Abstract
Implementing a per-episode prospective payment system (PPS) for home health services is one option for Medicare policy makers facing rapid increases in service use and expenditures. Analysis of data on recent episodes of Medicare home health care identified systematic differences in service patterns across provider types; these indicate potential differences in the capacity of agencies of different types to adjust to PPS. The second phase of a national demonstration, which is about to be implemented, will provide information on the extent to which the agency practices that generate much of the observed variation (such as the number of visits provided per episode) are susceptible to management decisions; and whether managers can and do respond to the incentives of per-episode prospective payment.
Introduction
Rapid increases in expenditures for home health services under the Medicare program provide the Health Care Financing Administration (HCFA) with a motivation to evaluate alternatives to the current system of cost-based reimbursement. This system provides few incentives for providers to deliver services in an efficient manner or to limit increases in costs. A PPS is one alternative payment approach that can provide such incentives. It is also one that Congress has mandated (Omnibus Budget Reconciliation Act of 1987) for consideration as an alternative for the Medicare program.
There are a number of possible approaches to prospective payment for home health care. Payments can be set prospectively for each visit provided, each month of care, each episode of care, or each month of program enrollment, for example. Each of these approaches cedes differing amounts of control (and provides different incentives) to providers. When prospective rates are set per visit, the provider has an incentive to provide that visit at lower cost in order to retain the difference between cost and rate as profit (or surplus). However, the payer, not the provider, is at risk for increases in the number of visits. Therefore, the payer has the incentive to monitor service use and is likely to assess each visit for eligibility and coverage in order to assure that it pays only for those visits for which it has an obligation to pay. When rates are set for units of service larger than a visit, e.g., an episode of care, the risks for increases in cost per visit and increases in the number of visits are shifted to the provider, and the payer need worry only about the number of episodes of care (i.e., admissions). The payer's review of the coverage of individual visits is likely to decrease, whereas the confirmation of the appropriateness of each admission is likely to intensify.
Under the National Home Health Agency Prospective Payment Demonstration, two of these alternatives are being tested. The demonstration, which began operation in 1990, is enrolling Medicare-certified agencies in five States (California, Florida, Illinois, Massachusetts, and Texas) and using a randomized treatment-control design to measure the impacts of PPS on home health agency (HHA) operations, organization, and finances. The demonstration is being implemented in two phases: Phase I has been testing a system where payment rates are set on a per visit basis; and Phase II, to begin in 1995, will test a system where rates are set for each episode of care provided.
Participation in the demonstration is voluntary, but it is hoped that the findings will be generalizable to the universe of Medicare home health providers. Therefore, steps have been taken to encourage participation by a broad range of agencies. Payment rates are set for each participating agency based on its own historical costs, so neither high-cost nor low-cost agencies are at a disadvantage. Participants' risk is further mitigated by stop-loss provisions that limit agencies' financial liability for costs that exceed the prospective payment rates. Finally, under the per episode phase of the demonstration, an algorithm will be implemented to adjust the payment rate for significant changes in a participating agency's case mix (relative to the time period on which its payment rate was based).
Even with such protection in place, however, it would be prudent to attempt to gain an understanding of how implementing per episode payment as a demonstration, let alone as policy, is likely to affect participating HHAs, and whether the impacts will differ systematically across definable types of agencies. Systematic differences in current patterns of utilization would place agencies of different types at different baseline points relative to the new payment approach. Although considerable variation in the pattern of gross Medicare home health service utilization across areas (Benjamin, 1986; Bishop and Skwara, 1993; Kenney, 1993) and types of patients (Branch et al., 1993) has been documented, no previous studies have used the demonstration's definition of the episode of care, or worked with data on such recent (1992-93) utilization.
The definition of an episode of home health care is not a straightforward matter. Unlike inpatient hospital care, where the stay is readily defined by the patient's continuous presence in the facility, home care is generally provided on an intermittent basis in the patient's home. For instance, a patient can receive a single visit every 30 to 45 days for a catheter change, receive no home health care in the interim, and still be considered an “active” patient on an agency's caseload. Although Medicare billing practices provide for the submission of separate admission and discharge bills for the beginning and ending of episodes of home care, agencies are not consistent in their use. For the implementation of the demonstration, therefore, we have chosen to define the episode as a fixed length of time following admission. The analysis presented here applies the demonstration's definition of an episode to the most recent available data on Medicare utilization, developing a simulated profile of utilization in terms of that episode definition. We attempted to answer the following questions:
On average, what proportion of services provided falls within the episode under the demonstration's definition? What proportion is provided outside the episode period?
What are the differences in current utilization patterns across agencies of different types (e.g., urban versus rural; voluntary/non-profit versus proprietary; or facility-based versus freestanding) with respect to the demonstration episode?
Are any observed systematic differences in baseline utilization patterns likely to be correlated with differences in response to the PPS incentives of the demonstration and, potentially, a PPS program?
We present descriptive statistics in the aggregate for episodes provided by agencies with specific characteristics, identifying statistically significant differences in practice patterns. This discussion is followed by the results of a multivariate analysis that seeks to isolate the relative contribution of individual agency characteristics to interagency differences by controlling for variation along multiple dimensions. Finally, we speculate on the potential significance of observed variation in current utilization for predicting potential behavior under the demonstration.
Data and Methods
Background: The Medicare Home Health Benefit
Medicare provides coverage for home health services under both Part A and Part B. If a beneficiary is eligible under both, the services are always provided under Part A To be eligible for services, the beneficiary:
Must be confined to his or her residence (“homebound”);
Must be under the care of a physician, who establishes and approves the plan of care and recertifies any continuing need for services at least every 2 months;
Must need part-time (fewer than 8 hours a day) or intermittent (4 or fewer days per week) skilled services, such as skilled nursing, physical therapy, or speech therapy services. (Service levels in excess of the part-time and intermittency criteria may be provided for temporary periods of time up to 21 days, or longer in exceptional circumstances, as long as the need for such levels of care is “finite and predictable.”)
If the beneficiary meets these eligibility criteria, additional services (occupational therapy, medical social services, home health aide services, medical supplies, and durable medical equipment) may also be provided.
Currently, Medicare reimburses participating HHAs for the reasonable costs incurred to provide covered visits to eligible beneficiaries up to cost caps established for each area of the country. Costs are calculated by each provider using the Home Health Agency Cost Report (HCFA Form-1728), which the provider submits to one of HCFA's nine contracted Regional Home Health Intermediaries (RHHIs) after the end of its fiscal year. RHHI staff review the Cost Report, assessing the costs allocated to Medicare for allowability under Medicare's guidelines, perform a desk audit and, potentially, an onsite audit of the provider's records. Before the final settlement and Notice of Program Reimbursement is issued, the RHHI may issue a tentative settlement and the provider may provide additional documentation to support claimed costs. Generally, within 18 months to 2 years after the end of the fiscal year, the provider will be informed of its final Medicare reimbursement for the year. In some cases, however, settlements of the Cost Report and resolution of subsequent appeals by the provider have been known to take 5 years or longer.
The burden of recordkeeping and reporting and the uncertainty surrounding final reimbursement for services provided are two of the major aspects of the Medicare home health program that providers find onerous. Under a PPS, cost reporting would (in theory) no longer be required because reimbursement would be based on prospectively set rates, not on costs as determined by the RHHI. In addition, the amount of payment would be known at the time the service is being provided, not several years after the service was provided and the costs incurred. These aspects of PPS make it very attractive to providers as well as to Medicare program managers. However, the fact that payment is not based on costs incurred means that payment could be higher than actual costs, generating a profit or surplus for the provider and costs to the payer higher than those under cost reimbursement; the converse (a loss for the provider and savings for the payer) would occur when payment is lower than costs incurred. This risk, as well the uncertainty surrounding any major program change, has created some hesitancy among providers and HCFA to move rapidly to a PPS system for home health. The demonstration seeks to reduce this uncertainty by providing information to help predict the impacts of an eventual ongoing PPS program.
Data
The utilization data used for this analysis were taken from home health claims obtained from HCFA's Standard Analytic File (SAF) system. Data for home health services delivered from January 1989 forward were obtained in February 1994 and included relatively complete information for services provided through September 1993. However, this data set contains the following inherent limitations:
Episodes in process at the end of the data coverage period (September 1993) are truncated.
Data from Medicare home health claims do not include actual dates for each service. Most agencies bill by calendar month, and the bill records in HCFA's data files contain only the aggregate number of visits by discipline. When arraying visits over time for the purposes of defining episodes, for this analysis, services were allocated evenly over the period between the “from” and “through” dates of each bill. This resulted in estimates of fractions of visits per episode and may have had the effect of artificially prolonging some episodes to the end of the calendar month.
Ideally, one would choose cost per episode as the measure of interest. However, given the current system of cost reimbursement, the actual cost of a home health visit is not determined until months later when the agency's Medicare Cost Report is settled. Charges more often reflect agency behavior toward other payers and, in many cases, are known to bear limited relation to expected Medicare payment to the agency for home health care. Therefore, we have used reimbursement (which is available from the claims) as a proxy for costs in these analyses. Reimbursement per visit is typically computed from a recently submitted Cost Report or Periodic Interim Payment report submitted by the agency.
The data on agency characteristics (certification/termination date, auspice, location, fiscal intermediary) were obtained from the Provider of Service (POS) file maintained by HCFA's Health Standards and Quality Bureau. A few beneficiary variables (age, gender, race, county of residence) were obtained from HCFA's Health Insurance Skeleton Eligibility Writeoff (HISKEW) file and appended to the record for each episode. In addition, primary diagnosis, as recorded on the first and last bill of each episode, was retained, but the individual International Classification of Diseases, 9th Revision, Clinical Modification codes were classified into 44 categories based on the body system affected.
Defining the Episode
For the demonstration, an episode of care will be defined as all services delivered during a period of 120 days following the initial admission of a beneficiary to Medicare home health care at a demonstration provider. Even if there is a gap in service during the 120 days (e.g., services are provided from day 1 to day 30 and then from day 100 to day 120), all will be considered to be part of a single episode. If services are still being provided at day 121 following admission, they will be considered to be related to the episode and will be paid on an “outlier” basis, i.e., at prospectively set per visit rates. The outlier portion of the episode will continue until there is a gap of 45 days during which no services are provided; any services delivered after a 45-day gap will be considered to start a new episode.
To apply this definition retrospectively to the claims data, each episode of care was defined as a spell of services provided to a single beneficiary by a single provider during 120 days following an admission to home health care. Claims were sorted by provider, beneficiary, and service dates. The first “from date” in calendar year 1992 was located. From there, the preceding 45 days were reviewed. If there was a service during this period, the episode was defined as a “phase-in” episode that was considered to continue until a 45-day gap in service was detected. If no phase-in episode was present, the first from-date was considered the beginning of an episode that was assumed to continue for at least 120 days. Beyond day 120, the first 45-day gap in services terminated the episode. Any services that occurred after day 120 but before such a gap were considered outlier visits related to the episode. If there were no visits between day 120 and day 165, any subsequent visits were considered to begin a new episode.
This definition of the episode is, admittedly, arbitrary. However, it was chosen for the demonstration because it is straightforward and easy to understand, providing clear and understandable incentives to agency administrators, and it supports modeling to predict the level of resource use (which are necessary if an algorithm for rate adjustments in response to changes in agency case mix is to be implemented, as under this demonstration.) Although episodes based on more clinically meaningful dimensions (such as “all care for a specific diagnosis”) were considered, they were felt to be too subjective for use here given that many Medicare home care beneficiaries have multiple diagnoses and the approach to assigning their priority on Medicare home health claims is not consistent across agencies. Using inpatient admissions when they occur during a period of home health care use to delimit an episode is another potential approach. This would also represent some change from current practice, because some agencies now discharge beneficiaries who are admitted to the hospital and readmit them to home care when they return home; others choose to keep their hospitalized beneficiaries on their active caseload while they are in the hospital and resume home care upon discharge from the hospital, reassessing the patients but not readmitting them. In addition, work conducted for HCFA (Phillips et al., 1992) using hospital stays of 3 days or more to delimit episodes of Medicare home health care found that using such a definition yielded only a very small increase in the accuracy of models that could be developed to predict the level of resources consumed.1 Such an approach may also introduce an undesirable incentive to agencies to maximize inpatient admissions among their patients.
To put the estimates developed here in perspective, it would, of course, be desirable to conduct full-blown sensitivity analyses in order to measure the impacts of using these alternative approaches to defining the episode. Although this was not possible, some incidental analyses that were performed suggest that the potential for major differences is limited.
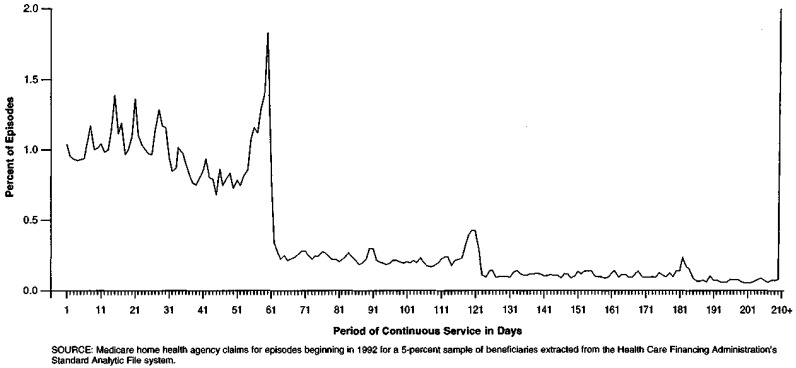
The first analysis looked at the actual continuous span of service (until a 45-day gap) without reference to the 120-day window. Figure 1 shows the distribution of episode end dates computed in this manner: a relatively smooth, though stepped, distribution with peaks every 60 days.2 This suggests that using a multiple of 60 days as the episode cutoff is the most reasonable approach.
Figure 1. Distribution of Episodes, by Period of Continuous Service in Days: Medicare Home Health Utilization, 1992.
A second perspective is provided by a few relevant statistics that were obtained while conducting preliminary analyses for defining episodes using a subsample of the claims data. We conducted a rough sensitivity analysis using alternative episode lengths and gaps and noted the impact on the number of episodes constructed. Given that a fixed pool of bills, visits, and costs were being allocated to episodes, a change in the number of episodes created would seem to serve as a reasonable proxy for changes in those measures. Using an episode length of 180 days rather than 120 days resulted in a 2.1-percent reduction in the number of episodes constructed, which caused a corresponding increase in the average visits and cost per episode. Preserving the length of 120 days but using a gap of 60 days rather than 45 days to define a new episode resulted in a 1.4-percent reduction in the number of episodes constructed; making both changes (180-day length and 60-day gap) resulted in a net reduction of 3.2 percent in the number of episodes. This should serve as an upper bound on the scope of the changes one would expect to see if these episode parameters were modified.
A third analysis examined visit “gaps” embedded in the episodes that had been defined as a period of 120 days following admission plus any outlier services from day 121 until a 45-day gap in services. Approximately 3.3 percent of these episodes included two periods of continuous service separated by a gap of 60 days or more without visits. This indicates the order of magnitude for the number of additional episodes that would have been created if we had used 60-day gaps in service rather than a fixed length of time following admission to define the episode.
Finally, we examined diagnostic category at the start and at the end of the episode to ascertain the frequency with which services being delivered under the final claim of the episode were for a medical condition unrelated to that listed on the admission claim. For 83.9 percent of the episodes, the beginning and ending claims carried primary diagnoses within the same category.
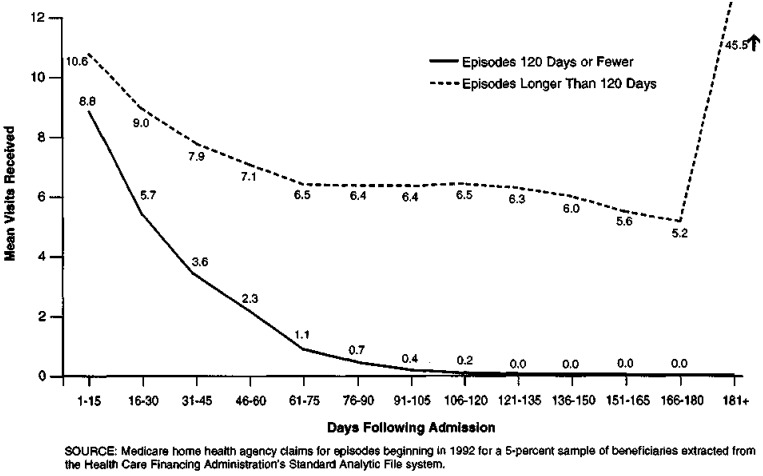
Figure 2 illustrates the distribution of visits across 15-day periods within episodes. One line shows the distribution for episodes that end by the 120th day following admission; the other line shows the distribution for episodes that lasted 120 days or longer. It can be seen that the longer episodes have more visits, on average, during every 15-day period. This suggests that those beneficiaries whose episodes last longest also receive more visits during the early stages of the episode. Conversely, those with the shortest episodes do not receive (on average) a more intense level of services during their short stays that might be masked when using a long (120-day) episode as the denominator to calculate the intensity of visits delivered.
Figure 2. Timing of Visits Within Episodes, by Length of Episode: Medicare Home Health Utilization, 1992.
File Construction
Using the full file, a total of approximately 38.5 million claims for services delivered during the period January 1989 through September 1993 were identified. Of these, approximately 13.1 million claims, made by 6,240 different provider agencies, were found to be associated with the 3.7 million episodes of care that began in 1992. Episodes containing no visits were dropped. A final cleaning step was to delete episodes delivered by providers who were either certified or terminated between January 1992 and July 1993 (because their data would definitely be truncated at one end or the other) and any episodes delivered by agencies who delivered a total of 50 visits or fewer during this period (because they were felt likely to be very unrepresentative of the general provider experience). This left a sample of 5,522 agencies that delivered a total of 2.3 million episodes of care that began in 1992.
For analyses of episodes, a 5-percent sample of beneficiaries was selected from those receiving care from these agencies, and all their episodes of care were assembled, yielding a sample of 113,306 episodes. At the outset, analyses with the full sample were also performed to validate the findings of the analyses conducted using the 5-percent sample. As the analysis proceeded and the results for the two samples were invariably found to be equivalent, the full-sample analyses were discontinued.
Findings
Overall, we find that mean average length of the 1992 Medicare home health episode was 157.4 days (Table 1), a figure that must be interpreted in the context of the minimum length of an episode being set at 120 days. Further examination, however, shows that the actual period of receipt of service for more than 74 percent of all episodes was less than the 120 days established as the minimum length of an episode for payment purposes. For these shorter episodes, the average duration of service was actually only 42.2 days. On the other hand, for the minority (25.9 percent) of episodes where the span of service actually exceeds 120 days, the average duration of service was 264.6 days.
Table 1. Medicare Home Health Care Utilization, by Measure of Utilization: 1992.
| Measure of Utilization | Mean | Median |
|---|---|---|
| Length of Episode (Days), All Episodes | 157.4 (88.7) |
120.0 |
| Percent of Episodes, Span of Service 120 Days or Fewer | 74.1 — |
— |
| Actual Span of Service, Episodes 120 Days or Fewer | 42.2 (29.2) |
37.0 |
| Percent of Episodes Exceeding 120 Days | 25.9 — |
— |
| Actual Span of Service, Episodes Exceeding 120 Days | 264.6 (122.0) |
233.0 |
| Mean Visits Per Total Episode, All Episodes | 50.3 (84.3) |
21.0 |
| Mean Visits During First 120 Days, All Episodes | 32.6 (37.2) |
19.3 |
| Mean Visits After First 120 Days, All Episodes | 17.8 (58.4) |
0.0 |
| Reimbursement Per Total Episode, All Episodes | $2,938 ($6,043) |
$1,334 |
| Reimbursement During First 120 Days, All Episodes | $1,952 ($4,337) |
$1,200 |
| Reimbursement After First 120 Days, All Episodes | $985 ($3,262) |
$0 |
NOTES: Numbers in parentheses are standard deviations of the mean. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Mean reimbursement per episode averaged $2,938 across all agencies. Of this amount, $1,952 (66 percent), on average, was for visits delivered during the first 120 days of the episode; the rest ($985) was for visits during the outlier period. This suggests that a per episode payment scheme based on the 120-day episode will likely result in a considerable proportion of services being paid for outside the per episode payment framework.
Agency location is often cited as a cause of variation in practice and costs. Medicare's home health cost caps recognize geographic differences in input costs and generally allow higher per visit payments to agencies in urban areas. However, we found that although rural agencies generally had significantly longer episodes of care (Table 2), mean reimbursement for these episodes was not significantly different from that for urban agencies. During the first 120 days of the episode, mean visits were virtually equal in urban and rural agencies, but mean reimbursement was 25 percent higher for urban agencies. In the outlier period, however, visits and reimbursement are significantly higher for the episodes provided by rural agencies.
Table 2. Episodes, by Agency Urban or Rural Location and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | Urban (n = 90,066) |
Rural (n = 21,786) |
||
|---|---|---|---|---|
|
|
|
|||
| Mean | Median | Mean | Median | |
| Mean Length of Episode (Days) |
*160.6 (33.8) |
150.4 |
*177.2 (38.9) |
168.6 |
| Percent of Episodes, Span of Service 120 Days or Fewer |
*72.8 (15.4) |
76.1 |
*66.1 (16.1) |
68.4 |
| Actual Span of Service, Episodes 120 Days or Fewer |
*42.4 (8.0) |
42.5 |
*43.5 (8.1) |
43.8 |
| Percent of Episodes Exceeding 120 Days |
*27.2 (15.4) |
23.9 |
*33.9 (16.1) |
31.6 |
| Actual Span of Service, Episodes Exceeding 120 Days |
*248.5 (55.0) |
249.5 |
*272.0 (54.0) |
276.8 |
| Mean Visits Per Total Episode, All Episodes |
*49.0 (82.6) |
21.0 |
*57.1 (92.7) |
22.0 |
| Mean Visits During First 120 Days, All Episodes | 32.8 (37.4) |
20.0 | 32.4 (36.7) |
19.0 |
| Mean Visits After First 120 Days, All Episodes |
*16.3 (56.6) |
0.0 |
*24.7 (66.1) |
0.0 |
| Reimbursement Per Total Episode, All Episodes | $2,966 ($6,368) |
$1,377 | $2,929 ($467) |
$1,224 |
| Reimbursement During First 120 Days, All Episodes |
*$2,030 ($4,768) |
$1,259 |
*1,696 ($1,910) |
$1,045 |
| Reimbursement After First 120 Days, All Episodes |
*$936 ($3,264) |
$0 |
*$1,232 ($3,335) |
$0 |
Statistically significant at .05 level.
NOTES: Numbers In parentheses are standard deviations of the means. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period and 42 agencies whose urban/rural status could not be determined from the Provider of Service file. Total number of episodes is 111,852.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Another potential determinant of practice pattern is agency auspice and control. For this analysis, we grouped the agencies into the same categories being used for sample stratification under the demonstration (voluntary/private non-profit [V/PNP]; proprietary; and facility-based), plus a fourth category, “government,” which is not considered eligible for the demonstration. Of these four types, proprietary agencies were found to have the longest episodes, on average, and the highest percent of episodes lasting more than 120 days (Table 3). It is not surprising, then, to find proprietary agencies with the highest mean per episode reimbursement However, even though mean episode length for proprietary agencies is only 4 percent higher than the next highest group (government), visits per episode were 57 percent higher than V/PNP agencies. Most of this large difference is due to services provided in the outlier period, where mean visits and reimbursement were each 85 percent higher than the next highest group (V/PNP).
Table 3. Episodes, by Agency Type and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | Voluntary/Private Non-Profit (n = 36,289) |
Government (n = 7,676) |
Facility-Based (n = 36,072) |
Proprietary (n = 33,245) |
||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Mean | Median | Mean | Median | Mean | Median | Mean | Median | |
| Mean Length of Episode (Days) | 161.7 (31.5) |
154.2 | 167.9 (36.2) |
159.7 | 160.4 (30.5) |
151.9 | 175.2 (42.5) |
163.7 |
| Percent of Episodes, Span of Service 120 Days or Fewer | 72.2 (14.2) |
74.6 | 70.3 (15.9) |
72.0 | 73.4 (13.7) |
75.9 | 66.4 (17.9) |
69.1 |
| Actual Span of Service, Episodes 120 Days or Fewer | 42.3 (7.6) |
42.6 | 41.9 (8.3) |
41.8 | 41.7 (7.2) |
41.7 | 44.7 (8.5) |
44.9 |
| Percent of Episodes Exceeding 120 Days | 27.8 (14.2) |
25.4 | 29.7 (15.9) |
28.0 | 26.6 (13.7) |
24.1 | 33.6 (17.9) |
30.9 |
| Actual Span of Service, Episodes Exceeding 120 Days | 252.4 (51.8) |
252.6 | 259.4 (63.5) |
264.9 | 253.3 (50.7) |
254.9 | 263.1 (57.8) |
266.3 |
| Mean Visits per Total Episode, All Episodes | 45.2 (74.6) |
20.0 | 37.9 (60.1) |
16.0 | 39.1 (63.8) |
18.0 | 70.9 (110.8) |
31.0 |
| Mean Visits During First 120 Days, All Episodes | 30.2 (33.8) |
18.3 | 24.0 (27.7) |
14.0 | 27.0 (30.6) |
17.0 | 43.1 (45.8) |
27.0 |
| Mean Visits After First 120 Days, All Episodes | 15.0 (51.8) |
0.0 | 13.9 (41.2) |
0.0 | 12.1 (42.6) |
0.0 | 27.8 (78.6) |
0.0 |
| Reimbursement per Total Episode, All Episodes | $2,611 ($7,787) |
$1,225 | $2,046 ($3,257) |
$904 | $2,563 ($3,968) |
$1,252 | $3,908 ($6,110) |
$1,753 |
| Reimbursement During First 120 Days, All Episodes | $1,799 ($6,896) |
$1,109 | $1,325 (1,578) |
$790 | $1,820 ($2,052) |
$1,139 | $2,408 ($2,593) |
$1,560 |
| Reimbursement After First 120 Days, All Episodes | $812 ($2,817) |
$0 | $720 ($2,183) |
$0 | $742 ($2,609) |
$0 | $1,500 ($4,329) |
$0 |
NOTES: Numbers in parentheses are standard deviations of the means. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period and agencies whose type could not be determined from the Provider of Service file. Total number of episodes is 113,282.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Because facility-based agencies are often considered to behave differently from freestanding providers and because of the control exerted by the sponsoring institution, we compared them with all other providers as a group (Table 4). Episodes provided by facility-based agencies were slightly shorter and had slightly lower mean reimbursement than did those provided by the cohort of freestanding providers, but their mean reimbursement per visit was higher.
Table 4. Episodes, by Agency Facility Relationship and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | Facility-Based (n = 36,072) |
Non-Facility-Based (n = 77,234) |
||
|---|---|---|---|---|
|
|
|
|||
| Mean | Median | Mean | Median | |
| Mean Length of Episode (Days) |
*160.4 (30.5) |
151.9 |
*169.8 (38.8) |
159.7 |
| Percent of Episodes, Span of Service 120 Days or Fewer |
*73.4 (13.7) |
75.9 |
*68.8 (16.7) |
71.5 |
| Actual Span of Service, Episodes 120 Days or Fewer |
*41.7 (7.2) |
41.7 |
*43.4 (8.3) |
43.6 |
| Percent of Episodes Exceeding 120 Days |
*26.6 (13.7) |
24.1 |
*31.2 (16.7) |
28.5 |
| Actual Span of Service, Episodes Exceeding 120 Days |
*253.3 (50.7) |
254.9 |
*259.2 (57.8) |
262.5 |
| Mean Visits Per Total Episode, All Episodes |
*39.1 (63.8) |
18.0 |
*55.5 (91.9) |
24.0 |
| Mean Visits During First 120 Days, All Episodes |
*27.0 (30.6) |
17.0 |
*35.1 (39.6) |
21.0 |
| Mean Visits After First 120 Days, All Episodes |
*12.1 (42.6) |
0.0 |
*20.4 (64.3) |
0.0 |
| Reimbursement Per Total Episode, All Episodes |
*$2,563 ($3,698) |
$1,252 |
*$3,113 ($6,791) |
$1,380 |
| Reimbursement During First 120 Days, All Episodes |
*$1,820 ($2,052) |
$1,139 |
*$2,014 ($5,062) |
$1,235 |
| Reimbursement After First 120 Days, All Episodes |
*$742 ($2,609) |
$0 |
*$1,099 ($3,520) |
$0 |
Statistically significant at .05 level.
NOTES: Numbers in parentheses are standard deviations of the means. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period and any agencies whose relationship to a facility could not be determined from the Provider of Service file. Total number of episodes is 113,306.
SOURCE: Medicare home health agency claims for all episodes beginning In 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Agency size is another factor that could potentially influence provider practice. Agencies that provide few home health visits overall, or provide few Medicare visits, may have fewer procedures in place for managing them. We found that episodes from providers in the group providing the fewest Medicare visits had the shortest mean episode length, the smallest proportion of episodes lasting more than 120 days, the lowest mean visits per episode, and the lowest mean reimbursement per episode (Table 5).
Table 5. Episodes, by Agency Size and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | Small Agency (n = 33,621) |
Medium Agency (n = 20,910) |
Large Agency (n = 58,773) |
|||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean | Median | Mean | Median | Mean | Median | |
| Mean Length of Episode (days) | 163.4 (35.5) |
153.4 | 173.3 (38.3) |
163.6 | 174.2 (37.4) |
166.4 |
| Percent of Episodes, Span of Service 120 Days or Fewer | 71.7 (15.9) |
74.8 | 67.8 (15.8) |
70.1 | 67.1 (15.4) |
69.4 |
| Actual Span of Service, Episodes 120 Days or Fewer | 41.9 (8.7) |
41.7 | 44.3 (6.3) |
44.2 | 45.2 (5.4) |
45.2 |
| Percent of Episodes Exceeding 120 Days | 28.3 (15.9) |
25.2 | 32.2 (15.8) |
29.9 | 32.9 (15.4) |
30.6 |
| Actual Span of Service, Episodes Exceeding 120 Days | 251.9 (60.8) |
254.8 | 268.3 (42.1) |
269.3 | 268.4 (40.3) |
269.7 |
| Mean Visits Per Total Episode, All Episodes | 42.1 (73.3) |
17.0 | 46.6 (77.9) |
20.0 | 56.3 (91.6) |
25.0 |
| Mean Visits During First 120 Days, All Episodes | 27.1 (33.0) |
16.0 | 30.3 (34.4) |
18.0 | 36.5 (39.8) |
22.9 |
| Mean Visits After First 120 Days, All Episodes | 15.0 (50.3) |
0.0 | 16.3 (54.2) |
0.0 | 19.9 (63.8) |
0.0 |
| Reimbursement Per Total Episode, All Episodes | $2,528 ($4,262) |
$1,100 | $2,739 ($4,375) |
$1,262 | $3,244 ($7,279) |
$1,527 |
| Reimbursement During First 120 Days, All Episodes | $1,669 ($2,019) |
$992 | $1,834 ($2,063) |
$1,132 | $2,156 ($5,686) |
$1,375 |
| Reimbursement After First 120 Days, All Episodes | $858 ($2,873) |
$0 | $904 ($3,000) |
$0 | $1,087 ($3,546) |
$0 |
NOTES: Agency size categories are defined as follows: Small = 20,000 or fewer Medicare visits, 1992; Medium = 20,001 to 34,999 Medicare visits, 1992; and Large = 35,000 or more Medicare visits in 1992. Numbers in parentheses are standard deviations of the means. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period. Total number of episodes is 113,304.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
For the demonstration, because prospective rates are developed based on each agency's historical costs, we exclude agencies that are newly certified because it was felt that a startup enterprise would have an unstable cost experience, likely to differ significantly from its costs in subsequent years. We decided to investigate whether recently certified agencies had practice patterns that differed systematically from those of providers who had been certified for longer periods of time (Table 6). We found that newer agencies have longer episodes, on average, more visits per episode, and much higher average episode reimbursement than agencies with a longer certification history. However, mean reimbursement per visit was virtually the same ($58.65 versus $58.39).
Table 6. Episodes, by Agency Medicare Certification Date and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | New Agencies (n = 9,514) |
Old Agencies (n = 103,792) |
||
|---|---|---|---|---|
|
|
|
|||
| Mean | Median | Mean | Median | |
| Length of Episode (Days) |
*178.0 (47.7) |
164.7 |
*164.9 (34.0) |
156.2 |
| Percent of Episodes, Span of Service 120 Days or Fewer |
*65.2 (20.0) |
68.3 |
*71.1 (15.0) |
73.7 |
| Actual Span of Service, Episodes 120 Days or Fewer |
*44.3 (9.9) |
44.4 |
*42.6 (7.6) |
42.7 |
| Percent of Episodes Exceeding 120 Days |
*34.8 (20.0) |
31.7 |
*28.9 (15.0) |
26.3 |
| Actual Span of Service, Episodes Exceeding 120 Days |
*259.6 (69.5) |
263.3 |
*256.9 (52.9) |
259.2 |
| Mean Visits Per Total Episode, All Episodes |
*69.8 (109.9) |
30.0 |
*48.5 (81.3) |
21.0 |
| Mean Visits During First 120 Days, All Episodes |
*41.7 (44.8) |
26.0 |
*31.7 (36.3) |
19.0 |
| Mean Visits After First 120 days, All Episodes |
*28.1 (78.5) |
0.0 |
*16.8 (56.1) |
0.0 |
| Reimbursement Per Total Episode, All Episodes |
*$4,094 ($6,222) |
$1,860 |
*$2,832 ($6,015) |
$1,294 |
| Reimbursement During First 120 Days, All Episodes |
*$2,524 ($2,710) |
$1,655 |
*$1,900 ($4,453) |
$1,168 |
| Reimbursement After First 120 Days, All Episodes |
*$1,570 ($4,361) |
$0 |
*$932 ($3,137) |
$0 |
Statistically significant at the .05 level.
NOTES: New = Medicare certification date after December 31, 1988; Old = Medicare certification date through December 31, 1988. Numbers in parentheses are standard deviations of the means. Excludes home health agencies that were certified, terminated, or delivered 50 or fewer visits during the period and any agencies whose certification date could not be determined from the Provider of Service file. Total number of episodes is 113,306.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Table 7 shows the distribution of visits within the episode by discipline. We see that skilled nursing visits comprised approximately one-half of all visits delivered, which is not surprising considering that they are most frequently the qualifying visits that allow other types of visits (especially home health aide) to be covered by Medicare. Of note, however, is volume of aide visits that are provided in the outlier period; beyond 120 days, aide visits comprise the majority of visits provided.
Table 7. Distribution of Visits Within Episodes, by Discipline and Measure of Utilization: Medicare Home Health Care Utilization, 1992.
| Measure of Utilization | Visits by Discipline | ||||
|---|---|---|---|---|---|
|
| |||||
| Total All Disciplines | Skilled Nursing | Home Health Aide | Physical Therapy | OT, ST, MSS | |
| All Episodes | |||||
| Mean Visits During First 120 Days | 32.6 | 15.9 | 11.5 | 3.9 | 1.3 |
| Percent of All Visits in Period | — | 48.8 | 35.3 | 12.0 | 3.9 |
| Mean Visits After First 120 Days | 17.8 | 7.1 | 9.7 | 0.7 | .3 |
| Percent of All Visits in Period | — | 39.9 | 54.5 | 3.9 | 1.7 |
| Mean Visits, Entire Episode | 50.4 | 23.0 | 21.2 | 4.6 | 1.6 |
| Percent of All Visits in Episode | — | 45.6 | 42.1 | 9.1 | 3.2 |
| Episodes 120 Days or Fewer | |||||
| Mean Visits Per Episode | 22.9 | 11.6 | 6.8 | 3.5 | 1.0 |
| Percent of All Visits in Episode | — | 50.7 | 29.7 | 15.3 | 4.4 |
| Episodes Exceeding 120 Days | |||||
| Mean Visits During First 120 Days | 60.4 | 28.3 | 24.8 | 5.2 | 2.1 |
| Percent of All Visits in Period | — | 46.9 | 41.1 | 8.6 | 3.5 |
| Mean Visits After First 120 Days | 68.6 | 27.4 | 37.3 | 2.7 | 1.2 |
| Percent of All Visits in Period | — | 39.9 | 54.4 | 3.9 | 1.7 |
| Mean Visits, Entire Episode | 129.0 | 55.7 | 62.1 | 7.9 | 3.3 |
| Percent of All Visits in Episode | — | 43.2 | 48.1 | 6.1 | 2.6 |
NOTES: Occupational therapy (OT), speech therapy (ST), and medical social services (MSS) have been combined.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Multivariate Analysis
Setting appropriate payment rates under a national PPS for home health requires an understanding of the components of episode cost and the variation in these components across geographic areas, agency types, and market characteristics. As noted in Table 3, for example, proprietary agencies are paid about $600 more, on average, for home health care provided during defined 120-day episodes than are non-profit agencies. This could result from a concentration of proprietary agencies in relatively high-wage areas, or from a tendency of proprietary agencies to provide more home health visits per week or per month. It might alternatively be the result of longer episodes of care furnished by proprietary agencies.
To clarify the relationship among agency characteristics, locality effects, and patient traits on reimbursement for episodes of care, separate linear regressions of reimbursement per visit, number of visits per day of episode, and duration of episode on local, agency, and patient characteristics were estimated. The influence of a specified variable of interest on the estimated reimbursement of an episode can thus be decomposed into its distinct effects on the constituent parts of episode reimbursement This decomposition is more easily carried out if the variables of interest are expressed in logarithms, because
| (1) |
The estimated percent effect of, for example, rural location on episode reimbursement can therefore be expressed as the sum of its effects on the number of days in the episode, reimbursement per visit, and visits per day. An alternative decomposition holds the duration of episode fixed at 120 days and, hence, resembles more closely the episode definition used under the demonstration. For a 120-day episode, the decomposition has only two terms:
| (2) |
The regression specification is the same for all dependent variables: The log of episode duration, reimbursement per visit, and number of visits are each regressed on a set of covariates representing locality and market effects, patient characteristics, and agency traits. Definitions of the dependent variables used in the analysis and their mean values are displayed in Table 8. Analyses were carried out for full episodes (120 days plus outlier period) that terminate only with the appearance of a 45-day gap in services and for the 120-day episode window only. The covariates used in the analysis are described below:
Table 8. Episode Characteristics and Variable Definitions: Medicare Home Health Care Utilization, 1992.
| Characteristic | Definition | Mean |
|---|---|---|
| Reimbursement Full Episode | Medicare Reimbursement for Episodes Terminated by 45-Day Gap Without Service | $2,854.60 |
| Reimbursement 120-Day Episode | Medicare Reimbursement for Episodes Terminated 120 Days After Initiation of Episode | $1,913.69 |
| Reimbursement per HHA Visit | Medicare Reimbursement Divided by Number of Visits In Full Episode | $63.86 |
| HHA Visits per Day of Full Episode | HHA Visits Divided by Number of Days in Full Episode | 0.55 |
| HHA Visits per Day of 120-Day Episode | HHA Visits Divided by Number of Days in 120-Day Episode. | 0.27 |
| Total HHA Visits: Full Episode | Number of HHA Visits in Full Episode | 48.84 |
| Total HHA Visits: 120-Day Episode | Number of HHA Visits in 120-Day Episode | 31.88 |
| Duration of Full Episode | Number of Days in Full Episode | 98.47 |
NOTES: HHA is home health agency.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
Locality and market variables are used as a proxy for labor cost and as a means of capturing geographic variability in practice patterns. Dummy variables are used for urban location and for location in the South, North Central, or West census region (Northeast is the omitted category). The Herfindahl index, defined as the sum of squares of the visit shares for all agencies providing service in the beneficiary's county of residence, was used as a measure of market concentration. The Herfindahl index must vary between zero and one, with higher values indicating greater concentration. High market concentration has sometimes been hypothesized to result in lower prices (reimbursement per visit) for health care services because the incentive to compete for consumers through cost-increasing amenities is reduced. Finally, dummy variables identifying the regional home health intermediary of the agency providing the episode were included, even though the coefficients are not reported in the results to follow.
Agency effects such as agency size and type of organization (non-profit, government, hospital-based, and proprietary) were seen (Tables 3-5) to be associated with pronounced disparities in number of visits, duration of episodes, and reimbursement per episode. Dummy variables were defined for agency type (non-profit is omitted), size, and market share. The dummy variables for agency size might appear at first to be problematic. Agencies that attain larger-than-average size surely do so in part by providing more visits per period to a given patient than do other agencies; they may also extend episodes for a longer time than do other agencies. However, because the regression equations are estimated at the episode level, not at the agency level, bias as the result of endogenous agency size can only arise from the effects of additional visits from a given episode on agency size and must therefore be quite small.
Patient characteristics can be expected to have stronger effects on the number of visits and duration of episodes than agency or locality effects. However, no such characteristics are available to us other than patient age, gender, and diagnosis. The age categories are included, with the disabled (under 65 years of age) omitted. Dummy variables for each of the 44 diagnostic categories were also included even though their coefficients are not reported. Although patient characteristics would be expected to have no effect on payment per visit for any given discipline, they may nevertheless affect mean episode payment per visit through their influence on the composition of visits (e.g., the proportion of visits that are skilled nursing, physical therapy, etc.) and so appear in the equation for payment per visit.
Regression estimates are displayed in Table 9. All regressors but two are dummy variables. Columns (1) and (2) show effects on reimbursement for full episodes and for 120-day episodes.4 The results show a marked effect of agency ownership on Medicare reimbursement for episodes of home health care. Proprietary agencies receive 22-24 percent more in reimbursement than non-profit agencies (the omitted category) and 38-40 percent more than government agencies. Total episode reimbursement also tends to increase with size; large agencies receive 24-26 percent more per episode than small agencies.5 Reimbursement falls with increases in industry concentration as measured by the Herfindahl index and rises with the market share of the agency providing the episode; a 10-percentage point increase in the market share of an episode's provider produces a one-tenth-of-1-percent increase in episode reimbursement Finally, episodes provided to male beneficiaries cost the Medicare program about 12 percent less, on average, than do episodes provided to women. There is no statistically significant relationship between episode reimbursement and beneficiary age.6
Table 9. Determinants of Home Health Episode Characteristics: Medicare Home Health Care Utilization, 1992.
| Characteristic | log(Reimb): Full Episode (1) |
log(Reimb): 120-Day Episode (2) |
log(Duration of Full Episode) (3) |
log(Reimb per HHA Visit) (4) |
log(HHA Visits per Day): Full Episode (5) |
log(Total Visits): Full Episode (6) |
log (Total Visits): 120-Day Episode (7) |
|---|---|---|---|---|---|---|---|
| Rural | *-0.135 | *-0.173 | *0.107 | *-0.118 | *-0.124 | -0.017 | *-0.052* |
| North Central | *-0.126 | *-0.121 | -0.019 | *0.011 | *-0.120 | *-0.138 | *-0.132* |
| West | -0.043 | -0.002 | *-0.213 | *0.173 | 0.002 | *-0.215 | *-0.175* |
| South | *0.049 | *0.038 | *0.035 | *-0.067 | *0.080 | *0.116 | *0.105* |
| North Central-Rural | *0.216 | *0.206 | 0.044 | *0.033 | *0.140 | *0.183 | *0.170* |
| West-Rural | *0.298 | *0.305 | *0.095 | *0.064 | *0.139 | *0.234 | *0.236* |
| South-Rural | *0.182 | *0.131 | *0.181 | 0.002 | -0.001 | *0.180 | *0.127* |
| Facility-Based | *0.077 | *0.098 | *-0.069 | *0.151 | -0.009 | *-0.075 | *-0.053* |
| Proprietary | *0.236 | *0.216 | *0.059 | *0.007 | *0.170 | *0.230 | *0.211* |
| Government | *-0.171 | *-0.161 | -0.043 | *0.023 | *-0.152 | *-0.195 | *-0.186* |
| Medium Size1 | *0.134 | *0.116 | *0.103 | *-0.026 | *0.057 | *0.160 | *0.143* |
| Large Size1 | *0.259 | *0.241 | *0.152 | -0.002 | *0.108 | *0.261 | *0.243* |
| Male | *-0.120 | *-0.095 | *-0.125 | *0.009 | -0.003 | *-0.128 | *-0.104* |
| Age 65-74 | -0.051 | <0.001 | *-0.120 | 0.003 | *0.067 | *-0.053 | -0.002 |
| Age 75-84 | 0.012 | *0.044 | *-0.057 | <0.001 | *0.070 | 0.012 | *0.044* |
| Age 85 or Over | 0.026 | *0.045 | *-0.049 | -0.002 | *0.077 | 0.027 | *0.047* |
| Herfindahl | *-0.141 | *-0.194 | *0.093 | *-0.098 | *-0.136 | *-0.043 | *-0.096* |
| Market Share | *0.103 | *0.058 | 0.148 | *-0.050 | 0.006 | 0.153 | *0.107* |
| R2 | 0.06 | 0.06 | 0.07 | 0.32 | 0.10 | 0.09 | 0.09 |
| n | 102,351 | 102,351 | 102,351 | 102,351 | 102,351 | 102,351 | 102,351 |
Statistically significant at .05 level.
Medium: supplied 20,000-35,000 Medicare HHA visits in year. Large: supplied > 35,000 Medicare HHA visits in the year.
NOTES: Reimb. is reimbursement. HHA is home health agency. RHHI is Regional Home Health Intermediary. Additional variables included in the model and not reported here are diagnosis categories and RHHI.
SOURCE: Medicare home health agency claims for all episodes beginning in 1992 for a 5-percent sample of beneficiaries extracted from the Health Care Financing Administration's Standard Analytic File system.
As previously noted, the logarithmic specification of the dependent variables permits a simple arithmetic decomposition of episode reimbursements. Each coefficient in column (10) may be expressed also as the sum of the corresponding coefficients in columns (3), (4), and (5) (or, alternatively, in [4] and [6]). Each coefficient in column (2) may be expressed as the sum of coefficients in columns (3) and (7). For example, nearly three-quarters of the 24-percent-greater episode reimbursement associated with proprietary versus non-profit agencies results from greater numbers of visits per day; about 20 percent results from increasing the duration of episodes, and only about 5 percent results from greater reimbursement per visit.
Virtually all (more than 95 percent) of the proprietary/non-profit difference in mean reimbursement for 120-day episodes is due to greater numbers of visits per episode. A somewhat different story emerges with respect to the effects of agency size. Large agencies receive 26.1 percent more per episode, primarily because episodes provided by large agencies last longer. About 42 percent of the reimbursement difference is due to greater numbers of visits per day and none is due to differences in reimbursement per visit. Yet another configuration of effects is provided by facility-based agencies. Although these agencies are paid 15.2 percent more per visit than are non-profits, episode payment for facility-based agencies is only 8.3 percent higher because episodes provided by facility-based agencies are about 7 percent shorter, on average, than those provided by non-profit agencies. (There are no differences in visits per day.)
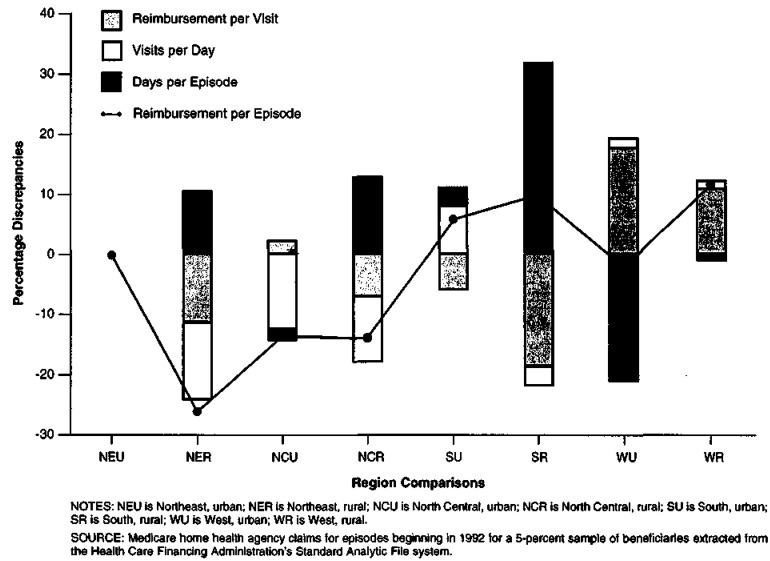
Regional mean values for Medicare reimbursement per episode of care, corrected for provider size, type, market share, beneficiary age and gender, and market concentration are computed by summing appropriate coefficients for region, rural location, and region-rural interaction. The implicit omitted category is the Northeast Region, urban location. In broad terms, Medicare home health episodes are more expensive in the South and West Regions than in the North Central and Northeast7. Computed regional differences by urban-rural location are shown in Figure 3. The percent difference between each region's reimbursement and the mean for urban episodes in the Northeast Region is given by the triangle. The location of this triangle is, in turn, given by the algebraic sum of the heights of the three stacked bars, each of which represents a component of the percent difference in reimbursement per episode as seen in equation (1). Although episode reimbursement is highest in the rural West and rural South, the components of reimbursement are quite different in the two areas. In the rural West, the high value of reimbursement per visit is accompanied by mean values of visits per day and duration of episode quite near the mean for the reference category. In the rural South, even a very low value for reimbursement per visit is insufficient to offset the effects of an extraordinarily long mean duration of home health care.
Figure 3. Components of Variation in Home Health Episode Reimbursement, by Region: Medicare Home Health Utilization, 1992.
Conclusions
This episode simulation and the data analysis have provided some preliminary answers to the questions we hoped to address. We performed several analyses to shed some light on the sensitivity of the utilization estimates to choice of approach to defining the home care episode (i.e., using a different length for the base episode, or a different gap for distinguishing between outlier care and a new episode, or even using service gaps alone to distinguish between episodes). We found that using any of the alternatives examined would likely make only a small percent difference in the number of episodes created. Given that we are dealing with a fixed pool of visits and charges to be allocated across the episodes we create, the impacts on visits per episode or charges per episode would likely be of the same order of magnitude. We then turned to the specific questions:
On average, what proportion of services provided falls within the episode under the demonstration's definition? What proportion is provided outside the episode period?
Based on the demonstration episode definition and Medicare utilization in 1992, 74 percent of all services would fall within the 120-day episode period. Approximately 26 percent of all services would be provided in the outlier period.
Episodes that end within 120 days following admission have a mean actual span of service of 42 days; those that extend into the outlier period have a mean length of 265 days.
The distribution of visits and charges is skewed to the right by a “tail” of very long episodes; although the median number of visits per episode overall is 21, the mean is 50.
For non-outlier episodes, the mean for total visits is 23; for those with outlier visits, the mean for total visits per episode is 129. Of these, 60 occur within the first 120 days, and 69 occur during the outlier period.
About one-half of all visits provided during episodes are skilled nursing visits. Home health aide visits represent about 30 percent of visits across all episodes and more than one-half of the total visits provided in the outlier period.
What are the differences in utilization Patterns across agencies of different types with respect to the demonstration episode?
Many significant differences were observed across episodes of care provided by agencies of different types. Univariate comparisons showed that episodes were, on average, longer for rural agencies, proprietary agencies, large agencies, new agencies, and freestanding agencies.
Multivariate analysis confirmed most of these initial impressions. Rural agencies' episodes were longer than urban agencies. Proprietary and large agencies had longer episodes, but their higher reimbursement per episode was found to be due to higher quantities of visits delivered rather than higher reimbursement per visit. The variability of episode duration and reimbursement by location might be the result of differences in the care requirements of beneficiaries, of regional differences in patterns of physician authorization for home care, and/or differences in the practices of RHHIs. Diagnosis alone is known to account for only a small proportion of the variance in home care utilization.
Proprietary agencies were seen to provide episodes that were longer than average and with a substantially greater “density” of visits per day than agencies of other types. However, whether these differences should properly be ascribed to differences in their patient population or differences in their incentives to furnish additional care could not be addressed with these data.
Are any observed systematic differences in baseline utilization patterns likely to be correlated with differences in response to the PPS incentives of the demonstration and, potentially, a PPS program?
First, we see that about 74 percent of the care delivered by the HHA will be subject to per episode payment, whereas, the rest will fall in the outlier period and will be paid on a per visit basis. Thus, a substantial portion of the agency's Medicare activity will not be subject to per episode payment. This might mute the agency's incentive to respond, or it might be seen as a “cushion,” allowing managers to be more creative with the care that is subject to per episode payment.
Many of the largest existing differences in reimbursement per episode are driven not by reimbursement per visit but by the quantity of visits provided during the episode. Assuming financial responsibility (and being at risk) for this aspect of the episode of care is precisely what distinguishes the per episode payment approach from the per visit approach. Thus, it would appear that the per episode demonstration, as designed, will provide managers with the freedom to manage exactly the parameters that they need to work with if they are to be able to respond to the incentives of per episode payment.
What is not known, however, is whether the existing utilization differences are driven by managers' choices or by external factors, such as physician practice patterns, RHHI practices, or patient characteristics, which are not amenable to the actions of agency staff. Although some maintain that “an agency with higher visits is better positioned because it can always reduce them,” we cannot know whether certain types of agencies are better positioned to respond to the incentives of the demonstration because we can not know, at this point, whether they are maintaining their current utilization profiles by design or by necessity.
This preliminary analysis has recast historical home health utilization in terms of the episode definition to be used for payment under Phase II of the National Home Health Agency Prospective Payment Demonstration. The demonstration will allow us to observe whether agency managers can, in fact, bring about changes in the patterns of care in their agencies (without adversely affecting quality of care or beneficiary access to services), whether the incentives provided by the demonstration are strong enough to get them to do so, and whether responses differ across agencies of different types and current utilization patterns. The information that the demonstration provides should inform the decision whether to implement an ongoing PPS program for Medicare home health services. And, should HCFA decide to proceed with a PPS program, the demonstration's real-world experience with PPS should inform the design of such a major transition in order to minimize dislocation in the home health industry and maximize the continuing access to services for Medicare beneficiaries.
Acknowledgments
The authors would like to thank Sophie Lo and Ronald Boheim for their prodigious efforts in the conversion of home health claims files into usable analytic data files; Jo Anne DeVito and Jennifer Levinson for their high standards in the preparation of the data tables included here; and Liz Mauser of the Health Care Financing Administration, Office of Research and Demonstration, for ongoing review of the manuscript and the many useful suggestions made.
Footnotes
The authors are with Abt Associates, Inc., Cambridge, Massachusetts. The opinions expressed are those of the authors and not necessarily those of Abt Associates, Inc. or HCFA
The occurrence of a hospital admission within the 120-day home health episode was found to affect the total home health cost of the episode, and a flag for the occurrence of such an admission has been included as one of the parameters of the demonstration's case-mix-adjustment algorithm.
This could be an artifact of our bill-based episode definition. However, if that were the case, one would expect to see peaks on the odd 30-day intervals as well—but they are not in evidence. This suggests that agencies have some incentive to discharge patients as they reach these 60-day milestones. One possible candidate for this incentive is avoidance of the logistical burdens of obtaining recertification of the continuing need for services from the beneficiary's physician.
Patient-specific and random effects clearly account for nearly all of the variation in episode reimbursement A one-way analysis of variance of the log of episode reimbursement was conducted separately for each of the four U.S. census regions. The ratio of the provider-specific to the error variance was less than 0.20 for the Northeast and was approximately 0.05 in each of the other three regions. This result suggests that provider-specific prospective payment rates will not seriously mute the financial risk facing providers. It also sets limits to the explanatory power of statistical models of episode reimbursement that have few measures of patient characteristics.
As noted, a small part of the size effect is surely definitional. Agency size, measured by total visits, increases with the number of episodes provided and with the number of visits per episode. This latter factor naturally causes reimbursement per episode to increase.
Though not shown, the size and statistical significance of the coefficients on the intermediary dummies indicates pronounced variation across intermediaries in the duration of episodes and number of visits, even after controlling for the other variables seen in Table 9. The general magnitude of variability may be gauged by two of the largest pairwise discrepancies. Other things held constant, episodes for agencies covered by Blue Cross of South Carolina were 37 percent longer than episodes for agencies covered by Blue Cross of Wisconsin. Episodes covered by Independence Blue Cross averaged more than 40 percent more visits (again, other things constant) than episodes covered by Aetna-Clearwater. For fixed 120-day spans, episodes covered by Aetna or Blue Cross of Iowa contained 20-30 percent more visits than episodes covered by Independence Blue Cross or Blue Cross of California Whether these differences reflect underlying variation in intermediary behavior concerning coverage and denials or unmeasured variability in provider or beneficiary characteristics cannot be discerned with these data.
The one exception to this generalization is the urban West, where episodes actually cost slightly less than in the urban Northeast.
Reprint Requests: Henry B. Goldberg, Abt Associates, Inc., 55 Wheeler Street, Cambridge, Massachusetts 02138.
References
- Benjamin AE. State Variations in Home Health Expenditures Under Medicare and Medicaid. Home Health Care Services Quarterly. 1986 Spring;7(1):5. doi: 10.1300/J027v07n01_02. [DOI] [PubMed] [Google Scholar]
- Bishop C, Skwara KC. Recent Growth of Medicare Home Health. Health Affairs. 1993 Fall;12(3):95. doi: 10.1377/hlthaff.12.3.95. [DOI] [PubMed] [Google Scholar]
- Kenney GM. Rural and Urban Differentials in Medicare Home Health Use. Health Care Financing Review. 1993 Summer;14(4):39–57. [PMC free article] [PubMed] [Google Scholar]
- Branch LG, Goldberg HB, Cheh VA, Williams J. Medicare Home Health: A Description of Total Episodes of Care. Health Care Financing Review. 1993 Summer;14(4):59–74. [PMC free article] [PubMed] [Google Scholar]
- Phillips BR, Brown RS, Schore JL, et al. Home Health Prospective Payment Demonstration: Case-Mix Analysis Using Demonstration Data. Dec, 1992. Report to the Health Care Financing Administration. Mathematica Policy Research. [Google Scholar]