Abstract
Functionality, as measured by activities of daily living (ADL), is the most important predictor of the cost of nursing home care. Data from a field-test version of the federally mandated Minimum Data Set (MDS) were examined using analysis of variance (ANOVA) and recursive partitioning methods to determine the relationships between ADL limitations and nursing cost (wage-weighted nursing time) among nursing home residents (n = 6,663). From this analysis, an index based on limitations in four ADLs was created. The developed ADL index is a readily determined measure of functional status useful in allocating nursing staff within nursing homes and in comparing the functional status of groups of residents, explaining 30 percent of variance in nursing costs among nursing home residents.
Introduction
Among nursing home residents, limitations in ADLs are the strongest determinants of the use of nursing resources (the cost of providing nursing care). For example, ADL limitations play a central role in all case-mix classification systems that predict nursing resource use in nursing homes (Schneider et al., 1988; Arling et al., 1987; Cameron, 1985; Cavaiola and Young, 1980; Morris et al., 1987). Measures of ADL limitations alone perform comparably with or better than several full case-mix classification systems in accounting for nursing resource use among residents (Fries, 1990).
Previous efforts to examine the relationships between ADL limitations and nursing resources have had several limitations. Most published studies that focus on nursing homes have used relatively limited indicators of ADL status (e.g., di- or trichotomous measures of performance of individual ADLs) (Minnesota Department of Health, 1986; Arling et al., 1987; Cameron, 1985). In addition, although many studies have examined the relationships of ADL limitations and nursing resources as part of efforts to develop case-mix classification systems (Schneider et al., 1988; Fries et al., 1994; Cameron, 1985; Minnesota Department of Health, 1986), relatively few have paid specific attention to the types and levels of ADL limitation among nursing home residents that account for the time spent by registered nurses (RNs), licensed practical nurses (LPNs), aides, and orderlies caring for residents.
The relevance of determining the specific relationships between ADL limitation and use of nursing resources in nursing homes is heightened by recent widespread implementation of the MDS (Morris et al., 1990, 1991). Virtually all nursing homes throughout the United States have implemented this assessment system, in compliance with recent Federal regulations. If the usefulness of these extensive data is to be maximized, the detailed information on ADL limitation included in the MDS must translate into information useful for decisions in resource allocation and clinical management.
Understanding the detailed relationships between patterns and types of ADL limitations and the use of nursing resources in nursing homes can aid in allocating staff resources within and among nursing homes to meet resident needs most efficiently and adequately. This is particularly likely to be true among residents who require primarily supportive, rather than specialized, nursing care, because specialized care may be associated with resident characteristics other than ADL limitations.
In addition, a global measure of ADL function that correlates with the use of nursing resources may be an appropriate summary indicator of residents' functional status to aid in comparing functional status among groups of residents and in evaluating changes in functional status in individuals or groups of residents over time.
The purposes of this article were twofold. First, we intended to use information contained in the MDS to describe more precisely the relationships between individual measures of ADL limitations and the use of nursing resources in nursing homes. In this, we could use ADL measures that were relatively rich in breadth (eight ADLs) and depth (i.e., separate four- or five-level measures for self-performance and level of human support for each ADL). Second, we wished to develop a summary scale of ADL limitations that was simple and accurate, and best correlated with the amount of nursing resources used by nursing home residents. As ADLs have been shown to be the best single predictors of resource use, this scale was also designed to be incorporated into a case-mix measurement system (Resource Utilization Groups, Version III [RUG-III]).
The goals of the study included neither the development of a comprehensive classification system for nursing home residents, as might be appropriate for the basis of a reimbursement system, nor the identification of all variables contributing to resource use in nursing homes, including those that may be correlated with ADL limitations. These issues were considered very briefly, by design, and only to facilitate the development of a simple, readily applicable summary measure of ADL limitations among nursing home residents. However, to examine the possibility that the receipt of specialized nursing care (e.g., wound care, ostomy care), which may be independent of ADL status, affected the relationships between ADL limitations and nursing resource use, these relationships were examined both among all residents and among the subset of residents without specialized nursing needs.
Methods
Data Collection
Our participation in a larger study to develop the RUG-III case-mix classification system for nursing home residents made available early MDS information for a large number of nursing home residents, along with detailed measures of their use of nursing resources. This offered the opportunity to examine in detail the relationships between ADL limitations and the use of nursing resources among nursing home residents.
The data were gathered in 1990 as part of the HCFA Multi-State Nursing Home Case-Mix and Quality (NHCMQ) demonstration project from a sample of 6,663 residents in 176 nursing homes in 6 States (Kansas, Mississippi, Maine, Nebraska, South Dakota, and Texas).1 Both the size of the sample and the fact that, for the first time, such data were derived from multiple States make it uniquely suited for this analysis. The nursing homes were not selected randomly, but were chosen to represent a broad spectrum of levels of care, with purposeful oversampling of heavy-care residents. To focus on appropriate nursing home care patterns, nursing homes with substandard staffing patterns, those with recent citations from State certification and licensure review, and those under litigation were excluded.
The survey instrument used in this phase of the NHCMQ demonstration project was an early version of the MDS for nursing home residents, called the Resident Status Measure (RSM). All ADL data and other relevant items from the RSM are virtually identical to those in the MDS. A 10-percent subsample of RSMs was tested for reliability, comparing a facility nurse assessor and the project's nurse reviewer. The Spearman-Brown reliability coefficients for the performance ADLs ranged from 0.77 (for bathing) to 0.88 (transferring). These correspond well to the excellent reliability reported in testing of the MDS (Morris et al., 1990; Hawes et al., 1992).
The other important portion of the data was the actual time spent by facility staff in caring for each resident. Every nurse and aide on sample units accumulated their own care time, with a variety of controls to assure valid data. They reported all the time they spent in direct hands-on care and in any other care that benefited individual residents, including care planning conferences, discussions with physicians or family, extensive charting, and so forth. Staff time spent with groups of residents was allocated to individuals. There was no attempt to collect the time by task, as we believe that this has the potential of skewing the data; only the actual times were recorded. Other time spent on routine charting, ward maintenance, meals, and breaks was also recorded, so that the total time each staff member spent on a shift could be reconciled with the total time allocated to all activities. These methods were augmented with frequent data checking during, and focused data checking immediately following, each shift, structured training, full pilot testing in each facility, and a 24-hour “hot-line.” We have successfully used this method of measuring staff time in seven separate studies.
Excluded from the sample were 275 residents (4 percent of the total sample) in Alzheimers units (units specializing in the care of cognitively impaired residents), who might receive nursing care designed to meet the needs of cognitively impaired residents independent of ADL function. Also excluded were 29 residents (fewer than 1 percent of the total sample) with missing values for one or more ADL performance variables.
Data Elements and Variable Definitions
Nursing resources were measured as patient-specific time spent by nursing personnel, including RNs, LPNs, aides, and orderlies. Patient-specific time was defined as all time spent by nursing personnel caring for an individual resident, including direct (hands-on) resident care and other time that was specifically attributable to an individual resident (e.g., resident care conferences or communication with families or physicians). Because our interest was in predicting resources devoted to resident care rather than the number of minutes of staff time, times spent by each type of nursing personnel were weighted according to their relative pay scales, with weights for RNs, LPNs, and aides of 1.34,1.02, and 0.67, respectively. These weights were based on previous work, and were defined as the mean facility-specific wage weight among 38 nursing homes in 5 States (New York, Pennsylvania, Illinois, Florida, and California) (Fries et al., 1989). Facility-specific wage weights were calculated as the mean wage rate for a facility, divided by the facility mean wage for all staff, to control for market wage conditions. Analyses from this previous study, the purpose of which was to derive a case-mix classification system for nursing home residents, demonstrated that the results were relatively insensitive to the particular weighting scheme applied, within a broad range of alternatives. Wage-weighted nursing minutes are referred to hereafter as “nursing cost.”
Information on eight ADLs was available for examination: eating, bed mobility, toileting, transferring, locomotion, bathing, dressing, and grooming. Table 1 lists the definitions of each ADL from the survey instrument.
Table 1. Definitions of Activities of Daily Living (ADL).
| ADL | Definition: Ability to— |
|---|---|
| Bed Mobility | Move to and from a lying position, turn side-to-side, and position body parts while in bed. |
| Eating | Eat and drink. |
| Transferring | Move to and from: bed, chair, wheelchair, standing (excluding toilet). |
| Toileting | Use toilet room, commode, bedpan, or urinal; transfer on and off toilet, cleanse, change pad, manage ostomy or catheter, adjust clothes. |
| Locomotion | Move between locations in his or her room and adjacent corridor on same floor. If in wheelchair, self-sufficiency once in chair. |
| Bathing | Take full-body bath or shower, sponge bath, and transfer in and out of tub or shower (excluding washing of back and hair). |
| Dressing | Put on, fasten, and take off all items of street clothing, including donning and removing prosthesis. |
| Grooming | Maintain personal hygiene, including combing hair, brushing teeth, shaving, applying makeup, washing and drying face, hands, and perineum (excludes baths and showers). |
NOTE: ADL definitions are equivalent with those used in the National Resident Assessment Instrument (Morris et al., 1990).
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Multi-State Nursing Home Case-Mix and Quality Demonstration Project, Resident Status Measure, 1990.
For each ADL, limitation was measured in two dimensions, described in Table 2. “ADL performance” indicated the level of self-performance attained by a resident during the most recent 7 days. For example, independent performance was defined by no more than two episodes of help or assistance, weight-bearing support, or full staff performance; or no more than 2 days of supervision or oversight during the past 7 days. Supervision in performance was defined as 3 days or more of supervision, with the occurrence of no more than two episodes of help or assistance, weight-bearing support, or full staff performance. The second measure, “ADL support,” indicated the maximum level of human assistance required by the resident for that ADL over the prior 7 days.
Table 2. Coding Scheme for Dimensions of Activities of Daily Living (ADL) Impairment.
| ADL Function | Definition |
|---|---|
| ADL Performance1 | |
| Independent | No more than two episodes of help or assistance, weight-bearing support, or full staff performance; and/or no more than 2 days of supervision. |
| Supervision | No more than two episodes of help or assistance, weight-bearing support, or full staff performance; and 3 or more days of supervision. |
| Limited Assistance | Three episodes or more of help or assistance, with two episodes or fewer of weight-bearing support or full staff performance. |
| Extensive Assistance | Three episodes or more of weight-bearing support or full staff performance, but not full staff performance during all episodes. |
| Totally Dependent | Full staff performance over the entire prior 7-day period. |
| ADL Support2 | |
| None | No setup or physical help. |
| Setup | Prearrangement of physical environment without assistance in actual performance. |
| One-Person Assist | Physical assistance with performance of task. |
| Two-Person Assist | Physical assistance with performance of task. |
During the past 7 days.
Maximum level required during previous 7 days.
NOTE: ADL definitions are equivalent with those used in the National Resident Assessment Instrument (Morris et al., 1990).
SOURCE: Health Care Financing Administration, Office of Research and Demonstrations: Multi-State Nursing Home Case-Mix and Quality Demonstration Project, 1990.
Analyses
There were two phases of analysis. The first phase reduced the number of ADL limitations under consideration, to avoid unnecessary complexity and redundancy in their measurement. This done, the second phase addressed an efficient summarization of the relevant ADLs.
Previous studies have demonstrated that the use of nursing resources in nursing homes may be explained by the measures of only a few ADLs, because of substantial intercorrelations among ADL functional levels. For example, in the RUG-II case-mix classification system, three (eating, transferring, and toileting) of seven ADLs were sufficient to explain time spent by nursing personnel (Schneider et al., 1988). This finding held, regardless of whether information on ADLs was introduced before or after other clinical information was considered in accounting for residents' nursing cost.
With information on five levels of performance and four levels of support for each of eight ADLs, empirical examination of all possible combinations was not feasible. Therefore, reducing the number of ADLs required some a priori decisions. Bathing was eliminated from analyses, because many nursing homes require staff to assist residents with bathing. Residents in these facilities who were classified as requiring assistance in bathing would not all actually be dependent in bathing. Empirical support for this decision came from the extremely (and artifactually) low frequency of independence in bathing.
We also considered whether other ADLs could be dropped. We focused first on dropping dressing and grooming. This decision was influenced in part by the role of the current analyses as groundwork for RUG-III and their potential incorporation into a payment system. Dressing and grooming are highly subject to reporting bias (intentional or unintentional upgrading of a resident's reported level of limitation). We were therefore reticent to include them; perfunctory and potentially unnecessary levels of assistance could be provided inexpensively to residents, for example, by regularly putting on a bracelet or combing a resident's hair, thereby classifying the resident as dependent.
Although we expected that dressing and grooming were redundant to other ADLs, we were concerned that, to the extent that ADLs are not perfectly related, some information would be lost. Therefore, we began by examining the extent to which information on some ADLs served as indirect measures of others. Analyses were based on the hierarchical structure of ADL limitations (Katz et al., 1963; Kempen and Suurmeijer, 1990; Spector et al., 1987; Travis and McAuley, 1990), in which functional loss in some ADLs generally occurs before functional loss in other ADLs. We determined the extent to which persons with limitations in “late loss” ADLs—those ADLs likely to be lost last in life (eating, bed mobility, transferring, toileting)—were also impaired in “early loss” ADLs (dressing and grooming). Residents who had no limitations in either of the early loss ADLs, but who were impaired in any of the remaining four (late loss) ADLs were defined as “violators.” The percentage of actual violators was compared with that expected if levels of ADL limitation were randomly distributed. Analyses alternatively included and excluded bed mobility and locomotion as late loss ADLs because measures of mobility have generally not been included in previous research on patterns of ADL limitations.
Early loss ADLs and locomotion were assessed further by their incremental impact on explained variance in nursing cost. First, an ANOVA model was formed for predicting nursing cost using the four late loss ADLs: eating, bed mobility, transferring, and toileting. We began with each possible pattern represented by the combination of performance levels for each of the four variables. However, the number of unique patterns found was large (approximately 1,000), making the ANOVA model computationally inappropriate. Therefore, for bed mobility, eating, transferring, and toileting, the performance levels of independent and supervision were combined. To further simplify the computation, each ADL was coded as an interval variable with four levels (1, 2, 3, 4), and the values were summed. Summed values were then treated as separate classes in the ANOVA models. (No significant information was lost through this simplification, because the explained variance achieved using the summed values closely approximated the theoretical maximum-explained variance achieved using each unique combination of ADL levels as a separate class in the ANOVA. The number of classes, however, was dramatically smaller using the summed values.) With this model representing the variance explanation achieved by the four late loss variables, performance measures for locomotion, dressing, and grooming were forced separately into the model, with each considered a categorical variable, and the resulting increment in explained variance was determined.
During our previous work in developing RUG-II (Schneider et al., 1988), many health professionals intuitively felt that three ADLs were too few to account fully for nursing cost, despite the argument of high intercorrelation. As a building block for RUG-III, therefore, we wished to use information from at least four ADLs in explaining nursing cost.
In addition to level of performance of ADLs, information was available on the level of support required (none, setup help, one-, and two-person assist). For each ADL, variables measuring support level were evaluated by comparing explained variance of nursing cost with and without adding information on support level to information on ADL performance level alone. A total of 10 meaningful combinations of ADL performance and support were examined for each ADL. (Ten other combinations are technically possible but illogical; e.g., ADL performance of “limited assistance” combined with “no ADL support.” The proportions of residents with illogical combinations of ADL performance and support were very low—1 percent for bed mobility, transferring, and toileting; and 4 percent for eating. For these residents, levels of support were recoded to the least dependent value consistent with their ADL performance category.) In sum, these analyses led to a subset of the ADLs, combining performance and support measures.
The goal of the second phase of the study was to develop a single summary measure of ADL performance and support that met three criteria: (1) the measure would be relatively easy to quantify and interpret; (2) the measure would result in relatively similar values for residents with similar patterns of ADL limitations; and (3) the measure would meet the requirements of a case-mix payment system. For example, increasing levels of limitation for an ADL (or summary measure of ADL status) may or may not represent similar increases in the amount of time required by nurses to care for a resident. To reflect nursing cost most adequately, a summary measure of ADL limitation should capture these types of associations. Our analyses focused on additive scales, as such summarization would be simple and easy to understand. Further, we expected to use the constructed RUG-III ADL index only to determine categorical ranges, so that its properties as an interval scale were not critical. One desirable property of the coding scheme, however, was that when entered into a linear regression model predicting nursing cost, the resulting mean residual values for each level of ADL limitation would approximate zero. In this way, the assigned numeric values for each level of ADL limitation would most adequately (on average) reflect nursing costs associated with a particular level of function.
As a measure of performance, the explained variance in nursing cost achieved using the RUG-III ADL index was compared with the maximum-explained variance achieved using the four measures of ADL function, in which each unique combination of ADL performance level was considered a separate class in an ANOVA model.
Once completed, the performance of the RUG-III ADL index was compared with two other widely used measures of ADL—the Katz index of ADL (Katz et al., 1970) and the Barthel index (Mahoney and Barthel, 1965). The Katz index includes information on eating, incontinence, transferring, toileting, dressing, and bathing. Residents are assigned one point for each area of dependency, to yield a measure of ADL function ranging from zero (independent) to six (most dependent). The Barthel index includes information on eating, transferring, grooming, toileting, bathing, walking (with a subcategory for wheelchair mobility), ascending and descending stairs, dressing, and incontinence (separately for bowel and bladder). For each activity, points are assigned that can take the values 0, 5,10, or 15, with lower values representing lower levels of performance. Values of the resulting Barthel index (modified as described later) ranged from zero (most dependent) to 90 (independent).
With few exceptions, the Katz and Barthel indexes could be approximated closely using information from items in the assessment instrument. Two items from the Katz or Barthel indexes (incontinence, use of wheelchair) required RSM items other than ADL performance measures. In instances where the precise wording of items was different among instruments, reasonable compromises were possible. For example, the Barthel index classifies residents' dependence in dressing according to whether the individual performs one-half the work of dressing independently, whereas the RSM classifies individuals for these ADLs according to the number (and type) of episodes of help required during a 7-day period. In this case, persons at the dressing performance levels of supervision or limited assistance were assigned Barthel intermediate dependence (requiring some assistance but performing more than one-half the work themselves); persons requiring extensive assistance or totally dependent were classified as Barthel completely dependent (performing less than one-half the work independently). In two instances, no meaningful compromise between instruments was possible. First, face washing is defined in the Barthel index as doing personal toilet but is included in the RSM definition of bathing. The Barthel index item doing personal toilet was nonetheless considered equivalent to the RSM performance item grooming. Second, information on residents' abilities to ascend and descend stairs was not available in the RSM, and was omitted from the emulated Barthel index.2
Our analyses here did not directly consider the effects of resident characteristics other than ADL status on nursing cost. This made possible two undesirable effects. First, nursing needs that are highly correlated with ADL limitations and actually account for nursing cost directly would not be identified. To address this problem, selected analyses were repeated after excluding residents with rehabilitation needs or requiring special medical care (e.g., residents who were comatose, quadriplegic, or undergoing endotracheal tube care). These excluded residents were identified as the first four of the major RUG-III hierarchy categories: Heavy Rehabilitation, Extensive Care, Special Care, and Clinically Complex (Fries et al., 1994). The remaining residents (n = 3,410) were labeled lower hierarchy and conformed to the three remaining major RUG-III categories of Reduced Physical Function, Behavior Problems, and Impaired Cognition. Second, nursing costs associated with caring for conditions that were independent of ADL limitations would not be explained. This, however, was not the goal of the present analysis, but rather was the focus of the work to develop RUG-III, a much more comprehensive classification system for nursing home residents. Nevertheless, the results obtained here, which explicitly account only for ADL factors associated with nursing cost, were likely to be of value, since ADL status accounts for the large majority of explained variance in nursing cost in any classification system.
Statistical Methods
Descriptive statistical methods, ANOVA, and regression modeling were employed in the analysis. The primary measure of the strength of the relationships between patterns of ADL limitations and nursing cost was the proportion of variance in nursing cost that is explained by a pattern of ADL limitations. For some analyses, a version of automatic interactions detection (AID) (Morgan and Sonquist, 1963) was used. In AID, the data points are recursively partitioned into subgroups by a series of splits, each split based on the values of a particular independent variable. For this study, ADLs were the independent variables, the values of which were represented by the levels of performance and/or support for the ADLs. AID searches for partitions that maximize the proportion of explained variance in the dependent variable, and rejects partitions that do not increase this proportion by at least 1 percent. (This criterion, a parallel to the more traditional statistical criterion of p < .05, is traditionally used in applications of AID [Morgan and Sonquist, 1963]). For each set of partitions, AID uses an ANOVA to compute the variance explanations of alternative splits. The advantage of AID is its focus on interaction terms, examining if different variables are important for different groups of residents. The AID classification technique has been used to develop RUGs and diagnosis-related groups (DRGs) for acute hospital patients. For our analysis, an interactive version of AID for personal computers was used (Austin Data Management Associates, 1991). For ADL classification systems that assumed a linear scale, ordinary least squares linear regression was used to determine the explained variance (and residuals performance) of the models.
Initial analyses examining patterns among ADL limitations and explained variance in nursing cost due to individual ADL measures were carried out on a two-thirds random subsample of residents, and later verified on the reserved one-third. Because no significant discrepancies were found between the results for the two samples, the remainder of the analyses were carried out on the entire sample. For clarity, results for all residents are presented here.
Results
The mean age (and standard deviation) of the population was 82.7 (11.4) years. Females comprised 73 percent of the sample. A total of 14 percent of residents were independent, and 21 percent were totally dependent, in the performance of all seven ADLs (bed mobility, eating, toileting, transferring, locomotion, dressing, and grooming). As expected, ADL performance and support levels were substantially correlated. For example, among the 2,226 residents who received only setup help in eating, 89.9 percent were either independent or required supervision in this activity. Conversely, among the 2,882 residents who were totally dependent in transferring, 34.7 percent required one-person support for this activity, and 64.4 percent required two-person support.
ADL Performance Levels
Using AID to examine the relationships between the performance level of each of the seven ADLs (excluding bathing) and nursing costs, variance explanation in nursing costs ranged from a low of 16.4 percent for grooming to a high of 25.2 percent for transferring. For each ADL except eating, AID grouped the ADL performance levels independent and supervision into a single group—i.e., coding them as separate levels did not significantly increase the variance explanation for nursing costs. Residents requiring supervision in eating (8.1 percent of residents) were grouped separately from residents who were independent, and all higher levels of dependence in eating were included in a third group.
Among the lower hierarchy residents, variance explanations for individual ADLs were higher, as expected, ranging from 22.6 percent for bed mobility to 35.1 percent for transferring. For four of the seven ADLs (toileting, locomotion, dressing, and grooming), AID clustered the ADL performance levels independent and supervision together.
These analyses demonstrated that for most ADLs, the nursing costs for residents classified as independent or requiring only supervision were not significantly different. Therefore, independent and supervision were collapsed to a single performance level for each ADL.
Nursing Costs and Individual ADL Items
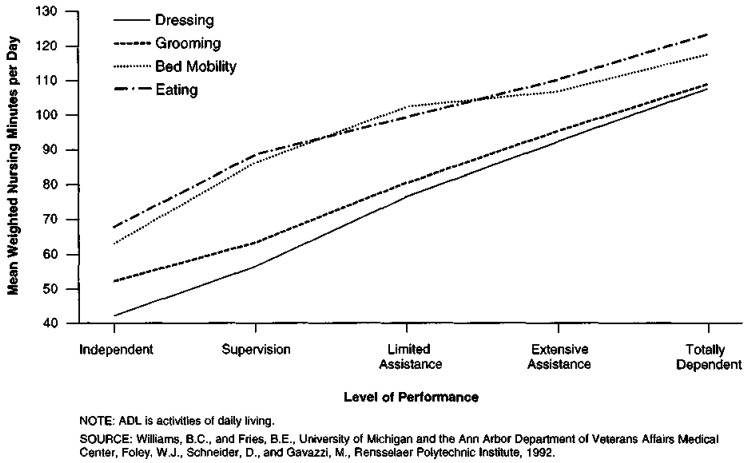
Increasing levels of limitation in ADL self-performance correlated well with increased nursing costs. Figure 1 shows that the mean nursing cost for each ADL increased with increasing levels of limitation in performance. (For simplicity, only four ADLs are shown; similar patterns were observed for the remaining ADLs.)
Figure 1. Mean Nursing Costs for Nursing Home Residents, by Type and Level of ADL Impairment.
Reducing the Number of ADLs
Among all residents, the percent violators of a sequential pattern of functional loss in early and late loss ADLs was fairly low, ranging from 10-25 percent, according to the threshold of dependence chosen (Table 3). Thus, only 10 percent of residents required more than limited assistance in any of eating, bed mobility, transferring, or toileting, and required less than extensive assistance in either dressing or grooming. In contrast, fully 70 percent of residents would be expected to meet these conditions if levels of ADL limitation were randomly distributed. These results also held among lower hierarchy residents, where the percent violators ranged from 9 to 23 percent, depending on the definition of dependence that was applied.
Table 3. Percent “Violators” of Sequential Pattern of Loss of ADL Function, by Individual ADL Performance.
| Individual ADL Performance Level1 | Percent Violators | |||
|---|---|---|---|---|
|
|
|
|||
| More Dependent in at Least One Late Loss ADL2 Than: | More Independent in at Least One Early Loss ADL3 Than: | All Residents (n = 6,359) |
Lower Hierarchy Residents (n = 3,410) |
Expected4 |
| Supervision | Extensive Assistance | 17 | 15 | 75 |
| Limited Assistance | Extensive Assistance | 10 | 9 | 70 |
| Supervision | Total Dependence | 25 | 23 | 44 |
| Limited Assistance | Total Dependence | 18 | 16 | 41 |
ADL performance level is defined as a combination of the two dependence levels.
Bed mobility, eating, transferring, and toileting.
Dressing and grooming.
Percent of residents with given characteristics that would be observed if levels of dependency in the six ADLs were randomly distributed.
NOTES: ADL is activities of daily living. Lower hierarchy residents are those patients in Resource Utilization Groups, Version III major categories Reduced Physical Function, Behavior Problems, or Impaired Cognition.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., and Gavazzi, M., Rensselaer Polytechnic Institute, 1992.
The results shown in Table 3 do not include locomotion as a late loss ADL. Including locomotion among the late loss ADLs increased the percent violators by 10 to 15 percent. Similar results were obtained by altering the definition of locomotion to include wheelchair-bound persons who wheeled themselves. In contrast, the exclusion of bed mobility from the ADL sequence did not substantially alter the percent violators.
These results demonstrated that, with few exceptions, residents with limitations in eating, bed mobility, transferring, or toileting (late loss ADLs) were also limited in dressing and grooming (early loss ADLs). Limitations in locomotion did not fit well as either late or early loss ADLs.
The performance measures for locomotion, dressing, or grooming did not substantially improve the amount of explained variance in nursing cost after accounting for performance levels for eating, bed mobility, transferring, and toileting (Table 4). In each case, explained variance increased by less than 1 percent. This finding was consistent among lower hierarchy residents.
Table 4. Incremental Effects of Measures of ADL Performance on Explained Variance in Weighted Nursing Time.
| ADL | Percent Explained Variance | |
|---|---|---|
|
| ||
| All Residents (n = 6,359) |
Lower Hierarchy Residents (n = 3,410) |
|
| Late Loss ADLs1 | 29.0 | 38.7 |
| Late Loss ADLs and Locomotion | 29.5 | 39.4 |
| Late Loss ADLs and Dressing | 29.4 | 39.3 |
| Late Loss ADLs and Grooming | 29.5 | 39.0 |
Late loss ADLs are: eating, bed mobility, transferring, and toileting.
NOTES: ADL is activities of daily living. Lower hierarchy residents are those patients in Resource Utilization Groups, Version III major categories Reduced Physical Function, Behavior Problems, or Impaired Cognition.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., and Gavazzi, M., Rensselaer Polytechnic Institute, 1993.
Nursing Costs and ADL Support
Among persons totally dependent or requiring extensive assistance in bed mobility, toileting, or transferring, AID consistently separated two-person assistance from other levels of support. The single exception was that persons requiring one-person support versus two-person support were grouped together for persons requiring extensive assistance in transferring. These relationships are shown in Table 5, which lists the mean nursing cost among persons who were most dependent in bed mobility, transferring, and toileting, by performance and support levels, along with information on statistically significant differences among groups. AID did not distinguish between one- and two-person support for eating, because few residents required two-person assistance for this ADL. Including information on ADL support increased variance explanation in nursing cost 1 to 4 percent over measures of ADL performance alone.
Table 5. Mean Weighted Nursing Minutes1 for Selected Activities of Daily Living (ADLs) and Performance Levels.
| ADL | ADL Support2 | |||
|---|---|---|---|---|
|
| ||||
| One-Person Assist | Two-Person Assist | |||
|
|
|
|||
| Extensive Assistance in ADL Performance | Total Dependence in ADL Performance | Extensive Assistance in ADL Performance | Total Dependence in ADL Performance | |
| Bed Mobility | 105.7 | 107.7 | 118.6 | 132.1 |
|
|
|
|
||
| Transferring | 98.4 | 95.7 | 109.2 | 123.8 |
|
|
|
|||
| Toileting | 95.9 | 104.2 | 107.2 | 124.0 |
|
|
|
|||
Total resident-specific nursing time per day, weighted by relative pay scales by type of nurse (registered nurse, licensed practical nurse, or nurse aide).
Groups not statistically distinguishable (p < .05) in accounting for nursing cost are underlined together.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., and Gavazzi, M., Rensselaer Polytechnic Institute, 1993.
During earlier work to develop the RUG-II case-mix classification system for nursing home residents, nursing advisory panels had strongly advocated separating persons requiring one- and two-person support into different groups. Grouping residents who require similar numbers of supportive helpers was thought important for informing nursing allocation decisions, regardless of the incremental explained variance resulting from distinguishing these two types of residents. Thus, although distinguishing levels of ADL support contributed little to explaining overall variance in nursing cost, it seemed important to include this distinction of two-person assistance for persons at the most dependent levels of bed mobility, transferring, or toileting. Therefore, for persons at either of the two most dependent levels of performance (totally dependent or requiring extensive assistance) for these three ADLs, one- and two-person assistance were distinguished.
The result of the first phase of analysis was to restrict our attention to four ADLs, combining information on self-performance and support for each as shown in Table 6.
Table 6. Resource Utilization Groups, Version III Activities of Daily Living (ADL) Index1.
| ADLs and Variables | Score |
|---|---|
| Bed Mobility, Toileting, and Transferring | |
| Independent or Supervision | 1 |
| Limited Assistance | 3 |
| Extensive Assistance or Total Dependence: | |
| One-Person Assist | 4 |
| Two-Person or More Assist | 5 |
| Eating | |
| Independent or Supervision | 1 |
| Limited Assistance | 2 |
| Extensive Assistance or Total Dependence (Including Feeding Tubes or Parenteral Feeding) |
3 |
Sum of the scores for the four ADL variables. Index ranges from 4-18.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., and Gavazzi, M., Rensselaer Polytechnic Institute, 1992.
Summary ADL Index
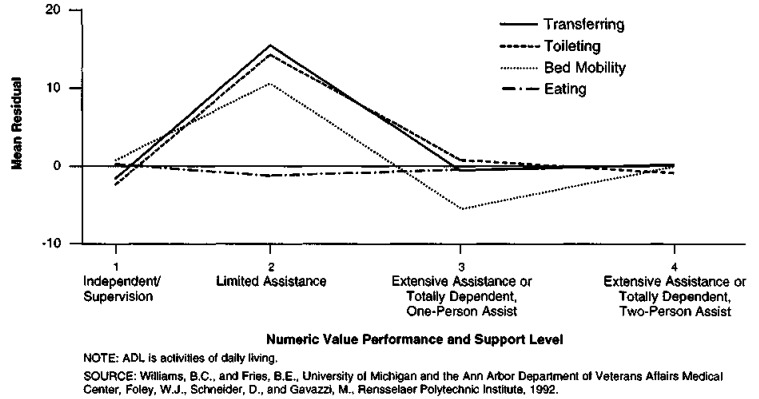
In developing an additive summary measure of ADL limitations, the simplest scheme was to code each level of ADL limitation as integers (i.e., coding levels of eating limitation as 1, 2, 3; and the remaining three ADLs as 1, 2, 3, 4). Using this approach, from 17 percent (for eating) to 27 percent (for transferring) of the variance in nursing cost was explained by individual ADLs. However, this coding scheme resulted in a large positive mean residual for bed mobility, transferring, and toileting at the second level of limitation (numeric value 2; limited assistance) when ADL level was regressed on nursing cost (Figure 2). That is, the average nursing cost among persons at the second level of ADL limitation was substantially more than twice that of persons at the first level of limitation (independent or supervision), contrary to the assumption made in assigning numeric values of 1 and 2 to the first and second levels of limitation, respectively. Alternative additive schemes, in which the numerical values representing limitation levels at or higher than the second level for bed mobility, transferring, and toileting were increased, performed significantly better than the strictly linear coding system. The best of these systems coded successive levels of limitation for bed mobility, transferring, and toileting as 1, 3, 4, 5 (Table 6). The resulting residual plots were significantly improved, with mean residual values closer to zero for each level of ADL limitation than alternative schemes. The final coding scheme, the RUG-III ADL index, is described in Table 6. Although further analysis might have identified yet superior weightings, the relatively simple scheme represented here made clinical sense and was deemed sufficient, especially given that the ADL index was to be used only within ranges and not as a truly numeric variable.
Figure 2. Mean Residuals Regressing ADL Limitation on Weighted Nursing Minutes, by Numerical Value of Performance and Support Level (n = 6,385).
In the RUG-III ADL index, scores for each of the four late loss ADLs are summed, resulting in values from 4 to 18. Using AID, this composite variable explained 28 percent of the variance in nursing cost among all residents. This compared favorably with the theoretical maximum-explained variance (31 percent) obtained by coding the four ADL measures as separate categorical variables in an ANOVA. Three groups were formed, consisting of residents whose index values were 4-7, 8-15, and 16-18, respectively. The index values, mean weighted nursing minutes, and standard deviations for the three groups are shown in Table 7. Among lower hierarchy residents, the RUG-III ADL index explained 36 percent of the variance in nursing cost. The groupings by RUG-III ADL index level among lower hierarchy residents were identical to those among all residents, except that the least impaired group was subdivided into two groups that included levels 4-5 and 6-7, respectively.
Table 7. Mean Nursing Costs, by RUG-III ADL Index Groups1.
| Group | RUG-III ADL Index Values | Mean Weighted Nursing Minutes2 | Standard Deviation |
|---|---|---|---|
| 1 | 4-7 | 49 | 36 |
| 2 | 8-15 | 98 | 49 |
| 3 | 16-18 | 127 | 62 |
Groups were identified using automatic interactions detection, and explained 28.4 percent of the variance in weighted nursing minutes.
Total resident-specific nursing minutes per day, weighted by relative pay scales by type of nurse (registered nurse, licensed practical nurse, or nurse aide).
NOTES: RUG-III is Resource Utilization Groups, Version III. ADL is activities of daily living.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., Gavazzi, M., Rensselaer Polytechnic Institute, 1992.
Comparative Performance of RUG-III ADL Index
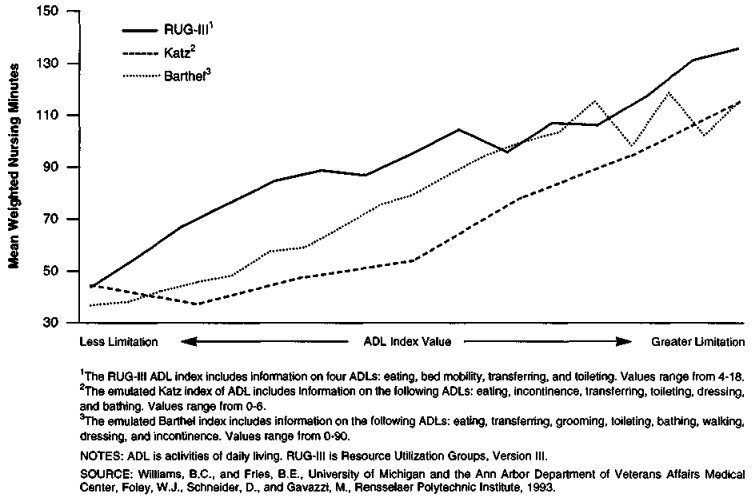
As expected, mean weighted nursing minutes increased with increasing levels of dependency for the RUG-III ADL index and the emulated Katz and Barthel indexes (Figure 3). The proportion of variance in weighted nursing minutes, explained by each index of ADL limitation when coded as a continuous variable and entered into a linear model, is shown in Table 8. Among all residents, the RUG-III ADL, Katz, and Barthel indexes explained 30, 24, and 26 percent of the variance in nursing cost, respectively. Among lower hierarchy residents, explained variance was 37 percent for the RUG-III ADL index, 35 percent for the Katz index, and 39 percent for the Barthel index.
Figure 3. Mean Weighted Nursing Minutes, by Level of ADL Limitation: 3 ADL Indexes.
Table 8. Explained Variance (R2) in Weighted Nursing Minutes, by ADL Index1.
| ADL Index | Percent Explained Variance | |
|---|---|---|
|
| ||
| All Residents (n = 6,373) |
Lower Hierarchy Residents (n = 3,410) |
|
| RUG-III ADL Index2 | 29.8 | 37.3 |
| Katz Index of ADL3 | 24.5 | 34.6 |
| Barthel Index4 | 26.5 | 39.5 |
Results from linear regression coding each index as continuous variable.
The RUG-III ADL index includes four categories: eating, bed mobility, transferring, and toileting.
Emulated using items from the Health Care Financing Administration (HCFA) Resident Status Measure (RSM). The emulated Katz index of ADL includes the following ADLs: eating, incontinence, transferring, toileting, dressing, and bathing.
Emulated using items from the HCFA RSM. The emulated Barthel index includes the following ADLs: eating, transferring, grooming, toileting, bathing, walking, dressing, and incontinence.
NOTES: ADL is activities of daily living. RUG-III is Resource Utilization Groups, Version III. Lower hierarchy residents are those patients in RUG-III major categories Reduced Physical Function, Behavior Problems, or Impaired Cognition.
SOURCE: Williams, B.C., and Fries, B.E., University of Michigan and the Ann Arbor Department of Veterans Affairs Medical Center, Foley, W.J., Schneider, D., and Gavazzi, M., Rensselaer Polytechnic Institute, 1993.
Discussion
The RUG-III ADL index is an easily determined summary measure of ADL limitation that corresponds well to directly measured wage-weighted nursing time among nursing home residents. Four ADLs—eating, bed mobility, transferring, and toileting—were used to create a weighted index that accounted for 30 percent of the variance in nursing cost among all residents, and 37 percent of the variance in nursing cost among residents without special nursing needs. The index performed comparably to or slightly better than two alternative measures that include information on a larger number of ADLs. It is thus likely that any measure of ADL limitations that is reasonably comprehensive and reliable will capture important distinctions in nursing costs among nursing home residents. The RUG-III ADL index, however, has several advantages over other available measures of ADL function. First, it is based on information taken directly from the MDS, which is now widely and routinely applied in nursing homes throughout the country. Second, it includes relatively few measures of ADL limitation, and so is relatively easy to determine. Finally, the RUG-III ADL index has been shown to correspond well to actual measurements of nursing time among nursing home residents.
The use of nursing resources among nursing home residents was largely accounted for by measuring resident performance in four late loss ADLs (eating, transferring, bed mobility, and toileting), without direct measurement of other ADLs (e.g., dressing and grooming). The sensibility of this approach was verified by the relatively low proportions of residents who were significantly impaired in dressing or grooming without substantial limitation in performance of all the late loss ADLs. By eliminating dressing and grooming from an account of ADL limitations, it is theoretically possible that nursing cost will be underestimated among the subgroup of residents with only mild limitations in dressing and grooming, but no limitations in late loss ADLs. The goal of this study, however, was to provide a simple measure of ADL status that would be applicable to the majority of residents. This possibility was examined in more detail in developing the RUG-III case-mix classification system, in which underestimating nursing cost among specific groups of residents is important. In the RUG-III development, explicitly including information on dressing and grooming among light-care residents did not substantially improve the ability to predict nursing costs beyond those obtained using other resident characteristics (Fries et al., 1994).
In discussions with nurses and aides during the development of the RUG-III case-mix classification system, supervision was reported to require substantial amounts of nursing time. The common perception was that time spent “standing by” in case a resident required help resulted in less time available for other duties. These results suggest, however, that low-level assistance is generally performed while carrying out other duties related to higher level ADL dependencies, and does not independently require substantial amounts of nursing resources.
Staff allocation decisions among residents at the most dependent levels of ADL performance will be affected by the need for a second person to assist in performance of the activity. The RUG-III ADL index captures this effect by directly accounting for the requirement for two-person versus one-person support among persons totally dependent or requiring extensive assistance in bed mobility, toileting, or transferring.
Among residents without specialized nursing or rehabilitation needs—the lower hierarchy residents—information on bed mobility, eating, toileting, and transferring explained greater amounts of variance in nursing cost than among all residents (38 versus 29 percent). Including further information here on limitations in other ADLs did not substantially increase explained variance. Furthermore, the relationships among ADL limitations were similar in the lower hierarchy and other residents. This was important for two reasons. First, it suggests that the demonstrated relationships between ADL limitations and nursing costs are unlikely to be confounded—that is, because of other nursing- or rehabilitation-related characteristics that are associated with ADL limitations. Second, among residents who have specialized nursing or rehabilitation needs, it may be important to account separately for particular nursing needs in addition to ADL limitations in predicting nursing costs. Among residents whose needs are primarily due to functional limitations, important differences in nursing costs may be determined using information on ADLs alone.
Conclusions
Our findings are consistent with, and substantially extend, previous research examining the relationships of ADL limitation with the use of nursing resources among nursing home residents. Although prior studies to develop alternative case-mix classification systems for nursing home residents have uniformly demonstrated a strong relationship between ADL limitations and the use of nursing resources, this article has examined in further detail the intricate relationships of ADL limitations and the use of nursing resources.
A potential limitation of this article is that the sample population was selected to over-represent heavy-care residents, and is therefore not representative of all nursing home residents. This bias has likely augmented our ability to study the full range of patterns of ADL limitations across residents and should not affect the analysis of the relationships between nursing resources and patterns of ADL limitations. Still, readers should take care in interpreting any reports of raw frequencies.
A primary application of the RUG-III ADL index will be as a building block for the RUG-III case-mix classification system. However, the RUG-III ADL index has two other applications—informing nursing resource allocation decisions and facilitating comparisons of the ADL status of individual or groups of nursing home residents.
Quantitative understanding of the relationship between nursing needs and patient characteristics can be useful for several types of decisions in nursing resource allocation, such as budget planning and tracking, contract negotiations, and risk reduction (Giovannetti and Johnson, 1990); and determining optimal staff mix (i.e., aides, LPNs, RNs) and daily or shift-based patient assignments to nursing staff (Cavaiola and Young, 1980). To our knowledge, only a few previous studies have directly addressed decisionmaking regarding nursing resource allocation in nursing homes based on resident characteristics (Fries, 1990). However, previous studies have generally estimated nursing resource use by aggregating task-specific time across a number of characteristics for each resident (e.g., Cavaiola and Young, 1980; Morris et al., 1987), rather than using directly measured resident-specific time, which provides a more accurate view of nursing time actually spent with residents.
The increasing availability of detailed information regarding nursing home residents will make it possible to compare the status of residents over time and with each other. The RUG-III ADL index can provide a meaningful summary of one dimension—functional status—of residents for such comparisons. For example, the proportions of residents in each of the three RUG-III ADL index groups (perhaps combined with information on other dimensions of resident status, such as the proportion of residents receiving rehabilitation services and other special therapies) could be used as a measure of the severity of illness among residents of different facilities or groups of facilities, or to identify significant functional decline among individuals or groups of residents over time. As such, a summary ADL index is a critical component of outcomes research, either directly or as a covariate to control for differences in functional status among residents.
An additional byproduct of the analyses presented here is increased information on the patterns of ADL function across the eight available ADLs, which will allow screening groups of MDS reports for poor data quality. Our experience with the MDS, as with previous assessment instruments, has shown that, while many combinations of levels are technically and logically feasible, it is possible to identify extremely unlikely patterns (e.g., dependence in late loss ADLs with independence in early loss ADLs). A group of assessments—for example, all those from a particular facility—with a number of residents' assessments containing unlikely combinations may indicate poor assessment, poor training, or inappropriate data manipulation.
Acknowledgments
The authors gratefully acknowledge the conceptual and technical advice of our HCFA Project Officer, Elizabeth Cornelius, as well as that of Robert Burke and David Mehr; and the assistance of Clare Weipert in preparing the manuscript.
The research presented in this article was supported in part by Cooperative Agreement Number 500-89-0046 with the Health Care Financing Administration (HCFA). Brent C. Williams is with the Department of Internal Medicine, University of Michigan Medical Center and the Geriatric Research, Education, and Clinical Center, Ann Arbor Department of Veterans Affairs Medical Center. Brant E. Fries is with the Institute of Gerontology, School of Public Health, University of Michigan and the Geriatric Research, Education, and Clinical Center, Ann Arbor Department of Veterans Affairs Medical Center. William J. Foley, Don Schneider, and Marie Gavazzi are with the Department of Decision Sciences and Engineering Systems, Rensselaer Polytechnic Institute. The opinions are those of the authors and do not represent official policy of HCFA, the University of Michigan, the U.S. Department of Veterans Affairs, or Rensselaer Polytechnic Institute.
Footnotes
Additional data from New York State were included for the final version of RUG-III, but were not initially available for these analyses.
Coding schemes for the emulated Katz and Barthel indexes are available upon request from the authors.
Reprint Requests: Brent C. Williams, M.D., M.P.H., University of Michigan Medical Center, Department of Internal Medicine, 3116 Taubman Center, Ann Arbor, Michigan 48109-0376
References
- Arling G, Nordquist RH, Brant BA, Capitman JA. Nursing Home Case Mix: Patient Classification by Nursing Resource Use. Medical Care. 1987 Jan;25(1):9–19. doi: 10.1097/00005650-198701000-00002. [DOI] [PubMed] [Google Scholar]
- Austin Data Management Associates. PC-Group. Austin, Texas: 1991. [Google Scholar]
- Cameron JM. Case Mix and Resource Use in Long-Term Care. Medical Care. 1985 Apr;23(4):296–309. doi: 10.1097/00005650-198504000-00002. [DOI] [PubMed] [Google Scholar]
- Cavaiola LJ, Young JP. An Integrated System for Patient Assessment and Classification and Nurse Staff Allocation for Long Term Care Facilities. Health Services Research. 1980;15(3):281–306. [PMC free article] [PubMed] [Google Scholar]
- Fries BE. Comparing Case-Mix Systems for Nursing Home Payment. Health Care Financing Review. 1990 Summer;11(4):103–119. [PMC free article] [PubMed] [Google Scholar]
- Fries BE, Schneider DP, Foley WJ, et al. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32:668–685. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Fries BE, Schneider DP, Foley WJ, Dowling M. Case-Mix Classification of Medicare Residents in Skilled Nursing Facilities: Resource Utilization Groups (RUG-T18) Medical Care. 1989 Sep;27(9):843–858. doi: 10.1097/00005650-198909000-00001. [DOI] [PubMed] [Google Scholar]
- Giovannetti P, Johnson JM. A New Generation Patient Classification System. Journal of Nursing Administration. 1990 May;20(5):33–40. [PubMed] [Google Scholar]
- Hawes C, Phillips CD, Mor V, et al. MDS Data Should be Used for Research. The Gerontologist. 1992;32:563–64. doi: 10.1093/geront/32.4.563b. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, et al. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. Journal of the American Medical Association. 1963 Sep;195(2):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in Development of the Index of ADL. The Gerontologist. 1970 Spring;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Kempen GI, Suurmeijer TP. The Development of a Hierarchical Polychotomous ADL-IADL Scale for Noninstitutionalized Elders. The Gerontologist. 1990;30(4):497–502. doi: 10.1093/geront/30.4.497. [DOI] [PubMed] [Google Scholar]
- Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Maryland State Medical Journal. 1965 Feb;14:61–65. [PubMed] [Google Scholar]
- Minnesota Department of Health. Facility Manual for Completing Case Mix Requests for Classification. Minneapolis: May, 1986. Unpublished manual. [Google Scholar]
- Morgan JN, Sonquist JA. Problems in the Analysis of Survey Data and a Proposal. Journal of the American Statistical Association. 1963 Jun;58(302):415–434. [Google Scholar]
- Morris JN, Hawes C, Fries BE, et al. Designing the National Resident Assessment Instrument for Nursing Homes. The Gerontologist. 1990 Jun;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- Morris JN, Hawes C, Murphy K, et al. Resident Assessment Instrument Training Manual and Resource Guide. Natick, Massachusetts: Eliot Press; 1991. [Google Scholar]
- Morris JN, Sherwood S, May MI, Bernstein E. FRED: An Innovative Approach to Nursing Home Level-of-Care Assignments. Health Services Research. 1987 Apr;22(1):117–138. [PMC free article] [PubMed] [Google Scholar]
- Schneider DP, Fries BE, Foley WJ, et al. Health Care Financing Review. 1988 Annual Supplement. Dec, 1988. Case Mix for Nursing Home Payment: Resource Utilization Groups, Version II; pp. 39–52. [PMC free article] [PubMed] [Google Scholar]
- Spector WD, Katz S, Murphy JB, Fulton JP. The Hierarchical Relationship Between Activities of Daily Living and Instrumental Activities of Daily Living. Journal of Chronic Disease. 1987;40(6):481–489. doi: 10.1016/0021-9681(87)90004-x. [DOI] [PubMed] [Google Scholar]
- Travis SS, McAuley WJ. Simple Counts of the Number of Basic ADL Dependencies for Long-Term Care Research and Practice. HSR: Health Services Research. 1990 Jun;25(2):349–360. [PMC free article] [PubMed] [Google Scholar]