Abstract
This article presents data on health care spending for the United States, covering expenditures for various types of medical services and products and their sources of funding from 1960 to 1993. Although these statistics show a slowing in the growth of health care expenditures over the past few years, spending continues to increase faster than the overall economy. The share of the Nation's health care bill funded by the Federal Government through the Medicaid and Medicare programs steadily increased from 1991 to 1993. This significant change in the share of health expenditures funded by the public sector has caused Federal health expenditures as a share of all Federal spending to increase dramatically.
Overview
The Nation spent $884.2 billion for health care in 1993, up 7.8 percent from 1992 levels. This rate of growth in spending is among the lowest rates of increase experienced in the past 33 years.
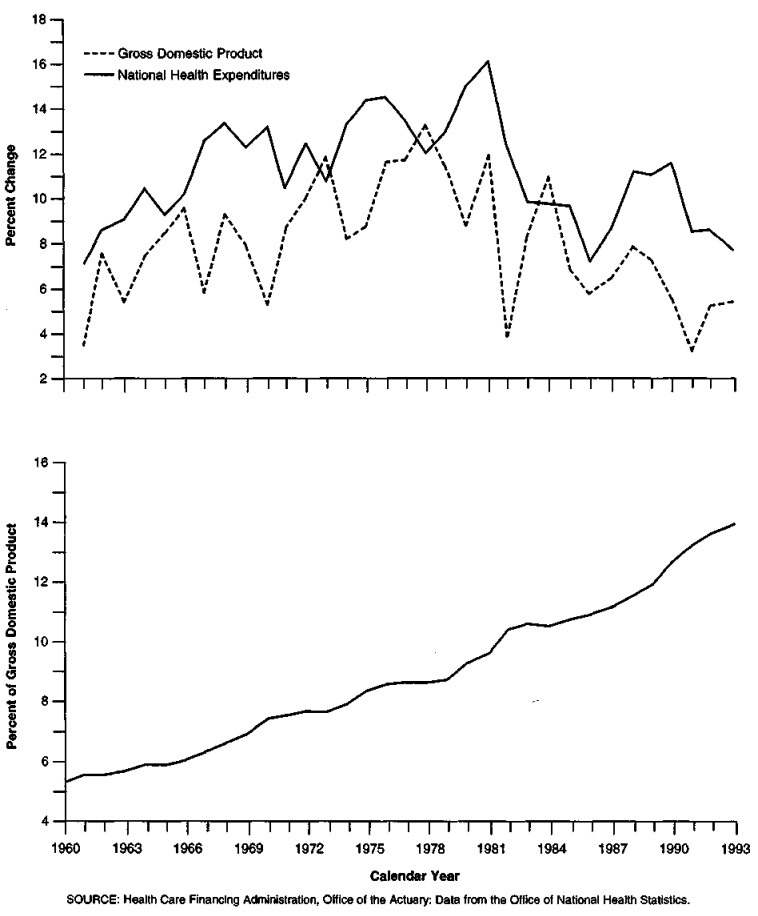
Although growth in overall health care spending slowed in 1993, it increased 2.4 percentage points faster than the output of the overall economy as measured by the gross domestic product (GDP). As a result, the share of GDP devoted to health care rose from 13.6 in 1992 to 13.9 percent in 1993 (Figure 1).
Figure 1. Percent Growth in National Health Expenditures and Gross Domestic Product, and National Health Expenditures as a Percent of Gross Domestic Product: Calendar Years 1960-93.
These data depict a health care system in transition. The rate of increase in health care spending has slowed to among the lowest rates of growth seen over the past three and a half decades, suggesting that the health care market is reacting to real or perceived pressures to contain cost growth. These reactions can be seen in the slowing rate of growth in most medical care service and product sectors expenditures since 1990.
The current low rates of growth in health care spending, together with slightly accelerated GDP growth since 1991, curbed the rapid increase in health care's share of GDP. This share had been increasing 0.6 percentage point or more in 1990 and 1991, twice the historical average. However, the deceleration in expenditure growth was not enough to alter the long-term trend: The 0.3-percentage point increase in health spending as a share of GDP, equal to the average increase in share experienced from 1960 to 1992, merely puts the United States back on its long-term trajectory. The United States continues to devote steadily increasing shares of the Nation's output to health care.
At the same time, the percentage of the population left uninsured climbed, despite the increased number of persons covered by the Medicaid program. The uninsured non-elderly population grew from 16.6 percent in 1991 to 17.4 percent in 1992 (Employee Benefit Research Institute, 1994), indicating an increase in the lack of affordable private health insurance coverage.
It remains unclear whether the moderation in health spending growth is a temporary lull in the health care crisis spurred by the threat of government intervention or the beginning of a long-term restructuring of the private health care system, the full impact of which on costs is only beginning to be seen in 1993.
This article details the following:
Americans spent 13.9 percent of the Nation's GDP on health care in 1993, up from 13.6 percent in 1992 and 13.2 percent in 1991. A combination of slower health care expenditure growth and faster GDP growth since the 1991 recession contributed to the slowdown in the increase in share of GDP spent on health.
From 1990 to 1993, growth slowed in every personal health care (PHC) expenditure category except dental services, where concerns over the spread of acquired immunodeficiency syndrome (AIDS) increased purchases of supplies, causing prices charged for services to rise.
Growth of expenditures in major sectors of acute-care services dropped from double-digit rates in 1990 to single-digit rates in 1993. For hospital care, growth slowed from 10.7 percent in 1990 to 6.7 percent in 1993; for physician services, from 10.3 percent to 5.8 percent; and for retail purchases of prescription drugs (a subset of non-durable medical products), from 14.5 percent to 6.8 percent. Together, expenditures for these three service/product categories accounted for 69.9 percent of all personal health care expenditures (PHCE) in 1993.
The fastest growing payer of health care was the Federal Government. Its share of the Nation's health care bill rose from 28.1 percent in 1990 to 31.7 percent in 1993. This was the first significant increase in the share of spending by Federal sources since the coverage of the disabled population by Medicare in the early 1970s.
From 1990 to 1993, Federal and State Medicaid spending increased at a 16.0-percent average annual rate, almost twice as fast as the 8.3-percent annual increase in overall spending. This rapid increase has several causes, including mandated program eligibility expansions, court decisions requiring higher reimbursement rates, and States' use of disproportionate share payments to hospitals with a large proportion of low-income patients.
The national health accounts (NHA) excludes certain Medicaid disproportionate share payments to hospitals offset by donations and taxes paid by the same facilities. This exclusion reduces State and local Medicaid payments, increasing the effective Federal match rate for Medicaid. In 1990, the Federal Government funded 56.6 percent of Medicaid expenditures; by 1993, that share had risen to 64.5 percent.
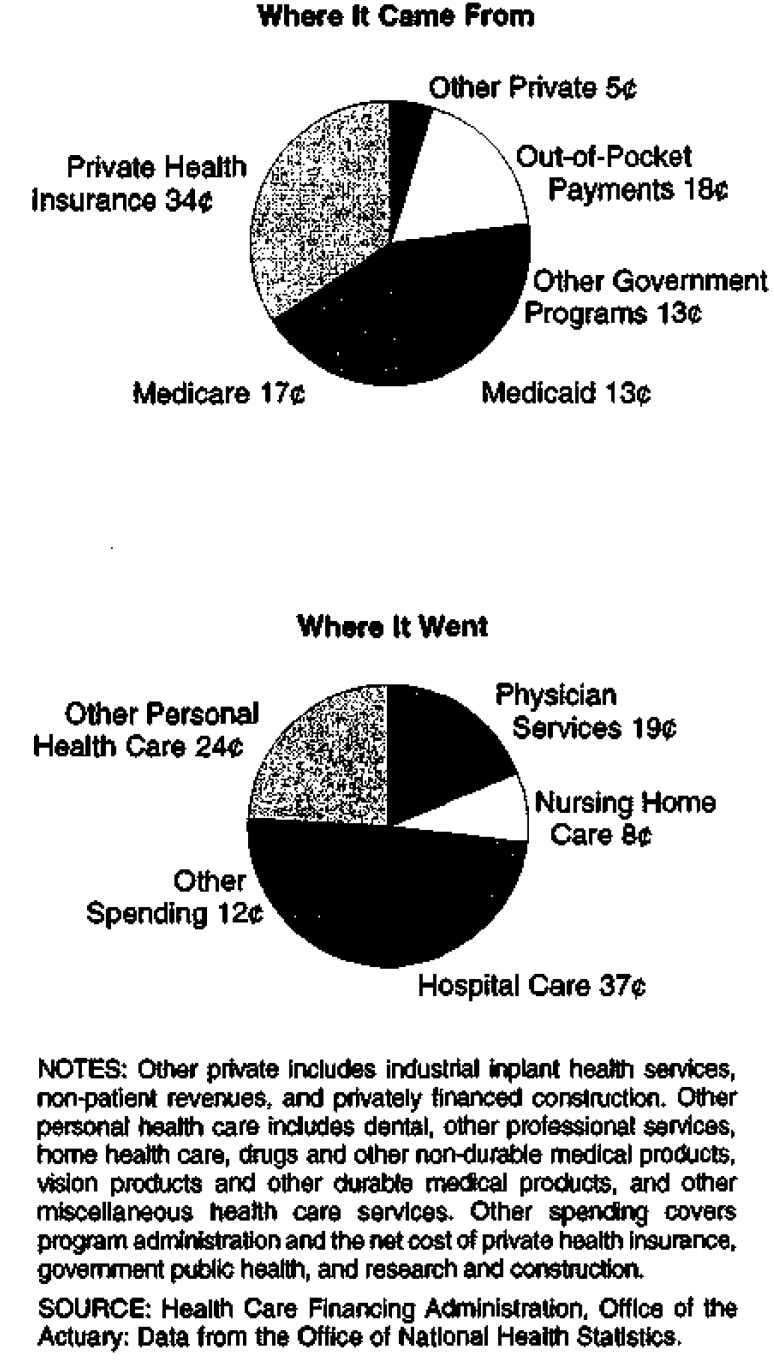
The Medicaid and Medicare programs spent $272.1 billion for health care in 1993, accounting for 30.8 percent of health spending (Figure 2) and 70.2 percent of all public funding of health care.
The major private payer of health care costs, private health insurance, paid for one-third of all health expenditures in 1993, the same share it has paid since 1988. The share of health spending from private out-of-pocket sources continued to decrease, falling to 17.8 percent of health spending in 1993 from 19.9 percent in 1990.
Figure 2. The Nation's Health Dollar: 1993.
This article presents an overview of health spending in the United States from 1960 to 1993. It concludes with detailed Tables 11-20 of health expenditures by type of service and source of funds. Data from these tables are highlighted throughout the article.
Table 11. National Health Expenditures Aggregate and Per Capita Amounts, Percent Distribution, and Average Annual Percent Growth, by Source of Funds: Selected Years 1960-93.
| Item | 1960 | 1970 | 1980 | 1985 | 1987 | 1989 | 1990 | 1991 | 1992 | 1993 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Billions | ||||||||||
| National Health Expenditures | $27.1 | $74.3 | $251.1 | $434.5 | $506.2 | $623.9 | $696.6 | $755.6 | $820.3 | $884.2 |
| Private | 20.5 | 46.6 | 145.8 | 259.4 | 298.6 | 370.7 | 410.0 | 432.9 | 462.9 | 496.4 |
| Public | 6.7 | 27.7 | 105.3 | 175.1 | 207.6 | 253.2 | 286.5 | 322.6 | 357.5 | 387.8 |
| Federal | 2.9 | 17.8 | 72.0 | 123.3 | 142.7 | 175.0 | 195.8 | 224.7 | 254.3 | 280.6 |
| State and Local | 3.7 | 9.9 | 33.3 | 51.8 | 64.8 | 78.2 | 90.7 | 98.0 | 103.2 | 107.3 |
| Number in Millions | ||||||||||
| U.S. Population1 | 190.1 | 214.8 | 235.1 | 246.8 | 251.5 | 256.4 | 259.4 | 262.2 | 265.1 | 268.0 |
| Amount in Billions | ||||||||||
| Gross Domestic Product | $513 | $1,011 | $2,708 | $4,039 | $4,540 | $5,251 | $5,546 | $5,725 | $6,020 | $6,343 |
| Per Capita Amount | ||||||||||
| National Health Expenditures | $143 | $346 | $1,068 | $1,761 | $2,013 | $2,433 | $2,686 | $2,882 | $3,094 | $3,299 |
| Private | 108 | 217 | 620 | 1,051 | 1,187 | 1,446 | 1,581 | 1,651 | 1,746 | 1,852 |
| Public | 35 | 129 | 448 | 709 | 825 | 987 | 1,105 | 1,230 | 1,348 | 1,447 |
| Federal | 15 | 83 | 306 | 500 | 568 | 682 | 755 | 857 | 959 | 1,047 |
| State and Local | 20 | 46 | 142 | 210 | 258 | 305 | 350 | 374 | 389 | 400 |
| Percent Distribution | ||||||||||
| National Health Expenditures | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private | 75.5 | 62.7 | 58.1 | 59.7 | 59.0 | 59.4 | 58.9 | 57.3 | 56.4 | 56.1 |
| Public | 24.5 | 37.3 | 41.9 | 40.3 | 41.0 | 40.6 | 41.1 | 42.7 | 43.6 | 43.9 |
| Federal | 10.7 | 24.0 | 28.7 | 28.4 | 28.2 | 28.0 | 28.1 | 29.7 | 31.0 | 31.7 |
| State and Local | 13.8 | 13.4 | 13.3 | 11.9 | 12.8 | 12.5 | 13.0 | 13.0 | 12.6 | 12.1 |
| Percent of Gross Domestic Product | ||||||||||
| National Health Expenditures | 5.3 | 7.4 | 9.3 | 10.8 | 11.1 | 11.9 | 12.6 | 13.2 | 13.6 | 13.9 |
| Average Annual Percent Growth From Previous Year Shown | ||||||||||
| National Health Expenditures | — | 10.6 | 12.9 | 11.6 | 7.9 | 11.0 | 11.6 | 8.5 | 8.6 | 7.8 |
| Private | — | 8.6 | 12.1 | 12.2 | 7.3 | 11.4 | 10.6 | 5.6 | 6.9 | 7.2 |
| Public | — | 15.3 | 14.3 | 10.7 | 8.9 | 10.4 | 13.2 | 12.6 | 10.8 | 8.5 |
| Federal | — | 19.8 | 15.0 | 11.4 | 7.6 | 10.7 | 11.9 | 14.8 | 13.2 | 10.3 |
| State and Local | — | 10.2 | 12.9 | 9.2 | 11.9 | 9.8 | 16.0 | 8.0 | 5.3 | 3.9 |
| U.S. Population | — | 1.2 | 0.9 | 1.0 | 1.0 | 1.0 | 1.1 | 1.1 | 1.1 | 1.1 |
| Gross Domestic Product | — | 7.0 | 10.4 | 8.3 | 6.0 | 7.5 | 5.6 | 3.2 | 5.2 | 5.4 |
July 1 Social Security area population estimates for each year, 1960-90. 1991-93 estimated by the Health Care Financing Administration.
NOTE: Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 20. Expenditures for Health Services and Supplies Under Public Programs, by Type of Expenditure and Program: 1993.
| Program Area | All Expenditures | Personal Health Care | Administration | Public Health Activities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Drugs and Other Medical Non-Durables | Vision Products and Other Medical Durables | Nursing Home Care | Other | ||||
|
| |||||||||||||
| Amount in Billions | |||||||||||||
| Public and Private Spending | $855.2 | $782.5 | $326.6 | $171.2 | $37.4 | $51.2 | $20.8 | $75.0 | $12.6 | $69.6 | $18.2 | $48.0 | $24.7 |
| All Public Programs | 370.9 | 337.0 | 182.9 | 58.1 | 1.7 | 10.6 | 11.4 | 9.2 | 4.2 | 43.6 | 15.3 | 9.2 | 24.7 |
| Federal Funds | 268.6 | 259.0 | 149.2 | 45.0 | 1.0 | 7.3 | 9.8 | 4.7 | 4.0 | 28.3 | 9.5 | 6.3 | 3.3 |
| State and Local Funds | 102.4 | 78.1 | 33.7 | 13.1 | 0.8 | 3.3 | 1.5 | 4.4 | 0.2 | 15.3 | 5.8 | 2.8 | 21.4 |
| Medicare | 154.2 | 151.1 | 92.7 | 34.8 | — | 5.6 | 8.1 | — | 3.7 | 6.1 | — | 3.1 | — |
| Medicaid1 | 117.9 | 112.8 | 42.4 | 12.5 | 1.5 | 1.4 | 3.2 | 7.7 | — | 36.0 | 8.1 | 5.1 | — |
| Federal | 76.1 | 73.2 | 32.1 | 7.6 | 0.9 | 0.8 | 1.8 | 4.5 | — | 20.8 | 4.8 | 2.9 | — |
| State and Local | 41.8 | 39.6 | 10.3 | 4.9 | 0.7 | 0.6 | 1.5 | 3.1 | — | 15.2 | 3.3 | 2.2 | — |
| Other State and Local Public Assistance Programs | 5.0 | 5.0 | 3.1 | 0.5 | 0.1 | 0.2 | 0.1 | 0.9 | 0.0 | 0.1 | 0.1 | — | — |
| Department of Veterans Affairs | 14.3 | 14.2 | 11.8 | 0.1 | 0.0 | — | — | 0.0 | 0.2 | 1.4 | 0.6 | 0.1 | — |
| Department of Defense2 | 13.4 | 13.3 | 10.4 | 1.8 | 0.0 | — | — | 0.1 | — | — | 0.9 | 0.2 | — |
| Workers' Compensation | 21.1 | 20.6 | 10.0 | 7.7 | — | 2.4 | — | 0.4 | 0.1 | — | — | 0.5 | — |
| Federal | 0.6 | 0.6 | 0.3 | 0.1 | — | 0.1 | — | 0.0 | 0.0 | — | — | 0.0 | — |
| State and Local | 20.5 | 20.0 | 9.7 | 7.5 | — | 2.3 | — | 0.4 | 0.1 | — | — | 0.5 | — |
| State and Local Hospitals3 | 10.3 | 10.3 | 10.3 | — | — | — | — | — | — | — | — | — | — |
| Other Public Programs for Personal Health Care4 | 10.0 | 9.7 | 2.1 | 0.8 | 0.1 | 0.9 | — | 0.0 | 0.1 | — | 5.6 | 0.3 | — |
| Federal | 6.7 | 6.6 | 1.8 | 0.7 | 0.1 | 0.7 | — | 0.0 | 0.1 | — | 3.2 | 0.1 | — |
| State and Local | 3.3 | 3.1 | 0.3 | 0.2 | 0.0 | 0.2 | — | 0.0 | 0.0 | — | 2.4 | 0.1 | — |
| Government Public Health Activities | 24.7 | — | — | — | — | — | — | — | — | — | — | — | 24.7 |
| Federal | 3.3 | — | — | — | — | — | — | — | — | — | — | — | 3.3 |
| State and Local | 21.4 | — | — | — | — | — | — | — | — | — | — | — | 21.4 |
| Medicare and Medicaid | 272.1 | 263.9 | 135.1 | 47.3 | 1.5 | 7.0 | 11.3 | 7.7 | 3.7 | 42.1 | 8.1 | 8.2 | — |
Excludes funds paid into the Medicare trust funds by States under buy-in agreements to cover premiums for Medicaid recipients.
Includes care for retirees and military dependents.
Expenditures not offset by revenues.
lncludes program spending for maternal and child health; vocational rehabilitation medical payments; temporary disability insurance medical payments; Public Health Service and other Federal hospitals; Indian health services; alcoholism, drug abuse, and mental health; and school health.
NOTES: 0.0 denotes amounts less than $50 million. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Trends in Types of Service
The 268 million residents of the United States and its territories spent $884.2 billion on health care in 1993, an increase of 7.8 percent from 1992. Americans spent $3,299 per person in 1993, $205 more than in the previous year.
The NHA contains two major components: health services and supplies (HSS) (those services and products that are currently consumed) and research and construction (those services and products from which benefits accrue now and in the future). Expenditures for HSS amounted to $855.2 billion in 1993. Research and construction expenditures, representing investment in future health care resources, amounted to $29.0 billion in 1993, a 5.8-percent increase from the 1992 level of $27.4 billion. HSS is further disaggregated into PHC, administration of public programs and net cost of private health insurance, and government public health activities.
Personal Health Care
PHCE grew to $782.5 billion in 1993, an increase of 7.2 percent from the $729.7 billion spent in 1992.
Public sources of funds, the amounts expended by governments, increased as a share of total PHCE in 1993. Public funds accounted for 43.1 percent of all PHCE in 1993, compared with 42.4 percent in 1992 and 39.6 percent in 1983. Medicare spending alone accounted for 19.3 percent of all PHCE in 1993, with Medicare and Medicaid accounting for one-third (33.7 percent) of all PHCE. In comparison, private funds accounted for 56.9 percent of PHCE in 1993, down slightly from 57.6 percent in 1992 and 60.4 percent in 1983. In 1993, private funding of PHCE was attributable mainly to private health insurance (33.0 percent) and out-of-pocket purchases (20.1 percent). A small amount of PHCE (3.5 percent) was funded through private non-patient sources, such as philanthropy and hospital revenues from cafeteria sales and educational programs.
Hospital Care
Hospital care expenditures amounted to $326.6 billion in 1993, accounting for 41.7 percent of PHCE. Hospital spending as a share of PHCE has generally been decreasing for the last decade, down 5 percentage points from the 46.7-percent share it held in 1983. That year marked major changes in hospital care: Medicare's prospective payment system (PPS) was initiated, and the effects of more stringent reviews of hospital inpatient stays by the private health insurance industry became observable.
In 1993, hospital care expenditure growth continued to decelerate for the third straight year, following a period of steady acceleration from 1986 to 1990. This slowdown was due to more rigorous hospital admission reviews and shorter lengths of stay, encouraged by most third-party payers. Admissions to community hospitals fell 1.1 percent from 1990 to 1993, accompanied by even greater reductions in inpatient days, off 6.8 percent. Admissions for patients 65 years of age or over grew 7.3 percent while inpatient days dropped 2.0 percent. However, for the population under 65 years of age, both inpatient days (-10.8 percent) and admissions (-5.5 percent) dropped (Table 1).
Table 1. Admissions, inpatient Days, and Length of Stay in Community Hospitals, by Age Group: Calendar Years 1986-93.
| Measurement | 1986 | 1987 | 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | 1990-93 |
|---|---|---|---|---|---|---|---|---|---|
| All Ages | |||||||||
| Admissions in Thousands | 33,825 | 33,634 | 33,496 | 33,176 | 33,017 | 32,670 | 32,411 | 32,652 | — |
| Inpatient Days in Thousands | 222,904 | 223,441 | 222,313 | 220,361 | 216,836 | 211,475 | 206,440 | 202,078 | — |
| Length of Stay in Days | 6.6 | 6.6 | 6.6 | 6.6 | 6.6 | 6.5 | 6.4 | 6.2 | — |
| Growth in Admissions | -2.1 | -0.6 | -0.4 | -1.0 | -0.5 | -1.1 | -0.8 | 0.7 | -1.1 |
| Growth in Inpatient Days | -1.4 | 0.2 | -0.5 | -0.9 | -1.6 | -2.5 | -2.4 | -2.1 | -6.8 |
| Change in Length of Stay in Days | 0.0 | 0.1 | -0.0 | 0.0 | -0.1 | -0.1 | -0.1 | -0.2 | -0.1 |
| 65 Years of Age or Over | |||||||||
| Admissions in Thousands | 10,795 | 10,841 | 11,062 | 11,190 | 11,379 | 11,659 | 11,860 | 12,209 | — |
| Inpatient Days in Thousands | 94,935 | 96,273 | 97,531 | 98,904 | 99,056 | 99,468 | 98,920 | 97,042 | — |
| Length of Stay in Days | 8.8 | 8.9 | 8.8 | 8.8 | 8.7 | 8.5 | 8.3 | 7.9 | — |
| Growth in Admissions | -1.0 | 0.4 | 2.0 | 1.2 | 1.7 | 2.5 | 1.7 | 2.9 | 7.3 |
| Growth in Inpatient Days | -0.6 | 1.4 | 1.3 | 1.4 | 0.2 | 0.4 | -0.6 | -1.9 | -2.0 |
| Change in Length of Stay in Days | 0.0 | 0.1 | -0.1 | 0.0 | -0.1 | -0.2 | -0.2 | -0.4 | -0.3 |
| Under 65 Years of Age | |||||||||
| Admissions in Thousands | 23,029 | 22,793 | 22,434 | 21,986 | 21,638 | 21,011 | 20,551 | 20,443 | — |
| Inpatient Days in Thousands | 127,969 | 127,168 | 124,782 | 121,457 | 117,781 | 112,007 | 107,520 | 105,036 | — |
| Length of Stay in Days | 5.6 | 5.6 | 5.6 | 5.5 | 5.4 | 5.3 | 5.2 | 5.1 | — |
| Growth in Admissions | -2.5 | -1.0 | -1.6 | -2.0 | -1.6 | -2.9 | -2.2 | -0.5 | -5.5 |
| Growth in Inpatient Days | -2.0 | -0.6 | -1.9 | -2.7 | -3.0 | -4.9 | -4.0 | -2.3 | -10.8 |
| Change in Length of Stay in Days | 0.0 | 0.0 | -0.0 | -0.0 | -0.1 | -0.1 | -0.1 | -0.1 | -0.0 |
SOURCE: (American Hospital Association: Data from the National Hospital Panel Survey, 1963-93).
Short-term, acute-care community hospitals delivered 88 percent of all hospital care in 1993, a share that has risen slightly over the last decade. Expenditures for inpatient services in community hospitals accounted for 64 percent of all hospital revenues in 1993. This share has fallen since the early 1980s, paralleling decreases in admissions and inpatient days, but has shown signs of stabilization in 1993.
Five percent of 1993 hospital expenditures were attributed to non-Federal, non-community hospitals ($17.7 billion). Psychiatric hospitals accounted for 85.0 percent of non-Federal, non-community hospital beds in 1992 (latest available information). Although admissions to psychiatric hospitals increased through 1992, the average length of stay for those admissions has dropped dramatically over the past decade (from 108 days in 1982 to 56 days in 1992) (American Hospital Association, 1993). This slowdown resulted primarily from the continued decrease (beginning in the 1970s) in the number of individuals previously treated in intermediate-care facilities for the mentally retarded (ICFs/MR) and the increased effects of managed care, which emphasizes outpatient treatment and limited inpatient stays.
The remaining 7 percent of 1993 hospital expenditures went to Federal hospitals ($21.8 billion). Growth in Federal hospital expenditures rose to 10.2 percent in 1991, a year in which expenditure growth in all other types of hospitals decelerated (Table 2). This acceleration was the result of the Gulf War.
Table 2. Hospital Expenditures, Percent Distribution, and Annual Percent Growth, by Type of Hospital: Calendar Years 1984-93.
| Type of Hospital | 1984 | 1985 | 1986 | 1987 | 1988 | 1989 | 1990 | 1991 | 1992 | 1993 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Millions | ||||||||||
| Total | $157,552 | $168,225 | $179,742 | $194,060 | $211,702 | $231,842 | $256,549 | $282,318 | $305,984 | $326,559 |
| Non-Federal | 145,212 | 154,953 | 165,764 | 179,354 | 196,466 | 215,415 | 238,754 | 262,704 | 285,477 | 304,784 |
| Community | 134,362 | 143,293 | 153,189 | 165,685 | 181,503 | 198,944 | 221,459 | 245,074 | 268,031 | 287,109 |
| Inpatient | 114,082 | 119,104 | 125,133 | 133,335 | 143,431 | 154,924 | 169,110 | 183,216 | 196,562 | 208,017 |
| Outpatient | 20,280 | 24,189 | 28,056 | 32,350 | 38,072 | 44,020 | 52,349 | 61,858 | 71,469 | 79,092 |
| Non-Community | 10,850 | 11,660 | 12,575 | 13,669 | 14,963 | 16,471 | 17,295 | 17,630 | 17,446 | 17,675 |
| Federal | 12,340 | 13,272 | 13,978 | 14,706 | 15,236 | 16,427 | 17,795 | 19,614 | 20,507 | 21,775 |
| Percent Distribution | ||||||||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Non-Federal | 92 | 92 | 92 | 92 | 93 | 93 | 93 | 93 | 93 | 93 |
| Community | 85 | 85 | 85 | 85 | 86 | 86 | 86 | 87 | 88 | 88 |
| Inpatient | 72 | 71 | 70 | 69 | 68 | 67 | 66 | 65 | 64 | 64 |
| Outpatient | 13 | 14 | 16 | 17 | 18 | 19 | 20 | 22 | 23 | 24 |
| Non-Community | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 6 | 5 |
| Federal | 8 | 8 | 8 | 8 | 7 | 7 | 7 | 7 | 7 | 7 |
| Annual Percent Growth | ||||||||||
| Total | 6.8 | 6.8 | 6.8 | 8.0 | 9.1 | 9.5 | 10.7 | 10.0 | 8.4 | 6.7 |
| Non-Federal | 6.7 | 6.7 | 7.0 | 8.2 | 9.5 | 9.6 | 10.8 | 10.0 | 8.7 | 6.8 |
| Community | 6.7 | 6.6 | 6.9 | 8.2 | 9.5 | 9.6 | 11.3 | 10.7 | 9.4 | 7.1 |
| Inpatient | 5.4 | 4.4 | 5.1 | 6.6 | 7.6 | 8.0 | 9.2 | 8.3 | 7.3 | 5.8 |
| Outpatient | 14.9 | 19.3 | 16.0 | 15.3 | 17.7 | 15.6 | 18.9 | 18.2 | 15.5 | 10.7 |
| Non-Community | 6.4 | 7.5 | 7.8 | 8.7 | 9.5 | 10.1 | 5.0 | 1.9 | -1.0 | 1.3 |
| Federal | 7.9 | 7.5 | 5.3 | 5.2 | 3.6 | 7.8 | 8.3 | 10.2 | 4.5 | 6.2 |
NOTE: Non-community, non-Federal hospitals include long-term care hospitals (where the average length of stay is 30 days or longer), psychiatric hospitals, alcohol- and chemical-dependency hospitals, units of institutions such as prison hospitals or college infirmaries, chronic disease hospitals, and some institutions for the mentally retarded.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Nearly all hospital care was financed by third parties, with only 2.8 percent paid by consumers in out-of-pocket expenditures. Coincident with recent decreases in out-of-pocket spending was a continued increase in private health insurance spending. In 1993, private health insurance financed 36.1 percent of hospital care, more than any other single payer. Public funding financed 56.0 percent, with the primary payers, Medicare and Medicaid, accounting for a 41.4-percent share. The remaining 5.2 percent of hospital revenues came from philanthropic and non-patient sources, such as hospital gift shops, parking facilities, and cafeterias.
Physician Services
Expenditures for physician services reached $171.2 billion in 1993 (21.9 percent of PHCE), an increase of 5.8 percent from the previous year. For the last 3 years, spending for physician services experienced the slowest growth since the early 1960s. This slow growth is linked to changes in the Medicare payment system and the expansion of managed care.
The Omnibus Budget Reconciliation Act of 1989 (Public Law 101-239) affected Medicare expenditures for physician services, beginning in 1990, by limiting the growth of reimbursement rates. Effective January 1,1992, this law also replaced the reasonable charge payment mechanism with the Medicare fee schedule (MFS) while establishing target rates of growth for physician services expenditures, and placed additional limits on the amount that non-participating physicians could charge Medicare beneficiaries for covered services (Federal Register, 1991).
As a result of the reductions already in place and anticipation of the upcoming MFS, 1991 growth of Medicare spending for physician services decelerated dramatically. When the MFS went into effect in 1992, growth of Medicare physician services slowed to only 3.1 percent. In 1993, as physicians became more familiar with the reimbursement rates and procedures, growth in Medicare spending accelerated to 7.6 percent.
During the same 3-year period, managed care became a larger part of physicians' practices, and more specialists began accepting prenegotiated fees for services provided. From 1988 to 1990, the percent of physicians with a managed-care contract remained relatively stable, around 61 percent. Starting in 1991, the percent of physicians contracting with at least one preferred provider organization (PPO), health maintenance organization (HMO), or individual practice arrangement rose an average of 5 percentage points a year. By 1993, three-fourths of all physicians had an arrangement with a managed-care plan (Emmons and Simon, 1994). The combination of changes in the Medicare reimbursement methodology and managed-care penetration caused overall growth in business receipts for physician offices and clinics to decelerate from 1991 to 1993.
According to the U.S. Bureau of the Census (1991-92), total taxable receipts for 1992 in offices and clinics of physicians amounted to $135.0 billion. For the same year, 42.2 percent, or $56.9 billion, of total receipts in offices and clinics of doctors of medicine resulted from the delivery of services in a doctor's office (Table 3). Services provided in a hospital setting accounted for $46.4 billion, two-thirds of which were for inpatient services and one-third for outpatient services. Laboratory and X-ray services, either furnished in the office or billed through the provider, amounted to 15.0 percent of physician services in 1992. The remaining portion of receipts was for services provided in nursing homes or private homes (0.7 percent), sales of prescription and non-prescription drugs, orthopedic appliances, and optical goods (1.2 percent), and other sources (6.5 percent).
Table 3. Taxable1 Receipts, by Type of Service Provided in Offices and Clinics of Doctors of Medicine: Calendar Years 1991-92.
| Type of Services | 1991 | 1992 |
|---|---|---|
| Amount in Millions | ||
| Total Receipts | $124,456 | $134,986 |
| Services Delivered in a Doctor's Office | 51,360 | 56,922 |
| Services Delivered in a Hospital | 44,623 | 46,391 |
| Inpatient | 29,929 | 30,568 |
| Outpatient | 14,694 | 15,823 |
| Services Delivered in Other Locations2 | 1,174 | 973 |
| Laboratory and X-Ray Services | 19,972 | 20,289 |
| Merchandise Sales3 | 1,434 | 1,620 |
| Other Sources4 | 5,893 | 8,791 |
| Percent Distribution | ||
| Total Receipts | 100.0 | 100.0 |
| Services Delivered in a Doctor's Office | 41.3 | 42.2 |
| Services Delivered in a Hospital | 35.9 | 34.4 |
| Inpatient | 24.0 | 22.6 |
| Outpatient | 11.8 | 11.7 |
| Services Delivered in Other Locations2 | 0.9 | 0.7 |
| Laboratory and X-Ray Services | 16.0 | 15.0 |
| Merchandise Sales3 | 1.2 | 1.2 |
| Other Sources4 | 4.7 | 6.5 |
NHE estimates of physician services also include receipts of tax-exempt physician offices and clinics (including HMOs), clinics and offices of osteopathic physicians, and receipts of independently billing laboratories.
Includes patient care services delivered in a nursing home or private residence.
Includes receipts from the sale of prescription and non-prescription drugs, optical goods, and orthopedic appliances.
Includes receipts not elsewhere classified.
SOURCE: (U.S. Bureau of the Census, 1984-92).
Approximately two-thirds of physician services, $113.1 billion, were financed through private sources in 1993. Out-of-pocket expenditures for physician services accounted for $26.2 billion; private health insurance, $84.1 billion; and non-patient revenue, $2.7 billion of spending in 1993.
Public funding, the source of the remaining one-third of physician expenditures, amounted to $58.1 billion and consisted primarily of Medicare and Medicaid. Medicaid paid $12.5 billion for physician services (7.3 percent), and Medicare paid $34.8 billion (20.3 percent).
Dental Services
Expenditures for dental services grew to $37.4 billion in 1993, an increase of 7.7 percent over the $34.7 billion spent in 1992. Since 1990, dental services was the only PHC category not to experience a deceleration in the rate of expenditure growth. One explanation for this atypical trend is concern about AIDS. Dental offices increased their purchases of disposable equipment and supplies to protect both patients and dental office personnel from the spread of AIDS.
Private funds accounted for 95.3 percent of dental service expenditures in 1993, a slight decrease from the 96.2 percent recorded in 1992. Within the private funds category, out-of-pocket expenditures for dental services remained steady at 50.0 percent in both 1992 and 1993, while private health insurance paid for 44.9 and 45.7 percent, respectively. Public sources of funds, primarily Medicaid, accounted for the remainder of the expenditures, 3.8 percent in 1992 and 4.7 percent in 1993.
Over the past 15 years, dental patients received more preventive care procedures relative to other dental procedures. The percentage of patients receiving diagnostic dental treatment consisting of oral examinations and X-rays increased from 51.7 percent in 1969 to 68.1 percent in 1990. The percentage of patients receiving one- and two-surface amalgam restorations decreased from 32.3 percent to 12.5 percent, while the percentage of patients receiving root canal and tooth extractions decreased from 12.7 percent in 1969 to 7.5 percent in 1990 (American Dental Association, 1994).
Other Professional Services
In 1993, $51.2 billion was spent for other professional services, an increase of 10.4 percent since 1992. This has consistently been one of the fastest growing segments of the NHA since 1960. (Only home health care has grown more rapidly over that 33-year period.) This is primarily the result of the growth of private health insurance coverage for licensed other professionals (such as chiropractors, psychologists, and optometrists) and freestanding specialty clinics (U.S. Bureau of Labor Statistics, 1980-93). Of total other professional services spending, 79.3 percent comes from out-of-pocket, private health insurance, and non-patient revenues sources. The remaining 20.7 percent is from public sources such as Medicaid, Medicare, and workers' compensation.
Home Health Care
The national health expenditures (NHE) category of home health care includes expenditures for services and supplies furnished by non-facility-based home health agencies (HHAs). Providers of home health care services include Medicare- and/or Medicaid-certified HHAs, non-certified HHAs, and persons delivering home health care services financed by Medicaid. In 1993, expenditures for home health care included in the NHE reached $20.8 billion. An additional $4.1 billion, not included in the NHE home health category, was expended for care furnished by facility-based—primarily hospital-based—HHAs (included with hospital care in this article). Including the hospital share, $24.9 billion was spent for home health care services in 1993 (Table 4).
Table 4. Total NHE, Medicare, Medicaid, and Other Spending for Home Health Care, Facility-Based and Non-Facility-Based: Selected Calendar Years 1960-93.
| Year | Total NHE Home Health | Medicare | Medicaid | Other Sources Total2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Total | Facility-Based HHA1 | Non-Facility-Based HHA2 | Total | Facility-Based HHA1 | Non-Facility-Based HHA2 | Total | Facility-Based HHA1 | Non-Facility-Based HHA2,3 | ||
|
| ||||||||||
| Amount in Millions | ||||||||||
| 1960 | $47 | $0 | $47 | — | — | — | — | — | — | $47 |
| 1970 | 193 | 11 | 182 | $69 | $9 | $60 | $17 | $2 | $15 | 107 |
| 1980 | 2,085 | 202 | 1,883 | 754 | 100 | 653 | 389 | 102 | 288 | 942 |
| 1985 | 5,558 | 622 | 4,936 | 1,944 | 346 | 1,598 | 1,180 | 276 | 904 | 2,434 |
| 1986 | 6,422 | 810 | 5,612 | 1,942 | 414 | 1,528 | 1,443 | 396 | 1,047 | 3,037 |
| 1987 | 6,946 | 1,025 | 5,921 | 1,912 | 446 | 1,466 | 1,803 | 579 | 1,225 | 3,231 |
| 1988 | 7,629 | 1,191 | 6,437 | 2,082 | 495 | 1,587 | 2,039 | 697 | 1,342 | 3,508 |
| 1989 | 9,444 | 1,368 | 8,076 | 2,580 | 602 | 1,978 | 2,471 | 766 | 1,706 | 4,392 |
| 1990 | 12,878 | 1,822 | 11,056 | 3,954 | 944 | 3,010 | 3,006 | 877 | 2,129 | 5,918 |
| 1991 | 15,613 | 2,435 | 13,178 | 5,696 | 1,440 | 4,255 | 3,477 | 995 | 2,482 | 6,441 |
| 1992 | 19,968 | 3,185 | 16,783 | 7,964 | 2,049 | 5,914 | 3,966 | 1,135 | 2,830 | 8,039 |
| 1993 | 24,858 | 4,078 | 20,781 | 10,862 | 2,790 | 8,072 | 4,518 | 1,287 | 3,231 | 9,478 |
Included in the hospital spending category of the national health accounts (NHA).
Estimated spending reported in the home health care category of the NHA.
Medicaid spending for home health care delivered by non-facility-based HHAs and providers not affiliated with a formal HHA.
NOTES: NHE is national health expenditures. HHA is home health agency.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Expenditures for home health care grew faster than any other category of PHC in 4 out of the past 5 years. Growth in spending for home health care decelerated slightly from 27.4 percent in 1992 to 23.8 percent in 1993.
Public financing accounted for about one-half of expenditures for home health care services. Medicare's share of public spending rose from 53.4 percent in 1989 to 70.9 percent in 1993. As a result of clarified home health coverage criteria, fewer Medicare claims are being denied. Almost all of the residual public spending was paid by Medicaid. The share of home health care paid for out of pocket has slowly decreased to 20.8 percent in 1993, down from a high of 24.7 percent in 1988. The balance of private spending, 24.4 percent in 1993, was split between private health insurance and non-patient revenue. As explained later, these estimates have been revised to reflect the broader home health industry portrayed by newly available data. These estimates still do not include home health services delivered by facility-based agencies (included in the NHE hospital category) or by unpaid caregivers. Also not included are services such as homemaker or social services, and nursing services provided by nurse registries classified as temporary-help agencies.
Preliminary data on HHAs from the National Center for Health Statistics' 1992 and 1993 National Home and Hospice Care Surveys show a 5.7-percent growth in the number of HHAs, from 7,000 in 1992 to 7,400 in 1993. This survey also shows the number of current patients (1.4 million in 1993) and discharged HHA patients (3.7 million in 1993), which increased 17.1 percent and 19.8 percent, respectively, from 1992 (Strahan, 1993, 1994).
Drugs and Other Medical Non-Durables
Retail purchases of drugs and other non-durable medical products were $75.0 billion in 1993 (Table 5), a 5.9-percent increase over the $70.8 billion in purchases in 1992. Retail purchases of prescription drugs were $48.8 billion in 1993, accounting for 65.2 percent of the purchases of non-durable medical products. The remaining 34.8 percent of the purchases of nondurable medical products were for over-the-counter (OTC) drugs and medical sundries. Purchases of OTC drugs and medical sundries were $26.1 billion in 1993, a 4.4-percent increase over the $25.0 billion in purchases in 1992.
Table 5. Expenditures for Drugs and Other Medical Non-Durables,1 by Source of Funds: Selected Years 1960-93.
| Source of Funds | 1960 | 1970 | 1980 | 1985 | 1987 | 1989 | 1990 | 1991 | 1992 | 1993 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Billions | ||||||||||
| Drugs and Other Non-Durable Medical Products | $4.2 | $8.8 | $21.6 | $37.4 | $45.4 | $54.4 | $61.2 | $67.1 | $70.8 | $75.0 |
| Prescription Drugs | 2.7 | 5.5 | 12.0 | 21.4 | 27.0 | 33.4 | 38.2 | 42.8 | 45.7 | 48.8 |
| Out-of-Pocket Payments | 2.6 | 4.5 | 7.9 | 11.7 | 14.2 | 16.9 | 18.2 | 19.3 | 20.4 | 21.2 |
| Third-Party Payments | 0.1 | 1.0 | 4.1 | 9.7 | 12.8 | 16.5 | 20.0 | 23.5 | 25.3 | 27.6 |
| Private Health Insurance | 0.0 | 0.5 | 2.4 | 6.6 | 8.5 | 11.1 | 13.6 | 15.8 | 17.1 | 18.4 |
| Medicaid | — | 0.4 | 1.4 | 2.5 | 3.4 | 4.2 | 5.1 | 6.2 | 6.7 | 7.7 |
| General Assistance | 0.0 | 0.0 | 0.1 | 0.4 | 0.5 | 0.8 | 0.9 | 0.9 | 0.9 | 0.9 |
| Other Government | 0.1 | 0.0 | 0.1 | 0.2 | 0.3 | 0.4 | 0.4 | 0.5 | 0.5 | 0.6 |
| Non-Prescription Drugs and Other Medical Non-Durables2 | 1.6 | 3.3 | 9.6 | 16.0 | 18.4 | 21.0 | 23.0 | 24.3 | 25.0 | 26.1 |
| Out-of-Pocket Payments | 1.6 | 3.3 | 9.6 | 16.0 | 18.4 | 21.0 | 23.0 | 24.3 | 25.0 | 26.1 |
| Percentage Distribution by Source of Funds Within Each Category | ||||||||||
| Prescription Drugs | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Out-of-Pocket Payments | 97 | 82 | 66 | 55 | 53 | 51 | 48 | 45 | 45 | 43 |
| Third-Party Payments | 3 | 18 | 34 | 45 | 47 | 49 | 52 | 55 | 55 | 57 |
| Private Health Insurance | 1 | 9 | 20 | 31 | 32 | 33 | 35 | 37 | 37 | 38 |
| Medicaid | — | 8 | 12 | 12 | 13 | 13 | 13 | 15 | 15 | 16 |
| General Assistance | 0 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Other Government | 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Non-Prescription Drugs and Other Medical Non-Durables2 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Out-of-Pocket Payments | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
This class of expenditure is limited to spending for products purchased in retail outlets. The value of drugs and other products provided by hospitals, nursing homes, or other health professionals is implicit in estimates of spending for these providers' services.
Assumes no third-party payments for non-prescription drugs and other medical non-durables.
NOTES: Numbers and percentages may not add to totals because of rounding. 0.0 denotes amounts less than $50 million.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Over the past 10 years, purchases of nondurable medical products have been a relatively stable portion of total PHCE, ranging from 9.6 to 10.0 percent For most of the past decade, retail purchases of prescription drugs have increased faster than total PHCE. In the 2 most recent years, however, the growth in retail purchases of prescription drugs has decelerated more rapidly than the growth in total PHCE. In 1992 and 1993, retail purchases of prescription drugs increased 7.0 and 6.8 percent, respectively, while total PHCE increased 8.8 and 7.2 percent This slowdown in the growth of prescription drug spending reflects recent changes in industry pricing practices, such as the increase in the number of manufacturers paying rebates, as well as increased penetration in the prescription drug market by managed-care plans.
Typically, third parties cover prescription drug purchases but not OTC medicines and sundries. For that reason, all third-party payments are assumed to be for prescription drugs. Therefore, the entire $26.1 billion of non-prescription items was attributed to out-of-pocket payments. An additional $21.2 billion in out-of-pocket payments went for prescription drug purchases or to cover copayments and deductibles for those with third-party coverage. Third parties paid for 56.5 percent of prescription drugs, or $27.6 billion, a share that has been increasing over the past 33 years. Third-party payments were dominated by private health insurance and Medicaid, with other government programs financing only a small portion.
Vision Products and Other Medical Durables
Expenditures for vision products and other medical durables amounted to $12.6 billion in 1993, an increase of 5.3 percent over the 1992 level of $12.0 billion. The durable medical equipment (DME) category includes retail purchases of eyeglasses and contact lenses and the purchase or rental of other durable medical products such as wheelchairs, crutches, hearing aids, and artificial limbs. Private sources of funds account for most DME purchases. The share of out-of-pocket payments for DME decreased slightly as a percent of total, from 60.9 percent in 1992 to 60.0 percent in 1993. The share of total DME expenditures financed by private health insurance also decreased—from 7.6 percent in 1992 to 7.0 percent in 1993. Public funding of DME expenditures, primarily Medicare payments, increased from 31.5 percent of the total in 1992 to 33.0 percent in 1993.
Nursing Home Care
Expenditures for nursing home care reached $69.6 billion in 1993, an increase of 6.3 percent from 1992. Growth in spending for nursing home care has decelerated for the third successive year from a high of 12.0 percent in 1990.
Nursing home expenditures are estimated in three parts: revenues of non-Federal facilities primarily providing some level of inpatient nursing care; Medicaid funding of ICFs/MR; and funding for care in Department of Veterans Affairs nursing homes.
Growth in spending for nursing home care other than in ICFs/MR (88 percent of total estimated expenditures for nursing home care) slowed from 8.2 percent in 1992 to 6.3 percent in 1993. This slowdown was the result of deceleration in the growth of nursing home personnel work-hours and unchanged growth in nursing home input prices. Aggregate hours worked by non-supervisory personnel in nursing- and related-care facilities decelerated from 4.2 percent in 1992 to 2.0 percent in 1993. HCFA's national nursing home input price index grew 4.0 percent in both 1992 and 1993.
These nursing home estimates imply that the average charge per day for care in nursing home facilities reached $106 in 1993, more than double the charge per day in 1983.
ICF/MR care is a Medicaid benefit first offered in 1973. In 1993, $8.3 billion was spent for ICF/MR care in nursing homes, 5.8 percent greater than in 1992. Revisions to the Medicaid estimating methodology reflect a gradual increase in the nursing home share of all ICF/MR expenditures from about 60 percent in 1980 to 90 percent in 1993. From 1973 to 1981, the rapid growth in spending for ICF/MR care raised the annual growth rates for total nursing home spending despite the relatively small amount of ICF/MR expenditures. Since that time, ICF/MR growth has had little effect on growth in total spending for nursing home care.
Public programs, mainly Medicaid, financed 62.6 percent of expenditures for nursing home care in 1993, the largest share ever funded by government. Medicaid accounted for 90 percent of public spending for nursing home care from 1972 to 1988, dropping to 82.6 percent in 1993. The drop in Medicaid's share was offset by a corresponding increase in Medicare's share. Medicare's share of public spending for nursing home care rose dramatically from 4.1 percent in 1988 to 14.0 percent in 1993. Most of this increase is attributable to provisions of the 1988 Medicare Catastrophic Coverage Act (MCCA) that became effective prior to repeal of the Act in 1989, and to clarification of program conditions for payment. Almost all nursing home care financed through private sources is paid by patients or their families. Out-of-pocket payments amounted to $23.0 billion in 1993.
Other Personal Health Care
In 1993, spending for other PHC reached $18.2 billion, 2.3 percent of all PHCE. Expenditures for this NHE category came from a variety of public programs (84.5 percent) and from industrial inplant health care services offered by employers at the work site (15.5 percent).
Medicaid paid for more than one-half of public expenditures for health screening services, certain home and community-based waiver services, case management, and additional miscellaneous services not included in any other PHC category. Also included in this category are expenditures for services through State and local school health and maternal and child programs, and Federal agency programs targeting veterans, military personnel, Native Americans, and persons with drug- and alcohol-dependency and mental health-related problems.
Administration and Net Cost of Private Health Insurance
Governments spent $9.2 billion in the administration of public programs in 1993, an 11.4-percent increase from 1992. Nine-tenths of these expenditures are attributable to the Medicare and Medicaid programs. Administrative costs accounted for 2.0 percent of all Medicare expenditures in 1993, and for 4.3 percent of all Federal, State, and local Medicaid expenditures. Philanthropic administration was estimated at $0.7 billion in 1993.
The difference between private health insurance premiums earned and benefits incurred is defined as the net cost of health insurance. Included in the net cost are administrative costs of insurers, net additions to reserves, rate credits and dividends, premium taxes, and profits or losses of insurance companies. Net cost amounted to $30.6 billion in 1992 and $38.1 billion in 1993. Growth in net cost increased 5.7 percent in 1992 and 24.5 percent in 1993. Lower-than-expected benefit costs, primarily in 1993, contributed to the sizable increase in net cost. Health care providers responded to the anticipation of health care reform by containing cost increases for goods and services. Another factor was increased physician participation in some form of managed care where prices for services are negotiated.
Government Public Health
Various levels of government spent $24.7 billion in public health activities in 1993. Almost nine-tenths of these expenditures, amounting to $21.4 billion, came through State and local health departments. The remaining $3.3 billion is comprised of expenditures by the Federal Government, concentrated in the U.S. Public Health Service's Centers for Disease Control and the monitoring activities of the Food and Drug Administration.
Spending for State and local public health programs amounted to $21.4 billion in 1993, an increase of 3.5 percent over the previous year. The sizable revision shown for 1991 (down $1.5 billion from previously published estimates) is the result of incorporating newly available survey data.
Research
The Nation spent $14.4 billion on noncommercial research activities in 1993, 1.1 percent more than in 1992. Only a small portion of non-commercial research was financed through private philanthropic sources—8.7 percent in 1993. The remainder came from Federal funds (77.0 percent), primarily through the National Institutes of Health, and from State and local governments (14.3 percent). These figures exclude spending by U.S. drug companies on research and development, estimated by the Pharmaceutical Research and Manufacturers of America (1994) at $12.6 billion.
Construction
Medical facility construction put in place (including new construction and renovation of existing hospitals, nursing homes, sanatoria, and convalescent homes) was valued at $14.6 billion for 1993, a 10.8-percent increase over 1992. According to statistics reported by the U.S. Bureau of the Census (1991), renovations of existing health care facilities could represent up to 70 percent of all new construction. Private business expenditures financed the largest share of all construction (69.4 percent), while the remaining funds came from philanthropy (4.8 percent), Federal Government (6.4 percent), and State and local governments (19.4 percent).
Trends in Sources of Funding
The division of spending between public and private sources of care changes periodically with the implementation of major new government programs or expansions in existing programs. From 1965 to 1967, the share of health expenditures funded from public sources jumped from 24.7 percent to 36.9 percent as the Medicare and Medicaid programs were implemented. Between 1972 and 1974, the public funding share jumped again, from 38.1 percent to 40.3 percent, as the Medicare program expanded coverage to the disabled population. For the next 17 years, the public share remained fairly constant, ranging from 40.3 percent to 41.9 percent of the NHE. Beginning in 1991, the public share began to rise, reaching 43.9 percent of the NHE in 1993. Growth in spending by the Medicaid and Medicare programs, exceeding growth in overall health expenditures, produced this shift. This growth is linked to Medicaid eligibility expansions, Medicaid disproportionate share payments to hospitals caring for a large proportion of low-income patients, the effect of the Boren Amendment, and continued growth in Medicare hospital admissions.
Private Sources
In 1993, consumers paid $157.5 billion out of pocket for the purchase of PHC, an increase of 4.6 percent from the previous year. Out-of-pocket payments accounted for 20.1 percent of PHCE. This share has been decreasing consistently across all services since 1960, as public programs and private health insurance pay a growing share of PHCE.
Since 1991, the portion of health care paid by private health insurance has remained relatively constant, hovering around 33 percent. Private health insurance premiums, amounting to $272.7 billion in 1992 and $296.1 billion in 1993, include premiums paid by employers or unions, employee share of employer- or union-sponsored premiums, and premiums paid entirely by persons purchasing policies independently or through associations. Since 1991, aggregate premium increases have remained in the single digits: 7.9 percent in 1992 and 8.6 percent in 1993. One factor that contributed to this trend is the overall deceleration in medical care price inflation. The medical care component of the Consumer Price Index for all urban consumers showed an increase of only 6.0 percent in 1993, the lowest in 4 years (U.S. Bureau of Labor Statistics, 1993).
Persons covered by private health insurance received benefits amounting to $242.1 billion in 1992 and $258.1 in 1993, an overall annual percentage increase of 8.2 percent and 6.6 percent, respectively. Employers, the largest purchasers of health insurance, continued to look for ways to lower health care costs while still providing employees with effective health care coverage. An increasingly effective method was the migration of employers out of indemnity plans into managed-care plans. In addition, employers who continued to offer traditional indemnity plans managed these plans more closely by increasing cost sharing with employees, limiting specific benefits (such as mental health), coordinating benefits among insurers, and implementing utilization management (Foster Higgins, 1994; KPMG Peat Marwick, 1993).
In 1993, $27.2 billion of PHCE was supported through non-patient revenues—that is, revenues received from philanthropic sources or from other non-patient services such as gift shop operations, cafeteria sales, and educational program revenues. Non-patient revenues financed 3.5 percent of PHCE. The majority of non-patient revenues (61.9 percent) funded hospital care.
Public Sources
Public sources paid for 43.9 percent of the NHE in 1993, a 2.8-percentage point increase in the public funding share since 1990. This rapidly rising public share came entirely from the Federal Government, whose share increased 3.6 percentage points during this period, while the share paid by State and local governments fell by 0.9 percentage point Federal responsibility for health care financing through the Medicare and Medicaid programs broadened in recent years with the clarification of payment rules and the widening of program eligibility requirements, as well as reasons discussed later.
The proportion of total government spending allocated to health programs continued to increase in 1993. Federal spending on health programs accounted for 18.6 percent of all Federal spending in 1993, up from 15.4 percent in 1990 (Table 6). State and local government spending on health programs was 12.4 percent of total spending in 1993, down from the prerecession high of 12.9 percent in 1990.
Table 6. Government Health Expenditures as a Percent of Total Government Expenditures: Selected Years 1960-93.
| Year | Federal Expenditures | State and Local Expenditures |
|---|---|---|
|
| ||
| Percent | ||
| 1960 | 3.1 | 7.8 |
| 1965 | 3.9 | 7.6 |
| 1966 | 5.2 | 7.5 |
| 1967 | 7.3 | 7.6 |
| 1970 | 8.5 | 7.8 |
| 1975 | 10.0 | 8.5 |
| 1980 | 11.7 | 9.9 |
| 1985 | 12.7 | 11.0 |
| 1990 | 15.4 | 12.9 |
| 1991 | 16.9 | 12.8 |
| 1992 | 17.4 | 12.6 |
| 1993 | 18.6 | 12.4 |
SOURCES: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics; and the U.S. Department of Commerce, Bureau of Economic Analysis.
Medicare
As of July 1, 1993, 36.3 million aged and disabled persons were enrolled in Medicare. The program spent $151.1 billion in PHC (benefit) payments for expenses incurred by the 29.0 million enrollees who received benefits in 1993 (Table 7). Growth in Medicare spending for PHC decelerated from 12.4 percent in 1992 to 11.6 percent in 1993. Excluding the exceptional growth observed in 1989 because of effects of legislation and clarification of program coverage criteria, the 1992 and 1993 growth rates were the highest since 1983.
Table 7. Personal Health Care Expenditures Under Medicare and Medicaid and Sources of Medicare Financing: Selected Calendar Years 1966-93.
| Medicare Financing
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Personal Health Care Expenditures
|
Population
|
Inpatient Hospital Deductible6 | Supplementary Medical Insurance Monthly Premium7 | Annual Maximum Taxable Earnings | Contribution Rate8,9 | |||||
| Year | Medicare and Medicaid2 | Medicare | Medicaid | Medicare1
|
Medicaid Recipients5 | |||||
| Enrollees3 | Users4 | |||||||||
|
| ||||||||||
| Amount in Billions | Number in Millions | Amount in Dollars | Percent | |||||||
| 1966 | $3.0 | $1.7 | $1.3 | 19.1 | 3.7 | — | $40 | $3.00 | $6,600 | 0.35 |
| 1967 | 7.8 | 4.8 | 3.0 | 19.5 | 7.2 | — | 40 | 3.00 | 6,600 | 0.50 |
| 1972 | 16.9 | 8.9 | 8.0 | 21.3 | 10.0 | 17.6 | 68 | 5.80 | 9,000 | 0.60 |
| 1973 | 19.3 | 10.2 | 9.1 | 23.5 | 10.2 | 19.6 | 72 | 106.30 | 10,800 | 1.00 |
| 1980 | 61.2 | 36.4 | 24.8 | 28.5 | 18.0 | 21.6 | 180 | 9.60 | 25,900 | 1.05 |
| 1985 | 109.5 | 70.3 | 39.2 | 31.1 | 22.3 | 21.8 | 400 | 15.50 | 39,600 | 1.35 |
| 1989 | 159.3 | 100.1 | 59.2 | 33.6 | 26.2 | 23.5 | 560 | 1131.90 | 48,000 | 1.45 |
| 1990 | 181.3 | 109.6 | 71.7 | 34.2 | 27.2 | 25.3 | 592 | 28.60 | 51,300 | 1.45 |
| 1991 | 210.4 | 120.5 | 89.9 | 34.9 | 27.7 | 28.3 | 628 | 29.90 | 125,000 | 1.45 |
| 1992 | 239.1 | 135.4 | 103.6 | 35.6 | 28.1 | 30.9 | 652 | 31.80 | 130,200 | 1.45 |
| 1993 | 263.9 | 151.1 | 112.8 | 36.3 | 1229.0 | 33.4 | 676 | 36.60 | 135,000 | 1.45 |
Hospital insurance and/or supplementary medical insurance (SMI).
Excludes buy-in premiums paid by Medicaid for SMI coverage of aged and disabled Medicaid recipients eligible for coverage.
Enrollees as of July 1 of specified year.
Enrollees with some reimbursement under Medicare during calendar year. Data through 1973 reflect aged users only. Data for 1974 and later include aged and disabled users.
Unduplicated count of Medicaid recipients during fiscal year.
As of January of specified year with the exception of 1966, for which July data are used.
As of July for 1966-83 and as of January for 1984 and later.
Employer and employee (each) and self-employed persons through 1983.
Effective in 1984, self-employed persons pay double this rate, the equivalent of both the employer and the employee share.
Monthly premiums for July and August 1973 were reduced to $5.80 and $6.10, respectively, by the Cost of Living Council.
Includes $27.90 SMI monthly premium and $4.00 catastrophic coverage monthly premium.
Estimated.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Medicare continues to increase its share of total spending for PHC. In 1993, Medicare financed 19.3 percent of total spending for PHC and 44.8 percent of the public share of PHCE. Annual Medicare expenditures for benefits increased from $109.6 billion in 1990 to $151.1 billion in 1993, or $41.5 billion. Most of this increase (58.3 percent) is attributable to spending for hospital care. Payments for home health care accounted for 12.2 percent of this increase; physician services, 11.7 percent; and all other services, 17.8 percent.
Medicare's share of funding for all hospital expenditures was 28.4 percent in 1993, the highest this share has been since the mid-1980s. An indication of increased hospital utilization for the Medicare population can be seen in data from the American Hospital Association (AHA). AHA National Hospital Panel Survey (1990-93) data indicate that the annual number of community hospital admissions for persons 65 years of age or over grew 7.3 percent between calendar years 1990 and 1993, while admissions for persons under 65 years of age declined by 5.5 percent. Inpatient days of care dropped for both groups over this period but more dramatically for the under 65 years of age group (a 10.8-percent drop compared with a 2.0-percent decline for the 65 years of age or over population).
Medicare primarily funds hospital care and physician services. Hospital care accounted for over 70 percent of Medicare benefits in the early 1980s but has steadily declined since then. In 1993, 61.3 percent of Medicare benefits were for hospital care and another 23.0 percent for physician services.
Medicare expenditures for hospital care reached $92.7 billion in 1993, an increase of 10.1 percent from 1992. These expenditures for hospital care services, including inpatient, outpatient, and hospital-based HHA services, grew at double-digit rates for the second consecutive year.
Medicare expenditures for physician services increased from $32.4 billion in 1992 to $34.8 billion in 1993, a growth of 7.6 percent. Strategies designed to decelerate the growth in Medicare spending for physician services effectively slowed growth from 12.2 percent in 1989 to 4.8 percent in 1991. Efforts to control growth continued with implementation of the MFS in January 1992. The MFS is based on a national Resource-Based Relative Value Scale and will be phased in over a 4-year period. Growth in Medicare spending for physician services slowed to 3.1 percent in 1992.
Medicare paid $8.1 billion for home health care furnished by non-facility-based HHAs in 1993. Annual growth in Medicare expenditures for home health care (36.5 percent in 1993) has ranged from 25 percent to 50 percent since its home health coverage criteria were clarified in 1988. Historically, with the exception of a few years in which more stringent regulations were applied, Medicare has financed 30-40 percent of the Nation's spending for home health care services.
Medicare spent $6.1 billion for skilled nursing facility (SNF) care in 1993, 35.3 percent more than in 1992. Spending in 1993 was almost sevenfold greater than spending in 1988. Dramatic changes in annual growth rates were triggered by Medicare's clarification of its conditions for payment of SNF benefits and the passing of the MCCA. Certain provisions of the MCCA affecting SNF payments became effective in 1989 before its repeal. Medicare's share of national spending for nursing home care grew from 2.1 percent in 1988 to 8.8 percent in 1993.
Medicaid
Medicaid expenditures, which equaled 14.4 percent of total PHCE in 1993, largely fund institutional services. In 1993, for example, hospital care and nursing home care accounted for 37.6 and 31.9 percent, respectively, of the $112.8 billion in combined Federal and State Medicaid spending. Medicaid continues to be the largest third-party payer of long-term care spending, financing 51.7 percent of nursing home care in 1993, a percentage that has been increasing for the last 4 years.
In 1992 and 1993, growth in Medicaid spending slowed to 15.3 percent and 8.8 percent, respectively, following 3 years of accelerating growth for almost all categories of service. Although decelerating, Medicaid expenditures have continued to grow because of the Boren Amendment (which requires reasonable and adequate payment for services rendered); Federal requirements for increased coverage of mothers and children and certain low-income, aged, and disabled Medicare enrollees; and increased payments to disproportionate share hospitals (DSH) (facilities serving a disproportionate share of Medicaid recipients or other low-income populations) (Letsch et al., 1992). These factors, coupled with general economic decline in 1990 and 1991, placed additional demands on States to finance their share of Medicaid expenditures.
Many States, under severe budget constraints, looked to creative financing techniques to meet their increasing Medicaid financial responsibilities. Efforts focused on soliciting voluntary donations from hospitals and imposing provider taxes on certain health care services. Collections of provider-based taxes and voluntary donations (T&D) were significantly higher in 1991 and 1992 than in 1993, when the 1991 Medicaid Voluntary Contribution and Provider-Specific Tax (MVCPT) Amendments (Public Law 102-234) took effect. These amendments were created in response to concern that the use of provider-related T&D to fund DSH payments contributed to spiraling Medicaid costs. They disallowed Federal matching funds for donations by, or on behalf of, health care providers and allowed only matching funds for broad-based taxes that did not hold taxpayers harmless for the cost of the tax. A grandfather clause was included in the legislation to allow for the use of provider donations and tax programs during a transition period. Most States were required to adhere to the new rule beginning in October 1992; however, two States were granted extensions until January 1, 1993, and nine States were granted extensions until July 1, 1993. The amendments immediately imposed a cap on taxes and donations—25 percent of the total non-Federal share of Medicaid program expenditures in that fiscal year (Health Care Financing Administration, 1992).
During the period in which States were seeking increased revenues, the Medicaid program focused increased attention on needy hospitals by enabling them to receive DSH payments which were eligible for Federal matching funds. However, concern developed that some States with T&D programs could repay providers for their T&D through the State's determination that the facility served a disproportionate share of the State's low-income population (Letsch et al., 1992), thus increasing T&D, DSH payments, and overall Medicaid expenditures. The 1991 MVCPT Amendments addressed this issue as well. Effective October 1,1992, was the imposition of a State limit on DSH payments of 12 percent of that State's Medicaid expenditures (not including administrative costs), as well as a national limit of 12 percent of total Medicaid program expenditures. Those States with DSH payments above the 12-percent limit were not permitted to increase aggregate DSH payments, and States with DSH payments below the limit were allowed to increase payments to allow for growth (Health Care Financing Administration, 1992).
For the purposes of the NHA, certain Medicaid DSH payments to hospitals that were offset by donations and taxes paid by the same facilities were excluded, because these payments netted out and did not contribute to overall hospital operation. When these amounts were removed from Medicaid program-based estimates for State and local government expenditures, Medicaid growth was dampened. For example, from 1990 to 1992, without accounting for offsetting T&D receipts, New Hampshire inpatient hospital care expenditures skyrocketed, growing 3,530 percent, and Texas inpatient hospital care spending grew 244 percent Before offsetting adjustments were made, total Medicaid hospital care expenditures nationwide grew 115 percent from 1990 to 1992; after offsetting adjustments, these expenditures grew 54.9 percent during the same period. Growth rates decelerated in 1993 after the MVCPT Amendments limited DSH payments and T&D.
Part of the impetus for the 1991 amendments was concern that increases in T&D and DSH could lead to a long-term realignment of Federal and State responsibilities for Medicaid by effectively increasing the Federal share of Medicaid spending (Merlis, 1991). Although the MVCPT Amendments contained rising costs, the Federal share of total Medicaid program obligations moved from 56.9 percent in 1990 to 57.3 percent in 1993. In addition, the exclusion of the amount of DSH payments offset by T&D reduced State and local Medicaid payments, creating even greater increases in the effective Federal match rate for Medicaid. The NHE Medicaid Federal match rate moved from 56.6 in 1990 to 64.5 percent in 1993 (Table 8).
Table 8. Differences in Medicaid Expenditures as Reported to HCFA and as Estimated in the National Health Expenditures, and Effective Match Rates: 1988-93.
| 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | |
|---|---|---|---|---|---|---|
| Amount in Billions | ||||||
| Reported Medicaid Fiscal Year Expenditures:1 | ||||||
| Total | $53.6 | $60.5 | $72.1 | $90.6 | $116.9 | $129.1 |
| Federal | 30.2 | 34.2 | 41.0 | 51.8 | 67.1 | 74.0 |
| State and Local | 23.4 | 26.3 | 31.1 | 38.8 | 49.8 | 55.1 |
| Estimated National Health Accounts Medicaid Calendar Year Expenditures:2 | ||||||
| Total | 55.1 | 62.3 | 75.4 | 93.9 | 108.0 | 117.9 |
| Federal | 31.0 | 35.4 | 42.7 | 56.7 | 68.3 | 76.1 |
| State and Local | 24.1 | 26.8 | 32.7 | 37.2 | 39.7 | 41.8 |
| Percent | ||||||
| Effective Medicaid Federal Match Rates From: | ||||||
| Medicaid Reports1 | 56.3 | 56.5 | 56.9 | 57.2 | 57.4 | 57.3 |
| National Health Accounts Estimates2 | 56.3 | 56.8 | 56.6 | 60.4 | 63.2 | 64.5 |
| Difference3 | 0.0 | 0.3 | -0.3 | 3.2 | 5.8 | 7.2 |
As reported in HCFA Form-64 (financial settlement sheet for Federal match computations). Excludes Medicaid buy-ins.
ln the national health accounts, disproportionate share payments offset by taxes and donations in the same hospital are excluded from State and local spending. Also excludes Medicaid buy-ins.
Differences in 1989 and 1990 are caused by the difference in calendar year and fiscal year.
NOTE: HCFA is the Health Care Financing Administration.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Other Government
Government programs other than Medicare and Medicaid accounted for 13.1 percent of the NHE. The share of health expenditures funded by these other government programs has steadily declined in every year, dropping from 24.5 percent of health spending in 1960 to 19.8 percent in 1970 and 16.6 percent in 1980, as expenditures under Medicare and Medicaid played increasingly important roles in funding health care for aged, disabled, and low-income persons. In general, these programs provide health care services in their own facilities, through public insurance-type programs, or as grants to facilities to provide care to target populations. Target populations include groups such as military personnel and their families, veterans, Native Americans, refugees, temporarily disabled workers, persons with mental disorders or substance abuse problems, and mothers and children.
Revisions to Data Sources and Methods
This section contains a selected description of the data sources and methodology used to estimate health care expenditures. This discussion is limited to revisions that have been introduced in this article. Detailed information on data sources and methods not covered here can be found in Lazenby et al. (1992).
Types of Service
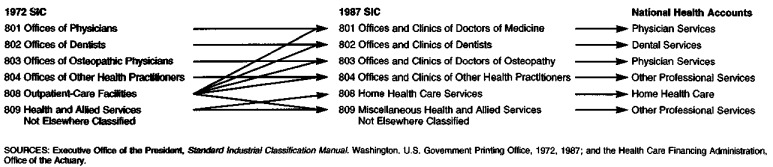
Many of the PHC component expenditure estimates presented here have been revised to incorporate the Standard Industrial Classification (SIC) revision introduced in 1987 (Executive Office of the President, 1987). SICs systematically classify all business establishments in the United States according to their economic activity and form the basis on which government-wide statistical information is collected. These codes are periodically revised according to information from government and other statistical users in order to capture the industrial structure of the Nation more effectively and to meet the statistical needs of policymakers. The 1987 revision contains several important changes to the health care sector. These changes permit the collection of government statistics that more accurately represent the major sectors of the health care industry.
The 1987 revision, the first comprehensive revision since 1972, contains changes to the classifications for offices and clinics of doctors of medicine, doctors of osteopathy, dentists, and other health practitioners, as well as outpatient clinics. In addition, the 1987 revision establishes a separate classification for home health care services. Previously, home health care was a portion of a broader SIC, health and allied services not elsewhere classified (Figure 3).
Figure 3. Comparison of 1972 and 1987 Standard Industrial Classifications (SIC) and National Health Expenditure Categories.
These changes affect the NHA in several ways. First, the changes combine clinics of physicians (including staff-model HMOs), dentists, and other health practitioners with the offices of these providers. Prior to the revisions, these clinics were reported in the NHE as part of other professional services. This revision more accurately portrays the entire range of services supplied by these providers, regardless of the site of care. Second, the creation of a home health care SIC separate from miscellaneous other health care SICs, permits government agencies to provide employment and business receipt information (valuable sources for NHE estimates) for this growing provider type for the first time.
The SIC revisions previously discussed were incorporated in the physician services estimates from 1977 forward based on data from the quinquennial Census of Service Industries (U.S. Bureau of the Census, 1977, 1982, 1987a) and the Services Annual Survey (SAS) (U.S. Bureau of the Census, 1984-92). Previously, estimates of spending for physician services required an addition of expenditures for services of salaried physicians in staff-model HMOs. This adjustment is no longer necessary because the 1987 SIC revision categorizes staff-model HMOs with offices and clinics of doctors of medicine.
In previous publications of the NHE (Letsch et al., 1992), estimates of dental expenditures were based primarily on statistics compiled and published by the Internal Revenue Service (IRS). Business receipts were summed for sole proprietorships, partnerships, and incorporated practices to form the bulk of the estimate. The steady deterioration of the timeliness and statistical variance of the IRS data beginning in the late 1970s prompted a modification of the estimation techniques used to compile the NHE. The SAS (U.S. Bureau of the Census, 1984-92) and the Census of Service Industries (U.S. Bureau of the Census, 1977, 1982, 1987a) that provide estimates of business receipts from dental establishments were used to construct this estimate.
From 1977 forward, expenditures for three major components of other professional services—licensed health professionals, specialty clinics, and miscellaneous health services—were estimated separately based on data from the SAS (U.S. Bureau of the Census, 1984-92) and the Census of Service Industries (U.S. Bureau of the Census, 1977, 1982, 1987a). For licensed other professionals, a portion of the optometrist receipts representing the dispensing of eyeglasses was deducted and reported instead under spending for DME. Since 1991, the SAS has been collecting information on the portion of optometrist receipts that represents business receipts from the sale of eyeglasses, increasing the accuracy of this adjustment
Home health care services became uniquely classified as an industry in the 1987 SIC Manual (Executive Office of the President, 1987). As this change was incorporated into the data collection systems of Federal Government agencies, revenue and employment data gradually became available. The new sources of data reflect a broader view of the home health service industry than could be inferred from Medicare and National League of Nursing data (Lazenby et al., 1992) used for earlier estimates. Therefore, estimates of expenditures for home health care presented in this article were revised upward for each year.
Data from the Census of Service Industries (U.S. Bureau of the Census, 1977, 1982, 1987a) were used to estimate home health service business receipts for 1987. Data on business receipts provided by the SAS (U.S. Bureau of the Census, 1984-92) were used to establish the level of home health expenditures for 1990-92. Expenditure growth in 1993 was estimated using growth in the number of non-government home health employee workhours (U.S. Bureau of Labor Statistics, 1992-93) and in home health input prices (Health Care Financing Administration, 1992-93). Revised expenditure estimates for 1960-86 were calculated from annual growth in the previous estimates.
The estimates of retail spending for prescription drugs were prepared using the preliminary results of a HCFA-sponsored study conducted by the Actuarial Research Corporation (ARC) (1994). The preliminary estimates of consumer spending on prescription drugs from the ARC study were based on manufacturers' sales to retail outlets. The ARC estimates of prescription drug spending by consumers were used to extrapolate the 1982 NHE estimates of prescription drug spending to 1992. The 1993 NHE estimates were prepared using data on the growth in prescription drug sales volume and prices gathered from industry sources. The result of the revised methodology was increased estimates of spending on prescription drugs for the years 1983 forward. The 1991 prescription drug estimate was increased by 15.0 percent. The final results of the ARC study will be incorporated in the next annual NHE update.
Revisions to nursing home expenditures presented in this report were caused primarily by a refinement to the procedure used to estimate Medicaid spending for ICF/MR nursing care. These refinements, described later, increased estimated expenditures for nursing home care from 1977-91.
Medicare program administrative expenses were revised to include the costs associated with the activities of Peer Review Organizations (PROs) and their predecessors, Professional Standard Review Organizations.
The value of new construction put in place (VPIP), estimated by the U.S. Bureau of the Census (1991), provided the basis for construction estimates. In 1991, the U.S. Bureau of the Census increased the level of VPIP from 1965 forward to reflect more accurately the amount of construction activity for the period. The substantial upward revisions to the private VPIP series—ranging from $0.3 billion for early years to $1.3 billion for 1991—were incorporated into NHE construction estimates for the first time.
Sources of Funding
Estimates of public expenditures for health care are derived from information furnished by the agency responsible for each program. Many of these statistics for the Federal Government are reported through the Budget Appendix of the United States. (Executive Office of the President, 1994).
There are few data sources available that comprehensively measure private sources of funding (out-of-pocket spending, private health insurance expenditures, or non-patient revenues) for the entire health care sector. Instead, estimates of private sources of funding are developed separately for each type of service because additional data from trade associations and other private sources are frequently available.
In general, estimates of total private expenditures for health care for each service were derived by subtracting all public sources of funding from the independently derived service expenditure totals. Private expenditures were then split into separate estimates for out-of-pocket, private health insurance, and non-patient revenue expenditures. These splits were based on information from the Consumer Expenditure Integrated Survey (U.S. Bureau of Labor Statistics, 1984-92); trade associations (e.g., American Hospital Association [1960-92], American Medical Association [1984-94], American Dental Association [1980-93], and Visiting Nurse Association of America [1988]); data from historical private health insurance studies (Carroll and Arnett, 1981); and periodic provider surveys such as the National Nursing Home Survey (National Center for Health Statistics, 1972, 1977, 1985). In addition, surveys of the non-institutionalized population's health care use and financing patterns, conducted over the past three decades, were examined in constructing historical estimates. The most recent survey of this type, the National Medical Expenditure Survey (Agency for Health Care Policy and Research, 1987) was integrated into these estimates. Beginning in 1991, the U.S. Bureau of the Census provided yet another source of receipts information for the offices and clinics of physicians, dentists, and other professionals and nursing homes in the SAS (U.S. Bureau of the Census, 1984-92).
Private health insurance benefits were estimated for each service in conjunction with the out-of-pocket estimates as discussed previously. Estimates for total private health insurance premiums were developed using financial data from the insurance industry. Net cost was estimated as the difference between insurance premiums and benefits.
To develop private health insurance premium estimates, estimates of premiums, benefits, and the net cost of private health insurance were formulated using information from the National Association of Blue Cross and Blue Shield (1960-93), Health Insurance Association of America (1994), Group Health Association of America, Inc. (1985-93), single-service dental plans, a survey of self-insured and prepaid health plans conducted by HCFA, and surveys of third-party administrators conducted by private organizations (Business Insurance, 1986-94; Employee Benefit Plan Review, 1985-93). The ratio of premiums to benefits developed from this insurance industry information was applied to the sum of private health insurance benefits estimated for each NHE service sector, thereby inflating benefits to premiums. These estimates were compared to estimates of private health insurance produced using the Employment Cost Index Survey (U.S. Bureau of Labor Statistics, 1984-93), the U.S. Bureau of Labor Statistics' Survey of Expenditures for Health Care Plans by Employers and Employees, 1992 (1993) and the Consumer Expenditure Integrated Survey (U.S. Bureau of Labor Statistics, 1984-92).
The only public source of funding to incorporate major revisions in methodology is Medicaid. Medicaid estimates for 1980 forward continue to be based on financial reports filed by State Medicaid agencies (HCFA Form-64). These reports contain total program expenditures by detailed service type. Beginning with estimates presented in this article, Medicaid expenditures were based on edited, State- and service-specific HCFA Form-64 data rather than national service aggregations.
Several adjustments to reported HCFA Form-64 data were necessary to fit the estimates into the framework of the NHA First, an expenditure estimate (based on HCFA Form-64 data) of Medicaid buy-ins to Medicare was deducted to avoid double counting when the programs are presented together. The second adjustment added an estimate of hospital-based home health care spending to hospital care and concomitantly subtracted it from home health care expenditures. Previously, the proportion of home health care expenditures reimbursed to hospital-based HHAs was derived from national Medicare program data. This method was revised to use State-specific rather than national Medicare proportions of hospital-based home health expenditures. These proportions were applied to State-specific Medicaid home health expenditures to derive the amount by State that is hospital-based and then summed to national totals.
The final adjustment counted that portion of reported program expenditures for ICFs/MR estimated to cover services in hospital-based facilities as hospital care rather than nursing home care. The movement toward the deinstitutionalization of the mentally retarded population, occurring since the late 1970s, triggered a modification in the previous methodology that assumed the share of hospital-based ICF/MR spending at 40 percent The revision incorporated the results of a facility-by-facility comparison of a 1982 University of Minnesota survey (Hill and Lakin, 1984) to AHA (1980-92) survey data for that same year. A relationship between University of Minnesota ICF/MR expenditures and AHA ICF/MR expenditures for 1982 was developed and then extrapolated to more recent years using AHA facility-specific expenditures, thus capturing any movements in the hospital share of ICFs/MR. The ratio of these hospital ICF/MR estimates (summed to a State level) to State-level Medicaid ICF/MR program data was used to construct a national hospital-based ICF/MR Medicaid estimate. Results of this new methodology confirmed that the Medicaid ICF/MR share of expenditures going to hospitals has continued to decrease throughout the 1980s, plummeting to just under 11 percent in 1993 from nearly 40 percent in 1980. This adjustment had no effect on the level of total hospital expenditures. However, it did lower previous estimates of Medicaid reimbursement for hospital care, and raise previous estimates of Medicaid reimbursement for nursing home care, where ICFs/MR is a separate component of that estimate.
Definitions
Types of Service
The NHA is a comprehensive measure of health spending by type of service and medical product and by source of funding. The NHA is arrayed in a three-dimensional matrix of health care services/products and funding sources over time. This structure permits both time-series and cross-sectional analyses.
The NHA contains varying levels of aggregation, with the most comprehensive level being the NHE. The NHE consists of all expenditures for medical services and products, government public health activities, administrative costs, net cost of private health insurance, non-commercial medical research, and construction of medical facilities. However, it excludes other indirect health care expenditures that may contribute to health status, such as government nutrition programs, safety programs, or public health programs such as water fluoridation and sanitation.
The NHE consists of HSS, a measure of current consumption of health care; and non-commercial research and construction of medical facilities, a measure of investment in health care. HSS measures spending for medical services and products, public health activities, administrative costs, and the net cost of private health insurance. PHC, a subset of HSS, measures spending for the delivery of medical services and the purchase of medical products. It consists of spending for hospital care, physician services, dental services, other professional services, home health care, nursing home care, durable and non-durable medical products, and miscellaneous other PHC.
Hospital care estimates cover spending for all hospital services provided to patients. Expenditures for hospital care cover fees charged for room and board, ancillary services such as operating room use, services of resident physicians, inpatient pharmacy services, hospital-based nursing home and home health care, and any other services billed by hospitals. Expenditures for services of physicians who bill independently for patients seen in hospitals are excluded.
The value of non-Federal hospital output is measured by total net revenues. This includes gross patient revenues (billed charges) reduced by the revenues of contractual adjustments with insurers, bad debts, and charity care. Also included are government tax appropriations; non-patient operating revenue, such as gift shop and cafeteria revenue, parking lot receipts, and educational program revenue; and non-patient, non-operating revenues, such as interest income, contributions, and grants. The value of Federal hospital output is measured in terms of Federal outlays for the operation of those facilities.
All hospitals in the United States and its outlying territories are represented in the NHA community and non-community hospitals estimates. Community hospitals are defined as non-Federal, acute-care hospitals whose average length of stay is less than 30 days and whose facilities and services are open to the general public. Non-community hospitals include long-term care hospitals, psychiatric hospitals, tuberculosis and other respiratory hospitals, chronic disease hospitals, alcohol- and chemical-dependency hospitals, some institutions for the mentally retarded, and hospital units of institutions such as prisons and college infirmaries. All Federal hospitals are also considered to be non-community hospitals, because they are not generally open to the public.
Non-Federal hospital estimates (both community and non-community) are constructed using AHA (1960-92) Annual Survey of Hospitals data. Federal hospital estimates are based on data from the Federal agencies that administer them.
Physician services include expenditures for services rendered by a Medical Doctor (M.D.) or by a Doctor of Osteopathy (D.O.) in an office or clinic (including ambulatory surgical centers and freestanding emergency medical centers). This category also includes services rendered by an M.D. or D.O. in hospitals if the physician bills independently for those services. Expenditures for services provided in staff-model and group-model HMO facilities are counted under physician services.
In addition to physician services provided in offices, clinics, and HMO establishments, the NHE category of physician services also includes expenditures for all laboratory services ordered through physicians' offices or clinics. Most of these services are billed though the physicians' offices or clinics; the remainder is independently billed by laboratories.
Professional fees received by physicians from hospitals are subtracted from the estimates of spending for physician services. Hospitals' professional fee arrangements with physicians include minimum guaranteed income, percentage of departmental billings, and bonuses. These fees are counted as hospital expenditures because they are paid from revenues received by hospitals based on services performed at that site. Including them under physician services would result in double counting these expenditures.
Expenditures for dental services capture payment for services received in offices or clinics of doctors of dental surgery or doctors of dental medicine. The receipts of dental laboratories are included in this category because all billings for dental laboratory services are assumed to be made through dental offices and are captured in the business receipts of dentists.
Other professional service expenditures include spending for services provided by independently practicing licensed health care practitioners other than physicians and dentists. Licensed other professionals include practitioners such as private duty nurses, chiropractors, psychologists, podiatrists, and optometrists. These expenditures also cover services delivered in kidney dialysis centers and in freestanding specialty outpatient clinics such as alcohol treatment centers, outpatient mental health clinics, and rehabilitation centers. In addition, this sector of the NHA includes spending for miscellaneous health and allied services not elsewhere classified and Medicare reimbursements for ambulance services.
Expenditures reported for home health care measure spending for medical care services delivered in the home by non-facility-based HHAs. Providers of home health care are establishments engaged primarily in furnishing skilled nursing or medical care in the home, under the supervision of a physician.
Expenditures for prescription drugs are limited to spending for products purchased from retail outlets. The value of drugs and other products provided to patients by hospitals (on an inpatient or outpatient basis) and nursing homes, and as part of a provider contact, is implicit in estimates of spending for each provider's services. The category of prescription drugs includes retail sales of human-use, dosage-form drugs, biologicals, and diagnostic products. The sales may occur in community or HMO pharmacies, grocery and department store pharmacies, mass merchandisers' pharmacies, or through mail-order establishment pharmacies.
Expenditures for non-prescription drugs and other medical sundries cover OTC drug purchases and purchases of other drug sundries, such as contraceptives and first-aid products. The estimate is based on personal consumption expenditures (PCE) (U.S. Bureau of Economic Analysis, 1960-93) for non-durable goods, a category of the GDP.
Expenditures for DME cover purchases of items such as eyeglasses, hearing aids, surgical appliances and supplies, bulk and cylinder oxygen, and equipment rental. This estimate, like that of non-prescription drugs, is based on PCE (Bureau of Economic Analysis, 1960-93) for durable goods.
Nursing home care expenditures measure the Nation's annual spending for inpatient nursing care. According to the 1987 SIC, nursing and personal-care facilities (SIC 805) are establishments engaged primarily in providing inpatient nursing and health-related personal care through active treatment programs for medical and health-related conditions. In addition to SNFs and intermediate care facilities, the estimates presented here include government outlays for care provided in nursing facilities operated by the Department of Veterans Affairs and for nursing services in ICFs/MR financed by the Medicaid program.
Other PHCE include private spending for inplant health services provided by employers to their workforce and public spending for miscellaneous services that are not classifiable elsewhere. Examples of these public expenditures include community-based waiver programs and case management funded by the Medicaid program; school-based health services; and shipboard or field-station medical operations of the Department of Defense.
The administrative costs incurred by government programs and philanthropic organizations, and the net cost of private health insurance are included in the administration and net cost of the private health insurance sector of the NHA The largest component of this estimate, the net cost of private health insurance, measures administrative costs faced by insurers and self-insurers, as well as insurers' net additions to reserves, rate credits and dividends, premium taxes, and profits and losses. Net costs are calculated as the difference between NHE benefits incurred and total premiums earned.
To the extent that information is available, this category also measures the administrative costs associated with operating government programs. For some programs, such as Medicare and Medicaid, these costs are easily measurable; for other programs, the costs can be estimated from budget information on overhead costs for a given government agency. For government programs for which no information was available, no estimate of administrative costs was made.
The smallest segment of administration and net cost of private health insurance is the administration of philanthropic organizations, which reflects indirect expenses of health-related activities in philanthropic establishments. These expenditures represent overhead expenses incurred by donor organizations that channel funds to research facilities or health providers.
In addition to funding the care of individual citizens, governments are involved in organizing and delivering health care in general, in the prevention and control of clinical health problems in the population, and in other such functions. In the NHA, spending for these activities is reported as government public health activity. Funding for health research and for construction of facilities is reported in their respective categories; spending for environmental functions (air and water pollution abatement, sanitation and sewage treatment, water supplies, etc.) is excluded.
Most Federal Government public health activity is funded through the Department of Health and Human Services. The Food and Drug Administration and the Centers for Disease Control account for an overwhelming majority of Federal spending in this area. Federal spending is taken from annual budget documents prepared by the various agencies and summarized in the Budget of the United States (Executive Office of the President, 1960-94).
State and local expenditures for public health programs are principally those made by State and local health departments. Their focus is primarily on the prevention and control of disease. Local centers for disease control, outpatient clinics, educational programs, and immunization clinics best illustrate the types of programs included in this category.
Research, shown separately in the NHA, are those activities carried out by nonprofit or government entities. Estimates of expenditures for non-commercial medical research were provided by the National Institutes of Health (1993), the agency responsible for 70 percent of these expenditures. Research and development expenditures by drug manufacturers are not included in this estimate, as those expenditures are treated as intermediate purchases under the definitions of national income accounting; that is, the value of that research is deemed to be recouped in the same year through the drug companies' sales.
Construction is limited to VPIP for hospitals, surgical and outpatient clinics, and nursing homes. Therefore, buildings that are used primarily for providers' offices are excluded. This measure includes new buildings; additions, alterations, and major replacements to existing buildings; mechanical and electrical installations; and site preparation. Maintenance and repairs are excluded, as are non-structural equipment such as X-ray machines and beds.
Private Sources of Funding
Out-of-pocket spending for health care consists of direct spending by consumers for all health care goods and services. This estimate includes the amount paid out of pocket for services not covered by insurance, as well as the amount of coinsurance and deductibles required by private health insurance and by public programs (such as Medicare and Medicaid) that are not covered by another third party. Payments to providers for services and goods that exceed the usual, customary, or reasonable charges paid by third parties are also included with direct patient spending. Out-of-pocket expenditures for private health insurance are excluded to avoid double counting with the NHA private health insurance category.
At the NHE level, private health insurance expenditures equal the premiums earned by private health insurers and HMOs, plus the premium equivalents of self-insurers. This figure is decomposed into benefits incurred (PHCE) and net cost (the difference between premiums or premium equivalents and benefits).
Non-patient revenues are those revenues received for which no direct patient-care services are rendered. The most widely recognized source of non-patient revenues is philanthropy. Philanthropic support may come directly from individuals or may be obtained through philanthropic fundraising organizations such as the United Way. Additionally, support may be obtained from foundations or corporations. Philanthropic revenues may be spent directly for patient care or may be held in an endowment fund to produce income to cover current expenses. For institutions such as hospitals, nursing homes, and HHAs, non-patient revenues also include income from the operation of gift shops, cafeterias, parking lots, and educational programs, as well as investment income.
Public Sources of Funding
Medicare
Medicare, a Federal insurance program created by title XVIII of the Social Security Act of 1965, was originally designed to protect persons 65 years of age or over from the high cost of health care. In 1972, the program was expanded to cover permanently disabled workers eligible for old age, survivors, and disability insurance benefits (and their dependents), as well as persons with end stage renal disease.
Medicare has two parts, each with its own trust fund. The hospital insurance (HI) program pays for inpatient hospital services, posthospital skilled nursing services, home health services, and hospice care. The supplementary medical insurance (SMI) program covers physician services, outpatient hospital services and therapy, and other services.
Unlike other Federal health programs, Medicare is not financed solely through general revenue (appropriations from general tax receipts). In 1993, 86.1 percent of income for the HI program (Table 9) came from a 1.45-percent payroll tax levied on employers and employees for the first $135,000 of wages. (Self-employed persons were required to contribute 2.9 percent, the equivalent of both the employers' and the employees' share of the HI tax.)
Table 9. Payments into Medicare Trust Funds and Percent Distribution, by Type of Fund and Source of Income: Selected Calendar Years 1967-93.
| Year and Source of Income | Total | Hospital Insurance Trust Fund | Supplementary Medical Insurance Trust Fund | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Amount in Billions | Percent Distribution | Amount in Billions | Percent Distribution | Amount in Billions | Percent Distribution | |
| 1967 | ||||||
| Total | $5.2 | 100.0 | $3.6 | 100.0 | $1.6 | 100.0 |
| Payroll Taxes | 3.2 | 62.0 | 3.2 | 89.8 | — | — |
| General Revenues | 1.2 | 24.1 | 0.3 | 8.8 | 0.9 | 58.4 |
| Premiums | 0.6 | 12.4 | — | — | 0.6 | 40.1 |
| Interest | 0.1 | 1.5 | 0.1 | 1.4 | 0.0 | 1.5 |
| 1972 | ||||||
| Total | $9.2 | 100.0 | $6.4 | 100.0 | $2.8 | 100.0 |
| Payroll Taxes | 5.8 | 62.9 | 5.8 | 90.5 | — | — |
| General Revenues | 1.8 | 19.7 | 0.4 | 6.7 | 1.4 | 49.5 |
| Premiums | 1.4 | 15.0 | — | — | 1.4 | 49.2 |
| Interest | 0.2 | 2.4 | 0.2 | 2.8 | 0.0 | 1.3 |
| 1983 | ||||||
| Total | $64.4 | 100.0 | $44.6 | 100.0 | $19.8 | 100.0 |
| Payroll Taxes | 37.6 | 58.4 | 37.6 | 84.4 | — | — |
| General Revenues | 19.2 | 29.8 | 14.3 | 9.7 | 14.9 | 75.0 |
| Premiums | 4.3 | 6.6 | 0.0 | 0.1 | 4.2 | 21.4 |
| Interest | 3.3 | 5.2 | 2.6 | 5.8 | 0.7 | 3.7 |
| 1993 | ||||||
| Total | $155.9 | 100.0 | $98.2 | 100.0 | $57.7 | 100.0 |
| Payroll Taxes | 84.5 | 54.2 | 84.5 | 86.1 | — | — |
| General Revenues | 41.9 | 26.9 | 0.4 | 0.5 | 41.5 | 71.9 |
| Premiums | 14.9 | 9.5 | 0.7 | 0.7 | 14.2 | 24.6 |
| Interest | 14.6 | 9.3 | 212.5 | 12.8 | 2.0 | 3.5 |
Includes a $3.5 billion lump-sum general revenue transfer for non-contributory military wage credits.
Includes a $1.8 billion transfer from the supplementary medical insurance catastrophic coverage reserve fund.
NOTES: 0.0 denotes less than $50 million. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
In 1993, the SMI program was financed through monthly premiums of $36.60 per enrollee and through general revenue. The general revenue share of SMI receipts grew from 49.5 percent in 1972 to 75.0 percent in 1983. In 1993, the general revenue share declined to 71.9 percent. The premium payment share of SMI income has grown since 1988. A provision of the MCCA mandated Medicaid coverage of aged and disabled Medicare enrollees with incomes below certain levels. Medicaid is required to pay Medicare premiums (buy-ins) for these enrollees. Prior to Medicaid coverage, these low-income persons were unable to afford the monthly SMI premium. The share of SMI enrollees who are Medicaid recipients for whom the State paid the SMI premium grew from 9.1 percent in 1988 to 11.9 percent in 1993.
Medicaid
Medicaid is funded jointly by Federal and State and local governments. In order for States to receive Federal matching funds, they must adhere to minimum requirements for eligibility and services set by the Federal Government. Within this broad framework, State governments are afforded considerable flexibility in designing the total scope of the program within the constraints of the State budgetary process. The Federal Government requires that all persons receiving income benefits under the Supplemental Security Income (SSI) program (covering aged, blind, and disabled individuals) and families qualifying for Aid to Families with Dependent Children (AFDC) automatically qualify for Medicaid benefits. Certain individuals with income and resources too high to qualify for SSI or AFDC are also mandatorily eligible for Medicaid. These eligibles include children under 6 years of age and pregnant women whose family income is below 133 percent of the Federal poverty level, certain low-income Medicare enrollees, and Social Security title IV-E recipients of foster care and adoption assistance. Currently, mandatory coverage of all children whose family income is at or below the poverty level is being phased in, with all needy children under 19 years of age obtaining coverage by 2002. States also have the option of providing Medicaid coverage to other more liberally defined categorically needy groups, extending coverage to medically indigent individuals or families, recipients of State supplementary payments, and other persons with income or resources below specified levels.
Aged and disabled Medicare enrollees with incomes below certain levels are mandatorily covered by Medicaid under the MCCA. These recipients are not eligible for full Medicaid benefits; Medicaid is required to pay only the Medicare premiums, deductibles, and coinsurance amounts. In addition, legislation in 1989 required Medicaid to pay a portion of the Medicare HI premium for certain low-income, disabled Medicare enrollees who, through rehabilitation and retraining, were able to return to work. Previously, after a specified period of time, these enrollees would have lost their eligibility for Medicare coverage. However, so that these working disabled persons are not penalized for returning to work, they are allowed to retain Medicare coverage by paying the monthly HI and SMI premiums. (Medicaid is not required to pay the SMI premium.)
The Federal Government also defines minimum services that must be provided to all or specified groups of Medicaid recipients. These services include inpatient and outpatient hospital services; physician care; rural health clinic services; laboratory and X-ray services; nursing home and home health care; and services of selected other health professionals. States may elect to provide additional services such as prescribed drugs, eyeglasses, dental care, and ICFs/MR.
Through State buy-in agreements, Medicaid purchases Medicare SMI (Part B) coverage for those eligible for both programs. For these dual-eligibles, Medicare is the primary payer for Medicare-covered services; Medicaid pays the deductibles and coinsurance amounts and provides additional Medicaid-covered health care services. To avoid double counting, the Medicaid estimates presented here do not include the $2.3 billion paid to Medicare by Medicaid in 1993 for buy-in premiums. Therefore, actual Medicaid PHCE were $115.1 billion in 1993.
In fiscal year 1993, there were 33.4 million persons who received some type of Medicaid benefit. AFDC recipients as a portion of total Medicaid recipients grew from just over two-thirds in 1990 to nearly three-fourths in 1993. However, they consumed approximately one-fourth of program benefits in 1990 and one-third in 1993. Conversely, the aged, blind, and disabled represented approximately one-fourth of all recipients, yet consumed more than two-thirds of program benefits (Table 10).
Table 10. Medicaid Recipients and Expenditures and Their Distributions, by Eligibility Category: Fiscal Years 1990-93.
| Eligibility Category | 1990 | 1991 | 1992 | 1993 |
|---|---|---|---|---|
| Recipients in Thousands: | ||||
| All Eligibility Categories1 | 25,255 | 28,277 | 30,926 | 33,432 |
| Aged, Blind, and Disabled | 6,920 | 7,428 | 8,194 | 8,879 |
| AFDC Families | 17,230 | 19,815 | 22,058 | 23,790 |
| Expenditures in Millions: | ||||
| All Eligibility Categories1 | $64,859 | $77,044 | $90,814 | $101,709 |
| Aged, Blind, and Disabled | 45,912 | 53,724 | 62,933 | 70,208 |
| AFDC Families | 17,690 | 22,071 | 26,676 | 30,109 |
| Recipients: | Percent Distribution of Program Benefits | |||
| All Eligibility Categories1 | 100.0 | 100.0 | 100.0 | 100.0 |
| Aged, Blind, and Disabled | 27.4 | 26.3 | 26.5 | 26.6 |
| AFDC Families | 68.2 | 70.1 | 71.3 | 71.2 |
| Expenditures: | ||||
| All Eligibility Categories1 | 100.0 | 100.0 | 100.0 | 100.0 |
| Aged, Blind, and Disabled | 70.8 | 69.7 | 69.3 | 69.0 |
| AFDC Families | 27.3 | 28.6 | 29.4 | 29.6 |
Includes children and aged and non-aged adults categorized as “other” or unknown not shown separately.
NOTES: Data reported on HCFA Form-2082. AFDC is Aid to Families with Dependent Children.
SOURCE: Health Care Financing Administration: Data from the Bureau of Data Management and Strategy, 1990-93.
Table 12. National Health Expenditures Aggregate Amounts and Average Annual Percent Change, by Type of Expenditure: Selected Years 1960-93.
| Type of Expenditure | 1960 | 1970 | 1980 | 1985 | 1987 | 1989 | 1990 | 1991 | 1992 | 1993 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Billions | ||||||||||
| National Health Expenditures | $27.1 | $74.3 | $251.1 | $434.5 | $506.2 | $623.9 | $696.6 | $755.6 | $820.3 | $884.2 |
| Health Services and Supplies | 25.4 | 69.0 | 239.4 | 418.1 | 487.9 | 601.8 | 672.2 | 730.8 | 792.9 | 855.2 |
| Personal Health Care | 23.9 | 64.8 | 220.1 | 380.5 | 453.8 | 550.5 | 612.4 | 670.8 | 729.7 | 782.5 |
| Hospital Care | 9.3 | 28.0 | 102.7 | 168.2 | 194.1 | 231.8 | 256.5 | 282.3 | 306.0 | 326.6 |
| Physician Services | 5.3 | 13.6 | 45.2 | 83.6 | 104.1 | 127.3 | 140.5 | 150.3 | 161.8 | 171.2 |
| Dental Services | 2.0 | 4.7 | 13.3 | 21.7 | 25.3 | 28.6 | 30.4 | 31.7 | 34.7 | 37.4 |
| Other Professional Services | 0.6 | 1.4 | 6.4 | 16.6 | 22.6 | 32.2 | 36.0 | 40.4 | 46.4 | 51.2 |
| Home Health Care | 0.0 | 0.2 | 1.9 | 4.9 | 5.9 | 8.1 | 11.1 | 13.2 | 16.8 | 20.8 |
| Drugs and Other Medical Non-Durables | 4.2 | 8.8 | 21.6 | 37.4 | 45.4 | 54.4 | 61.2 | 67.1 | 70.8 | 75.0 |
| Vision Products and Other Medical Durables | 0.8 | 2.0 | 4.5 | 7.1 | 8.1 | 9.6 | 10.5 | 11.3 | 12.0 | 12.6 |
| Nursing Home Care | 1.0 | 4.9 | 20.5 | 34.9 | 40.6 | 48.9 | 54.8 | 60.8 | 65.5 | 69.6 |
| Other Personal Health Care | 0.7 | 1.3 | 4.0 | 6.1 | 7.7 | 9.5 | 11.4 | 13.8 | 15.8 | 18.2 |
| Program Administration and Net Cost of Private Health Insurance | 1.2 | 2.8 | 12.1 | 25.3 | 19.4 | 32.3 | 38.3 | 37.0 | 39.5 | 48.0 |
| Government Public Health Activities | 0.4 | 1.4 | 7.2 | 12.3 | 14.6 | 19.0 | 21.6 | 22.9 | 23.7 | 24.7 |
| Research and Construction | 1.7 | 5.3 | 11.6 | 16.4 | 18.3 | 22.1 | 24.3 | 24.8 | 27.4 | 29.0 |
| Research1 | 0.7 | 2.0 | 5.5 | 7.8 | 9.1 | 11.3 | 12.2 | 12.9 | 14.2 | 14.4 |
| Construction | 1.0 | 3.4 | 6.2 | 8.6 | 9.2 | 10.8 | 12.1 | 11.9 | 13.2 | 14.6 |
| Average Annual Percent Change From Previous Year Shown | ||||||||||
| National Health Expenditures | — | 10.6 | 12.9 | 11.6 | 7.9 | 11.0 | 11.6 | 8.5 | 8.6 | 7.8 |
| Health Services and Supplies | — | 10.5 | 13.2 | 11.8 | 8.0 | 11.1 | 11.7 | 8.7 | 8.5 | 7.9 |
| Personal Health Care | — | 10.5 | 13.0 | 11.6 | 9.2 | 10.1 | 11.2 | 9.5 | 8.8 | 7.2 |
| Hospital Care | — | 11.7 | 13.9 | 10.4 | 7.4 | 9.3 | 10.7 | 10.0 | 8.4 | 6.7 |
| Physician Services | — | 9.9 | 12.8 | 13.1 | 11.6 | 10.6 | 10.3 | 7.0 | 7.6 | 5.8 |
| Dental Services | — | 9.1 | 11.1 | 10.2 | 8.2 | 6.3 | 6.1 | 4.2 | 9.6 | 7.7 |
| Other Professional Services | — | 8.8 | 16.3 | 21.2 | 16.6 | 19.4 | 11.8 | 12.3 | 14.8 | 10.4 |
| Home Health Care | — | 14.5 | 26.3 | 21.3 | 9.5 | 16.8 | 36.9 | 19.2 | 27.4 | 23.8 |
| Drugs and Other Medical Non-Durables | — | 7.6 | 9.4 | 11.6 | 10.2 | 9.5 | 12.5 | 9.5 | 5.5 | 5.9 |
| Vision Products and Other Medical Durables | — | 9.6 | 8.3 | 9.5 | 7.2 | 8.5 | 10.0 | 7.2 | 6.4 | 5.3 |
| Nursing Home Care | — | 17.4 | 15.5 | 11.3 | 7.8 | 9.8 | 12.0 | 10.9 | 7.8 | 6.3 |
| Other Personal Health Care | — | 6.5 | 12.0 | 8.8 | 12.1 | 11.4 | 19.1 | 21.4 | 14.4 | 15.0 |
| Program Administration and Net Cost of Private Health Insurance | — | 9.1 | 15.9 | 15.9 | -12.3 | 28.9 | 18.7 | -3.3 | 6.6 | 21.5 |
| Government Public Health Activities | — | 13.9 | 18.0 | 11.3 | 9.0 | 14.0 | 13.3 | 6.4 | 3.4 | 4.2 |
| Research and Construction | — | 12.2 | 8.1 | 7.1 | 5.7 | 9.9 | 10.0 | 1.8 | 10.8 | 5.8 |
| Research1 | — | 10.9 | 10.8 | 7.5 | 7.9 | 11.1 | 8.5 | 5.6 | 10.3 | 1.1 |
| Construction | — | 12.9 | 6.2 | 6.7 | 3.6 | 8.7 | 11.5 | -1.9 | 11.4 | 10.8 |
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from research expenditures, but are included in the expenditure class in which the product falls.
NOTE: Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 13. National Health Expenditures, by Source of Funds and Type of Expenditure: Selected Calendar Years 1960-93.
| Year and Type of Expenditure | Total | Private | Government | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| All Private Funds | Consumer | Other | Total | Federal | State and Local | ||||
|
| |||||||||
| Total | Out of Pocket | Private Insurance | |||||||
|
| |||||||||
| Amount in Billions | |||||||||
| 1960 | |||||||||
| National Health Expenditures | 27.1 | 20.5 | 19.2 | 13.4 | 5.9 | 1.3 | 6.7 | 2.9 | 3.7 |
| Health Services and Supplies | 25.4 | 19.8 | 19.2 | 13.4 | 5.9 | 0.6 | 5.7 | 2.3 | 3.4 |
| Personal Health Care | 23.9 | 18.8 | 18.4 | 13.4 | 5.0 | 0.4 | 5.1 | 2.1 | 3.0 |
| Hospital Care | 9.3 | 5.3 | 5.2 | 1.9 | 3.3 | 0.1 | 3.9 | 1.6 | 2.3 |
| Physician Services | 5.3 | 4.9 | 4.9 | 3.3 | 1.6 | 0.0 | 0.4 | 0.1 | 0.3 |
| Dental Services | 2.0 | 1.9 | 1.9 | 1.9 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Other Professional Services | 0.6 | 0.6 | 0.5 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Home Health Care | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Drugs and Other Medical Non-Durables | 4.2 | 4.2 | 4.2 | 4.1 | 0.0 | — | 0.1 | 0.0 | 0.0 |
| Vision Products and Other Medical Durables | 0.8 | 0.8 | 0.8 | 0.8 | 0.0 | — | 0.0 | 0.0 | 0.0 |
| Nursing Home Care | 1.0 | 0.8 | 0.8 | 0.8 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 |
| Other Personal Health Care | 0.7 | 0.2 | — | — | — | 0.2 | 0.5 | 0.3 | 0.2 |
| Program Administration and Net Cost of Private Health Insurance | 1.2 | 1.0 | 0.9 | — | 0.9 | 0.1 | 0.2 | 0.0 | 0.1 |
| Government Public Health Activities | 0.4 | — | — | — | — | — | 0.4 | 0.1 | 0.3 |
| Research and Construction | 1.7 | 0.7 | — | — | — | 0.7 | 1.0 | 0.7 | 0.3 |
| Research | 0.7 | 0.1 | — | — | — | 0.1 | 0.6 | 0.5 | 0.0 |
| Construction | 1.0 | 0.6 | — | — | — | 0.6 | 0.4 | 0.2 | 0.3 |
| 1980 | |||||||||
| National Health Expenditures | 251.1 | 145.8 | 133.4 | 61.3 | 72.1 | 12.4 | 105.3 | 72.0 | 33.3 |
| Health Services and Supplies | 239.4 | 141.3 | 133.4 | 61.3 | 72.1 | 7.9 | 98.1 | 66.8 | 31.3 |
| Personal Health Care | 220.1 | 133.1 | 125.4 | 61.3 | 64.1 | 7.7 | 87.0 | 63.4 | 23.6 |
| Hospital Care | 102.7 | 49.0 | 44.0 | 5.3 | 38.7 | 5.0 | 53.7 | 40.9 | 12.8 |
| Physician Services | 45.2 | 32.2 | 31.8 | 14.7 | 17.1 | 0.4 | 13.1 | 10.0 | 3.1 |
| Dental Services | 13.3 | 12.7 | 12.7 | 8.8 | 3.8 | 0.0 | 0.6 | 0.4 | 0.3 |
| Other Professional Services | 6.4 | 4.9 | 4.4 | 3.3 | 1.1 | 0.5 | 1.5 | 1.1 | 0.4 |
| Home Health Care | 1.9 | 0.9 | 0.6 | 0.3 | 0.3 | 0.3 | 0.9 | 0.8 | 0.1 |
| Drugs and Other Medical Non-Durables | 21.6 | 19.9 | 19.9 | 17.5 | 2.4 | — | 1.7 | 0.9 | 0.8 |
| Vision Products and Other Medical Durables | 4.5 | 3.9 | 3.9 | 3.5 | 0.4 | — | 0.6 | 0.5 | 0.1 |
| Nursing Home Care | 20.5 | 8.7 | 8.1 | 7.8 | 0.2 | 0.6 | 11.8 | 6.9 | 4.9 |
| Other Personal Health Care | 4.0 | 0.9 | — | — | — | 0.9 | 3.1 | 2.0 | 1.1 |
| Program Administration and Net Cost of Private Health Insurance | 12.1 | 8.2 | 8.0 | — | 8.0 | 0.2 | 3.9 | 2.1 | 1.8 |
| Government Public Health Activities | 7.2 | — | — | — | — | — | 7.2 | 1.2 | 6.0 |
| Research and Construction | 11.6 | 4.5 | — | — | — | 4.5 | 7.2 | 5.2 | 2.0 |
| Research | 5.5 | 0.3 | — | — | — | 0.3 | 5.2 | 4.7 | 0.5 |
| Construction | 6.2 | 4.2 | — | — | — | 4.2 | 2.0 | 0.6 | 1.5 |
| 1990 | |||||||||
| National Health Expenditures | 696.6 | 410.0 | 375.2 | 138.3 | 236.9 | 34.8 | 286.5 | 195.8 | 90.7 |
| Health Services and Supplies | 672.2 | 399.8 | 375.2 | 138.3 | 236.9 | 24.6 | 272.5 | 185.4 | 87.0 |
| Personal Health Care | 612.4 | 368.9 | 345.0 | 138.3 | 206.7 | 24.0 | 243.5 | 178.1 | 65.3 |
| Hospital Care | 256.5 | 119.2 | 105.5 | 9.8 | 95.7 | 13.8 | 137.3 | 103.4 | 33.9 |
| Physician Services | 140.5 | 95.0 | 92.4 | 25.3 | 67.1 | 2.7 | 45.5 | 36.3 | 9.1 |
| Dental Services | 30.4 | 29.5 | 29.4 | 15.3 | 14.1 | 0.1 | 0.9 | 0.5 | 0.4 |
| Other Professional Services | 36.0 | 29.5 | 26.9 | 14.9 | 12.0 | 2.6 | 6.5 | 4.3 | 2.2 |
| Home Health Care | 11.1 | 5.9 | 4.3 | 2.7 | 1.7 | 1.6 | 5.2 | 4.1 | 1.0 |
| Drugs and Other Medical Non-Durables | 61.2 | 54.8 | 54.8 | 41.2 | 13.6 | — | 6.5 | 3.1 | 3.4 |
| Vision Products and Other Medical Durables | 10.5 | 7.7 | 7.7 | 6.8 | 0.9 | — | 2.8 | 2.6 | 0.1 |
| Nursing Home Care | 54.8 | 25.0 | 24.0 | 22.3 | 1.7 | 1.0 | 29.8 | 18.2 | 11.6 |
| Other Personal Health Care | 11.4 | 2.2 | — | — | — | 2.2 | 9.1 | 5.6 | 3.6 |
| Program Administration and Net Cost of Private Health Insurance | 38.3 | 30.9 | 30.3 | — | 30.3 | 0.6 | 7.4 | 4.9 | 2.5 |
| Government Public Health Activities | 21.6 | — | — | — | — | — | 21.6 | 2.4 | 19.2 |
| Research and Construction | 24.3 | 10.2 | — | — | — | 10.2 | 14.1 | 10.4 | 3.7 |
| Research | 12.2 | 1.0 | — | — | — | 1.0 | 11.3 | 9.5 | 1.7 |
| Construction | 12.1 | 9.3 | — | — | — | 9.3 | 2.8 | 0.8 | 2.0 |
| 1991 | |||||||||
| National Health Expenditures | 755.6 | 432.9 | 396.1 | 143.3 | 252.8 | 36.8 | 322.6 | 224.7 | 98.0 |
| Health Services and Supplies | 730.8 | 422.8 | 396.1 | 143.3 | 252.8 | 26.7 | 308.0 | 214.0 | 94.0 |
| Personal Health Care | 670.8 | 393.2 | 367.2 | 143.3 | 223.9 | 26.1 | 277.6 | 206.0 | 71.6 |
| Hospital Care | 282.3 | 127.5 | 112.4 | 9.6 | 102.8 | 15.1 | 154.8 | 120.3 | 34.5 |
| Physician Services | 150.3 | 100.5 | 97.9 | 25.5 | 72.4 | 2.6 | 49.8 | 39.2 | 10.6 |
| Dental Services | 31.7 | 30.6 | 30.5 | 15.9 | 14.6 | 0.1 | 1.1 | 0.6 | 0.5 |
| Other Professional Services | 40.4 | 32.7 | 29.8 | 16.0 | 13.8 | 2.9 | 7.7 | 5.2 | 2.5 |
| Home Health Care | 13.2 | 6.4 | 4.7 | 2.9 | 1.7 | 1.7 | 6.8 | 5.6 | 1.2 |
| Drugs and Other Medical Non-Durables | 67.1 | 59.4 | 59.4 | 43.6 | 15.8 | — | 7.6 | 3.7 | 3.9 |
| Vision Products and Other Medical Durables | 11.3 | 7.9 | 7.9 | 7.0 | 0.9 | — | 3.4 | 3.2 | 0.1 |
| Nursing Home Care | 60.8 | 25.8 | 24.6 | 22.8 | 1.8 | 1.1 | 35.0 | 21.2 | 13.8 |
| Other Personal Health Care | 13.8 | 2.4 | — | — | — | 2.4 | 11.4 | 7.0 | 4.4 |
| Program Administration and Net Cost of Private Health Insurance | 37.0 | 29.6 | 28.9 | — | 28.9 | 0.6 | 7.5 | 5.3 | 2.2 |
| Government Public Health Activities | 22.9 | — | — | — | — | — | 22.9 | 2.7 | 20.2 |
| Research and Construction | 24.8 | 10.1 | — | — | — | 10.1 | 14.6 | 10.7 | 4.0 |
| Research | 12.9 | 1.1 | — | — | — | 1.1 | 11.8 | 9.9 | 1.9 |
| Construction | 11.9 | 9.0 | — | — | — | 9.0 | 2.8 | 0.7 | 2.1 |
| 1992 | |||||||||
| National Health Expenditures | 820.3 | 462.9 | 423.3 | 150.6 | 272.7 | 39.5 | 357.5 | 254.3 | 103.2 |
| Health Services and Supplies | 792.9 | 451.7 | 423.3 | 150.6 | 272.7 | 28.4 | 341.2 | 242.5 | 98.7 |
| Personal Health Care | 729.7 | 420.4 | 392.7 | 150.6 | 242.1 | 27.7 | 309.3 | 234.0 | 75.3 |
| Hospital Care | 306.0 | 134.0 | 118.1 | 9.0 | 109.1 | 15.9 | 172.0 | 137.3 | 34.7 |
| Physician Services | 161.8 | 108.4 | 105.7 | 26.1 | 79.6 | 2.7 | 53.4 | 41.5 | 11.9 |
| Dental Services | 34.7 | 33.4 | 33.2 | 17.4 | 15.9 | 0.1 | 1.3 | 0.8 | 0.6 |
| Other Professional Services | 46.4 | 37.3 | 34.4 | 18.8 | 15.5 | 3.0 | 9.1 | 6.3 | 2.8 |
| Home Health Care | 16.8 | 8.0 | 5.8 | 3.7 | 2.2 | 2.1 | 8.8 | 7.4 | 1.4 |
| Drugs and Other Medical Non-Durables | 70.8 | 62.6 | 62.6 | 45.4 | 17.1 | — | 8.2 | 4.1 | 4.1 |
| Vision Products and Other Medical Durables | 12.0 | 8.2 | 8.2 | 7.3 | 0.9 | — | 3.8 | 3.6 | 0.1 |
| Nursing Home Care | 65.5 | 26.0 | 24.8 | 22.9 | 1.8 | 1.2 | 39.5 | 24.8 | 14.7 |
| Other Personal Health Care | 15.8 | 2.6 | — | — | — | 2.6 | 13.2 | 8.1 | 5.0 |
| Program Administration and Net Cost of Private Health Insurance | 39.5 | 31.3 | 30.6 | — | 30.6 | 0.7 | 8.2 | 5.5 | 2.7 |
| Government Public Health Activities | 23.7 | — | — | — | — | — | 23.7 | 3.0 | 20.7 |
| Research and Construction | 27.4 | 11.2 | — | — | — | 11.2 | 16.3 | 11.8 | 4.5 |
| Research | 14.2 | 1.2 | — | — | — | 1.2 | 13.0 | 11.0 | 2.0 |
| Construction | 13.2 | 9.9 | — | — | — | 9.9 | 3.3 | 0.8 | 2.5 |
| 1993 | |||||||||
| National Health Expenditures | 884.2 | 496.4 | 453.6 | 157.5 | 296.1 | 42.8 | 387.8 | 280.6 | 107.3 |
| Health Services and Supplies | 855.2 | 484.3 | 453.6 | 157.5 | 296.1 | 30.7 | 370.9 | 268.6 | 102.4 |
| Personal Health Care | 782.5 | 445.5 | 415.5 | 157.5 | 258.0 | 30.0 | 337.0 | 259.0 | 78.1 |
| Hospital Care | 326.6 | 143.7 | 126.9 | 9.1 | 117.8 | 16.8 | 182.9 | 149.2 | 33.7 |
| Physician Services | 171.2 | 113.1 | 110.3 | 26.2 | 84.1 | 2.7 | 58.1 | 45.0 | 13.1 |
| Dental Services | 37.4 | 35.6 | 35.5 | 18.7 | 16.8 | 0.2 | 1.7 | 1.0 | 0.8 |
| Other Professional Services | 51.2 | 40.6 | 37.0 | 21.2 | 15.8 | 3.6 | 10.6 | 7.3 | 3.3 |
| Home Health Care | 20.8 | 9.4 | 6.9 | 4.3 | 2.5 | 2.5 | 11.4 | 9.8 | 1.5 |
| Drugs and Other Medical Non-Durables | 75.0 | 65.8 | 65.8 | 47.4 | 18.4 | — | 9.2 | 4.7 | 4.4 |
| Vision Products and Other Medical Durables | 12.6 | 8.5 | 8.5 | 7.6 | 0.9 | — | 4.2 | 4.0 | 0.2 |
| Nursing Home Care | 69.6 | 26.0 | 24.7 | 23.0 | 1.7 | 1.3 | 43.6 | 28.3 | 15.3 |
| Other Personal Health Care | 18.2 | 2.8 | — | — | — | 2.8 | 15.3 | 9.5 | 5.8 |
| Program Administration and Net Cost of Private Health Insurance | 48.0 | 38.8 | 38.1 | — | 38.1 | 0.7 | 9.2 | 6.3 | 2.8 |
| Government Public Health Activities | 24.7 | — | — | — | — | — | 24.7 | 3.3 | 21.4 |
| Research and Construction | 29.0 | 12.1 | — | — | — | 12.1 | 16.9 | 12.0 | 4.9 |
| Research | 14.4 | 1.2 | — | — | — | 1.2 | 13.1 | 11.1 | 2.1 |
| Construction | 14.6 | 10.9 | — | — | — | 10.9 | 3.8 | 0.9 | 2.8 |
NOTES: 0.0 denotes less than $50 million. Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from research expenditures, but are included in the expenditure class in which the product falls. Numbers may not add to totals because of rounding.
Table 14. Personal Health Care Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960-93.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $23.9 | $13.4 | $10.6 | $5.0 | $0.4 | $5.1 | $2.1 | $3.0 | — | — |
| 1970 | 64.8 | 25.4 | 39.5 | 15.3 | 1.6 | 22.5 | 14.7 | 7.8 | $7.3 | $5.1 |
| 1980 | 220.1 | 61.3 | 158.8 | 64.1 | 7.7 | 87.0 | 63.4 | 23.6 | 36.4 | 24.8 |
| 1985 | 380.5 | 98.8 | 281.7 | 119.8 | 13.9 | 148.0 | 111.3 | 36.7 | 70.3 | 39.2 |
| 1987 | 453.8 | 111.6 | 342.2 | 148.9 | 16.9 | 176.4 | 129.4 | 47.0 | 80.4 | 47.9 |
| 1989 | 550.5 | 127.8 | 422.7 | 186.8 | 21.6 | 214.3 | 158.6 | 55.7 | 100.1 | 59.2 |
| 1990 | 612.4 | 138.3 | 474.1 | 206.7 | 24.0 | 243.5 | 178.1 | 65.3 | 109.6 | 71.7 |
| 1991 | 670.8 | 143.3 | 527.5 | 223.9 | 26.1 | 277.6 | 206.0 | 71.6 | 120.5 | 89.9 |
| 1992 | 729.7 | 150.6 | 579.1 | 242.1 | 27.7 | 309.3 | 234.0 | 75.3 | 135.4 | 103.6 |
| 1993 | 782.5 | 157.5 | 625.0 | 258.0 | 30.0 | 337.0 | 259.0 | 78.1 | 151.1 | 112.8 |
| Per Capita Amount | ||||||||||
| 1960 | $126 | $70 | $56 | $26 | $2 | $27 | $11 | $16 | — | — |
| 1970 | 302 | 118 | 184 | 71 | 8 | 105 | 68 | 36 | (3) | (3) |
| 1980 | 936 | 261 | 676 | 273 | 33 | 370 | 270 | 100 | (3) | (3) |
| 1985 | 1,542 | 400 | 1,142 | 486 | 56 | 600 | 451 | 149 | (3) | (3) |
| 1987 | 1,804 | 444 | 1,361 | 592 | 67 | 701 | 515 | 187 | (3) | (3) |
| 1989 | 2,147 | 499 | 1,648 | 729 | 84 | 836 | 618 | 217 | (3) | (3) |
| 1990 | 2,361 | 533 | 1,828 | 797 | 92 | 939 | 687 | 252 | (3) | (3) |
| 1991 | 2,558 | 547 | 2,012 | 854 | 99 | 1,059 | 786 | 273 | (3) | (3) |
| 1992 | 2,752 | 568 | 2,184 | 913 | 105 | 1,167 | 882 | 284 | (3) | (3) |
| 1993 | 2,920 | 588 | 2,332 | 963 | 112 | 1,258 | 966 | 291 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 55.9 | 44.1 | 21.0 | 1.8 | 21.4 | 8.9 | 12.5 | — | — |
| 1970 | 100.0 | 39.1 | 60.9 | 23.6 | 2.5 | 34.7 | 22.7 | 12.0 | 11.3 | 7.8 |
| 1980 | 100.0 | 27.8 | 72.2 | 29.1 | 3.5 | 39.5 | 28.8 | 10.7 | 16.5 | 11.3 |
| 1985 | 100.0 | 26.0 | 74.0 | 31.5 | 3.6 | 38.9 | 29.3 | 9.6 | 18.5 | 10.3 |
| 1987 | 100.0 | 24.6 | 75.4 | 32.8 | 3.7 | 38.9 | 28.5 | 10.4 | 17.7 | 10.6 |
| 1989 | 100.0 | 23.2 | 76.8 | 33.9 | 3.9 | 38.9 | 28.8 | 10.1 | 18.2 | 10.7 |
| 1990 | 100.0 | 22.6 | 77.4 | 33.8 | 3.9 | 39.8 | 29.1 | 10.7 | 17.9 | 11.7 |
| 1991 | 100.0 | 21.4 | 78.6 | 33.4 | 3.9 | 41.4 | 30.7 | 10.7 | 18.0 | 13.4 |
| 1992 | 100.0 | 20.6 | 79.4 | 33.2 | 3.8 | 42.4 | 32.1 | 10.3 | 18.6 | 14.2 |
| 1993 | 100.0 | 20.1 | 79.9 | 33.0 | 3.8 | 43.1 | 33.1 | 10.0 | 19.3 | 14.4 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-90.1991-93 estimated by the Health Care Financing Administration. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 15. Hospital Care Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960-93.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $9.3 | $1.9 | $7.4 | $3.3 | $0.1 | $3.9 | $1.6 | $2.3 | — | — |
| 1970 | 28.0 | 2.5 | 25.5 | 9.6 | 0.9 | 15.0 | 9.9 | 5.1 | $5.3 | $2.2 |
| 1980 | 102.7 | 5.3 | 97.4 | 38.7 | 5.0 | 53.7 | 40.9 | 12.8 | 26.3 | 8.5 |
| 1985 | 168.2 | 8.8 | 159.4 | 61.0 | 8.3 | 90.1 | 71.1 | 19.0 | 48.9 | 13.7 |
| 1987 | 194.1 | 8.7 | 185.4 | 72.2 | 9.8 | 103.5 | 78.7 | 24.8 | 53.0 | 16.6 |
| 1989 | 231.8 | 9.7 | 222.2 | 88.1 | 12.4 | 121.7 | 93.0 | 28.7 | 62.8 | 20.9 |
| 1990 | 256.5 | 9.8 | 246.8 | 95.7 | 13.8 | 137.3 | 103.4 | 33.9 | 68.5 | 26.5 |
| 1991 | 282.3 | 9.6 | 272.7 | 102.8 | 15.1 | 154.8 | 120.3 | 34.5 | 74.9 | 34.5 |
| 1992 | 306.0 | 9.0 | 297.0 | 109.1 | 15.9 | 172.0 | 137.3 | 34.7 | 84.2 | 41.0 |
| 1993 | 326.6 | 9.1 | 317.4 | 117.8 | 16.8 | 182.9 | 149.2 | 33.7 | 92.7 | 42.4 |
| Per Capita Amount | ||||||||||
| 1960 | $49 | $10 | $39 | $17 | $1 | $21 | $8 | $12 | — | — |
| 1970 | 130 | 12 | 119 | 45 | 4 | 70 | 46 | 24 | (3) | (3) |
| 1980 | 437 | 23 | 414 | 165 | 21 | 228 | 174 | 55 | (3) | (3) |
| 1985 | 682 | 36 | 646 | 247 | 34 | 365 | 288 | 77 | (3) | (3) |
| 1987 | 772 | 35 | 737 | 287 | 39 | 411 | 313 | 99 | (3) | (3) |
| 1989 | 904 | 38 | 866 | 344 | 48 | 475 | 363 | 112 | (3) | (3) |
| 1990 | 989 | 38 | 951 | 369 | 53 | 530 | 399 | 131 | (3) | (3) |
| 1991 | 1,077 | 37 | 1,040 | 392 | 57 | 591 | 459 | 132 | (3) | (3) |
| 1992 | 1,154 | 34 | 1,120 | 412 | 60 | 649 | 518 | 131 | (3) | (3) |
| 1993 | 1,218 | 34 | 1,184 | 439 | 63 | 682 | 557 | 126 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 20.7 | 79.3 | 35.6 | 1.2 | 42.5 | 17.3 | 25.2 | — | — |
| 1970 | 100.0 | 9.0 | 91.0 | 34.3 | 3.2 | 53.5 | 35.2 | 18.2 | 18.8 | 8.0 |
| 1980 | 100.0 | 5.2 | 94.8 | 37.7 | 4.9 | 52.3 | 39.8 | 12.5 | 25.6 | 8.3 |
| 1985 | 100.0 | 5.2 | 94.8 | 36.3 | 4.9 | 53.6 | 42.3 | 11.3 | 29.1 | 8.1 |
| 1987 | 100.0 | 4.5 | 95.5 | 37.2 | 5.0 | 53.3 | 40.5 | 12.8 | 27.3 | 8.5 |
| 1989 | 100.0 | 4.2 | 95.8 | 38.0 | 5.3 | 52.5 | 40.1 | 12.4 | 27.1 | 9.0 |
| 1990 | 100.0 | 3.8 | 96.2 | 37.3 | 5.4 | 53.5 | 40.3 | 13.2 | 26.7 | 10.3 |
| 1991 | 100.0 | 3.4 | 96.6 | 36.4 | 5.3 | 54.8 | 42.6 | 12.2 | 26.5 | 12.2 |
| 1992 | 100.0 | 2.9 | 97.1 | 35.7 | 5.2 | 56.2 | 44.9 | 11.3 | 27.5 | 13.4 |
| 1993 | 100.0 | 2.8 | 97.2 | 36.1 | 5.2 | 56.0 | 45.7 | 10.3 | 28.4 | 13.0 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-90.1991-93 estimated by the Health Care Financing Administration. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 16. Physician Service Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960-93.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $5.3 | $3.3 | $2.0 | $1.6 | $0.0 | $0.4 | $0.1 | $0.3 | — | — |
| 1970 | 13.6 | 5.7 | 7.8 | 4.8 | 0.0 | 3.1 | 2.2 | 0.8 | $1.7 | $0.6 |
| 1980 | 45.2 | 14.7 | 30.6 | 17.1 | 0.4 | 13.1 | 10.0 | 3.1 | 8.0 | 2.5 |
| 1985 | 83.6 | 20.7 | 62.9 | 37.0 | 1.4 | 24.5 | 19.6 | 4.9 | 16.5 | 3.5 |
| 1987 | 104.1 | 22.8 | 81.4 | 47.2 | 2.0 | 32.1 | 25.9 | 6.2 | 21.8 | 4.5 |
| 1989 | 127.3 | 24.3 | 103.0 | 60.0 | 2.6 | 40.3 | 32.4 | 7.9 | 27.3 | 5.7 |
| 1990 | 140.5 | 25.3 | 115.2 | 67.1 | 2.7 | 45.5 | 36.3 | 9.1 | 30.0 | 7.1 |
| 1991 | 150.3 | 25.5 | 124.8 | 72.4 | 2.6 | 49.8 | 39.2 | 10.6 | 31.4 | 9.1 |
| 1992 | 161.8 | 26.1 | 135.7 | 79.6 | 2.7 | 53.4 | 41.5 | 11.9 | 32.4 | 11.2 |
| 1993 | 171.2 | 26.2 | 145.0 | 84.1 | 2.7 | 58.1 | 45.0 | 13.1 | 34.8 | 12.5 |
| Per Capita Amount | ||||||||||
| 1960 | $28 | $17 | $10 | $8 | $0 | $2 | $0 | $2 | — | — |
| 1970 | 63 | 27 | 37 | 22 | 0 | 14 | 10 | 4 | (3) | (3) |
| 1980 | 192 | 62 | 130 | 73 | 2 | 56 | 43 | 13 | (3) | (3) |
| 1985 | 339 | 84 | 255 | 150 | 6 | 99 | 80 | 20 | (3) | (3) |
| 1987 | 414 | 91 | 323 | 188 | 8 | 128 | 103 | 25 | (3) | (3) |
| 1989 | 497 | 95 | 402 | 234 | 10 | 157 | 126 | 31 | (3) | (3) |
| 1990 | 542 | 98 | 444 | 259 | 10 | 175 | 140 | 35 | (3) | (3) |
| 1991 | 573 | 97 | 476 | 276 | 10 | 190 | 149 | 40 | (3) | (3) |
| 1992 | 610 | 98 | 512 | 300 | 10 | 201 | 157 | 45 | (3) | (3) |
| 1993 | 639 | 98 | 541 | 314 | 10 | 217 | 168 | 49 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 62.7 | 37.3 | 30.2 | 0.1 | 7.1 | 1.4 | 5.7 | — | — |
| 1970 | 100.0 | 42.2 | 57.8 | 35.2 | 0.1 | 22.5 | 16.3 | 6.2 | 12.2 | 4.8 |
| 1980 | 100.0 | 32.4 | 67.6 | 37.9 | 0.8 | 28.9 | 22.1 | 6.8 | 17.6 | 5.5 |
| 1985 | 100.0 | 24.8 | 75.2 | 44.2 | 1.6 | 29.3 | 23.5 | 5.9 | 19.8 | 4.2 |
| 1987 | 100.0 | 21.9 | 78.1 | 45.3 | 2.0 | 30.8 | 24.9 | 6.0 | 21.0 | 4.3 |
| 1989 | 100.0 | 19.1 | 80.9 | 47.1 | 2.1 | 31.7 | 25.5 | 6.2 | 21.4 | 4.4 |
| 1990 | 100.0 | 18.0 | 82.0 | 47.7 | 1.9 | 32.4 | 25.9 | 6.5 | 21.3 | 5.1 |
| 1991 | 100.0 | 16.9 | 83.1 | 48.2 | 1.8 | 33.1 | 26.1 | 7.0 | 20.9 | 6.1 |
| 1992 | 100.0 | 16.1 | 83.9 | 49.2 | 1.7 | 33.0 | 25.7 | 7.4 | 20.0 | 6.9 |
| 1993 | 100.0 | 15.3 | 84.7 | 49.1 | 1.6 | 34.0 | 26.3 | 7.7 | 20.3 | 7.3 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $.50 for per capita amounts. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-90. 1991-93 estimated by the Health Care Financing Administration. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 17. Nursing Home Care Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960-93.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $1.0 | $0.8 | $0.2 | $0.0 | $0.1 | $0.1 | $0.1 | $0.1 | — | — |
| 1970 | 4.9 | 2.3 | 2.5 | 0.0 | 0.2 | 2.3 | 1.4 | 0.9 | $0.2 | $1.4 |
| 1980 | 20.5 | 7.8 | 12.6 | 0.2 | 0.6 | 11.8 | 6.9 | 4.9 | 0.4 | 11.0 |
| 1985 | 34.9 | 15.4 | 19.5 | 0.9 | 0.7 | 18.0 | 10.5 | 7.5 | 0.6 | 16.6 |
| 1987 | 40.6 | 17.3 | 23.2 | 1.3 | 0.8 | 21.2 | 12.3 | 8.8 | 0.6 | 19.6 |
| 1989 | 48.9 | 19.3 | 29.6 | 1.5 | 0.9 | 27.2 | 17.3 | 9.9 | 3.4 | 22.8 |
| 1990 | 54.8 | 22.3 | 32.5 | 1.7 | 1.0 | 29.8 | 18.2 | 11.6 | 2.4 | 26.3 |
| 1991 | 60.8 | 22.8 | 38.0 | 1.8 | 1.1 | 35.0 | 21.2 | 13.8 | 2.9 | 31.0 |
| 1992 | 65.5 | 22.9 | 42.6 | 1.8 | 1.2 | 39.5 | 24.8 | 14.7 | 4.5 | 33.7 |
| 1993 | 69.6 | 23.0 | 46.7 | 1.7 | 1.3 | 43.6 | 28.3 | 15.3 | 6.1 | 36.0 |
| Per Capita Amount | ||||||||||
| 1960 | $5 | $4 | $1 | $0 | $0 | $1 | $0 | $0 | — | — |
| 1970 | 23 | 11 | 12 | 0 | 1 | 11 | 6 | 4 | (3) | (3) |
| 1980 | 87 | 33 | 54 | 1 | 3 | 50 | 29 | 21 | (3) | (3) |
| 1985 | 141 | 63 | 79 | 3 | 3 | 73 | 43 | 30 | (3) | (3) |
| 1987 | 161 | 69 | 92 | 5 | 3 | 84 | 49 | 35 | (3) | (3) |
| 1989 | 191 | 75 | 116 | 6 | 4 | 106 | 68 | 39 | (3) | (3) |
| 1990 | 211 | 86 | 125 | 7 | 4 | 115 | 70 | 45 | (3) | (3) |
| 1991 | 232 | 87 | 145 | 7 | 4 | 134 | 81 | 53 | (3) | (3) |
| 1992 | 247 | 86 | 161 | 7 | 5 | 149 | 94 | 55 | (3) | (3) |
| 1993 | 260 | 86 | 174 | 6 | 5 | 163 | 106 | 57 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 80.0 | 20.0 | 0.0 | 6.4 | 13.6 | 6.9 | 6.7 | — | — |
| 1970 | 100.0 | 48.1 | 51.9 | 0.3 | 4.9 | 46.6 | 28.2 | 18.4 | 5.0 | 28.0 |
| 1980 | 100.0 | 38.3 | 61.7 | 1.1 | 3.1 | 57.6 | 33.8 | 23.8 | 2.0 | 53.6 |
| 1985 | 100.0 | 44.2 | 55.8 | 2.4 | 1.9 | 51.5 | 30.0 | 21.4 | 1.7 | 47.7 |
| 1987 | 100.0 | 42.7 | 57.3 | 3.2 | 1.9 | 52.2 | 30.4 | 21.8 | 1.5 | 48.4 |
| 1989 | 100.0 | 39.4 | 60.6 | 3.0 | 1.9 | 55.7 | 35.4 | 20.3 | 7.0 | 46.6 |
| 1990 | 100.0 | 40.6 | 59.4 | 3.2 | 1.9 | 54.3 | 33.3 | 21.1 | 4.4 | 47.9 |
| 1991 | 100.0 | 37.5 | 62.5 | 3.0 | 1.9 | 57.6 | 34.9 | 22.7 | 4.7 | 50.9 |
| 1992 | 100.0 | 35.0 | 65.0 | 2.8 | 1.9 | 60.3 | 37.9 | 22.4 | 6.9 | 51.4 |
| 1993 | 100.0 | 33.0 | 67.0 | 2.5 | 1.9 | 62.6 | 40.7 | 21.9 | 8.8 | 51.7 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $.50 for per capita amounts. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-90.1991-93 estimated by the Health Care Financing Administration. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 18. Other Personal Health Care Expenditures1 Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960-93.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare2 | Medicaid3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $8.4 | $7.3 | $1.0 | $0.1 | $0.2 | $0.7 | $0.4 | $0.3 | — | — |
| 1970 | 18.4 | 14.8 | 3.6 | 0.9 | 0.5 | 2.2 | 1.2 | 1.0 | NA | NA |
| 1980 | 51.7 | 33.5 | 18.2 | 8.1 | 1.7 | 8.5 | 5.6 | 2.8 | NA | NA |
| 1985 | 93.8 | 53.8 | 40.0 | 21.0 | 3.6 | 15.4 | 10.1 | 5.3 | NA | NA |
| 1987 | 115.0 | 62.8 | 52.2 | 28.3 | 4.3 | 19.7 | 12.5 | 7.1 | NA | NA |
| 1989 | 142.4 | 74.5 | 67.9 | 37.2 | 5.7 | 25.0 | 15.9 | 9.1 | NA | NA |
| 1990 | 160.6 | 80.9 | 79.6 | 42.2 | 6.5 | 30.9 | 20.2 | 10.7 | NA | NA |
| 1991 | 177.4 | 85.4 | 92.0 | 46.8 | 7.2 | 37.9 | 25.2 | 12.7 | NA | NA |
| 1992 | 196.4 | 92.6 | 103.8 | 51.6 | 7.9 | 44.3 | 30.3 | 14.0 | NA | NA |
| 1993 | 215.1 | 99.1 | 116.0 | 54.5 | 9.1 | 52.4 | 36.4 | 16.0 | NA | NA |
| Per Capita Amount | ||||||||||
| 1960 | $44 | $39 | $5 | $1 | $1 | $4 | $2 | $1 | — | — |
| 1970 | 86 | 69 | 17 | 4 | 2 | 10 | 6 | 4 | (4) | (4) |
| 1980 | 220 | 142 | 78 | 34 | 7 | 36 | 24 | 12 | (4) | (4) |
| 1985 | 380 | 218 | 162 | 85 | 14 | 62 | 41 | 21 | (4) | (4) |
| 1987 | 457 | 250 | 208 | 112 | 17 | 78 | 50 | 28 | (4) | (4) |
| 1989 | 555 | 291 | 265 | 145 | 22 | 98 | 62 | 36 | (4) | (4) |
| 1990 | 619 | 312 | 307 | 163 | 25 | 119 | 78 | 41 | (4) | (4) |
| 1991 | 677 | 326 | 351 | 179 | 27 | 145 | 96 | 48 | (4) | (4) |
| 1992 | 741 | 349 | 392 | 195 | 30 | 167 | 114 | 53 | (4) | (4) |
| 1993 | 803 | 370 | 433 | 203 | 34 | 196 | 136 | 60 | (4) | (4) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 87.8 | 12.2 | 1.4 | 2.8 | 8.0 | 4.7 | 3.3 | — | — |
| 1970 | 100.0 | 80.4 | 19.6 | 4.9 | 2.6 | 12.0 | 6.8 | 5.2 | NA | NA |
| 1980 | 100.0 | 64.7 | 35.3 | 15.6 | 3.3 | 16.4 | 10.9 | 5.5 | NA | NA |
| 1985 | 100.0 | 57.4 | 42.6 | 22.4 | 3.8 | 16.4 | 10.8 | 5.6 | NA | NA |
| 1987 | 100.0 | 54.6 | 45.4 | 24.6 | 3.7 | 17.1 | 10.9 | 6.2 | NA | NA |
| 1989 | 100.0 | 52.3 | 47.7 | 26.1 | 4.0 | 17.6 | 11.1 | 6.4 | NA | NA |
| 1990 | 100.0 | 50.4 | 49.6 | 26.3 | 4.1 | 19.2 | 12.6 | 6.7 | NA | NA |
| 1991 | 100.0 | 48.2 | 51.8 | 26.4 | 4.1 | 21.4 | 14.2 | 7.2 | NA | NA |
| 1992 | 100.0 | 47.1 | 52.9 | 26.3 | 4.0 | 22.6 | 15.4 | 7.1 | NA | NA |
| 1993 | 100.0 | 46.1 | 53.9 | 25.3 | 4.2 | 24.4 | 16.9 | 7.4 | NA | NA |
Versonal health care expenditures other than those for hospital care, physician services, and nursing home care.
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: NA is not available. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-90. 1991 -93 estimated by the Health Care Financing Administration. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 19. Personal Health Care Expenditures, by Type of Expenditure and Source of Funds: Selected Years 1980-93.
| Year and Source of Funds | Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Drugs and Other Medical Non-Durables | Vision Products and Other Medical Durables | Nursing Home Care | Other Personal Care |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Amount in Billions | ||||||||||
| 1980 | ||||||||||
| Personal Health Care Expenditures | $220.1 | $102.7 | $45.2 | $13.3 | $6.4 | $1.9 | $21.6 | $4.5 | $20.5 | $4.0 |
| Out-of-Pocket Payments | 61.3 | 5.3 | 14.7 | 8.8 | 3.3 | 0.3 | 17.5 | 3.5 | 7.8 | — |
| Third-Party Payments | 158.8 | 97.4 | 30.6 | 4.5 | 3.1 | 1.5 | 4.1 | 1.0 | 12.6 | 4.0 |
| Private Health Insurance | 64.1 | 38.7 | 17.1 | 3.8 | 1.1 | 0.3 | 2.4 | 0.4 | 0.2 | — |
| Other Private | 7.7 | 5.0 | 0.4 | 0.0 | 0.5 | 0.3 | — | — | 0.6 | 0.9 |
| Government | 87.0 | 53.7 | 13.1 | 0.6 | 1.5 | 0.9 | 1.7 | 0.6 | 11.8 | 3.1 |
| Federal | 63.4 | 40.9 | 10.0 | 0.4 | 1.1 | 0.8 | 0.9 | 0.5 | 6.9 | 2.0 |
| Medicare | 36.4 | 26.3 | 8.0 | — | 0.6 | 0.7 | — | 0.4 | 0.4 | — |
| Medicaid | 13.7 | 4.6 | 1.4 | 0.3 | 0.1 | 0.2 | 0.8 | — | 6.1 | 0.2 |
| Other | 13.3 | 9.9 | 0.6 | 0.1 | 0.4 | 0.0 | 0.0 | 0.1 | 0.4 | 1.8 |
| State and Local | 23.6 | 12.8 | 3.1 | 0.3 | 0.4 | 0.1 | 0.8 | 0.1 | 4.9 | 1.1 |
| Medicaid | 11.1 | 3.9 | 1.1 | 0.2 | 0.1 | 0.1 | 0.6 | — | 4.8 | 0.2 |
| Other | 12.5 | 8.9 | 2.0 | 0.1 | 0.3 | 0.0 | 0.2 | 0.1 | 0.0 | 0.9 |
| Total Medicaid | 24.8 | 8.5 | 2.5 | 0.5 | 0.2 | 0.3 | 1.4 | — | 11.0 | 0.4 |
| 1990 | ||||||||||
| Personal Health Care Expenditures | 612.4 | 256.5 | 140.5 | 30.4 | 36.0 | 11.1 | 61.2 | 10.5 | 54.8 | 11.4 |
| Out-of-Pocket Payments | 138.3 | 9.8 | 25.3 | 15.3 | 14.9 | 2.7 | 41.2 | 6.8 | 22.3 | — |
| Third-Party Payments | 474.1 | 246.8 | 115.2 | 15.1 | 21.1 | 8.4 | 20.0 | 3.7 | 32.5 | 11.4 |
| Private Health Insurance | 206.7 | 95.7 | 67.1 | 14.1 | 12.0 | 1.7 | 13.6 | 0.9 | 1.7 | — |
| Other Private | 24.0 | 13.8 | 2.7 | 0.1 | 2.6 | 1.6 | — | — | 1.0 | 2.2 |
| Government | 243.5 | 137.3 | 45.5 | 0.9 | 6.5 | 5.2 | 6.5 | 2.8 | 29.8 | 9.1 |
| Federal | 178.1 | 103.4 | 36.3 | 0.5 | 4.3 | 4.1 | 3.1 | 2.6 | 18.2 | 5.6 |
| Medicare | 109.6 | 68.5 | 30.0 | — | 3.3 | 3.0 | — | 2.5 | 2.4 | — |
| Medicaid | 40.6 | 14.9 | 4.2 | 0.4 | 0.3 | 1.1 | 3.0 | — | 14.8 | 2.0 |
| Other | 28.0 | 20.0 | 2.2 | 0.1 | 0.7 | — | 0.1 | 0.2 | 1.0 | 3.6 |
| State and Local | 65.3 | 33.9 | 9.1 | 0.4 | 2.2 | 1.0 | 3.4 | 0.1 | 11.6 | 3.6 |
| Medicaid | 31.2 | 11.6 | 2.9 | 0.3 | 0.2 | 1.0 | 2.2 | — | 11.5 | 1.5 |
| Other | 34.1 | 22.3 | 6.2 | 0.1 | 2.0 | 0.0 | 1.2 | 0.1 | 0.1 | 2.1 |
| Total Medicaid | 71.7 | 26.5 | 7.1 | 0.7 | 0.5 | 2.1 | 5.1 | — | 26.3 | 3.5 |
| 1991 | ||||||||||
| Personal Health Care Expenditures | 670.8 | 282.3 | 150.3 | 31.7 | 40.4 | 13.2 | 67.1 | 11.3 | 60.8 | 13.8 |
| Out-of-Pocket Payments | 143.3 | 9.6 | 25.5 | 15.9 | 16.0 | 2.9 | 43.6 | 7.0 | 22.8 | — |
| Third-Party Payments | 527.5 | 272.7 | 124.8 | 15.8 | 24.4 | 10.2 | 23.5 | 4.3 | 38.0 | 13.8 |
| Private Health Insurance | 223.9 | 102.8 | 72.4 | 14.6 | 13.8 | 1.7 | 15.8 | 0.9 | 1.8 | — |
| Other Private | 26.1 | 15.1 | 2.6 | 0.1 | 2.9 | 1.7 | — | — | 1.1 | 2.4 |
| Government | 277.6 | 154.8 | 49.8 | 1.1 | 7.7 | 6.8 | 7.6 | 3.4 | 35.0 | 11.4 |
| Federal | 206.0 | 120.3 | 39.2 | 0.6 | 5.2 | 5.6 | 3.7 | 3.2 | 21.2 | 7.0 |
| Medicare | 120.5 | 74.9 | 31.4 | — | 4.1 | 4.3 | — | 3.0 | 2.9 | — |
| Medicaid | 54.5 | 23.4 | 5.3 | 0.5 | 0.3 | 1.3 | 3.5 | — | 17.2 | 2.9 |
| Other | 31.0 | 22.0 | 2.5 | 0.1 | 0.8 | — | 0.1 | 0.2 | 1.2 | 4.1 |
| State and Local | 71.6 | 34.5 | 10.6 | 0.5 | 2.5 | 1.2 | 3.9 | 0.1 | 13.8 | 4.4 |
| Medicaid | 35.4 | 11.1 | 3.8 | 0.4 | 0.3 | 1.2 | 2.7 | — | 13.8 | 2.2 |
| Other | 36.2 | 23.4 | 6.8 | 0.1 | 2.2 | 0.0 | 1.3 | 0.1 | 0.1 | 2.2 |
| Total Medicaid | 89.9 | 34.5 | 9.1 | 0.9 | 0.6 | 2.5 | 6.2 | — | 31.0 | 5.1 |
| 1992 | ||||||||||
| Personal Health Care Expenditures | $729.7 | $306.0 | $161.8 | $34.7 | $46.4 | $16.8 | $70.8 | $12.0 | $65.5 | $15.8 |
| Out-of-Pocket Payments | 150.6 | 9.0 | 26.1 | 17.4 | 18.8 | 3.7 | 45.4 | 7.3 | 22.9 | — |
| Third-Party Payments | 579.1 | 297.0 | 135.7 | 17.3 | 27.6 | 13.1 | 25.3 | 4.7 | 42.6 | 15.8 |
| Private Health Insurance | 242.1 | 109.1 | 79.6 | 15.9 | 15.5 | 2.2 | 17.1 | 0.9 | 1.8 | — |
| Other Private | 27.7 | 15.9 | 2.7 | 0.1 | 3.0 | 2.1 | — | — | 1.2 | 2.6 |
| Government | 309.3 | 172.0 | 53.4 | 1.3 | 9.1 | 8.8 | 8.2 | 3.8 | 39.5 | 13.2 |
| Federal | 234.0 | 137.3 | 41.5 | 0.8 | 6.3 | 7.4 | 4.1 | 3.6 | 24.8 | 8.1 |
| Medicare | 135.4 | 84.2 | 32.4 | — | 5.0 | 5.9 | — | 3.4 | 4.5 | — |
| Medicaid | 65.9 | 30.1 | 6.6 | 0.6 | 0.4 | 1.5 | 3.9 | — | 19.1 | 3.7 |
| Other | 32.6 | 23.0 | 2.5 | 0.1 | 0.8 | — | 0.2 | 0.2 | 1.3 | 4.5 |
| State and Local | 75.3 | 34.7 | 11.9 | 0.6 | 2.8 | 1.4 | 4.1 | 0.1 | 14.7 | 5.0 |
| Medicaid | 37.7 | 10.9 | 4.5 | 0.5 | 0.3 | 1.3 | 2.8 | — | 14.6 | 2.7 |
| Other | 37.6 | 23.7 | 7.4 | 0.1 | 2.4 | 0.1 | 1.3 | 0.1 | 0.1 | 2.4 |
| Total Medicaid | 103.6 | 41.0 | 11.2 | 1.1 | 0.8 | 2.8 | 6.7 | — | 33.7 | 6.3 |
| 1993 | ||||||||||
| Personal Health Care Expenditures | 782.5 | 326.6 | 171.2 | 37.4 | 51.2 | 20.8 | 75.0 | 12.6 | 69.6 | 18.2 |
| Out-of-Pocket Payments | 157.5 | 9.1 | 26.2 | 18.7 | 21.2 | 4.3 | 47.4 | 7.6 | 23.0 | — |
| Third-Party Payments | 625.0 | 317.4 | 145.0 | 18.7 | 30.0 | 16.4 | 27.6 | 5.1 | 46.7 | 18.2 |
| Private Health Insurance | 258.0 | 117.8 | 84.1 | 16.8 | 15.8 | 2.5 | 18.4 | 0.9 | 1.7 | — |
| Other Private | 30.0 | 16.8 | 2.7 | 0.2 | 3.6 | 2.5 | — | — | 1.3 | 2.8 |
| Government | 337.0 | 182.9 | 58.1 | 1.7 | 10.6 | 11.4 | 9.2 | 4.2 | 43.6 | 15.3 |
| Federal | 259.0 | 149.2 | 45.0 | 1.0 | 7.3 | 9.8 | 4.7 | 4.0 | 28.3 | 9.5 |
| Medicare | 151.1 | 92.7 | 34.8 | — | 5.6 | 8.1 | — | 3.7 | 6.1 | — |
| Medicaid | 73.2 | 32.1 | 7.6 | 0.9 | 0.8 | 1.8 | 4.5 | — | 20.8 | 4.8 |
| Other | 34.7 | 24.4 | 2.7 | 0.1 | 0.9 | — | 0.2 | 0.3 | 1.4 | 4.7 |
| State and Local | 78.1 | 33.7 | 13.1 | 0.8 | 3.3 | 1.5 | 4.4 | 0.2 | 15.3 | 5.8 |
| Medicaid | 39.6 | 10.3 | 4.9 | 0.7 | 0.6 | 1.5 | 3.1 | — | 15.2 | 3.3 |
| Other | 38.5 | 23.4 | 8.2 | 0.1 | 2.7 | 0.1 | 1.3 | 0.2 | 0.1 | 2.5 |
| Total Medicaid | 112.8 | 42.4 | 12.5 | 1.5 | 1.4 | 3.2 | 7.7 | — | 36.0 | 8.1 |
NOTES: 0.0 denotes amounts less than $50 million. Medicaid expenditures exclude Part B premium payments to Medicare by States under buy-in agreements to cover premiums for eligible Medicaid recipients. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Acknowledgments
Estimates of the NHE are prepared in the Office of National Health Statistics, HCFA, under the general direction of Ross Arnett, Office Director, and Mark Freeland, Director of the Division of Health Cost Analysis. The authors are grateful for the helpful comments provided by Ross Arnett, Mark Freeland, Dan Waldo, Sally Burner, John Klemm, Mary Waid, and the staff of HCFA's Medicaid Bureau.
References
- Actuarial Research Corporation. National Health Accounts Drug Study. Annandale, VA.: 1994. Contract Number 500-94-0004. Prepared for the Health Care Financing Administration. [Google Scholar]
- Agency for Health Care Policy and Research. Data From the National Medical Expenditures Survey. Washington, DC.: 1987. Unpublished. [Google Scholar]
- American Dental Association. The 1990 Survey of Dental Services Rendered. Chicago: Jun, 1994. [Google Scholar]
- American Dental Association. Annual Survey of Dentists. Chicago: 1980-93. Unpublished. [Google Scholar]
- American Hospital Association. Hospital Statistics. Chicago: 1993. [Google Scholar]
- American Hospital Association. Annual Survey of Hospitals. Chicago: 1960-92. Unpublished. [Google Scholar]
- American Hospital Association. National Hospital Panel Survey. Chicago: 1990-93. Unpublished. [Google Scholar]
- American Medical Association. Unpublished Data From the Socio-Economic Monitoring System. Chicago: 1984-94. [Google Scholar]
- Business Insurance: Data From the Directory of Third Party Administrators. Chicago. 1986-94.
- Carroll MS, Arnett RH., III Private Health Insurance Plans in 1978 and 1979: A Review of Coverage, Enrollment, and Financial Experience. Health Care Financing Review. 1981 Sep;3(1):55–87. [PMC free article] [PubMed] [Google Scholar]
- Emmons DW, Simon CJ. Socioeconomic Characteristics of Medical Practice 1994. American Medical Association; Chicago: 1994. Recent Trends in Managed Care. [Google Scholar]
- Employee Benefit Plan Review: Data From the Survey of Third Party Claims Administrators. Chicago. 1985-93.
- Employee Benefit Research Institute. Sources of Health Insurance and Characteristics of the Uninsured. Washington, DC.: Jan, 1994. EBRI Issue Brief 145:5. [Google Scholar]
- Executive Office of the President. Budget of the United States. Washington: U.S. Government Printing Office; 1960-94. Office of Management and Budget. [Google Scholar]
- Executive Office of the President. Budget Appendix of the United States—1994. Washington: U.S. Government Printing Office; 1994. Office of Management and Budget. [Google Scholar]
- Executive Office of the President. Standard Industrial Classification Manual, 1987. Washington: U.S. Government Printing Office; 1987. Pub. NTIS (PB) 87-10012. Office of Management and Budget. [Google Scholar]
- Federal Register: Medicare Program: Fee Schedule for Physicians' Services, Fee Schedule Update for Calendar Year 1992 and Physician Performance Standard Rates of Increase for Federal FY 1992; Final Rule and Notice. No. 227. Vol. 56. Washington: U.S. Government Printing Office; Nov 25, 1991. pp. 59502–59819. Office of the Federal Register, National Archives and Records Administration. [Google Scholar]
- Foster Higgins. National Survey of Employer-Sponsored Health Plans, 1993. New York: 1994. [Google Scholar]
- Group Health Association of America, Inc. Data From the HMO Industry Survey. Washington, DC.: 1985-93. [Google Scholar]
- Health Care Financing Administration. Medicaid Voluntary Contribution and Provider Specific Tax Amendments of 1991 Program Summary. Washington: U.S. Government Printing Office; 1992. Medicaid Bureau. [Google Scholar]
- Health Care Financing Administration. Data From the Home Health Agency Input Price Index, 1991-93. Office of the Actuary; Washington, DC.: 1991-93. [Google Scholar]
- Health Insurance Association of America. Source Book of Health Insurance Data, 1994. Washington DC.: 1994. [Google Scholar]
- Hill BK, Lakin KC. Trends in Residential Services for Mentally Retarded People: 1977-82. Minneapolis Center for Residential and Community Services, University of Minnesota; 1984. Brief No. 23. [Google Scholar]
- KPMG Peat Marwick. Health Benefits in 1993. Newark, NJ.: 1993. [Google Scholar]
- Lazenby HC, Levit KR, Waldo DR, et al. National Health Accounts: Lessons From the U.S. Experience. Health Care Financing Review. 1992 Summer;13(4):89–104. [PMC free article] [PubMed] [Google Scholar]
- 30.Letsch SW, Lazenby HC, Levit KR, Cowan CA. National Health Expenditures, 1991. Health Care Financing Review. 1992 Winter;14(2):1. [PMC free article] [PubMed] [Google Scholar]
- Merlis M. Medicaid: Provider Donations and Provider-Specific Taxes. CRS Report for Congress. Congressional Research Service, The Library of Congress; Washington, DC.: Oct, 1991. [Google Scholar]
- National Association of Blue Cross and Blue Shield: Personal Communication. Chicago. 1960-93.
- National Center for Health Statistics. Data From the National Nursing Home Survey, 1972, 1977, and 1985. U.S. Department of Health and Human Services; Washington, DC.: 1972, 1977, 1982. [Google Scholar]
- National Institutes of Health. NIH Data Book 1993. Bethesda, MD.: Sep, 1993. NIH Pub. No. 93-1261. [Google Scholar]
- Pharmaceutical Research and Manufacturers of America. US Pharmaceutical R&D and Sales. Washington DC.: Feb, 1994. [Google Scholar]
- Strahan GW. Advance Data From Vital and Health Statistics. No. 235. Hyattsville, MD.: National Center for Health Statistics; Jul 28, 1993. An Overview of Home Health and Hospice Care Patients: Preliminary Data From the 1992 National Home and Hospice Care Survey. DHHS Pub. No. (PHS)93-1250. [PubMed] [Google Scholar]
- Strahan GW. Advance Data From Vital and Health Statistics. No. 256. Hyattsville, MD.: National Center for Health Statistics; 1994. An Overview of Home Health and Hospice Care Patients: Preliminary Data From the 1993 National Home and Hospice Care Survey. [PubMed] [Google Scholar]
- U.S. Bureau of the Census. Census of Service Industries. Washington: U.S. Government Printing Office; 1977, 1982, 1987a. [Google Scholar]
- U.S. Bureau of the Census. Census of Construction Industries. Washington: U.S. Government Printing Office; 1977, 1982, 1987b. [Google Scholar]
- U.S. Bureau of the Census. Current Construction Reports, Special Studies—Expenditures for Non-Residential Improvements and Repairs: 1989. Washington: U.S. Government Printing Office; 1991. [Google Scholar]
- U.S. Bureau of the Census. Services Annual Survey. Washington: U.S. Government Printing Office; 1984-92. [Google Scholar]
- U.S. Bureau of Labor Statistics. Current Establishment Survey. U.S. Department of Labor; Washington, DC.: 1992-93. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. Consumer Price Index Survey. U.S. Department of Labor; Washington, DC.: Jan-Dec. 1993. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. Employee Benefits Survey. U.S. Department of Labor; Washington, DC.: 1980-93. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. Employment Cost Index Survey. U.S. Department of Labor; Washington, DC.: 1984-93. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. Survey of Expenditures for Health Care Plans by Employers and Employees, 1992. U.S. Department of Labor; Washington, DC.: 1993. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. U.S. Department of Labor; Washington, DC.: 1984-92. Data From the Consumer Expenditure Integrated Survey Results for 1984-92. Unpublished. [Google Scholar]
- U.S. Bureau of Economic Analysis. Personal Consumption Expenditures. U.S. Department of Commerce; Washington, DC.: 1960-93. Unpublished. [Google Scholar]
- Visiting Nurse Association of America. Survey of Visiting Nurse Association of America Members. Denver: 1988. [Google Scholar]