Abstract
Context:
Regional pericarditis is elusive and difficult to diagnosis. Healthcare providers should be familiar with post-cardiac ablation complications as this procedure is now widespread and frequently performed. The management of regional pericarditis differs greatly from that of acute myocardial infarction.
Case report:
A 52 year-old male underwent atrial fibrillation ablation and developed severe mid-sternal chest pain the following day with electrocardiographic findings suggestive of acute myocardial infarction, and underwent coronary angiography, a left ventriculogram, and 2D transthoracic echocardiogram, all of which were unremarkable without evidence of obstructive coronary disease, wall motion abnormalities, or pericardial effusions. Ultimately, the patient was diagnosed with regional pericarditis. After diagnosis, the patient's presenting symptoms resolved with treatment including nonsteroidal anti-inflammatory agents and colchicine.
Conclusion:
This is the first reported case study of regional pericarditis status post cardiac ablation. Electrocardiographic findings were classic for an acute myocardial infarction; however, coronary angiography and left ventriculogram demonstrated no acute coronary occlusion or ventricular wall motion abnormalities. Healthcare professionals must remember that the electrocardiographic findings in pericarditis are not always classic and that pericarditis can occur status post cardiac ablation.
Keywords: Acute myocardial infarction, Regional pericarditis, Cardiac ablation
Introduction
Regional pericarditis remains an elusive and a difficult to diagnosis condition and is likely under-diagnosed. Most of the studies regarding regional pericarditis are in the setting of status post acute myocardial infarction (AMI).[1,2] Regional pericarditis presents secondary to localized pericardial inflammation resulting in localized ST-segment elevation that can mimic AMI.[3,4,5] Pericarditis is typically diagnosed with the presence of at least two of the following:
Chest pain;
Pericardial effusion;
Friction rub; and
However, friction rub and pericardial effusion are often not present and diagnostic criteria including these two findings would result in under-diagnosis.[2,7] The electrocardiographic changes of acute pericarditis occur in four stages. Stage 1 lasts several days to weeks and is characterized by widespread concave ST-segment elevations less than 5 mm, with reciprocal depression in leads aVR and V1. Except for leads aVR and V1, the PR-segment is usually depressed, reflecting abnormal atrial repolarization secondary to inflammation. Stage 2 lasts several days to weeks as well and results in the normalization of the ST-segment and PR-segment towards an isolelectric status. Stage 3 typically begins in the third week and may last for several weeks at which time the T-waves may become inverted. Lastly, stage 4 results in slow resolution of T-wave changes.[4,8] In contrast, there is currently no ECG or medical criteria for the diagnosis of regional pericarditis but rather it is a diagnosis of exclusion.
Case Presentation
A 52-year-old male with a past medical history significant for paroxysmal atrial fibrillation, dyslipidemia, and hypertension presented to our facility for an elective atrial fibrillation ablation after his atrial fibrillation became increasingly symptomatic and refractory to medical therapy. Electrocardiogram at time of elective ablation revealed a normal sinus rhythm with heart rate of 79 beats per minute and a normal early repolarization pattern with no other findings [Figure 1]. After a transesophageal echocardiogram (TEE) revealed no identifiable thrombus, the patient underwent the procedure. The patient underwent cryoablation of the pulmonary veins and the posterior wall of the left atrium. The left isthmus was ablated without successful bidirectional block despite aggressive ablation of the endocardial and epicardial region. The right isthmus was then ablated with successful bidirectional block. The patient tolerated the procedure well, with the maintenance of the activated clotting time (ACT) greater than 300 with heparin that was reversed with protamine sulfate after the procedure with removal of the right femoral vein sheaths. The patient was discharged later that day with sotalol 80 mg orally twice daily, clopidogrel 75 mg orally daily, and aspirin 325 mg orally daily.
Figure 1.
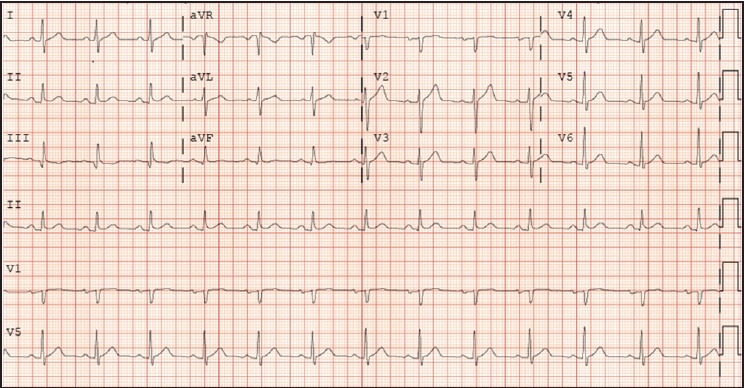
ECG revealing normal sinus rhythm with heart rate of 79 beats per minute and a normal early repolarization pattern prior to undergoing atrial fibrillation catheter ablation
The following day, the patient returned to the emergency department with nine out of ten chest pain that was mid-sternal in location. Electrocardiogram at time of presentation revealed normal sinus rhythm with heart rate 78 beats per minute with anterolateral ST-segment elevations in leads I and aVL and V2 -V4, reciprocal inferior ST-segment depressions in leads III and aVF and subtle PR-segment depressions [Figure 2]. Serum troponin I was 17.2 ng/ml, with a creatinine concentration of 0.97 mg/dl and hemoglobin level of 15 g/dl. Because of the evidence of ST-segment myocardial infarction (STEMI), the patient underwent emergent coronary angiography. Coronary angiography revealed no significant coronary artery disease (<50% luminal stenosis), with a left ventriculogram revealing an estimated left ventricular ejection fraction (LVEF) of 60% and no mitral valve regurgitation or regional wall motion abnormalities.
Figure 2.
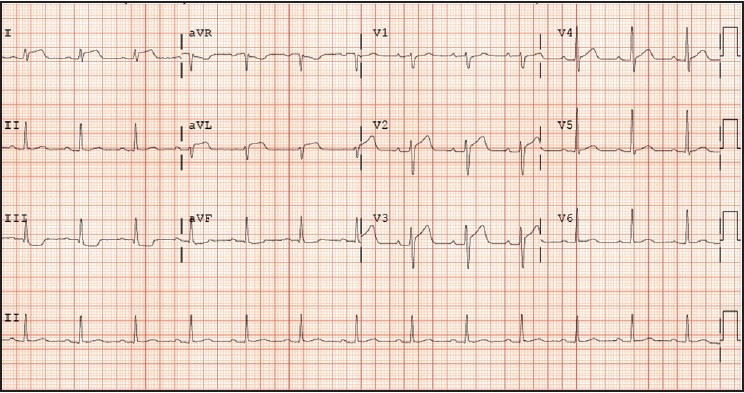
ECG status-post atrial fibrillation catheter ablation revealed normal sinus rhythm with anterolateral ST-segment elevations in leads I and aVL and V2-V4, reciprocal inferior ST-segment depressions in leads III and aVF and subtle PR-segment depressions
A 2D transthoracic echocardiogram (TTE) was performed the day following the left heart catheterization to evaluate for pericardial effusion, revealing a LVEF of 55-60%, normal left ventricular diastolic filling, and a normal pericardium with no evidence of pericardial effusion.
It was thought that patient was suffering from regional post-procedural pericarditis and treated with colchicine 0.6 mg orally and aspirin 325 mg orally with resolution of chest pain. The patient was then discharged the following day with colchicine 0.6 mg orally daily for 30 days, hydrocodone/acetaminophen 5 mg/325 mg orally every 8 hours as needed for pain, aspirin 325 mg orally daily, clopidogrel 75 mg orally daily, sotalol 80 mg orally twice daily, and pantoprazole 40 mg orally daily with resolution of chest pain.
Discussion
Our case report identifies the difficulty of further distinguishing regional pericarditis and STEMI. In this particular case, the ECG was considerably compelling for an acute anterior myocardial infarction despite pre-procedural ischemic evaluation that was negative prior to cardiac ablation. In the emergency department, a differential diagnosis of complications post-atrial fibrillation catheter ablation responsible for this ECG were considered, including coronary embolization from a left atrial thrombus, left circumflex artery damage from ablation, stress-induced cardiomyopathy, and pericardial effusion. Regional pericarditis became our diagnosis after exclusion of the above-mentioned causes. There is no known documented case report discussing regional pericarditis status post cardiac ablation.
Although, complications post atrial fibrillation catheter ablation have steadily decreased,[9] physicians should know and understand the possible complications and include regional pericarditis as a differential diagnosis.
In contrast to the findings of Rechenmacher et al.,[5] our case revealed an even more difficult diagnosis in that the ECG findings revealed reciprocal ST-segment depressions in inferior leads III and aVF that is atypical to previous ECG findings in cases diagnosed with regional pericarditis. Although there are currently no ECG criteria for the diagnosis of regional pericarditis, the absence of inverted T-waves may be suggestive of regional pericarditis in the right clinical setting, as once T-waves invert due to an AMI, they should remain inverted for weeks to months.[2]
As regional pericarditis becomes more recognized, healthcare providers will be able to make a rapid and accurate diagnosis that is imperative to provide appropriate management with patient satisfaction and avoid potential harmful therapies.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dorfman TA, Aqel R. Regional pericarditis: A review of the pericardial manifestations of acute myocardial infarction. Clin Cardiol. 2009;32:115–20. doi: 10.1002/clc.20444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliva PB, Hammill SC, Edwards WD. The electrocardiographic diagnosis of regional pericarditis in acute inferior myocardial infarction. Eur Heart J. 1993;14:1683–91. doi: 10.1093/eurheartj/14.12.1683. [DOI] [PubMed] [Google Scholar]
- 3.Oliva PB, Hammill SC, Edwards WD. Electrocardiographic diagnosis of postinfarction regional pericarditis. Ancillary observations regarding the effect of reperfusion on the rapidity and amplitude of T wave inversion after acute myocardial infarction. Circulation. 1993;88:896–904. doi: 10.1161/01.cir.88.3.896. [DOI] [PubMed] [Google Scholar]
- 4.Youssef G, Khouzam S, Sprung J, Bourke DL. Regional pericarditis mimicking myocardial infarction. Anesthesiology. 2001;95:261–4. doi: 10.1097/00000542-200107000-00039. [DOI] [PubMed] [Google Scholar]
- 5.Rechenmacher S, Jurewitz D, Southard J, Amsterdam E. Barking up the wrong tree: Regional pericarditis mimicking STEMI. Am J Med. 2013;126:679–81. doi: 10.1016/j.amjmed.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717–27. doi: 10.1016/S0140-6736(04)15648-1. [DOI] [PubMed] [Google Scholar]
- 7.Surawicz B, Lasseter KC. Electrocardiogram in pericarditis. Am J Cardiol. 1970;26:471–4. doi: 10.1016/0002-9149(70)90704-6. [DOI] [PubMed] [Google Scholar]
- 8.Spodick DH. Diagnostic electrocardiographic sequences in acute pericarditis: Significance of PR segment and PR vector changes. Circulation. 1973;48:575–80. doi: 10.1161/01.cir.48.3.575. [DOI] [PubMed] [Google Scholar]
- 9.Cappato R, Calkins H, Chen SA, Davies W, Lesaka Y, Kalman J, et al. Updated worldwide survey on the Methods, Efficacy, and Safety of Catheter Ablation for Human Atrial Fibrillation. Circ Arrhythm Electrophysiol. 2010;3:32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]


