Abstract
Every year, analysts in the Health Care Financing Administration present figures on what our Nation spends for health. As the result of a comprehensive re-examination of the definitions, concepts, methods, and data sources used to prepare those figures, this year's report contains new estimates of national health expenditures for calendar years 1960 through 1988. Significant changes have been made to estimates of spending for professional services and to estimates of what consumers pay out of pocket for health care. In the first article, trends in use of and expenditure for various types of goods and services are discussed, as well as trends in the sources of funds used to finance health care. In a companion article, the benchmark process is described in more detail, as are the data sources and methods used to prepare annual estimates of health expenditures.
Overview
Revised estimates from the National Health Accounts (NHA) show that spending for health in the United States during calendar year 1988 continued the trends seen in the last few years. Highlights of this article include the following:
Expenditures for health care in the United States totaled $539.9 billion in 1988, an increase of 10.4 percent from the previous year.
Expenditures averaged $2,124 per capita. Of that, $1,882 was for personal health care; the remainder was for research, construction, program administration, the net cost of private health insurance, and public health activities.
Spending for health amounted to 11.1 percent of the gross national product (GNP) in 1988, more than twice the share that it occupied in 1960.
Hospital expenditures, which increased 9.3 percent from 1987 through 1988, accounted for 39 percent of all health spending in the United States. Medicare and Medicaid, the two largest Federal programs for health care, financed more than one-third of the Nation's $211.8 billion hospital bill.
Spending for physician services increased 13.1 percent, to $105.1 billion. Concern over the rate of growth of expenditures has led to legislation designed to restrain the growth of Medicare physician outlays.
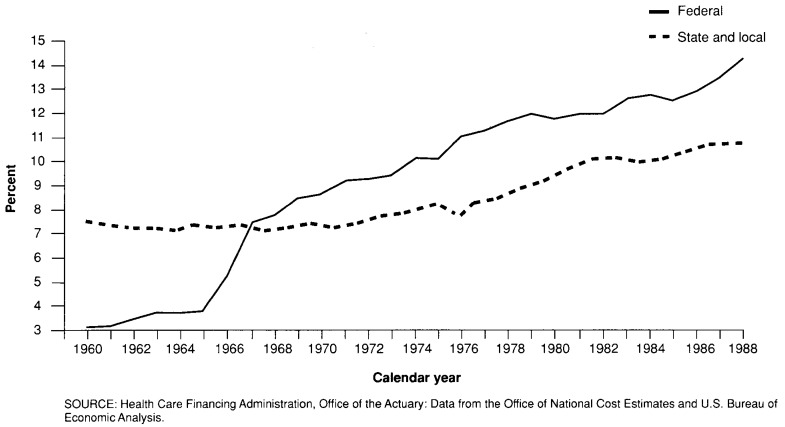
Federal Government programs financed 29.9 percent of personal health care expenditures in 1988, concentrating on hospital care. The share of all Federal expenditures accounted for by health care has been growing steadily, but the increase in 1987 and 1988 was particularly strong. The $157.8 billion of Federal spending in the NHA in 1988 represented 14 percent of all Federal expenditures.
In 1988, Medicare and Medicaid, two programs administered by the Health Care Financing Administration, accounted for 10 percent of the Federal budget.
State and local governments spent $69.6 billion for health care in 1988. As is true for the Federal Government, health care expenditures have accounted for an increasing share of total State and local expenditures. However, the growth in that share did not begin until the early 1970s; it reached 10.7 percent in 1988.
Private health insurance benefits in 1988 amounted to $155.2 billion, increasing 11.0 percent from the 1987 level and accounting for almost one-third of personal health care expenditures. Premiums increased 11.9 percent, to $174.9 billion.
Americans paid $113.2 billion out of pocket for health care in 1988, averaging 23.7 percent of personal health care expenditures. Some types of service are more heavily insured than others: For example, hospital patients on average paid 5.3 percent of their bills out of pocket, but consumers of drugs and vision products paid 70.7 percent of those costs out of pocket.
Since 1950, the share of disposable personal income that consumers devoted to out-of-pocket health care purchases has remained roughly constant, ranging between 3.0 and 3.9 percent.
Detailed Tables 13-22 at the end of this article show expenditures for health care for selected years 1960 through 1988, both by type of service and by source of funds. Data figures from the detailed tables are highlighted throughout this article.
Table 13. National health expenditures aggregate and per capita amounts, percent distribution, and average annual percent growth, by source of funds: Selected calendar years 1960-88.
| Item | 1960 | 1965 | 1970 | 1975 | 1980 | 1985 | 1986 | 1987 | 1988 |
|---|---|---|---|---|---|---|---|---|---|
| Amount in billions | |||||||||
| National health expenditures | $27.1 | $41.6 | $74.4 | $132.9 | $249.1 | $420.1 | $450.5 | $488.8 | $539.9 |
| Private | 20.5 | 31.3 | 46.7 | 77.8 | 143.9 | 245.2 | 259.8 | 280.5 | 312.4 |
| Public | 6.7 | 10.3 | 27.7 | 55.1 | 105.2 | 174.9 | 190.7 | 208.3 | 227.5 |
| Federal | 2.9 | 4.8 | 17.7 | 36.4 | 72.0 | 123.4 | 132.8 | 144.0 | 157.8 |
| State and local | 3.7 | 5.5 | 9.9 | 18.7 | 33.2 | 51.5 | 57.9 | 64.3 | 69.6 |
| Number in millions | |||||||||
| U.S. population1 | 190.1 | 204.0 | 214.8 | 224.7 | 235.2 | 247.1 | 249.5 | 251.8 | 254.2 |
| Amount in billions | |||||||||
| Gross national product | $515 | $705 | $1,015 | $1,598 | $2,732 | $4,015 | $4,232 | $4,524 | $4,881 |
| Per capita amount | |||||||||
| National health expenditures | $143 | $204 | $346 | $592 | $1,059 | $1,700 | $1,806 | $1,941 | $2,124 |
| Private | 108 | 154 | 217 | 346 | 612 | 992 | 1,041 | 1,114 | 1,229 |
| Public | 35 | 50 | 129 | 245 | 447 | 708 | 765 | 827 | 895 |
| Federal | 15 | 24 | 83 | 162 | 306 | 500 | 532 | 572 | 621 |
| State and local | 20 | 27 | 46 | 83 | 141 | 208 | 232 | 256 | 274 |
| Percent distribution | |||||||||
| National health expenditures | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private | 75.5 | 75.3 | 62.8 | 58.5 | 57.8 | 58.4 | 57.7 | 57.4 | 57.9 |
| Public | 24.5 | 24.7 | 37.2 | 41.5 | 42.2 | 41.6 | 42.3 | 42.6 | 42.1 |
| Federal | 10.7 | 11.6 | 23.9 | 27.4 | 28.9 | 29.4 | 29.5 | 29.5 | 29.2 |
| State and local | 13.8 | 13.2 | 13.3 | 14.1 | 13.3 | 12.2 | 12.9 | 13.2 | 12.9 |
| Percent of gross national product | |||||||||
| National health expenditures | 5.3 | 5.9 | 7.3 | 8.3 | 9.1 | 10.5 | 10.6 | 10.8 | 11.1 |
| Average annual percent growth from previous year shown | |||||||||
| National health expenditures | — | 8.9 | 12.3 | 12.3 | 13.4 | 11.0 | 7.2 | 8.5 | 10.4 |
| Private | — | 8.9 | 8.3 | 10.7 | 13.1 | 11.2 | 6.0 | 8.0 | 11.4 |
| Public | — | 9.1 | 21.9 | 14.8 | 13.8 | 10.7 | 9.1 | 9.2 | 9.2 |
| Federal | — | 10.6 | 29.8 | 15.5 | 14.6 | 11.4 | 7.6 | 8.4 | 9.6 |
| State and local | — | 7.9 | 12.6 | 13.5 | 12.1 | 9.2 | 12.5 | 11.1 | 8.2 |
| U.S. population | — | 1.4 | 1.0 | 0.9 | 0.9 | 1.0 | 1.0 | 1.0 | 0.9 |
| Gross national product | — | 6.5 | 7.6 | 9.5 | 11.3 | 8.0 | 5.4 | 6.9 | 7.9 |
July 1 social security area population estimates.
NOTE: Numbers and percent may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 22. Expenditures for health services and supplies under public programs, by type of expenditure and program: Calendar years 1980 and 1988.
| Program area | All expenditures | Personal health care | Administration | Public health activities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Total | Hospital care | Physician services | Dental services | Other professional services | Home health care | Drugs and other medical nondurables | Vision products and other medical durables | Nursing home care | Other | ||||
|
| |||||||||||||
| Amount in billions | |||||||||||||
| 1980 | |||||||||||||
| Public and private spending | $237.8 | $218.3 | $102.4 | $41.9 | $14.4 | $8.7 | $1.3 | $20.1 | $5.0 | $20.0 | $4.6 | $12.2 | $7.2 |
| All public programs | 98.1 | 87.1 | 54.6 | 12.6 | 0.6 | 1.7 | 1.0 | 1.7 | 0.6 | 10.5 | 3.7 | 3.8 | 7.2 |
| Federal funds | 66.8 | 63.5 | 41.3 | 9.7 | 0.4 | 1.3 | 0.8 | 0.8 | 0.5 | 6.1 | 2.5 | 2.1 | 1.2 |
| State and local funds | 31.4 | 23.6 | 13.3 | 3.0 | 0.3 | 0.4 | 0.1 | 0.8 | 0.1 | 4.4 | 1.2 | 1.8 | 6.0 |
| Medicare | 37.5 | 36.4 | 26.4 | 7.9 | — | 0.6 | 0.7 | — | 0.4 | 0.4 | — | 1.1 | — |
| Medicaid1 | 26.1 | 24.8 | 9.7 | 2.1 | 0.5 | 0.5 | 0.3 | 1.4 | — | 9.7 | 0.6 | 1.3 | — |
| Federal | 14.5 | 13.7 | 5.3 | 1.2 | 0.3 | 0.3 | 0.2 | 0.8 | — | 5.4 | 0.3 | 0.8 | — |
| State and local | 11.6 | 11.1 | 4.4 | 1.0 | 0.2 | 0.2 | 0.1 | 0.6 | — | 4.4 | 0.3 | 0.5 | — |
| Other State and local public assistance programs | 1.9 | 1.9 | 1.3 | 0.3 | 0.0 | 0.0 | 0.0 | 0.1 | — | 0.0 | 0.1 | — | — |
| Veterans Administration | 5.9 | 5.9 | 4.9 | 0.1 | 0.1 | — | — | 0.0 | 0.1 | 0.4 | 0.4 | 0.0 | — |
| Department of Defense2 | 4.3 | 4.3 | 3.7 | 0.3 | 0.0 | — | — | 0.0 | — | — | 0.3 | 0.0 | — |
| Workers' compensation | 5.2 | 4.0 | 2.0 | 1.7 | — | 0.1 | — | 0.1 | 0.1 | — | — | 1.2 | — |
| Federal | 0.1 | 0.1 | 0.1 | 0.0 | — | 0.0 | — | 0.0 | 0.0 | — | — | 0.0 | — |
| State and local | 5.0 | 3.8 | 1.9 | 1.6 | — | 0.1 | — | 0.1 | 0.1 | — | — | 1.2 | — |
| State and local hospitals3 | 5.6 | 5.6 | 5.6 | — | — | — | — | — | — | — | — | — | — |
| Other public programs for personal health care4 | 4.3 | 4.2 | 1.0 | 0.3 | 0.0 | 0.5 | — | 0.0 | 0.1 | — | 2.3 | 0.1 | — |
| Federal | 3.1 | 3.0 | 0.9 | 0.2 | 0.0 | 0.4 | — | 0.0 | 0.0 | — | 1.5 | 0.0 | — |
| State and local | 1.2 | 1.2 | 0.1 | 0.1 | 0.0 | 0.1 | — | 0.0 | 0.0 | — | 0.9 | 0.1 | — |
| Government public health activities | 7.2 | — | — | — | — | — | — | — | — | — | — | — | 7.2 |
| Federal | 1.2 | — | — | — | — | — | — | — | — | — | — | — | 1.2 |
| State and local | 6.0 | — | — | — | — | — | — | — | — | — | — | — | 6.0 |
| Medicare and Medicaid | 63.7 | 61.2 | 36.0 | 10.1 | 0.5 | 1.1 | 1.0 | 1.4 | 0.4 | 10.1 | 0.6 | 2.4 | — |
| 1988 | |||||||||||||
| Public and private spending | $520.5 | $478.3 | $211.8 | $105.1 | $29.4 | $22.5 | $4.4 | $41.9 | $10.8 | $43.1 | $9.3 | $26.3 | $15.9 |
| All public programs | 215.9 | 194.0 | 115.2 | 35.2 | 0.7 | 4.5 | 3.3 | 4.6 | 2.3 | 20.9 | 7.4 | 6.1 | 15.9 |
| Federal funds | 149.0 | 143.2 | 86.7 | 28.7 | 0.4 | 3.4 | 2.6 | 2.2 | 2.0 | 12.5 | 4.7 | 3.9 | 1.9 |
| State and local funds | 66.9 | 50.8 | 28.5 | 6.4 | 0.3 | 1.0 | 0.7 | 2.4 | 0.2 | 8.4 | 2.7 | 2.2 | 14.0 |
| Medicare | 91.8 | 89.7 | 58.3 | 24.9 | — | 2.1 | 1.8 | — | 1.9 | 0.8 | — | 2.0 | — |
| Medicaid1 | 55.1 | 52.3 | 20.2 | 3.8 | 0.6 | 1.4 | 1.5 | 3.6 | — | 19.1 | 2.1 | 2.8 | — |
| Federal | 31.1 | 29.4 | 11.2 | 2.2 | 0.3 | 0.8 | 0.8 | 2.1 | — | 10.8 | 1.2 | 1.6 | — |
| State and local | 24.1 | 22.9 | 8.9 | 1.6 | 0.3 | 0.6 | 0.7 | 1.5 | — | 8.4 | 0.9 | 1.2 | — |
| Other State and local public assistance programs | 3.9 | 3.9 | 2.6 | 0.4 | 0.1 | 0.0 | 0.0 | 0.6 | — | 0.1 | 0.1 | — | — |
| Veterans Administration | 10.0 | 10.0 | 7.7 | 0.2 | 0.0 | — | — | 0.0 | 0.1 | 1.0 | 1.0 | 0.0 | — |
| Department of Defense2 | 9.9 | 9.8 | 8.0 | 1.1 | 0.0 | — | — | 0.1 | — | — | 0.6 | 0.1 | — |
| Workers' compensation | 11.4 | 10.5 | 5.4 | 4.4 | — | 0.3 | — | 0.2 | 0.2 | — | — | 0.9 | — |
| Federal | 0.4 | 0.4 | 0.2 | 0.1 | — | 0.0 | — | 0.0 | 0.0 | — | — | 0.0 | — |
| State and local | 11.1 | 10.2 | 5.1 | 4.4 | — | 0.3 | — | 0.2 | 0.2 | — | — | 0.9 | — |
| State and local hospitals3 | 11.6 | 11.6 | 11.6 | — | — | — | — | — | — | — | — | — | — |
| Other public programs for personal health care4 | 6.4 | 6.2 | 1.4 | 0.5 | 0.0 | 0.7 | — | 0.0 | 0.1 | — | 3.6 | 0.2 | — |
| Federal | 4.0 | 4.0 | 1.1 | 0.3 | 0.0 | 0.5 | — | 0.0 | 0.1 | — | 1.9 | 0.0 | — |
| State and local | 2.4 | 2.3 | 0.2 | 0.1 | 0.0 | 0.1 | — | 0.0 | 0.0 | — | 1.7 | 0.1 | — |
| Government public health activities | 15.9 | — | — | — | — | — | — | — | — | — | — | — | 15.9 |
| Federal | 1.9 | — | — | — | — | — | — | — | — | — | — | — | 1.9 |
| State and local | 14.0 | — | — | — | — | — | — | — | — | — | — | — | 14.0 |
| Medicare and Medicaid | 146.9 | 142.0 | 78.5 | 28.6 | 0.6 | 3.4 | 3.3 | 3.6 | 1.9 | 19.9 | 2.1 | 4.9 | — |
Excludes funds paid into the Medicare trust funds by States under “buy-in” agreements to cover premiums for public assistance recipients and for people who are medically indigent.
Includes care for retirees and military dependents.
Expenditures not offset by revenues.
Includes program spending for maternal and child health; vocational rehabilitation medical payments; temporary disability insurance medical payments; Public Health Service and other Federal hospitals; Indian health services; alcoholism, drug abuse, and mental health; and school health.
NOTES: 0.0 denotes less than $50 million. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
The national health expenditures (NHE) estimates presented in this article have undergone significant revisions from the data previously published, affecting all years from 1960 through 1987. The size and sign of these revisions vary across the 28 years covered. However, the trends remain similar to those previously published. A discussion of the revisions and the methodology employed is presented in the companion article in this issue.
Expenditures by type of service
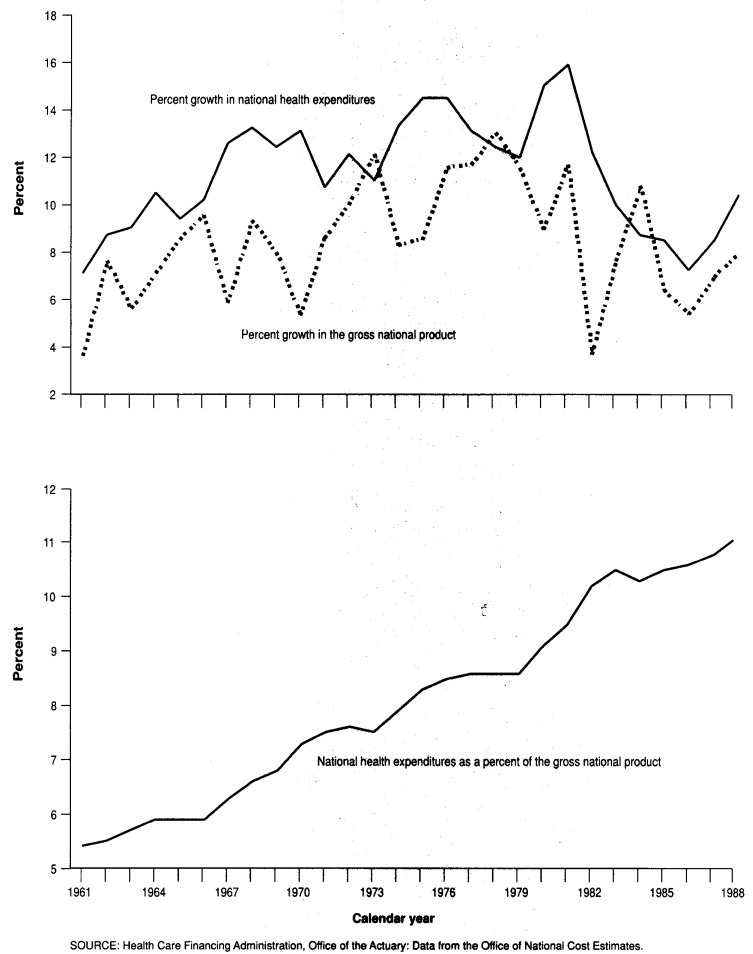
NHE reached $539.9 billion in 1988. This amounts to $2,124 for each of the 254 million people in the United States and its territories. In 1988, NHE amounted to 11.1 percent of GNP, up from 10.8 percent in 1987 and 5.3 percent in 1960 (Figure 1).
Figure 1. Percent growth in national health expenditures and gross national product, and national health expenditures as a percent of gross national product: Calendar years 1961-88.
After the 4 years of single-digit increases in health care spending experienced from 1984 through 1987, NHE grew 10.4 percent in 1988. This also was the fourth consecutive year in which growth in health care spending outpaced growth in the economy as a whole. Further, the gap between the two growth rates widened slightly in 1988, compared with that experienced in the 5 previous years.
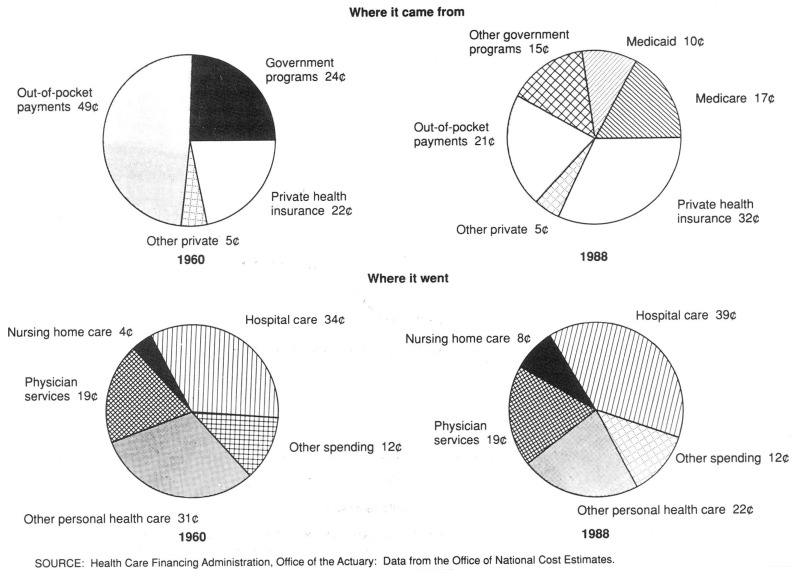
The financing structure of NHE has changed during the three decades covered in this article. In 1960, three-quarters (75.5 percent) of all health care spending came from private sources, with almost 50 percent coming from out-of-pocket spending by consumers. By 1988, the share financed by private sources had dropped to 57.9 percent, and private health insurance had become the predominant private payer (Figure 2). Out-of-pocket spending had dropped to 21 percent of all health expenditures.
Figure 2. The Nation's health dollar: 1960 and 1988.
During this period, public financing boomed. In 1960, public programs paid for one-quarter (24.5 percent) of all health care spending; by 1988, this share had increased to 42.1 percent. The greatest change in public funding took place in the Federal Government sector with the implementation of Medicare for the aged. This one program was the major cause for the Federal share of total health care spending rising from 11.6 percent in 1965 to 23.7 percent in 1967. Medicare continued to increase its share of funding for health expenditures, and that is why the public funding share grew to 41.6 percent in 1985, approximately where it has since remained.
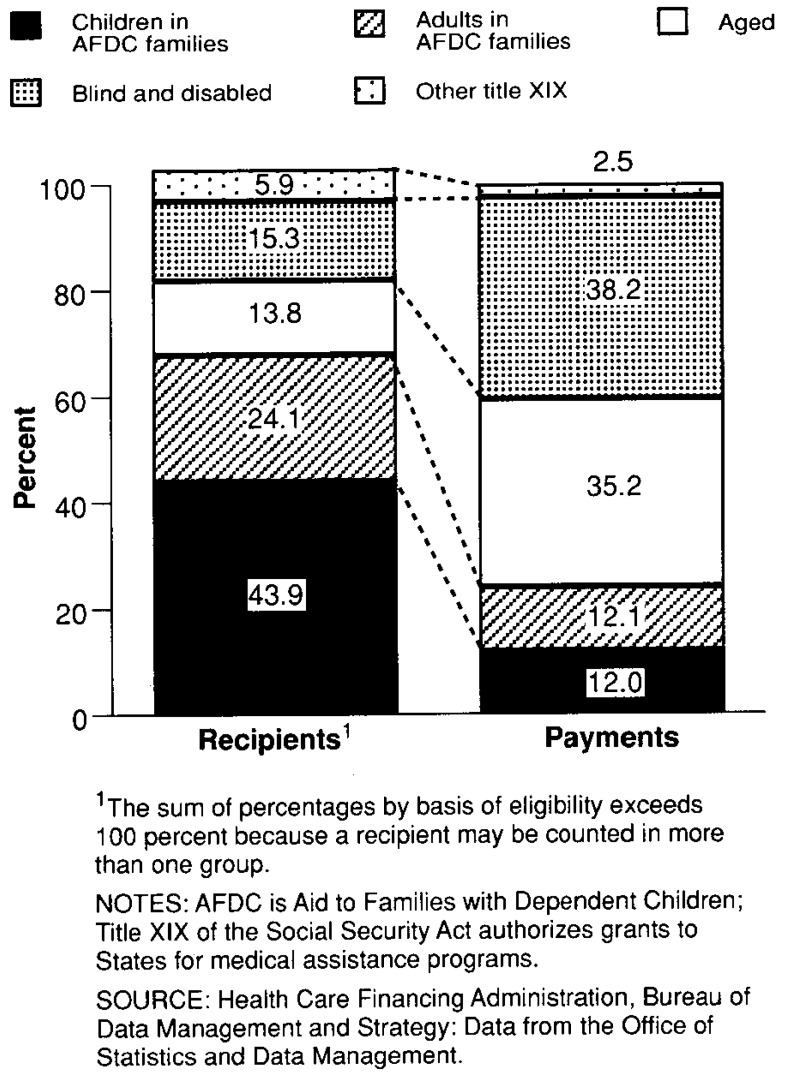
When introduced in mid-1966, Medicaid replaced existing programs for the poor, thereby minimizing any impact on share of public funding. In 1988, Medicaid (Federal and State combined) funded 10 percent of all health care expenditures, approximately the same proportion funded since 1975.
Levels of State and local funding, including the State and local portion of Medicaid, changed little over the last three decades. In 1988, non-Federal governments financed 12.9 percent of all health care expenditures, down from 13.8 percent in 1960.
Health services and supplies
Spending for health services and supplies grew to $520.5 billion in 1988, constituting 96 percent of all NHE. Excluded from this amount is spending for investment in the future of health care through research and construction of new facilities.
Spending for health services and supplies grew at approximately the same pace as did research and construction from 1960 through 1972, averaging 11 percent per year for health services and supplies and 12 percent per year for research and construction. Since 1972, however, growth in spending for health services and supplies has exceeded that for research and construction (11.9 and 7.0 percent annual growth, respectively). This differential growth indicates a change in priorities away from investment in the future delivery of services toward current consumption. (Note that the NHA exclude investment in capital equipment and spending for commercial research. Including the latter does raise the research and construction growth rate slightly from 1972 through 1988; no estimates of capital equipment purchase are available, so the effect of these investments is unknown.)
Personal health care expenditures
Eighty-nine percent of all NHE, $478.3 billion, is for personal health care—the purchase of medical care services and supplies by individuals. This amount represents a 10.0 percent growth in spending from 1987.
Personal health care includes services received by individuals in hospitals, nursing homes, offices of physicians, dentists, and other licensed medical professionals; home health care; drugs, vision care products, other durable and nondurable medical products; and miscellaneous health care. Excluded from personal health care are the costs of administering public programs, the net cost of private health insurance, government public health activity, research, and construction.
Consumers spent $113.2 billion directly out of pocket for personal health care services in 1988, financing 23.7 percent of all personal health care spending in this manner. The remaining health care expenditures were funded by third parties such as private health insurance (32.4 percent) and public programs (40.6 percent). The remainder (3.3 percent) was financed by business (through in-plant health care services), by philanthropic giving, and by other nonpatient revenue sources of hospitals, nursing homes, and home health agencies.
During the past 28 years, funding of personal health care services has changed dramatically. Consumers, through out-of-pocket payments, paid for less than one-half of the share of health care services in 1988 that they did in 1960. From 1960 through 1988, the share of personal health care spending financed through government programs almost doubled; for private health insurance, the share increased by more than 50 percent. Studies have shown that higher levels of consumption result from greater insurance coverage (Phelps, 1982). Some of the higher consumption reflects the removal of financial barriers to appropriate care; some may also reflect unnecessary consumption.
Factors accounting for growth
When studying health care spending trends, it is useful to distinguish the various factors that contribute to increasing health care costs. Although such an analysis focuses on the “hows” of growth rather than the “whys” (Freeland and Schendler, 1984), it provides a useful tool of reference when assessing the magnitude of the various influences.
An essential part of the analysis of factors contributing to growth is the determination of “real” or constant-dollar personal health care spending. This can best be done by constructing a time series that measures growth in spending as if prices had remained unchanged from the base period. The series is calculated by dividing each component of personal health care spending by an appropriate price index, then summing these pieces to a total.
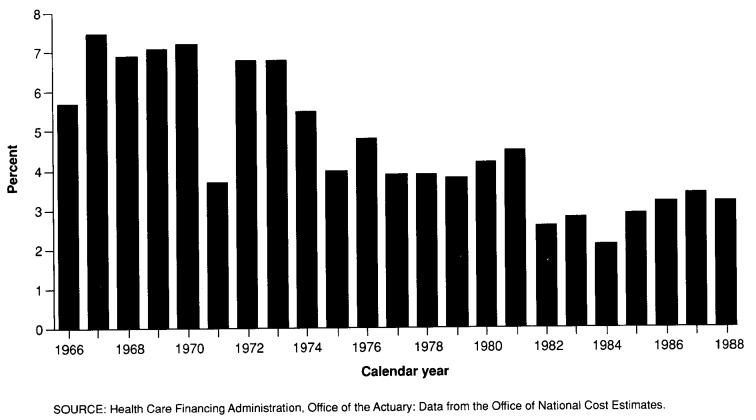
Growth in real personal health care expenditures (PHCE) varied over time, with some clearly definable eras of change since 1965 (Figure 3). The period 1966-70, following the implementation of the Medicare and Medicaid programs, was one of rapid growth in real PHCE, with an average annual growth rate of 7.2 percent. Because hospital expenditures are the largest component of PHCE, changes in hospital use have a substantial effect on the aggregate real rate of growth.
Figure 3. Annual percent growth in real personal health care expenditures: Calendar years 1966-88.
The low growth in real PHCE in 1971 is supported by American Hospital Association (AHA) panel survey data, which shows low growth in the numbers of adjusted admissions (0.8 percent), adjusted inpatient days (−1.1 percent), and surgical procedures (2.1 percent) (American Hospital Association, 1963-89). The economic stabilization period (1972-74) is characterized by low prices and high utilization. The AHA panel survey data, using the same three indicators of utilization, also support this description. Following this time of high real growth, the period 1975-81 was relatively stable, with an average annual growth rate of 4.2 percent. Beginning in 1982, private initiatives to reduce hospital use began to produce results in terms of fewer hospital days for the population under age 65. This was followed in 1983 by the phasing in of Medicare's prospective payment system (PPS). After 1985, real spending began to accelerate once again, but to a pace that is slower than the 4.6-percent annual growth for the period 1965-88.
One way to identify the pressures on health spending is to allocate the growth in PHCE among four factors: general price inflation, industry-specific medical price inflation, population growth, and all other factors per capita. This analysis makes use of an identity equation:
where E is expenditure, M is a medical care index, G is an economywide price index, and P is population. The first term of the identity expression is a measure of medical prices relative to those in the economy as a whole. The final term is a residual; it can be called intensity or real expenditure per capita. Given that prices and population are explicitly represented, real expenditure per capita is driven by “all other factors”
In a section at the end of the companion article in this issue, a fixed-weight price index for the health sector is described. This index is used to measure overall medical price inflation. Using the GNP fixed-weight price index, it is possible to remove the effect of overall inflation from the PHCE fixed-weight price index, leaving medical price inflation that is in excess of general inflation.
With the effect of medical price inflation removed from growth in PHCE and general inflation removed from medical price inflation, the last explicit factor to be removed is growth in population. Population growth was almost constant during the period 1960-88. Therefore, the contribution to growth in PHCE remained fairly constant.
“All other factors” reflect a variety of influences that are difficult to disaggregate. Anything that causes changes in use and intensity per capita (as well as all measurement error) is included in this category. Technology, changes in the age and sex composition of the population, changes in real income, and increases in third-party payments contribute to increased use and intensity of health care services (Fuchs, 1990).
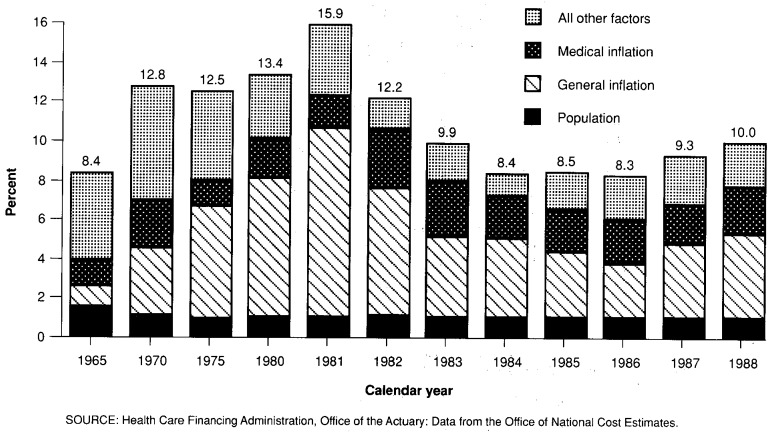
The contribution of all other factors to growth in PHCE was greatest in the period 1965-70, when they caused more than one-half of the growth (Figure 4). In 1982, these factors were at their lowest, accounting for only 13 percent of PHCE growth.
Figure 4. Factors accounting for average annual growth in personal health care expenditures: Selected calendar years 1965-88.
General and medical price inflation has always accounted for a substantial part of the increase in PHCE. In 1982, the effect of this type of price inflation was at its highest, accounting for 78 percent of growth in PHCE.
In 1988, PHCE rose 10.0 percent, with 23 percent of that growth caused by growth in all other factors. General price inflation contributed 43 percent, medical price inflation added 24 percent, and population changes caused 10 percent of the overall growth (Figure 4).
Elements of personal health care
Hospital care
In 1988, hospitals received $211.8 billion in revenue, 9.3 percent more than they received the year before. These revenues included those for services delivered to inpatients and outpatients, for physician services billed through the hospitals (mainly for the services of anesthesiologists, radiologists, and pathologists, but also medical residents), for drugs dispensed during hospitalization, and for services rendered by hospital-based home health agencies. Nursing-home-type care provided in a hospital facility is also counted here.
Forty-four percent of all personal health care spending was for hospital services in 1988. During the 28-year period covered in this article, that share grew steadily from 39 percent in 1960 to 48 percent in 1982, and then fell gradually to the current level.
Public funds financed 54.4 percent of all hospital care in 1988: Medicare alone paid for 27.5 percent of all services, and Medicaid paid for 9.5 percent. The Department of Veterans Affairs (DVA) and the Department of Defense together furnished 7 percent of hospital services, and State and local tax subsidies to hospitals paid for more than 5 percent.
Private funds financed 46 percent of all hospital services in 1988. Private health insurance, most of which is purchased through employers, paid for 35.4 percent. Consumers paid directly for 5.3 percent out of pocket. Hospitals received another 4.9 percent of revenues from nonpatient sources, including philanthropy, nonpatient services (e.g., educational programs, gift shops, cafeterias, office space rental), and investment income.
The relative amounts of hospital care financed by private and public sources changed with the implementation of Medicare. Since 1967, however, those shares have changed very little. Prior to the implementation of Medicare, private funds accounted for about three-fifths of hospital revenue. By 1967, the first full year of Medicare and Medicaid program operation, that share had fallen to 46 percent, where it has since remained.
Trends within the private sector reveal an interesting pattern. Private health insurance benefits covered the same proportion of hospital spending in 1988 as they did in 1960. Almost the entire reduction in the overall private share took place in out-of-pocket payments, which fell from 20.7 percent of all hospital expenditures in 1960 to 5.3 percent in 1988. In 1960, out-of-pocket payments for hospital care were four-sevenths the size of private health insurance benefits; by 1988, out-of-pocket payments were only one-seventh the size of insurance benefits.
Changes in the share of out-of-pocket payments and private insurance benefits attest to the desire of most Americans to minimize the risk of excessive out-of-pocket spending for hospital services. The slight increase in the share of out-of-pocket spending in 1988 may indicate an emerging trend by private insurers to increase cost sharing through higher copayments and deductibles for hospital services.
From 1960 to the present, the Federal Government has gradually assumed more responsibility for funding hospital services, especially after 1965 through the Medicare and Medicaid programs, offsetting declines in State and local funding of hospital services.
Short-term, acute care community hospitals delivered 86 percent of all hospital care in 1988, mostly through inpatient services. However, revenues from care delivered through emergency rooms and outpatient clinics have been growing more rapidly than have inpatient care revenues since 1967 and now account for almost one-fifth (17 percent) of all revenues received by community hospitals (Table 1). This growth has been especially noticeable since 1984, when the Medicare prospective payment system (PPS) imposed inpatient payment limits based on diagnosis-related groups. PPS, coupled with private sector initiatives to cut health insurance costs, prompted providers to push many services formerly delivered on an inpatient basis to an outpatient setting. In 1988, the growth rate for outpatient revenues (17.2 percent) exceeded the growth rate for inpatient revenues (8.3 percent) by a wide margin. Despite the shift to outpatient services, overall hospital growth appears to be less than would have been expected had PPS not been implemented.
Table 1. Hospital revenues, percent distribution, and average annual percent growth: Selected calendar years 1960-88.
| Type of hospital | 1960 | 1965 | 1970 | 1975 | 1980 | 1985 | 1986 | 1987 | 1988 |
|---|---|---|---|---|---|---|---|---|---|
| Amount in millions | |||||||||
| Total | $9,275 | $14,040 | $27,932 | $52,392 | $102,399 | $167,941 | $179,288 | $193,729 | $211,766 |
| Non-Federal | 7,834 | 12,160 | 24,939 | 47,143 | 93,707 | 154,956 | 165,788 | 179,451 | 196,856 |
| Community | — | — | 20,816 | 41,801 | 85,601 | 143,311 | 153,214 | 165,796 | 182,329 |
| Inpatient | — | — | 18,831 | 37,103 | 74,530 | 121,680 | 127,351 | 135,431 | 146,729 |
| Outpatient | — | — | 1,985 | 4,698 | 11,071 | 21,631 | 25,863 | 30,365 | 35,600 |
| Noncommunity | — | — | 4,123 | 5,342 | 8,106 | 11,645 | 12,574 | 13,655 | 14,527 |
| Federal | 1,441 | 1,880 | 2,993 | 5,249 | 8,692 | 12,985 | 13,500 | 14,278 | 14,910 |
| Percent distribution | |||||||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Non-Federal | 84 | 87 | 89 | 90 | 92 | 92 | 92 | 93 | 93 |
| Community | — | — | 75 | 80 | 84 | 85 | 85 | 86 | 86 |
| Inpatient | — | — | 67 | 71 | 73 | 72 | 71 | 70 | 69 |
| Outpatient | — | — | 7 | 9 | 11 | 13 | 14 | 16 | 17 |
| Noncommunity | — | — | 15 | 10 | 8 | 7 | 7 | 7 | 7 |
| Federal | 16 | 13 | 11 | 10 | 8 | 8 | 8 | 7 | 7 |
| Average annual percent growth from previous year shown | |||||||||
| Total | — | 8.6 | 14.7 | 13.4 | 14.3 | 10.4 | 6.8 | 8.1 | 9.3 |
| Non-Federal | — | 9.2 | 15.4 | 13.6 | 14.7 | 10.6 | 7.0 | 8.2 | 9.7 |
| Community | — | — | — | 15.0 | 15.4 | 10.9 | 6.9 | 8.2 | 10.0 |
| Inpatient | — | — | — | 14.5 | 15.0 | 10.3 | 4.7 | 6.3 | 8.3 |
| Outpatient | — | — | — | 18.8 | 18.7 | 14.3 | 19.6 | 17.4 | 17.2 |
| Noncommunity | — | — | — | 5.3 | 8.7 | 7.5 | 8.0 | 8.6 | 6.4 |
| Federal | — | 5.5 | 9.8 | 11.9 | 10.6 | 8.4 | 4.0 | 5.8 | 4.4 |
NOTE: Noncommunity non-Federal hospitals include long-term care hospitals (where the average length of stay is 30 days or longer), psychiatric hospitals, alcoholism and chemical-dependency hospitals, units of institutions such as prison hospitals or college infirmaries, chronic disease hospitals, and some institutions for the mentally retarded.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Noncommunity non-Federal hospitals accounted for $14.5 billion of hospital revenues. These hospitals include long-term care hospitals (where the average length of stay is 30 days or longer), psychiatric hospitals, alcoholism and chemical-dependency hospitals, units of institutions such as prison hospitals or college infirmaries, chronic disease hospitals, and some institutions for the mentally retarded. Primarily as a result of the deinstitutionalization of the mentally retarded from large, State-operated facilities during the 1970s, the share of hospital revenues generated by these facilities has fallen from 15 percent in 1970 to 7 percent in 1988 (Table 1).
Federal hospitals received revenues of $14.9 billion in 1988, most of which came from the Federal Government. Hospitals operated by the Federal Government include DVA facilities; Army, Air Force, and Navy hospitals; Indian Health Service hospitals; the National Institutes of Health hospital; Federal prison hospitals; and other miscellaneous Federal facilities. During the early 1980s, the Federal Government divested itself of all of its Public Health Service hospitals and no longer operates these facilities, which began as facilities for merchant sailors but evolved into hospitals that served the indigent population.
The NHA estimate of hospital expenditures measures revenues that hospitals expect to receive. Based on their gross revenues (before discounts), non-Federal hospitals charged patients $204.7 billion in 1987 (Table 2). After an allowance of $36.4 billion for contractual adjustments to third-party payers such as private health insurers, Medicare, and Medicaid, a writeoff of $8.8 billion for bad debt, another $4.2 billion in charity care, and $2.7 billion in other nonrecoverable charges, non-Federal hospitals received $152.6 billion in net revenues from patient care. These patient revenues amounted to 88.7 percent of all revenues received by non-Federal hospitals.
Table 2. Revenues of non-Federal hospitals in the United States: Financial years 1980-87.
| Hospital financial year | Gross revenues (charges to patients) | Deductions from revenue | Net revenue from patients | Other operating revenue | Non-operating revenue | Total net revenue from all sources | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Contractual adjustments | Bad debt | Charity | Other | Total | Tax appropriations | Other | |||||
| All non-Federal hospitals | Amount in billions | ||||||||||
| 1980 | $93.2 | $10.8 | $3.4 | $1.4 | $0.7 | $76.9 | $8.0 | $5.3 | $2.7 | $2.1 | $87.0 |
| 1981 | 110.5 | 13.3 | 4.0 | 1.8 | 0.9 | 90.7 | 8.9 | 5.8 | 3.1 | 2.3 | 102.1 |
| 1982 | 130.7 | 17.0 | 4.7 | 2.1 | 1.2 | 105.8 | 9.8 | 6.5 | 3.3 | 2.9 | 118.5 |
| 1983 | 150.5 | 23.0 | 5.7 | 2.4 | 1.5 | 117.9 | 10.0 | 6.7 | 3.3 | 3.2 | 131.1 |
| 1984 | 161.7 | 23.9 | 7.2 | 2.7 | 1.8 | 126.2 | 10.4 | 7.0 | 3.4 | 3.4 | 140.0 |
| 1985 | 170.1 | 23.4 | 7.3 | 2.7 | 1.4 | 135.2 | 10.4 | 6.6 | 3.8 | 4.1 | 149.8 |
| 1986 | 185.0 | 28.1 | 8.0 | 4.1 | 1.6 | 143.3 | 13.0 | 8.2 | 4.8 | 3.9 | 160.2 |
| 1987 | 204.7 | 36.4 | 8.8 | 4.2 | 2.7 | 152.6 | 15.6 | 10.2 | 5.4 | 3.8 | 172.0 |
| State and local hospitals | |||||||||||
| 1980 | $18.4 | $1.5 | $1.3 | $0.7 | $0.3 | $14.7 | $5.8 | $5.2 | $0.6 | $0.7 | $21.2 |
| 1981 | 21.3 | 1.8 | 1.4 | 1.0 | 0.3 | 16.8 | 6.2 | 5.6 | 0.6 | 0.6 | 23.8 |
| 1982 | 24.6 | 2.3 | 1.6 | 1.0 | 0.4 | 19.3 | 6.8 | 6.2 | 0.6 | 0.8 | 26.9 |
| 1983 | 28.3 | 3.5 | 2.0 | 1.1 | 0.7 | 21.0 | 7.0 | 6.4 | 0.5 | 0.9 | 28.9 |
| 1984 | 29.6 | 3.3 | 2.7 | 1.2 | 0.9 | 21.5 | 7.2 | 6.7 | 0.6 | 0.7 | 29.5 |
| 1985 | 30.5 | 3.5 | 2.4 | 1.1 | 0.4 | 23.0 | 6.8 | 6.2 | 0.7 | 0.9 | 30.7 |
| 1986 | 31.7 | 4.0 | 2.4 | 2.2 | 0.2 | 22.9 | 8.5 | 7.6 | 0.9 | 0.8 | 32.2 |
| 1987 | 33.5 | 4.9 | 2.6 | 2.1 | 0.4 | 23.5 | 10.5 | 9.6 | 0.9 | 0.8 | 34.8 |
| All-non Federal hospitals | Revenue as a percent of total net revenues from all sources | ||||||||||
| 1980 | 107.1 | 12.4 | 3.9 | 1.6 | 0.8 | 88.4 | 9.2 | 6.1 | 3.1 | 2.4 | 100.0 |
| 1981 | 108.3 | 13.0 | 3.9 | 1.8 | 0.9 | 88.8 | 8.7 | 5.7 | 3.1 | 2.3 | 100.0 |
| 1982 | 110.3 | 14.3 | 4.0 | 1.8 | 1.0 | 89.3 | 8.3 | 5.5 | 2.8 | 2.4 | 100.0 |
| 1983 | 114.8 | 17.6 | 4.3 | 1.8 | 1.1 | 90.0 | 7.6 | 5.1 | 2.5 | 2.4 | 100.0 |
| 1984 | 115.6 | 17.1 | 5.1 | 1.9 | 1.3 | 90.2 | 7.4 | 5.0 | 2.4 | 2.4 | 100.0 |
| 1985 | 113.6 | 15.6 | 4.9 | 1.8 | 1.0 | 90.3 | 7.0 | 4.4 | 2.5 | 2.7 | 100.0 |
| 1986 | 115.5 | 17.6 | 5.0 | 2.5 | 1.0 | 89.4 | 8.1 | 5.1 | 3.0 | 2.4 | 100.0 |
| 1987 | 119.0 | 21.2 | 5.1 | 2.5 | 1.6 | 88.7 | 9.1 | 5.9 | 3.2 | 2.2 | 100.0 |
| State and local hospitals | |||||||||||
| 1980 | 87.0 | 7.0 | 6.1 | 3.1 | 1.3 | 69.4 | 27.4 | 24.6 | 2.8 | 3.2 | 100.0 |
| 1981 | 89.8 | 7.6 | 6.0 | 4.3 | 1.3 | 70.6 | 26.2 | 23.6 | 2.6 | 2.5 | 100.0 |
| 1982 | 91.5 | 8.5 | 5.8 | 3.8 | 1.7 | 71.7 | 25.3 | 23.1 | 2.2 | 3.0 | 100.0 |
| 1983 | 97.9 | 12.2 | 6.9 | 3.9 | 2.3 | 72.6 | 24.2 | 22.3 | 1.9 | 3.2 | 100.0 |
| 1984 | 100.4 | 11.3 | 9.2 | 3.9 | 2.9 | 73.1 | 24.5 | 22.7 | 1.9 | 2.4 | 100.0 |
| 1985 | 99.1 | 11.5 | 8.0 | 3.6 | 1.2 | 74.8 | 22.3 | 20.1 | 2.1 | 3.0 | 100.0 |
| 1986 | 98.4 | 12.5 | 7.4 | 6.7 | 0.6 | 71.2 | 26.3 | 23.6 | 2.8 | 2.5 | 100.0 |
| 1987 | 96.3 | 14.2 | 7.4 | 6.1 | 1.0 | 67.5 | 30.1 | 27.6 | 2.5 | 2.4 | 100.0 |
NOTES: Revenues differ from those presented in the National Health Accounts tables. Data in this table cover a mixture of financial years reported by hospitals; also, Federal hospitals are not included. Numbers and percents may not add to totals because of rounding.
SOURCE: American Hospital Association, Hospital Data Center: Data from the Annual Survey of Hospitals for 1980-87.
The remaining 11.3 percent (derived from Table 2) of hospital revenues in 1987 came from sources not directly related to patient services: 5.9 percent ($10.2 billion) came from State and local subsidies, 3.2 percent from hospital services unrelated to patient care (operation of gift shops, cafeterias, parking lots, etc.), and another 2.2 percent from non-operating revenue (philanthropic giving, grants, and investment income).
The revenue picture for State and local hospitals differs dramatically from that of all other non-Federal facilities. State and locally owned facilities received only 67.5 percent of their revenue from patient sources in 1987. Their dependence on tax appropriations to subsidize operation is great and growing: 27.6 percent of all their revenues came from this source in 1987.
State and local hospitals' gross revenues (charges to patients before discounts) were 16 percent of all patient charges in non-Federal hospitals in 1987. Yet these facilities provided almost one-half of all charity care delivered by non-Federal hospitals and absorbed 30 percent of all hospital bad debt. The share of net revenue devoted to charity care by State and local hospitals—6.1 percent in 1987—doubled from 1980 through 1987.
Each month, AHA surveys 2,000 community hospitals for information on utilization and financial experience. In 1988, this National Hospital Panel Survey showed that U.S. community hospitals operated 942,300 beds (Table 3); provided 222.3 million inpatient days of care (44 percent of which was for the elderly) at an average cost of $632 per day; and tallied 33.5 million admissions (the elderly accounted for 33 percent), costing an average of $4,194 each (American Hospital Association, 1963-89). The average length of stay for all patients was 6.6 days, although the elderly stayed an average of 2.2 days longer. In addition, hospitals received an average of $126 per visit for each of the 296.1 million outpatient visits recorded in 1988. Community hospitals' profit margin in 1988 was 4.8 percent of total net revenue.
Table 3. Selected indicators from the American Hospital Association panel survey of community hospitals: Selected calendar years 1963-88.
| Calendar year | Number of beds in thousands | Occupancy rate | Admissions in millions | Inpatient days in millions | Average length of stay in days | Outpatient visits in millions | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Total | Age 65 or over | Under age 65 | Total | Age 65 or over | Under age 65 | All ages | Age 65 or over | Under age 65 | ||||
| 1963 | 695.5 | 77.2 | 26.0 | — | 26.0 | 196.0 | — | 196.0 | 7.5 | — | 7.5 | 77.7 |
| 1965 | 724.8 | 76.9 | 26.7 | — | 26.7 | 203.5 | — | 203.5 | 7.6 | — | 7.6 | 91.2 |
| 1970 | 830.7 | 77.6 | 30.1 | 6.2 | 23.9 | 235.3 | 78.4 | 156.9 | 7.8 | 12.6 | 6.6 | 136.6 |
| 1975 | 906.0 | 74.6 | 33.4 | 8.0 | 25.4 | 246.6 | 89.7 | 156.9 | 7.4 | 11.2 | 6.2 | 192.6 |
| 1980 | 970.5 | 75.9 | 37.6 | 10.5 | 27.0 | 269.6 | 109.1 | 160.5 | 7.2 | 10.4 | 5.9 | 217.8 |
| 1981 | 986.9 | 75.8 | 37.9 | 10.8 | 27.0 | 273.0 | 112.3 | 160.7 | 7.2 | 10.4 | 5.9 | 220.9 |
| 1982 | 997.7 | 74.5 | 37.9 | 11.3 | 26.6 | 271.4 | 114.2 | 157.2 | 7.2 | 10.1 | 5.9 | 223.3 |
| 1983 | 1,003.7 | 72.2 | 37.7 | 11.8 | 25.9 | 264.5 | 114.3 | 150.2 | 7.0 | 9.7 | 5.8 | 229.6 |
| 1984 | 992.6 | 66.6 | 36.3 | 11.5 | 24.8 | 241.8 | 103.0 | 138.8 | 6.7 | 8.9 | 5.6 | 232.8 |
| 1985 | 974.6 | 63.6 | 34.5 | 10.9 | 23.6 | 226.1 | 95.5 | 130.6 | 6.5 | 8.8 | 5.5 | 243.4 |
| 1986 | 963.1 | 63.4 | 33.8 | 10.8 | 23.0 | 222.9 | 94.9 | 128.0 | 6.6 | 8.8 | 5.6 | 263.6 |
| 1987 | 954.5 | 64.1 | 33.6 | 10.8 | 22.8 | 223.4 | 96.3 | 127.2 | 6.6 | 8.9 | 5.6 | 278.9 |
| 1988 | 942.3 | 64.5 | 33.5 | 11.1 | 22.4 | 222.3 | 97.5 | 124.8 | 6.6 | 8.8 | 5.6 | 296.1 |
| Average annual percent growth from previous year shown | ||||||||||||
| 1963 | — | — | — | — | — | — | — | — | — | — | — | — |
| 1965 | 2.1 | −0.2 | 1.3 | — | 1.3 | 1.9 | — | 1.9 | 0.6 | — | 0.6 | 8.4 |
| 1970 | 2.8 | 0.2 | 2.4 | — | −2.2 | 3.0 | — | −5.1 | 0.5 | — | −2.9 | 8.4 |
| 1975 | 1.8 | −0.8 | 2.1 | 5.2 | 1.2 | 0.9 | 2.7 | −0.0 | −1.1 | −2.3 | −1.2 | 7.1 |
| 1980 | 1.4 | 0.4 | 2.4 | 5.6 | 1.2 | 1.8 | 4.0 | 0.5 | −0.6 | −1.6 | −0.8 | 2.5 |
| 1981 | 1.7 | −0.2 | 0.9 | 3.0 | 0.0 | 1.2 | 2.9 | 0.1 | 0.4 | −0.1 | 0.1 | 1.4 |
| 1982 | 1.1 | −1.6 | 0.0 | 4.1 | −1.6 | −0.6 | 1.7 | −2.1 | −0.6 | −2.3 | −0.6 | 1.1 |
| 1983 | 0.6 | −3.1 | −0.5 | 4.7 | −2.8 | −2.5 | 0.1 | −4.5 | −2.0 | −4.4 | −1.7 | 2.8 |
| 1984 | −1.1 | −7.8 | −3.7 | −2.6 | −4.2 | −8.6 | −9.9 | −7.6 | −5.1 | −7.5 | −3.5 | 1.4 |
| 1985 | −1.8 | −4.5 | −4.9 | −5.2 | −4.7 | −6.5 | −7.2 | −5.9 | −1.7 | −2.1 | −1.3 | 4.5 |
| 1986 | −1.2 | −0.3 | −2.1 | −1.0 | −2.5 | −1.4 | −0.6 | −2.0 | 0.6 | 0.4 | 0.5 | 8.3 |
| 1987 | −0.9 | 1.2 | −0.6 | 0.4 | −1.0 | 0.2 | 1.4 | −0.6 | 0.8 | 1.0 | 0.4 | 5.8 |
| 1988 | −1.3 | 0.5 | −0.4 | 2.0 | −1.6 | −0.5 | 1.3 | −1.9 | −0.1 | −0.7 | −0.3 | 6.2 |
NOTES: Data labeled “Age 65 or over” corresponds closely to Health Care Financing Administration information on all Medicare beneficiaries, both aged and disabled. Numbers and percents may not add to totals because of rounding.
SOURCE: American Hospital Association: National Hospital Panel Survey Reports. Chicago, 1963-88.
The AHA panel survey also shows how hospitals have been forced to deal with reversals in long-established utilization trends that began in 1982.
Community hospitals experienced rapid growth in hospital revenues during 1980 and 1981. These increases affected employers, who were the primary providers of health insurance for their employees and who faced large increases in health insurance premiums. Employers sought ways to lower the cost of this fringe benefit. They experimented with health maintenance organizations, preferred provider organizations and utilization review, and required second opinions. Many large employers opted to self-insure for health care costs, enabling them to avoid State-mandated benefit coverage and State premium taxes. (Self-insurance falls under the purview of the Employee Retirement Income Security Act [ERISA], a federally regulated program that supersedes State requirements.)
Beginning in 1981, hospitals experienced no growth in hospital admissions for the population under age 65, followed by declines of 1.0-4.7 percent in the number of admissions each year through 1988 (Table 3). Average length of stay for the population under age 65 dropped during the period 1982-88, resulting in an even more pronounced fall in the number of inpatient days used by this age cohort.
In 1984, the Medicare population, primarily those 65 years of age or over, followed suit. In October 1983, Medicare began to implement PPS, which paid hospitals on the basis of the average cost for treating patients with a specific diagnosis. This replaced a cost-based reimbursement system, under which hospitals were paid on the basis of costs incurred in treating a patient. PPS encouraged timely discharge of patients, because a hospital would incur additional expense and no additional revenue for longer stays.
The impact on hospital utilization was immediate. The average length of stay in community hospitals dropped from 10.1 days in 1982 to 8.9 days in 1984 for the population 65 years of age or over. At the same time, admissions to community hospitals for the elderly fell 2.6 percent in 1984 and 5.2 percent in 1985. The overall result was a drop in inpatient days of 9.9 percent in 1984 and 7.2 percent in 1985 (Table 3).
The combined effect of both private and public sector initiatives caused the occupancy rate in community hospitals, which had been hovering at about 76 percent, to fall to 63.4 percent in 1986. Only reductions in the number of beds in operation, which peaked at more than 1 million in 1983 and then fell to 942,300 by 1988, raised the occupancy rate to 64.5 percent in 1988, 14 percentage points lower than the peak rate in 1968 (78.5 percent, data not shown).
Physician services
Expenditures for physician services have come under increasing scrutiny in the past several years, especially after the passage of PPS. PPS was intended to staunch the rising tide of hospital expenditures, and indeed, hospital utilization did slow during the 1980s. However, use of physician services and the associated costs have continued to rise. There also is growing concern that the benefits of many medical services and procedures are not commensurate with their costs (Physician Payment Review Commission, 1989). These factors led to growing pressure to find ways to slow the growth of expenditures for physician services, resulting in the passage of physician payment reform legislation in 1989. The data presented here show the trends that led to the passage of that legislation.
The physician expenditure estimates include spending for services received through offices of physicians or osteopathic physicians, spending for independent medical laboratory charges that are billed directly by the lab to the consumer, and benefits provided by salaried physicians in health maintenance organizations (HMOs).
The 1988 level of spending for physician services was $105.1 billion, up 13.1 percent from the 1987 level of $93.0 billion (Table 4). Physician services expenditure experienced average annual growth of 13.2 percent from 1986 through 1988, a rate exceeded only by the 16.5-percent average annual growth from 1979 through 1981 (a time of high economywide price inflation).
Table 4. Expenditures for physician services and professional fees paid to physicians by hospitals: Selected years 1960-88.
| Year | Total | Physician services without fees | Hospital professional fees |
|---|---|---|---|
|
| |||
| Amount in billions | |||
| 1960 | $5.4 | $5.3 | $0.1 |
| 1965 | 8.5 | 8.2 | 0.3 |
| 1970 | 14.2 | 13.6 | 0.6 |
| 1975 | 24.4 | 23.3 | 1.1 |
| 1980 | 44.4 | 41.9 | 2.5 |
| 1985 | 77.6 | 74.0 | 3.6 |
| 1986 | 86.0 | 82.0 | 4.0 |
| 1987 | 97.4 | 93.0 | 4.4 |
| 1988 | 109.8 | 105.1 | 4.7 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates from the Office of National Cost Estimates.
The physician expenditure share of PHCE declined from 1965 through the early 1980s as the hospital share increased. With the implementation of PPS, this trend has been reversed, with physician services expenditures making up for the drop in the hospital share. Physician services serve as both a complement to and a substitute for inpatient care. Prior to PPS, the complementarity was stressed: Each day in the hospital generated at least one physician visit. In the last several years, it is the substitutability that has been emphasized, as more and more procedures that had been done on an inpatient basis are performed in outpatient settings.
There has been substantial growth in physician supply. The total number of non-Federal physicians engaged in patient care almost doubled from 1965 through 1987, growing from 237,500 to 455,700 (American Medical Association, to be published). The number of active physicians per 100,000 population in those years was 124 and 189, respectively.
Data on the demand for physician services during the past 5 years show a change in the mix of services provided. A composite measure that includes hospital days (assuming one physician visit per patient per day), surgical procedures, and physician contacts in other than inpatient settings is used to measure use of physician services.
According to data from the AHA panel survey, inpatient days decreased 16.0 percent from 1983 through 1988. Except for a small increase in 1987, growth was negative in every year of the period, the largest decline being 8.6 percent in 1984, with the implementation of PPS. The overall decline in inpatient days over the period was partially offset by the increase in the number of surgical procedures, which grew a total of 7.4 percent (American Hospital Association, 1963-89).
It appears that some of the services previously performed in the hospital are now taking place in physician offices. Physician contacts in nonhospital settings increased 10.7 percent from 1983 through 1987. This contrasts with a decrease of 0.3 percent from 1976 through 1981 (National Center for Health Statistics, 1966-87).
When the three components of physician use are combined, the net effect is a cumulative increase in use of 7.9 percent from 1983 through 1988.
Another indication of the increased activity in physician offices is the growth of employment after 1983. According to data from the Bureau of Labor Statistics (1972-89), employment in offices of physicians has grown 5.6 percent per year, with the strongest growth (8.5 percent) occurring in 1988. Hours worked per week by nonsupervisory employees increased over the past 3 years after decreases in each of the previous 8 years. American Medical Association (1984-88) data also show an increase during the past several years in the number of hours physicians spent in direct patient activity per week.
Price inflation was the biggest factor contributing to the growth of expenditures for physician services. The physician services component of the Consumer Price Index (CPI) increased at a 6.9-percent annual rate from 1960 through 1988. With the exception of 1972 and 1973, when price controls were in effect, growth of physician prices outpaced overall price inflation during the entire period. Price inflation decelerated in the early 1980s, reaching a 12-year low of 5.8 percent in 1985, and then increased, remaining slightly above 7 percent for the last 3 years. When the effects of price inflation have been removed from the total, real expenditures grew at a 4.1-percent annual rate from 1960 through 1983; growth was slightly higher in the period after PPS was implemented, averaging 4.4 percent per year.
Over time, the private share of spending for physician services has fallen. Prior to 1966, 93 percent of physician services expenditures was paid for by private funds. With the implementation of the Medicare and Medicaid programs, this share dropped to 77 percent and has been decreasing gradually to its current level of 67 percent. The advent of Medicare affected out-of-pocket spending much more than it did private insurance benefits: The out-of-pocket share dropped to almost two-thirds of its pre-Medicare level, while the insurance share dropped almost imperceptibly. It appears that many of the elderly who had health insurance policies quickly converted them to medigap policies or continued their private coverage because they were unsure of the Medicare Part B benefits.
After Medicare's initial impact, the private health insurance share again began to increase and now pays for almost one-half (47.6 percent) of all spending on physician services. There are several factors that could account for this growth. There has been a slow but steady increase in the number of people with private health insurance coverage. The strong growth of HMOs and preferred provider organizations with minimal or no coinsurance and deductibles, combined with the increased number of policies with individual or family limits on out-of-pocket spending, has reduced the amount that is paid out of pocket. Problems with attempts to coordinate health insurance benefits, particularly in two-worker families in which both have employer-sponsored coverage, have resulted in some unknown amount of duplicate payments for the same service.
Since the implementation of Medicare, the out-of-pocket share of spending for physician services has continued to fall, although not nearly as rapidly as it had from 1965 through 1968. By 1988, the share had fallen to 18.9 percent of total spending. In 1960, out-of-pocket payments were twice the size of private health insurance benefits; by 1988, they were two-fifths the size of those benefits.
After private insurance, Medicare is the next largest payer of physician expenditures, accounting for 23.6 percent of the total in 1988. Medicare's share has grown every year since 1972 except for 1984, when a freeze on the growth of physician fees was implemented.
Various measures, such as physician fee freezes, have met with only short-term success in controlling the growth in program expenditures for physician services. This has led to a reform in the way Medicare will reimburse physicians for their services. Beginning in 1992, payments to physicians will be made on a fee schedule based on a resource-based relative value scale. Resource inputs include total work performed by the physician, practice costs (such as rent and wages), and malpractice insurance premiums. Other methods for controlling costs have also been enacted, such as volume performance standards and the combination of a target reimbursement level with the new fee schedule. It remains to be seen whether these changes will be any more effective than physician fee freezes in stemming the growth of expenditures for physician services.
Prior to this benchmark of the NHA, an element of double counting occurred because income earned by physicians through fee arrangements with hospitals was counted in the NHA both in hospital and in expenditures for physician services. Professional fees paid by hospitals to physicians are expense items for those hospitals. Thus, the fees account for a portion of hospital charges and revenues, which form the basis of national health expenditures for hospital care. However, those same medical professional fees were also counted in spending for physician services, because physician service expenditures were based on practice income. (A similar problem existed for dental fees but was insignificant compared with the double counting of physician fees.) To eliminate this problem, medical professional fees are now subtracted from physician revenues.
The fee arrangements previously counted twice in the NHA include minimum guaranteed income, percentage of departmental billings, and bonuses. With the decline in hospital admissions in recent years, hospitals are increasing their use of these types of incentives to attract physician business to their facilities (Burda, 1990). However, other hospital arrangements with medical professionals, including salaries and lease arrangements, did not pose a similar problem, because income from these arrangements is not part of practice income.
About one-quarter of all non-Federal physicians providing patient care (excluding residents) had some kind of financial arrangement with hospitals in 1981, yielding an average net fee of $59,500 (American Medical Association, 1983). These figures imply that physician income from hospitals was $4.7 billion, or 10 percent of 1981 national expenditures for physician services. However, some of this income includes salary arrangements and therefore must be excluded (self-employed and corporate physician business receipts do not include outside salaries of physicians). Unpublished data from the AHA were used to estimate this salary portion of income from hospitals, and the adjustment made to physician receipts to eliminate hospital professional fees is shown in Table 4.
Dental services
From 1960 through 1988, dental expenditures grew at an average annual rate of 10.2 percent, with more rapid growth in the 1970s and early 1980s. Expenditures reached $29.4 billion in 1988, an 8.5-percent increase from the previous year. Per capita spending for dental services amounted to $116.
Most of the financing for dental care in the United States comes from private sources; public spending, primarily Medicaid, accounted for only 3 percent of total dental expenditures. Private health insurance coverage for dental services had experienced rapid growth from 1970 through 1982, averaging 33.9 percent annually, as employers expanded services covered by private health insurance. Part of this expansion was the result of employers switching from traditional fee-for-service insurance arrangements to HMOs and PPOs. To attract their employees to these plans, employers offered added dental coverage to “sweeten the pot.” Other employers dropped traditional purchased insurance in favor of self-insurance, and some used the one-time savings from this move to offer their employees more coverage for the same price.
The trend of increasing dental coverage may be changing as businesses grapple with the rising cost of employee benefits. Dental plan participation was available to 56 percent of full-time employees with health insurance in medium and large firms in 1980; the proportion peaked at 77 percent in 1984 and then fell to 71 percent in 1986 (Jain, 1988) and to 66 percent in 1988. As a result, the annual growth in dental insurance expenditures from 1982 through 1988 slowed to 9.9 percent.
Out-of-pocket spending by consumers has been decreasing as a percentage of the total dental expenditures. In 1960, it accounted for 97 percent of the total; by 1988, it had fallen to 55 percent.
According to the National Center for Health Statistics's (1966-87) Health Interview Survey, Americans averaged 2.0 visits per year to dental offices in 1986, up from 1.6 in 1965. From 1965 through 1969, dental visits per capita decreased 1.5 percent per year. They increased 1.3 percent per year during the 1970s, and that growth accelerated to 2.7 percent per year in the 1980s. These changes in growth parallel the expansion of dental insurance coverage.
The mix of employees in the dental office is changing, with more services being performed by less skilled, lower paid employees. There was an average annual increase of 3.7 percent from 1983 through 1987 in the number of non-dentist employees (dental hygienists, technicians, etc.) in private practice dental offices. The number of dentists in private practice increased only 1.5 percent per year during the same period. Reflecting these growth rates, the ratio of support personnel to private practice dentists was 3.1 in 1983 and 3.4 in 1987 (American Dental Association, 1989).
Changes in dental disease incidence have permitted shifts to lower skilled employees. These changes include improved prevention of caries; a lower incidence of periodontal disease than had been projected; and a decline in tooth loss and edentulism (Brown, 1989). All these combine to change the complexity of dental services provided, which in turn allows more dental services to be provided by auxiliary personnel.
The change in the mix of services provided is reflected in changes in intensity per dental visit. From 1965 through 1980, intensity per visit (dollar cost per visit divided by the dental services component of the CPI) grew 3.2 percent per year on average. From 1981 through 1988, it decreased 2.6 percent per year.
Other professional services
This category includes spending for services of health practitioners other than physicians and dentists and expenditures for services rendered in outpatient clinics. (Expenditures for home health agencies, which previously were included in this category, are now shown separately.) A total of $22.5 billion was spent in 1988 for these other services, 5 percent of total PHCE. About 80 percent of these expenditures were paid for by private funds, with 37 percent paid by private health insurance, 32 percent paid directly by the consumer, and about 12 percent coming from philanthropic funds in the form of gifts and grants to clinics. Another 15 percent came from Federal funds (Medicare paid slightly more than 9 percent), and the remainder came from State and local funds.
From 1960 through 1988, the private share of funding for other professional services decreased 14 percentage points and the distribution among private payers changed dramatically. Private health insurance increased from 2 percent to 37 percent; however, this change is somewhat misleading. Until recent years, reported data from insurers did not separately show other professional service benefits, through a certain amount of these services is known to have been purchased under major medical coverage. Some of the growth in insurance payments for these services is attributable to prepaid plans: HMOs encourage the use of other health professionals in place of more costly physician services. Philanthropy's share of expenditure grew from 4 percent to 12 percent, and the out-of-pocket share dropped from 87 percent to 32 percent during this period.
Federal programs, primarily Medicare, absorbed the decline in the private share. State and local funding rose slightly as a percent of total spending through the late 1960s and then gradually declined to about 5 percent by 1980, where it has since remained.
In 1988, spending for care in outpatient clinics (kidney dialysis centers, rehabilitation centers, alcohol treatment centers, drug treatment centers, etc.) amounted to $12.2 billion, a 12.8-percent increase over the previous year. From 1960 through 1988, outpatient clinic expenditures grew at an average annual rate of 21.5 percent. Reflecting this rapid growth, clinics now account for a larger share of total expenditures. In 1960, they represented 9 percent of other professional expenditures and were comprised mostly of community health centers (CHCs). In 1988, they accounted for 54 percent of spending in the category, but CHCs represented only 5 percent.
It is difficult to find solid data on clinics in the United States. The principal Federal statistical agencies rely upon the Standard Industrial Classification (SIC) to group establishments. In the SIC used during the period covered by this article, the distinction between clinics and physician offices was not very clear. In addition, outpatient clinics in the SIC include staff-model HMOs; however, data collectors admit that many other types of HMOs may also be counted as outpatient clinics. For example, network HMOs act as insurers only, with services provided by participating physicians. Possible inclusion of these entities could skew estimates of outpatient clinics. Results of the 1987 economic census and implementation of the revised SIC should improve the capture of clinic information.
One type of clinic for which hard data are available at present is the CHCs. These clinics provide outpatient care for the poor, basically through neighborhood clinics. Prior to 1965, the main goal of these centers was to provide maternal and child health care, and principal funding came from the Maternal and Child Health Care program. In 1965, CHCs were placed under the auspices of the Office of Economic Opportunity (OEO). The program was expanded and the number of centers grew to cover more of the medically indigent. In 1974, OEO was dismantled, and responsibility for CHC funding fell to the Health Services Administration and the Alcohol, Drug Abuse, and Mental Health Administration (ADAMHA).
In 1988, CHC expenditures amounted to $1.0 billion in 549 centers. Public expenditures accounted for $0.7 billion, 73 percent of the total. This share has been slowly declining since 1960, with private health insurance and out-of-pocket spending accounting for the difference. According to unpublished data from the Health Resources and Services Administration (1983-88), Federal grants still account for 46 percent of total CHC expenditures, covering such programs as CHC grants, migrant health programs, black lung clinics, and Appalachian health programs. Besides Federal grants, CHCs receive payment from Medicare, Medicaid, other third parties and direct patient payments, plus State and local funds.
Spending for other licensed health practitioners reached $10.3 billion in 1988, up 10.3 percent from the 1987 level. This category includes expenditures for services rendered by chiropractors, optometrists, podiatrists, psychologists, and private duty nurses, among others. Growth in expenditures for these practitioners paralleled that of the other professional services category over the 28-year period, but at a lower rate: 11.0 percent per annum, compared with 13.8 percent for the other professional services category.
According to data from the Health Resources and Services Administration, the number of professional health practitioners has been growing steadily since the mid-1970s (Bureau of Health Professions, 1988). The supply of optometrists increased 22.1 percent from 1975 through 1986, and the number of podiatrists increased 50.7 percent during the same period. With the number of health professionals growing faster than the population, the ratio of the number of professionals to population has increased as well.
Personal income, in both nominal and real terms, increased during the 1970s, allowing people to spend more on what previously could have been considered discretionary types of health care. Growth in the number of health professionals, indicating the possibility of provider-induced demand, combined with the increased ability of consumers to pay for these services to produce very strong growth in this type of expenditure during the 1970s.
In addition to factors already mentioned, increased outpatient mental health benefits and alcohol and drug abuse treatment coverage offered by employer-sponsored private health insurance in recent years have led to strong growth in expenditures for the services of psychologists and outpatient treatment centers (clinics).
Home health care
The home health segment of the NHA measures a portion of the Nation's annual expenditures for medical care services delivered in the home. Medical care expenditures included are defined as preventive, supportive, therapeutic, or rehabilitative. Providers of home health care services presented here are Medicare-certified non-facility-based home health agencies (HHAs) and people delivering home health care services financed by Medicaid. The broader home health care industry definition of services, which is beyond the scope of the NHA, includes supportive social services, respite care, and adult day care.
Expenditures for services and supplies furnished by non-facility-based home health care agencies was $4,427 billion in 1988, an increase of 5.9 percent from spending in 1987 (Table 5). Growth in spending for home health care has slowed dramatically from the 30.9-percent average experienced from 1973 through 1984 to 6.3 percent per year from 1984 through 1988.
Table 5. Total NHE, Medicare, Medicaid, and other spending for home health care, facility-based and non-facility-based: Selected calendar years, 1970-88.
| Year | Total NHE home health | Medicare | Medicaid | Other total2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Total | Facility-based HHA1 | Non-facility-based HHA2 | Total | Facility-based HHA1 | Non-facility-based HHA2 | Total | Facility-based HHA1 | Non-facility-based HHA2 3 | ||
|
| ||||||||||
| Amount in millions | ||||||||||
| 1970 | $154 | $11 | $143 | $69 | $9 | $60 | $17 | $2 | $15 | $68 |
| 1975 | 446 | 42 | 404 | 222 | 29 | 193 | 99 | 13 | 86 | 125 |
| 1980 | 1,494 | 147 | 1,347 | 754 | 99 | 654 | 362 | 48 | 314 | 378 |
| 1985 | 4,401 | 561 | 3,841 | 2,133 | 365 | 1,769 | 1,142 | 196 | 946 | 1,126 |
| 1986 | 4,719 | 734 | 3,985 | 2,202 | 452 | 1,750 | 1,408 | 282 | 1,126 | 1,109 |
| 1987 | 5,041 | 859 | 4,182 | 2,211 | 508 | 1,703 | 1,753 | 351 | 1,402 | 1,077 |
| 1988 | 5,439 | 1,012 | 4,427 | 2,375 | 567 | 1,808 | 1,920 | 445 | 1,475 | 1,144 |
Included in the hospital spending category of the National Health Accounts (NHA).
Estimated spending reported in the home health care category of the NHA.
Medicaid spending for home health care delivered by non-facility-based HHAs and providers not affiliated with a formal HHA.
NOTES: NHE is national health expenditures; HHA is home health agency.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Spending for home health care furnished by facility-based HHAs is included with hospital care in this article. Including the hospital share, $5.439 billion was spent for home health care services in 1988. Recent studies estimate annual industrywide spending of $8.7 billion for home health care services (Rivlin and Wiener, 1988). The expanded industry definition of home health care services includes services delivered by non-Medicare providers and facility-based agencies, as well as services currently beyond the scope of the NHA.
Direct payments from patients or their families accounted for 46 percent of the private financing (about 12 percent of total spending) and the residual private share was split between private health insurance and nonpatient revenue. Estimates from research into long-term care financing options indicate that perhaps 20 percent of industrywide home health care expenditures (including those delivered by non-Medicare-certified providers and support services) is paid out of pocket (Rivlin and Wiener, 1988).
In 1988, public sources financed 75 percent of the home health services described in this article. More than one-half of the public spending was paid by Medicare and the rest by Medicaid. Medicare paid $1.8 billion for the 30 million visits and supplies furnished in the homes of Medicare beneficiaries in 1988 (Health Care Financing Administration, 1989).
In order to evaluate the spending estimates presented in this section, it is essential to understand both the extent and nature of HHA participation in the Medicare program. The number of facilities certified to participate in Medicare peaked at almost 6,000 in 1986 but declined to 5,700 in 1988. Data from three-quarters of these facilities (4,200) were used to construct these estimates. The broader home health care industry consists of about 11,000 agencies (Hoyer, 1990).
Changes occurring in the types of home health care agencies certified to participate in Medicare can be traced to legislation in 1980 and in 1983. The 1980 legislation eased Medicare certification requirements for proprietary HHAs in States without licensure laws (Ruther and Helbing, 1988). With implementation of Medicare's PPS in 1983, hospital presence in the home health care market has strengthened (Waldo, Levit, and Lazenby, 1986). The share of charges for home health care services billed to Medicare by facility-based agencies has grown from 15 percent in 1982 to 25 percent in 1988; proprietary facilities' share has more than doubled (Table 6). (For a more detailed discussion of changes occurring in the home health care industry, refer to the 1985 report on national health expenditures [Waldo, Levit, and Lazenby, 1986].)
Table 6. Distribution of charges for Medicare home health services, by type of agency: Calendar years 1982 and 1988.
| Type of agency | 1982 | 1988 |
|---|---|---|
|
| ||
| Percent | ||
| All agencies | 100 | 100 |
| Facility-based | 15 | 25 |
| Non-facility-based | 85 | 75 |
| Proprietary | 14 | 34 |
| Private nonprofit | 26 | 15 |
| Visiting nurse association | 32 | 20 |
| All other | 14 | 7 |
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Data from the 40-percent Home Health Agency Skeleton File.
The home health care expenditure estimate is extremely sensitive to changes in the Medicare program, as the estimate is based on Medicare data. The number of HHAs participating in Medicare, types of participating HHAs, and the mix of services offered by each, as well as Medicare coverage, reimbursement, and administrative policies, are reflected in the expenditure estimate. In 1988, Medicare clarified its home health coverage criteria and instituted measures to reduce the number of home health claim denials. The negative growth rates experienced in 1986 and 1987 were reversed, and Medicare spending increased by 6.1 percent. Because Medicare home health care expenditures are used to construct the total home health care estimate, growth of these expenditures strongly paralleled Medicare's home health care growth.
Drugs and other medical nondurables
Americans spent $41.9 billion on prescription drugs, over-the-counter (OTC) medicines, and other nondurable medical sundries in 1988. Spending for drugs and other nondurable medical products was one of the slowest growing components of personal health care in 1988, rising 8.5 percent from 1987 levels. This category accounted for 9 percent of all personal health care spending in 1988, down from 18 percent in 1960.
Prescription drugs purchased in retail outlets, including pharmacies, grocery stores, other retail stores, and mail-order houses, amounted to $27.1 billion in 1988 (Table 7), accounting for 65 percent of expenditures for drugs, and other nondurable medical products. Third-party payers typically pay for prescription drugs but not for OTC medicines. Therefore, most public and private insurance payments can be counted as reimbursement for prescription drugs.
Table 7. Expenditures for drugs and other medical nondurables, by source of funds: Calendar year 1988.
| Source of funds | Drugs and other medical nondurables | Prescription drugs | Nonprescription drugs and other medical nondurables1 |
|---|---|---|---|
| Amount in billions | |||
| Total | $41.9 | $27.1 | $14.8 |
| Out-of-pocket payments | 30.1 | 15.3 | 14.8 |
| Third-party payers | 11.8 | 11.8 | — |
| Private health insurance | 7.2 | 7.2 | — |
| Medicaid | 3.6 | 3.6 | — |
| General assistance | 0.6 | 0.6 | — |
| Other government programs | 0.3 | 0.3 | — |
| Percent distribution | |||
| Total | 100 | 100 | 100 |
| Out-of-pocket payments | 72 | 56 | 100 |
| Third-party payers | 28 | 44 | — |
| Private health insurance | 17 | 27 | — |
| Medicaid | 9 | 13 | — |
| General assistance | 1 | 2 | — |
| Other government programs | 1 | 1 | — |
Assumes no third-party payments for nonprescription drugs and other medical nondurables.
NOTE: Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Under that assumption, consumers paid for all nonprescription drugs and other medical nondurables out of pocket. These payments amounted to $14.8 billion in 1988. In addition, consumers directly paid another $15.3 billion for prescription drugs, with the remaining 44 percent of prescription drugs financed by third-party payers. Medicaid paid for 13 percent of all prescription drugs, and private health insurance financed 27 percent (derived from Table 7).
The aged population consumes a disproportionate share of prescription drugs. In 1977, for example, people 65 years of age or over used three times as many prescription drugs per capita as did the rest of the population (Kasper, 1982). Comparison of NHE data with estimates made for the Medicare Catastrophic Coverage Act of 1988 (Department of Health and Human Services, 1989) suggests that the elderly, who constituted 12 percent of the total population in 1988, accounted for 35 percent of prescription drug expenditures in that year.
To combat the high cost of prescription medicines for the elderly, several States initiated programs to assist elderly residents. These expenditures, listed in the NHA as part of State-operated general assistance programs, have grown rapidly in the handful of States that provide this benefit. New Jersey and Pennsylvania, which operate the largest of these assistance programs, spent $286 million on prescription drugs for the elderly in 1988—almost one-half of all drug expenditures in the general assistance programs.
Vision products and other medical durables
This category covers retail purchase or rental of such items as eyeglasses, other durable medical equipment, and hearing aids. Spending for these items reached $10.8 billion in 1988, growing at an average annual rate of 9.7 percent from 1960 through 1988. The majority of the funding (70 percent of the total) comes from consumers' out-of-pocket payments. Although most public programs do not cover these items, the public share of spending has grown from 2 percent in 1960 to 21 percent in 1988. Medicare is the primary program providing public funding.
The largest component of durable medical equipment (DME) is ophthalmic products (eyeglass lenses and frames, contact lenses, etc.) A detailed breakdown of this NHA category is available only in GNP benchmark years, the most recent of which was 1977. At that time, vision products accounted for 72 percent of total expenditures for DME. Orthopedic and prosthetic appliances and devices accounted for 13 percent of DME spending in that year, hearing aids and batteries for 10 percent, and equipment and supplies for the remaining 5 percent.
Nursing home care
The nursing home component of the NHA measures the Nation's annual expenditures for professionally supervised inpatient nursing care prescribed by a physician. National spending for nursing home care reached $43.1 billion in 1988, an increase of 8.5 percent from 1987 spending. Data from the Bureau of Labor Statistics (1972-89) show that growth in aggregate hours worked by nonsupervisory personnel in nursing and related care facilities (SIC 805) slowed from 4.8 percent in 1985 to 3.0 percent in 1988. Growth in nursing home employment showed a similar trend.
Part of the growth in spending for nursing home care from 1973 through 1981 was the result of rapid expansion in spending for services in intermediate care facilities for the mentally retarded (ICFs/MR), most of which are included under the general heading of nursing homes. ICF/MR care is a Medicaid benefit first offered in 1973. In 1988, $3.7 billion in ICF/MR expenditures (60 percent of the total) was spent in nursing homes. Despite the relatively small size of ICF/MR spending, these payments raised the growth rate for total nursing home spending in every year from 1973 through 1981. The rate of growth of ICF/MR, spending slowed from 46.3 percent in 1981 to 5.5 percent in 1988. Subsequent to the deceleration in growth of ICF/MR spending in 1982, ICF/MR expenditures have grown at about the same rate as total spending for nursing home care.
Growth in spending for nursing home care other than in ICFs/MR also slowed in almost every year since 1981. Part of this slowdown is the result of a deceleration in the growth of input prices paid by nursing homes. The Health Care Financing Administration's national nursing home input price index grew at an average annual rate of 5.0 percent during the 7-year period from 1981 through 1988, compared with a 9.0-percent annual growth from 1973 through 1981.
Almost 40 percent of the increase in expenditures for nursing home care other than for ICFs/MR from 1987 through 1988 was attributable to general price inflation, and 25 percent to inflation specific to the nursing home industry. Growth of the aged population in 1988 accounted for 23 percent of the growth in nursing home spending. Changes in the amounts and mix of nursing home goods and services account for the rest of the growth.
Estimates used in preparation of the NHE statistics show that the average charge per day for care in nursing home facilities reached $72 in 1988, triple the charge per day reported in the 1976-77 National Nursing Home Survey (National Center for Health Statistics, 1977).
The share of nursing home care financed by public programs declined from a high of 53.4 percent in 1981 to 48.6 percent in 1988. Almost all of that decline was in Medicaid's share. (Medicaid accounts for more than 90 percent of public spending for nursing home care.) Use of nursing home care by Medicaid and Medicare patients had been declining. However, growth in Medicare spending for skilled nursing home care rose in 1988 as a result of clarification of Medicare's conditions for payment.
Most of nursing home care financed from private sources is paid directly by patients or their families. However, not all of these direct payments are paid out of savings, investment, or pension income. In recent years, approximately 40 percent of the out-of-pocket spending comes from social security benefits paid to patients or their representatives.
According to data from the 1985 National Nursing Home Survey, 40 percent of nursing home residents in the survey period were 85 years of age or over. The resident rate per 1,000 population increases with age, from 12.5 residents per 1,000 population 65-74 years of age to 220 per 1,000 for people 85 years of age or over (National Center for Health Statistics, 1985). Growth of the age-85-or-over cohort is expected to continue to outpace growth of the total aged population into the next century.
Utilization data from various studies conducted by the National Center for Health Statistics (1972, 1977, and 1985) show slowing of annual growth rates in the number of beds, days of care, and number of residents for selected periods covering the past two decades (Table 8).
Table 8. Average annual percent growth in nursing home use and beds: Selected years 1963-88.
| Period | Beds | Days | Residents | Beds per 1,000 people 85 years of age or over | Population age | |
|---|---|---|---|---|---|---|
|
| ||||||
| 65 years or over | 85 years or over | |||||
|
| ||||||
| Average annual percent growth | ||||||
| 1963-64 | 9.1 | 11.0 | 13.5 | 6.0 | 1.8 | 2.9 |
| 1964-71 | 10.4 | 10.4 | 9.8 | 5.1 | 1.9 | 5.0 |
| 1971-76 | 4.5 | 4.1 | 5.5 | −0.5 | 2.2 | 5.0 |
| 1976-85 | 1.6 | 1.7 | 1.5 | −2.6 | 2.2 | 4.2 |
| 1971-88 | 2.3 | — | — | −1.9 | 2.2 | 4.2 |
SOURCE: National Center for Health Statistics: Data developed by Health Care Financing Administration, Office of the Actuary.
The number of nursing home beds is not growing as quickly as is the population most in need of them. The nursing home bed supply grew at an average annual rate of 2.3 percent from 1971 through 1988, reaching 1.6 million in 1988. During the same period, the population 85 years of age or over (the elderly aged) grew 4.2 percent per year, resulting in an annual decline of almost 1.9 percent in beds per 1,000 elderly aged. With occupancy rates hovering at 90 percent, there appears to be a need for more long-term care beds.
Under current public budget constraints, advocacy groups for the aged population are concerned about shrinking Federal funds available for construction and maintenance of Department of Veterans Affairs (DVA) nursing facilities. With a growing population of aged veterans to care for, the overflow of veteran patients from DVA nursing facilities could compete for the available supply of private beds, depriving Medicaid patients of access to care. DVA patients may be admitted before Medicaid patients because the DVA payment rate is likely to be more generous than State-controlled Medicaid rates. Nursing homes, seeking to maximize profits, may also prefer DVA patients to Medicare patients. Medicare coverage of nursing home care is limited to skilled care for a relatively short stay, and Medicare patients requiring longer or less intensive nursing home care may become dependent upon Medicaid. Across the nursing home industry, lack of private financing and low profitability (3 percent in 1984 [Moglen et al., 1989]) because of current public reimbursement policies provide little incentive for expansion.
The increasing need for long-term care financing mechanisms has prompted private health insurers to experiment with long-term care coverage policies. Private health insurance has offered some coverage of nursing home care since the mid-1960s. Currently, long-term care policies are being marketed; by the end of 1989, 1.5 million policies had been sold (Health Insurance Association of America, 1990). However, benefits paid have never accounted for more than 1 percent of total spending for nursing home care. Purchase and ownership requirements, as well as coverage and benefit restrictions of currently marketed long-term care private health insurance policies, may prove them to be of little assistance in relieving the burden of patients who are paying for nursing home care (Wilson and Weissert, 1989).
Other personal health care
This category provides a catchall for funds that are known to be spent for health care but for which the object is unknown or not classifiable elsewhere. A total of $9.3 billion was expended for other personal health care in 1988. For example, expenses for shipboard and field health stations operated by the Department of Defense are in this category, as are nonhospital expenditures by the Alcohol, Drug Abuse, and Mental Health Administration. School health programs constitute a large portion of State and local expenditures in the category. The private expenditure in this category is for industrial in-plant services, discussed later in this article. An explanation of changes made to the definition of this category can be found in the companion article in this issue.
Government public health activity
Public health functions of Federal, State, and local governments accounted for $15.9 billion in 1988, about 3 percent of all NHE.
Federal Government public health spending increased twice as fast as did State and local spending in 1988, reaching $1.9 billion, with the Centers for Disease Control (CDC) accounting for almost 40 percent of that amount. The 15.9-percent growth in Federal spending resulted from large increases in CDC's budget for infectious disease prevention, mainly related to acquired immunodeficiency syndrome (AIDS). State and local public health agencies spent $14.0 billion delivering community health services, primarily through their respective health departments.
Other national health expenditures
National health expenditures devoted to nonprofit research and to construction of medical facilities were $19.4 billion in 1988. This amount represents less than 4 percent of all NHE. Expenditures for research and construction were almost evenly split between these two components. Spending for noncommercial research and development amounted to $9.9 billion, up 10.1 percent from 1987 (Table 9). Most of the funding for noncommercial research (80 percent in 1988) came from the Federal Government. State and local governments funded 12 percent of research in 1988 through the activities of public colleges and universities, and philanthropic funds financed the remaining 8 percent.
Table 9. Total medical research expenditures, including commercial research by drug companies: Selected calendar years 1960-88.
| Calendar year | Research expenditures | ||
|---|---|---|---|
|
| |||
| Total | Noncommercial | Commercial | |
|
| |||
| Amount in billions | |||
| 1960 | $0.9 | $0.7 | $0.2 |
| 1965 | 1.8 | 1.5 | 0.3 |
| 1970 | 2.5 | 2.0 | 0.5 |
| 1975 | 4.2 | 3.3 | 0.8 |
| 1980 | 7.0 | 5.4 | 1.5 |
| 1985 | 11.0 | 7.8 | 3.2 |
| 1986 | 12.3 | 8.5 | 3.7 |
| 1987 | 13.3 | 9.0 | 4.3 |
| 1988 | 14.9 | 9.9 | 5.0 |
NOTE: Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Research expenditures of drug and medical supply companies are excluded from the NHA. This type of research—commercial in nature—is treated as a business expense and is financed through sales of goods or services counted elsewhere in the NHA. In 1988, the commercial pharmaceutical industry spent $5.0 billion on the development of new drugs (Table 9), which would increase total research by approximately 50 percent over the amount estimated for noncommercial research alone.
Expenditures for the construction and renovation of hospitals, nursing homes, medical clinics, and medical research facilities amounted to $9.5 billion in 1988. Construction of hospital facilities slowed from 1984 through 1986 as a result of low occupancy rates in community hospitals. This overcapacity resulted from public and private sector initiatives in the early 1980s to reduce the growth in hospital spending, which led to reductions in admissions and lengths of stay. Hospitals were reluctant to embark on construction projects given such low occupancy rates during this period.
In 1987 and 1988, construction expenditures grew, rising 15.3 percent in 1988. It appears that construction projects held in abeyance during the mid-1980s are taking place. Some of this construction occurs in hospitals: Eager to attract patients and physicians, they are embarking on construction and renovation projects to increase their competitive edge.
In 1988, three-quarters of all construction was funded through the private sector, that is, through private philanthropy, hospital reserves, and debt financing, including tax-exempt bonds. The remaining 25 percent was financed by the Federal (9 percent) and State and local (16 percent) governments.
Expenditures by source of funds
The basic redistribution of expenditures between private and government sources appears to have reached a rough equilibrium during the 1980s. In 1960, private payments accounted for 75.5 percent of national health expenditures; the Federal Government paid for 10.7 percent (mostly through the Department of Defense and the Veterans Administration), and State and local governments financed the remaining 13.8 percent. Throughout the late 1960s and the 1970s, the Federal share grew, while the consumer share fell, and the State and local share remained constant. By 1980, private sources accounted for 57.8 percent of expenditures for health, the Federal Government for 28.9 percent, and State and local government for 13.3 percent. Since 1980, these fractions have changed very little.
Private funds
Private health insurance
Private health insurers earned $174.9 billion in premiums in 1988, an increase of 11.9 percent from 1987. Insurers incurred benefit obligations totaling $155.2 billion. The net cost of private health insurance—that is, the difference between premiums earned and benefits paid—amounted to $19.7 billion.
Private health insurance paid for almost one-third (32.4 percent) of all personal health care services delivered. The most heavily insured services are those for which the cost per unit of service is greatest. Because 81 percent of all private health insurance is obtained through employer-sponsored plans (Moyer, 1989), the most heavily insured services are also those services used by the nonelderly working population. Because the nonelderly use nursing home care infrequently, this service tends to be excluded from the package of benefits supplied by employers, accounting, in part, for the low share of private health insurance benefits paid for nursing home care.
In 1988, private health insurance paid for 35.4 percent of hospital care, 47.6 percent of physician services, 42.1 percent of dental services, and 36.9 percent of other professional services. Private health insurance funded only 7.0 percent of home health care, 18.4 percent of drugs and other medical nondurable products, and 8.8 percent of vision products and other medical durable products. It paid for 1.1 percent of nursing home care.
The share of personal health care financed by private health insurance grew steadily from 1960 through 1988, with the exception of a small drop in share when Medicare and Medicaid were implemented in 1966. During the period 1967-88, the share of hospital services paid for by private health insurance remained stable at about 35 percent. In all other services, however, the share has risen.
As the cost of health care rose, there was an increased demand by workers for broader health insurance coverage. During the late 1970s and early 1980s, many large companies switched to self-insurance in an effort to contain the growth of health care costs. Self-insurance fell under the jurisdiction of the Federal ERISA laws, allowing employers to avoid State premium taxes and State-mandated benefits. Self-insuring provided employers with a one-time reduction in costs often used to expand covered services.
About 75 percent of all Americans (or 181.4 million persons) are covered by some type of private health insurance. Eighty-nine percent of those who are covered are under the age of 65 (Moyer, 1989).
From 1980 through 1986, a series of laws was enacted to make Medicare a secondary payer to other insurers for Medicare-covered services provided to three groups of beneficiaries. First, the legislation made Medicare the second payer when claims are also covered by automobile, no-fault, or any liability insurance. Second, Medicare is a secondary payer during the first year of eligibility for people with end stage renal disease. The third—and largest—group affected by secondary-payer legislation is aged Medicare enrollees employed in certain organizations offering private health insurance coverage. This group also includes Medicare enrollees covered as dependents under a spouse's employer-sponsored policy. The savings to the Medicare program were $1.9 billion in fiscal year 1988, with those savings presumably paid by other third-party insurers (Health Care Financing Administration, 1990).
Out of pocket
Consumers spent $113.2 billion out of pocket for personal health care services in 1988, a 10.5-percent increase from 1987. This amount includes all spending for coinsurance and deductibles required by third-party insurers, payment for services not covered by insurers at all, and payment for charges in excess of “reasonable and customary” charges allowed by third parties. Excluded from this category are out-of-pocket payments for private health insurance premiums and out-of-pocket payments that are subsequently reimbursed by a third party.
Currently, slightly less than one-quarter (23.7 percent) of all personal health care costs are paid out of pocket. This share fell from 55.9 percent in 1960 to 23.7 percent in 1988. There appears to be a desire on the part of consumers to keep out-of-pocket spending at a target level. When out-of-pocket spending is compared with disposable income, the out-of-pocket share has remained fairly constant since 1950, between 3.0 and 3.9 percent of disposable income (Table 10). Despite the rapid rise in health care prices, consumers in general think that they have managed to insulate themselves from the brunt of escalating costs through the use of third-party insurers, either private or public. However, these costs have not been avoided, but merely deferred, and will be paid in the form of higher health insurance premiums, lower cash wages, higher prices, or a combination thereof (Levit, Freeland, and Waldo, 1989).
Table 10. Out-of-pocket spending for health care as a percent of disposable income: Selected calendar years 1950-88.
| Calendar year | Disposable income1 in billions | Out-of-pocket expenditures | |
|---|---|---|---|
|
| |||
| Health care in billions | As percent of disposable income | ||
| 1950 | $207.5 | 2$7.1 | 23.4 |
| 1955 | 278.8 | 29.1 | 23.3 |
| 1960 | 358.9 | 13.3 | 3.7 |
| 1965 | 486.8 | 19.0 | 3.9 |
| 1970 | 715.6 | 25.6 | 3.6 |
| 1975 | 1,142.8 | 38.5 | 3.4 |
| 1980 | 1,918.0 | 58.4 | 3.0 |
| 1985 | 2,838.7 | 91.7 | 3.2 |
| 1986 | 3,013.3 | 96.8 | 3.2 |
| 1987 | 3,205.9 | 102.4 | 3.2 |
| 1988 | 3,477.8 | 113.2 | 3.3 |
Estimated by the Department of Commerce, Bureau of Economic Analysis.
Historical data as published by the Social Security Administration, Office of Research and Statistics: Compendium of National Health Expenditure Data. DHEW Pub. No. (SSA) 76-11927. Department of Health, Education, and Welfare. Washington U.S. Government Printing Office Jan. 1976.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
The share of care funded out of pocket varies by type of service. For hospital care, consumers pay directly for 5.3 percent of their care; for drugs and other nondurable medical products, and vision products and other durable products, consumers pay more than 70 percent of the cost.
Nonpatient revenues including philanthropy
Health care providers received $14.6 billion in nonpatient revenues during 1988, an 8.5-percent increase since 1987. Nonpatient revenues in the form of philanthropic giving or income from other nonpatient sources subsidized 3 percent of personal health care spending, up from 1 percent in 1960. More than 6 percent of research and construction is funded by philanthropy, a substantial reduction from the 26 percent funded by philanthropy in 1960.
Philanthropy finances health care in every personal health care category except drugs and other medical nondurables and vision products and other medical durables. Other nonpatient sources of revenue, such as revenue derived from the operation of cafeterias, gift shops, and parking lots and from investment income, are used by hospitals and nursing homes to offset expenses incurred in delivering patient care. To a limited extent, home health agencies also cover expenses with nonpatient revenues other than philanthropy.
Industrial in-plant spending and private financing of construction
In the NHA, spending by business for health is limited to two types of expenditure: construction financed from reserves or private debt, and industrial in-plant expenditures. Private health insurance premiums, Medicare taxes, and other employer expenses are included elsewhere. (If one were to aggregate these expenses, it would be seen that business' share of health expenditures has been rising over time [Levit, Freeland, and Waldo, 1989].)
Industrial in-plant expenditures are defined as those made for facilities or supplies provided by employers for the health needs of their employees. These on-site or off-site services account for less than 1 percent of the total employers' payroll (Institute for Social Research, 1957), but the cost of these health programs is recovered through savings in worker productivity and absenteeism (Tsai, Baun, and Bernacki, 1987).
In 1988, employers spent $1.9 billion on industrial in-plant services. This is an increase of 8.2 percent from 1987. During the past 30 years, there has been a trend to increase this expenditure. From 1960 through 1973, the amount spent on industrial in-plant services grew slowly. From 1974 through 1987, it grew at a faster rate because of the rising cost of health care.
Establishments providing health care services vary in complexity, purpose, and size. Larger companies are more likely to have more comprehensive services, including medical personnel such as full-time or part-time physicians and/or nurses on their payroll, whereas smaller companies are more likely to have a health station or a first-aid kit for on-the-job illnesses or accidents (Kleinfeld et al., 1972). Employers offer different services, depending upon their business. For example, a manufacturer of precision instruments may pay for vision care, but a producer of toxic materials may offer physical exams (Klem and McKiever, 1952). Some companies require physical exams before hiring employees (Kleinfeld et al., 1972), which may produce a secondary savings by detecting potential problems at an early stage.
Because most absences are the result of non-occupational illnesses, preventive health practices save employers money and increase productivity (Lynch et al., 1990). Healthy employees have healthier attitudes if they are not worried about health status and are less likely to use sick leave (Jones, Bly, and Richardson, 1990). In the long run, reducing illness is advantageous to both the employee and the employer.
Government spending
During the last 28 years, two trends have developed regarding government spending for health. First, government programs have accounted for an increasing share of total spending. Second, health spending has accounted for an increasing share of government budgets.
In 1988, public programs paid for 42.1 percent of NHE. This proportion has changed little since the early 1970s, but is considerably higher than the 25-percent share that antedated the Medicare program. Government involvement with health care financing varies by type of service. For example, public funds covered 54.4 percent of hospital care and 48.6 percent of nursing home care in 1988, but only 10.9 percent of nondurables and 2.5 percent of dental services.
Medicare and Medicaid are the two largest government programs. Between them, they financed 30 percent of personal health care expenditures in 1988 and accounted for three-quarters of all such public spending.
Health care spending by government programs has accounted for an increasing share of both Federal and State and local government budgets (Figure 5). Implementation of the Medicare program in mid-1966 raised the health share of the Federal budget, although an upward trend in that share was already in evidence. Growth in the share of State and local budgets occupied by health was less the result of acceleration of health expenditures than it was a slowdown in growth of other expenditures.
Figure 5. Government health expenditures as a percent of total government expenditures: Calendar years 1960-88.
Medicare
Medicare is a Federal insurance program, created by Title XVIII of the Social Security Act in 1965, that began coverage in July 1966. It was originally designed to protect people 65 years of age or over from the high cost of health care. In 1972, it was expanded to cover permanently disabled workers and their dependents eligible for old age, survivors, and disability insurance benefits, as well as people with end stage renal disease.
Medicare has two parts, each with its own trust fund. The hospital insurance (HI) program pays for inpatient hospital services, home health care services, and hospice care. The supplementary medical insurance (SMI) program covers physician services, outpatient hospital services and therapy, and a few other services.
Unlike other Federal health programs, Medicare is not financed solely by general revenue (appropriations from general tax receipts). In 1988, 90.7 percent of the income for the HI program (Table 11) came from a 1.45-percent payroll tax levied on employers and on employees for the first $45,000 of wages. (Self-employed people were required to contribute 2.9 percent, the equivalent of both the employer's and the employee's share of the HI tax.)
Table 11. Payments into Medicare trust funds and percent distribution, by type of fund and source of income: Selected calendar years, 1967-88.
| Year and source of income | Total | Hospital insurance trust fund | Supplementary medical insurance trust fund | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Amount in billions | Percent distribution | Amount in billions | Percent distribution | Amount in billions | Percent distribution | |
| 1967 | ||||||
| Total | $5.2 | 100.0 | $3.6 | 100.0 | $1.6 | 100.0 |
| Payroll taxes | 3.2 | 62.0 | 3.2 | 89.8 | — | — |
| General revenues | 1.2 | 24.1 | 0.3 | 8.8 | 0.9 | 58.4 |
| Premiums | 0.6 | 12.4 | — | — | 0.6 | 40.1 |
| Interest | 0.1 | 1.5 | 0.1 | 1.4 | 0.0 | 1.5 |
| 1972 | ||||||
| Total | 9.2 | 100.0 | 6.4 | 100.0 | 2.8 | 100.0 |
| Payroll taxes | 5.8 | 62.9 | 5.8 | 90.5 | — | — |
| General revenues | 1.8 | 19.7 | 0.4 | 6.7 | 1.4 | 49.5 |
| Premiums | 1.4 | 15.0 | — | — | 1.4 | 49.2 |
| Interest | 0.2 | 2.4 | 0.2 | 2.8 | 0.0 | 1.3 |
| 1982 | ||||||
| Total | 54.6 | 100.0 | 38.0 | 100.0 | 16.6 | 100.0 |
| Payroll taxes | 34.9 | 64.0 | 34.9 | 91.9 | — | — |
| General revenues | 13.3 | 24.4 | 1.0 | 2.7 | 12.3 | 74.1 |
| Premiums | 3.7 | 6.8 | 0.0 | 0.1 | 3.7 | 22.3 |
| Interest | 2.6 | 4.8 | 2.0 | 5.3 | 0.6 | 3.6 |
| 1988 | ||||||
| Total | 105.1 | 100.0 | 69.2 | 100.0 | 35.8 | 100.0 |
| Payroll taxes | 62.8 | 59.8 | 62.8 | 90.7 | — | — |
| General revenues | 26.8 | 25.5 | 0.6 | 0.8 | 26.2 | 73.1 |
| Premiums | 8.8 | 8.4 | 0.0 | 0.1 | 8.8 | 24.5 |
| Interest | 6.7 | 6.4 | 5.8 | 8.4 | 0.9 | 2.4 |
NOTES: 0.0 denotes less than $50 million. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
The SMI program was financed by monthly premium payments of $24.80 per enrollee and by general revenue. The general revenue share of SMI receipts grew from 49.5 percent in 1972 to 73.1 percent in 1988. Since 1984, premiums have been set to cover 25 percent of the costs incurred by aged beneficiaries.
Medicare is consuming an increasing share of the Federal budget. Medicare benefit payments under the HI and SMI programs reached $85.7 billion in fiscal year 1988, about 8 percent of the total $1.1 trillion Federal budget. In fiscal year 1980, payments for benefits covered by Medicare represented 6 percent of the Federal budget.
Almost 30 million aged and 3 million disabled people were enrolled in Medicare in 1988 (Table 12). The program spent $89.7 billion in personal health care (benefit) payments for expenses incurred in 1988 by the 24.9 million Medicare users who received benefits. Growth in Medicare spending for personal health care accelerated to 9.8 percent in 1988 from the 8.4-percent growth experienced in 1987.
Table 12. Personal health care expenditures under Medicare and Medicaid and sources of Medicare financing: Calendar years 1966-88.
| Year | Personal health care expenditures | Population | Medicare financing | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Medicare and Medicaid1 | Medicare | Medicaid | Medicare2 | Medicaid recipients5 | Inpatient hospital deductible6 | SMI monthly premium7 | Annual maximum taxable earnings | Contribution rate8 | ||
|
| ||||||||||
| Enrollees3 | Users4 | |||||||||
|
| ||||||||||
| Amount in billions | Number in millions | Amount in dollars | Percent | |||||||
| 1966 | $2.9 | $1.6 | $1.3 | 19.1 | 3.7 | — | $40 | $3.00 | $6,600 | 0.35 |
| 1967 | 7.9 | 4.9 | 3.0 | 19.5 | 7.2 | — | 40 | 3.00 | 6,600 | 0.50 |
| 1968 | 9.3 | 5.9 | 3.4 | 19.8 | 7.9 | — | 40 | 4.00 | 7,800 | 0.60 |
| 1969 | 10.8 | 6.8 | 4.0 | 20.1 | 8.6 | — | 44 | 4.00 | 7,800 | 0.60 |
| 1970 | 12.3 | 7.2 | 5.1 | 20.5 | — | — | 52 | 5.30 | 7,800 | 0.60 |
| 1971 | 14.5 | 8.1 | 6.4 | 20.9 | 9.4 | — | 60 | 5.60 | 7,800 | 0.60 |
| 1972 | 16.8 | 8.8 | 8.0 | 21.3 | 10.0 | 17.6 | 68 | 5.80 | 9,000 | 0.60 |
| 1973 | 19.2 | 10.2 | 9.1 | 23.5 | 10.2 | 19.6 | 72 | 96.30 | 10,800 | 1.00 |
| 1974 | 23.4 | 12.8 | 10.6 | 24.2 | 11.8 | 21.5 | 84 | 6.70 | 13,200 | 0.90 |
| 1975 | 28.6 | 15.7 | 12.9 | 25.0 | 13.0 | 22.0 | 92 | 6.70 | 14,100 | 0.90 |
| 1976 | 33.4 | 18.9 | 14.5 | 25.7 | 14.1 | 22.8 | 104 | 7.20 | 15,300 | 0.90 |
| 1977 | 38.6 | 22.1 | 16.6 | 26.5 | 14.9 | 22.8 | 124 | 7.70 | 16,500 | 0.90 |
| 1978 | 44.3 | 25.8 | 18.5 | 27.2 | 15.9 | 22.0 | 144 | 8.20 | 17,700 | 1.00 |
| 1979 | 51.3 | 30.1 | 21.2 | 27.9 | 16.9 | 21.5 | 160 | 8.70 | 22,900 | 1.05 |
| 1980 | 61.2 | 36.4 | 24.8 | 28.5 | 18.0 | 21.6 | 180 | 9.60 | 25,900 | 1.05 |
| 1981 | 72.7 | 43.8 | 28.9 | 29.0 | 18.9 | 22.0 | 204 | 11.00 | 29,700 | 1.30 |
| 1982 | 81.9 | 51.4 | 30.6 | 29.5 | 18.8 | 21.6 | 260 | 12.20 | 32,400 | 1.30 |
| 1983 | 92.0 | 58.5 | 33.6 | 30.0 | 19.7 | 21.6 | 304 | 12.20 | 35,700 | 1.30 |
| 1984 | 100.3 | 64.3 | 36.0 | 30.5 | 20.7 | 21.6 | 356 | 14.60 | 37,800 | 101.30 |
| 1985 | 109.8 | 70.1 | 39.7 | 31.1 | 22.3 | 21.8 | 400 | 15.50 | 39,600 | 101.35 |
| 1986 | 118.2 | 75.4 | 42.9 | 31.7 | 23.1 | 22.5 | 492 | 15.50 | 42,000 | 101.45 |
| 1987 | 130.0 | 81.7 | 48.2 | 32.4 | 24.3 | 23.2 | 520 | 17.90 | 43,800 | 101.45 |
| 1988 | 142.0 | 89.7 | 52.3 | 33.0 | 1124.9 | 22.9 | 540 | 24.80 | 45,000 | 101.45 |
Excludes “buy-in” premiums paid by Medicaid for SMI coverage of aged and disabled Medicaid recipients eligible for coverage.
Hospital insurance and/or supplementary medical insurance.
Enrollees as of July 1 of specified year.
Enrollees with some reimbursement under Medicare during calendar year. Data through 1973 reflect aged users only. Data for 1974 and later include aged and disabled users.
Unduplicated count of Medicaid recipients during fiscal year.
As of January of specified year with the exception of 1966, for which July data are used.
As of July for 1966-83 and as of January for 1984-88.
Employer and employee (each) and self-employed people through 1983.
Monthly premiums for July and August 1973 were reduced to $5.80 and $6.10, respectively, by the Cost of Living Council.
Self-employed people pay double this rate, the equivalent of both the employer and the employee share.
Estimated.
NOTES: SMI is supplementary medical insurance. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
In 1988, Medicare financed 46.3 percent of the public share of personal health care expenditures and 18.8 percent of total spending for personal health care. Sixty-five percent of Medicare benefits were for hospital care; another 28 percent were paid for physician services.
In October 1983, prospective payment using diagnosis-related groups was implemented for Medicare hospital inpatients. The goal of PPS was to slow rapidly growing Medicare expenditures by encouraging hospitals and physicians to consider the economic consequences of prescribed courses of treatment. As a result of PPS, other cost-containment measures, and a slowdown in the rate of overall inflation, growth in Medicare payments for hospital care decelerated from 21.4 percent in 1980 to a low of 5.2 percent in 1986. Medicare expenditures for all hospital care services (including inpatient, outpatient, and hospital-based home health agency services) grew 8.0 percent in 1988, reaching $58.3 billion.
Medicare spending for physician services grew more than twice as fast as program spending for hospital care from 1984 through 1988. Medicare's share of total expenditures for physician services—24 percent in 1988—increased in almost every year since 1973. A freeze on physician fees for Medicare services was imposed in 1984 to slow the double-digit growth in these payments.
In 1984, incentives were devised to encourage physician participation in the Medicare program. Participating-provider legislation was enacted not only to reduce total expenditures for physician services but also to limit Medicare beneficiaries' burden for balance billing amounts. Participating physicians agree to accept Medicare's determination of reasonable charges for all their Medicare patients and do not bill these patients for any additional charges. The number of participating physicians and suppliers has been growing. In April 1988, 37 percent of the 665,000 billing arrangements signed by physicians were agreements to participate in the program, compared with 27 percent in 19861.
The freeze on fees of Medicare participating physicians was eased in 1986, as growth in program expenditures for physician services slowed from 17.9 percent in 1983 to 14.0 percent in 1988. Growth in fees paid to nonparticipating physicians (those who choose to bill Medicare patients for amounts exceeding the Medicare-determined reasonable charge) is being restrained by Congress.
Reductions in Medicare payments for overpriced procedures, fee schedules based on a resource-based relative value scale, and a mechanism for adjusting growth in Medicare physician payments based on volume performance standards are all examples of current attempts to control the growth in Medicare spending for physician services. Relative value scales have been developed to measure the resource-input costs of work expended by the physician, practice costs, and malpractice insurance costs.
The Medicare Catastrophic Coverage Act of 1988 attempted the first major expansion of the Medicare program since the inclusion of disabled beneficiaries and people with renal disease in 1973. Coverage of prescription drugs and other health services, as well as liberalized coverage of inpatient hospital, skilled nursing, and home health benefits were to be phased in over several years beginning in 1989. HI benefits of $4.4 billion were incurred in calendar year 1989 as a result of the new legislation. However, financing mechanisms designed to pay for these expanded services brought a storm of protest from aged taxpayers and the Act was repealed in December 1989 before the expanded SMI and prescription drug benefits were implemented.
Medicaid
In 1988, Medicaid spent $52.3 billion of combined Federal and State funds, which accounted for 10.9 percent of personal health care spending. Medicaid expenditures are largely institutional, with 39 percent spent on hospital care and 37 percent spent on nursing home care. Medicaid continues to be the largest third-party payer of long-term care, financing 44.4 percent of nursing home care in 1988. Medicaid benefit expenditures were 8.4 percent higher than in 1987.
Medicaid is a federally supported and State-administered program that funds medical care for certain low-income individuals and families. The program was created by Title XIX of the Social Security Act in 1965. Those covered include persons who are eligible to receive some type of cash payment from either the Supplemental Security Income for the Aged, Blind, and Disabled program or the Aid to Families with Dependent Children program (AFDC). Additionally, States may provide Medicaid coverage to the medically needy, that is, people who are not eligible to receive cash assistance, but who have incomes that fall below a certain level after deducting medical expenses.
Title XIX of the Social Security Act requires that State Medicaid programs provide certain basic services: inpatient and outpatient hospital care, physician care, skilled nursing home care, rural health clinic services, laboratory and X-ray services, home health care to persons 21 years of age or over, early and periodic screening, diagnosis, and treatment to persons under 21 years of age, and family planning services. States may elect to provide additional services such as drugs, eyeglasses, private-duty nursing, intermediate care facilities, inpatient psychiatric care for the aged and persons under 21 years of age, physical therapy, and dental care.
Medicaid is financed jointly with Federal and State funds. The Federal share of spending varies from State to State, depending inversely on the State's per capita income; currently, it ranges from 50 to 80 percent of each State's total expenditures. Medicaid is a vendor-payment program, which means payment for covered services is made directly to the provider of the service. Providers who elect to participate in the program must accept Medicaid reimbursement levels (and coinsurance, if any) as payment in full.
Although two-thirds (67.0 percent) of Medicaid recipients in fiscal year 1988 qualified because they were members of an AFDC family, these recipients consumed only one-fourth (24.1 percent) of the benefits. Conversely, the aged, blind, and disabled, who accounted for 29 percent of Medicaid recipients, consumed nearly three-fourths (73.4 percent) of the benefits (Figure 6).
Figure 6. Percent distribution of Medicaid recipients and payments, by basis of eligibility: Fiscal year 1988.
Through State buy-in agreements, Medicaid will purchase Medicare SMI for people who are eligible for both programs, a practice known as “buy-in.” For those “dual-eligibles,” Medicare is the primary payer for Medicare-covered services, and Medicaid pays the deductibles and coinsurance and supplements with additional covered health care services. To avoid double counting, the Medicaid estimates presented here do not include the $716 million paid to Medicare by Medicaid in 1988 for buy-in premiums. Therefore, actual Medicaid program expenditures were $55.8 billion in 1988.
In fiscal year 1988, there were 22.9 million people who received some type of Medicaid benefit (Table 12). The number of Medicaid recipients has increased rapidly in recent years, as a result of program expansions. Changes in eligibility requirements have allowed many low-income pregnant women, children, and Medicare beneficiaries to become eligible.
The 1988 Medicare Catastrophic Coverage Act requires Medicaid to pay the Medicare premiums, deductibles, and coinsurance for certain aged, blind, and disabled beneficiaries—those whose incomes are below certain levels. These provisions of the Act were left in force when the remainder of the Act's provisions were repealed. The new recipients are not eligible for full Medicaid benefits; they receive only medigap-type coverage. More nursing home patients have also become eligible as a result of increased allowable assets and income to the spouse at home.
Department of Defense
The Department of Defense (DoD) assumes responsibility for the health care needs of the Nation's active and retired military forces and their dependents and survivors. An outlay of $9.8 billion (13 percent of DoD outlays for salaries and benefits) was spent for health care in fiscal 1988. Health care costs constitute a rising share of the DoD budget: They accounted for 10 percent of salaries and benefits in fiscal year 1984.
Most of DoD health care expenditures are made in its own health care system. The Department operates 168 hospitals and more than 600 clinics, providing 4.4 million hospital days of care and 47 million outpatient visits in fiscal year 1989.
The Civilian Health and Medical Program of the Uniformed Services (CHAMPUS) was created in 1956 to supplement care provided in DoD facilities. Originally designed for use by dependents of active duty personnel, CHAMPUS was expanded in 1966 to include retired servicemen and their dependents, and survivors of retired and active personnel. By the end of 1989, 5.9 million people were eligible for benefits. The program provides coverage when distance, diagnosis, or availability precludes treatment in a DoD facility. CHAMPUS beneficiaries are liable for nominal coinsurance amounts not charged to users of DoD facilities. CHAMPUS benefits are secondary to Medicare whenever dual eligibility exists. As an indication of its size, CHAMPUS covered 2.1 million inpatient days of hospital care and 8.2 million physician outpatient visits during fiscal year 1989.
Department of Veterans Affairs
The Department of Veterans Affairs (DVA), formerly the Veterans Administration, provides a full range of health care services to the Nation's eligible veterans. The Department must provide medical care to veterans with a service-connected disability and to low-income veterans. Other eligible veterans may be accepted at DVA facilities if space and resources are available. This latter group may face coinsurance and deductible charges under the program.
Health care services provided by the DVA and counted in the NHA include inpatient and outpatient treatment, nursing home care, and medical research. In addition, the Civilian Health and Medical Program of the Veterans Administration (CHAMPVA) was established in 1975 to provide for the medical care of spouses and dependents of disabled and deceased veterans.
To meet its obligations in 1988, the DVA maintained 172 medical centers, 119 nursing homes, and 233 outpatient clinics (including 61 independent clinics), providing care for 1.2 million inpatient admissions and 23 million outpatient visits (Department of Veterans Affairs, 1989). In addition, it contracts with non-DVA providers when DVA facilities are unavailable. In 1988, 27,000 patients were admitted to non-DVA hospitals, and 1.8 million visits were made to private physicians under the auspices of the DVA. DVA expenditures for health in the NHA totaled $10.0 billion in 1988, a 4.0-percent increase over the previous year.
Of its 1988 total spending, the DVA allocated $7.7 billion to hospital care, $1.0 billion to nursing home care, and $0.2 billion to physician services. The DVA also spent $0.1 billion on nondurable and durable medical products. Overall, the Department and its predecessor agency experienced an average annual growth of 8.9 percent in total expenditures from 1960 through 1988.
One of the most pressing problems facing the DVA is care for an aging veteran population. In 1965, the DVA established 1,000 nursing home beds in its medical care facilities. Since then, nursing home care has grown from 1 percent of DVA medical expenditures to 10 percent, averaging 23.8-percent growth per year. In 1988, there were 6.4 million veterans 65 years of age or over, 24 percent of the total number of veterans. By the year 2000, the DVA projects that there will be 8.9 million aged veterans—37 percent of the total veteran population. Currently, the DVA supports 30,000 nursing home beds in DVA-administered nursing homes, in State veterans' homes, and through contracts with private nursing homes. Given the projected number of aged veterans, DVA planners feel that the number of beds supported by the DVA will need to double by the turn of the century.
In addition to developing plans to deal with the demand for nursing home beds, the DVA is studying alternative levels of care for chronically ill, frail, and elderly veterans, including “foster home” programs; rehabilitation services; geriatric dentistry focusing on oral health and disease in the elderly; and a comprehensive, cost-effective quality care program for veterans with dementias such as Alzheimer's disease.
Vietnam-era veterans, who numbered 8.3 million in 1988 and comprised 30 percent of the veteran population, possess a quite-different set of needs than do aged veterans. DVA response to those needs includes providing care for and recognizing the special needs of the homeless, as an estimated 30 percent of the homeless are veterans. A program was established for homeless, chronically ill veterans to provide psychiatric, medical, and community-based residential care.
Two additional medical conditions face the Department. To date, the DVA has treated 5,073 cases of AIDS and has designated AIDS research as a special research initiative, establishing 6 research centers. Further, approximately one-quarter of all Vietnam veterans have post-traumatic stress disorder or other postwar psychological problems, and these problems will remain at significant levels for the next decade.
Other government programs
The Federal Indian Health Service provides personal health care and public health services to more than 1 million Indians and Alaskan natives through a network of hospitals and clinics (Indian Health Service, 1989). In 1988, $865 million was spent by the Indian Health Service in the delivery of health services.
The Alcohol, Drug Abuse, and Mental Health Administration provides Federal support for treatment, prevention, research, and training. In 1988, Federal spending was $832 million on this program.
In 1988, State and local government programs funded $3.9 billion of medical care for the poor who are not eligible for Medicaid and for services not eligible for Federal contributions under Medicaid.
Except for the program for Federal workers, workers' compensation programs are independent State-administered income-maintenance programs that provide benefits for work-related disability and death. Approximately 33 percent of the benefits paid by these programs in 1985 was for medical services for workers, and the remaining 67 percent was for income-loss payments for workers and survivors (Nelson, 1988). Health and medical benefits amounted to $10.5 billion in 1988. (Income loss payments are outside the scope of the NHA.)
Table 14. National health expenditures aggregate amounts and average annual percent growth, by type of expenditure: Selected calendar years 1960-88.
| Type of expenditure | 1960 | 1965 | 1970 | 1975 | 1980 | 1985 | 1986 | 1987 | 1988 |
|---|---|---|---|---|---|---|---|---|---|
| Amount in billions | |||||||||
| National health expenditures | $27.1 | $41.6 | $74.4 | $132.9 | $249.1 | $420.1 | $450.5 | $488.8 | $539.9 |
| Health services and supplies | 25.4 | 38.2 | 69.1 | 124.7 | 237.8 | 404.7 | 434.5 | 471.6 | 520.5 |
| Personal health care | 23.9 | 35.6 | 64.9 | 116.6 | 218.3 | 367.2 | 397.7 | 434.7 | 478.3 |
| Hospital care | 9.3 | 14.0 | 27.9 | 52.4 | 102.4 | 167.9 | 179.3 | 193.7 | 211.8 |
| Physician services | 5.3 | 8.2 | 13.6 | 23.3 | 41.9 | 74.0 | 82.1 | 93.0 | 105.1 |
| Dental services | 2.0 | 2.8 | 4.7 | 8.2 | 14.4 | 23.3 | 24.7 | 27.1 | 29.4 |
| Other professional services | 0.6 | 0.9 | 1.5 | 3.5 | 8.7 | 16.6 | 18.3 | 20.2 | 22.5 |
| Home health care | 0.0 | 0.1 | 0.1 | 0.4 | 1.3 | 3.8 | 4.0 | 4.2 | 4.4 |
| Drugs and other medical nondurables | 4.2 | 5.9 | 8.8 | 13.0 | 20.1 | 32.3 | 35.6 | 38.6 | 41.9 |
| Vision products and other medical durables | 0.8 | 1.2 | 2.0 | 3.1 | 5.0 | 8.4 | 9.5 | 9.8 | 10.8 |
| Nursing home care | 1.0 | 1.7 | 4.9 | 9.9 | 20.0 | 34.1 | 36.7 | 39.7 | 43.1 |
| Other personal health care | 0.7 | 0.8 | 1.4 | 2.7 | 4.6 | 6.8 | 7.6 | 8.4 | 9.3 |
| Program administration and net cost of private health insurance | 1.2 | 1.9 | 2.8 | 5.1 | 12.2 | 25.2 | 23.4 | 22.4 | 26.3 |
| Government public health activities | 0.4 | 0.6 | 1.4 | 3.0 | 7.2 | 12.3 | 13.5 | 14.5 | 15.9 |
| Research and construction | 1.7 | 3.5 | 5.3 | 8.3 | 11.3 | 15.4 | 16.0 | 17.2 | 19.4 |
| Research1 | 0.7 | 1.5 | 2.0 | 3.3 | 5.4 | 7.8 | 8.5 | 9.0 | 9.9 |
| Construction | 1.0 | 1.9 | 3.4 | 5.0 | 5.8 | 7.6 | 7.4 | 8.2 | 9.5 |
| Average annual percent growth from previous year shown | |||||||||
| National health expenditures | — | 8.9 | 12.3 | 12.3 | 13.4 | 11.0 | 7.2 | 8.5 | 10.4 |
| Health services and supplies | — | 8.5 | 12.6 | 12.5 | 13.8 | 11.2 | 7.4 | 8.5 | 10.4 |
| Personal health care | — | 8.3 | 12.8 | 12.4 | 13.4 | 11.0 | 8.3 | 9.3 | 10.0 |
| Hospital care | — | 8.6 | 14.7 | 13.4 | 14.3 | 10.4 | 6.8 | 8.1 | 9.3 |
| Physician services | — | 9.2 | 10.6 | 11.4 | 12.5 | 12.1 | 10.9 | 13.3 | 13.1 |
| Dental services | — | 7.3 | 10.8 | 12.1 | 11.7 | 10.1 | 6.4 | 9.6 | 8.5 |
| Other professional services | — | 7.4 | 11.8 | 18.3 | 19.9 | 13.9 | 10.0 | 10.2 | 11.6 |
| Home health care | — | 9.6 | 19.7 | 23.2 | 27.2 | 23.3 | 3.7 | 4.9 | 5.9 |
| Drugs and other medical nondurables | — | 6.8 | 8.4 | 8.1 | 9.1 | 9.9 | 10.2 | 8.7 | 8.5 |
| Vision products and other medical durables | — | 9.0 | 10.1 | 8.8 | 10.1 | 11.0 | 13.6 | 3.4 | 10.1 |
| Nursing home care | — | 11.6 | 23.4 | 15.4 | 15.0 | 11.3 | 7.5 | 8.2 | 8.5 |
| Other personal health care | — | 3.5 | 10.7 | 14.6 | 11.0 | 8.4 | 11.2 | 10.5 | 10.5 |
| Program administration and net cost of private health insurance | — | 10.5 | 7.5 | 12.8 | 19.3 | 15.5 | −7.2 | −4.2 | 17.7 |
| Government public health activities | — | 10.8 | 17.1 | 17.0 | 18.9 | 11.3 | 9.6 | 7.8 | 9.1 |
| Research and construction | — | 15.2 | 9.0 | 9.2 | 6.4 | 6.4 | 3.7 | 7.8 | 12.6 |
| Research1 | — | 17.1 | 5.1 | 11.2 | 10.4 | 7.4 | 9.5 | 4.9 | 10.1 |
| Construction | — | 13.9 | 11.8 | 8.0 | 3.3 | 5.4 | −2.4 | 11.1 | 15.3 |
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but they are included in the expenditure class in which the product falls.
NOTE: Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 15. National health expenditures, by source of funds and type of expenditure: Selected calendar years 1960-88.
| Year and type of expenditure | Total | Private Consumer | Government | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| All private funds | Consumer | Other | |||||||
|
|
|
||||||||
| Total | Out of pocket | Private insurance | Total | Federal | State and local | ||||
|
| |||||||||
| Amount in billions | |||||||||
| 1960 | |||||||||
| National health expenditures | $27.1 | $20.5 | $19.2 | $13.3 | $5.9 | $1.3 | $6.7 | $2.9 | $3.7 |
| Health services and supplies | 25.4 | 19.8 | 19.2 | 13.3 | 5.9 | 0.5 | 5.7 | 2.3 | 3.4 |
| Personal health care | 23.9 | 18.8 | 18.4 | 13.3 | 5.0 | 0.4 | 5.1 | 2.1 | 3.0 |
| Hospital care | 9.3 | 5.3 | 5.2 | 1.9 | 3.3 | 0.1 | 3.9 | 1.6 | 2.3 |
| Physician services | 5.3 | 4.9 | 4.9 | 3.3 | 1.6 | 0.0 | 0.4 | 0.1 | 0.3 |
| Dental services | 2.0 | 1.9 | 1.9 | 1.9 | 0.0 | — | 0.0 | 0.0 | 0.0 |
| Other professional services | 0.6 | 0.6 | 0.5 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Home health care | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | — | — | — |
| Drugs and other medical nondurables | 4.2 | 4.2 | 4.2 | 4.1 | 0.0 | — | 0.1 | 0.0 | 0.0 |
| Vision products and other medical durables | 0.8 | 0.8 | 0.8 | 0.8 | 0.0 | — | 0.0 | 0.0 | 0.0 |
| Nursing home care | 1.0 | 0.8 | 0.8 | 0.8 | — | 0.1 | 0.1 | 0.1 | 0.1 |
| Other personal health care | 0.7 | 0.2 | — | — | — | 0.2 | 0.5 | 0.3 | 0.2 |
| Program administration and net cost of private health insurance | 1.2 | 1.0 | 0.9 | — | 0.9 | 0.1 | 0.2 | 0.0 | 0.1 |
| Government public health activities | 0.4 | — | — | — | — | — | 0.4 | 0.1 | 0.3 |
| Research and construction | 1.7 | 0.7 | — | — | — | 0.7 | 1.0 | 0.7 | 0.3 |
| Research | 0.7 | 0.1 | — | — | — | 0.1 | 0.6 | 0.5 | 0.0 |
| Construction | 1.0 | 0.6 | — | — | — | 0.6 | 0.4 | 0.2 | 0.3 |
| 1965 | |||||||||
| National health expenditures | 41.6 | 31.3 | 29.0 | 19.0 | 10.0 | 2.3 | 10.3 | 4.8 | 5.5 |
| Health services and supplies | 38.2 | 29.9 | 29.0 | 19.0 | 10.0 | 0.8 | 8.3 | 3.3 | 5.0 |
| Personal health care | 35.6 | 28.4 | 27.7 | 19.0 | 8.7 | 0.7 | 7.3 | 3.0 | 4.3 |
| Hospital care | 14.0 | 8.8 | 8.5 | 2.8 | 5.7 | 0.3 | 5.3 | 2.2 | 3.1 |
| Physician services | 8.2 | 7.6 | 7.6 | 5.0 | 2.7 | 0.0 | 0.6 | 0.1 | 0.4 |
| Dental services | 2.8 | 2.8 | 2.8 | 2.7 | 0.1 | — | 0.0 | 0.0 | 0.0 |
| Other professional services | 0.9 | 0.8 | 0.7 | 0.7 | 0.0 | 0.0 | 0.1 | 0.0 | 0.1 |
| Home health care | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | — | — | — |
| Drugs and other medical nondurables | 5.9 | 5.7 | 5.7 | 5.6 | 0.1 | — | 0.1 | 0.1 | 0.1 |
| Vision products and other medical durables | 1.2 | 1.2 | 1.2 | 1.2 | 0.1 | — | 0.0 | 0.0 | 0.0 |
| Nursing home care | 1.7 | 1.2 | 1.1 | 1.1 | 0.0 | 0.1 | 0.5 | 0.2 | 0.3 |
| Other personal health care | 0.8 | 0.2 | — | — | — | 0.2 | 0.6 | 0.3 | 0.3 |
| Program administration and net cost of private health insurance | 1.9 | 1.5 | 1.3 | — | 1.3 | 0.2 | 0.4 | 0.1 | 0.3 |
| Government public health activities | 0.6 | — | — | — | — | — | 0.6 | 0.2 | 0.4 |
| Research and construction | 3.5 | 1.5 | — | — | — | 1.5 | 2.0 | 1.6 | 0.4 |
| Research | 1.5 | 0.2 | — | — | — | 0.2 | 1.3 | 1.3 | 0.1 |
| Construction | 1.9 | 1.3 | — | — | — | 1.3 | 0.6 | 0.3 | 0.3 |
| 1970 | |||||||||
| National health expenditures | $74.4 | $46.7 | $42.3 | $25.6 | $16.7 | $4.4 | $27.7 | $17.7 | $9.9 |
| Health services and supplies | 69.1 | 44.1 | 42.3 | 25.6 | 16.7 | 1.8 | 24.9 | 15.8 | 9.1 |
| Personal health care | 64.9 | 42.5 | 40.8 | 25.6 | 15.2 | 1.7 | 22.4 | 14.6 | 7.8 |
| Hospital care | 27.9 | 13.0 | 12.1 | 2.5 | 9.6 | 0.9 | 14.9 | 9.8 | 5.1 |
| Physician services | 13.6 | 10.6 | 10.6 | 5.8 | 4.8 | 0.0 | 3.0 | 2.1 | 0.8 |
| Dental services | 4.7 | 4.5 | 4.5 | 4.2 | 0.2 | — | 0.2 | 0.1 | 0.1 |
| Other professional services | 1.5 | 1.1 | 1.0 | 0.9 | 0.1 | 0.1 | 0.4 | 0.2 | 0.1 |
| Home health care | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 |
| Drugs and other medical nondurables | 8.8 | 8.3 | 8.3 | 8.0 | 0.3 | — | 0.5 | 0.2 | 0.2 |
| Vision products and other medical durables | 2.0 | 1.9 | 1.9 | 1.8 | 0.1 | — | 0.1 | 0.1 | 0.0 |
| Nursing home care | 4.9 | 2.6 | 2.4 | 2.3 | 0.0 | 0.2 | 2.3 | 1.4 | 0.9 |
| Other personal health care | 1.4 | 0.3 | — | — | — | 0.3 | 1.1 | 0.6 | 0.5 |
| Program administration and net cost of private health insurance | 2.8 | 1.7 | 1.5 | — | 1.5 | 0.1 | 1.1 | 0.6 | 0.5 |
| Government public health activities | 1.4 | — | — | — | — | — | 1.4 | 0.6 | 0.8 |
| Research and construction | 5.3 | 2.6 | — | — | — | 2.6 | 2.8 | 1.9 | 0.8 |
| Research | 2.0 | 0.2 | — | — | — | 0.2 | 1.7 | 1.6 | 0.2 |
| Construction | 3.4 | 2.3 | — | — | — | 2.3 | 1.0 | 0.4 | 0.7 |
| 1975 | |||||||||
| National health expenditures | 132.9 | 77.8 | 71.5 | 38.5 | 32.9 | 6.3 | 55.1 | 36.4 | 18.7 |
| Health services and supplies | 124.7 | 74.5 | 71.5 | 38.5 | 32.9 | 3.0 | 50.2 | 33.2 | 17.0 |
| Personal health care | 116.6 | 71.3 | 68.4 | 38.5 | 29.9 | 2.9 | 45.3 | 31.0 | 14.4 |
| Hospital care | 52.4 | 23.8 | 22.4 | 4.4 | 18.0 | 1.4 | 28.5 | 19.8 | 8.7 |
| Physician services | 23.3 | 16.8 | 16.8 | 7.6 | 9.1 | 0.0 | 6.5 | 4.7 | 1.8 |
| Dental services | 8.2 | 7.8 | 7.8 | 6.8 | 1.0 | — | 0.5 | 0.3 | 0.2 |
| Other professional services | 3.5 | 2.6 | 2.3 | 1.7 | 0.6 | 0.4 | 0.9 | 0.6 | 0.3 |
| Home health care | 0.4 | 0.1 | 0.1 | 0.0 | 0.0 | 0.1 | 0.3 | 0.2 | 0.0 |
| Drugs and other medical nondurables | 13.0 | 12.0 | 12.0 | 11.2 | 0.8 | — | 1.0 | 0.5 | 0.5 |
| Vision products and other medical durables | 3.1 | 2.8 | 2.8 | 2.7 | 0.2 | — | 0.2 | 0.2 | 0.1 |
| Nursing home care | 9.9 | 4.7 | 4.3 | 4.2 | 0.1 | 0.5 | 5.2 | 3.1 | 2.1 |
| Other personal health care | 2.7 | 0.5 | — | — | — | 0.5 | 2.2 | 1.6 | 0.7 |
| Program administration and net cost of private health insurance | 5.1 | 3.2 | 3.1 | — | 3.1 | 0.2 | 1.8 | 1.2 | 0.7 |
| Government public health activities | 3.0 | — | — | — | — | — | 3.0 | 1.0 | 2.0 |
| Research and construction | 8.3 | 3.3 | — | — | — | 3.3 | 5.0 | 3.2 | 1.7 |
| Research | 3.3 | 0.3 | — | — | — | 0.3 | 3.1 | 2.8 | 0.3 |
| Construction | 5.0 | 3.1 | — | — | — | 3.1 | 1.9 | 0.5 | 1.4 |
| 1980 | |||||||||
| National health expenditures | $249.1 | $143.9 | $131.8 | $58.4 | $73.4 | $12.1 | $105.2 | $72.0 | $33.2 |
| Health services and supplies | 237.8 | 139.7 | 131.8 | 58.4 | 73.4 | 7.8 | 98.1 | 66.8 | 31.4 |
| Personal health care | 218.3 | 131.3 | 123.7 | 58.4 | 65.3 | 7.6 | 87.1 | 63.5 | 23.6 |
| Hospital care | 102.4 | 47.8 | 42.8 | 5.3 | 37.5 | 5.0 | 54.6 | 41.3 | 13.3 |
| Physician services | 41.9 | 29.2 | 29.2 | 11.3 | 18.0 | 0.0 | 12.6 | 9.7 | 3.0 |
| Dental services | 14.4 | 13.7 | 13.7 | 9.4 | 4.4 | — | 0.6 | 0.4 | 0.3 |
| Other professional services | 8.7 | 6.9 | 6.0 | 3.8 | 2.2 | 0.9 | 1.7 | 1.3 | 0.4 |
| Home health care | 1.3 | 0.4 | 0.2 | 0.1 | 0.1 | 0.1 | 1.0 | 0.8 | 0.1 |
| Drugs and other medical nondurables | 20.1 | 18.5 | 18.5 | 16.0 | 2.5 | — | 1.7 | 0.8 | 0.8 |
| Vision products and other medical durables | 5.0 | 4.4 | 4.4 | 3.9 | 0.4 | — | 0.6 | 0.5 | 0.1 |
| Nursing home care | 20.0 | 9.5 | 8.8 | 8.7 | 0.2 | 0.6 | 10.5 | 6.1 | 4.4 |
| Other personal health care | 4.6 | 0.9 | — | — | — | 0.9 | 3.7 | 2.5 | 1.2 |
| Program administration and net cost of private health insurance | 12.2 | 8.4 | 8.1 | — | 8.1 | 0.2 | 3.8 | 2.1 | 1.8 |
| Government public health activities | 7.2 | — | — | — | — | — | 7.2 | 1.2 | 6.0 |
| Research and construction | 11.3 | 4.2 | — | — | — | 4.2 | 7.0 | 5.2 | 1.8 |
| Research | 5.4 | 0.3 | — | — | — | 0.3 | 5.2 | 4.7 | 0.5 |
| Construction | 5.8 | 4.0 | — | — | — | 4.0 | 1.9 | 0.6 | 1.3 |
| 1985 | |||||||||
| National health expenditures | 420.1 | 245.2 | 225.8 | 91.7 | 134.1 | 19.3 | 174.9 | 123.4 | 51.5 |
| Health services and supplies | 404.7 | 239.2 | 225.8 | 91.7 | 134.1 | 13.4 | 165.5 | 116.3 | 49.2 |
| Personal health care | 367.2 | 218.7 | 205.8 | 91.7 | 114.1 | 12.9 | 148.5 | 111.6 | 36.9 |
| Hospital care | 167.9 | 76.5 | 68.3 | 8.8 | 59.5 | 8.2 | 91.4 | 71.5 | 19.9 |
| Physician services | 74.0 | 49.9 | 49.8 | 16.1 | 33.7 | 0.0 | 24.1 | 19.2 | 4.9 |
| Dental services | 23.3 | 22.6 | 22.6 | 13.5 | 9.1 | — | 0.6 | 0.3 | 0.3 |
| Other professional services | 16.6 | 13.5 | 11.3 | 6.1 | 5.2 | 2.2 | 3.1 | 2.4 | 0.8 |
| Home health care | 3.8 | 1.1 | 0.7 | 0.4 | 0.3 | 0.4 | 2.7 | 2.3 | 0.5 |
| Drugs and other medical nondurables | 32.3 | 29.2 | 29.2 | 24.1 | 5.2 | — | 3.0 | 1.5 | 1.6 |
| Vision products and other medical durables | 8.4 | 6.8 | 6.8 | 6.1 | 0.7 | — | 1.6 | 1.4 | 0.2 |
| Nursing home care | 34.1 | 17.6 | 16.9 | 16.6 | 0.3 | 0.7 | 16.5 | 9.7 | 6.8 |
| Other personal health care | 6.8 | 1.4 | — | — | — | 1.4 | 5.4 | 3.5 | 2.0 |
| Program administration and net cost of private health insurance | 25.2 | 20.5 | 20.0 | — | 20.0 | 0.5 | 4.7 | 3.2 | 1.4 |
| Government public health activities | 12.3 | — | — | — | — | — | 12.3 | 1.4 | 10.9 |
| Research and construction | 15.4 | 6.0 | — | — | — | 6.0 | 9.4 | 7.2 | 2.2 |
| Research | 7.8 | 0.5 | — | — | — | 0.5 | 7.3 | 6.4 | 0.9 |
| Construction | 7.6 | 5.5 | — | — | — | 5.5 | 2.1 | 0.8 | 1.3 |
| 1986 | |||||||||
| National health expenditures | $450.5 | $259.8 | $239.7 | $96.8 | $142.9 | $20.0 | $190.7 | $132.8 | $57.9 |
| Health services and supplies | 434.5 | 253.7 | 239.7 | 96.8 | 142.9 | 14.0 | 180.8 | 125.2 | 55.6 |
| Personal health care | 397.7 | 235.6 | 222.1 | 96.8 | 125.3 | 13.5 | 162.1 | 120.5 | 41.6 |
| Hospital care | 179.3 | 80.7 | 72.1 | 8.6 | 63.5 | 8.6 | 98.6 | 75.5 | 23.0 |
| Physician services | 82.1 | 54.7 | 54.7 | 16.3 | 38.3 | 0.0 | 27.4 | 21.9 | 5.4 |
| Dental services | 24.7 | 24.1 | 24.1 | 14.1 | 9.9 | — | 0.7 | 0.3 | 0.3 |
| Other professional services | 18.3 | 14.8 | 12.5 | 6.5 | 6.0 | 2.2 | 3.5 | 2.7 | 0.8 |
| Home health care | 4.0 | 1.1 | 0.7 | 0.4 | 0.3 | 0.4 | 2.9 | 2.4 | 0.5 |
| Drugs and other medical nondurables | 35.6 | 31.9 | 31.9 | 25.9 | 6.0 | — | 3.6 | 1.7 | 1.9 |
| Vision products and other medical durables | 9.5 | 7.7 | 7.7 | 6.9 | 0.8 | — | 1.8 | 1.6 | 0.2 |
| Nursing home care | 36.7 | 19.0 | 18.3 | 18.0 | 0.4 | 0.7 | 17.6 | 10.5 | 7.2 |
| Other personal health care | 7.6 | 1.6 | — | — | — | 1.6 | 6.0 | 3.8 | 2.2 |
| Program administration and net cost of private health insurance | 23.4 | 18.1 | 17.7 | — | 17.7 | 0.5 | 5.2 | 3.3 | 2.0 |
| Government public health activities | 13.5 | — | — | — | — | — | 13.5 | 1.4 | 12.1 |
| Research and construction | 16.0 | 6.0 | — | — | — | 6.0 | 9.9 | 7.6 | 2.3 |
| Research | 8.5 | 0.7 | — | — | — | 0.7 | 7.8 | 6.7 | 1.1 |
| Construction | 7.4 | 5.3 | — | — | — | 5.3 | 2.1 | 0.9 | 1.2 |
| 1987 | |||||||||
| National health expenditures | 488.8 | 280.5 | 258.7 | 102.4 | 156.2 | 21.8 | 208.3 | 144.0 | 64.3 |
| Health services and supplies | 471.6 | 273.8 | 258.7 | 102.4 | 156.2 | 15.2 | 197.8 | 135.9 | 61.9 |
| Personal health care | 434.7 | 256.9 | 242.3 | 102.4 | 139.8 | 14.7 | 177.8 | 130.9 | 46.9 |
| Hospital care | 193.7 | 87.5 | 78.1 | 8.7 | 69.3 | 9.4 | 106.2 | 80.4 | 25.8 |
| Physician services | 93.0 | 61.8 | 61.8 | 17.8 | 43.9 | 0.0 | 31.2 | 25.2 | 6.0 |
| Dental services | 27.1 | 26.4 | 26.4 | 15.4 | 11.0 | — | 0.7 | 0.4 | 0.3 |
| Other professional services | 20.2 | 16.0 | 13.6 | 6.5 | 7.0 | 2.4 | 4.1 | 3.2 | 1.0 |
| Home health care | 4.2 | 1.1 | 0.8 | 0.5 | 0.3 | 0.3 | 3.1 | 2.4 | 0.7 |
| Drugs and other medical nondurables | 38.6 | 34.5 | 34.5 | 27.5 | 6.9 | — | 4.2 | 2.0 | 2.2 |
| Vision products and other medical durables | 9.8 | 7.8 | 7.8 | 6.9 | 0.9 | — | 2.0 | 1.8 | 0.2 |
| Nursing home care | 39.7 | 20.2 | 19.4 | 19.0 | 0.4 | 0.8 | 19.5 | 11.4 | 8.2 |
| Other personal health care | 8.4 | 1.7 | — | — | — | 1.7 | 6.7 | 4.2 | 2.5 |
| Program administration and net cost of private health insurance | 22.4 | 16.9 | 16.4 | — | 16.4 | 0.5 | 5.5 | 3.4 | 2.1 |
| Government public health activities | 14.5 | — | — | — | — | — | 14.5 | 1.6 | 12.9 |
| Research and construction | 17.2 | 6.7 | — | — | — | 6.7 | 10.5 | 8.1 | 2.4 |
| Research | 9.0 | 0.7 | — | — | — | 0.7 | 8.2 | 7.0 | 1.2 |
| Construction | 8.2 | 5.9 | — | — | — | 5.9 | 2.3 | 1.1 | 1.3 |
| 1988 | |||||||||
| National health expenditures | $539.9 | $312.4 | $288.1 | $113.2 | $174.9 | $24.3 | $227.5 | $157.8 | $69.6 |
| Health services and supplies | 520.5 | 304.6 | 288.1 | 113.2 | 174.9 | 16.5 | 215.9 | 149.0 | 66.9 |
| Personal health care | 478.3 | 284.3 | 268.4 | 113.2 | 155.2 | 15.9 | 194.0 | 143.2 | 50.8 |
| Hospital care | 211.8 | 96.6 | 86.3 | 11.3 | 75.0 | 10.3 | 115.2 | 86.7 | 28.5 |
| Physician services | 105.1 | 70.0 | 69.9 | 19.9 | 50.0 | 0.0 | 35.2 | 28.7 | 6.4 |
| Dental services | 29.4 | 28.7 | 28.7 | 16.3 | 12.4 | — | 0.7 | 0.4 | 0.3 |
| Other professional services | 22.5 | 18.0 | 15.4 | 7.1 | 8.3 | 2.6 | 4.5 | 3.4 | 1.0 |
| Home health care | 4.4 | 1.1 | 0.8 | 0.5 | 0.3 | 0.3 | 3.3 | 2.6 | 0.7 |
| Drugs and other medical nondurables | 41.9 | 37.3 | 37.3 | 29.6 | 7.7 | — | 4.6 | 2.2 | 2.4 |
| Vision products and other medical durables | 10.8 | 8.6 | 8.6 | 7.6 | 1.0 | — | 2.3 | 2.0 | 0.2 |
| Nursing home care | 43.1 | 22.1 | 21.3 | 20.8 | 0.5 | 0.8 | 20.9 | 12.5 | 8.4 |
| Other personal health care | 9.3 | 1.9 | — | — | — | 1.9 | 7.4 | 4.7 | 2.7 |
| Program administration and net cost of private health insurance | 26.3 | 20.3 | 19.7 | — | 19.7 | 0.5 | 6.1 | 3.9 | 2.2 |
| Government public health activities | 15.9 | — | — | — | — | — | 15.9 | 1.9 | 14.0 |
| Research and construction | 19.4 | 7.8 | — | — | — | 7.8 | 11.5 | 8.8 | 2.7 |
| Research | 9.9 | 0.7 | — | — | — | 0.7 | 9.1 | 7.9 | 1.2 |
| Construction | 9.5 | 7.1 | — | — | — | 7.1 | 2.4 | 0.9 | 1.5 |
NOTES: 0.0 denotes less than $50 million. Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but are included in the expenditure class in which the product falls. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 16. Personal health care expenditures aggregate and per capita amounts and percent distribution, by source of funds: Selected calendar years 1960-88.
| Year | Total | Out-of-pocket payments | Third-party payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private health insurance | Other private funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and local | ||||||||
| Amount in billions | ||||||||||
| 1960 | $23.9 | $13.3 | $10.5 | $5.0 | $0.4 | $5.1 | $2.1 | $3.0 | — | — |
| 1965 | 35.6 | 19.0 | 16.6 | 8.7 | 0.7 | 7.3 | 3.0 | 4.3 | — | — |
| 1970 | 64.9 | 25.6 | 39.3 | 15.2 | 1.7 | 22.4 | 14.6 | 7.8 | $7.2 | $5.1 |
| 1975 | 116.6 | 38.5 | 78.0 | 29.9 | 2.9 | 45.3 | 31.0 | 14.4 | 15.7 | 12.9 |
| 1980 | 218.3 | 58.4 | 159.9 | 65.3 | 7.6 | 87.1 | 63.5 | 23.6 | 36.4 | 24.8 |
| 1985 | 367.2 | 91.7 | 275.5 | 114.1 | 12.9 | 148.5 | 111.6 | 36.9 | 70.1 | 39.7 |
| 1986 | 397.7 | 96.8 | 300.9 | 125.3 | 13.5 | 162.1 | 120.5 | 41.6 | 75.4 | 42.9 |
| 1987 | 434.7 | 102.4 | 332.3 | 139.8 | 14.7 | 177.8 | 130.9 | 46.9 | 81.7 | 48.2 |
| 1988 | 478.3 | 113.2 | 365.1 | 155.2 | 15.9 | 194.0 | 143.2 | 50.8 | 89.7 | 52.3 |
| Per capita amount | ||||||||||
| 1960 | $126 | $70 | $55 | $26 | $2 | $27 | $11 | $16 | — | — |
| 1965 | 175 | 93 | 81 | 42 | 3 | 36 | 15 | 21 | — | — |
| 1970 | 302 | 119 | 183 | 71 | 8 | 104 | 68 | 36 | (3) | (3) |
| 1975 | 519 | 172 | 347 | 133 | 13 | 202 | 138 | 64 | (3) | (3) |
| 1980 | 928 | 248 | 680 | 277 | 32 | 370 | 270 | 100 | (3) | (3) |
| 1985 | 1,486 | 371 | 1,115 | 462 | 52 | 601 | 452 | 149 | (3) | (3) |
| 1986 | 1,594 | 388 | 1,206 | 502 | 54 | 650 | 483 | 167 | (3) | (3) |
| 1987 | 1,726 | 407 | 1,319 | 555 | 58 | 706 | 520 | 186 | (3) | (3) |
| 1988 | 1,882 | 445 | 1,436 | 610 | 63 | 763 | 564 | 200 | (3) | (3) |
| Percent distribution | ||||||||||
| 1960 | 100.0 | 55.9 | 44.1 | 21.0 | 1.7 | 21.4 | 8.9 | 12.5 | — | — |
| 1965 | 100.0 | 53.4 | 46.6 | 24.3 | 1.9 | 20.4 | 8.3 | 12.0 | — | — |
| 1970 | 100.0 | 39.5 | 60.5 | 23.4 | 2.6 | 34.6 | 22.6 | 12.0 | 11.1 | 7.8 |
| 1975 | 100.0 | 33.1 | 66.9 | 25.6 | 2.5 | 38.9 | 26.6 | 12.3 | 13.4 | 11.1 |
| 1980 | 100.0 | 26.8 | 73.2 | 29.9 | 3.5 | 39.9 | 29.1 | 10.8 | 16.7 | 11.4 |
| 1985 | 100.0 | 25.0 | 75.0 | 31.1 | 3.5 | 40.4 | 30.4 | 10.0 | 19.1 | 10.8 |
| 1986 | 100.0 | 24.3 | 75.7 | 31.5 | 3.4 | 40.8 | 30.3 | 10.5 | 19.0 | 10.8 |
| 1987 | 100.0 | 23.6 | 76.4 | 32.2 | 3.4 | 40.9 | 30.1 | 10.8 | 18.8 | 11.1 |
| 1988 | 100.0 | 23.7 | 76.3 | 32.4 | 3.3 | 40.6 | 29.9 | 10.6 | 18.8 | 10.9 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 social security area population estimates. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 17. Hospital care expenditures aggregate and per capita amounts and percent distribution, by source of funds: Selected calendar years 1960-88.
| Year | Total | Out-of-pocket payments | Third-party payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private health insurance | Other private funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and local | ||||||||
| Amount in billions | ||||||||||
| 1960 | $9.3 | $1.9 | $7.4 | $3.3 | $0.1 | $3.9 | $1.6 | $2.3 | — | — |
| 1965 | 14.0 | 2.8 | 11.3 | 5.7 | 0.3 | 5.3 | 2.2 | 3.1 | — | — |
| 1970 | 27.9 | 2.5 | 25.4 | 9.6 | 0.9 | 14.9 | 9.8 | 5.1 | $5.3 | $2.2 |
| 1975 | 52.4 | 4.4 | 48.0 | 18.0 | 1.4 | 28.5 | 19.8 | 8.7 | 11.5 | 4.6 |
| 1980 | 102.4 | 5.3 | 97.1 | 37.5 | 5.0 | 54.6 | 41.3 | 13.3 | 26.4 | 9.7 |
| 1985 | 167.9 | 8.8 | 159.1 | 59.5 | 8.2 | 91.4 | 71.5 | 19.9 | 48.5 | 15.5 |
| 1986 | 179.3 | 8.6 | 170.7 | 63.5 | 8.6 | 98.6 | 75.5 | 23.0 | 51.0 | 16.5 |
| 1987 | 193.7 | 8.7 | 185.0 | 69.3 | 9.4 | 106.2 | 80.4 | 25.8 | 54.0 | 18.5 |
| 1988 | 211.8 | 11.3 | 200.5 | 75.0 | 10.3 | 115.2 | 86.7 | 28.5 | 58.3 | 20.2 |
| Per capita amount | ||||||||||
| 1960 | $49 | $10 | $39 | $17 | $1 | $21 | $8 | $12 | — | — |
| 1965 | 69 | 13 | 55 | 28 | 1 | 26 | 11 | 15 | — | — |
| 1970 | 130 | 12 | 118 | 45 | 4 | 69 | 46 | 24 | (3) | (3) |
| 1975 | 233 | 20 | 214 | 80 | 6 | 127 | 88 | 39 | (3) | (3) |
| 1980 | 435 | 23 | 413 | 159 | 21 | 232 | 176 | 56 | (3) | (3) |
| 1985 | 680 | 36 | 644 | 241 | 33 | 370 | 289 | 81 | (3) | (3) |
| 1986 | 719 | 35 | 684 | 255 | 35 | 395 | 303 | 92 | (3) | (3) |
| 1987 | 769 | 35 | 735 | 275 | 37 | 422 | 319 | 103 | (3) | (3) |
| 1988 | 833 | 44 | 789 | 295 | 41 | 453 | 341 | 112 | (3) | (3) |
| Percent distribution | ||||||||||
| 1960 | 100.0 | 20.7 | 79.3 | 35.6 | 1.2 | 42.5 | 17.3 | 25.2 | — | — |
| 1965 | 100.0 | 19.6 | 80.4 | 40.9 | 1.9 | 37.6 | 15.4 | 22.2 | — | — |
| 1970 | 100.0 | 9.0 | 91.0 | 34.4 | 3.2 | 53.4 | 35.1 | 18.3 | 18.8 | 8.1 |
| 1975 | 100.0 | 8.4 | 91.6 | 34.4 | 2.8 | 54.5 | 37.9 | 16.6 | 21.9 | 8.8 |
| 1980 | 100.0 | 5.2 | 94.8 | 36.6 | 4.9 | 53.3 | 40.4 | 12.9 | 25.8 | 9.4 |
| 1985 | 100.0 | 5.2 | 94.8 | 35.4 | 4.9 | 54.4 | 42.5 | 11.9 | 28.9 | 9.2 |
| 1986 | 100.0 | 4.8 | 95.2 | 35.4 | 4.8 | 55.0 | 42.1 | 12.8 | 28.5 | 9.2 |
| 1987 | 100.0 | 4.5 | 95.5 | 35.8 | 4.9 | 54.8 | 41.5 | 13.3 | 27.9 | 9.5 |
| 1988 | 100.0 | 5.3 | 94.7 | 35.4 | 4.9 | 54.4 | 40.9 | 13.4 | 27.5 | 9.5 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 social security area population estimates. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 18. Physician care expenditures aggregate and per capita amounts and percent distribution, by source of funds: Selected calendar years 1960-88.
| Year | Total | Out-of-pocket payments | Third-party payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private health insurance | Other private funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and local | ||||||||
| Amount in billions | ||||||||||
| 1960 | $5.3 | $3.3 | $2.0 | $1.6 | $0.0 | $0.4 | $0.1 | $0.3 | — | — |
| 1965 | 8.2 | 5.0 | 3.2 | 2.7 | 0.0 | 0.6 | 0.1 | 0.4 | — | — |
| 1970 | 13.6 | 5.8 | 7.8 | 4.8 | 0.0 | 3.0 | 2.1 | 0.8 | 1.6 | 0.6 |
| 1975 | 23.3 | 7.6 | 15.6 | 9.1 | 0.0 | 6.5 | 4.7 | 1.8 | 3.4 | 1.6 |
| 1980 | 41.9 | 11.3 | 30.6 | 18.0 | 0.0 | 12.6 | 9.7 | 3.0 | 7.9 | 2.1 |
| 1985 | 74.0 | 16.1 | 57.9 | 33.7 | 0.0 | 24.1 | 19.2 | 4.9 | 16.6 | 2.8 |
| 1986 | 82.1 | 16.3 | 65.7 | 38.3 | 0.0 | 27.4 | 21.9 | 5.4 | 18.9 | 3.2 |
| 1987 | 93.0 | 17.8 | 75.1 | 43.9 | 0.0 | 31.2 | 25.2 | 6.0 | 21.8 | 3.5 |
| 1988 | 105.1 | 19.9 | 85.2 | 50.0 | 0.0 | 35.2 | 28.7 | 6.4 | 24.9 | 3.8 |
| Per capita amount | ||||||||||
| 1960 | $28 | $17 | $10 | $8 | $0 | $2 | $0 | $2 | — | — |
| 1965 | 40 | 24 | 16 | 13 | 0 | 3 | 1 | 2 | — | — |
| 1970 | 63 | 27 | 36 | 22 | 0 | 14 | 10 | 4 | (3) | (3) |
| 1975 | 104 | 34 | 70 | 41 | 0 | 29 | 21 | 8 | (3) | (3) |
| 1980 | 178 | 48 | 130 | 76 | 0 | 54 | 41 | 13 | (3) | (3) |
| 1985 | 299 | 65 | 234 | 137 | 0 | 97 | 78 | 20 | (3) | (3) |
| 1986 | 329 | 65 | 263 | 154 | 0 | 110 | 88 | 22 | (3) | (3) |
| 1987 | 369 | 71 | 298 | 174 | 0 | 124 | 100 | 24 | (3) | (3) |
| 1988 | 414 | 78 | 335 | 197 | 0 | 138 | 113 | 25 | (3) | (3) |
| Percent distribution | ||||||||||
| 1960 | 100.0 | 62.7 | 37.3 | 30.2 | 0.1 | 7.1 | 1.4 | 5.7 | — | — |
| 1965 | 100.0 | 60.6 | 39.4 | 32.5 | 0.1 | 6.8 | 1.4 | 5.4 | — | — |
| 1970 | 100.0 | 42.8 | 57.2 | 35.2 | 0.1 | 21.9 | 15.8 | 6.1 | 11.8 | 4.6 |
| 1975 | 100.0 | 32.8 | 67.2 | 39.3 | 0.1 | 27.9 | 20.1 | 7.8 | 14.6 | 7.1 |
| 1980 | 100.0 | 26.9 | 73.1 | 42.9 | 0.1 | 30.2 | 23.1 | 7.1 | 19.0 | 5.1 |
| 1985 | 100.0 | 21.8 | 78.2 | 45.6 | 0.0 | 32.6 | 25.9 | 6.6 | 22.4 | 3.9 |
| 1986 | 100.0 | 19.9 | 80.1 | 46.7 | 0.0 | 33.3 | 26.7 | 6.6 | 23.1 | 3.9 |
| 1987 | 100.0 | 19.2 | 80.8 | 47.3 | 0.0 | 33.5 | 27.1 | 6.4 | 23.5 | 3.8 |
| 1988 | 100.0 | 18.9 | 81.1 | 47.6 | 0.0 | 33.4 | 27.3 | 6.1 | 23.6 | 3.6 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $.50 for per capita amounts. Per capita amounts based on July 1 social security area population estimates. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 19. Nursing home care expenditures aggregate and per capita amounts and percent distribution, by source of funds: Selected calendar years 1960-88.
| Year | Total | Out-of-pocket payments | Third-party payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private health insurance | Other private funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and local | ||||||||
| Amount in billions | ||||||||||
| 1960 | $1.0 | $0.8 | $0.2 | 0.0 | $0.1 | $0.1 | $0.1 | $0.1 | — | — |
| 1965 | 1.7 | 1.1 | 0.6 | 0.0 | 0.1 | 0.5 | 0.2 | 0.3 | — | — |
| 1970 | 4.9 | 2.3 | 2.5 | 0.0 | 0.2 | 2.3 | 1.4 | 0.9 | $0.2 | $1.4 |
| 1975 | 9.9 | 4.2 | 5.8 | 0.1 | 0.5 | 5.2 | 3.1 | 2.1 | 0.3 | 4.7 |
| 1980 | 20.0 | 8.7 | 11.3 | 0.2 | 0.6 | 10.5 | 6.1 | 4.4 | 0.4 | 9.7 |
| 1985 | 34.1 | 16.6 | 17.5 | 0.3 | 0.7 | 16.5 | 9.7 | 6.8 | 0.6 | 15.2 |
| 1986 | 36.7 | 18.0 | 18.7 | 0.4 | 0.7 | 17.6 | 10.5 | 7.2 | 0.6 | 16.2 |
| 1987 | 39.7 | 19.0 | 20.7 | 0.4 | 0.8 | 19.5 | 11.4 | 8.2 | 0.6 | 18.0 |
| 1988 | 43.1 | 20.8 | 22.2 | 0.5 | 0.8 | 20.9 | 12.5 | 8.4 | 0.8 | 19.1 |
| Per capita amount | ||||||||||
| 1960 | $5 | $4 | $1 | $0 | $0 | $1 | $0 | $0 | — | — |
| 1965 | 8 | 5 | 3 | 0 | 0 | 2 | 1 | 1 | — | — |
| 1970 | 23 | 11 | 12 | 0 | 1 | 11 | 6 | 4 | (3) | (3) |
| 1975 | 44 | 19 | 26 | 0 | 2 | 23 | 14 | 10 | (3) | (3) |
| 1980 | 85 | 37 | 48 | 1 | 3 | 45 | 26 | 19 | (3) | (3) |
| 1985 | 138 | 67 | 71 | 1 | 3 | 67 | 39 | 28 | (3) | (3) |
| 1986 | 147 | 72 | 75 | 1 | 3 | 71 | 42 | 29 | (3) | (3) |
| 1987 | 158 | 75 | 82 | 2 | 3 | 78 | 45 | 32 | (3) | (3) |
| 1988 | 169 | 82 | 88 | 2 | 3 | 82 | 49 | 33 | (3) | (3) |
| Percent distribution | ||||||||||
| 1960 | 100.0 | 80.0 | 20.0 | 0.0 | 6.4 | 13.6 | 6.9 | 6.7 | — | — |
| 1965 | 100.0 | 64.5 | 35.5 | 0.1 | 5.8 | 29.5 | 13.0 | 16.5 | — | — |
| 1970 | 100.0 | 48.2 | 51.8 | 0.3 | 4.9 | 46.6 | 28.2 | 18.4 | 5.0 | 28.0 |
| 1975 | 100.0 | 42.1 | 57.9 | 0.7 | 4.8 | 52.3 | 30.8 | 21.6 | 2.9 | 47.5 |
| 1980 | 100.0 | 43.3 | 56.7 | 0.9 | 3.1 | 52.7 | 30.7 | 21.9 | 2.1 | 48.6 |
| 1985 | 100.0 | 48.6 | 51.4 | 1.0 | 1.9 | 48.5 | 28.5 | 20.0 | 1.7 | 44.6 |
| 1986 | 100.0 | 49.0 | 51.0 | 1.0 | 1.9 | 48.1 | 28.5 | 19.5 | 1.6 | 44.1 |
| 1987 | 100.0 | 47.8 | 52.2 | 1.0 | 1.9 | 49.2 | 28.6 | 20.6 | 1.6 | 45.2 |
| 1988 | 100.0 | 48.4 | 51.6 | 1.1 | 1.9 | 48.6 | 29.0 | 19.6 | 1.9 | 44.4 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $.50 for per capita amounts. Per capita amounts based on July 1 social security area population estimates. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 20. Other personal health care expenditures1 aggregate and per capita amounts and percent distribution, by source of funds: Selected calendar years 1960-88.
| Year | Total | Out-of-pocket payments | Third-party payments | Medicare2 | Medicaid3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private health insurance | Other private funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and local | ||||||||
| Amount in billions | ||||||||||
| 1960 | $8.4 | $7.3 | $1.0 | $0.1 | $0.2 | $0.7 | $0.4 | $0.3 | — | — |
| 1965 | 11.7 | 10.2 | 1.5 | 0.3 | 0.3 | 0.9 | 0.5 | 0.4 | — | — |
| 1970 | 18.5 | 14.9 | 3.6 | 0.8 | 0.5 | 2.3 | 1.3 | 1.0 | $0.1 | $0.8 |
| 1975 | 31.0 | 22.3 | 8.6 | 2.6 | 0.9 | 5.1 | 3.4 | 1.7 | 0.5 | 1.9 |
| 1980 | 54.1 | 33.2 | 20.9 | 9.7 | 1.9 | 9.3 | 6.3 | 3.0 | 1.7 | 3.3 |
| 1985 | 91.2 | 50.2 | 41.0 | 20.5 | 4.0 | 16.5 | 11.3 | 5.2 | 4.4 | 6.1 |
| 1986 | 99.7 | 53.9 | 45.8 | 23.1 | 4.2 | 18.5 | 12.6 | 6.0 | 4.8 | 7.0 |
| 1987 | 108.3 | 56.9 | 51.5 | 26.2 | 4.4 | 20.9 | 13.9 | 6.9 | 5.3 | 8.3 |
| 1988 | 118.4 | 61.2 | 57.2 | 29.7 | 4.8 | 22.7 | 15.3 | 7.4 | 5.7 | 9.2 |
| Per capita amount | ||||||||||
| 1960 | $44 | $39 | $5 | $1 | $1 | $4 | $2 | $1 | — | — |
| 1965 | 57 | 50 | 7 | 1 | 1 | 4 | 2 | 2 | — | — |
| 1970 | 86 | 70 | 17 | 4 | 2 | 11 | 6 | 5 | (4) | (4) |
| 1975 | 138 | 99 | 38 | 12 | 4 | 23 | 15 | 8 | (4) | (4) |
| 1980 | 230 | 141 | 89 | 41 | 8 | 40 | 27 | 13 | (4) | (4) |
| 1985 | 369 | 203 | 166 | 83 | 16 | 67 | 46 | 21 | (4) | (4) |
| 1986 | 400 | 216 | 184 | 93 | 17 | 74 | 50 | 24 | (4) | (4) |
| 1987 | 430 | 226 | 204 | 104 | 18 | 83 | 55 | 28 | (4) | (4) |
| 1988 | 466 | 241 | 225 | 117 | 19 | 89 | 60 | 29 | (4) | (4) |
| Percent distribution | ||||||||||
| 1960 | 100.0 | 87.8 | 12.2 | 1.4 | 2.7 | 8.0 | 4.7 | 3.3 | — | — |
| 1965 | 100.0 | 87.4 | 12.6 | 2.2 | 2.6 | 7.8 | 4.0 | 3.8 | — | — |
| 1970 | 100.0 | 80.6 | 19.4 | 4.3 | 2.7 | 12.4 | 7.2 | 5.2 | 0.7 | 4.4 |
| 1975 | 100.0 | 72.2 | 27.8 | 8.5 | 3.0 | 16.4 | 10.9 | 5.5 | 1.7 | 6.2 |
| 1980 | 100.0 | 61.4 | 38.6 | 17.9 | 3.6 | 17.2 | 11.7 | 5.6 | 3.1 | 6.1 |
| 1985 | 100.0 | 55.1 | 44.9 | 22.5 | 4.4 | 18.1 | 12.4 | 5.7 | 4.8 | 6.7 |
| 1986 | 100.0 | 54.1 | 45.9 | 23.2 | 4.2 | 18.6 | 12.6 | 6.0 | 4.8 | 7.0 |
| 1987 | 100.0 | 52.5 | 47.5 | 24.2 | 4.1 | 19.3 | 12.8 | 6.4 | 4.9 | 7.7 |
| 1988 | 100.0 | 51.7 | 48.3 | 25.1 | 4.0 | 19.2 | 13.0 | 6.3 | 4.9 | 7.8 |
Personal health care expenditures other than those for hospital care, physician services, and nursing home care.
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $50 for per capita mounts. Per capita amounts based on July 1 social security area population estimates. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Table 21. Personal health care expenditures, by type of expenditure and selected sources of payment: Selected calendar years 1980-88.
| Source of payment | Total | Hospital care | Physician services | Dental services | Other professional services | Home health care | Drugs and other medical nondurables | Vision products and other medical durables | Nursing home care | Other personal care |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Amount in billions | ||||||||||
| 1980 | ||||||||||
| Personal health care expenditures | $218.3 | $102.4 | $41.9 | $14.4 | $8.7 | $1.3 | $20.1 | $5.0 | $20.0 | $4.6 |
| Out-of-pocket payments | 58.4 | 5.3 | 11.3 | 9.4 | 3.8 | 0.1 | 16.0 | 3.9 | 8.7 | — |
| Third-party payments | 159.9 | 97.1 | 30.6 | 5.0 | 4.9 | 1.2 | 4.2 | 1.0 | 11.3 | 4.6 |
| Private health insurance | 65.3 | 37.5 | 18.0 | 4.4 | 2.2 | 0.1 | 2.5 | 0.4 | 0.2 | — |
| Other private | 7.6 | 5.0 | 0.0 | — | 0.9 | 0.1 | — | — | 0.6 | 0.9 |
| Government | 87.1 | 54.6 | 12.6 | 0.6 | 1.7 | 1.0 | 1.7 | 0.6 | 10.5 | 3.7 |
| Federal | 63.5 | 41.3 | 9.7 | 0.4 | 1.3 | 0.8 | 0.8 | 0.5 | 6.1 | 2.5 |
| Medicare | 36.4 | 26.4 | 7.9 | — | 0.6 | 0.7 | — | 0.4 | 0.4 | — |
| Medicaid | 13.7 | 5.3 | 1.2 | 0.3 | 0.3 | 0.2 | 0.8 | — | 5.4 | 0.3 |
| Other | 13.4 | 9.7 | 0.5 | 0.1 | 0.4 | — | 0.0 | 0.1 | 0.4 | 2.2 |
| State and local | 23.6 | 13.3 | 3.0 | 0.3 | 0.4 | 0.1 | 0.8 | 0.1 | 4.4 | 1.2 |
| Medicaid | 11.1 | 4.4 | 1.0 | 0.2 | 0.2 | 0.1 | 0.6 | — | 4.4 | 0.3 |
| Other | 12.5 | 8.9 | 2.0 | 0.1 | 0.2 | 0.0 | 0.2 | 0.1 | 0.0 | 0.9 |
| Total Medicaid | 24.8 | 9.7 | 2.1 | 0.5 | 0.5 | 0.3 | 1.4 | — | 9.7 | 0.6 |
| 1985 | ||||||||||
| Personal health care expenditures | 367.2 | 167.9 | 74.0 | 23.3 | 16.6 | 3.8 | 32.3 | 8.4 | 34.1 | 6.8 |
| Out-of-pocket payments | 91.7 | 8.8 | 16.1 | 13.5 | 6.1 | 0.4 | 24.1 | 6.1 | 16.6 | — |
| Third-party payments | 275.5 | 159.1 | 57.9 | 9.7 | 10.5 | 3.4 | 8.2 | 2.3 | 17.5 | 6.8 |
| Private health insurance | 114.1 | 59.5 | 33.7 | 9.1 | 5.2 | 0.3 | 5.2 | 0.7 | 0.3 | — |
| Other private | 12.9 | 8.2 | 0.0 | — | 2.2 | 0.4 | — | — | 0.7 | 1.4 |
| Government | 148.5 | 91.4 | 24.1 | 0.6 | 3.1 | 2.7 | 3.0 | 1.6 | 16.5 | 5.4 |
| Federal | 111.6 | 71.5 | 19.2 | 0.3 | 2.4 | 2.3 | 1.5 | 1.4 | 9.7 | 3.5 |
| Medicare | 70.1 | 48.5 | 16.6 | — | 1.4 | 1.8 | — | 1.3 | 0.6 | — |
| Medicaid | 21.9 | 8.4 | 1.6 | 0.3 | 0.5 | 0.5 | 1.4 | — | 8.4 | 0.7 |
| Other | 19.7 | 14.5 | 1.0 | 0.0 | 0.5 | — | 0.1 | 0.1 | 0.7 | 2.7 |
| State and local | 36.9 | 19.9 | 4.9 | 0.3 | 0.8 | 0.5 | 1.6 | 0.2 | 6.8 | 2.0 |
| Medicaid | 17.8 | 7.1 | 1.2 | 0.2 | 0.4 | 0.5 | 1.1 | — | 6.8 | 0.6 |
| Other | 19.1 | 12.9 | 3.7 | 0.1 | 0.3 | 0.0 | 0.5 | 0.2 | 0.0 | 1.4 |
| Total Medicaid | 39.7 | 15.5 | 2.8 | 0.5 | 0.9 | 0.9 | 2.5 | — | 15.2 | 1.3 |
| 1986 | ||||||||||
| Personal health care expenditures | 397.7 | 179.3 | 82.1 | 24.7 | 18.3 | 4.0 | 35.6 | 9.5 | 36.7 | 7.6 |
| Out-of-pocket payments | 96.8 | 8.6 | 16.3 | 14.1 | 6.5 | 0.4 | 25.9 | 6.9 | 18.0 | — |
| Third-party payments | 300.9 | 170.7 | 65.7 | 10.6 | 11.8 | 3.5 | 9.6 | 2.6 | 18.7 | 7.6 |
| Private health insurance | 125.3 | 63.5 | 38.3 | 9.9 | 6.0 | 0.3 | 6.0 | 0.8 | 0.4 | — |
| Other private | 13.5 | 8.6 | 0.0 | — | 2.2 | 0.4 | — | — | 0.7 | 1.6 |
| Government | 162.1 | 98.6 | 27.4 | 0.7 | 3.5 | 2.9 | 3.6 | 1.8 | 17.6 | 6.0 |
| Federal | 120.5 | 75.5 | 21.9 | 0.3 | 2.7 | 2.4 | 1.7 | 1.6 | 10.5 | 3.8 |
| Medicare | 75.4 | 51.0 | 18.9 | — | 1.6 | 1.8 | — | 1.5 | 0.6 | — |
| Medicaid | 24.0 | 9.1 | 1.8 | 0.3 | 0.6 | 0.6 | 1.7 | — | 9.0 | 0.8 |
| Other | 21.1 | 15.4 | 1.2 | 0.0 | 0.5 | — | 0.1 | 0.1 | 0.8 | 3.0 |
| State and local | 41.6 | 23.0 | 5.4 | 0.3 | 0.8 | 0.5 | 1.9 | 0.2 | 7.2 | 2.2 |
| Medicaid | 18.9 | 7.3 | 1.3 | 0.2 | 0.5 | 0.5 | 1.2 | — | 7.1 | 0.6 |
| Other | 22.7 | 15.7 | 4.1 | 0.1 | 0.4 | 0.0 | 0.6 | 0.2 | 0.0 | 1.6 |
| Total Medicaid | 42.9 | 16.5 | 3.2 | 0.5 | 1.0 | 1.1 | 2.9 | — | 16.2 | 1.4 |
| 1987 | ||||||||||
| Personal health care expenditures | $434.7 | $193.7 | $93.0 | $27.1 | $20.2 | $4.2 | $38.6 | $9.8 | $39.7 | $8.4 |
| Out-of-pocket payments | 102.4 | 8.7 | 17.8 | 15.4 | 6.5 | 0.5 | 27.5 | 6.9 | 19.0 | — |
| Third-party payments | 332.3 | 185.0 | 75.1 | 11.7 | 13.6 | 3.7 | 11.1 | 2.9 | 20.7 | 8.4 |
| Private health insurance | 139.8 | 69.3 | 43.9 | 11.0 | 7.0 | 0.3 | 6.9 | 0.9 | 0.4 | — |
| Other private | 14.7 | 9.4 | 0.0 | — | 2.4 | 0.3 | — | — | 0.8 | 1.7 |
| Government | 177.8 | 106.2 | 31.2 | 0.7 | 4.1 | 3.1 | 4.2 | 2.0 | 19.5 | 6.7 |
| Federal | 130.9 | 80.4 | 25.2 | 0.4 | 3.2 | 2.4 | 2.0 | 1.8 | 11.4 | 4.2 |
| Medicare | 81.7 | 54.0 | 21.8 | — | 1.9 | 1.7 | — | 1.7 | 0.6 | — |
| Medicaid | 26.4 | 10.0 | 2.0 | 0.3 | 0.7 | 0.7 | 1.9 | — | 9.8 | 1.0 |
| Other | 22.7 | 16.4 | 1.4 | 0.1 | 0.6 | — | 0.1 | 0.1 | 0.9 | 3.2 |
| State and local | 46.9 | 25.8 | 6.0 | 0.3 | 1.0 | 0.7 | 2.2 | 0.2 | 8.2 | 2.5 |
| Medicaid | 21.8 | 8.4 | 1.5 | 0.3 | 0.6 | 0.7 | 1.4 | — | 8.1 | 0.8 |
| Other | 25.1 | 17.4 | 4.4 | 0.1 | 0.4 | 0.0 | 0.8 | 0.2 | 0.1 | 1.7 |
| Total Medicaid | 48.2 | 18.5 | 3.5 | 0.6 | 1.3 | 1.4 | 3.3 | — | 18.0 | 1.7 |
| 1988 | ||||||||||
| Personal health care expenditures | 478.3 | 211.8 | 105.1 | 29.4 | 22.5 | 4.4 | 41.9 | 10.8 | 43.1 | 9.3 |
| Out-of-pocket payments | 113.2 | 11.3 | 19.9 | 16.3 | 7.1 | 0.5 | 29.6 | 7.6 | 20.8 | — |
| Third-party payments | 365.1 | 200.5 | 85.2 | 13.1 | 15.4 | 3.9 | 12.3 | 3.2 | 22.2 | 9.3 |
| Private health insurance | 155.2 | 75.0 | 50.0 | 12.4 | 8.3 | 0.3 | 7.7 | 1.0 | 0.5 | — |
| Other private | 15.9 | 10.3 | 0.0 | — | 2.6 | 0.3 | — | — | 0.8 | 1.9 |
| Government | 194.0 | 115.2 | 35.2 | 0.7 | 4.5 | 3.3 | 4.6 | 2.3 | 20.9 | 7.4 |
| Federal | 143.2 | 86.7 | 28.7 | 0.4 | 3.4 | 2.6 | 2.2 | 2.0 | 12.5 | 4.7 |
| Medicare | 89.7 | 58.3 | 24.9 | — | 2.1 | 1.8 | — | 1.9 | 0.8 | — |
| Medicaid | 29.4 | 11.2 | 2.2 | 0.3 | 0.8 | 0.8 | 2.1 | — | 10.8 | 1.2 |
| Other | 24.1 | 17.1 | 1.7 | 0.1 | 0.6 | — | 0.1 | 0.1 | 1.0 | 3.5 |
| State and local | 50.8 | 28.5 | 6.4 | 0.3 | 1.0 | 0.7 | 2.4 | 0.2 | 8.4 | 2.7 |
| Medicaid | 22.9 | 8.9 | 1.6 | 0.3 | 0.6 | 0.7 | 1.5 | — | 8.4 | 0.9 |
| Other | 27.9 | 19.5 | 4.9 | 0.1 | 0.5 | 0.0 | 0.8 | 0.2 | 0.1 | 1.8 |
| Total Medicaid | 52.3 | 20.2 | 3.8 | 0.6 | 1.4 | 1.5 | 3.6 | — | 19.1 | 2.1 |
NOTES: 0.0 denotes less than $50 million. Medicaid expenditures include Part B premium payments to Medicare by States under “buy-in” agreements to cover premiums for eligible Medicaid recipients. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Cost Estimates.
Footnotes
These two companion articles were prepared by the following members of the Office of National Cost Estimates, Office of the Actuary: Ross H. Amett, III, Louis A. Blank, Aaron P. Brown, Cathy A. Cowan, Carolyn S. Donham, Mark S. Freeland, Helen C. Lazenby, Suzanne W. Letsch, Katharine R. Levit, Brenda T. Maple, Patricia A. McDonnell, Sally T. Sonnefeld, Madie W. Stewart, and Daniel R. Waldo.
Reprint requests: Carol Pearson, Office of National Cost Estimates, L-1, EQ05, 6325 Security Boulevard, Baltimore, Maryland 21207.
The number of participating-provider billing arrangements reflects physicians who are participating in at least one practice setting. A physician participating in his or her private practice but not in his or her group practice is counted as participating. If the physician chose to participate in both settings, the number of arrangements would be two.
References
- American Dental Association. Unpublished data developed by RRC, Inc Bryan, Tex. 1989. [Google Scholar]
- American Hospital Association. Data from the Annual Survey of Hospitals. 1963-88. [Google Scholar]
- American Hospital Association. Data from the National Hospital Panel Survey. 1963-89. [Google Scholar]
- American Medical Association. Socioeconomic Characteristics of Medical Practice 1983. Chicago: 1983. Physicians' financial arrangements with hospitals. [Google Scholar]
- American Medical Association. Data from the Socio-economic Monitoring System. 1984-88. [Google Scholar]
- American Medical Association. Physician Characteristics and Distribution in the US. 1988. Chicago: To be published. [Google Scholar]
- Brown LJ. Contrasting the economic outlook for dentistry and medicine. The Journal of Medical Practice Management. 1989 Summer;5(1):8–17. [PubMed] [Google Scholar]
- Burda D. And what is your bid for this loyal admitter? Please, don't hold back. Modern Healthcare. 1990 Jan.20(2):22–30. [PubMed] [Google Scholar]
- Bureau of Government Financial Operations. Monthly Treasury Statement of Receipts and Outlays of the United States Government. Washington: U.S. Government Printing Office; 1984-88. Department of the Treasury. [Google Scholar]
- Bureau of Health Professions, Health Resources and Services Administration. Sixth Report to the President and Congress on the Status of Health Personnel in the United States. Washington: U.S. Government Printing Office; Jun, 1988. DHHS Pub. No. HRS-P-OD-88-1. Public Health Service. [Google Scholar]
- Bureau of Labor Statistics. Supplement to Employment and Earnings. Department of Labor; Washington, D.C.: 1972-89. [Google Scholar]
- Department of Health and Human Services. Report to Congress: Expenses Incurred by Medicare Beneficiaries for Prescription Drugs. Washington, D.C.: May, 1989. Unpublished report. [Google Scholar]
- Department of Veterans Affairs. Annual Report 1988. Washington: U.S. Government Printing Office; Jul, 1989. Pub. No. GPO-1989-244-526/00524. [Google Scholar]
- Freeland M, Schendler C. Health Care Financing Review. No. 3. Vol. 5. Washington: U.S. Government Printing Office; Spring. 1984. Health spending in the 1980's: Integration of clinical practice patterns with management. HCFA Pub. No. 03169. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Fuchs V. The health sector's share of the gross national product. Science. 1990 Feb.247:534–538. doi: 10.1126/science.2300814. [DOI] [PubMed] [Google Scholar]
- Health Care Financing Administration, Office of Research and Demonstrations. Data from the 40-percent Home Health Agency Skeleton File. 1989. [Google Scholar]
- Health Care Financing Administration. Medicare secondary payer. Jan. 1990. Medicare Decision Support System Data Evaluation Report. Draft report. [Google Scholar]
- Health Insurance Association of America. Data from the HIAA Long-term Care Insurance Survey. Mar. 1990. [Google Scholar]
- Health Resources and Services Administration, Department of Health and Human Services. Data from the BHCDANET Information System. 1983-88. [Google Scholar]
- Hoyer, R.: National Association for Home Care. Personal communication. Washington, D.C. 1990.
- Indian Health Service. Justification of Appropriation: Estimates for Committee on Appropriations. Public Health Service; Rockville, Md.: 1989. [Google Scholar]
- Institute for Social Research. Employee health services: A study of managerial attitudes and evaluations. Ann Arbor, Mich.: University of Michigan; Sept. 1957. [Google Scholar]
- Jain R. Employer-sponsored dental insurance eases the pain. Monthly Labor Review. 1988 Oct.111(10):18–23. [PubMed] [Google Scholar]
- Jones R, Bly J, Richardson J. A study of a work site health promotion program and absenteeism. Journal of Occupational Medicine. 1990 Feb.32(2):95–99. [PubMed] [Google Scholar]
- Kasper J. National Health Care Expenditures Study Data Preview 9. Public Health Service; Hyattsville, Md.: Apr. 1982. Prescribed medicines: Use, expenditures, and sources of payment. DHHS Pub. No. (PHS) 82-3320. [Google Scholar]
- Kleinfeld M, Messite J, Wolf M, Ratajack R. Occupational health and safety services in New York State. Journal of Occupational Medicine. 1972 Sept.14(9):693–699. [PubMed] [Google Scholar]
- Klem M, McKiever M. Small Plant Health and Medical Programs. Federal Security Agency, Public Health Service; Washington, D.C.: May, 1952. [Google Scholar]
- Levit K, Freeland M, Waldo D. Health Care Financing Review. No. 3. Vol. 10. Washington: U.S. Government Printing Office; Spring. 1989. Health spending and ability to pay: Business, individuals, and government. HCFA Pub. No. 03280. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Lynch W, Golaszewski T, Clearie A, et al. Impact of a facility-based corporate fitness program on the number of absences from work due to illness. Journal of Occupational Medicine. 1990 Jan.32(1):9–12. doi: 10.1097/00043764-199001000-00006. [DOI] [PubMed] [Google Scholar]
- Moglen, G., Wolfe, R., and Jordan, D.: Internal Revenue Service. Personal communication. Washington, D.C. 1989.
- Moyer ME. A revised look at the number of uninsured Americans. Health Affairs. 1989 Summer;8(2):102–110. doi: 10.1377/hlthaff.8.2.102. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics, Department of Health and Human Services. Data from the National Nursing Home Survey. 1972, 1977 and 1985. [Google Scholar]
- National Center for Health Statistics, Department of Health and Human Services. Data from the National Health Interview Survey. 1966-87. [Google Scholar]
- Nelson J. Social Security Bulletin. No. 1. Vol. 51. Washington: U.S. Government Printing Office; Jan. 1988. Workers' compensation: Coverage, benefits, and costs, 1985. Pub No. 13-11700. Office of Research and Statistics, Social Security Administration. [PubMed] [Google Scholar]
- Phelps C. Health Care Costs: The Consequences of Increased Cost Sharing. Santa Monica, Calif.: The RAND Corporation; Nov. 1982. [Google Scholar]
- Physician Payment Review Commission. Annual Report to Congress, 1989. Washington, D.C.: Apr. 1989. [Google Scholar]
- Rivlin A, Wiener J. Caring for the Disabled Elderly. Washington, D.C.: The Brookings Institution; 1988. [PubMed] [Google Scholar]
- Ruther M, Helbing C. Health Care Financing Review. No. 1. Vol. 10. Washington: U.S. Government Printing Office; Fall. 1988. Use and cost of home health agency services under Medicare. HCFA Pub. No. 03274. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Tsai S, Baun W, Bernacki E. Relationship of employee turnover to exercise adherence in a corporate fitness program. Journal of Occupational Medicine. 1987 Jul;29(7):572–575. [PubMed] [Google Scholar]
- Waldo DR, Levit KR, Lazenby H. Health Care Financing Review. No. 1. Vol. 8. Washington: U.S. Government Printing Office; Oct. 1986. National health expenditures, 1985. HCFA Pub. No. 03224. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Wilson C, Weissert W. Private long-term care insurance: After coverage restrictions is there anything left? Inquiry. 1989 Winter;26:493–507. [PubMed] [Google Scholar]