several years before death. Average reimbursements for decedents were above the average for all aged Medicare beneficiaries 5 calendar years before death. For some causes of death—diabetes mellitus, COPD, nephritis, and chronic liver disease—average reimbursements were significantly above average 5 calendar years before death. This pattern reflects the chronic nature of these illnesses and the frequent medical interventions they provoke.
The impact of some causes of death on health care use was limited primarily to the last year or two of life. Persons dying of malignant neoplasms, acute myocardial infarctions, and accidents did not exhibit a pattern of chronic heavy use of services. Those dying of malignant neoplasms incurred high costs, nonetheless, because of their heavy use of services during a relatively short time.
Although the average cost of health care in the last years of life is substantially higher than the Medicare program average for many causes, it cannot be ascertained from these data whether costs are inappropriately high. Claims histories only for persons who died were examined; no attempt was made to analyze the experience of persons who survived following expensive treatment. Because long-term prognoses are very difficult to predict for many severely ill persons, no conclusions were reached on whether the levels of expenses shown in this article are appropriate or not, given the information usually available at the time treatment decisions are made.
Some indirect evidence on appropriateness of care in the last 12 months of life was presented by Scitovsky (1989), who gathered expenditure data by type of service for 216 aged decedents in Northern California. She found that the amount and intensity of hospital services used was greater for persons who were younger and functionally unimpaired in their last year of life. Older and more impaired persons used much more supportive care (nursing home and home health care), suggesting that high technology care was used primarily on patients who would be expected to have a better prognosis.
The reimbursement ratios presented in this article reflect the natural progression of many of the conditions included in the study. Among cancer sites, for example, the pattern of expenses for cancer of the respiratory organs contrasts with that for breast cancer. The annual reimbursement ratio for breast cancer decedents exceeds 1.0 for 6 calendar years before death, whereas the reimbursement ratio for respiratory cancer decedents does not significantly exceed 1.0 until the second calendar year before the year of death. The annual reimbursement ratios for breast cancer are greater than those for respiratory cancer for all but the last calendar year. Undoubtedly, these patterns reflect differences in survival times after diagnosis for the two types of cancer. During the period 1973-79 the 5-year survival rate for aged breast cancer patients was 53 percent; and for lung cancer (the most common type of respiratory cancer), it was 7 percent (Ries et al., 1983). Despite higher costs in the final calendar year for respiratory cancer (reimbursement ratios of 6.57 versus 6.04), costs during the 6-year study period were 13 percent lower for respiratory cancer (combined reimbursement ratios of 2.34 versus 2.70). The longer survival times for breast cancer, and consequent need for medical attention over a longer period, resulted in higher total Medicare costs even though costs for respiratory cancer decedents were higher in the last year of life.
In this article, we examined the relationship between age at death and medical care costs in the last years of life. On the average, expenses in the last 3 calendar years of life decreased steadily after age 74, although for heart disease decedents, expenses did not begin to decline until very advanced ages. One explanation for the decrease in expenses may be the greater frailty of the oldest of the aged, who, once they get sick, may succumb more quickly than younger persons. For example, for cancer patients, a decrease in survival time with advanced age has been noted (Ries et al., 1983). In addition, perhaps “heroic” measures are less often taken for the frail elderly.
The pattern of lower expenses at older ages may have implications for future Medicare expenditures. For example, if the widespread adoption of health prevention measures delays the onset of chronic diseases, deaths from these conditions may be delayed to more advanced ages. Although greater longevity increases the length of time Medicare enrollees are covered, Medicare costs may not increase proportionately if the pattern of lower expenses for older decedents continues. As noted previously, however, Medicare expenses do not include the costs of most nursing home care, which increase substantially with age. Scitovsky (1989) found that total medical care expenses in the last year, including nursing home expenses, were somewhat lower for the very old than for the younger aged.
Future Medicare program costs will also be determined in part by the mix of causes of death. From 1968 to 1985, the percents of total deaths of people 65 years of age or over due to heart disease and stroke declined from 45.5 percent to 42.2 percent and from 14.5 percent to 9.0 percent, respectively (National Center for Health Statistics, 1987; National Center for Health Statistics, 1971). These causes of death tend to be relatively less expensive to the Medicare program. The percent of deaths from malignant neoplasms (a relatively costly cause of death) rose during that period from 14.9 percent to 20.3 percent. If these trends continue, they might be expected to act to increase future Medicare costs over what they would otherwise be, although their impact will be affected in part by changes in the average age of death, as well as in treatment patterns and other factors.
It was found that only about 40 percent of persons with heart disease as the underlying cause of death and only about 44 percent of persons with stroke as the underlying cause of death were hospitalized for those diseases during their last 2 calendar years of life. Undoubtedly, some of these people die suddenly without ever being hospitalized for the disease that caused their death. In other cases, the hospital diagnosis may reflect comorbidities contributing to the person's death, such as respiratory disease in the case of a person with heart disease. However, the low percent of persons hospitalized for a diagnosis related to their underlying cause of death also raises questions about the accuracy of diagnosis from each information source. Analysis of hospital diagnosis and cause of death at the person level from files such as the one created for this study may shed light on the accuracy of data from these data sources (Gittlesohn and Senning, 1979). Accurate data are gaining in importance as both hospital data and cause of death data are increasingly being applied to fields such as evaluation of the effectiveness and outcomes of care.
During their last 6 years of life, 16 percent of decedents 70 years of age or over did not have above average expenses in any year, and a further 52 percent had above average expenses only in one or two years. The fact that most individuals had only one or two high-cost years suggests that heavy use of services tends to be episodic in the last years of life. It should be noted that an episode of illness could have begun late in one calendar year and extended into the next one. Neither year would have been high, but the episode would have been. Despite this limitation, it is suggested that, even in their last 6 years, most people have very high cost episodes in only one or two years.
Technical note
Tests of statistical significance
In order to test whether reimbursement ratios in Table 2 were statistically significantly different than 1, we tested whether an equivalent hypothesis was true, namely, whether average cause-of-death-specific reimbursements minus average reimbursements for all aged beneficiaries equal zero. Two-tailed tests were used. We computed t-statistics according to the formula:
where
| R̅c = | Average cause-of-death-specific reimbursements for the 5-percent sample of decedents. |
| R̅a = | Average reimbursements for the 1-percent sample of all aged beneficiaries. |
| V(R̅c) = | Estimated variance of the average cause-of-death specific reimbursements. |
| V(R̅a) = | Estimated variance of the average reimbursements for all aged beneficiaries. |
The formula for t is only approximate because we make a simplifying assumption that R̅c and R̅a are independent.
We estimated V(R̅a) using an estimated coefficient of variation for Medicare reimbursements. The coefficient of variation, defined as the standard error divided by the mean, has been estimated to be 2.6 for Medicare reimbursements (Beebe, 1987). The estimated variance of the average reimbursements for all aged beneficiaries was then computed using the formula:
where
n = number of persons in the 1-percent sample of all aged beneficiaries.
Because many tests of statistical significance were conducted simultaneously in Table 2, we defined the α level for each test using the Dunn Multiple Comparison Test (Kirk, 1968). This procedure produced an overall 5-percent level of significance for each column in Table 2 by using an α level of 0.0025 for each individual test.
Estimating percent of expenses incurred
In order to estimate the percent of 1979 expenses going to the care of beneficiaries who were in their last 12 months of life in 1979, we estimated average expenses (in 1979 dollars) in the last 12 months of life for our sample of decedents as follows. Although 12 months of expenses for 1979 decedents usually included some expenses from 1978, these 1978 expenses (adjusted to 1979 dollars) were used to estimate expenses incurred in 1979 for persons who died in 1980 (e.g., for a person dying on July 1, 1980, his or her expenses incurred in the last half of 1979 were for care delivered in the last 12 months of life). We could not directly identify the 1979 expenses that were incurred in the last 12 months of life for 1980 decedents because we did not have death dates for our sample beyond 1979.
Similar reasoning applied to estimating the percent of expenses incurred for care rendered in the last 24 months of life.
Because our data base contained Medicare expenses of individuals summarized by calendar year, we estimated expenses for the last 12 and 24 months of life as follows. We computed average 1979 and 1978 (inflation adjusted) expenses for persons dying in January 1979, February 1979, etc. Assuming a uniform distribution of deaths within each month, these average expenses represented estimates of average expenses in the last 16 days of life, last 45 days of life, and so forth to the last 715 days of life. Then a curve was fitted to these points to estimate average expenses in the last 12 months and last 24 months of life. This procedure was followed separately for beneficiaries dying of each of the three major causes of death.
Lastly, the average expense in the last 12 and 24 months of life for each major cause was divided by total Medicare expenses in 1979 to estimate the percent of 1979 expenses going for care of beneficiaries who were in their last 12 and 24 months of life, by cause of death.
Figure 3. Reimbursement ratios for aged Medicare decedents who died in 1979, by hospital and physician expenses: Cancer, 1974-79.
Acknowledgments
The authors thank Marian Gornick, Stephen Jencks, M.D., and Feather Davis, Ph.D., for their helpful comments on previous drafts of this article. In addition, the authors wish to express their appreciation to Mary Ann Stevenson, Evelyne Rabey, and Ronald Prihoda for their extensive programming and data processing work for this project. They also thank Delores Russell for her assistance in compiling and tabulating data.
Footnotes
Reprint requests: Gerald F. Riley, Health Care Financing Administration, Room 2504, Oak Meadows Building, 6325 Security Boulevard, Baltimore, Maryland 21207.
Previous studies of Medicare use in the last year of life have shown that decedents used more than six times the average per capita reimbursements. The ratio in this article is lower because costs in the last calendar year of life rather than in the last 12 months were used.
The numbers presented here on the percent of Medicare expenses attributable to care rendered in the last year of life are slightly higher than those presented in 1987 by Riley et al. (Table 1) because of the different estimation methods used. The availability of multiyear data on a calendar year basis for this article permits more accurate estimation of Part B expenses for specific months than was possible in the earlier article. The estimation methods are described in the “Technical note.”
References
- Beebe, J.: Office of Research and Demonstrations, Health Care Financing Administration. Personal communication, 1987.
- Gittlesohn A, Senning J. Studies on the reliability of vital and health records: I. Comparison of cause of death and hospital record diagnoses. American Journal of Public Health. 1979 Jul;69(7):680–689. doi: 10.2105/ajph.69.7.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk R. Experimental Design: Procedures for the Behavioral Sciences. Brooks/Cole Publishing Co., Inc.; Belmont, Calif.: 1968. [Google Scholar]
- Lubitz J, Prihoda R. Health Care Financing Review. No. 3. Vol. 5. Washington: U.S. Government Printing Office; Spring. 1984. The use and costs of Medicare services in the last 2 years of life. HCFA Pub. No. 03169. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Monthly Vital Statistics Report. No. 12. Vol. 19. Public Health Service; Rockville, Md.: Mar. 1971. Advance report of final mortality statistics, 1968. Supp. [Google Scholar]
- National Center for Health Statistics. Monthly Vital Statistics Report. No. 5. Vol. 36. Public Health Service; Hyattsville, Md.: Aug. 1987. Advance report of final mortality statistics, 1985. Supp. DHHS Pub. No. (PHS) 87-1120. [Google Scholar]
- Public Health Service and Health Care Financing Administration. International Classification of Diseases, 9th Revision, Clinical Modification. 2nd. Washington: U.S. Government Printing Office; Sept. 1980. DHHS Pub. No. (PHS) 80-1260. Public Health Service. [Google Scholar]
- Ries L, Pollock E, Young J. Cancer patient survival: Surveillance, epidemiology, and end results program, 1973-1979. Journal of the National Cancer Institute. 1983 Apr.70(4):693–707. [PubMed] [Google Scholar]
- Riley G, Lubitz J, Prihoda R, Rabey E. The use and costs of Medicare services by cause of death. Inquiry. 1987 Fall;24(3):233–244. [PubMed] [Google Scholar]
- Roos N, Montgomery P, Roos L. Health care utilization in the years prior to death. The Milbank Quarterly. 1987;65(2):231–254. [PubMed] [Google Scholar]
- Scitovsky A. Medical care in the last 12 months of life: The relation between age, functional status, and medical care expenditures. The Milbank Quarterly. 1989;66(4):640–660. [PubMed] [Google Scholar]
- Waldo DR, Levit KR, Lazenby H. Health Care Financing Review. No. 1. Vol. 8. Washington: U.S. Government Printing Office; Fall. 1986. National health expenditures, 1986. HCFA Pub. No. 03224. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]