Abstract
Background:
Anatomical variations of the recurrent laryngeal nerve (RLN) such as extralaryngeal terminal bifurcation is an important risk for its motor function.
Aims:
The objective is to study surgical anatomy of bilateral bifurcation of the RLNs in order to decrease risk of vocal cord palsy in patients with bifurcated nerves.
Materials and Methods:
Surgical anatomy including terminal bifurcation was established in 292 RLNs of 146 patients. We included patients with bilateral bifurcation of RLN in this study. Based on two anatomical landmarks (nerve-artery crossing and laryngeal entry), the cervical course of RLN was classified in four segments: Pre-arterial, arterial, post-arterial and pre-laryngeal. According to these segments, bifurcation point locations along the cervical course of RLNs were compared between both sides in bilateral cases.
Results:
RLNs were exposed throughout their entire courses. Seventy (48%) patients had bifurcated RLNs. We identified terminal bifurcation in 90 (31%) of 292 RLNs along the cervical course. Bilateral bifurcation was observed in 20 (28.6%) patients with bifurcated RLNs. Bifurcation points were located on arterial and post-arterial segments in 37.5% and 32.5% of cases, respectively. Pre-arterial and pre-laryngeal segments contained bifurcations in 15% of cases. Comparison of both sides indicated that bifurcation points were similar in 5 (25%) and different in 15 (75%) patients with bilateral bifurcation. Permanent nerve injury did not occur in this series.
Conclusion:
Bilateral bifurcation of both RLNs was observed in approximately 30% of patients with extralaryngeal bifurcation which is a common anatomical variation. Bifurcation occurred in different segments along cervical course of RLN. Bifurcation point locations differed between both sides in the majority of bilateral cases. Increasing surgeons’ awareness of this variation may lead to safely exposing bifurcated nerves and prevent the injury to extralaryngeal terminal branches of RLN.
Keywords: Anatomic variation, Nerve injury, Thyroid, Vocal cord palsy
Introduction
The safety of thyroid operations may be affected by anatomical variations of the recurrent laryngeal nerve (RLN), which increases the risk of nerve injury. Complete knowledge of every variation is an important to minimise complication rates during thyroidectomy.[1] Bilateral variations of both right and left RLNs in the same patient increase the risk of vocal cord palsy and may have catastrophic outcomes. Extralaryngeal terminal bifurcation of RLN is a common variation, which is macroscopically identified by surgical dissection along the cervical course of the nerve.[2] Terminal branches may have similar proportions, and must be fully exposed with care to preserve their integrity and avoid vocal cord dysfunction.
Anatomical features and bifurcation point locations are quite variable along the cervical course of RLN. These features were previously discussed in total thyroidectomy cases.[2] Besides variations of extralaryngeal terminal bifurcations, variable locations of division points create many combinations that can complicate dissection of the nerve, and thus, increase the importance of this variation. Bilateral occurrence of terminal bifurcation makes dissection even more challenging, and increases the risk of nerve injury by two-fold. Therefore, complete knowledge of anatomical locations of bifurcation points aids in identifying and preserving both branches, decreases complication rates and increases the safety of surgery.
In this study, we attempted to identify and expose bilateral extralaryngeal terminal bifurcations of both RLNs from a series of total thyroidectomy cases, in order to establish anatomical features of bifurcated nerves based on bifurcation point locations along the cervical course of the nerve to elucidate the surgical importance of this variation.
Materials and Methods
This prospective study evaluated surgical anatomy of RLN in 146 patients with surgical thyroid diseases, who were treated with total thyroidectomy between May 2009 and October 2013. Informed consent was obtained from every patient prior to the surgery. To provide a standard dissection technique, the procedure was performed by the same surgeon. A possible presence of extralaryngeal terminal bifurcation of RLN was macroscopically determined, and the bifurcation point location along the cervical course of the nerve was identified according to adjacent structures. Lateral sides (unilateral or bilateral) of the terminal division were also established during the procedure.
Technique for dissection of RLN
After freeing and medially mobilising lateral lobes in the both sides of thyroid gland by the classical surgical approach, the inferior thyroid arteries (ITA) were identified, and isolated, a loop of silk suture was placed around the arteries for traction. With the usual lateral approach, RLNs were identified below the artery, and fully isolated at both sides. The nerve was carefully exposed in the tracheoesophageal groove up to its laryngeal entry point. Dissection was performed using a binocular loupe (× 2.5 magnification). If macroscopically and clearly delineated terminal bifurcation of the nerve was identified along its cervical course, the anatomical features of these branches in bilateral cases were macroscopically studied to compare the anatomical differences between both sides.
Extralaryngeal terminal bifurcation of RLN
Division of RLN occurs along its cervical course prior to laryngeal entry. The branches of similar dimensions were observed during the surgery, and entered into the larynx separately at different points.
Classification of terminal bifurcation of the nerve
The classification was based on the bifurcation point location according to relatively constant landmarks, that is the neuro-vascular (RLN and ITA) crossing point and the laryngeal entry point of the nerve. The location of bifurcation point are classified in four segments of RLN along its cervical course, as previously reported[2]:
Arterial segment: Bifurcation occurs at or closely adjacent to neurovascular crossing of RLN and ITA;
Post-arterial segment: Bifurcation occurs after (distal to) neurovascular crossing;
Pre-laryngeal segment: Bifurcation occurs in the most distal (15 mm to laryngeal entry) segment of the RLN; and
Pre-arterial segment: Bifurcation occurs before (proximal to) neurovascular crossing.
Patients with extralaryngeal terminal bifurcation of both right and left RLNs were included in the study. The incidence of unilateral and bilateral bifurcation was determined. Bifurcation point locations along the cervical course of RLNs in bilateral cases were classified according to the four segments. Anatomical features of bifurcated nerves were compared to establish similarities or differences between two sides.
Results
Extralaryngeal terminal bifurcations of RLNs were observed in 70 (48%) of 146 patients undergone with total thyroidectomy and 90 (31%) of 292 RLNs. We observed bilateral bifurcation in 20 (13.7%) of 146 patients and 20 (28.6%) of 70 patients with bifurcated nerves [Table 1].
Table 1.
Total thyroidectomy cases with RLN bifurcation
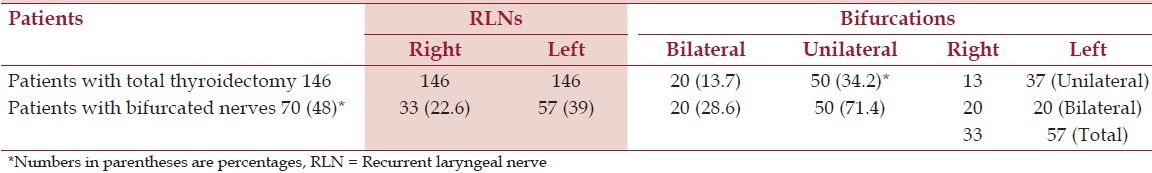
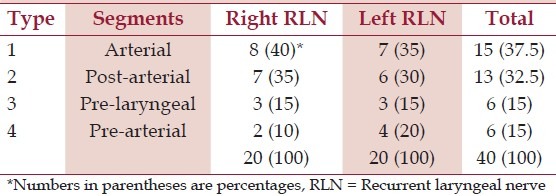
Bifurcation point locations along the cervical course of RLN were another important result of the study. Forty RLNs in 20 patients with bilateral bifurcation were classified according to the anatomical location of division points. 37.5% terminal bifurcations of RLNs were located in the arterial segment. Pre-laryngeal and pre-arterial locations of RLN bifurcation were seldom encountered [Table 2].
Table 2.
The location of bifurcation points on 40 RLNs in 20 patients with bilateral bifurcation
According to anatomical segments of the RLN, 5 (25%) patients with bilateral bifurcation of RLN presented similar locations of bifurcation point on both sides. Locations of bifurcation were different in 15 (75%) patients with bilateral bifurcation of RLN. The locations of bilateral bifurcations were found either in the same anatomical segments [Figure 1] or in different anatomical segments [Figure 2]. Permanent nerve injury and vocal cord palsy were not observed in our present study.
Figure 1.
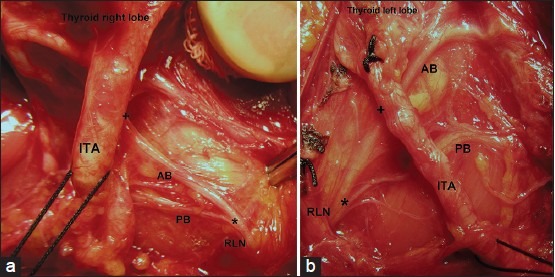
Extralaryngeal terminal bifurcation of both recurrent laryngeal nerves (RLN). Right (a) and left (b) sides of the same patient. Bifurcation points (*) are located in the same (pre-arterial) segments along cervical course of the nerve. ITA: Inferior thyroid artery. AB: Anterior branch. PB: Posterior branch. (*) Bifurcation point. (+) Neuro-vascular (RLN and ITA) crossing
Figure 2.
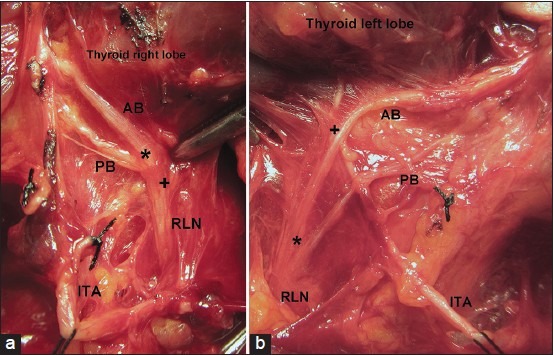
Extralaryngeal terminal bifurcation of both recurrent laryngeal nerves (RLN). Right (a) and left (b) sides of the same patient. Bifurcation points (*) are located in different (right arterial and left pre-arterial) segments along cervical course of the nerve. ITA: Inferior thyroid artery. AB: Anterior branch. PB: Posterior branch. (*) Bifurcation point. (+) Neuro-vascular (RLN and ITA) crossing
Discussion
In this study, rates of extralaryngeal terminal bifurcation (31%) in the exposed RLNs and those of bifurcation (48%) in patients undergoing total thyroidectomy indicate the common occurrence of this anatomical variation. Indeed, surgeons frequently encounter bifurcated nerves during thyroidectomies. Moreover, results from the previous studies support our findings. Surgical studies of thyroidectomies have reported that bifurcation of RLN is common. However, some studies showed quite different results: Kandil et al.,[3,4] reported bifurcation in 34% and 43% of dissected RLNs, Beneragama et al.,[5] in 36%, Paradeep et al.,[6] in 30.7%, Cernea et al.,[7] in 64.5% and Casella et al.,[1] in 18.5% of RLNs. The awareness of possible variations of terminal bifurcation of RLN is of importance, from a surgical point of view, because a well exposing bifurcation and larger branches of the nerve separately prevents the possibility of nerve injury during thyroid surgery. Inadvertent division of a branch may lead to significant vocal cord palsy, despite the surgeon believing that the nerve may be preserved.[4,8] RLN is particularly prone to be injured in cases of extralaryngeal bifurcation located near ITA or the suspensory ligament of Berry, which may develop in approximately one-third of patients.[9] Based on these findings together with the results from our study, it is suggested that bilateral bifurcation occurrence in the same patient may further increase the risk of nerve injury. Our study aimed to increase surgeons’ awareness of possible variations of bilateral bifurcation of RLN based on anatomical features of both left and right sides.
Extralaryngeal terminal bifurcation of RLN may occur unilaterally at one side or bilaterally at both sides. Unilateral bifurcation of RLN was observed in 71.4% of our 70 patients with bifurcated nerves. Bilateral variation was identified in 13.7% of our patients undergoing thyroidectomy cases in 28.6% of patients with bifurcated nerves. Our results showed that unilateral bifurcation was more frequent than bilateral bifurcation. Casella et al.,[1] reported the rate of bilateral bifurcation at 3.7%, Serpell et al.,[8] at 8.9% and Beneragama et al.,[5] at 18% of the patients who underwent total thyroidectomy, these rates are comparable with the rate found in our present study. Kandil et al.,[3,4] reported 27% and 33.3% of bilateral bifurcation in patients undergone with total thyroidectomy, which was also in agreement with the prevalence of bilateral bifurcation that we observed in 28.6% of patients with bifurcated nerves.
Bilaterally branched RLNs or bilateral anatomical variations threaten nerve integrity even under experienced hands. Identification of the anatomical location of the bifurcation point along the cervical course of the nerve is crucial to securely and properly expose all branches of the nerve, and to protect nerve integrity without inadvertent injury to neural structures. In our study, we determined various locations of division points of the exposed RLN. Nerve bifurcation occurred in arterial and post-arterial segments in 70% of our patients with bilateral variations. Besides these two common findings, we also determined another two division point locations. Bifurcation of the nerve seldom occurred proximal to ITA (pre-arterial). The division point was rarely observed in close proximity to the laryngeal entry of the nerve (pre-laryngeal). Bilateral bifurcation point locations were similar in 25% of our patients. There was discordance between both sides in the majority of our bilateral cases. This anatomical discordance between both sides can make the preservation of the motor function considerably difficult. Anatomical courses of RLNs were different when comparing the right with left nerves in one patient. Therefore, anatomical discordance between both sides of bifurcated nerves was an expected result. Extralaryngeal bifurcation of RLN is a variation that carries great importance for the preservation of nerve integrity and function. We believe that familiarity with bifurcation of RLN and bifurcation point locations along the cervical course of the nerve are considerably helpful for surgeon to avoid nerve injury.
During thyroidectomy, surgeons attempting to locate RLN must consider that approximately half of the patients have a bifurcated nerve. When identifying a bifurcated nerve in one side, surgeons must consider that there is approximately a 30% possibility for the presence of a bifurcated nerve in the contralateral side. Because of a relatively high rate of bilateral bifurcation of RLN, surgeons must be extremely cautious of exposing the nerve bilaterally to preserve the motor function of its extralaryngeal branches. The variability of bifurcation point locations along the cervical course of the nerve requires complete knowledge regarding the surgical anatomy of extralaryngeal bifurcation of RLN, therefore, extensive experience on RLN identification and exposure is necessary.
In case of unilateral or bilateral bifurcation, the location of motor fibres in nerve branches has an extreme importance for the preservation of the motor function. Many authors have reported that motor fibres are located exclusively in the anterior branch.[1,3,4,8,10] Incorrect identification of a relatively larger posterior branch as the main trunk of the nerve and inadvertent division of motor fibres (anterior branch) may lead to laryngeal muscle palsy, although surgeons believe that the nerve may be preserved. This anatomical variation cannot be predicted preoperatively and might be associated with higher rate of nerve injury.[11] Anatomical variations such as extralaryngeal bifurcation of the nerve are good examples of high-risk situations. Bilateral bifurcation may further increase the risk of nerve injury. Variability in the surgical anatomy of nerve bifurcation is a significant threat to the safety of thyroid surgery.
Conclusion
Bilateral terminal bifurcation of RLN is a frequent occurrence in patients who have bifurcated RLN prior to its laryngeal entry. Bifurcation points are located at various segments along the cervical course of the nerve. Location points may differ in left and right sides in the same patient in the majority of bilateral cases. Great anatomical variability in the bifurcated nerve may increase the risk of the injury to the motor branch. Therefore, a visual identification of all terminal branches of RLN may be extremely helpful for the preservation of the motor function of bifurcated nerves. Safe exposure of terminal branches minimises injury rates of RLN.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Casella C, Pata G, Nascimbeni R, Mittempergher F, Salerni B. Does extralaryngeal branching have an impact on the rate of postoperative transient or permanent recurrent laryngeal nerve palsy? World J Surg. 2009;33:261–5. doi: 10.1007/s00268-008-9832-1. [DOI] [PubMed] [Google Scholar]
- 2.Gurleyik E. Extralaryngeal terminal division of the inferior laryngeal nerve: Anatomical classification by a surgical point of view. J Thyroid Res. 2013;2013:731250. doi: 10.1155/2013/731250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kandil E, Abdel Khalek M, Aslam R, Friedlander P, Bellows CF, Slakey D. Recurrent laryngeal nerve: Significance of the anterior extralaryngeal branch. Surgery. 2011;149:820–4. doi: 10.1016/j.surg.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Kandil E, Abdelghani S, Friedlander P, Alrasheedi S, Tufano RP, Bellows CF, et al. Motor and sensory branching of the recurrent laryngeal nerve in thyroid surgery. Surgery. 2011;150:1222–7. doi: 10.1016/j.surg.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Beneragama T, Serpell JW. Extralaryngeal bifurcation of the recurrent laryngeal nerve: A common variation. ANZ J Surg. 2006;76:928–31. doi: 10.1111/j.1445-2197.2006.03899.x. [DOI] [PubMed] [Google Scholar]
- 6.Pradeep PV, Jayashree B, Harshita SS. A closer look at laryngeal nerves during thyroid surgery: A descriptive study of 584 nerves. Anat Res Int. 2012;2012:490390. doi: 10.1155/2012/490390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cernea CR, Hojaij FC, De Carlucci D, Jr, Gotoda R, Plopper C, Vanderlei F, et al. Recurrent laryngeal nerve: A plexus rather than a nerve? Arch Otolaryngol Head Neck Surg. 2009;135:1098–102. doi: 10.1001/archoto.2009.151. [DOI] [PubMed] [Google Scholar]
- 8.Serpell JW, Yeung MJ, Grodski S. The motor fibers of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg. 2009;249:648–52. doi: 10.1097/SLA.0b013e31819ed9a4. [DOI] [PubMed] [Google Scholar]
- 9.Barczynski M, Konturek A, Stopa M, Hubalewska-Dydejczyk A, Richter P, Nowak W. Clinical value of intraoperative neuromonitoring of the recurrent laryngeal nerves in improving outcomes of surgery for well differentiated thyroid cancer. Pol Przegl Chir. 2011;83:196–203. doi: 10.2478/v10035-011-0030-8. [DOI] [PubMed] [Google Scholar]
- 10.Barczynski M, Nowak W, Sancho JJ, Sitges-Serra A. The motor fibers of the recurrent laryngeal nerves are located in the anterior extralaryngeal branches. Ann Surg. 2010;251:773–4. doi: 10.1097/SLA.0b013e3181d57a59. [DOI] [PubMed] [Google Scholar]
- 11.Chiang FY, Lu IC, Chen HC, Chen HY, Tsai CJ, Hsiao PJ, et al. Anatomical variations of recurrent laryngeal nerve during thyroid surgery: How to identify and handle the variations with intraoperative neuromonitoring. Kaohsiung J Med Sci. 2010;26:575–83. doi: 10.1016/S1607-551X(10)70089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


