Abstract
Background:
Triage at emergency department is performed to identify those patients who are relatively more serious and require immediate attention and treatment. Despite current methods of triage, trauma continues to be a leading cause of morbidity and mortality.
Aims:
This study was to evaluate the predictive value of shock index (SI) and modified shock index (MSI) for hospital mortality among adult trauma patients.
Materials and Methods:
In this prospective longitudinal study, all adult patients who sustained trauma enrolled as per as inclusion/exclusion criteria. After the collection of data, SI and MSI were calculated accordingly. All parameters were again recorded hourly and calculations were done at six-hour intervals. Further, to achieve a value that can be analyzed, we determined threshold value for vital signs, which set the threshold values as heart rate at 120 beats per minute, systolic blood pressure at less than 90, and SI at cut-off 0.5-0.9 and MSI at less than 0.7 to more than 1.3.
Results:
We analyzed 9860 adult trauma patients. Multivariate regression analysis demonstrated that heart rate more than 120 beats per minute, systolic blood pressure less than 90 mmHg, and diastolic blood pressure (DBP) less than 60 mmHg correlate with hospital stay and mortality rate. MSI <0.7 and >1.3 had higher odds of mortality as compared to other predictors.
Conclusions:
MSI is an important marker for predicting the mortality rate and is significantly better than heart rate, systolic blood pressure, DBP and SI alone. Therefore, modified SI should be used in the triage of serious patients, including trauma patients in the emergency room.
Keywords: Modified shock index, Shock index, Trauma, Trauma patients
Introduction
Triage at emergency department is performed to identify patients who are relatively more serious and require immediate attention and treatment. Despite current methods of triage, trauma continues to be a leading cause of morbidity and mortality. At most medical institutions, this triage is being done by senior nurses or resident doctors. This triage is usually based on the age of patients, presenting history, patients’ vital signs, level of consciousness, and obvious severity of injury.[1] We worked to study an easy, less technical, and reproducible marker to easily predict the outcome of trauma patients in the emergency room. This will result into an objective triage at the emergency room.
Presently, various clinical parameters including heart rate (HR), pulse rate (PR), blood pressure (BP), shock index (SI), and modified shock index (MSI) are analyzed to predict the severity of serious patients at an emergency room in various retrospective studies.[1,2] We worked on these parameters to assess their correlation with the outcome of the trauma patients in the present prospective cohort study. SI is calculated by dividing HR by systolic blood pressure (SBP).[1] SI can be used to predict the severity of hypovolemic shock. Previous studies[2,3,4] have found that patients with SI more than 0.9 had a greater mortality rate. Liu et al.[5] observed that these emergency patients are complex. They reported that in addition to SBP, diastolic blood pressure (DBP) is also vital to predict the severity of these patients. They also observed that HR more than 120 beats per minute, SBP less than 90 mmHg and DBP less than 60 mmHg correlated with mortality rates of emergency patients. They recommended incorporation of DBP in the assessment of these patients. In contrast to the traditional beliefs, they found a non-significant correlation of SI of 0.5-0.9 with mortalities of these emergency patients.[5] In another study,[6] SI has been shown to assist in identification of shock states in poly trauma patients. They also found that SI correlates with hospital stay, duration of stay in ICU, duration of ventilatory support, and use of blood. Despite the evidences that SI is a good tool, doubts have been raised regarding whether SI stood good for all age groups, especially for elderly patients. The present prospective study was designed to analyze the relationship of SI and MSI with the outcome of adult trauma patients at an institutional level II trauma center.
Materials and Methods
This is a prospective longitudinal study of all trauma patients presenting at an institutional level II trauma center since January 2013 to Dec 2013. An approval from the institutional ethics committee was obtained to carry out the study. This trauma center is a tertiary referral center serving both urban and rural patients of all socioeconomic status. All adult patients sustaining trauma and presenting to the emergency room were evaluated for inclusion. All patients who were referred from another hospital after the first aid, died within the first six hours of arrival, patients less than 18 years and those with incomplete data were excluded. Following data of included patients were collected at the time of admission: Age of patients, gender, heart rate, systolic blood pressure, diastolic blood pressure, level of consciousness. SI and MSI were accordingly calculated using the following formulas:
SI = HR/SBP
MSI = HR/MAP
MAP = [(DBP × 2) + SBP]/3
(Where; HR = Heart rate; SBP = Systolic Blood pressure; DBP = Diastolic blood pressure; MAP = Mean arterial pressure)
All parameters were again recorded at hourly manner and calculations of MSI and SI were done at six hours. To achieve a value that can be analyzed, we determined the threshold value for vital signs based on cut off to observe in a study,[5] which set the threshold values as HR at 120 beats per minute, SBP at less than 90 mmHg and SI at cut off 0.5-0.9 and MSI at less than 0.7 to more than 1.3. For each parameter, any value surpassing the cut-off limits at any hourly monitoring was recorded for evaluation. The end point of the present study was hospital stay, ICU stay, and in-hospital mortality.
Statistical analysis
Multivariate logistic regression analysis was made using SAS software. The confidence level of the study was kept at 95% and a P value less than 0.05 indicated a statistically significant association.
Results
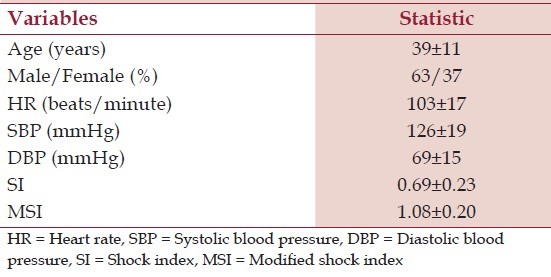
Out of total 16673 trauma patients, 13338 were adult patients. Out of these, 1333 (10%) patients were referred cases from other hospital after the primary resuscitation there. Total 249 (1.8%) patients died within six hour of hospital arrival. As per protocol, these referred and expired cases were excluded from the study. The records of 1896 (14.2%) were incomplete; therefore, these patients were also excluded. We analyzed total 9860 patients in the present study. Most common modes of injury in our study were road traffic accident (59.3%) followed by firearm injury in 14.9% of patients. Amongst these 373 (3.8%) patients were shifted to ICU and 800 (8.1%) died within seven days of admission. Table 1 describes the patients' characteristics in the derivation and validation.
Table 1.
Patients characteristics in the derivation and validation sets (n = 9860)
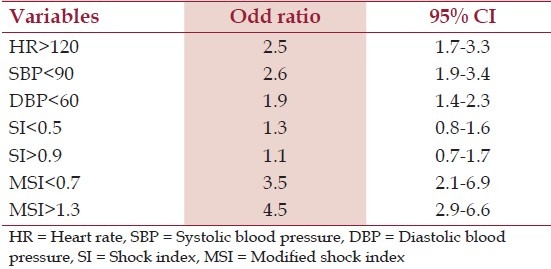
Multivariate regression analysis demonstrated that HR more than 120 beats per minute, SBP less than 90 mmHg and DBP less than 60 mmHg correlate with mortality rate. When age and sex were also included in regression analysis to account for these effects on results, we found no significant association between age of patients and outcome (P = 0.058) and sex of patient and outcome (P = 0.68). [Table 2] shows various parameters and their correlation with mortality prediction.
Table 2.
Prediction of mortality based on multivariate logistic regression
Discussion
Most trauma centers triage the trauma patients presenting to their emergency room into life threatening, possible life threatening and no urgency. However, it is practically difficult to quantify the severity of these life-threatening conditions. In a previous study,[5] the vital signs such as SBP less than 90 mmHg, DBP less than 60 mmHg, and HR more than 120 beats per minute were found to be the important predictors of outcome of these emergency patients. The observations and results of the present study confirm the above observations.
In the present study, we observed that among traditionally used predictors SBP <90 mmHg had the maximum odds of mortality (OR = 2.6); however, both cut-offs of MSI, viz. <0.7 and >1.3, had higher odds of mortality (1.2 times and 1.55 times higher than for SBP <90 mmHg), thus showing the relative superiority of MSI in the prediction of hospital mortality.
SI is known as hemodynamic stability indicator. This index is used to assess the amount of blood loss and the degree of hypovolemic shock. It is considered as a better marker for assessing the severity of shock than HR and BP alone. Thus, in clinical practice, SI has been used to assess the severity of emergency patients. However, while calculating SI, DBP is totally neglected. Most studies[1,7,8,9,10,11] used SBP to predict the outcome of the emergency patients. However, in a retrospective study, DBP was observed as an indicator of the severity of the patients.[5] The mean blood pressure can best represent tissue perfusion status. MSI indicates the stroke volume and systemic vascular resistance.[5] High MSI shows a value of stroke volume and low systemic vascular resistance, a sign of hypodynamic circulation. However, low MSI indicates a hyperdynamic state. Therefore, both high and low MSI indicates the serious state of the emergency patients. MSI was considered as a better marker for mortality rate prediction.[5] One of the limitations of the present study was our inability to control the large data loss owing to lack of coordination between different hospital departments. Despite this limitation, in the present prospective study, we observed that MSI of less than 0.7 and more than 1.3 is associated with significantly higher mortality rate. MSI takes into account valuable information related with cardiovascular and hemodynamic stability by incorporating HR, SBP, and DBP, thus making it a comprehensive tool for assessment. Moreover, it is easy to calculate. Although MAP is a function of SBP and DBP, most of the monitors used in trauma centre settings record it as a separate entity and hence, the calculation remains an easy task to perform.
In conclusion, the present prospective study results show that MSI, as a potential marker for predicting the mortality rate and is significantly better than HR, SBP, DBP, and SI alone. Thus, MSI emerges as a better and improved predictor for prediction of hospital mortality in adult trauma patients in the emergency room.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Mutschler M, Nienaber U, Munzberg M, Wölfl C, Schoechl H, Paffrath T, et al. TraumaRegister DGU®. The shock index revisited – a fast guide to transfusion requirement? A retrospective analysis on patients derived from the Trauma Register DGU. Crit Care. 2013;17:R172. doi: 10.1186/cc12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67:1426–30. doi: 10.1097/TA.0b013e3181bbf728. [DOI] [PubMed] [Google Scholar]
- 3.Rady MY, Smithline HA, Blake H, Nowak R, Rivers E. Comparison of shock index and conventional vital signs to identify acute, critical illness in emergency department. Ann Emerg Med. 1994;24:685–90. doi: 10.1016/s0196-0644(94)70279-9. [DOI] [PubMed] [Google Scholar]
- 4.Talmor D, Jones AE, Rubinson L, Howell MD, Shapiro NI. Simple triage scoring system predicting death and the need for critical care resources for use during epidemics. Crit Care Med. 2007;35:1251–6. doi: 10.1097/01.CCM.0000262385.95721.CC. [DOI] [PubMed] [Google Scholar]
- 5.Liu YC, Liu JH, Fang ZA, Guang-liang S, Jun X, Zhi-wei Qi, et al. Modified shock index and mortality rate of emergency patients. World J Emerg Med. 2012;3:114–7. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimme K, Pape H, Probst C, Seelis M, Sott A, Harwood P, et al. Calculation of different triage scores based on the German trauma registry. Eur J Trauma. 2005;31:480–7. [Google Scholar]
- 7.McNab A, Burns B, Bhullar I, Chesire D, Kerwin A. An analysis of shock index as a correlate for outcomes in trauma by age group. Surgery. 2013;154:384–7. doi: 10.1016/j.surg.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Lalezarzadeh F, Wisniewski P, Huynh K, Loza M, Gnanadev D. Evaluation of prehospital and emergency department systolic blood pressure as a predictor of in-hospital mortality. Am Surg. 2009;75:1009–14. doi: 10.1177/000313480907501032. [DOI] [PubMed] [Google Scholar]
- 9.Holcomb JB, Salinas J, McManus JM, Miller CC, Cooke WH, Convertino VA. Manual vital signs reliably predict need for life saving interventions in trauma patients. J Trauma. 2005;59:821–8. doi: 10.1097/01.ta.0000188125.44129.7c. [DOI] [PubMed] [Google Scholar]
- 10.Eastridge BJ, Salinas J, McManus JG, Blackburn L, Bugler EM, Cooke WH, et al. Hypotension begins at 110 mm Hg: Redefining “hypotension” with data. J Trauma. 2007;63:291–7. doi: 10.1097/TA.0b013e31809ed924. [DOI] [PubMed] [Google Scholar]
- 11.Hasler RM, Nuesch E, Juni P, Bouamra O, Exadaktylos AK, Lecky F. Systolic blood pressure below 110 mmHg is associated with increased mortality in penetrating major trauma patients: Multicenter cohort study. Resuscitation. 2012;83:476–81. doi: 10.1016/j.resuscitation.2011.10.018. [DOI] [PubMed] [Google Scholar]


