Abstract
In this article, a payment model is developed for a hospital system with both acute- and chronic-stay psychiatric patients. “Transition pricing” provides a balance between the incentives of an episode-based system and the necessity of per diem long-term payments. Payment is dependent on two new psychiatric resident classification systems for short- and long-term stays. Data on per diem cost of inpatient care, by day of stay, was computed from a sample of 2,968 patients from 100 psychiatric units in 51 Department of Veterans Affairs (VA) Medical Centers. Using a 9-month cohort of all VA psychiatric discharges nationwide (79,337 with non-chronic stays), profits and losses were simulated.
Introduction
The implementation of the prospective payment system (PPS) for Medicare patients in acute care hospitals on October 1, 1983, represented a major change in the policy and technology of paying for-medical care in the United States. No longer were facilities reimbursed based solely on historic costs, but rather saw in their new payments a direct link to the types of patients they treated and thereby the resources involved in that care. However, at its inception, psychiatric hospitals and “distinct part” units of general hospitals (along with rehabilitation units and a few others) were given the option of being exempted from PPS (Widem et al., 1984). A major reason for the exemption was concern about the application of a case-mix measure, central to the PPS methodology; in psychiatric care, there was a poor correlation between diagnosis and resource use (Lee and Forthofer, 1983; Taube, Lee, and Forthofer, 1984a, 1984b; Taube et al., 1985; Goldman et al., 1984; Jencks, Goldman, and McGuire, 1985; Frank and Lave, 1985a, 1985b). In particular, the PPS method of measuring case mix—diagnosis-related groups (DRGs) (Fetter et al., 1980; Federal Register, 1991)—appears less predictive of length of stay (LOS), resource use, and clinical treatment patterns for psychiatric patients than for their medical or surgical counterparts (English et al., 1986; Ashcraft et al., 1989; Rupp, Steinwachs, and Salkever, 1984). A likely explanation is that the DRGs amassed all psychiatric diagnoses in a single group.
During this same period, the VA (the former Veterans Administration) implemented the Resource Allocation Methodology (RAM) system for funding hospitals based on DRGs (Rosenheck, Massari, and Astrachan, 1990). Psychiatric care was not excluded from the RAM system, as it was from Medicare PPS. In the following discussions, however, we have not made any distinction between the design of payment and of allocation systems, as none needs to be made.1
In 1990, after concerns were raised with regard to potential inequities in the system, the VA RAM was suspended. Behind this action were concerns about the built-in incentives for inappropriate admissions and volume in a system without adequate safeguards, the lack of links to quality of patient care, and the inadequacies of using an acute care classification model for the growing long-term care population to which the VA has a special commitment. Payment for long-term psychiatric care was one factor that led to the dismantling of RAM. Development work on a revised system was authorized to include consideration of classification systems to be employed (Horgan and Jencks, 1987).
We describe here the design of a unified short- and long-stay payment system for psychiatric inpatient care that is applicable to both the VA and non-VA settings. This payment system addresses some unique properties of inpatient psychiatric care, including care for substance abuse. It recognizes that psychiatric care involves both short-term acute care patients and long-term patients with hospital stays that at times exceed several decades. For short-term patients, we employ a new patient classification system that we have shown to be significantly superior to DRGs in explaining episode costs (Ashcraft et al., 1989). For long-term patients, we use a second new classification system that predicts per diem resource use (Fries et al., 1990). These two classification systems are then balanced in a prototype payment model that provides incentives for discharge of acute care patients, yet also finances chronic care appropriately.
Background
Much of the impact that DRGs have had on the health care system has resulted from PPS and the policy of paying facilities a fixed price for an inpatient episode of a particular type of patient, regardless of how long that patient stays or the resources that patient actually uses. This payment model removes the previous incentives that hospitals had to retain patients and thereby accumulate revenue in excess of their cost, especially at the end of a stay. On the other hand, PPS creates incentives to discharge patients as early as possible, and there is now controversy about whether there are too many premature discharges (McCarthy, 1988; Vladeck, 1988). Such changes have been documented by DesHarnais, Wroblewski, and Schumacher (1990) for psychiatric patients who were or were not exempted from PPS.
A well-designed payment system must combine an accurate patient classification system with a payment model that addresses clearly identified goals, including the creation of incentives for appropriate facility behavior. In this article, we consider the current DRG-PPS system in light of its strengths and weaknesses for paying for acute and chronic psychiatric care in hospitals.
Acute Psychiatric Care
Although the incentives intrinsic in PPS appear appropriate for acute inpatient psychiatry, the DRG classification system is not effective. For example, Taube, Lee, and Forthofer (1984a, 1984b) reported that DRGs explain less than 8 percent of the differences in LOS. Similar results have been reported by others (Morrison and Wright, 1985; Schumacher et al., 1986; English et al., 1986; Ashcraft, Fries, and Nerenz, 1989) and summarized in Goldman, Taube, and Jencks (1987). Furthermore, as Frank and Lave (1985b) point out, many of these analyses were performed at the aggregate level of a hospital rather than at the level of the patient, thereby probably magnifying the percentage explanation. If the explanation of resource use (connoted “variance explanation” or “reduction in variance”) is indeed close to zero, prospective payment for psychiatric patients based on DRGs would be essentially random.
There are several reasons for the poor results of DRGs in explaining LOS in psychiatric care. First, in psychiatry, diagnosis is exceedingly complex and, compared with other sectors of acute care, criteria are less well defined. Similarly, treatment patterns are less well defined, with multiple clinically accepted care modalities for similar diagnoses (e.g., Wells, 1985). DRGs do well in differentiating surgical cases because this treatment is less variable. Second, the DRGs are based on diagnoses in the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) (Public Health Service and Health Care Financing Administration, 1980), which in turn were based on the Diagnostic and Statistical Manual of Mental Disorders, Second Edition (DSM-II). Newer systems of diagnosis, e.g., DSM, Third Edition, Revised (DSM-III-R) (American Psychiatric Association, 1987), provide a broader assessment of patients and appear to better describe them, at least for clinical purposes.2 In particular, Goldman, Taube, and Jencks (1987) suggest that the lack of two of the five “axes” of DSM-III-R (i.e., severity of psychosocial stressors and highest level of adaptive functioning) is a critical problem. Finally, the DRGs, by construction, were based solely on the limited patient data available in the Uniform Hospital Discharge Data Set (UH-DDS).
In previous work, our premise was that there were data elements beyond those in the UHDDS that were nevertheless available and effective in understanding LOS. Our acute care classification system, Psychiatric Patient Classifications (PPCs), was derived using nationwide data from VA Medical Centers. During a 9-month period in 1985-86, data were obtained on all psychiatric discharges from all VA Medical Centers (n = 116,191). A questionnaire describing patients' medical and psychological conditions augmented the standard VA discharge abstracts. We derived a total of 74 PPC categories to explain LOS on a split sample, then validated this system on the remaining observations. Only acute episodes (up to 100 days long) were examined. These were first divided into 12 psychiatric diagnostic groups (PDGs), each of which was subdivided to form from 4 to 9 PPCs. Overall, the 74 PPCs explain 18 percent of the variation in LOS in both the development and validation samples, a considerable improvement over the 3.5 percent we computed for the DRGs (Ashcraft et al., 1989). Five variables from the questionnaire, unique to this study, were found to be predictive of LOS for some of the diagnostic categories: (1) disturbed state; (2) admission to a special post-traumatic stress disorder (PTSD) treatment unit; (3) first admission for this condition; (4) assistance with at least one of the activities of daily living (ADLs); and (5) severity of symptoms on admission, based on a modification of the Global Assessment of Function Scale (American Psychiatric Association, 1987). Care was taken in the choice of variables as well as in the definition of groups to assure that these characteristics could be validly and reliably measured and that incentives for appropriate care were in place.
Chronic Psychiatric Care
Inpatient psychiatry also includes care of patients with chronic conditions who stay well beyond the acute phase of their illness, and many of whom are essentially in permanent custodial care. Many of these patients are in PPS-exempted facilities such as State or county hospitals and are paid on a per diem basis. Our own VA data from 1986 suggest that nearly one-third of patients in psychiatric beds at a given point in time are “chronic” patients according to the definition described later. Given the high variability in LOS—in many cases, discharge is determined only by how long the patient lives—it is unlikely that anything other than a per diem payment system would be fair to facilities and control their risk of excessively long, expensive, and underpaid stays. It is possible to augment such a system with incentives for discharge or improvement in patients' morbidity, potentially at the level of the facility rather than at the patient level.
Chronic psychiatric care has many similarities to long-term care in nursing homes, for which payment has always been on a per diem basis. This similarity can be extended to help conceptualize a classification system which recognizes patient characteristics that explain differences in daily resource use. In long-term care institutions, functionality, such as the ability to perform ADLs (e.g., eating, toileting, etc.), plays a major role in explaining resource use (Schneider et al., 1988).
We believe that, in previous work (Fries et al., 1990), we were the first to consider which characteristics would explain actual, measured daily resource use for chronic psychiatric residents. For the development of a classification system for long-stay patients, a cross-sectional stratified sample of 2,968 psychiatric residents was formed. Data included an extremely broad assessment of patients' medical conditions, functional capabilities, mental deficits, treatments, etc., as well as direct measurement of each patient's daily resource use. These data were collected by nursing staff on the inpatient units, trained by project staff. Of the sample, 890 were designated as long-stay patients by virtue of either placement on a chronic-care unit, or a stay in excess of 100 days by the time of the survey. The Long-Stay Psychiatric Patient Categories (LPPCs) were derived to explain per diem total cost. The following five patient conditions were found to be useful in classifying residents: (1) aggressive behavior; (2) self-destructive behavior; (3) withdrawal; (4) wandering; and (5) psychotic behavior. With just 6 patient categories based on these variables, the LPPC system explains 11.4 percent of the variability in per diem resource use. Although this explanation appears low, there are no standards or even alternative systems with which to compare this system.
Payment Systems
The exemption of psychiatric facilities has removed them from the cost-containment incentives inherent in a case-based payment system (such as PPS) and has provided unwanted incentives to place or transfer psychiatric patients (Frank and Lave, 1985a). Thus, although there has been measurable progress on the definition of case mix in psychiatry, there has been little focus on the design of a payment system that would incorporate these case-mix measures. The episode basis for PPS would be inappropriate for chronic, long-term psychiatric inpatients. On the other hand, a per diem payment system for long-term patients, if applied to all psychiatric inpatient care, would vitiate critical incentives to keep LOS short for acute inpatients.
Only a few “mixed” short- and long-stay systems have been suggested, most notably the modified PPS proposed by Freiman, Mitchell, and Rosenbach (1988) and the “declining prospective per diem” system proposed by Frank and Lave (1986). Both of these proposals take a single payment model (either per discharge or per diem PPS) and adjust some of its features to take into account the wide variability in LOS for psychiatric inpatients. The proposal by Freiman, Mitchell, and Rosenbach (1988) preserves the incentives of the PPS for shortening LOS, but expands the use of outlier payments for both unusually long and unusually short stays in order to match payments more closely to actual incurred costs. The proposal by Frank and Lave (1986) is based on per diem payment, but introduces the concept of three per diem rates: (1) high—to cover the costs of initial work-up and stabilization; (2) declining—to recognize the lower costs of routine inpatient care; and (3) low—for extended, custodial care costs. The declining payment over time represents the incentive for not keeping patients too long. Our proposed model differs from both of these prior proposals by explicitly combining the approaches of episode and per diem payment in a single model that can cover psychiatric stays of any length.
Combining Acute and Chronic Payment Systems
Given the advantages and disadvantages of both the per episode and per diem systems, we consider here a mixed, unified approach to paying for psychiatric care. Short-stay patients would be paid on an episode basis (using the PPCs), whereas the longest-staying patients are paid on a per diem basis (using the LPPCs), accumulating additional payments (e.g., WWUs) for each day of stay. The fixed-price payment encourages efficiency by keeping acute stays short. This payment is based on the average cost of all stays of a given type (PPC). On the other hand, very long-staying patients will need to accumulate payment at close to the actual cost for each day of stay; otherwise the value of a long stay—in some cases several years—will be inaccurate and unfair to the chronic care facility. For the remaining stays, those neither the shortest nor the longest, we suggest a third payment option that provides a smooth “bridge” for paying for stays that are neither short nor long. We have denoted this entire system (including episode payment for acute stays, per diem payment for chronic stays, and an augmented per diem payment for intermediate stays) “transition pricing.”
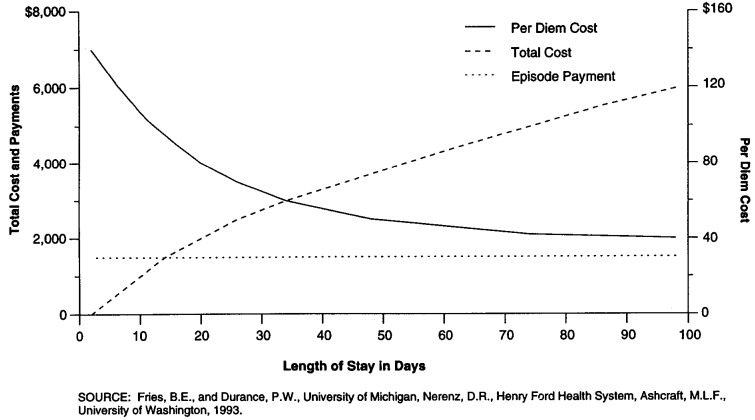
Two components are critical to describe the effect of a payment system based on LOS: cost and payment. Figure 1 displays a hypothetical distribution of the cost of each day of a hospital stay where the first day costs about $140 (the scale is displayed on the right) and the one-hundredth day costs about $40. Higher costs are expected in the earliest days of an average acute stay (Carter and Melnick, 1990), with more moderate costs for later days. Once a patient is chronically institutionalized, the average cost per day is essentially constant. The LOS at which the per diem cost curve becomes flat (the “custodial” level) we denote the “stability point.”
Figure 1. Hypothetical Per Diem Cost, Total Cost, and Fixed-Payment Functions for Acute and Long-Term Psychiatric Episodes, by Length of Stay.
A more useful form of displaying this cost relationship with LOS is the cumulative cost of a stay, also displayed for our hypothetical cost distribution in Figure 1. For any LOS, this is constructed by accumulating the per diem cost curve for all days of stay, up to and including the given LOS, and provides the total cost of an episode of care with that LOS. In our hypothetical example, after 100 days, the total accumulated costs would be about $6,000. Diagnosis, comorbidities, care patterns, and many other factors will affect the shape of these curves.
The third curve presented in Figure 1 represents one possible payment option as a function of LOS. The example presented is a fixed pure episode price—for all LOSs, a single fixed price is paid. Here we focus on all stays shorter than a very large trim point (100 days) at which a different type of payment may occur. The difference between the payment and cost curves indicates that for LOSs of less than a “break-even” point (about 14 days), the facility is paid more than its true cost, whereas the reverse is true for stays that exceed this LOS. These provide a clear and strong incentive to discharge patients with the shortest stays possible. Again, the payment level can be expected to differ by type of patient, and perhaps by type of facility. If the price is computed as the frequency-weighted average cost for all stays up to the trim point, then adjusting the trim point affects the payment level and the break-even point.
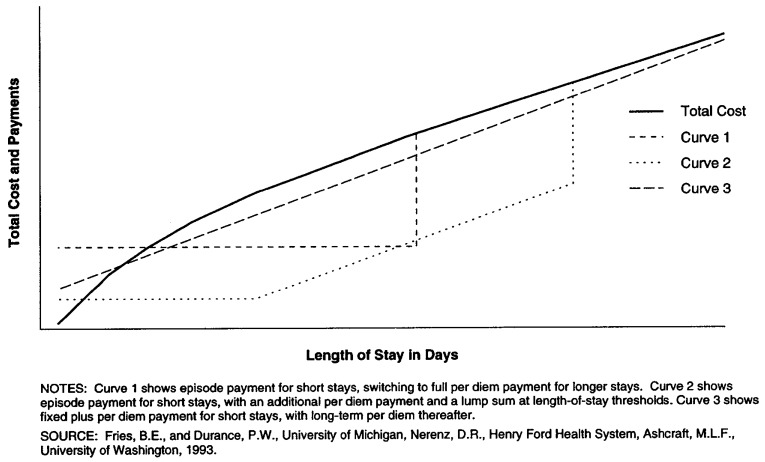
We suggest that such episode pricing, now normative payment practice for non-psychiatric acute care in the United States,3 is appropriate for short, acute stays—those that are shorter than a specified trim point. The interesting complexities occur when we consider options for integrating payment for stays that exceed a trim point. The primary difficulty is adjusting payment for long-staying residents to reimburse the facility for the losses accumulated by exceeding the break-even point in the episode-based portion of the payment system. We see these difficulties by reviewing several illustrative alternative payment systems. All involve an episode payment of some sort for short stays, and an additional per diem payment thereafter. Because of different possibilities for linking fixed episode payment with per diem payment, this system could operate in several manners, as shown in Figures 2 and 3:
Figure 2. Three “Mixed” Payment Models for Acute and Long-Term Psychiatric Episodes.
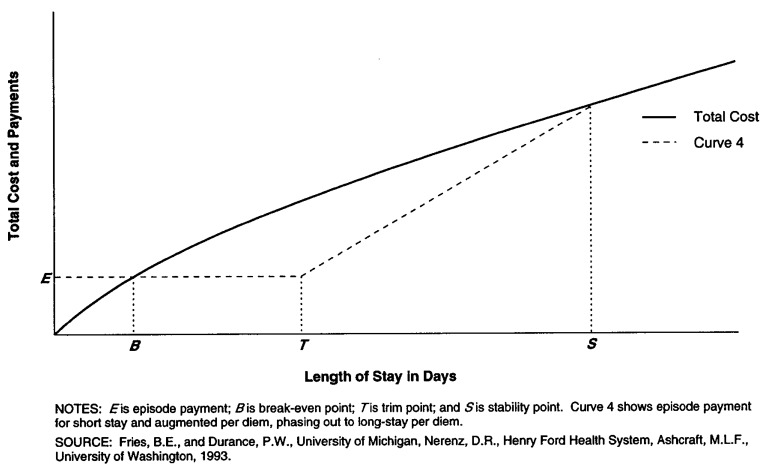
Figure 3. Transition Pricing Payment Model for Acute and Long-Term Psychiatric Episodes.
Episode Payment for Short Stays, Switching to Full Per Diem Payment for Longer Stays—This system mimics the current PPS without outliers; it recognizes the two types of patients and pays differently for each (Curve 1, Figure 2). At the threshold between the two systems, there can be a potentially large increase of payment according to the patient's short- and long-stay classification.
Episode Payment for Short Stays, with an Additional Per Diem Payment and a Lump Sum at LOS Thresholds—This system mimics the current PPS. After the trim point, a per diem payment is added to the payment. Eventually, however, the patient is classified as a long-staying patient, and a lump sum is provided to alleviate the accumulated loss (Curve 2, Figure 2).
Fixed Plus Per Diem Payment for Short Stays, with Long-Term Per Diem Thereafter—These models do not provide the short-stay discharge incentives of episode models, but prevent a large loss from accumulating. On the other hand, they may significantly overpay for short stays. The particular incentives depend on the per diem payment function. Curve 3 in Figure 2 displays a case where very short stays are profitable, but all others will be a loss.
Episode Payment for Short Stay, Additional and Augmented Per Diem, Phasing Out to Long-Stay Per Diem—The losses in the short-stay portion of a long stay are recouped gradually over the intermediate period of stay, as shown in Figure 3.
Three observations influenced our payment system design. First, a large change in payment caused by keeping a patient hospitalized an additional day (e.g., when staying an additional day will make the patient eligible for a block outlier payment) will encourage such prolongation of stay. Therefore, such large changes should be avoided. Second, the payment for long stays needs to be close to the actual cost, as any difference will provide unreasonable penalty or benefit to a facility that has little option to discharge a chronic stay patient. Finally, the payment for a particular LOS may be substantially different from the cost of this stay. Differences between these two represent the primary opportunity for developing incentives for appropriate discharge. This permits, for example, the incentive for early discharge of acute care patients.
We find that the “transition pricing” system (Figure 3) best meets these criteria. For any given set of diagnoses, it defines three payment sectors. For acute patients staying shorter than a trim point (T), there is a constant episode payment (E) provided. Stays shorter than the breakeven point (B) will provide revenues in excess of cost (“profit”); conversely those from B to T will result in a loss. For stays in excess of the stability point (S), where patients are determined to be long staying, days provide essentially equal marginal increases in cost. The marginal daily payment is set equal to the constant per-diem cost (D), determined by the long-staying case-mix category. It follows that stays exceeding the stability point will, on average, always break even. Finally, the payment for the transition sector from T to S is determined by the straight line between E (at LOS T) and the cumulative cost at S. By construction, all such stays will result in a loss. In the current modeling, we assumed that the overall payments would be exactly set to the overall costs, although this is not necessary to the design (e.g., a profit margin could be added). We should note that this “payment neutrality” balancing is not the same as “budget neutrality,” as the total cost and payment of the system are free to respond to changes in the numbers of inpatient days or episodes.
If Ct is the cumulative cost for a stay of length t, and f(t) is the frequency of all stays of this length, then the total transition pricing payment for any LOS (t) is computed as for each of the three payment sectors by:
| (1) |
Determining E requires equating total payment and total cost; the payment neutrality requires that:
| (2) |
By removing the equal payment and cost for t > S and using B where PB = CB, an alternate formulation of (2) equating the profit and loss from two regions is:
| (3) |
The payment function P(t) for any diagnosis can be computed in a series of steps. The stability point is first determined. We used the following three criteria for determining our values of S: (1) insofar as possible, we sought a common S for most PDGs, as this would simplify the system (we should note that this criterion is in no way crucial for the model); (2) the change in cost per day at S was approximately $0.25, a value which was determined somewhat arbitrarily; and (3) clinicians suggested that stays in excess of 100 days represented a different type of patient. Thus S was set at 100 days, a value close to that employed by at least one other group (Taube, Lee, and Forthofer, 1984a) in classifying LOSs. For four PDGs (2 [Alcohol Use Disorders], 3 [Opioid and Other Substance Abuse Disorders], 11 [Personality Disorders], and 12 [Impulse Control, Adjustment Disorders, and All Other Mental Disorders]), there were very few stays in excess of 80 days, so this lower threshold was used. Within each PPC, we then set 7 to the mean LOS plus twice its standard deviation, after eliminating LOSs exceeding S. Empirically, 95 percent of the observations had LOSs no more than the specified T. Finally, given S and T, E is computed so as to meet the payment neutrality represented in equation 3. In practice, a first approximation of E is given by the average episode cost for stays within the trim point, but this value has to be increased slightly to account for the expected loss for stays in the transition sector (again, in the third sector, the average profit is expected to be zero). We estimated the values of E for each type of diagnosis by an iterative search.
We report here the calculation of cumulative cost curves and payment functions for a sample of VA psychiatric inpatients. The primary purpose of these calculations is to demonstrate their feasibility and to analyze the distribution of actual VA discharges into gain and loss regions based on the cost and payment curves.
Methods
Data Collection
The primary data used to design and simulate a psychiatric payment system were derived from two sources. First, we obtained data on all psychiatric discharges from VA facilities during a 9-month period from June 1985 to February 1986. There were 116,191 stays with a primary psychiatric diagnosis, a regular discharge, and a LOS of at least 2 days. For each stay, the facility completed a short assessment describing the resident. These data, combined with other administrative data describing the stay, were used to derive the PPCs (Ashcraft et al., 1989) and to classify patients into PPCs for the current study.
The second data set was derived from a study of the daily costs of VA psychiatric care (Fries et al., 1990). For a stratified sample of 100 psychiatric units in 51 VA Medical Centers, we measured the time spent by different hospital staff directly or indirectly caring for patients over a 24-hour period. Staff involved included nurses, aides, therapy staff, physicians, psychologists, etc. The staff times were then wage-weighted to develop a per diem measure of staff cost. A subset of these data, describing patients with long stays (more than 100 days) or on chronic care units, has previously been used to derive the LPPCs; additional details of these data are available in the description of this study (Fries et al., 1990). Overall, we obtained usable data from a total of 2,968 patients cared for in 100 units in 51 VA Medical Centers. Three-quarters of this sample (2,255) had LOSs of fewer than 100 days at the time of data collection. We employed the full data set here to determine the relationship between cost and LOS.
Determining Cost Functions
Cost functions were estimated using the daily cost data set. Rather than estimate a single cost curve, we determined that differences could be discerned between cost curves for several major categories of psychiatric illnesses, represented by the PDGs (Table 1). As mentioned earlier, examination of the curves showed that establishing S at either 100 or 80 days would be appropriate for each PDG. Hospital resources for acute stays are provided both for diagnosis and for treatment. Over time, the costs of diagnosis can be expected to decline rapidly towards zero, whereas treatment costs will decline less rapidly to a constant representing the maintenance of a chronically ill patient. We represented the combined effect of this pair of cost phenomena using a four-parameter double-negative exponential model. For stays shorter than the S in each PDG, we first attempted to estimate (for each day of stay [t]) the model:
Table 1. Percent of Population, Variance Explanation, and Type of Fitted Per Diem Cost Equation, by Psychiatric Diagnostic Group (PDG).
| PDG Number | Description | Population1 | Variance Explanation2 | Type of Fitted Per Diem Cost Equation3 |
|---|---|---|---|---|
|
| ||||
| Percent | ||||
| 1 | Organic Mental Disorders | 4.62 | 8.5 | Double exponential |
| 2 | Alcohol Use Disorders | 34.61 | 2.1 | Single exponential |
| 3 | Opioid and Other Substance Use Disorders | 6.22 | 3.5 | Linear |
| 4 | Schizophrenic Disorders | 21.91 | 9.8 | Double exponential |
| 5 | Other Psychotic Disorders (NEC/NOS) | 4.99 | 8.1 | Double exponential |
| 6 | Bipolar Disorders | 5.15 | 2.8 | Single exponential |
| 7 | Major Depressions | 5.19 | (4) | (4) |
| 8 | Other Specific and Atypical Affective Disorders | 5.65 | (4) | (4) |
| 9 | Post-Traumatic Stress Disorder | 3.36 | 10.8 | Linear |
| 10 | Anxiety Disorders (NOS) | 1.64 | (5) | (5) |
| 11 | Personality Disorders | 2.02 | 23.5 | Double exponential |
| 12 | Impulse Control, Adjustment Disorders, and All Other Mental Disorders | 4.57 | 16.7 | Single exponential |
ln sample of all psychiatric discharges, excluding stays of more than 100 days (n = 79,337).
ln sample with time measurements (n = 2,199).
Detailed specifications of fitted models available upon request from the authors.
Combined with Bipolar Disorders.
Combined with Post-Traumatic Stress Disorder.
NOTES: NEC is not elsewhere classified. NOS is not otherwise specified.
SOURCE: Fries, B.E., and Durance, P.W., University of Michigan, Nerenz, D.R., Henry Ford Health System, Ashcraft, M.L.F., University of Washington, 1993.
where parameters β1, β2, β3, and β4 were fit to the measured daily resource consumption. Three of the rarer PDGs were combined when it was determined that they had similar cost curves and the cornbination made clinical sense. Thus, a total of nine curves were fit. The four-parameter model fit well for four of the PDGs. For the remainder, the computations did not converge, indicating the appropriateness of a single (two-parameter) negative exponential model. In two of these cases, a linear model (α + β*t, with fitted slope β and intercept α) was superior to the exponential one based on parameter significance and overall variance explanation. The cost-fitting results used for each PDG are described in Table 1.
Beyond the stability point, the average cost per day (and thereby the marginal per diem payment) was then computed for each LPPC category.
Simulating a Payment System
The final step combined discharge data, LOSs, and the estimated cost functions to calculate a simulated payment for each discharge in the VA data set. After eliminating stays longer than S (which would be paid based on LPPCs but would have no impact on a facility's profit or loss), the remaining patient stays (n = 79,337) were classified into PPCs. Next, the payment functions were determined, as in equation 1. Using transition pricing, the relative payment was computed for each stay in the data base. Distributions of discharges across gain and loss regions of the cumulative cost curves were determined (Figure 4), and linear regression models were used to determine whether facility characteristics (e.g., teaching status, bed size) were predictive of gain or loss at the individual discharge level.
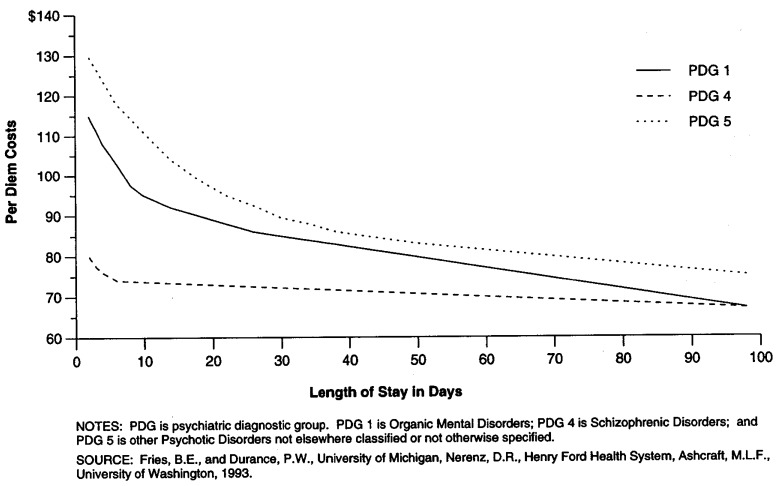
Figure 4. Fitted Per Diem Cost Curves for Acute Psychiatric Episodes.
Results
Across the 12 PDGs, the fitted cost equations explained from 2 to 23.5 percent of the variance in daily cost beyond that already accounted for by the mean daily cost (Table 1). Figure 4 shows the fitted cost functions for three illustrative PDGs.
As expected, we found the cost functions for each PDG to decline monotonically with increasing LOS. However, the “peak” of costs in the first 3 days was less than had been expected. For example, the average daily cost of the first 3 days of care ($114.82) for PDG 1 (Organic Mental Disorders) was only 18.1 percent higher than that of the next 11 days' average ($97.22). PDG 11 (Personality Disorders) demonstrated the greatest change of the non-linear cost curves. It had the highest initial cost ($124.74) and declined to 33 percent of this level after 7 days. On the other hand, 4 of the non-linear cost curves resulted in less than an 8-percent decline from the initial cost during the first week. Thus, many of the cost curves were relatively flat, but all declined over time.
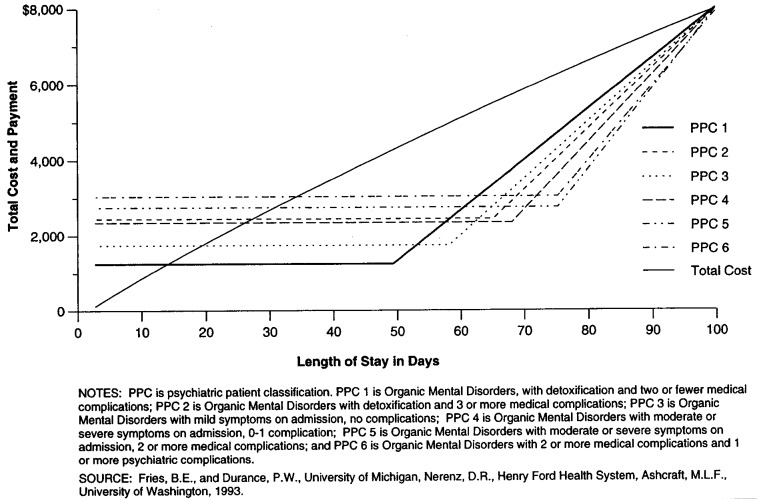
The transition pricing payments were determined by sequentially determining S, then, for each PPC, T at the 95th percentile of LOS, and finally, E by an iterative search. The payment curves for PDG 1, representing PPCs 1 through 6, are given in Figure 5, along with the cost curve. By computing the total payments (including those for stays beyond the stability point), we were able to calibrate our relative payments in real dollars. Each workload unit was worth $1.45 in 1986 dollars.
Figure 5. Total Cost and Payment, by Length of Stay for Acute Psychiatric Episodes.
In the case of PPC 1 (Organic Mental Disorders with Detoxification and Two or Fewer Medical Complications), S was set to 100 days. From the LOS distribution for the 3,669 patients of this type, we calculated T to be 49 days. Using equations 1 and 2, we determined iteratively that E was $1,301. Thus, for this PPC, the total payment would be $1,301 for all stays of up to 49 days (Figure 5). Every stay of fewer than 13 days would result, on average, in a profit. For stays in excess of 49 days, the total payment would increase by $132.24 per day up to a total payment of $8,048 for a stay of 100 days. Beyond this, the payment would be increased by the cost of the LPPC category into which the patient was placed, and the average cost and payment of additional days would be equal.
Table 2 contains the average, standard deviation, minimum, and maximum values for the payment, estimated cost, and net income for all 79,337 stays in the data set. The stays are divided in the table into three profit and loss regions. The first (LOS less than B) represents financial gain; the second and third (stays between B and T and stays between T and S) represent financial loss. (Again, the fourth region, representing stays beyond S, is excluded because payment and cost are set equal by construction in the model.) With transition pricing, the first two regions have similar average revenues, but the costs in the second region lead to losses almost equal to the profits in the first sector. Stays in the third region are relatively rare (5 percent of all non-chronic stays), yet contribute the largest average loss. Although payment and cost are skewed distributions, net income is very close to normally distributed (not shown).
Table 2. Estimated Revenue, Cost, and Profit in Dollars for Short-Stay Episodes,1 by Payment Regions.
| Payment Region | Payment Values | |||
|---|---|---|---|---|
|
| ||||
| Average | Standard Deviation | Minimum | Maximum | |
| Total | ||||
| Revenue | 2,343 | 953 | 418 | 9,846 |
| Cost | 2,343 | 1,634 | 180 | 9,846 |
| Profit | 0 | 1,223 | −4,440 | 4,320 |
| Length of Stay | 25.6 | 18.8 | 2 | 2100 |
| n = 79,3373 | ||||
| Payment Regions | ||||
| Episodes Less than B: | ||||
| Revenue | 2,246 | 709 | 418 | 4,555 |
| Cost | 1,346 | 775 | 180 | 4,475 |
| Profit | 899 | 662 | 2 | 4,320 |
| Length of Stay | 13.9 | 8.5 | 2 | 44 |
| n = 41,534 | ||||
| Episodes Longer Than B but Less Than T: | ||||
| Revenue | 2,207 | 733 | 418 | 4,555 |
| Cost | 3,092 | 1,260 | 446 | 7,621 |
| Profit | −885 | 818 | −4,261 | −1 |
| Length of Stay | 34.2 | 13.6 | 5 | 74 |
| n = 33,852 | ||||
| Episodes Longer Than T: | ||||
| Revenue | 4,535 | 1,809 | 1,019 | 9,846 |
| Cost | 6,411 | 1,378 | 3,201 | 9,846 |
| Profit | −1,876 | 976 | −4,440 | 0 |
| Length of Stay | 75.3 | 13.0 | 32 | 2100 |
| n = 3,951 | ||||
< = 100 days.
Stability point for most of the psychiatric patient classifications.
Number of psychiatric discharges with non-chronic stays.
NOTES: B is break even point; T is trim point.
SOURCE: Fries, B.E., and Durance, P.W., University of Michigan, Nerenz, D.R., Henry Ford Health System, Ashcraft, M.L.F., University of Washington, 1993.
With the potential variation between cost, payment, and profit at the individual case level, we were concerned about whether certain types of VA facilities would be adversely affected by this payment model. Three major facility characteristics were examined for such a reimbursement bias: (1) teaching affiliation; (2) psychiatric bed complement; and (3) whether the facility is designated as specializing in long-term psychiatric care.4
Each of the three characteristics was incorporated as an independent variable in a regression model with the individual discharge as the unit of analysis. We examined the relationship to payment, estimated cost, and net income for all discharges with LOS within trim points (n = 79,337). Except for one, all of the models showed significant relationships, but this was primarily due to the large sample size. None of these variables explained slightly more than 1 percent of the variance (Table 3). Similar findings were seen for multivariate models using these same variables.
Table 3. Percent Variance Explanation1 for Models Relating Facility Characteristics with Payment, Cost, and Net Payment, for Acute and Long-Term Psychiatric Episodes.
| Characteristic | Payment | Cost | Net Payment |
|---|---|---|---|
| Teaching | 20.0 | 0.0 | 0.1 |
| Psychiatric Beds | 0.1 | 0.9 | 1.1 |
| RAM Group | 0.1 | 0.4 | 0.6 |
Variance explanation is the analysis of variance Eta-squared statistic for categorical variables (teaching and the resource allocation methodology [RAM] group), otherwise it is the R-squared statistic of a linear regression.
Not significant (p = .220); all others are significant at the p < .0001 level.
SOURCE: Fries, B.E., and Durance, P.W., University of Michigan, Nerenz, D.R., Henry Ford Health System, Ashcraft, M.L.F., University of Washington, 1993.
Discussion
The principal purpose of this study was to develop a feasible system combining payment for acute and long-term psychiatric care. Transition pricing appears to meet both clinical and policy goals. It provides strong incentives for early discharge of acute patients, yet recognizes that a significant percentage of admissions remain hospitalized for long periods of time for chronic conditions. Therefore, it represents a prototype of combining long- and short-stay payment in a single system, with the potential for bundling acute care and long-term nursing home care.
Implementation of such a system will require new administrative structures and raise a variety of additional design issues. Some of these include:
Payment System Design. The full design of a payment system will also need to address whether the system will acknowledge differences between facilities such as market costs (input price adjustment) and peer groupings (with different payments for particular types of facilities, based on size, mission, location, etc.).
Responsiveness. For the per diem part of the payment model, there may be a need for more than one assessment of patients during extended hospital stays. Tradeoffs would have to be made between the costs of collecting data for classifying patients multiple times during long stays and the increased precision of resource allocation resulting from reclassification. The exact nature of the tradeoffs may differ across facilities, creating the need for some policy direction from the VA, the Health Care Financing Administration, or other major payers on how often reclassification should be done.
Data Requirements and DRG Environment. The system requires several new data elements beyond those which are required for the DRG system. The total number of new data elements required for patient classification (10 for PPCs and LPPCs combined) is not large, but any collection of new data adds to administrative burden. Cost studies that assign dollar values to relative values for workload will be an ongoing process at the payer level, but the time studies that led to the relative values themselves would only need to be done if the model was applied in a distinctly different setting or if significant changes in practice patterns evolved over time. The additional costs of administration would have to be viewed as the cost of increasing fairness in the payment system and the introduction of stronger incentives for cost control at the provider level. Our experience has been that the availability of patient-level information provides an excellent opportunity to design and implement effective quality surveillance and assurance systems. This multiple use of such data encourages its accuracy, and thereby its perceived value.
Monitoring and Auditing. Procedures will have to be developed to ensure that the data reported by facilities represent an accurate picture of patients' conditions. The obvious financial incentives for “upcoding” patients into more lucrative categories will have to be set against quality assurance, auditing, and utilization review procedures that identify and correct inaccurate patient classifications. Such auditing, most appropriately, would also include monitoring for inappropriate discharges: for example, premature or delayed discharge of residents whose stays could be expected to have fallen in the high-loss region of transition pricing.
Incentives and Disincentives. A variety of additional efficiency and quality incentives can be implicitly or explicitly incorporated in the payment system. The system itself is designed to reward shorter stays for acute patients and efficient per diem care for chronic patients. Implementation and evaluation of the system should attend closely to whether any additional incentives need to be added, for instance, for moving chronic patients through treatment into other categories that represent clinical improvement, but lower per diem reimbursement. Other alternatives include incentives to improve the status of or discharge long-staying patients. It should be noted that independent of any other incentive, facilities will still wish to discharge long-staying residents in order to meet their mission of care and to provide the opportunity to use a bed thus freed for a short-stay (and potentially profitable) patient.
A number of other implementation issues have also been raised by others, including Cohen, Holahan, and Liu, 1986; Frank and Lave, 1986; and Frank et al., 1986. These include: setting policies on the mix of local, regional, or national costs to be used as a basis for setting price levels; adopting a different payment rate for “short-stay outliers;” and allowing local or regional variations in preferred practice patterns to determine LOS trim points or payment levels. Our proposed model is not uniquely exempt from these difficult policy issues.
Although we have demonstrated the application of transition pricing in psychiatry using our two patient classification systems—PPCs and LPPCs—these are not strictly necessary for implementation. The same type of system could, for example, be implemented using DRGs for acute care and a flat per diem rate for long-staying patients. However, such a system could be criticized on the grounds of the poor performance of DRGs for psychiatry and the substantial differences found in per diem costs among long-stay patients.
The simulation of the transition pricing system for psychiatric care in the VA required the computation of a large number of parameters and functions. A finding of interest during these calculations was the lack of high-cost days early in acute stays. Given that a flurry of activity usually accompanies a new admission, charges for the first day or two are typically much higher than those of later days (Carter and Melnick, 1990). We were surprised to see relatively small differences between costs in the first days and later costs. One reason for the difference in patterns may be that the Carter and Melnick findings were based on billed charges, with nursing time billed at a flat per diem rate across all days of stay. Ancillaries were therefore the significant variable item, and ancillaries are indeed used more frequently during initial workup and diagnosis. In our VA data, nursing and other care-giver time was explicitly measured and valued in the calculation of daily costs. Other high-cost items early in an acute stay were not measured, including the cost of diagnostic or therapeutic procedures and expendable or durable medical equipment. Our data therefore emphasize different costs and may be less likely to have included items most variable across days of stay.
The distribution of discharges across gain and loss regions of LOS suggested that a small number of patients with moderately long stays would be a significant concern under this payment model. Those patients discharged between T and S made up only 5 percent of VA discharges in the data set, but had the largest loss on a per-case basis. The magnitude of the loss for each patient would diminish with each day of additional stay up to S, but the cumulative loss close to T would be significant. Currently, there is no particular incentive for VA (or non-VA) facilities to avoid these moderately long stays. However, with such a model in place, there would be strong incentives to identify patients clearly and early as either acute or chronic and avoid LOSs near T. This would conceivably work to the disadvantage of extended length treatment and rehabilitation inpatient programs, unless a new PPC class was created for a defined class of patients receiving an identifiable mode of treatment that required LOSs in the 45- to 60-day range.
Finally, the lack of strong statistical relationships between facility characteristics and gains and losses under the payment model is encouraging. In principle, payment should be based on patient characteristics alone, and should not result in biased payment for any specific type of facility. Results of the regression analyses indicated that patients would not be consistently under-or over-reimbursed in teaching versus non-teaching, psychiatric versus general medical and surgical, or large versus small facilities. Although individual facilities could have a preponderance of either gains or losses (depending on their individual case mixes and treatment patterns), the preliminary results indicated that all major classes of facilities would have a relatively balanced mix of both gains and losses and therefore the potential for profitability.
We believe that the proposed model would be applicable in non-VA settings. We recognize that there are many differences between VA and non-VA patient populations. Users of VA medical services are predominantly male. They have lower educational levels and are more likely to be unmarried than veterans in general or the population as a whole. They are older than either veterans in general or the population as a whole (U.S. Department of Veterans Affairs, 1990). However, although there are undoubtedly a number of other differences between the VA patient population and the general population of psychiatric patients, these differences do not alter the fundamental characteristics of either the model or its underlying patient classification systems. The payment model is designed for any treatment setting in which the possibility of both acute and chronic inpatient care exists. The patient classification systems include the entire spectrum of psychiatric diagnosis and levels of severity.
One difference that would have to be addressed is the potential for patients in non-VA settings who have long stays to split those stays across more than one institution and receive payment from more than one payer (e.g., Medicare and Medicaid). The “catchup per diem” (middle) region of the payment model is best suited for a situation in which a single inpatient facility and single payer are involved in a given patient's long stay. Losses incurred earlier in a stay are made up later. If a patient was transferred to a long-stay facility at an intermediate LOS, and if a different payer became involved in the long-term care portion of the stay, the catchup per diem would be more difficult to implement than in a single organization like the VA. In addition, use of the model in non-VA settings would probably require a modest-sized replication of the study reported here in order to identify any significant differences in patterns of care, staffing levels, or salary levels that would justify recalculation of cumulative cost curve parameters such as trim points, stability points, or daily costs.
The proposed system would be applicable in settings other than psychiatry as well. Any patient group that has both acute and long-term care could conceivably be paid on a transition pricing model that combines the key features that we propose: fixed payment for an acute care episode, per-diem payment for long, custodial stays, and a catchup per diem during a transition period that gradually eliminates the losses accumulated during the late stages of the acute stay. In this case, DRGs for acute care stays and a long-stay per diem classification system such as Resource Utilization Groups (Fries et al., 1994) might be appropriate classification systems.
The development of alternative payment systems does not ensure appropriate levels of funding for the provision of quality of care. Nevertheless, providing equitable distribution of available funds, recognizing differences in actual resource use for different types of residents, and providing incentives for appropriate care can assure that these funds are used most effectively and efficiently.
Acknowledgments
The authors would like to acknowledge the assistance of biostatistician Dr. Andrzej Galecki of the Michigan Geriatric Research and Training Center.
The research presented here was supported in part by the Department of Veterans Affairs Great Lakes Regional Office, Ann Arbor Geriatric Research, Education, and Clinical Center, and the University of Michigan Geriatric Research and Training Center. Brant E. Fries is with the Institute of Gerontology and School of Public Health, University of Michigan, and the Geriatric Research, Education, and Clinical Center, Ann Arbor Department of Veterans Affairs Medical Center. Paul W. Durance is with Health Services Research and Development, Department of Veterans Affairs, and the School of Public Health, University of Michigan. David R. Nerenz is with the Center for Health System Studies, Henry Ford Health System. Marie L.F. Ashcraft is with the Seattle Department of Veterans Affairs Medical Center and the Department of Health Services, University of Washington.
Footnotes
The VA does not pay its facilities directly on a per case basis. It allocates the total dollars provided for inpatient care by Congress. Each DRG is assigned an allocation unit—weighted workload units (WWUs). At year end, each facility produces a WWU total associated with its discharges and the weights assigned to each one. The hospital's share for the next fiscal year is determined by its WWU total in relation to the total pool of WWUs for all 172 inpatient facilities (Rosenheck, Massari, and Astrachan, 1990).
There is yearly updating of the DRGs, so that new concepts (e.g., from DSM-III-R) are incorporated; nevertheless, the orignal DRG derivation predates these developments.
The PPS has statistically derived trim points for each DRG. Stays within the trim point are paid at a fixed price, whereas outlier stays are reimbursed with an additional perdiem.
More detailed simulation of facility-level effects, using a larger set of facility characteristics, is being taken on as a separate analysis and will be presented in a future publication.
Reprint requests: Brant E. Fries, Ph.D., Institute of Gerontology, University of Michigan, 300 North Ingalls, Ann Arbor, Michigan 48109-2007.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised. Washington DC.: 1987. [Google Scholar]
- Ashcraft MLF, Fries BE, Nerenz DR, et al. A Psychiatric Patient Classification System: An Alternative to Diagnosis-Related Groups. Medical Care. 1989 May;27(5):543–557. doi: 10.1097/00005650-198905000-00009. [DOI] [PubMed] [Google Scholar]
- Carter GM, Melnick GA. How Services and Costs Vary By Day of Stay for Medicare Hospital Stays. RAND Corporation; Santa Monica, CA.: 1990. Report No. R-3870-ProPAC. [Google Scholar]
- Cohen J, Holahan J, Liu K. Financing Long-Term Care for the Mentally III: Issues and Options. Washington, DC.: The Urban Institute; Jul, 1986. Grant Number NIMH-278-85-0022. Prepared for the National Institutes of Mental Health. [Google Scholar]
- DesHarnais SI, Wroblewski R, Schumacher D. How the Medicare Prospective Payment System Affects Psychiatric Patients Treated in Short-Term General Hospitals. Inquiry. 1990 Winter;27:382–388. [PubMed] [Google Scholar]
- English JT, et al. Diagnosis-Related Groups and General Hospital Psychiatry: The APA Study. American Journal of Psychiatry. 1986;143:131–139. doi: 10.1176/ajp.143.2.131. [DOI] [PubMed] [Google Scholar]
- Federal Register: Proposed Changes to DRG Classification and Weighting Factors. No. 106. Vol. 56. Washington: U.S. Government Printing Office; Jun 3, 1991. pp. 25181–25265. Office of the Federal Register, National Archives and Records Administration. [Google Scholar]
- Fetter RB, Shin Y, Freeman JL, et al. Case Mix Definition by Diagnosis-Related Groups. Medical Care Supplement. 1980 Feb;18(2):1–53. [PubMed] [Google Scholar]
- Frank RG, Lave JR. The Impact of Medicaid Benefit Design on Length of Hospital Stay and Patient Transfers. Hospital and Community Psychiatry. 1985a;36(7):749–753. doi: 10.1176/ps.36.7.749. [DOI] [PubMed] [Google Scholar]
- Frank RG, Lave JR. The Psychiatric DRGs: Are They Different? Medical Care. 1985b Oct;23(10):1148–1155. doi: 10.1097/00005650-198510000-00003. [DOI] [PubMed] [Google Scholar]
- Frank RG, Lave JR. Per Case Prospective Payment for Psychiatric Inpatients: An Assessment and Alternatives. Journal of Health Politics, Policy and Law. 1986 Spring;11(1):83–96. doi: 10.1215/03616878-11-1-83. [DOI] [PubMed] [Google Scholar]
- Frank RG, Lave JR, Taube CA, et al. The Impact of Medicare's Prospective Payment System on Psychiatric Patients Treated in Scatterbeds. Cambridge, MA.: National Bureau of Economic Research; Sep, 1986. Working Paper Number 2030. [PubMed] [Google Scholar]
- Freiman MP, Mitchell JB, Rosenbach ML. Simulating Policy Options for Psychiatric Care in General Hospitals Under Medicare's PPS. Archives of General Psychiatry. 1988 Nov;45:1032–1035. doi: 10.1001/archpsyc.1988.01800350066009. [DOI] [PubMed] [Google Scholar]
- Fries BE, Nerenz DR, Falcon SP, et al. A Classification System for Long-Staying Psychiatric Patients. Medical Care. 1990 Apr;28(4):311–323. doi: 10.1097/00005650-199004000-00003. [DOI] [PubMed] [Google Scholar]
- Fries BE, Schneider D, Foley W, et al. Refining a Case-Mix Measure for Nursing Homes—Resource Utilization Groups (RUG-III) Medical Care. doi: 10.1097/00005650-199407000-00002. To be published. [DOI] [PubMed] [Google Scholar]
- Goldman HH, et al. Prospective Payment for Psychiatric Hospitalization: Questions and Issues. Hospital and Community Psychiatry. 1984;35(5):460–464. doi: 10.1176/ps.35.5.460. [DOI] [PubMed] [Google Scholar]
- Goldman HH, Taube CA, Jencks SF. The Organization of the Psychiatric Inpatient Services System. Medical Care Supplement. 1987 Sep;25(9):S6–S21. [PubMed] [Google Scholar]
- Horgan C, Jencks SF. Research on Psychiatric Classification and Payment Systems. Medical Care Supplement. 1987 Sep;25(9):S22–S36. [PubMed] [Google Scholar]
- Jencks SF, Goldman HH, McGuire TG. Challenges in Bringing Exempt Psychiatric Services Under a Prospective Payment System. Hospital and Community Psychiatry. 1985;36(7):764–769. doi: 10.1176/ps.36.7.764. [DOI] [PubMed] [Google Scholar]
- Lee ES, Forthofer RN. Evaluation of the DHHS Proposed Diagnostic Related Groups (DRGs) For Mental Health. Rockville, MD.: National Institutes of Mental Health; Sep 30, 1983. Final Report to NIMH. [Google Scholar]
- McCarthy CM. DRGs: Five Years Later. New England Journal of Medicine. 1988;318:1683. doi: 10.1056/NEJM198806233182510. [DOI] [PubMed] [Google Scholar]
- Morrison LJ, Wright G. Medicare Prospective Payment for Alcohol, Drug Abuse, and Mental Health Services. 1985 Dec 31; Executive Summary of Contract Number NIMH-278-84-0011(DB). Macro Systems. [Google Scholar]
- Public Health Service and Health Care Financing Administration. International Classification of Diseases, 9th Revision, Clinical Modification. Washington: U.S. Government Printing Office; Sep, 1980. DHHS Pub. No. 80-1260. Public Health Service. [Google Scholar]
- Rosenheck R, Massari L, Astrachan BM. The Impact of DRG-Based Budgeting on Inpatient Psychiatric Care in Veterans Administration Medical Centers. Medical Care. 1990 Feb;28(2):124–134. doi: 10.1097/00005650-199002000-00003. [DOI] [PubMed] [Google Scholar]
- Rupp A, Steinwachs DM, Salkever DS. The Effect of Hospital Payment Methods on the Pattern and Cost of Mental Health Care. Hospital and Community Psychiatry. 1984;35(5):456–459. doi: 10.1176/ps.35.5.456. [DOI] [PubMed] [Google Scholar]
- Schumacher DN, et al. Prospective Payment for Psychiatry—Feasibility and Impact. New England Journal of Medicine. 1986 Nov 20;315(21):1331–1336. doi: 10.1056/NEJM198611203152106. [DOI] [PubMed] [Google Scholar]
- Taube C, Lee ES, Forthofer RN. DRGs in Psychiatry. Medical Care. 1984a;22(7):597–610. doi: 10.1097/00005650-198407000-00002. [DOI] [PubMed] [Google Scholar]
- Taube C, Lee ES, Forthofer RN. Diagnosis-Related Groups for Medical Disorders, Alcoholism, and Drug Abuse: Evaluation and Alternatives. Hospital and Community Psychiatry. 1984b;36(7):452–455. doi: 10.1176/ps.35.5.452. [DOI] [PubMed] [Google Scholar]
- Taube C, Thompson JW, Burns BJ, et al. Prospective Payment and Psychiatric Discharges From General Hospitals With and Without Psychiatric Units. Hospital and Community Psychiatry. 1985;36(7):754–759. doi: 10.1176/ps.36.7.754. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. Survey of Medical System Users. Office of Planning and Management Analysis; Washington, DC.: 1990. Report OPMA-M-043-90-2. [Google Scholar]
- Vladeck BC. Hospital Prospective Payment and the Quality of Care. New England Journal of Medicine. 1988;319:1411. doi: 10.1056/NEJM198811243192109. [DOI] [PubMed] [Google Scholar]
- Wells KB. Depression as a Tracer Condition for the National Study of Medical Care Outcomes: Background Review. Santa Monica, CA.: RAND; Jul, 1985. Contract Number R-3293-RWJ/JHK. [Google Scholar]
- Widem P, Pincus HA, Goldman HH, et al. Prospective Payment for Psychiatric Hospitalization: Context and Background. Hospital and Community Psychiatry. 1984;35(5):447–451. doi: 10.1176/ps.35.5.447. [DOI] [PubMed] [Google Scholar]