Abstract
Psychiatric, rehabilitation, long-term care, and children's facilities have remained under the reimbursement system established under the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 (Public Law 97-248). The number of TEFRA facilities and discharges has been increasing while their average profit rates have been steadily declining. Modifying TEFRA would require either rebasing the target amount or adjusting cost sharing for facilities exceeding their cost target. Based on our simulations of alternative payment systems, we recommend rebasing facilities' target amounts using a 50/50 blend of own costs and national average costs. Cost sharing above the target amount could be increased to include more government sharing of losses.
Introduction
TEFRA included provisions that changed Medicare's method of reimbursement for all inpatient hospital stays. Prior to TEFRA, section 223 limits constrained only routine costs. TEFRA extended these limits to both routine and ancillary costs. Hospital costs were reimbursable up to a limit which was the lesser of a hospital-specific cost target and a peer group target. There were seven peer groups based on bed size and urbanicity. All hospitals were reimbursed under TEFRA for 1 year only, fiscal year (FY) 1983. Beginning in October 1983, Medicare discharges from general acute care hospitals shifted to the prospective payment system (PPS) based on diagnosis-related groups (DRGs).
Certain specialized facilities were excluded from PPS and continue to be paid under the TEFRA system. These are psychiatric, rehabilitation, long-term care, children's, cancer, and drug and alcohol treatment facilities. Psychiatric and rehabilitation distinct-part units of general hospitals were also exempt from PPS. Excluded facilities were exempted from PPS because it was believed that differences in the types of care provided and the settings for this care were unsuited to a rate system based on national averages. The national data base used for creating DRGs either did not include or under-represented these groups.
Since the implementation of PPS, comparatively little research has focused on the financial impact of TEFRA on PPS-exempt hospitals and units, in spite of the increasing number of facilities (Table 1). Harrow and Cromwell (1990) found that the average facility loss per case was between 3 and 6 percent of their average cost. The study concluded that the TEFRA system would impose larger and larger losses over time. Studies conducted by the Prospective Payment Assessment Commission (1991) reached similar conclusions.
Table 1. Trends in the Number and Medicare Utilization of Prospective Payment System-Exempt Facilities: 1986-88.
| Type of Facility | 1986 | 1987 | 1988 | Percent Change 1986-88 | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Number of Facilities | Discharges | Number of Facilities | Discharges | Number of Facilities | Discharges | Number of Facilities | Discharges | |
| Psychiatric | 1,132 | 197,116 | 1,266 | 214,039 | 1,392 | 238,911 | 22.97 | 21.20 |
| Units | 761 | 121,616 | 856 | 135,010 | 930 | 149,839 | 22.21 | 23.21 |
| Hospitals | 371 | 75,500 | 410 | 79,029 | 462 | 89,072 | 24.53 | 17.98 |
| Rehabilitation | 446 | 84,988 | 521 | 102,742 | 590 | 121,271 | 32.29 | 42.69 |
| Units | 382 | 57,311 | 453 | 69,627 | 512 | 82,948 | 34.03 | 44.73 |
| Hospitals | 64 | 27,677 | 68 | 33,115 | 78 | 38,323 | 21.88 | 38.47 |
| Long-Term Care | 68 | 14,646 | 62 | 13,106 | 67 | 14,520 | −1.47 | −0.86 |
| Children's | 55 | 2,141 | 60 | 2,298 | 58 | 2,281 | 5.45 | 6.54 |
Amid rising concerns that the TEFRA system was imposing undue financial hardship on excluded facilities, renewed attention was devoted to the development of alternatives to TEFRA. For example, Cromwell et al. (1990) studied alternative payment systems for psychiatric facilities, and Langenbrunner et al. (1989) provided a complete discussion of payment options for excluded facilities. In addition, the Omnibus Budget Reconciliation Act (OBRA) of 1990 (Public Law 101-508) contained provisions that mandated the Health Care Financing Administration (HCFA) to develop alternative approaches to the reimbursement of PPS-excluded facilities.
The purpose of this article is to respond to the OBRA 1990 mandate by answering two important research questions. First, has the financial performance of TEFRA-excluded facilities continued to deteriorate? Second, if facilities have performed poorly, what modifications could be made to TEFRA to make reimbursement more efficient and equitable?
It should be recognized at the start that not all facilities should be guaranteed to make a profit or even to break even. Inefficient providers should be encouraged to change their management behaviors. The TEFRA system was designed as a cost-sharing reimbursement system subject to a target ceiling on payments that would encourage cost containment. The updating of such targets was the problem. While each facility's per discharge payment began with its own cost base, the same annual updates permitted PPS-included hospitals were applied to excluded facilities as well. Hence, rate updates may have no relation to changes in patient severity, case mix, or treatment innovations. Over time, payment levels could (and do) bear less and less of a relationship to costs, generating more and more financial losers. This is a serious concern. Although any flat rate or ceiling payment system will lead to winners and losers, by grafting a PPS-determined update onto the TEFRA cost-sharing arrangement, the government may have inadvertently treated some facilities unfairly. In reclaiming excess profits from PPS-included hospitals through artificially low updates, the government ignored the fact that it had already reclaimed most of the profits from PPS-excluded facilities through retrospective cost settlements. Growing numbers of TEFRA facilities losing money on Medicare patients has serious equity and efficiency concerns. Facilities serving the public well may be driven out of business by inadequate updates through no fault of their own.
The first part of this article provides an overview of TEFRA financial status. Profit rates per case are calculated for excluded facilities for 3 years (1986, 1987, and 1988) by facility type, region, urbanicity, ownership, and bed size. The distributions of profit rates are also examined across these years to further illustrate changes in profitability.
The second part of this article investigates several alternative reimbursement systems. The alternatives are limited to extensions of the current system and do not attempt to include a case-based PPS for psychiatric or rehabilitation care. Rather, changes in the boundaries of the current system are investigated. Nine basic models, including one incorporating only OBRA 1990 changes, are simulated on 1988 data. All address in one way or another the lack of government sharing in facility Medicare losses. The alternatives are described in detail later in the article.
TEFRA System
There are two generations of TEFRA that pertain to this study: the system that was in place during the years analyzed in this report (1986, 1987, and 1988); and the current system modified by OBRA 1990. The early TEFRA system is that outlined in section 101 of TEFRA and affects excluded hospitals and units after 1982 (Federal Register, 1990). In 1992, changes to the original TEFRA went into effect based on adjustments defined in OBRA 1990. The impact of these changes is not reflected in our cost report data that end in 1988. However, it is necessary to understand the current system because the simulations of alternative systems use the OBRA 1990 cost-sharing system as a baseline. That is, OBRA 1990 payment algorithms are simulated on 1988 costs to show how alternative sharing arrangements would have produced a different distribution of winners and losers.
The basic cost control mechanisms in TEFRA are referred to as target amounts. Target amounts represent a cost per discharge ceiling for Medicare patients of excluded facilities, calculated individually for each facility. This amount is based on facilities' average costs in their base year, trended forward each year based on an inflation factor. In general, a facility is reimbursed according to how their current average costs per Medicare discharge compare with their current target amount per discharge.
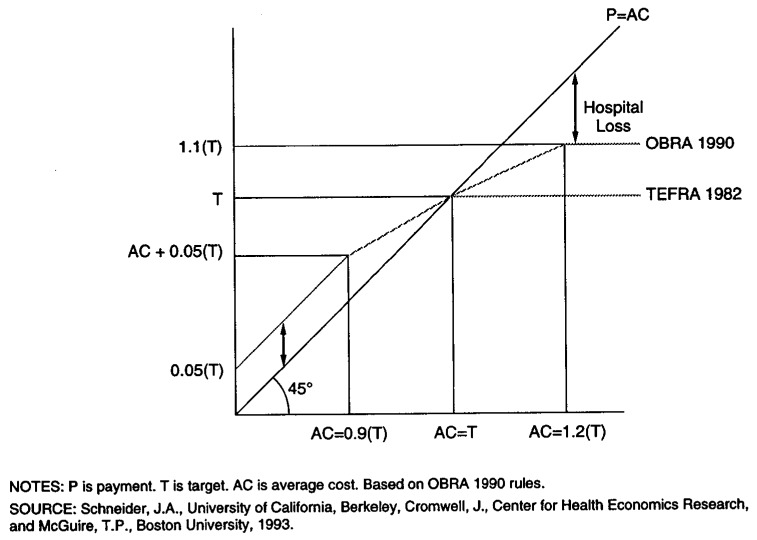
The original TEFRA (1982-91) made payments to hospitals based on the payment algorithms shown in Figure 1. If a facility's average costs (AC) in a given year were less than their target amount (T), the facility would be reimbursed their full average cost plus an incentive payment. The size of the incentive payment was set at 5 percent of the target amount if average costs were below 90 percent of the target. The size of the incentive payment was reduced to one-half the difference (between average costs and the target) if AC fell between 90 percent of the target and 100 percent of the target. Facilities with average costs above the target were reimbursed only the target amount; that is, there was no cost sharing in that range.
Figure 1. The Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 Versus the Omnibus Budget Reconciliation Act (OBRA) of 1990.
Under the OBRA 1990 provisions, one important change was made allowing some degree of cost sharing for facilities with average costs exceeding the target amount. The system reimburses the same way for facilities with AC less than the target. However, above the target, facilities are allowed to share some of their losses. Between 90 percent of the target and 120 percent of the target, facilities are reimbursed one-half the difference of AC and T. This creates a new effective ceiling, and payments cannot exceed 110 percent of the target amount.
One important methodological issue is the TEFRA system's exception policy. The Secretary of Health and Human Services is required by OBRA 1990 to provide a target amount exception to hospitals and distinct part units that can show that “events beyond the hospital's control, or extraordinary circumstances, including changes in case mix and volume,” have changed their cost structure significantly. This includes increases in wages as well as changes in applicable technology that increase costs. Records of requests for exceptions and decisions on exceptions are not automated. In addition, there is a lag time before an exception appears as an increased target amount or payment amount on the cost report. Thus, it is difficult to accurately account for exceptions when analyzing cost report data. In general, one can assume that the losses shown later are overstated where facilities have received retrospective adjustments, but by how much is unknown. Of more concern is the dynamic divergence of costs and payments among providers prior to adjustments. This suggests further restructuring in order to avoid turning TEFRA into an exceptions-based system.
Data
The primary sources of data for our analysis are the Medicare Cost Reports from PPS-excluded facilities for FYs 1986-88. The data base contains cost and utilization information for all excluded hospitals and excluded units within hospitals. The reports in this file are those with cost-reporting periods beginning on or after October 1, 1985 and before October 1, 1989. The types of PPS-exempt hospitals that are included are psychiatric, rehabilitation, long-term care, and children's. Also included are excluded rehabilitation and psychiatric distinct-part units of general hospitals. We did not include information for other types of excluded facilities because small sample sizes precluded statistically meaningful analysis. There are more than 5,000 records on the file, two-thirds of which are units of general hospitals.
The cost reports on this file contain information on costs and utilization that enable the Medicare program to determine reasonable costs and TEFRA payment amounts for each excluded facility. Cost data include inpatient routine, ancillary, and total operating costs (excluding capital). Utilization data include days and discharges. Cost and utilization data applicable to the Medicare program are provided separately. Also included on this file are TEFRA target and payment amounts.
Data from the American Hospital Association Annual Survey were merged with the file to enable the identification of hospital ownership, bed size, teaching status, occupancy rate, urban or rural location, and region. Data elements from the HCFA Impact Analysis Public Use file were also merged. These data provide information on hospital teaching status, disproportionate share status, and urban or rural location.
Before the file was analyzed, the data were extensively reviewed for missing elements, typographical errors, logical inconsistencies, and implausible data. Many of the problem cases were corrected after further review with HCFA staff. However, a number of cases were dropped from analysis either because of incomplete data or unreconcilable problems. Cases indicating a reporting period other than 12 months were deleted. These represented approximately 2.5 percent of all the hospitals and units in the file. Cases reporting no Medicare discharges were also deleted, rather than attempt to impute missing or zero discharge data.
The most extensive data cleaning effort was the examination of outliers, defined as the top and bottom 1 percent of cases in each provider type and year cell, based on a Medicare profit rate. Outlier target amounts, payments, and total margins (difference between payment and actual cost) were also used to identify possible problem cases. No systematic criterion for deleting outliers was imposed; rather, each case was examined individually. HCFA payment policy determination staff were consulted about the most grievous cases. A total of 26 hospitals and units (one-half of 1 percent) were deleted completely, and another 17 cases (one-third of 1 percent) had 1 or 2 years of data completely dropped.
It is conceivable that a portion of the cases marked for deletion were valid cases. For example, in the case of distinct part units of short-term acute care hospitals, incentives driven by PPS may have resulted in cost shifting to non-PPS units, thus potentially distorting the true financial status of the unit. While these are legitimate concerns, given the limitations of our data we were not able to distinguish cost-shifting behavior from other types of data quality issues.
Edited and cleaned data were divided into two analytic files. One file contained data for all hospitals and units; the other only for a cohort of facilities with data present in all 3 years. The cohort file contained 4,143 observations (1,381 each year). The cohort file was used to analyze financial impacts of TEFRA, and the complete file (5,291 observations) was used for payment system simulations. Note that as a result of deleting outliers and subsetting to facilities present in ail 3 years (in the case of the cohort file), the numbers of observations on our analytic files differ from the numbers presented in Table 1.
Financial Impact on Excluded Facilities
All data presented in this section are based on the cohort file, which only includes facilities reporting data for all 3 years. Unless specified differently on the tables, all of the statistics presented are weighted by Medicare discharges. Results for children's hospitals are de-emphasized because of their very small Medicare caseloads. Also, the small number of observations (28 on the cohort file) cause problems when analyzing facility characteristics, such as bed size groupings and regional groupings. Similar small sample problems apply to long-term care facilities, although results for these facilities are more important to HCFA because of their treatment of a relatively large number of Medicare patients. Profit rates per discharge are presented as the principal measure of financial status and are defined as the Medicare margin per discharge divided by Medicare average costs per discharge.
Across all types of facilities, Medicare profit rates were negative in every year—declining rapidly from −5.6 percent in 1986 to −10.8 percent in 1988 (data not shown). Different types of excluded facilities treat very different kinds of patients. Therefore, it is useful to examine each type of facility separately.
All four facility types had negative Medicare profit rates in each of the 3 years (Table 2). For psychiatric, children's, and long-term care facilities, profit rates ranged between −13 and −14 percent by 1988, versus rehabilitation facilities at −6.1 percent. Payments per case to rehabilitation facilities grew by 5.3 percent from 1986 to 1988, while average costs per case grew 7.5 percent during the time period. For other types of facilities, average costs grew nearly twice as fast as Medicare payments.
Table 2. Average Values for Measures of TEFRA Impact for a Cohort of Excluded Facilities, by Facility Type, 1986-88.
| Type of Facility and Impact Measures | 1986 | 1987 | 1988 | Percent Change 1986-88 |
|---|---|---|---|---|
| Psychiatric | ||||
| Average Cost per Case | $4,519 | $4,889 | $5,332 | 18.0 |
| Target Amount per Case | 4,376 | 4,547 | 4,765 | 8.9 |
| Medicare Payment per Case | 4,159 | 4,311 | 4,521 | 8.7 |
| Payment Margin per Case | −360 | −578 | −811 | −125.3 |
| Profit Rate per Case in Percent1 | −6.1 | −9.7 | −12.9 | −111.5 |
| Average Length of Stay2 | 19.0 | 19.1 | 18.9 | −0.5 |
| Medicare Dependency in Percent3 | 19.0 | 18.8 | 21.1 | 11.1 |
| Average Medicare Discharges | 173 | 176 | 185 | 6.9 |
| n = 927 | ||||
| Rehabilitation | ||||
| Average Cost per Case | $8,521 | $8,793 | $9,160 | 7.5 |
| Target Amount per Case | 8,562 | 8,773 | 9,084 | 6.1 |
| Medicare Payment per Case | 8,092 | 8,266 | 8,523 | 5.3 |
| Payment Margin per Case | −429 | −527 | −637 | −58.5 |
| Profit Rate per Case in Percent1 | −4.5 | −5.3 | −6.1 | −35.6 |
| Average Length of Stay2 | 23.9 | 23.4 | 22.3 | −6.7 |
| Medicare Dependency in Percent3 | 61.1 | 59.3 | 62.1 | 1.6 |
| Average Medicare Discharges | 201 | 215 | 226 | 12.4 |
| n = 384 | ||||
| Children's | ||||
| Average Cost per Case | $6,756 | $7,197 | $9,295 | 37.6 |
| Target Amount per Case | 7,700 | 8,062 | 8,431 | 9.5 |
| Medicare Payment per Case | 6,391 | 6,724 | 7,605 | 19.0 |
| Payment Margin per Case | −365 | −473 | −1,690 | −363 |
| Profit Rate per Case in Percent1 | −5.0 | −4.4 | −14.2 | −184 |
| Average Length of Stay2 | 6.9 | 6.5 | 6.9 | 0.0 |
| Medicare Dependency in Percent3 | 0.8 | 0.7 | 0.7 | −12.5 |
| Average Medicare Discharges | 71 | 65 | 66 | −7.0 |
| n = 28 | ||||
| Long-Term Care | ||||
| Average Cost per Case | $8,539 | $9,527 | $11,561 | 35.4 |
| Target Amount per Case | 8,769 | 9,035 | 10,217 | 16.5 |
| Medicare Payment per Case | 8,115 | 8,641 | 10,023 | 23.5 |
| Payment Margin per Case | −424 | −887 | −1,538 | −262.7 |
| Profit Rate per Case in Percent1 | −6.2 | −9.4 | −14.2 | −129 |
| Average Length of Stay2 | 27.1 | 28.8 | 33.0 | 21.8 |
| Medicare Dependency in Percent3 | 40.4 | 36.7 | 43.8 | 8.4 |
| Average Medicare Discharges | 275 | 266 | 290 | 5.5 |
| n = 42 |
Profit rate per case = (payment margin per case)/(average cost per case).
Average length of stay = (Medicare days)/(Medicare discharges).
Medicare dependency = (Medicare discharges)/(total discharges).
NOTES: TEFRA is Tax Equity and Fiscal Responsibility Act of 1982. Statistics shown are weighted averages based on Medicare discharges. Medicare dependency is weighted by total discharges.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Rehabilitation facilities were the only group to have reduced average length of stay. While they may have implemented other types of cost controls, their 6.7-percent decrease in average length of stay from 1986 to 1988 was likely an important factor in their slower than average increase in average costs.
Rehabilitation and long-term care facilities tend to have higher proportions of Medicare patients than children's and psychiatric facilities. In 1988, rehabilitation facility patients were 62 percent Medicare and long-term care facilities were 44 percent Medicare. It is likely that these types of facilities were more affected by the incentives of TEFRA reimbursement. Psychiatric facilities became slightly more dependent on Medicare, reaching 21.1 percent in 1988.
Financial Performance By Facility Characteristics
In order to determine if some categories of facilities were doing better or worse than others, we compared profit rates and costs by urbanicity, region, facility type, and bed size for psychiatric and rehabilitation facilities with enough observations. There were too few hospitals to enable separate analyses of facility characteristics between hospitals and units.
Psychiatric Facilities
Rural psychiatric facilities were worse off than their urban counterparts in all 3 years (Table 3). Although average costs for rural facilities were still much lower in 1988, they were increasing nearly three times faster than average payments, while urban average costs were rising at roughly twice the rate of urban payments (data not shown). The result was that rural psychiatric facilities had a profit rate of −19.3 percent by 1988. The gap between urban and rural average profit rates failed to converge during the time period. Rather, the gap worsened from 3.5 percentage points in 1986 to 7.1 percentage points in 1988.
Table 3. Average Medicare Profit Rates and Cost per Case, by Psychiatric and Rehabilitation Facility Characteristics: 1986-88.
| Facility Characteristic | Psychiatric | Rehabilitation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Medicare Average Profit Rate per Case | Medicare Cost per Case | Medicare Average Profit Rate per Case | Medicare Cost per Case | |||||||
|
|
|
|||||||||
| n | 1986 | 1987 | 1988 | 1988 | n | 1986 | 1987 | 1988 | 1988 | |
|
| ||||||||||
| Percent | Percent | |||||||||
| Overall | 927 | −6.1 | −9.7 | −12.9 | $5,332 | 384 | −4.5 | −5.3 | −6.1 | $9,103 |
| Rural | 143 | −9.3 | −15.1 | −19.3 | 4,215 | 31 | −13.7 | −11.8 | −14.3 | 7,396 |
| Urban | 781 | −5.8 | −9.1 | −12.2 | 5,453 | 353 | −4.0 | −4.9 | −5.7 | 9,253 |
| Region | ||||||||||
| New England | 53 | −12.9 | −18.7 | −20.4 | 7,330 | 17 | −4.2 | −5.9 | −8.4 | 9,519 |
| Middle Atlantic | 173 | −4.5 | −9.3 | −12.8 | 6,647 | 67 | −1.6 | −4.1 | −5.6 | 8,557 |
| South Atlantic | 157 | −7.8 | −12.2 | −15.8 | 4,897 | 36 | −7.1 | −11.6 | −14.4 | 9,713 |
| East North Central | 188 | −4.7 | −6.8 | −10.9 | 5,277 | 84 | −4.1 | −3.9 | −3.1 | 9,453 |
| East South Central | 40 | −5.8 | −7.3 | −10.8 | 4,189 | 9 | 0.7 | −2.5 | −2.7 | 8,426 |
| West North Central | 98 | −4.4 | −8.0 | −13.6 | 4,536 | 39 | −6.7 | −6.5 | −4.4 | 8,102 |
| West South Central | 73 | −6.0 | −10.0 | −11.6 | 5,118 | 29 | −6.7 | −6.4 | −13.6 | 7,772 |
| Mountain | 43 | −5.7 | −8.7 | −10.6 | 4,482 | 29 | −10.0 | −9.3 | −5.9 | 8,954 |
| Pacific | 102 | −8.1 | −11.2 | −11.3 | 4,999 | 74 | −6.7 | −4.2 | −3.6 | 11,555 |
| Facility Type | ||||||||||
| Units | 651 | −5.6 | −9.0 | −12.1 | 5,158 | 335 | −6.1 | −6.7 | −8.0 | 9,357 |
| Hospitals | 276 | −7.2 | −11.4 | −14.8 | 5,695 | 49 | −1.1 | −2.2 | −2.0 | 8,728 |
| Non-Profit | 158 | −8.9 | −14.5 | −18.6 | 5,891 | 44 | −0.1 | −1.1 | −1.3 | 8,838 |
| For-Profit | 118 | −4.7 | −6.8 | −9.0 | 5,433 | 5 | −9.7 | −13.6 | −7.5 | 7,950 |
| Medicare Discharges per Year | ||||||||||
| Less Than 49 | 100 | −9.7 | −12.4 | −16.7 | 6,930 | 31 | −15.1 | −25.6 | −22.0 | 14,408 |
| 49-83 | 149 | −9.1 | −12.4 | −17.0 | 5,662 | 66 | −10.2 | −12.5 | −17.0 | 11,821 |
| 84-144 | 247 | −10.4 | −12.0 | −16.8 | 5,303 | 84 | −9.0 | −9.7 | −10.8 | 10,540 |
| 145-239 | 229 | −6.9 | −12.3 | −14.1 | 5,174 | 102 | −6.6 | −6.5 | −10.5 | 9,627 |
| 240 or More | 202 | −3.6 | −7.1 | −10.6 | 5,339 | 101 | −1.8 | −3.0 | −2.8 | 8,490 |
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Psychiatric facility profit rates varied little by region. The one striking difference was New England facilities—in all 3 years they had much lower profit rates than other regions of the country. This may be due to the extraordinary wage increases in New England during the study years. For the entire United States, from 1986 to 1989, average payroll expenses for full-time equivalent employees of non-Federal psychiatric facilities increased 17.6 percent, nominally. During the same time period, average payroll expenses of psychiatric facilities in New England increased 25.3 percent (American Hospital Association, 1987, 1990, 1991). Such extraordinary increases in wages give New England the highest average costs of all regions in absolute terms for each year from 1986 to 1988.
Psychiatric units in general hospitals fared somewhat better than freestanding psychiatric hospitals. Among hospitals, non-profit institutions lost twice as much per Medicare case as their for-profit counterpart.
A strong positive relationship exists between the per case profitability and the number of discharges. Very small psychiatric facilities with fewer than 49 Medicare care discharges, for example, lost 16.7 percent per case in 1988 versus a 10.6-percent average loss in facilities discharging more than 239 cases. Average costliness per case is inversely related to volume, which explains the better financial performance of larger facilities.
Rehabilitation Facilities
Like psychiatric facilities, rehabilitation facilities in rural areas had lower average Medicare profit rates in all years—the gap narrowing by only 1 percentage point by 1988 (Table 3). Regional differences in general were not striking. The relative success of facilities located in the East South Central region is overshadowed by the small number of observations for that cell.
Unlike psychiatric facilities, rehabilitation units in general hospitals have done worse than freestanding rehabilitation hospitals, although profit rates for hospitals were falling faster. Units may have suffered from a slower percent increase in payments: 4.5 percent for units compared with 7.3 percent for hospitals. As previously mentioned, PPS-related incentives may have caused cost-shifting to units. This may be acceptable in terms of the overall management tactic of the hospital. Comparisons between non-profit and for-profit hospitals should be made with caution, given the small number of for-profit hospitals.
Profitability is even more strongly related to volume among rehabilitation facilities. Facilities with over 239 discharges lost only 2.8 percent per case in 1988 versus 22.0 percent in very small facilities. This is due to a 70-percent cost differential: $14,408 versus $8,490.
Distributional Trends in Financial Indicators
Distributional trends give a better understanding of the worsening financial performance of excluded facilities. Base-year target amounts under TEFRA are equal to base-year average costs; therefore we would expect profit rates to be clustered around zero in or around the base year. The design of the TEFRA system was intended to keep profit rates clustered around zero over time by allowing target amounts to grow by an inflation factor. Facilities faced with extraordinary circumstances could apply for a target exception. These two adjustment mechanisms were thought to be sufficient to prevent worsening overall Medicare profit rates. One very important question is whether, over time, the distribution of profit rates is becoming more dispersed as average costs increase faster than payments. A continual decrease in average profit rates was not an intentional result of the TEFRA system.
Profit rates for psychiatric and rehabilitation facilities did become very dispersed over time. The gap between the upper and lower 25th percentile widened considerably during the 3 years. In general, profit rates below the median deteriorated while those above the median remained relatively constant. A closer examination of systematic winners and losers will provide a better understanding of why the gap has widened.
Consistent Winners and Losers
The distributional findings imply that profit rates are not uniformly falling for all excluded facilities and that there is a cohort of facilities that are consistently winning or losing under TEFRA. Consistent TEFRA winners are defined as those facilities with average Medicare profit rates in the upper 33 percent in all 3 years of our study. Consistent TEFRA losers are defined as those facilities with average Medicare profit rates in the lower 33 percent in all 3 years. For psychiatric facilities, there were 133 consistent winners (14 percent) and 159 consistent losers (17 percent)(Table 4). Rehabilitation facilities had a slightly higher number of winners than losers—57 winners compared with 53 losers. Again, sample sizes were too small to include long-term care and children's hospitals in this part of the analysis.
Table 4. Trends in Selected Financial Impact Variables for Facilities That are Consistent Winners or Losers1: 1986-88.
| Facility Characteristic | Psychiatric (n = 927) | Rehabilitation (n = 384) | ||
|---|---|---|---|---|
|
|
|
|||
| Winners | Losers | Winners | Losers | |
| Number of Facilities | 133 | 159 | 57 | 53 |
| Percent of Facilities | 14.3 | 17.1 | 14.8 | 13.8 |
| Average Medicare Target Amount Per Case | ||||
| 1986 | $5,442 | $3,203 | $11,199 | $6,193 |
| 1987 | 5,728 | 3,337 | 11,348 | 6,342 |
| 1988 | 6,037 | 3,487 | 11,696 | 6,475 |
| Percent Change, 1986-88 | 10.9 | 8.9 | 4.4 | 4.5 |
| Average Medicare Cost Per Case | ||||
| 1986 | $4,198 | $4,721 | $9,085 | $8,329 |
| 1987 | 4,386 | 5,372 | 9,024 | 8,959 |
| 1988 | 4,764 | 5,980 | 9,270 | 9,694 |
| Percent Change, 1986-88 | 13.5 | 26.7 | 2.0 | 16.4 |
| Average Medicare Profit Per Case | Percent | |||
| 1986 | 6.4 | −28.3 | 5.6 | −25.2 |
| 1987 | 6.2 | −35.9 | 5.7 | −27.9 |
| 1988 | 5.3 | −40.1 | 5.7 | −31.8 |
| Percent Change, 1986-88 | −17.2 | −41.7 | 1.8 | −26.2 |
Winners and losers are defined according to facility type. Winners are those facilities with average Medicare profit rates in the highest 33 percent in all 3 years. Losers are those facilities having average Medicare profit rates in the lowest 33 percent in all 3 years.
NOTE: Means are weighted by Medicare discharges.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Perhaps the most interesting finding here is the large number of facilities consistently in the same fertile during the time period. The probability of falling into either the high or low group is 33 percent in any year, because the groups contain, by definition, one-third of the annual sample. The statistical chances of a facility randomly falling into the same group all 3 years is 3.6 percent (1/3 × 1/3 × 1/3 = .036), assuming an equal probability of selection each year. In practice, equal selection probabilities each year are unlikely because of the difficulty in changing cost structures significantly in the short run. Still, the number of facilities consistently winning or losing is roughly four times the expected number, implying that a larger than expected number of facilities are systematically benefiting from TEFRA, while another group (also unexpectedly large in number) is systematically losing ground under TEFRA.
Winners' profit rates decreased slower than those of losers. Winning rehabilitation facilities actually showed a slight increase in their average profit rate (Table 4). Losers' profit rates were the result of rapidly increasing average costs per case which failed to track target amounts. Rapidly rising average costs were most likely because of changes in case mix or extraordinary wage changes. In the case of psychiatric facilities, losers' average costs grew at a rate three times that of the target amount. Also remarkable are the large, systematic differences in target amounts between winners and losers.
Characteristics of Winners and Losers
Psychiatric Facilities
Psychiatric facilities located in rural areas are more likely to be consistent losers (Table 5). One-fourth of rural psychiatric facilities are consistent losers under TEFRA, while only 16 percent of urban facilities are losers. Among consistent winners, urban and rural areas shared the same percentage—14 percent. Variation by region was not striking; however, consistent with results presented earlier, New England had a disproportionate share of consistent losers (28 percent losers versus 6 percent winners). Joining New England was the South Atlantic region with 24 percent losers, although the South Atlantic region had a higher proportion of winners than New England (14 percent).
Table 5. Percentage of Facilities That are Consistent Winners or Losers,1 by Psychiatric and Rehabilitation Facility Characteristics: 1988.
| Facility Characteristic | Psychiatric | Rehabilitation | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Overall n | Winners | Losers | Overall n | Winners | Losers | |
|
| ||||||
| Percent | Percent | |||||
| Overall | 927 | 14.3 | 17.2 | 384 | 14.8 | 13.8 |
| Rural | 143 | 14.7 | 25.2 | 31 | 6.5 | 32.3 |
| Urban | 781 | 14.3 | 15.6 | 353 | 15.6 | 12.2 |
| Region | ||||||
| New England | 53 | 5.7 | 28.3 | 17 | 11.8 | 23.5 |
| Middle Atlantic | 173 | 6.9 | 11.0 | 67 | 13.4 | 3.0 |
| South Atlantic | 157 | 14.0 | 23.6 | 36 | 8.3 | 30.6 |
| East North Central | 188 | 18.6 | 14.4 | 84 | 20.2 | 13.1 |
| East South Central | 40 | 25.0 | 15.0 | 9 | 22.2 | 22.2 |
| West North Central | 98 | 16.3 | 17.3 | 39 | 17.9 | 7.7 |
| West South Central | 73 | 16.4 | 16.4 | 29 | 3.4 | 24.1 |
| Mountain | 43 | 18.6 | 13.9 | 29 | 20.7 | 20.7 |
| Pacific | 102 | 14.7 | 19.6 | 74 | 13.5 | 9.5 |
| Facility Type | ||||||
| Units | 651 | 12.3 | 14.9 | 335 | 13.4 | 14.0 |
| Hospitals | 276 | 19.2 | 22.5 | 49 | 24.5 | 12.2 |
| Non-Profit | 158 | 13.9 | 31.0 | 44 | 25.0 | 11.4 |
| For-Profit | 18 | 26.3 | 11.0 | 5 | 20.0 | 20.0 |
| Medicare Discharges per Year | ||||||
| Less Than 49 | 100 | 17.8 | 15.2 | 31 | 3.3 | 25.0 |
| 49-83 | 149 | 15.9 | 15.6 | 66 | 9.0 | 16.3 |
| 84-144 | 247 | 12.5 | 18.9 | 84 | 8.2 | 16.3 |
| 145-239 | 229 | 13.4 | 19.3 | 102 | 18.2 | 15.0 |
| 240 or More | 202 | 14.9 | 13.9 | 101 | 23.3 | 6.5 |
| Volume Change2 | ||||||
| Increase | 526 | 15.2 | 15.0 | 239 | 16.7 | 10.9 |
| Decrease | 321 | 15.0 | 19.3 | 113 | 11.5 | 22.1 |
| No Change | 80 | 6.3 | 22.5 | 32 | 12.5 | 6.3 |
| 1986 Target Amount3 | ||||||
| High | 232 | 25.4 | 7.3 | 96 | 29.2 | 3.1 |
| Medium | 463 | 13.4 | 13.4 | 192 | 1.0 | 16.7 |
| Low | 232 | 5.2 | 34.5 | 96 | 28.1 | 18.8 |
Winners and losers are defined according to facility type. Winners are those facilities with average Medicare profit rates in the highest 33 percent in all 3 years. Losers are those facilities having average Medicare profit rates in the lowest 33 percent in all 3 years.
Volume change is measured according to the percent change in Medicare discharges from 1986 to 1988. Increase = percent change in volume greater than 3 percent; decrease = negative percent change in volume greater than 3 percent; no change = percent change in volume between 3 percent and −3 percent.
1986 target amount ranges are based on quartiles. High = top 25 percent in 1986; medium = middle 50 percent in 1986; low = bottom 25 percent in 1986.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Whether a psychiatric facility wins or loses does not seem to depend on whether the facility is a hospital or a unit. An interesting finding, however, is that a larger proportion of hospitals are consistently either winning or losing. A total of about 42 percent of all psychiatric hospitals are consistently in the same profit rate tertile over the years. This contrasts to 27 percent for psychiatric units. It is likely that hospitals cannot adjust as quickly to changing conditions as units. Consistent with the findings presented on Table 3, for-profit hospitals are more likely to be winners and non-profit hospitals are more likely to be losers.
Facilities with greater numbers of discharges tend not to be consistent winners or losers. The notable exception is large rehabilitation facilities where more than 23 percent were consistently among the top one-third in terms of profitability while 6.5 percent consistently lost.
Volume changes during the time period may explain some of the differences between winners and losers.1 Both winners and losers were equally likely to have had volume increases; however, losers were more likely to have decreases in volume. It is difficult to determine the direction of causation; that is, are losers discharging (and admitting) fewer Medicare patients as a partial remedy to their Medicare financial status? Or are declining discharges a sign of another problem, such as declining market share?
Interestingly, the most robust difference between psychiatric facility winners and losers is in their target amounts. Winners were much more likely to have high target amounts in the top quartile in 1986. Losers were much more likely to have low target amounts in 1986. To further investigate this finding, we stratified average Medicare profit rates according to when facilities were TEFRA certified, which closely approximates their TEFRA base year. As expected, the earlier a facility was certified, the lower its target amount and average profit rate. This was true for both psychiatric and rehabilitation facilities and provides a further reason for rebasing costs for all facilities.
Rehabilitation Facilities
Some of the winner and loser characteristics described earlier are evident for rehabilitation facilities as well (Table 5). For instance, losers tended to be disproportionately rural and from New England and South Atlantic regions. Like psychiatric facilities, consistent winners and losers were spread evenly among units. The distribution of winners and losers across bed size was very similar to that of psychiatric facilities—larger facilities were more likely to be losers.
Some differences are notable. Rehabilitation hospitals are more likely to be winners. Among psychiatric facilities, hospitals are slightly less likely to be winners. Also unlike psychiatric facilities, nonprofit institutions were more likely to be winners, though interpretation is limited because of small sample sizes.
Rehabilitation facilities with increasing Medicare volume were more likely to be winners, whereas those with decreasing volume tended to be losers. Rehabilitation facilities with high 1986 target amounts were much more likely to be winners. Surprisingly, those with low 1986 target amounts were also more likely to be winners. Many of these facilities may have already changed volume prior to our time period, which would partly explain this result.
In summary, the financial picture of TEFRA facilities appears to be worsening over time. The distribution of average Medicare profit rates is becoming increasingly negative and more dispersed as facilities fail to keep average costs per discharge in line with target amounts. Reasons for this difficulty are not directly identifiable, although it is likely that changes in patient severity and area labor wages have contributed to changes in average costs that are not completely accounted for in target updates. Although our inability to completely account for target exceptions is likely to overestimate ultimate losses after adjustments, it is doubtful that the profit rate trends presented here are meaningfully affected. How can these trends be slowed without resulting in further program outlays? That is, how can the system be changed to spread the risk more equitably?
Simulations of Alternative Payment Systems
As the TEFRA payment year becomes more and more removed from the base year, average facility losses rise and become more variable. Concern over outdated base year target amounts has led to new interest in TEFRA reimbursement refinements. Modifications can vary along two dimensions: (1) the prospective method for setting the target amount; and (2) given the target amount, the retrospective cost sharing between Medicare and the facility.
Three Alternatives for Target Amounts
We simulated three approaches to setting target amounts on rebased costs, always maintaining budget neutrality, in the sense that Medicare outlays in the rebased year are unchanged.
Proportional Targets
In this simulation, the target amount is a constant proportion of facility average cost in the (rebased) base year. To assure budget neutrality with respect to HCFA outlays, target amounts are less than average cost in the rebased year because facility cost inflation exceeded target updates. The constant proportional (P) reduction used to set target amounts must be iteratively determined depending on the cost-sharing rule chosen. Proportional targets are evenhanded in the sense that all average costs are regarded as equally legitimate and then reduced proportionally.
Blended Targets
In this simulation, the target amount is a blend of rebased facility and national average costs. As with proportional targets, blended target amounts must be discounted to assure budget neutrality. A weighted average (50/50; 75/25) of each facility's rebased costs and the national average was constructed. Own-facility costs, in turn, were based on a 2-year average (1987-88) to minimize random year-to-year changes in base period costs. National average costs were also adjusted for each facility's area labor costs, using HCFA's 1988 hospital wage index file. The proportion of labor-related costs (.807) was based on the sum of wages, employee benefits, professional fees, business and computer services, etc., for TEFRA facilities (Federal Register, 1990). Blended targets allow a target amount well above rebased costs for low-cost facilities and below rebased costs for high-cost facilities.
Maximum Targets
In this simulation, the target amount is facility-rebased average cost subject to an upper limit. Each facility's target amount is set equal to its own average cost in the rebased year until it exceeds a uniform maximum target amount chosen iteratively to ensure budget neutrality. Establishing maximum targets is most beneficial for facilities in the middle range of costs, permitting recovery of full rebased costs until costs exceed a maximum.
Each approach to rescaling a facility's target after rebasing has its advantages and disadvantages. Proportional targets consider all costs as legitimate with each facility sharing equally percentage-wise in any redistributions. Blended targets reject the notion that low-cost facilities should share equally with high-cost facilities in any redistributions. By blending in a national rate with their own rate, then scaling targets to achieve payment neutrality, lower-cost facilities are less affected. One could argue that this is fairer in that they have better controlled their costs over time. Setting a maximum target on rebased costs is even more stringent on high-cost facilities. It assumes that all costs above the maximum are illegitimate. No one knows, of course, how much of a facility's costs are legitimate, or how efficient it is. These three approaches to setting targets, we believe, give policymakers options ranging from a very generous to a very strict interpretation of the legitimacy of high-cost outliers.
Three Alternatives for Cost Sharing
Target amounts prospectively limit Medicare outlays during the rate year. Unforeseen random shocks may occur, however, that could result in excessive or inadequate payments to particular facilities. To address this problem, three methods of retrospective HCFA-facility cost sharing were simulated (Figure 2).
Figure 2. Three Alternatives for the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 Cost Sharing.
OBRA 1990
This is the current cost-sharing arrangement and is indicated by line X (or ABCDFX) in Figure 2. If actual average cost at the end of the period is at or below 90 percent of the target amount, 0.9T, the facility receives actual average cost plus 5 percent of the target. There is a range of 50/50 cost sharing from 90 percent of the target to 120 percent (1.2T) of the target. Payment per case effectively is limited to 110 percent of the target amount.
Enhanced TEFRA
We gave the name enhanced TEFRA to alternative Y or line ABCEFGY. Cost sharing at or below the target is the same as OBRA 1990. In contrast to OBRA 1990, a facility is held to the target amount if average cost is at the target amount or above, up to 110 percent (1.1T) of the target amount (range CE), much like the PPS for acute hospitals. For average costs above 110 percent of the target amount, Medicare is assumed to share continuously 50/50 in the excess, without limit.
Limited Enhanced TEFRA
Option Z (or line ABCEFGZ) is the same as enhanced TEFRA except that Medicare cost sharing is limited (arbitrarily) to 150 percent of the target amount. Maximum payment per discharge is limited, therefore, to 120 percent of the target.
These three cost-sharing options differ most for facilities with costs in excess of 150 percent of their own target amount. Under OBRA 1990, Medicare marginal revenue is zero for facilities with costs above 1.2T; under enhanced TEFRA, marginal revenue is zero between 1.0 and 1.1T and 50 percent after 1.1T; and under limited enhanced TEFRA, marginal revenue is zero again after 1.5T.
Like the range of methods for setting prospective target amounts, we simulate a second range for settling payments retrospectively. The more one considers cost deviations above targets to be illegitimate, the less cost sharing would be recommended. OBRA 1990 is least generous, and enhanced TEFRA with unlimited 50/50 cost sharing is most generous. As before, we do not know what proportion of costs in excess of targets are unnecessary, if any, in a given institution. Policymakers must review the likely impacts of alternative sharing arrangements, shown later, and decide on a fair method.
Initial Simulations
Tables 6 and 7 for psychiatric and rehabilitation facilities, respectively, illustrate the simulated impacts of three ways of rebasing target amounts, interacted with three different cost-sharing payment methods. (Results for the other two facility types are available upon request from the authors.) The first three rows of each table report results after rebasing individual facility targets and applying the alternative cost-sharing schemes. All facility targets have been rebased using a 2-year average (1987-88) of per discharge costs in order to smooth out year-to-year fluctuations. They are then made budget neutral according to the rebased target method. The bottom row reports simulation results using actual, single year, 1988 (non-rebased) target amounts along with the current, more generous, OBRA 1990 cost-sharing rules. As such, these figures constitute the baseline for all other comparisons.
Table 6. Comparison of Ten Simulated Payment Schemes: Psychiatric Facilities.
| Rebased Target Method | Cost-Sharing Arrangement | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OBRA 1990 | Enhanced TEFRA With 50 Percent Sharing Above 110 Percent of Target | Limited Enhanced TEFRA With Maximum Payment = 120 Percent of Target | ||||||||||
|
|
|
|
||||||||||
| Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | ||||
|
|
|
|
||||||||||
| T10 | B10 | T10 | B10 | T10 | B10 | |||||||
|
| ||||||||||||
| Percent | ||||||||||||
| Proportional Targets | −10.8 | −3.2 | −20.8 | 79.4 | −9.4 | 0.1 | −15.4 | 92.1 | −9.5 | 0.1 | −15.4 | 86.1 |
| Blended (50/50) Targets | −5.8 | 6.3 | −23.6 | 55.9 | −6.2 | 6.3 | −21.6 | 84.7 | −6.5 | 6.3 | −18.7 | 60.9 |
| Maximum Targets | −5.3 | 4.5 | −21.9 | 20.3 | −6.9 | 4.3 | −21.0 | 75.8 | −7.2 | 4.4 | −19.8 | 20.6 |
| Non-Rebased Actual 1988 Targets | −9.0 | 6.3 | −34.4 | 67.8 | — | — | — | — | — | — | — | — |
NOTES: OBRA 1990 is Omnibus Budget Reconciliation Act of 1990. TEFRA is Tax Equity and Fiscal Responsibility Act of 1982. Average margin is weighted average TEFRA facility margin; T10 is top 10 percent threshold; B10 is bottom 10 percent threshold; R-squared is percent of cost variation explained by payment system. Proportional targets: Uniform percent reduction in all facility targets derived from 2-year (1987 and 1988) average costs. Blended (50/50) Targets: Facility target based on 50/50 weighting of own 2 year (1987 and 1988) average costs per Medicare discharge and national average cost, adjusted for local wage differences. Maximum targets: Target set equal to a 2-year own-facility average costs up to a maximum.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Table 7. Comparison of Ten Simulated Payment Schemes: Rehabilitation Facilities.
| Rebased Target Method | Cost-Sharing Arrangement | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OBRA 1990 | Enhanced TEFRA With 50 Percent Sharing Above 110 Percent of Target | Limited Enhanced TEFRA With Maximum Payment = 120 Percent of Target | ||||||||||
|
|
|
|
||||||||||
| Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | ||||
|
|
|
|
||||||||||
| T10 | B10 | T10 | B10 | T10 | B10 | |||||||
|
| ||||||||||||
| Percent | ||||||||||||
| Proportional Targets | −2.9 | 2.7 | −8.1 | 98.3 | −0.7 | 6.3 | −14.5 | 78.8 | −2.1 | 5.5 | −14.9 | 32.4 |
| Blended (50/50) Targets | −4.0 | 3.7 | −11.5 | 92.1 | −0.8 | 6.5 | −14.3 | 90.0 | −2.8 | 5.5 | −14.9 | 79.1 |
| Maximum Targets | −4.0 | 3.7 | −11.5 | 86.1 | −0.8 | 6.5 | −14.3 | 84.4 | −2.7 | 5.5 | −13.4 | 40.4 |
| Non-Rebased Actual 1988 Targets | −2.9 | 6.3 | −25.2 | 88.6 | — | — | — | — | — | — | — | — |
NOTES: OBRA 1990 is Omnibus Budget Reconciliation Act of 1990. TEFRA Is Tax Equity and Fiscal Responsibility Act of 1982. Average margin is weighted average TEFRA facility margin; T10 is top 10 percent threshold; B10 is bottom 10 percent threshold; R-squared is percent of cost variation explained by payment system. Proportional targets: Uniform percent reduction in all facility targets derived from 2 year (1987 and 1988) average costs. Blended (50/50) Targets: Facility target based on 50/50 weighting of own 2 year (1987 and 1988) average costs per Medicare discharge and national average cost, adjusted for local wage differences. Maximum targets: Target set equal to a 2-year own-facility average costs up to a maximum.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files; 1986-88.
The OBRA 1990 columns are interpreted as the effects of retrospectively applying OBRA 1990 revised payment methods to 1988 actual, unadjusted, facility costs under three alternative ways of rebasing targets plus the original method (in bottom row). The second set of columns reports results for the enhanced TEFRA system that allows for continuous sharing of losses (50/50) beyond a 110-percent corridor. The third set of columns shows the impact of applying an upper limit of 150 percent to Federal cost sharing, i.e., limited enhanced TEFRA.
If OBRA 1990 payment methods had been applied to 1988 actual target amounts, the average psychiatric case would have lost 9 percent in 1988 (Table 6). Although negative, this 9 percent loss is still nearly 4 percentage points better than facilities actually experienced under the TEFRA payment system in existence in 1988 without any cost-sharing above the target amount (Table 3). The improvement is clearly due to a greater sharing of losses within 120 percent of the target amount.
Compared with this 9 percent loss, the average case would have lost 10.8 percent if target amounts had been rebased to average 1987-88 costs then proportionally constrained to total outlays for 1988. This slight difference is due to the fact that the rebased proportional targets were based on each facility's 2-year average costs and not 1988 costs alone.
Psychiatric facilities on average would have done much better under OBRA 1990 if 50/50 blended or maximum targets were used instead of a proportional reduction in all rebased costs. Losses per case would have averaged only 5.3 to 5.8 percent. This is true even though the same payment system (OBRA 1990) is being used to allocate the same, budget neutral, total Medicare outlays for 1988. Average profits improve because of the inverse correlation of costs and facility size (as measured by the number of Medicare discharges). That is, blended or maximum target approaches re-allocate more payments away from smaller, high-cost facilities to larger, lower-cost facilities, as compared with a proportional rebasing of payments that takes a constant percentage from all facilities. This re-allocation greatly improves the discharge-weighted average margin of the industry as a whole.
Distributional effects under OBRA 1990 show substantial improvement in the bottom 10 percent using blended or maximum targets versus actual 1988 targets, but at the cost of a lower R2. A simple proportional reduction in a facility's rebased target amount produces payments under OBRA 1990 that most closely correlate with actual 1988 costs (79.4 percent). The top and bottom 10 percent, however, imply losses for nearly all facilities (note that the top 10 percent threshold is negative) as targets are proportionally reduced and the redistribution burden is shared by all facilities. At the other extreme, applying maximum target limits produces payments that correlate only 0.20 with the variation in costs. This is due to very large losses among high-cost facilities.
Under enhanced TEFRA, where losses are shared equally beyond 110 percent of a facility's target, average losses per psychiatric case would be slightly lower under proportional targets than with constrained cost sharing (−9.4 versus −10.8 percent). More importantly, payments would track costs far better than under OBRA 1990 rules (compare R2 for enhanced and limited enhanced TEFRAs). The bottom decile threshold for losing facilities also would improve to −15.4 percent. Applying a cost-sharing cap on high cost facilities (limited enhanced TEFRA) produces very similar results to those when no limit is applied to the cost sharing, especially using 50/50 blended targets.
Simulation results for rehabilitation facilities (Table 7) are similar to those shown in Table 6 across the payment schemes, although average losses are not as great. Compared with the inequalities in margins using non-rebased actual targets, the distribution of rehabilitation margins is compressed using any of the alternative target methods. Interestingly, a 50/50 blended target under OBRA 1990 rules would produce a greater average loss (4.0 percent) than would the use of actual targets. This appears to be due to lower positive profits on the part of some facilities. Blended targets produce a smaller average loss under greater sharing arrangements.
These results support a blended target approach to rebasing. Payments correlate nearly as well (and sometimes better) with costs without rebasing and produce fewer big losers. Proportional targets would produce much larger cross-subsidies of high-cost by low-cost facilities, resulting in practically no winners. Maximum targets appear too draconian unless some form of continuous sharing is applied.
Further Simulations
Results from Tables 6 and 7 encouraged us to focus on a 50/50 blended target approach with further modifications in the cost-sharing arrangement for high-cost outliers:
The enhanced TEFRA cost-sharing scheme was further modified to begin 50/50 sharing only after costs exceeded 120 percent of the target amount instead of 110 percent.
The limited enhanced TEFRA cost-sharing scheme was further modified to continue 25 percent sharing above 150 percent of the target amount.
Widening the non-sharing corridor from 110 percent to 120 percent of the target redistributes extra payments away from facilities within 110 percent and 120 percent of the target to facilities where costs are either below or well above their targets. Alternatively, continuing 25 percent sharing beyond 150 percent of the blended target will redistribute more payments from winners (or smaller losers) to big, high-cost losers.
The effects of these refinements are shown in Table 8 for all four TEFRA facility types. The table now shows the top and bottom 5 percent thresholds for the modified sharing arrangements to better indicate extreme outlier impacts. The results of applying OBRA 1990 sharing rules using blended targets are shown in the first set of columns for comparison. In general, these modified cost-sharing arrangements produce similar average profit rates and thresholds, implying little overall difference between the existing OBRA 1990 system with a blended prospective target and systems with even greater retrospective cost sharing. Marked differences still exist (as shown for psychiatric facilities) between current OBRA 1990 using actual 1988 targets (with average profits of −9 percent) and any method with greater cost sharing. More limited (25 percent) cost sharing after costs exceed 150 percent of a facility's target produces almost identifical average profit rates with slight reductions in the bottom 5 percent threshold (suggesting slightly fewer facilities with very large losses). Average losses clearly vary by facility type, with rehabilitation facilities faring best and children's hospitals faring worst.
Table 8. Comparison of Modified Cost-Sharing Payment Arrangements Using a 50/50 Percent Blended Target.
| Rebased Target Method | Cost-Sharing Arrangement | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OBRA 1990 With 50/50 Percent Blended Target | Enhanced TEFRA With 50 Percent Sharing Above 120 Percent of Target | Limited Enhanced TEFRA With 50 Percent Sharing Between 110-150 Percent; 25 Percent Sharing Thereafter | ||||||||||
|
| ||||||||||||
| Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | Average Margin | Threshold | R2 | ||||
|
|
|
|
||||||||||
| T5 | B5 | T5 | B5 | T5 | B5 | |||||||
|
| ||||||||||||
| Percent | ||||||||||||
| Psychiatric (n = 1,083) |
−5.8 | 6.3 | −23.6 | 56 | −5.7 | 6.9 | −23.7 | 84 | −5.9 | 6.7 | −22.4 | 75 |
| Rehabilitation (n = 475) |
−0.7 | 6.3 | −14.5 | 79 | −1.4 | 7.0 | −20.5 | 87 | −0.9 | 7.0 | −16.8 | 88 |
| Children's (n = 30) |
−10.4 | 8.2 | −34.9 | 57 | −11.8 | 13.4 | −28.5 | 75 | −12.3 | 12.7 | −32.9 | 73 |
| Long-Term care (n = 47) |
−2.2 | 11.8 | −33.5 | 54 | −3.4 | 15.7 | −33.0 | 83 | −3.8 | 15.4 | −40.7 | −73 |
NOTES: OBRA 1990 is Omnibus Budget Reconciliation Act of 1990. TEFRA is Tax Equity and Fiscal Responsibility Act of 1982. Average margin is weighted average TEFRA facility margin; T5 is top 5 percent threshold; B5 is bottom 5 percent threshold; R-squared is percent of cost variation explained by payment system. Proportional targets: Uniform percent reduction in all facility targets derived from 2-year (1987 and 1988) average costs. Blended (50/50) Targets: Facility target based on 50/50 weighting of own 2 year (1987 and 1988) average costs per Medicare discharge and national average cost, adjusted for local wage differences. Maximum targets: Target set equal to a 2-year own-facility average costs up to a maximum.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Effects by Facility Characteristic
Table 9 decomposes the effects of the limited enhanced TEFRA cost-sharing option, modified by reducing Federal cost sharing to 25 percent beyond 150 percent of the target amount. Profit rates, even with extensive sharing, would still differ systematically by urban or rural location for psychiatric facilities, although both areas would enjoy significant improvements compared with the −19 to −23 percent rates shown in Table 3. Smaller psychiatric and rehabilitation facilities would also incur higher average losses as do facilities in New England and Mid-Atlantic States. Small facilities would continue to experience greater losses, but the greater average losses in large facilities shown in Table 3 disappear.
Table 9. Simulated Profits, by Facility Characteristic, Using 50/50 Percent Blended Target1, 50 Percent Cost Sharing Between 110-150 Percent, and 25 Percent Cost Sharing Thereafter.
| Facility Characteristic | Psychiatric | Rehabilitation | ||
|---|---|---|---|---|
|
|
|
|||
| n | Average Profit Rate | n | Average Profit Rate | |
|
| ||||
| Percent | Percent | |||
| Rural | 171 | −4.0 | 38 | −2.8 |
| Urban | 907 | −7.1 | 436 | −3.0 |
| Ownership | ||||
| For-Profit | 224 | −7.2 | 38 | −2.9 |
| Non-Profit | 859 | −6.4 | 437 | −3.0 |
| Region | ||||
| New England | 94 | −11.0 | 22 | −7.5 |
| Middle Atlantic | 182 | −8.7 | 77 | −0.4 |
| South Atlantic | 185 | −7.3 | 50 | −7.4 |
| East North Central | 205 | −6.9 | 99 | −3.3 |
| East South Central | 54 | −3.2 | 18 | −2.1 |
| West North Central | 110 | −4.8 | 46 | −0.6 |
| West South Central | 87 | −7.5 | 42 | −2.4 |
| Mountain | 54 | −4.5 | 39 | −2.0 |
| Pacific | 112 | −1.0 | 82 | −3.6 |
| 1988 Medicare Discharges2 | ||||
| Small | 277 | −8.7 | 122 | −7.2 |
| Medium | 534 | −5.9 | 234 | −2.9 |
| Large | 272 | −5.7 | 119 | −1.1 |
Blend: 50/50 percent facility target based on 50/50 weighting of own 1987 and 1988 average costs per Medicare discharge and national average cost.
Small = smallest 25 percent of facilities; medium = median 50 percent of facilities; large = largest 25 percent of facilities.
SOURCE: Health Care Financing Administration: PPS-Exempt Hospitals and Excluded Units files, 1986-88.
Policy Recommendations
Setting Target Amounts and Cost-Sharing Parameters
The current OBRA 1990 payment system for excluded facilities has a very limited cost-sharing option. It is also based on outdated 1982-83 cost-based target amounts. It is important that the system be rebased periodically to better reflect the true cost of care within different facilities. Based on our theoretical and empirical research, we are recommending a modified OBRA 1990 payment system that rebases each facility's target amount using a 50/50 blend of its own costs and those of its peers. A blended rate forces facilities to compete, to some extent, with their peers. It also allows low-cost facilities to earn significant profits in the first year and allows HCFA to emphasize its interest in maintaining efficient payments and rewarding low-cost facilities. Peer group costs would be a weighted national average of facility Medicare costs per discharge adjusted by the local HCFA hospital wage index.
Three parameters control the degree of retrospective cost sharing. First, policy-makers must set the width of the non-sharing corridor, if any. In many of our simulations, in contrast to OBRA 1990, no sharing took place if costs ranged from 1.1 to 1.2 times the target amount. Consistent with the PPS outlier corridors, this discourages facilities from raising costs by relatively minor amounts to maximize reimbursement. The no-sharing corridor could extend further or, conversely, be eliminated entirely (as under OBRA 1990) and have cost sharing run continuously from 90 percent of the target upward. Second, the sharing proportion must be set. In all our simulations, a 50/50 percent sharing was used, which has prima facie validity, as the government and the provider share equally in short-run costs above the target amount. And third, policymakers have the option of either setting a limit on government cost sharing or reducing the cost-sharing percentage at very high cost levels (or possibly both, although this option was not simulated). Our simulations either set a ceiling on cost sharing at 150 percent of the target amount or reduced the continuous sharing rate from 50 percent to 25 percent at 150 percent of the target. Statistically, there was little to choose between the two. Least disruptive would be to modify the OBRA 1990 rules as little as possible by extending 50 percent cost sharing to 150 percent of the target with no sharing thereafter. The limited sharing up to 120 percent of a facility's target allowed under OBRA 1990 seems too restrictive, given the wide observed swings in yearly costs.
Several potential advantages accrue to a broader retrospective sharing of costs by the government. Greater cost sharing reduces selection bias effects. If facilities lose too much on Medicare patients, they may begin to refuse to accept them, which limits access. Greater cost sharing may also be more equitable if more costly facilities treat a more difficult case mix, either by random luck in a particular year or if their case mix becomes systematically more costly after the rebased target amounts have been set.
A fundamental difference should be noted between our simulated results and the way the system would actually work. Target amounts would be adjusted to be budget neutral in the rebased year, but actual cost sharing would not necessarily be budget neutral at the end of the first rate period, as was implicitly the case in all of our simulations. A system with cost sharing is fundamentally different than Medicare's PPS, which is blind to cost increases above the update factor. Although in future years the TEFRA target amount would not be a function of future costs, rooted as it is in the rebased year (except for minor updates for input prices), final payments would continue to depend on incurred costs. Facilities with costs consistently above the updated target would receive consistently higher payments than implied by their target. This may be appropriate in some cases where the facility faces an underlying source of cost increase beyond its control. It may be inappropriate in other cases where facilities attempt to shift costs to maximize Medicare reimbursement. For this reason, HCFA should be conservative in its cost-sharing arrangement.
For-Profit Facilities Using Blended Targets
Psychiatric inpatient coverage is limited under the Medicare program. Once a patient exhausts his or her 190 days, remaining institutional days go uncovered. For-profit psychiatric facilities generally treat Medicare patients until their coverage runs out and then transfer them to public facilities. Thus, the former might show much higher average covered costs per discharge. So long as target amounts are based on a facility's own base period costs, as in current TEFRA, ownership introduces no payment biases, but we are recommending a blended target amount based on national average as well as own-facility costs. For-profit hospitals could have a lower blended target versus their current target to the extent that their high covered-day (and cost) proportion is not completely reflected in the national average that includes public hospitals. While this issue needs further consideration if blended targets and budget neutrality are imposed during a rebasing, our proposed cost-sharing methodology addresses most of the problem. If proprietary facilities were disproportionately constrained by the rebased target amount, their losses would be partially shared by winning public hospitals through the cost-sharing mechanism (up to a limit).
Rebasing Using Multiple Year Costs
Clearly, TEFRA target amounts must be rebased. Rebasing should be done using more than a single year's cost information in order to smooth out short-run discontinuities in facility cost and patient patterns. We used 1987 and 1988, but 3 years might be better. Two years, on the other hand, avoids working with outdated costs. HCFA should use the most current years from the cost reports. Lags in these reports will necessitate the usual update through the first rate year.
Rebasing with Budget Neutrality
Unless rebasing target amounts is done within an overall budget neutrality cap, Medicare payments to excluded facilities would rise significantly. Presuming Medicare budget neutrality would be maintained in the rebased year, this requires iterating on the target amounts to be consistent with the selected mode of cost sharing. Our simulations generally required 5 to 10 iterations before budget neutrality was achieved within each of the 4 provider types.
Rebasing Old Versus New Facilities
A systematic, inverse relation exists between the length of time a facility has been in the TEFRA program and its Medicare profit rate. Recently certified facilities start with their own average costs as target amounts instead of being constrained to an outdated target amount that has been slowly updated over several years. Rebasing all target amounts, then applying budget neutrality in prorating all targets, addresses this inequity. All facilities within a group would have their blended targets updated to full costs in the first iteration. Then, all targets and payments would be prorated downwards to insure budget neutrality in the rebased year. The net effect would be to disproportionately increase the target amounts and payments to older facilities.
Updating Target Amounts
Target amounts would be fixed as of the rebased year and then updated using the HCFA market basket index of input prices and excluded-facility cost weights. Applying the PPS update factor to excluded hospitals was mistaken because it included a downward adjustment for excess profits in short-term general hospitals. TEFRA hospital profits have always been severely constrained by the retrospective profit-sharing provision, which was absent in PPS, and excluded facility updates should not have included the “market basket minus” feature.
A potentially serious limitation of inflating target amounts by a national PPS update factor is that it fails to reflect case-mix or local changes in operating costs. The cost-sharing provisions are meant to adjust for these problems in the short run. Nevertheless, target amounts can rapidly become irrelevant if significant case-mix or area wage changes have taken place. Thus, target amounts should be adjusted periodically for new values of the HCFA wage index, and HCFA should also continue to pursue case-mix adjustments. A modified DRG payment system may be feasible for some excluded facilities, or target amounts could be rebased regularly after adjusting average facility costs for some index of case-mix severity.
Eliminating the Exceptions Process
HCFA has continued to support a burdensome exceptions process for TEFRA facilities. We are recommending that it be eliminated. Its purpose is to adjust target amounts and payments for cost-increasing factors outside the facility's control. This is necessary under an old TEFRA system that shared in facility profits but in none of the losses. Once targets are rebased and updated using the full market basket index and the cost-sharing corridor is extended, the need to grant further exceptions is unnecessary. HCFA can set the width of the sharing corridor and possibly extend sharing at a lower percentage to eliminate any need for unique exceptions.
Acknowledgments
This research was funded by the Health Care Financing Administration (HCFA) under Cooperative Agreement Number 99-C-98526/1-08 to the Health Policy Consortium (Boston University, the Center for Health Economics Research, and The Urban Institute). John E. Schneider was with the Center for Health Economics Research when this research was completed; he is now with the Department of Health Services and Policy Analysis, University of California, Berkeley. Jerry Cromwell is with the Center for Health Economics Research. Thomas P. McGuire is with the Department of Economics, Boston University. The views and opinions expressed are those of the authors and do not necessarily reflect the opinions of HCFA, the Health Policy Consortium, or any of its sponsors.
Footnotes
A volume “increase” is equal to a percent change (from 1986 to 1988) in volume greater than 3 percent; a “decrease” is a negative percent change in volume greater than −3 percent; and “no change” in volume is a percent change in volume between +3 and −3 percent.
Reprint requests: Jerry Cromwell, Ph.D., Center for Health Economics Research, 300 Fifth Avenue, Waltham, Massachusetts 02154.
References
- American Hospital Association. Hospital Statistics. 1987, 1990 and 1991. Chicago: 1987, 1990, and 1991. [Google Scholar]
- Cromwell J, Harrow B, McGuire TP, et al. TEFRA Psychiatric Hospital and Unit Peer Group and Case Outlier Analyses. Waltham, MA.: Health Economics Research, Inc.; Jan, 1990. HHS Contract Number 100-88-0037, DHHS/ASPE. Prepared for the Health Care Financing Administration. [Google Scholar]
- Federal Register: Rules and Regulations. No. 171. Vol. 55. Washington: U.S. Government Printing Office; Sep 4, 1990. Office of the Federal Register. National Archives and Records Administration. [Google Scholar]
- Harrow B, Cromwell J. Impact Analysis of the TEFRA System for Reimbursement of PPS-Excluded Hospitals. Waltham, MA.: Center for Health Economics Research; Apr, 1990. Cooperative Agreement Number 99-C-98526/1-06. Prepared for the Health Care Financing Administration. [Google Scholar]
- Langenbrunner JC, Willis P, Jencks SF, et al. Developing Payment Refinements and Reforms Under Medicare for Excluded Hospitals. Health Care Financing Review. 1989 Spring;10(3):91–108. [PMC free article] [PubMed] [Google Scholar]
- Prospective Payment Assessment Commission. Medicare and The American Health Care System: Report to Congress. Washington, DC.: Jun, 1991. Jun, 1992. [Google Scholar]