Abstract
This annual article presents information on health care costs by business, households, and government. Households funded 35 percent of expenditures in 1990, government 33 percent, and business, 29 percent. During the last decade, health care costs continued to grow at annual rates of 8 to 16 percent. Burden measures show that rapidly rising costs faced by each sponsor sector are exceeding increases in each sector's ability to fund them.
Increased burden is particularly acute for business. The authors discuss the problems these rising costs pose for business, particularly small business, and some of the strategies businesses employ to constrain this cost growth.
Introduction
National health expenditures consumed 12.2 percent of the gross national product (GNP) in 1990 (Levit et al., 1991) and are expected to rise to 16.4 percent of GNP in the year 2000 (Sonnefeld et al., 1991). These increases raise concern over the availability of resources to pay for upwardly spiraling health care costs—resources that differ by sponsor. By measuring the burden health care costs impose on each sponsor, we can track mounting pressure within the separate sponsor sectors that will trigger change. These pressures have been building for both business and government for several decades; however, for the household sector, increasing health care cost burdens are only beginning to be felt.
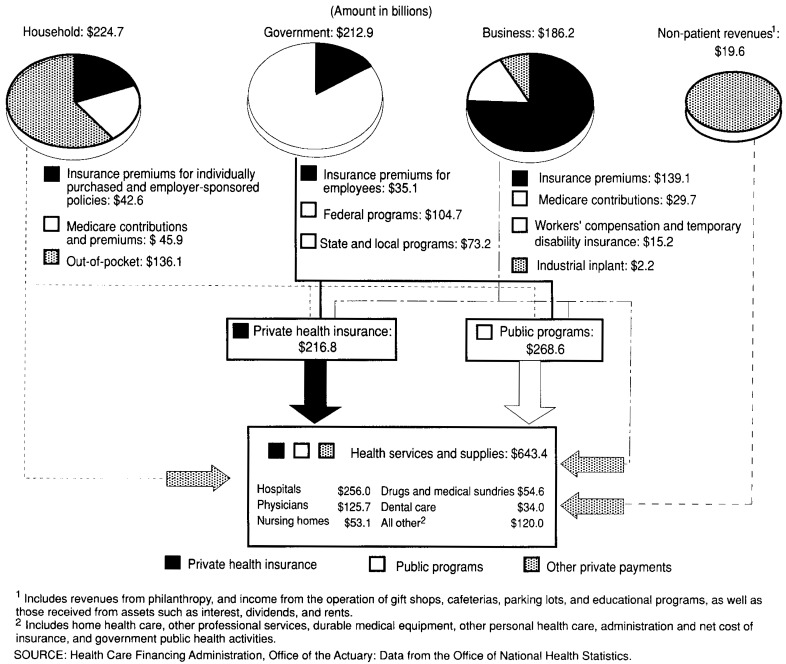
The analysis presented in this article builds on the national health accounts (NHA), which present spending by health care bill payers such as Medicaid, Medicare, and private health insurance. The NHA estimates are rearranged and disaggregated to permit an examination of sponsors of health care who provide funding to bill payers. These major sponsors of health care are business, households, government, and non-patient revenues. Their spending is measured as expenditures for health services and supplies (HSS) that represent the cost of health care excluding research and construction. Some payments for HSS by sponsors pass through health care bill payers such as insurance and government, while other payments (e.g., out-of-pocket, non-patient revenues) flow directly into the health care system (Figure 1). In this article, one additional level of payer is revealed beyond those presented in NHA. Ultimately, however, the individual bears the primary responsibility of paying for health care through health insurance premiums, out-of-pocket costs, philanthropic contributions to health organizations, income taxes, earnings reduced by increases in employers' health insurance costs, and higher cost of products.
Figure 1. Flow of funds from sponsors of health care into the health care system: United States, 1990.
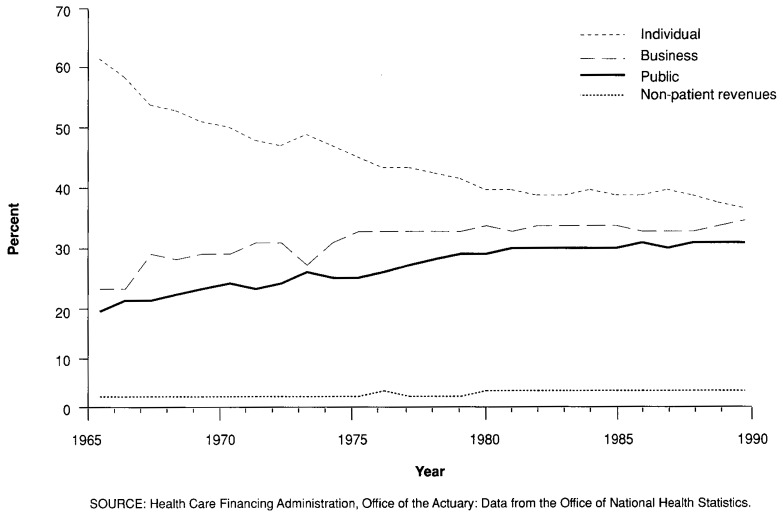
HSS amounted to $643.4 billion in 1990, an increase of 10.5 percent since 1989, the third consecutive year that HSS has grown at double-digit rates. Over time, the primary responsibility for sponsoring health care costs shifted from the household to other sources, such as business and government. In 1965, households paid for 61 percent of all HSS, with business accounting for 17 percent and public programs accounting for 21 percent. By 1990, the distribution of payments changed, so that each of the major components accounted for approximately one-third of the health care cost (Figure 2). Because of these changes, business is becoming extremely concerned over the costs of health care and the amount of resources being consumed. This was especially true in 1990, as the United States entered a recession. The recession caused growth in consumer spending for most goods and services to slow down, while spending for health care continued to grow unabated.
Figure 2. Percent of expenditures for health services and supplies, by payer: United States, 1965-90.
Business paid $186.2 billion for health care in 1990 (Table 1), 29 percent of HSS. Business estimates include expenditures for all types of organizations—sole proprietorships, partnerships, and corporations. These payments cover employer contributions to health insurance premiums for employees, mandatory employer contributions to the Medicare hospital insurance trust fund, workers' compensation medical premiums, temporary disability medical insurance, and industrial inplant services.
Table 1. Expenditures for health services and supplies, by type of payer: United States, selected calendar years 1965-90.
| Type of payer | 1965 | 1970 | 1975 | 1980 | 1985 | 1986 | 1987 | 1988 | 1989 | 1990 |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Amount in billions | ||||||||||
| Total | $38.2 | $69.1 | $124.7 | $238.9 | $407.2 | $438.9 | $476.8 | $526.2 | $582.1 | $643.4 |
| Private | 30.3 | 50.1 | 86.2 | 162.1 | 278.9 | 302.9 | 327.2 | 362.8 | 397.5 | 430.4 |
| Private business | 6.5 | 15.1 | 28.8 | 64.8 | 115.0 | 127.3 | 133.6 | 153.1 | 169.7 | 186.2 |
| Employer contribution to private health insurance premiums | 5.4 | 11.2 | 20.9 | 48.4 | 85.4 | 93.6 | 96.7 | 112.9 | 125.7 | 139.1 |
| Employer contribution to Medicare hospital insurance trust fund1 | 0.0 | 2.1 | 5.0 | 10.5 | 20.3 | 23.3 | 24.7 | 26.3 | 28.4 | 29.7 |
| Workers' compensation and temporary disability insurance | 0.8 | 1.4 | 2.4 | 5.1 | 7.8 | 8.8 | 10.5 | 12.0 | 13.6 | 15.2 |
| Industrial inplant health services | 0.2 | 0.3 | 0.5 | 0.9 | 1.4 | 1.6 | 1.7 | 1.9 | 2.1 | 2.2 |
| Household | 23.1 | 33.6 | 54.9 | 90.3 | 152.0 | 162.7 | 179.8 | 194.3 | 210.3 | 224.7 |
| Employee contribution to private health insurance premiums and individual policy premiums | 4.1 | 4.6 | 8.9 | 16.2 | 28.4 | 28.9 | 35.3 | 34.9 | 39.2 | 42.6 |
| Employee and self-employment contributions and voluntary premiums paid to Medicare hospital insurance trust fund1 | 0.0 | 2.4 | 5.7 | 12.0 | 24.0 | 27.6 | 29.5 | 31.4 | 33.8 | 35.7 |
| Premiums paid by individuals to Medicare supplementary medical insurance trust fund | 0.0 | 1.0 | 1.7 | 2.7 | 5.2 | 5.2 | 6.1 | 8.7 | 11.2 | 10.2 |
| Out-of-pocket health spending | 19.0 | 25.6 | 38.5 | 59.5 | 94.4 | 100.9 | 108.8 | 119.3 | 126.1 | 136.1 |
| Non-patient revenue | 0.6 | 1.5 | 2.5 | 7.0 | 12.0 | 12.9 | 13.8 | 15.4 | 17.5 | 19.6 |
| Public | 7.9 | 18.9 | 38.5 | 76.7 | 128.3 | 135.9 | 149.6 | 163.4 | 184.6 | 212.9 |
| Federal Government | 3.4 | 10.4 | 21.3 | 42.5 | 69.0 | 70.4 | 77.3 | 84.2 | 96.2 | 113.9 |
| Employer contributions to private health insurance | 0.2 | 0.3 | 1.2 | 2.2 | 4.3 | 3.9 | 4.9 | 6.4 | 8.1 | 9.2 |
| Adjusted Medicare | 0.0 | 2.0 | 3.3 | 11.1 | 20.4 | 18.5 | 20.0 | 20.8 | 25.5 | 31.5 |
| Medicare | 0.0 | 7.6 | 16.4 | 37.5 | 72.2 | 77.4 | 83.4 | 90.5 | 102.6 | 111.2 |
| Less Medicare hospital trust fund contributions and premiums | 0.0 | 4.7 | 11.3 | 23.7 | 46.6 | 53.7 | 57.3 | 61.0 | 65.9 | 69.5 |
| Less Medicare supplementary medical insurance premiums | 0.0 | 1.0 | 1.7 | 2.7 | 5.2 | 5.2 | 6.1 | 8.7 | 11.2 | 10.2 |
| Health program expenditures (excluding Medicare) | 3.3 | 8.2 | 16.8 | 29.2 | 44.3 | 48.0 | 52.4 | 57.0 | 62.6 | 73.1 |
| Medicaid | 0.0 | 2.9 | 7.4 | 14.5 | 23.1 | 25.4 | 27.9 | 31.0 | 35.4 | 42.9 |
| Department of Veterans Affairs | 1.2 | 1.8 | 3.5 | 5.9 | 8.6 | 9.1 | 9.6 | 10.0 | 10.6 | 11.4 |
| Department of Defense | 1.0 | 1.8 | 2.8 | 4.3 | 7.6 | 8.4 | 9.3 | 9.8 | 10.4 | 11.5 |
| Other programs2 | 1.2 | 1.8 | 3.0 | 4.4 | 4.9 | 5.2 | 5.6 | 6.2 | 6.2 | 7.4 |
| State and local government | 4.5 | 8.5 | 17.2 | 34.2 | 59.3 | 65.5 | 72.3 | 79.1 | 88.4 | 99.1 |
| Employer contributions to private health insurance | 0.3 | 0.6 | 1.9 | 6.7 | 16.0 | 16.7 | 17.9 | 20.2 | 23.4 | 25.9 |
| Employer contributions to Medicare hospital insurance trust fund | 0.0 | 0.2 | 0.7 | 1.3 | 2.2 | 2.7 | 3.1 | 3.3 | 3.7 | 4.1 |
| Health expenditures by program | 4.2 | 7.6 | 14.6 | 26.3 | 41.1 | 46.1 | 51.4 | 55.6 | 61.2 | 69.1 |
| Medicaid | 0.0 | 2.5 | 6.1 | 11.6 | 18.6 | 19.8 | 22.9 | 23.9 | 26.8 | 32.3 |
| Hospital subsidies | 2.6 | 3.4 | 5.2 | 6.2 | 7.8 | 10.0 | 11.2 | 12.4 | 13.1 | 14.1 |
| Other programs3 | 1.6 | 1.8 | 3.3 | 8.5 | 14.7 | 16.3 | 17.3 | 19.3 | 21.3 | 22.7 |
Includes one-half of self-employment contribution to Medicare hospital insurance trust fund.
Includes Maternal and Child Health, Vocational Rehabilitation, Alcohol, Drug, and Mental Health Administration, Indian Health Service, Office of Economic Opportunity (1965-74), and other miscellaneous general hospital and medical programs and public health activities.
Includes other public and general assistance, Maternal and Child Health, Vocational Rehabilitation, and public health activities.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
The employer contribution to employee health insurance premiums accounts for the largest portion of private business health spending: $139.1 billion, or 75 percent. The second-largest component is the employer contribution to the Medicare hospital insurance trust fund, which, at $29.7 billion, holds a 16-percent share. Workers' compensation, temporary disability insurance, and industrial inplant health services comprise the remaining $17.4 billion, or 9 percent of private business health spending. Since the advent of Medicare and Medicaid in 1966, these component shares of private business health care expenditures have remained stable.
Despite stability of each business components' share of business health spending, business' overall share of HSS has risen. Each major component contributed to rising business health care costs and caused the business share of the total health care bill to grow. The expansion of employer-paid insurance in both the number of workers and dependents covered and in breadth of coverage is well known. Employers also shared in paying for public insurance premiums of their employees through Federal Income Compensation Act (FICA) taxes for Medicare. The growth in Medicare contributions was the result of increases in either the annual maximum taxable earnings, on which the employers' and employees' Medicare contribution was applied, or the contribution rates, or both. In 1966, the maximum taxable earnings level was $6,600 with a contribution rate of 0.35 percent; by 1990, these had risen to $51,000 and 1.45 percent, respectively.
Household spending accounted for $224.7 billion, or 35 percent, of expenditures in 1990. This total covered spending for health insurance premiums, including the employee contribution to employer-sponsored or individually purchased policies, contributions and premiums to Medicare trust funds, and out-of-pocket payments. Out-of-pocket spending includes copayments, deductibles, and payments for services not covered by insurance (for individuals with either limited or no insurance).
Household spending as a share of HSS has felt the largest impact, as the sources of health care payments changed over time. In 1965, households accounted for 61 percent of all HSS expenditures; by 1990, households accounted for 35 percent (Table 2). This change is in part a result of the advent of Medicare, Medicaid, and other public programs that increased the government role in paying for health care of the elderly and indigent. Also, employer-sponsored insurance grew dramatically throughout this time period. Insurance is the major cause of business health care cost rising from 17 percent of HSS in 1965 to 29 percent in 1990. Employer-sponsored insurance plans reallocated health care expenses from the household to private and public employers.
Table 2. Percent distribution of expenditures for health services and supplies, by type of payer: United States, selected calendar years 1965-90.
| Type of payer | 1965 | 1970 | 1975 | 1980 | 1985 | 1986 | 1987 | 1988 | 1989 | 1990 |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Percent distribution | ||||||||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Private | 79 | 73 | 69 | 68 | 68 | 69 | 69 | 69 | 68 | 67 |
| Private business | 17 | 22 | 23 | 27 | 28 | 29 | 28 | 29 | 29 | 29 |
| Household (individual) | 61 | 49 | 44 | 38 | 37 | 37 | 38 | 37 | 36 | 35 |
| Non-patient revenue | 2 | 2 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Public | 21 | 27 | 31 | 32 | 32 | 31 | 31 | 31 | 32 | 33 |
| Federal Government | 9 | 15 | 17 | 18 | 17 | 16 | 16 | 16 | 17 | 18 |
| State and local government | 12 | 12 | 14 | 14 | 15 | 15 | 15 | 15 | 15 | 15 |
NOTE: Columns may not add to totals shown because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Non-patient revenues, including philanthropic funds, providers' interest income, and revenues from other non-patient care activities, were $19.6 billion in 1990. Non-patient revenue estimates transfer directly from the NHA and have been responsible for 3 percent of HSS since 1980 (Table 2) and 2 percent from 1965 to 1980.
Public expenditures from general revenues, which include spending for some of Medicare and all of Medicaid, reached $212.9 billion in 1990. This spending accounts for 33 percent of HSS. Public expenditures in this payer taxonomy include payments for health care programs such as Medicaid, Medicare, U.S. Department of Defense, maternal and child health, and other Federal and State and local programs. For the purpose of realigning payments to the sponsors of health care, the estimates for Medicare include only general revenue funds. These funds flow into the Medicare trust fund from taxes. The other sources of funds for Medicare, premiums and contributions, are allocated to the health care sponsor (households or business) that paid them. Public expenditures also include insurance premiums for employees of government agencies. In 1990, these insurance premiums amounted to $9.2 billion for Federal employees and $25.9 billion for State and local employees.
Business expenditures
In 1990, expenditures by private business accounted for 29 percent of health services and supplies, or $186.2 billion. Private business financed health care through contributions to the Medicare hospital insurance trust fund ($29.7 billion), payments for the medical portion of workers' compensation and temporary disability insurance premiums ($15.2 billion), and industrial inplant health services ($2.2 billion). The primary method of business support of health care is through the provision of health insurance for employees. The premiums for health insurance cost business $139.1 billion in 1990, an increase of 10.6 percent from 1989.
These aggregate private business health insurance premiums summarize the experience of business nationally. They represent the experience of all sizes of establishments in all industries. These premiums for hospital, medical, dental, prescription drug, and vision coverage include those paid to insurance companies, Blue Cross and Blue Shield organizations, and health maintenance organizations, as well as the costs incurred by businesses that self-insure health care benefits. These aggregate private business health insurance premiums cover only the employer contributions for policies of current workers, retirees, former workers, and dependents. They measure the aggregate financial impact on business of the provision of health care benefits to workers.
Other private sector surveys report growth rates for employer-sponsored health insurance that are higher than, although not necessarily inconsistent with, those estimated in this article. A. Foster Higgins (1991) reports growth rates in premiums per covered employee of 21.5 percent for fee-for-service plans in 1990 and for all plans of 17.1 percent. The Health Insurance Association of America (HIAA) survey cites premium increases of 14 percent per covered worker (Sullivan and Rice, 1991). Close examination of these statistics reveals differences in what these growth rates measure (employer-only versus employer and employee costs; aggregate versus per employee costs) and scope of business (and governments) covered.
Employers' role in providing insurance
Private health insurance became established as a fringe benefit of employment during World War II. During this period of labor shortages, employers began to use fringe benefits, including health benefits, to entice marginal non-workers into the labor force and to discourage existing workers from changing jobs (Starr, 1982). Since World War II, private health insurance has grown to become an acknowledged and accepted “responsibility” of business, a role that continues today.
Business accepted the function of primary provider of health insurance for the non-elderly population, encouraged by insurance companies, government, and employees. First, insurers preferred employer groups because they reduced private health insurers' risk of adverse selection and provided insurance companies with a mechanism for reducing their marketing, enrollment, and premium collection costs below those encountered when selling to individuals.
Second, government supported employer-sponsored private health insurance by offering tax incentives that encouraged business to assume this role of health insurance sponsor. Government tax rules treated health insurance premiums as a business expense that reduces a business' gross taxable income. It also excluded these benefits from workers' taxable gross income, raising the effective wage rate to the employee without incurring additional cost to the employer. These tax incentives promoted public policy objectives of making health care accessible and affordable without direct government intervention.
Third, employees continue to view health insurance benefits as a major factor in their decisions to change or remain in a job (Katz, 1991). Insurance companies, government, and workers have reinforced business' historical role as providers of health insurance. Therefore, businesses today believe that employers should be the source of health insurance benefits for their employees and dependents (Woolsey, 1991).
Whereas both employers and employees derive advantages from employers' role in sponsoring health insurance, pressure for change is mounting, as recorded by recently conducted polls. A Robert Wood Johnson Foundation survey of business executives found that, despite its positive aspects, changes would be required to enhance the health care system, particularly in the area of value received for expenditures (Johnson, 1991). In addition, more than one-third of large employers surveyed by the Washington Business Group on Health would favor a national health system if medical costs grow over the next 3 years at rates of 15 percent or more (Woolsey, 1991). As health care costs reach the projected 16.4 percent of GNP by the year 2000 (Sonnefeld et al., 1991), the burdens borne by business will have an ever-increasing impact. The rising costs, in addition to these attitudes expressed by business, will be instrumental in triggering any health care reform.
Rising business health care costs
Employers' role in providing health care coverage has existed for more than half of this century. Both employers and employees view this role as an important benefit in attracting and keeping workers. But the cost of health care sponsored by employers has increased almost threefold over the past decade alone—from $64.8 billion in 1980 to $186.2 billion in 1990. Three-quarters of 1990 business expenditures for health care—$139.1 billion—went for the employer share of private health insurance premiums. These premiums financed 22 percent of costs for HSS in the United States in 1990 and provided coverage to 140.4 million workers and their dependents and another 11.4 million non-workers and their dependents (Fu Associates Ltd., 1991).
The burden that health care imposes on business has soared over the past 25 years (Table 3). In 1990, employer health care costs consumed 3.9 percent of the gross private domestic product of the Nation, almost four times the share these costs represented in 1965. As a share of total compensation of labor, business health care spending climbed to 7.1 percent in 1990, up from 4.9 percent in 1980 and 2.0 percent in 1965. In 1990, health care costs represented 45.5 percent of all fringe benefits provided to employees, more than double the share of fringe benefits in 1965 (22.4 percent). To gauge the size of health care expenditures, business health care expenditures can be compared with profits. These statistics show that health care spending by business equaled 61.1 percent of corporate profits1 before tax and was greater than the amount of corporate profits after tax (107.9 percent) in 1990. These comparisons highlight business concerns about the burden that rising costs are placing on their ability to continue providing these benefits.
Table 3. Expenditures for health services and supplies as a percent of business income, expense, or profit: United States, selected calendar years 1965-90.
| Business health spending as a share of | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Total business receipts3 | Gross private domestic product4 | Labor compensation | Corporate profits1,2 | ||||
|
|
|
||||||
| Total compensation5 | Wages and salaries5 | Fringe benefits5 | Before tax | After tax | |||
|
| |||||||
| Percent | |||||||
| 1965 | 0.4 | 1.0 | 2.0 | 2.2 | 22.4 | 8.4 | 14.0 |
| 1970 | 0.7 | 1.7 | 3.1 | 3.5 | 29.2 | 19.8 | 36.1 |
| 1975 | 0.8 | 2.1 | 3.9 | 4.5 | 28.5 | 21.3 | 34.3 |
| 1980 | 0.9 | 2.7 | 4.9 | 5.8 | 31.7 | 27.3 | 42.6 |
| 1985 | 1.2 | 3.3 | 6.1 | 7.2 | 38.9 | 51.3 | 89.9 |
| 1986 | 1.3 | 3.4 | 6.3 | 7.5 | 40.5 | 57.5 | 110.4 |
| 1987 | 1.3 | 3.4 | 6.2 | 7.3 | 40.8 | 48.5 | 90.1 |
| 1988 | 1.3 | 3.6 | 6.5 | 7.7 | 43.2 | 48.3 | 84.8 |
| 1989 | NA | 3.7 | 6.9 | 8.1 | 45.1 | 55.1 | 98.3 |
| 1990 | NA | 3.9 | 7.1 | 8.5 | 45.5 | 661.1 | 6107.9 |
Based on July 1990 data from the U.S. Department of Commerce national income and product accounts.
A similar concept of “profits” for sole proprietorships and partnerships is not available.
Business receipts for sole proprietorships and total receipts of partnerships and corporations based on Internal Revenue Service data.
Reflects health costs embedded in the unduplicated value of intermediate and final goods; based on data from the U.S. Department of Commerce national income and product accounts.
For employees in private industry.
Estimated. U.S. Department of Commerce benchmark revisions will not be available until November 1991.
NOTE: NA is not available.
SOURCE: Health Care Financing Administration. Office of the Actuary: Data from the Office of National Health Statistics.
Rising health care costs have had a profound effect on the coverage of workers. The U.S. Bureau of the Census conducts the Current Population Survey that collects information on the health insurance status of individuals each March. Data for 1990 reveal that three-quarters of the uninsured population, 25.0 million persons, reside in families in which the greatest income earner works full time. These data show an estimated increase of 28 percent in the number of uninsured full-time workers and their dependents since 1980. During this time period, the number of all full-time workers and their dependents increased 7.9 percent (Fu Associates Ltd., 1991). This shows that full-time employment does not guarantee health insurance coverage and has become less able to guarantee coverage over the last decade. If the percentage of full-time workers and their dependents that were uninsured in 1990 had been the same as in 1980, business' share of HSS and the burden that these costs imposed on business would be even greater than shown here.
Dilemmas of small business
The business share of HSS, 29 percent in 1990, is not borne evenly across all business. Small employers are disadvantaged in their ability to provide health insurance benefits to their workers. The problem of uninsured workers manifests itself most noticeably in small business with fewer than 100 workers. These establishments employ 40.8 million workers, or two-fifths of civilian employees in full-time or part-time jobs. The U.S. Department of Labor conducted surveys on workers in small establishments (fewer than 100 employees) for 1990 and in medium and large establishments for 1989. These statistics show that 92 percent of full-time employees in medium and large firms participate in employer-sponsored plans, compared with 69 percent of full-time employees in small establishments (U.S. Bureau of Labor Statistics, 1991).
Part of the cause of uninsured employees of small businesses can be linked to the health insurance premium costs faced by these companies. Employer-sponsored health insurance premiums paid by small business exceed those paid by larger companies for the same benefit package. These higher costs affect small business' ability to compete with larger firms in both labor and product markets.
Higher costs in the provision of health insurance benefits for small business result from several factors. First, the health insurance marketplace is becoming more fragmented. Increasingly, insurers are basing insurance rates on an individual company's claims history (experience rating), rather than pooling all sizes of employers in an area to share the insurance risk (community rating). This process segments the insurance market into lower risk (i.e., lower cost) large employers and higher risk (i.e., higher cost) small employers (Arnett and Trapnell, 1984).
Second, larger companies are also more likely to take advantage of cost savings resulting from self-insuring employee health care. Self-insuring reduces costs to employers by eliminating State premium taxes, profits paid to insurance companies, and the marketing costs and commissions embedded in premiums, while retaining the interest earned on reserves held to cover claims. Self-insured businesses also can eliminate State-mandated benefits (McDonnell et al., 1986).
Third, small business' competitive disadvantage in the acquisition of health insurance is compounded by tax laws that discriminate against small firms in favor of corporations. Corporations can write off 100 percent of their medical premium expense. Small businesses that are classified as sole proprietorships, partnerships, and S-corporations are permitted to deduct only 25 percent of premiums.
Finally, it is possible that insurers may choose not to provide coverage for certain industries where small businesses are prevalent. Industries include those with higher risk occupations, higher likelihood of litigation (e.g., physicians and lawyers), or higher incidence of drug and alcohol abuse or of acquired immunodeficiency syndrome (AIDS). These exclusions constrain many small employers by reducing the number of companies from which they can seek coverage.
High insurance premiums frequently force small businesses to change policies in search of more favorable rates. New policies subject employees to pre-existing-condition exclusions, jeopardizing access to care for employees most in need of coverage.
Small businesses face additional problems from the 1985 Consolidated Omnibus Budget Reconciliation Act (COBRA) that forces employers with 20 or more employees to make available group insurance protection to former employees for 18 months after separation and for their dependents for 3 years. COBRA mandates that premiums charged by employers equal no more than 102 percent of the premiums paid by similar active workers. According to recent studies, COBRA claims per worker exceeded those of active employees by 33-100 percent, (Huth, 1991) and smaller companies reported higher claims costs per beneficiary than do larger ones (Towers Perrin/The National Association of Manufacturers, 1991). COBRA drives up employer premium costs because active workers must subsidize higher costs of former employees. This legislation is particularly adverse to small businesses that not only face higher costs for their COBRA beneficiaries but that frequently experience higher employee turnover rates.
Retiree health care
Employers offering health benefits to current and future retirees face new challenges that will likely increase their future share of health care costs. Most employers operate on a pay-as-you-go basis for retiree health care, purchasing policies or paying claims as they arise. As the number of retirees increases in relation to the number of current workers, these benefits will become more difficult to fund. Beginning in 1993 and gradually implemented over many years, the Financial Accounting Standards Board (FASB) will require employers to account for accrued retiree health benefit liabilities from the date that employees are hired until they become eligible for benefits. Estimates of the accrued cost of these benefits that will enter financial statements range from $400 billion to $2 trillion (Adler, 1991). FASB will force employers to recognize future health insurance liabilities as they are incurred, greatly increasing the current overall book value of employer-sponsored health care.
Business strategies in containing costs
Employers are taking steps aimed at reducing their share of health care costs. Elimination of employer-sponsored health insurance coverage is one drastic solution to rising health care costs that businesses—particularly small ones—have used. Some large companies have sought temporary relief from the relentless rise of health care costs through self-insurance. That option is less viable for small business.
Seventeen States have already instituted and another 10 are considering exemptions from State-mandated benefits for small firms that have not contributed to health insurance coverage for their workers during the past 12 months. State-mandated benefits raise costs faced by business in supplying health care coverage to employees because a specific set of benefits must be included in employer-sponsored health plans. The “bare-bones” policy alternative permits employers to provide basic private health insurance coverage for employees who previously lacked employer-sponsored coverage.
Some small firms are experimenting with 50/50 coinsurance plans that require employees to contribute one-half the cost of medical care services up to a certain limit before stop-loss coverage kicks in. These plans provide employees with an incentive to use services judiciously, as they must contribute one-half of the cost from out-of-pocket sources. These plans can mean premium reductions of 10-20 percent from those charged for conventional plans that require employees to contribute 20 percent of the cost of services (Landes, 1991).
The rising cost of retiree health care and the new FASB requirements have caused employers to re-evaluate their retiree health benefit programs. Business has employed or is considering strategies to minimize future health care costs by this group of beneficiaries. These include fixing employer contributions to future health care plans; gauging employer contribution to length of employment and increasing the basic eligibility requirements; offering minimal plans to younger retirees; increasing deductibles and out-of-pocket maximum expenditures by retirees; and requiring active workers to contribute currently to future health care benefits (Quinn, 1991).
Business summary
In summary, employer-sponsored private health insurance has been in existence for half a century in the United States. Historically, employers believed their role in sponsorship of health insurance for their workers to be appropriate and worthwhile. Prospective workers typically examine these benefits when choosing a job and often make their employment decision based on the availability and breadth of these benefits. But rapidly rising health care costs are forcing businesses to re-evaluate their role with regard to private health insurance. Small businesses in particular face tremendous problems in affording and keeping this benefit for their employees, while still maintaining competitive prices for their products. Many strategies are being used in an attempt to reduce these costs. Through 1990, however, a reduction in overall cost or in business' share of the Nation's rapidly rising health care bill does not appear to have occurred.
Households
Households spent $224.7 billion on health care during calendar year 1990, an increase of 6.8 percent from 1989. The largest single category of payments by families is for out-of-pocket medical expenditures, financing 21.2 percent of HSS expenditures in 1990. These expenditures pay for services not covered by insurers and for copayments and deductibles required by insurers for covered health care services. Additional family expenditures for health care include spending for health insurance purchased individually or through employers, contributions to the Medicare hospital insurance trust fund through payment of FICA taxes, a small amount of voluntary premiums paid by individuals to the Medicare hospital insurance trust fund, and premiums paid to the Medicare supplementary medical insurance trust fund.
The spending for which individuals are responsible has grown at a slower pace than overall health care costs for most years since 1965, primarily because of the falling share of health expenditures paid from out-of-pocket sources. Public and private health insurance assumed greater responsibility for health care costs during this period. Since 1980, contributions to the Medicare hospital insurance trust fund and premiums paid to the Medicare hospital and supplementary medical insurance trust funds have risen as a share of total health care costs. These increases have offset most, but not all, of the small declines in the out-of-pocket share of health care costs.
As a result of slower growth than that of overall health care costs, households' share of the Nation's health care bill fell from 61 percent in 1965 to 49 percent in 1970, 38 percent in 1980, and 35 percent in 1990. Although this share continued to fall during the past decade, it fell less rapidly than it had previously. It appears that efforts by other sectors to shift some proportion of the costs back to households have slowed the decline in share paid by households, but not to the point that that share has begun to rise.
Health care costs financed by households must be funded from available income. Therefore, their share of adjusted personal income is used to measure the burden of such costs on families. After maintaining a stable share from 1965 to 1980, households' share of personal income devoted to health care began to gradually rise from 4.1 percent in 1980 to 5.0 percent in 1990 (Table 4). Calculations made using data from the 1989 Bureau of Labor Statistics' Consumer Expenditure Survey show health care spending as a share of income after taxes at 4.9 percent for all households. Households where the reference person is 65 years of age or over show a significantly higher share of income going to health care—11.5 percent in 1989. The elderly not only use more care, some of which must be paid from income, but these out-of-pocket costs affect the elderly's disposable income disproportionately.
Table 4. Expenditures for health services and supplies as a percent of household (individual) income: United States, selected calendar years 1965-90.
| Year | Individual heatlh spending as a share of adjusted personal income2 | Health spending as a share of income after taxes1 | |
|---|---|---|---|
|
| |||
| All ages | Reference person 65 years of age or over3 | ||
|
| |||
| Percent | |||
| 1965 | 4.2 | — | — |
| 1970 | 4.1 | — | — |
| 1972-73 | — | 5.1 | 8.9 |
| 1975 | 4.3 | — | — |
| 1980 | 4.1 | — | — |
| 1985 | 4.7 | 4.8 | 11.0 |
| 1986 | 4.7 | 4.9 | 11.8 |
| 1987 | 4.9 | 4.6 | 10.7 |
| 1988 | 4.9 | 5.0 | 12.5 |
| 1989 | 4.9 | 4.9 | 11.5 |
| 1990 | 5.0 | — | — |
Calculated from the Consumer Expenditure Integrated Survey of the U.S. Bureau of Labor Statistics. In this survey, the institutionalized population, including nursing home residents, were excluded, so spending for nursing home care covers only a small portion of total days of care.
Personal income adjusted to include personal Medicare contributions and to exclude certain transfer payments (medical benefits for Medicare, Medicaid, workers' compensation, and temporary disability insurance).
Consumer expenditure data are tabulated by age of reference person. These households may include some individuals under 65 years of age. Similarly, individuals 65 years or over who reside in households where the reference person is under 65 years of age are excluded.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Households are insulated from the full costs of health care. For services covered by private insurance, households are responsible for copayments and/or deductibles, with the insurance paying a substantial portion of the charges. Families make their decision to purchase and utilize services based on a greatly reduced out-of-pocket perceived price at the point of purchase—prices that only include a portion of the full costs. The average price of the remaining portion of privately insured services is more adequately reflected in prepaid private health insurance premiums. To the extent that the cost of this premium is shared with an employer, the household may be unaware of and/or unaffected by the true price paid for health care services. Private health insurance plays an important social function by spreading one person's excessive medical costs over all similarly insured persons. However, the benefits of risk sharing through insurance also provide incentives for overuse of services and the purchasing of higher priced services than would otherwise be the case.
Recent surveys indicate that households in general do not currently feel burdened by the costs of health care. Results of an Employee Benefit Research Institute (EBRI) survey of citizens' attitudes toward the health care system indicated that Americans are satisfied with the health care system as it currently exists and would balk at major share increases in their responsibility for financing employer-sponsored health insurance premiums. Only one-half of the respondents were willing to pay $2,000 for their share of premiums, despite the fact that employers pay considerably more per employee for this benefit (Shalowitz, 1991).
The Federal Government promotes the use of employers as a mechanism for providing health insurance through the tax system. By excluding the employer-paid portion of employer-sponsored health insurance premiums from employees' taxable gross income, the Federal Government partially subsidizes health care benefits. It also achieves policy objectives in providing a mechanism for affordable and accessible health care for more workers than would otherwise be the case. In fiscal 1990, the Federal Government experienced revenue loss of $26.4 billion as a result of the exclusion of this employer benefit from individual's gross income. In other words, individuals would have paid an additional $26.4 billion in taxes if the employer-paid portion of health insurance premiums were taxable income to individuals (Executive Office of the President, 1991). This amount is not included in the accounting framework presented in this article.
Public sector payments
In 1990, Federal and State and local governments paid $212.9 billion for the financing and delivery of health care services. Governments as employers spent $35.1 billion providing health insurance coverage for its workers. In their role of promoting public policy and redistributing income, governments also target specific population groups with their health care spending. This encompasses expenditures such as those by the U.S. Departments of Defense and of Veterans Affairs for the operation of their own facilities. Also included are grants for needy population groups, such as the elderly, the poor, mothers and children, American Indians, school children, and the disabled; expenditures for public health activities; and State and local government hospital subsidies. Excluded from government expenditures are dedicated tax revenues paid into trust funds for specific programs, such as Medicare. Only general revenue contributions in support of programs such as Medicare are included. Government expenditures for health increased 15.3 percent from 1989 to 1990, 4.8 percentage points faster than the growth in overall health spending. This caused the share of expenditures financed by the public sector to increase slightly to 33 percent. Increases in general revenue contributions to Medicare contributed to this change.
The major cause, however, was increases in the Medicaid program, up 20.7 percent in 1990. Medicaid expenditures, jointly funded by Federal and State governments, increased from $62.3 billion in 1989 to $75.2 billion in 1990. These increases are at least partially attributable to the additional 1.7 million people on the Medicaid roles in 1990.
The Federal Government's health spending as a share of Federal revenues reached 17.2 percent in 1990, up from 15.2 percent in 1989. Since 1965, the proportion of Federal revenues spent on health care rose from 3.5 percent, prior to the introduction of Medicare and Medicaid, to 7.3 percent in 1970 and 11.6 percent in 1980 (Table 5).
Table 5. Expenditures for health services and supplies as a share of Federal and State and local government revenues: United States, selected calendar years 1965-90.
| Year | Federal Government health spending as a share of Federal revenues1 | State and local government health spending as a share of State and local revenues2 |
|---|---|---|
|
| ||
| Percent | ||
| 1965 | 3.5 | 7.5 |
| 1970 | 7.3 | 8.3 |
| 1975 | 11.0 | 10.2 |
| 1980 | 11.6 | 12.6 |
| 1985 | 14.4 | 13.5 |
| 1986 | 14.2 | 13.9 |
| 1987 | 13.7 | 14.4 |
| 1988 | 14.5 | 14.7 |
| 1989 | 15.2 | 15.4 |
| 1980 | 17.2 | 16.3 |
Excludes contributions to social insurance because these came directly from businesses and individuals. These funds are for dedicated purposes and are not part of the general revenue pool of funds from which health spending can be financed. Based on July 1991 data from the U.S. Department of Commerce national income and product accounts.
Excludes contributions to social insurance, as explained in footnote 1, and Federal grants in aid, such as Federal Medicaid grants to States. Based on July 1991 data from the U.S. Department of Commerce national income and product accounts.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
State and local government health spending as a share of revenues increased from 15.4 percent in 1989 to 16.3 percent in 1990. Medicaid is the second-largest State government budget component after education, so rapid increases in these expenditures in combination with the recession in 1990 severely strained State resources (Stropko et al., 1991).
Non-patient revenues
Non-patient revenues funded 3 percent of all health care spending in 1990, a share maintained throughout the past decade. Non-patient revenues consist of philanthropic expenditures for health care services and other revenue sources of institutions such as hospitals, home health agencies, and nursing homes that are not directly associated with the delivery of services. The latter includes revenues from sources such as gift shops, cafeterias, and parking lots. In 1990, $19.6 billion of health expenditures were funded from this source.
Methodology
In this article, we look at HSS by who sponsors the provision of health care services. HSS covers the cost of all personal health care goods and services, government public health activities, administrative costs of public programs, and the net cost of private health insurance. The sponsors of health care may be households, governments, or business. Spending on health care does not always flow directly from the sponsor into the health care system but can pass through intermediaries, such as insurers and governments. These payments in turn are allocated to the different types of health care services. For example, households, business, and governments each pay health insurance premiums: households through direct purchase of policies or through employees' contributions to employer-sponsored health insurance; business and government employers through contributions to employee health insurance plans. These premiums sum to $216.8 billion, the amount of private health insurance premiums in the NHA. Health insurance premiums are used to pay for the health care benefits or services delineated in the NHA, plus health insurers' administrative expenses and profits and/or retained earnings.
Most of the estimates (such as workers' compensation and non-patient revenues) presented in this article come directly from the NHA and are reassigned to separate sponsor categories. Other estimates also come from the NHA, although they must be disaggregated before reassignment. Two NHA estimates are affected by this disaggregation and reassignment: Medicare and private health insurance. Data sources used in Medicare disaggregation include the Annual Report of the Board of Trustees of the Federal Hospital Insurance Trust Fund (1991), Annual Report of theBoard of Trustees of the Federal Supplementary Medical Insurance Trust Fund (1991), and unpublished detailed data on Medicare hospital insurance tax liability from the Social Security Administration. Private health insurance estimates are split into private and public employer-paid premiums and household-paid premiums using data from the Bureau of Economic Analysis (BEA), U.S. Chamber of Commerce, Health Care Financing Administration, the U.S. Bureau of the Census, and the Office of Personnel Management.
A full description of methods used to produce these estimates has been published in previous articles (Levit and Cowan, 1990; Levit, Freeland, and Waldo, 1989). Any revisions to these methods are listed in the next section.
Revisions
There have been some revisions to the procedures and data sources used in the preparation of these estimates. Changes affect estimates for 1974 and later. The first change is to the private employer-sponsored health insurance estimates. The primary source of historic estimates of employer contributions to private health insurance premiums is the U.S. Department of Commerce, Bureau of Economic Analysis. The BEA estimates are used to quantify the private employer portion of the health insurance premiums for 1965-77. BEA will be revising its estimates of employer-paid premiums as part of its periodic benchmark. These revisions will affect estimates for 1978 and later, and were scheduled to be available in late 1991. In the interim, estimates have been developed that follow BEA's methods but that incorporate minor methodological changes and new or revised data sources. For private employers, premiums are estimated using the U.S. Chamber of Commerce survey of employee benefits (U.S. Chamber Research Center, 1990) and NHA estimates of insurance premiums. Estimates of insurance premiums were recently benchmarked (Office of National Cost Estimates, 1990) and current estimates presented here reflect those revisions.
Second, the data sources and estimation procedures for premiums paid by State and local governments for their employees were also revised. The current estimates integrate data from the 1982 and 1987 Census of Governments (U.S. Bureau of the Census, 1991). With the availability of these surveys, the estimates for State and local expenditures for employee health insurance were revised back to 1978.
A third revision affected estimates for household spending on health insurance premiums. For 1965-90, estimates of household contributions to health insurance premiums were developed using NHA estimates for health insurance premiums. The NHA estimate was reduced by the amount of revised employer-paid private and government premiums, resulting in the estimate of household premium payments for health insurance. New methods and data for estimating employer-paid health insurance premiums for private business and State and local governments caused household premium estimates to be revised for the period 1974 and forward.
Lastly, the estimates for this sponsor taxonomy are based on the NHA. The NHA are revised annually to incorporate newly released data. Because the NHA are the basis for this article, these annual revisions will affect the payer disaggregation. Recent significant changes in the NHA resulted from new data from the personal consumption expenditures (PCE) detail tables, produced every 5 years in conjunction with the GNP benchmark revisions. These tables provide component information on non-durable and durable medical products. The most recent detail table, 1982, became available for the 1990 update of the NHA, resulting in revisions to NHA estimates for non-durable and durable medical components. These revisions during the 1990 NHA update raised the 1989 non-durable medical product expenditures estimates by $6.0 billion and lowered durable medical product estimates by $2.1 billion. The out-of-pocket and private health insurance estimates for these two components were also revised back to 1978 as a result of the 1982 PCE detail tables. These revisions affected the total of health services and supplies and the allocation between out-of-pocket and health insurance premiums from 1978 forward.
A more complete description of these and other revisions to NHA estimates upon which the payer estimates are based can be found in Levit et al. (1991).
Summary
From 1965 to 1990, the cost of health services and supplies grew from $38.2 billion to $643.4 billion. For both business and government, rising health care costs imposed an ever-increasing burden as growth in their ability to finance these costs failed to keep pace. For households, the impact of rising costs on their ability to pay began to increase slightly in the mid-1980s. By 1990, the share of personal income devoted to health care reached 5.0 percent, up from 4.2 percent in 1965 and 4.1 percent in 1980.
While government provided health care coverage for the elderly, poor, disabled, and other special disadvantaged groups, business emerged as the primary source of health care coverage for workers and their dependents. Small businesses, in particular, have felt the burden of health care costs mount. Both insurers and governments are developing plans aimed at easing that burden for small employers. For all sizes of companies, the pending FASB regulations will make business' retiree health care costs more apparent and will undoubtedly alter the type and quantity of retiree benefits offered in the future.
Acknowledgments
This article was prepared under the general direction of Mark Freeland, Director of the Division of Health Cost Analysis. The authors wish to acknowledge the assistance of Sally Burner in providing disaggregation of insurance by type of insurer, Patricia McDonnell for researching insurance issues that arose during the preparation of this article and of private employer-sponsored health insurance estimates, and Louis Blank for investigating new insurance data sources. The authors are grateful to colleagues in the Office of National Health Statistics for their advice and comments: Ross Arnett, Mark Freeland, Charlie Fisher, Helen Lazenby, Suzanne Letsch, Dan Waldo, Sally Burner, and Patricia McDonnell.
Footnotes
Reprint requests: Anna Long, Office of National Health Statistics, L-1, EQ05, 6325 Security Boulevard, Baltimore, Maryland 21207.
A similar concept of “profits” for sole proprietorships and partnerships is not available.
References
- A. Foster Higgins. Health Care Benefits Survey: Report 1, Indemnity Plans: Cost, Design and Funding. Princeton, NJ.: A Foster Higgins; 1991. [Google Scholar]
- Alder S. Firms seek to minimize cost of retiree medical. Business Insurance. 1991 Jul 29;25(30):40. [Google Scholar]
- Arnett RH, Trapnell GR. Health Care Financing Review. 2. Vol. 6. Washington: U.S. Government Printing Office; Winter. 1984. Private health insurance: New measures of a complex and changing industry; pp. 31–42. HCFA Pub. No. 03195. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Board of Trustees of the Federal Hospital Insurance Trust Fund. 1991 Annual Report of the Board of Trustees of the Federal Hospital Insurance Trust Fund. Washington: May 17, 1991. [Google Scholar]
- Board of Trustees of the Federal Supplementary Medical Insurance Trust Fund. 1991 Annual Report of the Board of Trustees of the Federal Supplementary Medical Insurance Trust Fund. Washington: May 17, 1991. [Google Scholar]
- Executive Office of the President. Budget of the United States Government. Washington: U.S. Government Printing Office; 1991. Office of Management and Budget. [Google Scholar]
- Fu Associates Ltd. Unpublished results from tabulations of the Current Population Survey under Health Care Financing Administration Contract No 500-90-0010. Arlington, VA.: 1991. [Google Scholar]
- Huth SA. COBRA costs average of 150% of active costs. Employee Benefit Plan Review. 1991 Oct.46(4):14–19. [Google Scholar]
- Johnson C. Health system is flawed: CEOs. Business Insurance. 1991 Apr.25(15):1. [Google Scholar]
- Katz A. Benefits important in job search: Poll. Business Insurance. 1991 Jul 22;25(29):3. [Google Scholar]
- Landes J. 50/50 health plans start catching on. National Underwriter. 1991 Jan.3:7. [Google Scholar]
- Levit KR, Cowan CA. Health Care Financing Review. 2. Vol. 12. Washington: U.S. Government Printing Office; Winter. 1990. Burden of health care costs: Business, households, and governments; pp. 127–137. HCFA Pub. No. 03316. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Levit KR, Freeland MS, Waldo DR. Health Care Financing Review. 3. Vol. 10. Washington: U.S. Government Printing Office; Spring. 1989. Health spending and ability to pay: Business, individuals, and government; pp. 1–11. HCFA Pub. No. 03280. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Levit KR, Lazenby HC, Cowan CA, Letsch SW. Health Care Financing Review. 1. Vol. 13. Washington: U.S. Government Printing Office; Fall. 1991. National health expenditures, 1990; pp. 29–54. HCFA Pub. No. 03321. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- McDonnell P, Guttenberg A, Greenberg L, Arnett RH. Health Care Financing Review. 2. Vol. 8. Washington: U.S. Government Printing Office; Winter. 1986. Self-insured health plans; pp. 1–16. HCFA Pub. No. 03226. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Office of National Cost Estimates. Health Care Financing Review. 4. Vol. 11. Washington: U.S. Government Printing Office; Summer. 1990. Revisions to the national health accounts and methodology; pp. 42–54. HCFA Pub. No. 03298. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Quinn JB. Future retirees likely to see reductions in health benefits. The Washington Post. 1991 Aug.:3. Section H. [Google Scholar]
- Shalowitz D. Having their cake …: Americans like health benefits, but not the cost. Business Insurance. 1991 Apr.25(14):3. [Google Scholar]
- Sonnefeld ST, Waldo DR, Lemieux JA, McKusick DA. Health Care Financing Review. 1. Vol. 13. Washington: U.S. Government Printing Office; Fall. 1991. Projections of health care spending through the year 2000; pp. 1–27. HCFA Pub. No. 03321. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Starr P. The Social Transformation of American Medicine. New York: Basic Books, Inc.; 1982. [Google Scholar]
- Stropko EP, Clayton A, Tilson S . Medicaid Expansions: Coverage Improves but State Fiscal Problems Jeopardize Continued Progress. Washington: U.S. General Accounting Office; Jun, 1991. GAO Pub. No. GAO/HRD-91-78. [Google Scholar]
- Sullivan CB, Rice T. The health insurance picture in 1990. Health Affairs. 1991 Summer;10(2):104–115. doi: 10.1377/hlthaff.10.2.104. [DOI] [PubMed] [Google Scholar]
- Towers Perrin/The National Association of Manufacturers. COBRA survey results. Medical Benefits. 1991 Jul 30;8(14):3. [Google Scholar]
- U.S. Bureau of the Census. 1987 Census of Governments: Public Employment: Government Costs for Employee Benefits. Washington: U.S. Government Printing Office; Mar. 1991. U.S. Department of Commerce. [Google Scholar]
- U.S. Bureau of Labor Statistics. BLS reports on its first survey of employee benefits in small private establishments. U.S. Department of Labor; Washington: Jun 10, 1991. Press release. [Google Scholar]
- U.S. Chamber Research Center. Employee Benefits Survey Data from Benefit Year 1989, 1990 Edition. U.S. Chamber of Commerce; Washington: 1990. [Google Scholar]
- Woolsey C. Not ready to give up: Employers still want to provide health coverage. Business Insurance. 1991 May 20;25(20):3. [Google Scholar]