Abstract
The dynamics of financing health care among various levels of government and the private sector are rapidly changing; structural relationships among health care providers are also being altered. These changes are placing increased importance on State-level expenditure estimates that will be instrumental in measuring the differential impact of Federal policies and State-specific initiatives on individual States. This article presents personal health care expenditures (PHCE) for 1980-93. Statistics show wide variation in level and rate of growth of regional spending per person. These statistics also quantify differences in both the percent of health care costs in each State borne by Medicare and Medicaid and in the proportion of each State's economy devoted to the provision of health care.
Introduction
State health expenditure accounts (SHEA) are important building blocks for health care policy analysis. Like its national health expenditure (NHE) account counterpart (Levit et al., 1994), SHEA provides a framework for measuring health care spending on services and products and the sources of revenue used to pay those costs. As a time-series measure, it also tracks changes in spending patterns over time and can record the impact of policy changes on payers and providers of health care. In the future, SHEA may also serve as a basis for projecting future State health costs or as controls for further disaggregation of costs to substate areas. The State accounts presented in this article expand on earlier published estimates (Levit et al., 1993; Levit, 1985) to present spending by State for all PHCE for 1980-93. Medicare and Medicaid spending for each personal health category are also included.
The current effort to develop and expand SHEA began during the 1993-94 health reform debate, as policymakers began to question the effect of national policy options on individual States. Those health reform efforts waned; subsequently, the focus has shifted to the efforts of States as they grapple with the continued rise in the number of uninsured, lack of availability of health insurance to many employed workers, mandated Medicaid expansions, State budget constraints, aging populations, and uncompensated care.
Some States are moving forward with changes to their health care delivery and payment systems. For example, Oregon is rationing Medicaid services to fund expansion of services to more persons; Florida has instituted purchasing alliances that make affordable insurance policies available to small businesses. More global proposals are under consideration by Congress that would affect the payment system through Medicare vouchers and/or Medicaid block grants. These changes would affect payers responsible for reimbursing providers for more than one-third of health care spending in 1993. Measuring and analyzing the differential impact of such changes on States will be a daunting task.
For many States, only fragmented information on health care spending within their borders is available, making informed policy decisions difficult. Several States have undertaken the task of comprehensively measuring the costs of this swelling economic sector; these statistics have proven invaluable in decisionmaking. But the lack of consistency in definitions and data among accounts developed by individual States make interstate comparisons difficult at best. Consequently, States have little information to use in comparing their experience with that of neighboring States.
The SHEA for 1980-93 are a step forward in providing consistent State-level health care expenditure information. These accounts present spending by State of provider of services, measuring the impact of health care on each State's economy. In addition, regional costs per capita and some possible causes for different levels and growth of spending are discussed. For most services, per capita costs are not analyzed by State because border crossing by patients to neighboring States to receive services distorts this measure.1 At the regional level, the net effect of border crossing is minimal. Development is under way on border-crossing adjustments that will permit interstate comparisons of per capita costs for 1991. These residence-based estimates that will permit a more complete analysis of spending difference by State will be available later this year. Further work is in progress to develop the information necessary to convert 1992 and 1993 PHCE from State of provider to State of residence, so that time-series per capita spending estimates can be analyzed.
Tables 11-28, presented at the end of this article, list State and regional estimates of PHCE for each service type, PHCE as a share of gross State product (GSP), and Medicare and Medicaid expenditures.
Table 11. Personal Health Care Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 216,525 | 375,236 | 608,246 | 727,377 | 778,510 | 10.3 |
| New England | 12,804 | 22,213 | 38,282 | 44,427 | 47,449 | 10.6 |
| Connecticut | 3,151 | 5,588 | 9,976 | 11,572 | 12,216 | 11.0 |
| Maine | 928 | 1,590 | 2,702 | 3,196 | 3,433 | 10.6 |
| Massachusetts | 6,651 | 11,261 | 19,170 | 21,969 | 23,421 | 10.2 |
| New Hampshire | 701 | 1,388 | 2,522 | 3,117 | 3,452 | 13.0 |
| Rhode Island | 975 | 1,705 | 2,731 | 3,173 | 3,428 | 10.2 |
| Vermont | 397 | 681 | 1,182 | 1,400 | 1,499 | 10.8 |
| Mideast | 44,387 | 76,067 | 123,174 | 145,912 | 155,994 | 10.2 |
| Delaware | 559 | 999 | 1,710 | 2,081 | 2,260 | 11.3 |
| District of Columbia | 1,389 | 2,282 | 3,535 | 4,018 | 4,285 | 9.1 |
| Maryland | 4,077 | 7,033 | 11,839 | 14,171 | 15,154 | 10.6 |
| New Jersey | 6,459 | 11,638 | 19,951 | 23,978 | 25,741 | 11.2 |
| New York | 20,142 | 33,231 | 53,716 | 62,928 | 67,033 | 9.7 |
| Pennsylvania | 11,762 | 20,883 | 32,423 | 38,736 | 41,521 | 10.2 |
| Great Lakes | 40,186 | 65,206 | 99,946 | 118,537 | 126,240 | 9.2 |
| Illinois | 11,706 | 18,362 | 27,422 | 32,856 | 34,747 | 8.7 |
| Indiana | 4,569 | 7,678 | 12,549 | 15,259 | 16,401 | 10.3 |
| Michigan | 9,358 | 14,779 | 21,972 | 25,458 | 27,136 | 8.5 |
| Ohio | 10,120 | 17,406 | 26,682 | 31,433 | 33,456 | 9.6 |
| Wisconsin | 4,433 | 6,982 | 11,322 | 13,530 | 14,502 | 9.5 |
| Plains | 16,594 | 27,375 | 42,220 | 49,608 | 52,761 | 9.3 |
| Iowa | 2,599 | 3,920 | 6,020 | 6,962 | 7,341 | 8.3 |
| Kansas | 2,262 | 3,586 | 5,508 | 6,562 | 6,903 | 9.0 |
| Minnesota | 4,241 | 7,289 | 11,511 | 13,328 | 14,194 | 9.7 |
| Missouri | 4,823 | 8,190 | 12,592 | 14,890 | 15,949 | 9.6 |
| Nebraska | 1,460 | 2,277 | 3,477 | 4,137 | 4,400 | 8.9 |
| North Dakota | 629 | 1,154 | 1,619 | 1,920 | 2,021 | 9.4 |
| South Dakota | 580 | 960 | 1,493 | 1,809 | 1,953 | 9.8 |
| Southeast | 43,634 | 79,689 | 136,582 | 165,841 | 178,023 | 11.4 |
| Alabama | 3,158 | 5,448 | 9,157 | 11,228 | 12,060 | 10.9 |
| Arkansas | 1,745 | 3,003 | 4,847 | 5,752 | 6,111 | 10.1 |
| Florida | 9,795 | 19,897 | 35,127 | 41,958 | 44,811 | 12.4 |
| Georgia | 4,570 | 8,471 | 15,287 | 18,620 | 20,104 | 12.1 |
| Kentucky | 2,716 | 4,721 | 7,826 | 9,745 | 10,384 | 10.9 |
| Louisiana | 3,577 | 6,494 | 9,888 | 12,067 | 13,014 | 10.4 |
| Mississippi | 1,768 | 2,935 | 4,714 | 5,663 | 6,187 | 10.1 |
| North Carolina | 4,211 | 7,303 | 13,700 | 16,889 | 18,241 | 11.9 |
| South Carolina | 2,092 | 3,725 | 6,699 | 8,364 | 9,029 | 11.9 |
| Tennessee | 4,069 | 7,210 | 12,177 | 15,086 | 16,203 | 11.2 |
| Virginia | 4,347 | 7,863 | 13,254 | 15,636 | 16,682 | 10.9 |
| West Virginia | 1,586 | 2,618 | 3,904 | 4,832 | 5,197 | 9.6 |
| Southwest | 18,639 | 34,032 | 54,923 | 67,078 | 72,370 | 11.0 |
| Arizona | 2,452 | 4,857 | 8,480 | 9,897 | 10,635 | 11.9 |
| New Mexico | 920 | 1,792 | 2,895 | 3,567 | 3,878 | 11.7 |
| Oklahoma | 2,578 | 4,348 | 6,279 | 7,521 | 8,041 | 9.1 |
| Texas | 12,689 | 23,035 | 37,268 | 46,092 | 49,816 | 11.1 |
| Rocky Mountains | 5,372 | 9,652 | 14,951 | 18,133 | 19,561 | 10.5 |
| Colorado | 2,735 | 5,035 | 7,724 | 9,359 | 10,066 | 10.5 |
| Idaho | 627 | 1,058 | 1,657 | 2,092 | 2,277 | 10.4 |
| Montana | 621 | 1,039 | 1,606 | 1,938 | 2,103 | 9.8 |
| Utah | 1,051 | 1,929 | 3,170 | 3,827 | 4,118 | 11.1 |
| Wyoming | 337 | 592 | 794 | 918 | 998 | 8.7 |
| Far West | 34,909 | 61,002 | 98,168 | 117,841 | 126,111 | 10.4 |
| Alaska | 447 | 887 | 1,239 | 1,490 | 1,573 | 10.2 |
| California | 26,524 | 46,267 | 74,116 | 88,215 | 94,178 | 10.2 |
| Hawaii | 919 | 1,671 | 2,733 | 3,260 | 3,485 | 10.8 |
| Nevada | 836 | 1,534 | 2,767 | 3,477 | 3,747 | 12.2 |
| Oregon | 2,356 | 3,844 | 6,137 | 7,349 | 7,999 | 9.9 |
| Washington | 3,828 | 6,799 | 11,176 | 14,051 | 15,129 | 11.1 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 28. Medicaid Personal Health Care Expenditures as a Share of Total Personal Health Care Expenditures, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 |
|---|---|---|---|---|---|
|
| |||||
| Percent | |||||
| United States | 11.4 | 10.4 | 11.8 | 14.3 | 14.5 |
| New England | 14.6 | 13.0 | 15.9 | 18.2 | 16.6 |
| Connecticut | 11.0 | 11.2 | 12.8 | 16.0 | 16.4 |
| Maine | 15.9 | 15.5 | 16.6 | 20.9 | 21.0 |
| Massachusetts | 16.3 | 13.7 | 18.1 | 17.9 | 15.8 |
| New Hampshire | 10.7 | 8.8 | 10.3 | 21.2 | 12.9 |
| Rhode Island | 16.4 | 15.1 | 17.6 | 23.0 | 23.1 |
| Vermont | 15.8 | 12.8 | 13.4 | 16.2 | 15.5 |
| Mideast | 16.2 | 15.5 | 16.2 | 19.1 | 19.1 |
| Delaware | 8.4 | 7.3 | 8.0 | 10.6 | 11.0 |
| District of Columbia | 11.8 | 13.3 | 11.8 | 14.8 | 15.8 |
| Maryland | 10.8 | 9.1 | 10.1 | 12.8 | 12.7 |
| New Jersey | 11.7 | 10.1 | 12.4 | 14.8 | 15.0 |
| New York | 22.4 | 23.0 | 23.4 | 26.3 | 26.9 |
| Pennsylvania | 11.0 | 9.3 | 9.8 | 13.3 | 12.3 |
| Great Lakes | 11.2 | 10.8 | 11.5 | 14.1 | 14.3 |
| Illinois | 11.1 | 9.3 | 8.8 | 12.8 | 13.3 |
| Indiana | 8.6 | 10.0 | 12.2 | 15.8 | 16.9 |
| Michigan | 12.8 | 11.5 | 12.3 | 13.8 | 14.2 |
| Ohio | 8.6 | 10.5 | 12.5 | 14.5 | 13.9 |
| Wisconsin | 17.0 | 14.5 | 13.2 | 14.8 | 14.7 |
| Plains | 9.6 | 9.5 | 10.5 | 12.7 | 12.7 |
| Iowa | 9.4 | 9.4 | 10.9 | 13.0 | 13.1 |
| Kansas | 8.8 | 7.5 | 9.2 | 10.4 | 11.1 |
| Minnesota | 14.4 | 14.1 | 12.9 | 14.6 | 15.7 |
| Missouri | 6.5 | 6.7 | 8.6 | 12.0 | 10.3 |
| Nebraska | 7.7 | 7.5 | 9.5 | 12.0 | 12.7 |
| North Dakota | 8.2 | 10.7 | 12.4 | 13.2 | 13.3 |
| South Dakota | 10.5 | 9.9 | 11.5 | 13.3 | 13.5 |
| Southeast | 9.1 | 8.2 | 10.4 | 13.0 | 13.4 |
| Alabama | 9.3 | 8.0 | 8.9 | 10.7 | 10.6 |
| Arkansas | 14.2 | 12.5 | 12.6 | 16.0 | 16.5 |
| Florida | 4.3 | 4.8 | 7.3 | 9.7 | 10.5 |
| Georgia | 10.6 | 9.1 | 10.4 | 12.3 | 13.7 |
| Kentucky | 11.8 | 11.5 | 13.9 | 16.7 | 16.2 |
| Louisiana | 11.7 | 11.5 | 14.8 | 19.3 | 20.5 |
| Mississippi | 12.6 | 9.7 | 13.4 | 17.0 | 16.8 |
| North Carolina | 10.2 | 9.3 | 11.5 | 13.6 | 14.1 |
| South Carolina | 12.7 | 9.5 | 13.7 | 14.9 | 14.7 |
| Tennessee | 9.4 | 8.6 | 12.1 | 14.1 | 13.5 |
| Virginia | 8.7 | 7.2 | 7.9 | 9.5 | 9.7 |
| West Virginia | 7.1 | 6.9 | 11.2 | 19.3 | 20.7 |
| Southwest | 7.4 | 6.7 | 8.8 | 11.9 | 12.1 |
| Arizona | 0.0 | 2.1 | 6.7 | 12.0 | 11.9 |
| New Mexico | 8.2 | 8.6 | 10.3 | 14.2 | 14.9 |
| Oklahoma | 11.2 | 10.6 | 11.5 | 13.4 | 12.6 |
| Texas | 8.0 | 6.8 | 8.7 | 11.5 | 11.9 |
| Rocky Mountains | 7.6 | 6.9 | 8.6 | 10.5 | 11.2 |
| Colorado | 7.0 | 6.1 | 7.4 | 8.5 | 9.6 |
| Idaho | 8.4 | 7.1 | 9.9 | 12.9 | 12.7 |
| Montana | 11.0 | 10.0 | 12.3 | 14.4 | 15.3 |
| Utah | 7.4 | 7.9 | 9.0 | 11.3 | 11.6 |
| Wyoming | 4.5 | 5.0 | 9.0 | 13.4 | 13.7 |
| Far West | 10.9 | 8.7 | 9.4 | 11.4 | 12.2 |
| Alaska | 8.8 | 7.8 | 12.5 | 14.6 | 17.4 |
| California | 11.5 | 9.0 | 9.4 | 11.1 | 12.0 |
| Hawaii | 10.6 | 8.5 | 7.7 | 9.1 | 10.2 |
| Nevada | 5.9 | 4.5 | 5.5 | 9.5 | 9.2 |
| Oregon | 7.9 | 6.8 | 8.9 | 11.2 | 11.9 |
| Washington | 9.9 | 9.1 | 11.3 | 13.6 | 14.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Highlights
The GSP measures the value of goods and services produced in each State. Nationwide, health care expenditures in 19922 represented 12.1 percent of total GSP, up from 8.1 percent in 1980. By State, 1992 health spending ranged from 15.7 percent of GSP in West Virginia to 5.7 percent in Alaska.
Health spending's share of GSP increased most rapidly in Louisiana and West Virginia. In these States, the GSP share rose 7.0 percentage points or more between 1980 and 1992, compared with 4.1 percentage points nationwide during the same period.
U.S. PHCE per capita grew 9.3 percent annually between 1980 and 1992. The fastest growth occurred in the Southeast, where spending increased at a 10.1-percent annual rate; the slowest growth occurred in the Far West, where spending increased at an 8.2-percent annual rate.
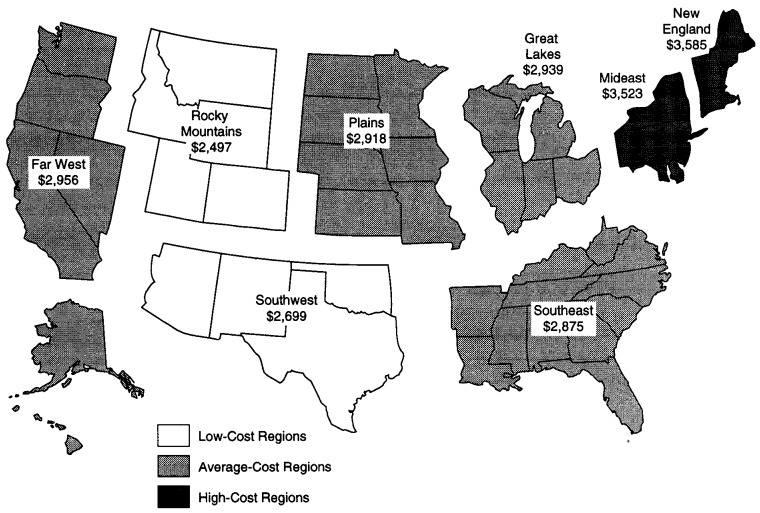
New England led the Nation in health spending per capita: In 1993, New England's PHCE spending averaged $3,585, 19 percent higher than the U.S. average. As it has since 1980, the Rocky Mountains continued to spend the lowest amounts per capita: PHCE spending amounted to $2,497 per capita in 1993,17 percent below the U.S. average.
The Medicare and Medicaid programs funded more than one-third of all PHCE in 1993. By State, funding of health care by these two programs ranged from 44.6 percent in New York to 23.8 percent in Alaska.
Personal Health Care
PHCE in the United States reached $778.5 billion in 1993, growing at an average annual rate of 10.3 percent since 1980. PHCE measures spending on therapeutic goods or services rendered to treat or prevent a specific disease or condition in a specific person (Lazenby et al., 1992). In 1993, Americans spent an average of $3,020 on PHCE per person, more than three times the $953 per person spent in 1980 (Table 1). During this period, spending per capita in the Southeast grew the fastest, averaging 10.1 percent annually. The Far West region, maintaining the highest concentration of health maintenance organization (HMO) enrollees in the Nation, experienced the slowest growth in PHCE per capita (8.2 percent annually).
Table 1. Personal Health Care Expenditures per Capita and Average Annual Percent Growth, by Region: Selected Calendar Years 1980-93.
| Region of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
| United States | $953 | $1,577 | $2,439 | $2,852 | $3,020 | 9.3 |
| New England | 1,035 | 1,743 | 2,896 | 3,365 | 3,585 | 10.0 |
| Mideast | 1,050 | 1,778 | 2,818 | 3,310 | 3,523 | 9.8 |
| Great Lakes | 964 | 1,574 | 2,375 | 2,777 | 2,939 | 9.0 |
| Plains | 964 | 1,573 | 2,387 | 2,765 | 2,918 | 8.9 |
| Southeast | 825 | 1,418 | 2,297 | 2,715 | 2,875 | 10.1 |
| Southwest | 870 | 1,408 | 2,163 | 2,551 | 2,699 | 9.1 |
| Rocky Mountains | 815 | 1,347 | 2,048 | 2,377 | 2,497 | 9.0 |
| Far West | 1,065 | 1,693 | 2,421 | 2,799 | 2,956 | 8.2 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
New England led the Nation in the level of health spending per capita: In 1993, New England's PHCE spending averaged $3,585 (Figure 1), 19 percent higher than the U.S. average. Per capita health spending in New England, the Mideast, and the Southeast grew faster than the nationwide per capita from 1980 to 1993. Per capita PHCE in all other regions grew more slowly than the U.S. average, and their per capita spending relative to the U.S. average fell. As it has since 1980, the Rocky Mountains continued to spend the lowest amounts per capita: PHCE spending in 1993 amounted to $2,497 per capita, 17 percent below the U.S. average.
Figure 1. Per Capita Personal Health Care Expenditures, by Region of Provider:1 1993.
1 United States per capita equals $3,020.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Nationwide, the distribution of services among PHCE categories shifted significantly between 1980 and 1993. While hospital care remained the single largest component of PHCE, its prominence declined from 46.9 percent in 1980 to 41.6 percent in 1993. Most of this decline, concentrated in the 1983-88 period, resulted from the implementation of the Medicare prospective payment system (PPS) and the tightening of admission and length-of-stay guidelines by private health insurers. These public and private sector actions were aimed at reducing the growth of hospital spending. Larger PHCE shares for physician, other professional, and home health services offset most of the decline in hospital share. By region and State, the largest declines in hospital share of PHCE occurred in New England and the States of Massachusetts, Rhode Island, and Maryland. Massachusetts, with 54.8 percent of PHCE for hospital care, spent the highest proportion of any State on hospital care in 1980; by 1993, that share had fallen more than any other State's share to 42.8 percent. Almost no change in hospital share occurred in Montana, Alaska, South Dakota, Texas, or South Carolina, while the hospital share of PHCE increased in three States (Arkansas, Idaho, and Hawaii).
Medicare and Medicaid funded more than one-third of all PHCE in 1993, up from 28.2 percent in 1980. By State, funding for health care by these two programs ranged from 44.6 percent in New York to 23.8 percent in Alaska.
One way of measuring the importance of health spending on a State's economy is as a share of GSP GSP measures the market value of goods and services produced by the labor and property located within a State (Beemiller and Dunbar, 1994). SHEA measure the value of output for the health care industry. In 1992 (the latest year for which GSP is available), health care accounted for 12.1 percent of GSP nationwide, up from 8.1 percent in 1980. In West Virginia, the health care sector represented 15.7 percent of the 1992 GSP; in Florida, 15.6 percent (Table 2). In contrast, Alaska consumed 5.7 percent of its output in health care.
Table 2. Personal Health Care Expenditures, by Region and State as a Percent of Gross State Product: Selected Calendar Years 1980-921.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 |
|---|---|---|---|---|
|
| ||||
| Percent | ||||
| United States | 8.1 | 9.3 | 11.0 | 12.1 |
| New England | 9.1 | 9.7 | 11.7 | 12.9 |
| Connecticut | 7.8 | 8.5 | 10.6 | 11.7 |
| Maine | 9.2 | 10.2 | 11.7 | 13.3 |
| Massachusetts | 9.9 | 10.2 | 12.4 | 13.6 |
| New Hampshire | 7.7 | 8.3 | 10.7 | 12.2 |
| Rhode Island | 10.2 | 11.6 | 13.2 | 14.7 |
| Vermont | 8.3 | 9.1 | 10.5 | 11.8 |
| Mideast | 8.7 | 9.8 | 11.4 | 12.5 |
| Delaware | 7.6 | 8.4 | 8.7 | 8.8 |
| District of Columbia | 7.8 | 8.9 | 9.6 | 9.9 |
| Maryland | 9.0 | 9.5 | 10.8 | 12.2 |
| New Jersey | 7.2 | 8.1 | 9.6 | 10.7 |
| New York | 9.1 | 9.7 | 11.5 | 12.6 |
| Pennsylvania | 9.1 | 11.7 | 13.3 | 14.5 |
| Great Lakes | 8.3 | 9.6 | 11.2 | 12.2 |
| Illinois | 8.1 | 9.1 | 10.1 | 11.2 |
| Indiana | 7.8 | 9.4 | 11.3 | 12.5 |
| Michigan | 9.1 | 9.7 | 11.7 | 12.5 |
| Ohio | 8.2 | 10.2 | 12.0 | 13.0 |
| Wisconsin | 8.3 | 9.5 | 11.4 | 12.4 |
| Plains | 8.5 | 9.8 | 11.5 | 12.3 |
| Iowa | 7.7 | 9.4 | 11.0 | 11.7 |
| Kansas | 8.1 | 8.9 | 10.7 | 11.7 |
| Minnesota | 8.6 | 10.1 | 11.5 | 12.1 |
| Missouri | 9.2 | 10.4 | 12.2 | 13.3 |
| Nebraska | 8.3 | 9.0 | 10.3 | 11.1 |
| North Dakota | 8.3 | 10.6 | 13.5 | 14.7 |
| South Dakota | 8.8 | 9.9 | 11.6 | 12.0 |
| Southeast | 8.1 | 9.6 | 11.8 | 12.9 |
| Alabama | 8.9 | 10.4 | 13.0 | 14.4 |
| Arkansas | 8.8 | 10.4 | 12.6 | 13.1 |
| Florida | 10.2 | 12.2 | 14.4 | 15.6 |
| Georgia | 8.2 | 8.8 | 11.2 | 12.1 |
| Kentucky | 7.4 | 9.4 | 11.7 | 12.9 |
| Louisiana | 5.5 | 7.7 | 10.8 | 12.5 |
| Mississippi | 8.0 | 9.6 | 11.9 | 12.8 |
| North Carolina | 7.1 | 7.7 | 9.7 | 10.6 |
| South Carolina | 7.7 | 8.8 | 10.5 | 12.0 |
| Tennessee | 9.0 | 10.6 | 12.8 | 13.9 |
| Virginia | 7.5 | 8.3 | 9.4 | 10.2 |
| West Virginia | 8.5 | 11.3 | 13.9 | 15.7 |
| Southwest | 6.3 | 7.8 | 10.3 | 11.5 |
| Arizona | 8.3 | 10.0 | 12.5 | 13.4 |
| New Mexico | 5.6 | 7.8 | 10.7 | 11.2 |
| Oklahoma | 6.8 | 8.5 | 11.0 | 12.5 |
| Texas | 6.1 | 7.3 | 9.8 | 11.1 |
| Rocky Mountains | 6.5 | 8.1 | 10.1 | 10.8 |
| Colorado | 7.3 | 8.8 | 10.6 | 11.3 |
| Idaho | 6.4 | 8.1 | 9.1 | 10.0 |
| Montana | 6.7 | 9.5 | 12.0 | 12.7 |
| Utah | 6.9 | 8.1 | 10.3 | 10.8 |
| Wyoming | 3.1 | 4.4 | 6.3 | 7.0 |
| Far West | 7.9 | 8.9 | 9.7 | 11.0 |
| Alaska | 2.9 | 3.4 | 4.5 | 5.7 |
| California | 8.3 | 9.1 | 9.8 | 11.2 |
| Hawaii | 7.4 | 9.3 | 9.4 | 9.8 |
| Nevada | 7.1 | 8.4 | 8.7 | 9.4 |
| Oregon | 7.8 | 9.7 | 10.9 | 11.7 |
| Washington | 7.5 | 9.3 | 10.0 | 11.0 |
Latest year for which gross State product is available.
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
A State's share of GSP devoted to health care is influenced by the age distribution of its population. People 65 years of age or over consume four times as much health care as those under 65 years of age (Waldo et al., 1989). In both West Virginia and Florida in 1993,15.3 percent or more of the population was 65 years of age or over (Table 3), compared with 12.7 percent nationwide. In Alaska, only 4.5 percent of the population is elderly.
Table 3. Total Population and Population 65 Years of Age or Over, by Region and State: July 1,1980 and July 1,1993.
| Region and State | Total Population | 65 Years of Age or Over | 65 Years of as a Age or Over Percent of Total | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| 1980 | 1993 | Average Annual percent Growth 1980-93 | 1980 | 1993 | Average Annual Percent Growth 1980-93 | 1980 | 1993 | |
|
| ||||||||
| Thousands | Thousands | |||||||
| United States | 227,225 | 257,783 | 1.0 | 25,707 | 32,773 | 1.9 | 11.3 | 12.7 |
| New England | 12,372 | 13,235 | 0.5 | 1,529 | 1,833 | 1.4 | 12.4 | 13.9 |
| Connecticut | 3,113 | 3,278 | 0.4 | 368 | 461 | 1.8 | 11.8 | 14.1 |
| Maine | 1,127 | 1,240 | 0.7 | 142 | 171 | 1.5 | 12.6 | 13.8 |
| Massachusetts | 5,746 | 6,018 | 0.4 | 730 | 843 | 1.1 | 12.7 | 14.0 |
| New Hampshire | 924 | 1,124 | 1.5 | 104 | 134 | 2.0 | 11.2 | 11.9 |
| Rhode Island | 949 | 1,000 | 0.4 | 128 | 155 | 1.5 | 13.4 | 15.5 |
| Vermont | 513 | 576 | 0.9 | 58 | 70 | 1.4 | 11.4 | 12.1 |
| Mideast | 42,272 | 44,278 | 0.4 | 5,104 | 6,076 | 1.4 | 12.1 | 13.7 |
| Delaware | 595 | 698 | 1.2 | 60 | 87 | 3.0 | 10.0 | 12.5 |
| District of Columbia | 638 | 579 | -0.7 | 74 | 77 | 0.3 | 11.6 | 13.3 |
| Maryland | 4,228 | 4,958 | 1.2 | 399 | 551 | 2.5 | 9.4 | 11.1 |
| New Jersey | 7,376 | 7,859 | 0.5 | 865 | 1,069 | 1.6 | 11.7 | 13.6 |
| New York | 17,567 | 18,153 | 0.3 | 2,166 | 2,389 | 0.8 | 12.3 | 13.2 |
| Pennsylvania | 11,868 | 12,030 | 0.1 | 1,540 | 1,903 | 1.6 | 13.0 | 15.8 |
| Great Lakes | 41,694 | 42,956 | 0.2 | 4,520 | 5,522 | 1.6 | 10.8 | 12.9 |
| Illinois | 11,435 | 11,686 | 0.2 | 1,268 | 1,475 | 1.2 | 11.1 | 12.6 |
| Indiana | 5,491 | 5,706 | 0.3 | 589 | 728 | 1.6 | 10.7 | 12.8 |
| Michigan | 9,256 | 9,460 | 0.2 | 918 | 1,167 | 1.9 | 9.9 | 12.3 |
| Ohio | 10,801 | 11,061 | 0.2 | 1,176 | 1,476 | 1.8 | 10.9 | 13.3 |
| Wisconsin | 4,712 | 5,044 | 0.5 | 568 | 677 | 1.4 | 12.0 | 13.4 |
| Plains | 17,208 | 18,082 | 0.4 | 2,209 | 2,525 | 1.0 | 12.8 | 14.0 |
| Iowa | 2,914 | 2,821 | -0.2 | 389 | 436 | 0.9 | 13.4 | 15.5 |
| Kansas | 2,369 | 2,535 | 0.5 | 308 | 352 | 1.1 | 13.0 | 13.9 |
| Minnesota | 4,085 | 4,524 | 0.8 | 482 | 568 | 1.3 | 11.8 | 12.6 |
| Missouri | 4,922 | 5,235 | 0.5 | 650 | 741 | 1.0 | 13.2 | 14.2 |
| Nebraska | 1,572 | 1,613 | 0.2 | 207 | 229 | 0.8 | 13.1 | 14.2 |
| North Dakota | 654 | 637 | -0.2 | 81 | 94 | 1.1 | 12.4 | 14.7 |
| South Dakota | 691 | 716 | 0.3 | 91 | 105 | 1.1 | 13.2 | 14.7 |
| Southeast | 52,881 | 61,927 | 1.2 | 6,255 | 8,369 | 2.3 | 11.8 | 13.5 |
| Alabama | 3,900 | 4,181 | 0.5 | 442 | 546 | 1.6 | 11.3 | 13.1 |
| Arkansas | 2,289 | 2,426 | 0.4 | 314 | 361 | 1.1 | 13.7 | 14.9 |
| Florida | 9,840 | 13,726 | 2.6 | 1,704 | 2,526 | 3.1 | 17.3 | 18.4 |
| Georgia | 5,486 | 6,902 | 1.8 | 520 | 698 | 2.3 | 9.5 | 10.1 |
| Kentucky | 3,664 | 3,794 | 0.3 | 412 | 484 | 1.3 | 11.2 | 12.8 |
| Louisiana | 4,223 | 4,290 | 0.1 | 406 | 489 | 1.4 | 9.6 | 11.4 |
| Mississippi | 2,525 | 2,640 | 0.3 | 290 | 330 | 1.0 | 11.5 | 12.5 |
| North Carolina | 5,899 | 6,952 | 1.3 | 608 | 867 | 2.8 | 10.3 | 12.5 |
| South Carolina | 3,135 | 3,630 | 1.1 | 290 | 427 | 3.0 | 9.2 | 11.8 |
| Tennessee | 4,600 | 5,094 | 0.8 | 520 | 651 | 1.7 | 11.3 | 12.8 |
| Virginia | 5,368 | 6,473 | 1.4 | 509 | 712 | 2.6 | 9.5 | 11.0 |
| West Virginia | 1,951 | 1,818 | -0.5 | 239 | 278 | 1.2 | 12.2 | 15.3 |
| Southwest | 21,426 | 26,815 | 1.7 | 2,186 | 2,985 | 2.4 | 10.2 | 11.1 |
| Arizona | 2,738 | 3,945 | 2.8 | 311 | 532 | 4.2 | 11.4 | 13.5 |
| New Mexico | 1,309 | 1,616 | 1.6 | 117 | 178 | 3.3 | 8.9 | 11.0 |
| Oklahoma | 3,041 | 3,233 | 0.5 | 378 | 440 | 1.2 | 12.4 | 13.6 |
| Texas | 14,338 | 18,022 | 1.8 | 1,379 | 1,836 | 2.2 | 9.6 | 10.2 |
| Rocky Mountains | 6,592 | 7,834 | 1.3 | 577 | 817 | 2.7 | 8.8 | 10.4 |
| Colorado | 2,909 | 3,564 | 1.6 | 249 | 359 | 2.8 | 8.6 | 10.1 |
| Idaho | 948 | 1,100 | 1.2 | 95 | 130 | 2.5 | 10.0 | 11.8 |
| Montana | 789 | 841 | 0.5 | 85 | 112 | 2.1 | 10.8 | 13.4 |
| Utah | 1,473 | 1,860 | 1.8 | 110 | 164 | 3.1 | 7.5 | 8.8 |
| Wyoming | 474 | 470 | -0.1 | 37 | 51 | 2.5 | 7.9 | 10.9 |
| Far West | 32,780 | 42,656 | 2.0 | 3,329 | 4,646 | 2.6 | 10.2 | 10.9 |
| Alaska | 405 | 598 | 3.0 | 12 | 27 | 6.5 | 2.9 | 4.5 |
| California | 23,801 | 31,217 | 2.1 | 2,432 | 3,299 | 2.4 | 10.2 | 10.6 |
| Hawaii | 968 | 1,166 | 1.4 | 77 | 138 | 4.6 | 8.0 | 11.8 |
| Nevada | 810 | 1,382 | 4.2 | 67 | 156 | 6.7 | 8.3 | 11.3 |
| Oregon | 2,641 | 3,035 | 1.1 | 306 | 417 | 2.4 | 11.6 | 13.7 |
| Washington | 4,155 | 5,259 | 1.8 | 435 | 610 | 2.6 | 10.5 | 11.6 |
SOURCE: ( U.S. Bureau of the Census, 1994).
Hospital Care
Americans spent $323.9 billion for hospital care in 1993, accounting for 41.6 percent of PHCE. These expenditures paid for all hospital-based services provided to patients and billed by the hospital. The annual rate of growth in total hospital expenditures decelerated for the third straight year in 1993 because of more rigorous hospital reviews and shorter lengths of stay encouraged by most third-party payers. Annual growth in spending during the 1980-93 period averaged 9.4 percent; the growth rates in both 1992 (8.4 percent) and 1993 (6.7 percent) fell below this 13-year average.
The five States exhibiting the highest average annual growth rate in hospital expenditures for 1980-93 were New Hampshire, South Carolina, New Mexico, Hawaii, and Georgia. Higher-than-average demand for hospital services in these States paralleled their higher-than-average population growth, while high demand for hospital services in Georgia and Hawaii also corresponded to growth in the number of community hospital inpatient days (American Hospital Association, 1993). Four States exhibited annual expenditure growth under 8 percent for this 13-year period: Iowa, Kansas, Michigan, and Illinois. Population growth in these States was one-half or less than the overall U.S. rate; both community hospital admissions and inpatient days showed declines greater than the overall U.S. rate (American Hospital Association, 1993).
In 1993, 88 percent of all hospital care expenditures in the United States was spent in short-term, acute-care community hospitals. Regionally, this share varied from 85.1 percent in the Southwest to 92.4 percent in the Great Lakes. In Alaska, a large number of Federal hospitals deliver care to the Native American and defense communities. This State recorded the smallest percentage of hospital care expenditures in community hospitals (61.8 percent) of any State.
Five States accounted for more than one-third (37.4 percent) of total spending for hospital care in 1993: California, New York, Texas, Pennsylvania, and Florida. Not surprisingly, these States also boasted the highest resident population counts. From a regional perspective, two regions, the Mideast and the Southeast, accounted for 44.2 percent of total hospital expenditures in 1993. The share of total hospital expenditures held by 6 of the 8 regions has remained relatively constant over the last 13 years. However, the share of hospital spending in the Great Lakes region, driven by the decline in the share of spending in Illinois, dropped from 19.3 percent in 1980 to 16.7 percent in 1993. More than offsetting this decline, the share of spending in the Southeast region rose from 20.3 percent in 1980 to 23.4 percent in 1993, driven by share increases in Florida, Georgia, and North Carolina. Slow population growth contributed to the decline in share of total hospital expenditures in the Great Lakes region, as stronger-than-average population growth contributed to an increased share of spending in the Southeast.
In 1993, the level of regional hospital spending per capita varied significantly across the Nation. Spending per capita for hospital care in New England and the Mideast averaged, respectively, 15 and 21 percent more than the U.S. per capita (Table 4). The Great Lakes, Plains, and Southeast regions each showed per capita spending levels approximately equal to the U.S. average. In the Southwest, Rocky Mountains, and Far West, the regional per capita expenditures dropped below the U.S. average by 9 to 20 percent.
Table 4. Regional per Capita Personal Health Care Expenditures as a Percent of U.S. Spending: Calendar Years 1980 and 1993.
| Region of Provider | Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Drugs and Other Medical Non-Durables | Vision Products and Other Medical Durables | Nursing Home Care | Other Personal Health Care |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Percent | ||||||||||
| 1980 | ||||||||||
| United States | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| New England | 109 | 117 | 84 | 104 | 101 | 135 | 93 | 84 | 146 | 128 |
| Mideast | 110 | 114 | 93 | 101 | 97 | 203 | 95 | 110 | 147 | 125 |
| Great Lakes | 101 | 105 | 97 | 101 | 101 | 75 | 98 | 99 | 98 | 92 |
| Plains | 101 | 102 | 96 | 91 | 105 | 64 | 94 | 110 | 136 | 81 |
| Southeast | 87 | 87 | 90 | 78 | 81 | 74 | 102 | 84 | 67 | 91 |
| Southwest | 91 | 86 | 102 | 84 | 91 | 62 | 108 | 116 | 76 | 89 |
| Rocky Mountains | 86 | 79 | 90 | 101 | 93 | 58 | 90 | 114 | 79 | 124 |
| Far West | 112 | 102 | 138 | 147 | 137 | 81 | 110 | 102 | 79 | 95 |
| 1993 | ||||||||||
| United States | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| New England | 119 | 115 | 105 | 119 | 119 | 132 | 106 | 94 | 172 | 179 |
| Mideast | 117 | 121 | 102 | 108 | 113 | 139 | 102 | 115 | 150 | 114 |
| Great Lakes | 97 | 100 | 92 | 96 | 91 | 73 | 98 | 100 | 114 | 79 |
| Plains | 97 | 98 | 91 | 90 | 91 | 72 | 90 | 103 | 126 | 96 |
| Southeast | 95 | 97 | 92 | 83 | 93 | 128 | 105 | 91 | 79 | 96 |
| Southwest | 89 | 91 | 88 | 81 | 97 | 93 | 97 | 99 | 67 | 101 |
| Rocky Mountains | 83 | 80 | 84 | 106 | 86 | 60 | 85 | 112 | 68 | 112 |
| Far West | 98 | 87 | 130 | 129 | 108 | 60 | 99 | 97 | 59 | 88 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
From 1980 to 1993, most regions exhibited only small changes in their per capita spending for hospital care relative to the U.S. average. For the Southeast and Far West, however, spending relative to the U.S. average changed dramatically. In the Southeast in 1980, spending per capita was 13 percent below the U.S. average; by 1993, spending per capita had moved to within 3 percentage points of the U.S. average. In the Far West in 1980, hospital spending per capita approximated the national average (102 percent); by 1993, spending had plunged to 13 percent below the U.S. average. This region maintains the highest penetration of HMO enrollees (29.3 percent) (InterStudy, 1991-95) and the highest percentage of the population receiving Medicaid services (14.2 percent) which account, in part, for smaller spending shares in the hospital sector.
Physician Services
From 1980 to 1993, expenditures for physician services in the United States averaged an annual growth of 10.8 percent. These expenditures totaled $171.2 billion and accounted for 22.0 percent of PHCE in 1993. These expenditures include care provided in offices and clinics of physicians, care provided and billed by physicians for hospital visits, services provided at ambulatory surgical centers, and independent medical laboratory costs. These expenditures also cover spending for physician services provided through HMOs, specifically including all services provided at staff-model HMOs.3 Professional fees received by physicians from hospitals are excluded from physician expenditures; these fees are paid from hospital revenues and are included with hospital estimates.
Many different factors influence growth in physician expenditures, including changes in population and its distribution by age and disability status, physician concentrations, personal income per capita, managed-care penetration, physician practice patterns, and type of insurance coverage (or lack thereof). The States with the fastest annual growth rates in physician expenditures during 1980-93 were New Hampshire (14.8 percent) and Nevada (13.1 percent). The slowest growing States included Wyoming, Michigan, Iowa, Montana, the District of Columbia, West Virginia, and Nebraska, each with average annual growth rates below 9.0 percent.
New England, the region with the fastest average annual growth, moved in rank from the lowest per capita physician spending region in 1980 to the second highest in 1993, as the region substituted physician services for more expensive hospitalizations. Per capita personal income growth (U.S. Bureau of Economic Analysis, 1994) and growth in physicians per 100,000 residents (Table 5) in New England were the highest in the United States during this period. The Great Lakes showed the slowest growth (9.5 percent) in spending per capita for physician services. This region also experienced the slowest regional growth in population in the United States, but maintained near average growth in per capita personal income, physicians per 100,000 residents, and per capita PHCE. The level of physician spending per capita ranged from 84 percent of the U.S. average in the Rocky Mountains to 130 percent in the Far West (Table 4). The Far West region maintained the highest per capita spending for physician services for the entire 13-year period. Higher-than-average physician expenditures per capita in the Far West region in 1993 have been offset by lower per capita spending in other components of spending, such as hospital, nursing home, and home health care. While the penetration of HMOs4 influenced the choice of services in the Far West in 1993, PHCE per capita for the Far West amounted to $2,956, just below the U.S. average in 1993.
Table 5. Physicians1 per 100,000 Residents and Average Annual Percent Growth: Calendar Years 1980 and 1993.
| Region | 1980 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|
| United States | 124 | 164 | 2.2 |
| New England | 146 | 206 | 2.7 |
| Mideast | 140 | 198 | 2.7 |
| Great Lakes | 116 | 156 | 2.3 |
| Plains | 113 | 151 | 2.3 |
| Southeast | 104 | 147 | 2.6 |
| Southwest | 112 | 141 | 1.8 |
| Rocky Mountains | 120 | 153 | 1.9 |
| Far West | 151 | 175 | 1.1 |
Includes non-Federal office-based physicians practicing in the United States (excluding the Pacific Islands, Virgin Islands, and Puerto Rico) and active non-Federal doctors of osteopathy.
SOURCES: Data from the American Medical Association and the American Osteopathic Associations; Estimates prepared by the Office of National Health Statistics, Health Care Financing Administration.
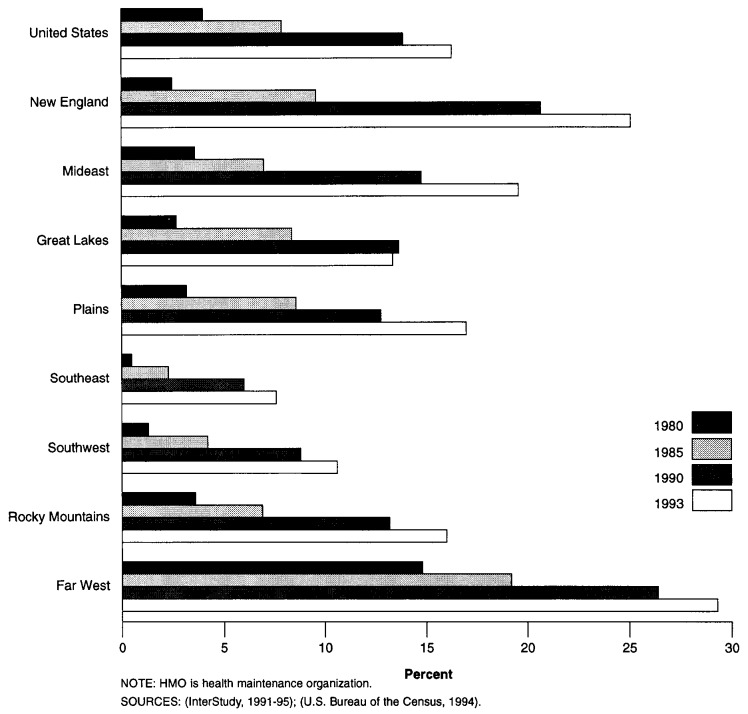
HMOs are growing rapidly, asserting more influence on physician expenditures. In 1993, 16.3 percent of the U.S. population—42 million individuals—were enrolled in HMOs (Figure 2), up from 4.0 percent in 1980. As more individuals have enrolled in HMOs, the mix of services delivered has changed. HMOs are perceived as controlling costs by negotiating favorable payment rates with health care providers, reducing hospital visits and lengths of stays, limiting access to specialized services, and emphasizing preventive care.
Figure 2. HMO Enrollment as a Percent of Population, by Region: 1980-93.
During this same period, many physicians in private practice have entered into agreements with managed-care plans, such as group-model HMOs, individual practice associations (IPAs), and preferred provider organizations (PPOs). In 1988,61 percent of physicians in practice had a managed-care contract; by 1993 this number had grown to 75 percent (Emmons and Simon, 1994). In 1993, the regions with the greatest managed-care participation rates by physicians were the Far West and the Great Lakes, both with 82 percent. The Far West region also had the highest percentage of the population enrolled in HMOs throughout the 1980-93 period (29.3 percent in 1993). This region, which includes California, was a front runner of the HMO movement and had a large percentage of the population enrolled in HMOs before the 1980s (InterStudy, 1991). In contrast, the Southeast had the lowest penetration of HMO enrollment per population in 1993 (7.6 percent). This region also experienced the highest growth in enrollment, increasing at an average annual rate of 23.4 percent between 1980 and 1993.
Dental Services
Expenditures for dental services grew from $13.3 billion in 1980 to $37.4 billion in 1993, increasing at an 8.3-percent average annual rate. This rate of growth made this component the slowest growing medical care category in PHCE. In 1980, spending for dental services was 6.2 percent of PHCE nationwide; by 1993, this share had dropped to 4.8 percent.
Six States exhibited double-digit average annual growth rates throughout the 1980-93 period: Alaska, New Hampshire, Maine, Utah, Florida, and Nevada. Three States showed average annual growth rates below 7 percent: Michigan, Iowa, and Montana. With the exception of Maine, States experiencing double-digit growth in dental spending were growing more rapidly in population than the United States overall for the 1980-93 period; similarly, population growth in the slowest growing dental spending States was minimal or negative.
By region, dental spending per capita in the Far West, New England, Mideast, and Rocky Mountains ranged from 6 to 29 percent above the U.S. average in 1993. In the Great Lakes, Plains, Southeast, and Southwest, spending per capita fell below the U.S. average by 4 to 19 percent. These spending differentials paralleled differences in personal income per capita, except in the Rocky Mountain region, where personal income per capita was 92 percent of the U.S. per capita. These spending differentials also paralleled the differences in the concentration of dentists (American Dental Association, 1993) by region, except in the Great Lakes, where the concentration was at the U.S. level.
Other Professional Services
Other professional services collectively represent the second fastest growing component of PHCE, averaging 17.4 percent growth for the period 1980-93. This segment reached $51.2 billion in 1993, accounting for 6.6 percent of PHCE. Other professional services expenditures include spending for services provided in offices and clinics of licensed other professionals such as chiropractors, optometrists, and podiatrists. Additionally, spending in kidney dialysis clinics, alcohol treatment centers, rehabilitation clinics, and other specialty clinics and other health care establishments not elsewhere classified are included with other professional services. Medicare ambulance expenditures are also included in this category.
The regions with the fastest growth were the Southeast and Southwest, both with average annual growth of 18.9 percent. Slowest growing regions included the Plains and Great Lakes. In 1993, per capita spending was 19 percent higher than the U.S. average in New England and 14 percent lower in the Rocky Mountains (Table 4). The Far West region showed the most change in per capita spending, dropping from 37 percent to 8 percent above the U.S. average from 1980 to 1993.
Nevada had the highest growth in expenditures for other professional services for the 1980-93 period (21.3 percent). Similar to the trend shown in physician expenditures, population increases drove the exceptionally high growth in other professional expenditures in Nevada. Other States with high growth included Delaware, Georgia, Maryland, and North Carolina. The lowest average annual growth rates (15.0 percent or less) in the United States were found in Iowa, Idaho, Wyoming, North Dakota, and Minnesota.
Home Health Care
Home health care expenditures totaled $23.0 billion in 1993, 3.0 percent of all PHCE. Although the smallest component of PHCE in 1980, home health care did not retain this rank for long: It grew faster than any other personal health spending category since 1980, averaging increases of 19.1 percent annually.
Expenditures for home health care in SHEA cover spending for services and products provided by public and private freestanding home health agencies. These agencies may be certified to participate in either Medicare and/or Medicaid, or certified in neither program. Agencies delivering Medicaid-funded personal-care services in the home are also counted here. Personal-care services under Medicaid can cover a broader range of services in the home and be delivered by a wider range of qualified persons than those narrowly specified under Medicare and Medicaid as home health benefits. Expenditures for home health services that are delivered through hospital-based agencies are excluded from the SHEA category of home health care; expenditures for those services are counted with hospital expenditures.
Several factors coalesced to boost the demand for home health services in the 1980-93 period. Home health care use is concentrated in the elderly population. This population cohort increased in size at a faster rate than the overall population, rising from 11 percent of total population in 1980 to 13 percent in 1993. Medicare pays for a high percentage of health care expenditures for this burgeoning population group. During this period, major changes to Medicare stimulated the use of home health services by the elderly. In the early 1980s, the 3-day prior hospitalization requirement and the 100-visit limit were dropped. This period also saw the expansion in the availability of health care technologies deliverable in the home. In the mid-1980s, introduction of the hospital PPS encouraged physicians to discharge hospitalized beneficiaries sooner, and researchers theorized that patients would require more frequent followup care in the home. Higher utilization did not initially materialize due to certain administrative and regulatory changes that occurred during the mid-1980s (Helbing, Sangl, and Silverman, 1993). The most important factor, however, occurred in the late 1980s: The coverage rules that had been the basis for intermediaries' denial of beneficiaries' coverage for home health services were clarified to broaden and more uniformly interpret the “part-time and intermittent” care requirement for coverage (Vladeck and Miller, 1994).
These changes encouraged more uniform spending on behalf of the elderly for home health services across States, although spending for home health services in rural States remained lower than the U.S. average. In the Mideast, where the provision of home health services was already well-established and expenditures per aged person greatly exceeded the U.S. average (Table 6), spending on home health services grew more slowly than the U.S. average—13.4 percent annually. In contrast, spending per aged person in the Southeast was lower than the U.S. average in 1980, but spending grew at an average annual rate of 21.7 percent to boost spending per aged person above the U.S. average by 1993. In predominantly rural regions such as the Rocky Mountains and Plains, however, development of the home health care market proceeded more slowly; spending per aged person remained well below the U.S. average and grew at only average rates throughout the 1980-93 period. Researchers speculate that the concentration of home health users (predominantly the elderly) in rural areas is not dense enough to support financially viable home health providers. Longer travel times to deliver services in rural areas may increase costs above reimbursement levels (Kenney, 1993).
Table 6. Regional Home Health Care and Nursing Home Care Expenditures per Aged Person as a Percent of U.S. Spending per Aged Person: Calendar Years 1980 and 1993.
| Region | Home Health Care | Nursing Home Care |
|---|---|---|
|
| ||
| Percent | ||
| 1980 | ||
| United States | 100 | 100 |
| New England | 124 | 134 |
| Mideast | 190 | 138 |
| Great Lakes | 78 | 103 |
| Plains | 56 | 120 |
| Southeast | 71 | 64 |
| Southwest | 69 | 84 |
| Rocky Mountains | 75 | 103 |
| Far West | 90 | 88 |
| 1993 | ||
| United States | 100 | 100 |
| New England | 121 | 158 |
| Mideast | 129 | 139 |
| Great Lakes | 72 | 112 |
| Plains | 65 | 115 |
| Southeast | 120 | 74 |
| Southwest | 107 | 77 |
| Rocky Mountains | 74 | 83 |
| Far West | 71 | 69 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Together, home health care and nursing home services provide long-term care for patients who need continuing care in less acute care settings (e.g., persons recently discharged from the hospital). Depending on the intensity of care, availability of other home care givers, availability of nursing home beds and home health providers, and social norms of an area, choices are made by the consumer between these two long-term care services. The substitution of home health services for nursing home care by patients can be seen in long-term spending patterns across States and regions. Nationwide in 1993, one-quarter of long-term care services purchased from freestanding home health agencies and freestanding nursing homes5 were for home health services. In the Southeast and Southwest, these data show that patients have a higher preference for care delivered in the home: At least one-third of long-term care was purchased from freestanding home health agencies. In rural Plains States where elderly population density is low, only 16.5 percent of long-term care services are delivered by freestanding home health agencies.
The two largest payers of home health services are Medicare and Medicaid. Together these two programs paid for 39.4 percent of home health services nationwide in 1980, rising to 48.7 percent in 1993. In 1993, funding by these programs ranged from 34.6 percent of services in the Plains (where spending on home health services per elderly person is the lowest in the Nation) to 63.9 percent of home health services in New England (where home health spending per elderly person exceeded the U.S. average).
Over 50 percent of all U.S. Medicaid spending on home health care was spent under New York's Medicaid program in 1993, down from 60 percent in 1980. Approximately three-fourths of New York's $1.6 billion expenditures on home health care in 1993 was delivered as personal-care services.
Drugs and Other Medical Non-Durables
This category represents expenditures for prescription and over-the-counter drugs and sundries. This class of expenditure is limited to spending that occurs in retail outlets such as food stores, drug stores, HMO pharmacies, or through mailorder pharmacies. In 1993, it represented 9.6 percent of PHCE nationwide.
Expenditures for non-durable medical products reached $75.0 billion in 1993. Regional spending per capita for nondurable medical products clustered closely around the U.S. average, ranging from 97 percent of the U.S. per capita in the Southwest to 106 percent in New England. In two regions, the Plains and Rocky Mountains, however, spending per capita on non-durable medical products was 10 or more percent below the U.S. average. Similar expenditure patterns existed in physician services, suggesting that lower utilization of physician services may result in fewer prescriptions being written and filled.
Like per capita spending levels, aggregate spending growth between 1980-93 varied little among regions: New England grew the fastest at 10.6 percent average annual rate while growth in the Plains was the slowest at 9.1 percent average annual rate. Nevada and Florida led the nation in spending growth for non-durable products, with average annual rates of 12.6 percent and 12.1 percent, respectively.
Two-thirds of spending for non-durable medical products went for the purchase of prescription drugs in 1993. The largest amounts spent on prescription drugs occurred in California, New York, Texas, and Florida. States with the fastest average annual prescription drug spending growth for the entire 1980-93 period included Nevada at 15.8 percent, Utah at 14.2 percent, Arizona at 14.7 percent, and Florida at 13.7 percent. Three of these States—Arizona, Nevada, and Florida—experienced some of the fastest growth in total and elderly population in the Nation. Growth in expenditures in these States stemmed, in part, from the large growth in the population 65 years of age or over: In these States, the average annual rate of growth among the elderly population increased from 3.1 to 6.7 percent between 1980-93, compared with 1.9 percent for the Nation. Although the average cost per prescription shows little variation between age categories, the absolute number of prescriptions dispensed was much greater for persons 65 years of age or over, magnifying the effect of large elderly population growth on increases in drug spending.
Vision Products and Other Medical Durables
Expenditures for vision products and other durable medical equipment (DME) cover items such as eyeglasses, hearing aids, surgical appliances and supplies, bulk and cylinder oxygen, and medical equipment rentals. At $12.6 billion in 1993, it is the smallest PHCE category, amounting to 1.6 percent of all spending.
Expenditures for DME in 1993 were largest for the States of California, New York, Texas, and Florida. These States also have a large number of residents over 65 years of age. Florida, ranking fourth in total expenditures, has 2.5 million residents over 65 years of age, representing 18.4 percent of that State's total population. States with low concentrations of those over 65 years of age and small total populations, such as Wyoming and Vermont, contributed the least to total expenditures for DME.
Expenditure growth slowed from 1990-93 for all States, reflecting the overall rate of growth evident in national expenditure estimates. The Southeast experienced the fastest rate of DME expenditure growth of all regions, with rates as high as 11.1 percent in 1990. During the 1980-93 period, however, three out of four States with the highest rate of expenditure growth (Nevada, Hawaii, and Washington) are found in the Far West.
Nursing Home Care
Expenditures for nursing home care are the fourth largest category of spending in SHEA In 1993, spending for nursing home care totaled $66.2 billion, 8.5 percent of all PHCE. These expenditures grew at an average annual rate of 10.7 percent between 1980 and 1993.
Spending for nursing home care covers care provided in freestanding nursing and personal-care facilities. Providers include Medicare- and Medicaid-certified skilled nursing and intermediate care facilities as well as facilities that are not certified. Expenditures for care in facilities that are hospital-based are excluded from this category of spending; such expenditures are captured under hospital care spending.
Average annual growth in regional spending for nursing home care for the 1980-93 period ranged from a high of 12.4 percent in the Southeast region to a low of 9.4 percent in the Plains and the Far West. This trend in the Southeast region is not surprising because the Southeast had faster-than-average growth among the aged population. This population cohort is the most likely to require nursing home care.
Average per capita nursing home expenditures for the 65 years of age or over population were $2,020 in 1993. Regionally, the New England, Mideast, Plains, and Great Lakes regions experienced nursing home care spending per aged person that ranged from 12 to 58 percent higher than the U.S. average. In contrast, spending in the Far West, Southeast, Southwest, and Rocky Mountains ranged from 17 to 31 percent below the U.S. average (Table 6).
Nationwide, nursing home expenditures per aged person increased 8.7 percent annually from 1980 to 1993. Spending in New England, the Southeast, and the Great Lakes, all high-cost regions, grew faster than the United States overall. Spending in the Southwest, Rocky Mountains, and Far West, all low-cost regions, grew slower than the U.S. average. Only the Mideast region grew at about the same rate as the U.S. overall.
Factors that affect regional differences in spending and rates of growth for nursing home care are similar to those for other components of health care spending. The number of people 65 years of age or over, the aged share of the population, health status, and per capita personal income or wealth of the populations influence the demand for nursing home care. Also, traditional societal values may affect the choice of long-term care treatment settings for the disabled elderly, favoring either nursing home care or home health care. Constraints on the supply of nursing home care include nursing home resource costs (Prospective Payment Assessment Commission, 1995) and the availability of beds (Harrington, Swan, and Grant, 1988; Harrington and Estes, 1994). States can control the growth in nursing home bed supply through certificate-of-need programs. By restraining the growth in bed supply, States can constrain their rapidly growing Medicaid spending for nursing home care. Nationwide, Medicaid funded 49.0 percent of nursing home care in 1993; the low Medicare share, at 6.5 percent in 1993, reflected the more stringent requirements for covered services.
Nursing home expenditures in SHEA do not capture all nursing home-type spending. Not only are hospital-based nursing homes excluded, but so are expenditures for nursing care provided in swing beds of acute-care facilities. In addition, long-term care facilities specifically for Alzheimer's patients are out of scope in SHEA because these patients predominantly require custodial rather than medical care.
Other Personal Health Care
Other personal health care (OPHC) expenditures increased from $4.0 billion in 1980 to $18.0 billion in 1993, an annual rate of 12.4 percent OPHC spending amounted to 2.3 percent of PHCE in 1993. Expenditures for OPHC cover spending for publicly and privately funded health care that is not provided through health care establishments and is therefore not captured elsewhere in SHEA OPHC services are provided through non-medical locations such as job sites, schools, military field-stations, or community centers where delivery of medical services is incidental to the function of the site. For the Nation, Medicaid accounted for about 11 percent of OPHC total in 1980, increasing to 45 percent by 1993. The unusually rapid growth in Medicaid OPHC spending stemmed from the introduction and expansion of home and community-based waivers and “other” miscellaneous Medicaid services.
The five States exhibiting the highest average annual growth rates (between 15.9 and 21.2 percent) in OPHC spending were Rhode Island, Oregon, New Hampshire, Maine, and Vermont. These high growths can be traced back to large increases in the OPHC Medicaid expenditures that exhibited increases ranging from 28.9 to 47.3 percent annually. The State with the lowest average annual growth in OPHC expenditures was Ohio, at 8.2 percent.
Medicare
Medicare financed $150.4 billion (19.3 percent) of total U.S. PHCE in 1993. Medicare spending increased at an average annual rate of 11.6 percent from 1980 to 1993.
Medicare primarily funds acute-care (hospital and physician) services for aged and disabled enrollees. In 1993, Medicare funded 29.1 percent of the Nation's expenditures for hospital care and 20.2 percent of total spending for physician services, about 3 percent more than was funded in 1980. From 1980 to 1993, Medicare funding of medical durables increased from 9.4 percent to 29.2 percent, non-hospital nursing home care from 1.7 percent to 6.5 percent, and non-hospital home health care from 26.9 percent to 34.9 percent.
The distribution of Medicare expenditures by type of service differed by region. In 1993, hospital care accounted for $94.2 billion (62.7 percent) of the $150.4 billion spent by Medicare for personal health care in the United States. Four of eight regions had shares higher than the U.S. average for hospital care, ranging from 69.1 percent in the Plains to 65.5 percent in the Mideast (Table 7). Two regions had shares that approximated the U.S. average—New England and the Southwest. The Southeast and Far West exhibited shares lower than the U.S. average. In 1993, the Far West and Plains, more than any other regions, deviated from the national distribution of services. In the Far West, the smallest percent of Medicare expenditures of any region went for hospital care (57.8 percent), while the percent spent on physician services (28.5 percent) was the highest of any region. In the Plains, 69.1 percent of all Medicare spending went for hospital care, offset by lower-than-average percentages spent in all other service sectors. The share of Medicare spending for home health was high in both New England (8.1 percent) and the Southeast (7.9 percent).
Table 7. Number of Medicare Enrollees, Medicare Expenditures for Personal Health Care, and Distribution by Type of Service, by Region: Calendar Year 1993.
| Region | Number of Enrollees1 (Thousands) |
Total Personal Health Care (Millions) |
Type of Service | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Hospital Care | Physician Services | Other Professional Services | Home Health Care | Medical Durables | Nursing Home Care | |||
|
| ||||||||
| Percent | ||||||||
| United States | 35,557 | $150,374 | 62.7 | 23.0 | 3.7 | 5.3 | 2.5 | 2.9 |
| New England | 1,988 | 8,829 | 63.0 | 19.2 | 4.1 | 8.1 | 1.4 | 4.2 |
| Mideast | 6,520 | 30,438 | 65.5 | 22.9 | 3.5 | 3.1 | 2.8 | 2.2 |
| Great Lakes | 6,071 | 23,508 | 65.7 | 21.1 | 3.4 | 4.2 | 2.4 | 3.2 |
| Plains | 2,738 | 9,861 | 69.1 | 20.8 | 3.1 | 2.7 | 2.2 | 2.2 |
| Southeast | 9,150 | 38,805 | 59.5 | 23.0 | 4.1 | 7.9 | 3.0 | 2.6 |
| Southwest | 3,211 | 13,271 | 62.7 | 21.8 | 4.1 | 7.2 | 2.3 | 2.0 |
| Rocky Mountains | 898 | 3,104 | 65.8 | 19.8 | 2.7 | 5.0 | 2.8 | 4.0 |
| Far West | 4,955 | 22,558 | 57.8 | 28.5 | 3.7 | 4.2 | 1.7 | 4.1 |
Number of aged and disabled persons enrolled in the Hospital and/or Supplementary Medical Insurance Programs as of July 1,1993, by area of residence. U.S. total includes enrollees with unknown State of residence.
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
By State, the share of total Medicare expenditures attributable to hospital care ranged from 75.4 percent in Alaska to 51.6 percent in Florida. Physician services accounted for 31.4 percent in Hawaii and 16.6 percent in Alaska. Tennessee had the highest share attributable to home health care but almost the lowest shares for hospital care and physician services.
States that were the most costly to the Medicare program were primarily States where the largest number of Medicare enrollees reside. The age and gender composition and health and disability status of this population contributed to regional variation in aggregate and per enrollee expenditures by affecting the volume and intensity of services used (Helbing, Sangl, and Silverman, 1992). However, many other factors contributed to regional differences, such as provider practice patterns, population density, managed-care penetration, and provider resource costs (Prospective Payment Assessment Commission, 1995). Regional variation in provider resource costs are affected in part by differences in area wages and other costs of operating a business (input prices), State dictated specialized training requirements, and regulations designed by States to control the growth in public program medical care spending. The population density of rural contrasted with urban areas may affect the number of providers willing to serve an area.
Per enrollee Medicare PHCE for the United States grew 9.5 percent annually from $1,300 in 1980 to $4,229 in 1993. Regionally, growth in PHCE per enrollee ranged from 10.7 percent in the Southeast to 8.4 percent in the Great Lakes and Plains. Spending levels by region ranged from 10.4 percent above the U.S. average in the Mideast ($4,668 per enrollee) to 18.3 percent below the U.S. average in the Rocky Mountains ($3,456 per enrollee).
Medicaid
Medicaid expenditures amounted to $112.8 billion in 1993, accounting for 14.5 percent of PHCE. Annual growth from 1980-93 averaged 12.5 percent. However, from 1989 to 1992, the growth rates in total Medicaid expenditures exceeded this 13-year average. The largest growth rates (21.3 percent and 25.5 percent) occurred in 1990 and 1991, as a result of the disproportionate share hospital (DSH) program (see Levit et al., 1994 for further information). The annual rate of growth in total Medicaid expenditures decelerated in 1992 and 1993, primarily due to the deceleration in Medicaid hospital expenditures resulting from DSH program caps. Nationally, the Medicaid expenditure growth rate slowed to 8.7 percent in 1993.
The Federal Government defines minimum services that must be provided to all or specified groups of Medicaid recipients in order for States to receive Federal matching funds. States can also receive Federal assistance for funding if they elect to provide other optional services. The minimum services that must be provided are: inpatient and outpatient hospital services; physician care; rural health clinic services; laboratory and X-ray services; nurse practitioners' and nurse-midwife services; nursing home and home health care; early and periodic screening, diagnosis, and treatment; family planning services and supplies; and services of selected other health professionals. As of October 1994, there were 34 different optional services that States could choose to provide. Examples of these optional services include: podiatrists' services; optometrists' services; chiropractors' services; clinic services; physical therapy services; prosthetic devices; prescribed drugs; transportation services; hospice care services; respiratory care services; and tuberculosis-related services. There is considerable variation among States as to the types of optional services provided. The States offering the most optional services were Wisconsin (31), and Illinois, Indiana, and Minnesota (30). Louisiana and Delaware offered only 15 of the 34 optional services. All States offered prescription drug services, and most States offered transportation services and prosthetic devices; however, relatively few States offered respiratory care services and tuberculosis-related services.
The largest shares of total Medicaid expenditures in 1993 were in New York, California, Texas, Pennsylvania, and Florida, together totaling 40 percent of Medicaid spending nationwide. From a regional perspective, two regions, the Mideast and the Southeast, accounted for 47.7 percent of total Medicaid expenditures in 1993. The share of Medicaid spending in the Mideast region declined from 29.1 percent to 26.5 percent from 1980 to 1993, while the share of spending in the Southeast grew from 16.1 percent in 1980 to 21.2 percent in 1993. The remaining regions maintained relatively constant shares of spending during the last 13 years.
The highest Medicaid spending occurred in New York, with expenditures 91 percent higher per recipient than the U.S. average. California maintained very low costs per recipient—32 percent below the U.S. average. Only Mississippi had relative spending per recipient lower than California (Table 8).
Table 8. Medicaid Recipients, Medicaid Cost-per-Recipient Index, and Medicaid Recipients-per-Population Index, by Region and State: 1993.
| Region and State | Medicaid Recipients1 (Thousands) |
Cost-per-Recipient Index2 | Recipients-per-Population Index3 |
|---|---|---|---|
| United States | 32,664 | 1.00 | 1.00 |
| New England | 1,618 | 1.41 | 0.97 |
| Connecticut | 334 | 1.73 | 0.80 |
| Maine | 169 | 1.24 | 1.07 |
| Massachusetts | 765 | 1.40 | 1.00 |
| New Hampshire | 79 | 1.63 | 0.56 |
| Rhode Island | 191 | 1.20 | 1.51 |
| Vermont | 81 | 0.83 | 1.10 |
| Mideast | 5,393 | 1.60 | 0.96 |
| Delaware | 69 | 1.05 | 0.78 |
| District of Columbia | 120 | 1.63 | 1.64 |
| Maryland | 445 | 1.25 | 0.71 |
| New Jersey | 794 | 1.41 | 0.80 |
| New York | 2,742 | 1.91 | 1.19 |
| Pennsylvania | 1,223 | 1.21 | 0.80 |
| Great Lakes | 5,094 | 1.03 | 0.94 |
| Illinois | 1,396 | 0.96 | 0.94 |
| Indiana | 565 | 1.42 | 0.78 |
| Michigan | 1,172 | 0.96 | 0.98 |
| Ohio | 1,491 | 0.91 | 1.06 |
| Wisconsin | 471 | 1.31 | 0.74 |
| Plains | 1,863 | 1.04 | 0.81 |
| Iowa | 289 | 0.96 | 0.81 |
| Kansas | 243 | 0.92 | 0.76 |
| Minnesota | 425 | 1.52 | 0.74 |
| Missouri | 609 | 0.78 | 0.92 |
| Nebraska | 165 | 0.99 | 0.81 |
| North Dakota | 62 | 1.25 | 0.77 |
| South Dakota | 70 | 1.10 | 0.77 |
| Southeast | 8,635 | 0.80 | 1.10 |
| Alabama | 522 | 0.71 | 0.98 |
| Arkansas | 339 | 0.86 | 1.10 |
| Florida | 1,745 | 0.78 | 1.00 |
| Georgia | 955 | 0.83 | 1.09 |
| Kentucky | 618 | 0.79 | 1.29 |
| Louisiana | 751 | 1.03 | 1.38 |
| Mississippi | 504 | 0.60 | 1.51 |
| North Carolina | 898 | 0.83 | 1.02 |
| South Carolina | 470 | 0.82 | 1.02 |
| Tennessee | 909 | 0.70 | 1.41 |
| Virginia | 576 | 0.82 | 0.70 |
| West Virginia | 347 | 0.90 | 1.51 |
| Southwest | 3,340 | 0.76 | 0.98 |
| Arizona | 404 | 0.91 | 0.81 |
| New Mexico | 241 | 0.69 | 1.18 |
| Oklahoma | 387 | 0.76 | 0.94 |
| Texas | 2,308 | 0.74 | 1.01 |
| Rocky Mountains | 664 | 0.96 | 0.67 |
| Colorado | 281 | 1.00 | 0.62 |
| Idaho | 100 | 0.84 | 0.71 |
| Montana | 89 | 1.05 | 0.84 |
| Utah | 148 | 0.93 | 0.63 |
| Wyoming | 46 | 0.86 | 0.78 |
| Far West | 6,056 | 0.74 | 1.12 |
| Alaska | 65 | 1.22 | 0.86 |
| California | 4,834 | 0.68 | 1.22 |
| Hawaii | 110 | 0.93 | 0.74 |
| Nevada | 88 | 1.13 | 0.50 |
| Oregon | 325 | 0.85 | 0.85 |
| Washington | 633 | 0.99 | 0.95 |
Data reported on HCFA Form-2082 for fiscal year 1993.
Calendar year State health expenditures divided by fiscal year recipient counts.
Fiscal year recipient counts divided by calendar year population counts.
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
The five States exhibiting the highest annual growth rate for total Medicaid expenditures in 1993 were Alaska, Colorado, Georgia, Hawaii, and Oregon. All five States showed growth rates greater than the U.S. recipient growth rate, although none showed unusually high growth in recipients in fiscal year 1993. Four States experienced declines in Medicaid expenditures in 1993: New Hampshire, Missouri, Massachusetts, and Pennsylvania. In Pennsylvania, the decrease in numbers of Medicaid recipients accounted for the slight decrease in expenditures. In New Hampshire, limits on Medicaid DSH payments largely contributed to the decrease in spending: DSH payments accounted for 33 percent of total Medicaid payments in 1991, nearly 60 percent in 1992, and only 8.8 percent in 1993 (Table 9).
Table 9. State Medicaid Payments to Disproportionate Share Hospitals (DSH) as a Share of Total State Medicaid Expenditures and as a Share of Total Medicaid DSH Payments, by Region and State: Calandar Years 1992-93.
| Region and State | 1992 | 1993 | |||
|---|---|---|---|---|---|
|
|
|
||||
| State DSH as a Share of State Medicaid Spending | State DSH as a Share of U.S. DSH | State DSH as a Share of State Medicaid Spending | State DSH as a Share of U.S. DSH | ||
|
| |||||
| Percent | |||||
| United States | 16.6 | 100.0 | 15.4 | 100.0 | |
| New England | 19.1 | 8.9 | 16.2 | 7.3 | |
| Connecticut | 22.2 | 2.4 | 21.5 | 2.5 | |
| Maine | 21.0 | 0.8 | 24.7 | 1.0 | |
| Massachusetts | 12.3 | 2.8 | 13.8 | 2.9 | |
| New Hampshire | 59.9 | 2.3 | 8.8 | 0.2 | |
| Rhode island | 11.2 | 0.5 | 12.9 | 0.6 | |
| Vermont | 10.3 | 0.1 | 8.4 | 0.1 | |
| Mideast | 18.1 | 29.3 | 16.7 | 28.6 | |
| Delaware | 2.2 | 0.0 | 2.2 | 0.0 | |
| District of Columbia | 5.6 | 0.2 | 7.1 | 0.3 | |
| Maryland | 6.3 | 0.7 | 4.2 | 0.5 | |
| New Jersey | 31.1 | 6.4 | 29.6 | 6.6 | |
| New York | 17.0 | 16.3 | 15.9 | 16.4 | |
| Pennsylvania | 19.0 | 5.7 | 16.6 | 4.9 | |
| Great Lakes | 9.3 | 9.0 | 7.4 | 7.7 | |
| Illinois | 7.5 | 1.8 | 5.5 | 1.4 | |
| Indiana | 8.9 | 1.2 | 1.3 | 0.2 | |
| Michigan | 15.6 | 3.2 | 14.8 | 3.3 | |
| Ohio | 10.0 | 2.6 | 10.1 | 2.7 | |
| Wisconsin | 0.4 | 0.1 | 0.4 | 0.0 | |
| Plains | 15.5 | 5.7 | 14.5 | 5.6 | |
| Iowa | 0.5 | 0.0 | 0.4 | 0.0 | |
| Kansas | 28.0 | 1.1 | 25.2 | 1.1 | |
| Minnesota | 2.2 | 0.2 | 1.5 | 0.2 | |
| Missouri | 41.3 | 4.3 | 44.8 | 4.2 | |
| Nebraska | 0.6 | 0.0 | 0.6 | 0.0 | |
| North Dakota | 0.0 | 0.0 | 0.0 | 0.0 | |
| South Dakota | 0.0 | 0.0 | 0.0 | 0.0 | |
| Southeast | 17.1 | 21.3 | 16.2 | 22.3 | |
| Alabama | 35.1 | 2.4 | 34.5 | 2.5 | |
| Arkansas | 0.3 | 0.0 | 0.3 | 0.0 | |
| Florida | 4.8 | 1.1 | 5.4 | 1.4 | |
| Georgia | 13.3 | 1.8 | 11.8 | 1.9 | |
| Kentucky | 16.4 | 1.5 | 8.5 | 0.8 | |
| Louisiana | 38.3 | 5.2 | 38.7 | 5.9 | |
| Mississippi | 15.5 | 0.9 | 15.3 | 0.9 | |
| North Carolina | 14.6 | 1.9 | 14.1 | 2.1 | |
| South Carolina | 35.6 | 2.6 | 34.9 | 2.7 | |
| Tennessee | 20.4 | 2.5 | 20.7 | 2.6 | |
| Virginia | 10.1 | 0.9 | 8.5 | 0.8 | |
| West Virginia | 9.1 | 0.5 | 10.3 | 0.6 | |
| Southwest | 19.6 | 9.1 | 19.6 | 9.9 | |
| Arizona | 0.0 | 0.0 | 7.5 | 0.5 | |
| New Mexico | 2.4 | 0.1 | 1.6 | 0.1 | |
| Oklahoma | 2.2 | 0.1 | 2.4 | 0.1 | |
| Texas | 28.9 | 8.9 | 26.9 | 9.1 | |
| Rocky Mountains | 16.4 | 1.8 | 6.5 | 0.8 | |
| Colorado | 38.4 | 1.8 | 14.2 | 0.8 | |
| Idaho | 0.4 | 0.0 | 0.4 | 0.0 | |
| Montana | 0.0 | 0.0 | 0.2 | 0.0 | |
| Utah | 1.1 | 0.0 | 1.0 | 0.0 | |
| Wyoming | 0.1 | 0.0 | 0.1 | 0.0 | |
| Far West | 19.2 | 14.9 | 20.1 | 17.8 | |
| Alaska | 3.6 | 0.0 | 5.4 | 0.1 | |
| California | 22.5 | 12.8 | 23.6 | 15.3 | |
| Hawaii | 13.7 | 0.2 | 13.0 | 0.3 | |
| Nevada | 22.6 | 0.4 | 24.5 | 0.5 | |
| Oregon | 2.1 | 0.1 | 2.3 | 0.1 | |
| Washington | 11.6 | 1.3 | 12.5 | 1.5 | |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
In 1993, 40.9 percent of all Medicaid expenditures in the U.S. were attributable to hospital care, 28.8 percent to nursing home care, 11.1 percent to physician care, 7.2 percent to other personal care, 6.8 percent to drugs, 2.8 percent to freestanding home health care, 1.4 percent to dental care, and 1.2 percent to other professional care. Institutional care in hospitals and nursing homes accounted for nearly 70 percent of Medicaid spending in 1993, while long-term care (nursing home and home health care) accounted for approximately 32 percent of all Medicaid spending. Medicaid hospital care expenditures as a percentage of total Medicaid expenditures in the Far West and the Southwest were above the national share (49.2 percent and 46.1 percent, respectively), while New England showed the lowest share, at 30.9 percent Nursing home care expenditures varied from a high of 39.8 percent of total Medicaid expenditures in New England to a low of 15.9 percent in the Far West; the share of Medicaid spending on physician care was 16 percent in the Southeast but only 7 percent in the Mideast and New England.
In the current State health care reform climate, the Medicaid program is poised to face significant change. Already, increased emphasis on Medicaid managed care has resulted in enrolling nearly one-quarter of all Medicaid recipients in some type of managed-care program and has led to the approval and implementation of statewide 1115 waivers as a part of a larger health care reform effort (Lewin-VHI, Inc., 1995). Section 1115 waivers allow the Secretary of the Department of Health and Human Services to waive Federal Medicaid requirements in the Social Security Act and authorize experimental, pilot, or demonstration projects (such as enrolling recipients in managed-care plans). Prior to 1993, section 1115 waivers principally involved limited research projects. In 1993, however, the Secretary authorized expansion of statewide 1115 waivers, opening the way for approval of statewide demonstrations in Florida, Hawaii, Kentucky, Oregon, Rhode Island, South Carolina, Tennessee, and Ohio. (Arizona has had an approved 1115 waiver for over a decade.) Also, several States have submitted 1115 waiver applications for smaller programs which target specific populations (Lewin-VHI, Inc., 1995). Much of the emphasis of these current statewide 1115 programs is on delivery of health care benefits through lower-cost capitated managed-care plans that would permit expansion of the Medicaid program to more poor people. Additionally, the prospect of block grants will give States more flexibility in program eligibility and covered services. The effect of these programs and proposals on State Medicaid expenditures is yet to be fully realized.
Population
One factor that affected the level and growth in spending across most health care sectors was population. In 1993, California was by far the most populous State, with an estimated 31.2 million residents (Table 3). New York, Texas, and Florida ranked second through fourth, respectively, in population size. Together, these four States accounted for 31 percent of the 257.8 million persons residing in the United States.
Growth in health spending is directly related to population growth. Between 1980 and 1993, the resident population grew at an average annual rate of 1.0 percent nationwide. The fastest growth occurred in Nevada, where population swelled at a 4.2-percent average annual rate. Growth in Alaska, Arizona, and Florida, up 3.0,2.8, and 2.6 percent, respectively, followed close behind. These States also experienced some of the most rapid growths in elderly population. Since die elderly use more health services than other age groups, those States where the elderly population grew more rapidly than the United States experienced more rapidly growing spending, all other factors being equal. Nationwide, the elderly population averaged 1.9 percent growth during this period. In States with high total population growth, the elderly population also grew at a faster average annual rate than the U.S. average rate: 6.7 percent in Nevada, 6.5 percent in Alaska, 4.2 percent in Arizona, and 3.1 percent in Florida. Several areas lost population between 1980 and 1993: the District of Columbia, West Virginia, North Dakota, Iowa, and Wyoming.
The level of health spending is also related to the distribution of the aged population in a State. The 32.8 million persons 65 years of age or over in the United States accounted for 12.7 percent of the population in 1993, up from 11.3 percent in 1980. The elderly share of population was highest in Florida (18.4 percent). Pennsylvania, Rhode Island, Iowa, and West Virginia also showed elderly shares of population greater than 15 percent. At the opposite extreme, the elderly population shares in Alaska and Utah each were less than 9 percent in 1993. All other factors being equal, the level of health spending per person will be higher in States where the elderly comprise a larger share of the total population.
Sources and Methods
The structure of SHEA parallels that of the NHE accounts. SHEA uses the same definitions and, to the extent possible, the same data sources as NHE (Lazenby et al., 1992). This structure clusters health services according to the establishment providing those services; for products, this structure groups retail purchases of medical products according to product classification. For purposes of health expenditure accounting, this establishment-based structure has both strengths and weaknesses. Strength comes from the wealth of uniform State-level information collected by the Federal Government and private organizations on an establishment basis. These data also permit uniformity in concepts, collection methods, and data processing, which allows us to make valid interstate comparisons.
Establishment-based structure eases the collection of data by reducing requirements for providers to disaggregate their revenue according to the specific service provided. The Federal Government has created an establishment-based structure for data collection codified in the Standard Industrial Classification (SIC) Manual (Executive Office of the President, 1987). These SICs form the basis for the service categories used in SHEA (Table 10).
Table 10. Classification of Establishments by Standard Industrial Classification, 1987.
| Industry Group Number | Industry |
|---|---|
| 801 | Offices and Clinics of Doctors of Medicine |
| 802 | Offices and Clinics of Dentists |
| 803 | Offices and Clinics of Doctors of Osteopathy |
| 804 | Offices and Clinics of Other Health Practitioners |
| 805 | Nursing and Personal Care Facilities |
| 806 | Hospitals |
| 807 | Medical and Dental Laboratories |
| 808 | Home Health Agencies |
| 809 | Miscellaneous Health and Allied Services, Not Elsewhere Classified |
SOURCE: (Executive Office of the President, 1987).
This structure may not meet all the analytical needs of researchers and policymakers because it does not measure spending for narrowly-defined “services,” but for establishment services overall. For example, hospital establishments provide hospital care, but may also provide nursing home care in long-term units and serve as a home health care agency; hospitals also furnish prescription drugs to patients and employ physicians who provide services to patients. We include all revenues received from these billed services and products in hospital expenditures, rather than with other similar services.
Establishment-based expenditures mean that spending is in the State of the provider rather than in the State of residence of the beneficiary of services. People are able to cross borders to receive health care services. Therefore, the population of a State is not necessarily an accurate reflection of persons using the services of providers in that State. Therefore, we do not generally compute per capita health spending using State-of-provider expenditure data. In some services and for regions where net border crossing is small, per capita expenditures are presented.
The next phase of SHEA will estimate border crossing for health care services, adjusting State-of-provider expenditures to a location of beneficiary residence. We will produce per capita expenditures at this point, and interstate comparisons of spending will be made.
Revisions
U.S. expenditure totals presented in the tables in this article will differ occasionally from NHE totals (Levit et al, 1994). First, spending in U.S. territories and by the Department of Defense at foreign military bases are included in the NHE but excluded from the U.S. totals reported in SHEA. Second, U.S. expenditure totals for nursing homes are lower than those published in NHE. In this article, we have removed expenditures for hospital-based nursing home services from nursing home expenditures. This methodological change will be incorporated into the next NHE report. It was necessary to include this revision because hospital-based nursing home spending is greater in some States than others. This would result not only in overstating spending on freestanding nursing home care and PHCE, but in distorting the distribution of this spending across States. Third, home health expenditures are higher than the published NHE. This revision, also methodological in nature, counts revenues received by government agencies in the delivery of health services in the home. As with the nursing home revision, this change will be incorporated into the next NHE report.
We have also made revisions to previously published State expenditures for hospital care, physician services, and prescription drugs (Levit et al., 1993). For hospitals, this estimate remained the same methodologically, but small revisions to spending by State resulted from the receipt of new data. Second, spending by State for physician services was revised to incorporate new levels from the recently released 1992 Census of Service Industries (CSI) (U.S. Bureau of the Census, 1977, 1982, 1987, 1992). Third, a revision was made to prescription drugs to incorporate an age-gender factor into the extrapolation methodology. This minor revision affected 1988-93 expenditure estimates.
Hospital Care
Hospital care expenditure estimates (SIC 805) reflect spending for all hospital services provided to patients for which the hospital bills. Expenditures include revenues received for room and board charges, ancillary charges such as operating room fees, charges for the services of resident physicians, inpatient pharmacy charges, charges for hospital-based nursing home care and care delivered by hospital-based home health agencies, and fees for any other services billed by the hospital. We exclude expenditures for services of physicians who bill independently for services delivered to patients in hospitals.
Non-Federal hospital estimates are measured using American Hospital Association (AHA) Annual Survey data that capture information from registered and non-registered hospitals in the United States. To meet the definitions of SHEA, we modify AHA data in four ways. First, data from each year's survey is combined to create a longitudinal file containing one multiple-year record for each hospital; hospital characteristics contained on this record are edited for consistency. Second, hospital revenues are imputed from expense data using revenue-to-expense ratios provided by AHA Third, individual hospitals' imputed accounting year revenues are converted to a calendar year basis. Finally, when complete calendar year data is not available for a facility through calendar year 1993, the latest available data is extrapolated using patterns of acceleration and deceleration observed in AHA Panel Survey data. Federal hospital estimates are based on data from either the Federal agencies that administer those facilities or AHA.
Physician Services
We estimate expenditures for physician services (SICs 801 and 803) in three pieces: expenditures in private physician offices and clinics; fees of independently-billing laboratories; and professional fees received by physicians from hospitals. Expenditures in private physician offices and clinics are based on business receipts from taxable establishments and revenues from tax-exempt establishments reported in the CSI (U.S. Bureau of the Census, 1977, 1982, 1987, 1992). We use receipt and revenue distributions for these years to estimate spending by State. For taxable establishments, we estimate intervening years using business receipts for sole proprietorships, partnerships, and corporations from the Internal Revenue Services' Business Master File (BMF) (U.S. Internal Revenue Service, 1977-92). Growth in wages and salaries for physicians' offices and clinics (U.S. Bureau of Labor Statistics, 1994) is used to estimate 1993. For tax-exempt physician offices and clinics, estimates for census years are interpolated and extrapolated using civilian population (U.S. Bureau of the Census, 1994). Expenditures in tax-exempt and taxable establishments are separately scaled to national totals.
The distribution of laboratory fees parallels the distribution of physician expenditures. We distribute the U.S. total for laboratory fees to States using total physician expenditures.
We reduce expenditures for State physician services by the amount of professional fees paid by hospitals to physicians. Professional fees are distributed to States based on professional fee expenses from the AHA Annual Survey for 1980,1985, and 1990-93. Expenditures by State for intervening years are estimated by interpolating AHA-based estimates using community hospital revenues by State. We scale the results to U.S. totals.
We have introduced one major revision to State expenditures for physician services since our previous publication (Levit et al., 1993). Since that time, the 1992 CSI has become available. This information is linked to the 1987 CSI, producing revisions to estimates for 1988 and later years.
Dental Services
Expenditures for dental services (SIC 802) are estimated using CSI and BMF data in the same manner as taxable establishments for physician offices and clinics. To estimate 1993 spending, we extrapolate the 1992 CSI-based estimates using growth in wages and salaries in dental offices and clinics (U.S. Bureau of Labor Statistics, 1994).
Other Professional Services
Spending for other professional services (SICs 804 and 809) is estimated in three segments. The first segment, expenditures for the services of licensed professionals such as chiropractors, optometrists, podiatrists, and independently practicing nurses, is estimated using CSI and BMF data in the same manner as taxable establishments for physician offices and clinics. For the second segment, we distribute expenditures in specialty clinics and for miscellaneous professional services to States using data from the CSI for 1977, 1982, 1987, and 1992. CSI-based expenditures for each State are interpolated and extrapolated for intervening years using civilian population. The final piece, spending for Medicare ambulance services, is estimated using the distribution of expenditures for Medicare other professional services. We control State spending for each segment to national totals.
Home Health Care
Like the estimates for professional services, expenditure estimates for freestanding home health care (SIC 808) are based on revenue estimates for taxable businesses and receipt information for tax-exempt businesses collected every 5 years by the CSI. Because the standard industrial classification for home health agencies (SIC 808) was first created with the release of the 1987 Standard Industrial Classification Manual (Executive Office of the President, 1987), collection of separate State data for estimating spending for this service category is available for 1987 and 1992 only. Data from these two surveys are benchmarks for private spending on freestanding home health services by State. We develop separate estimates of spending for government-supplied home health services (not surveyed by the CSI) for 1987 and 1992 using the relationship between Medicare reimbursements to home health agencies for government-owned agencies and all agencies for 1988 and 1992. We sum expenditures for services from government and private home health agencies. The 1987 and 1992 estimates are interpolated and extrapolated for 1980 through 1991 using expenditures for home health services paid by Medicare and Medicaid. For 1993, we extrapolate 1992 CSI-based spending using the growth in private and government wages and salaries paid by home health care establishments (U.S. Bureau of Labor Statistics, 1994). Distributions are controlled to national estimates of freestanding home health expenditures.
Drugs and Other Medical Non-Durables
Prescription and non-prescription drug and sundry expenditure estimates are based on retail sales data reported in the 1977, 1982, and 1987 Census of Retail Trade, Merchandise Line Sales (U.S. Bureau of the Census, 1977, 1982, 1987). Intervening years are interpolated using population data. Estimates for 1988 and after are extrapolated using adjusted State population data. These adjustments measure the variation in drug use and costs due to the age-gender composition of the population within each State. These adjustments are constructed from prescription drug expenditure and use information collected in the 1987 National Medical Expenditure Survey (NMES) (Agency for Health Care Policy and Research, 1987). NMES data show that the average cost per prescription is much greater for males than females in most age categories, and that the number of prescriptions dispensed is much greater for females than males of every age. The data also show an increase in the number of prescriptions dispensed as age increases.
Revisions to previously published prescription drug expenditure estimates by State result from the increase in expenditure levels shown in recently-released national health expenditure estimates (Levit et al., 1994). At that time, we introduced preliminary results from a HCFA-sponsored study conducted by Actuarial Research Corporation (1994). The revised methodology increased spending from 1983 forward. California and Florida, the two States most heavily affected by the revision, showed increases of $0.9 billion and $0.5 billion, respectively. We attribute a small portion of revision for 1988 and later years, however, to the use of an age-gender adjusted population used in deriving our expenditure estimates. Previously, we assumed that State prescription drug costs per capita grew at similar rates, regardless of that States' age and gender composition.
Vision Products and Other Medical Durables
State expenditure estimates for durable medical goods are derived by scaling the distribution of optical goods sales by State to our national expenditure estimates. To measure optical goods sales for retail establishments, State data from the Census of Retail Trade are used for 1977,1982 and 1987. Business receipts for offices of optometrists reported in the 1977, 1982, 1987, and 1992 CSI are used to distribute optical sales that occur in those types of establishments. According to data from the 1992 CSI, these sales represent 23 percent of all retail sales of optical goods nationwide. We rely upon population statistics to extrapolate and interpolate estimates of optical sales for years when actual retail sales are not available.
Nursing Home Care
Expenditures for nursing home care cover services delivered in nursing and personal-care facilities (SIC 805). Estimates are given for four facility types: private nursing homes; State and local nursing homes; nursing homes operated by the Department of Veterans Affairs (DVA); and intermediate care facilities for the mentally retarded (ICFs/MR).
To estimate spending in private facilities, revenues for taxable businesses and receipts for tax-exempt businesses collected by State in the CSI in 1977, 1982, 1987, and 1992 are used. We interpolate and extrapolate revenues and receipts by State using wages and salaries paid in private nursing home establishments (U.S. Bureau of Labor Statistics, 1994). To estimate expenditures in government nursing homes, we inflate wages and salaries for State and local government nursing facilities to revenues. We estimate spending for nursing home care in DVA facilities from State-specific data furnished by the Department. Medicaid expenditures for nursing home care in ICFs/MR from data reported by Medicaid State agencies on HCFA Form-64 are used to estimate spending for this facility type.
We have revised national expenditure estimates for nursing home care since the latest publication of NHE (Levit et al., 1994). This revision eliminates expenditures for nursing home care provided in long-term care units of hospitals from nursing home spending, removing duplication in expenditures between the hospital and nursing home components of NHE.
Other Personal Health Care
Privately funded OPHC consists of industrial inplant services provided by employers for the health care needs of their employees. These services may be provided either onsite or offsite. We estimate expenditures for industrial inplant services using the number of occupational health nurses (American Nurses' Association, 1979; U.S. Public Health Service, 1986, 1994) and average annual wages in the health services sector (U.S. Bureau of Economic Analysis, 1969-93).
Public expenditures include Medicaid and States' general medical assistance spending for health screening services, certain home and community-based waivers, case management, and transportation services. Expenses for shipboard facilities and field stations operated by the Department of Defense and expenditures for certain services funded through State and local maternal and child health programs, school health programs, and Federal agency programs targeting veterans, military personnel, Native Americans, and persons with drug- and alcohol-dependency and mental health-related problems are also covered in this category. We use agency-supplied data to estimate government spending for each OPHC program.
Medicare
We estimate 1991 Medicare spending by State of provider from payments recorded in Medicare's National Claims History (NCH) files. These detailed claim records permit us to assemble expenditures for each SHEA service category. Because of the detail available, 1991 Medicare expenditures can be estimated more precisely than any other year. Payments for each type of service from 1980-90 and from 1992-93 were extrapolated using unpublished tabulations of Medicare reimbursements by program service category and State. When State-of-provider data was unavailable, extrapolations were performed using State-of-beneficiary reimbursement information. We adjusted distributions for each year to equal NHE expenditure estimates.
Medicare payments for services provided to enrollees in Medicare managed-care plans are separately estimated. We allocate national totals by type of service to States based on payments to managed-care organizations by State of beneficiary residence.
Medicaid
Medicaid estimates are based on financial information reports (HCFA Form-64) filed by State Medicaid agencies. These reports show total and service-specific program expenditures. However, we adjusted reported program data to fit the estimates into the framework of SHEA.
The first adjustment splits home health spending into expenditures flowing to hospital-based and freestanding home health care establishments based on ratios supplied from Medicare program data. We add estimates of hospital-based home health care spending to Medicaid hospital care expenditures and subtract it from Medicaid home health care expenditures. A similar adjustment is made for nursing homes. The second adjustment counts that portion of reported program expenditure for ICFs/MR estimated to cover services in hospital-based facilities as hospital care rather than nursing home care.
Additionally, for the purposes of SHEA, we exclude certain Medicaid disproportionate share payments to hospitals that are offset by donations and taxes paid by the same facilities because these payments net out and do not contribute to overall hospital operation (Levit et al, 1994).
Table 12. Hospital Care Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 101,510 | 166,545 | 254,239 | 303,461 | 323,919 | 9.4 |
| New England | 6,467 | 10,332 | 15,540 | 17,855 | 19,056 | 8.7 |
| Connecticut | 1,396 | 2,328 | 3,664 | 4,193 | 4,380 | 9.2 |
| Maine | 460 | 735 | 1,119 | 1,280 | 1,376 | 8.8 |
| Massachusetts | 3,646 | 5,628 | 8,159 | 9,380 | 10,034 | 8.1 |
| New Hampshire | 313 | 590 | 1,056 | 1,233 | 1,388 | 12.2 |
| Rhode Island | 481 | 760 | 1,095 | 1,237 | 1,314 | 8.1 |
| Vermont | 174 | 290 | 447 | 532 | 562 | 9.5 |
| Mideast | 21,568 | 34,346 | 52,968 | 62,586 | 67,330 | 9.2 |
| Delaware | 259 | 434 | 709 | 854 | 937 | 10.4 |
| District of Columbia | 913 | 1,469 | 2,133 | 2,437 | 2,612 | 8.4 |
| Maryland | 2,034 | 2,980 | 4,655 | 5,516 | 5,926 | 8.6 |
| New Jersey | 2,763 | 4,751 | 7,857 | 9,406 | 10,312 | 10.7 |
| New York | 9,582 | 14,585 | 22,739 | 26,387 | 28,001 | 8.6 |
| Pennsylvania | 6,017 | 10,126 | 14,876 | 17,987 | 19,540 | 9.5 |
| Great Lakes | 19,590 | 30,093 | 42,984 | 50,835 | 54,172 | 8.2 |
| Illinois | 6,217 | 8,998 | 12,400 | 14,744 | 15,621 | 7.4 |
| Indiana | 2,125 | 3,399 | 5,288 | 6,473 | 6,998 | 9.7 |
| Michigan | 4,482 | 6,882 | 9,500 | 11,008 | 11,711 | 7.7 |
| Ohio | 4,808 | 8,026 | 11,419 | 13,394 | 14,305 | 8.8 |
| Wisconsin | 1,959 | 2,788 | 4,377 | 5,216 | 5,537 | 8.4 |
| Plains | 7,810 | 12,261 | 18,012 | 21,116 | 22,252 | 8.4 |
| Iowa | 1,179 | 1,733 | 2,634 | 2,996 | 3,111 | 7.8 |
| Kansas | 1,090 | 1,607 | 2,300 | 2,771 | 2,868 | 7.8 |
| Minnesota | 1,740 | 2,716 | 4,094 | 4,674 | 4,796 | 8.2 |
| Missouri | 2,532 | 4,172 | 5,986 | 7,077 | 7,652 | 8.9 |
| Nebraska | 681 | 1,060 | 1,587 | 1,881 | 2,003 | 8.8 |
| North Dakota | 313 | 524 | 717 | 853 | 903 | 8.5 |
| South Dakota | 275 | 450 | 694 | 863 | 920 | 9.8 |
| Southeast | 20,585 | 36,181 | 58,466 | 71,001 | 75,835 | 10.6 |
| Alabama | 1,590 | 2,606 | 4,015 | 5,028 | 5,301 | 9.8 |
| Arkansas | 746 | 1,313 | 2,109 | 2,546 | 2,723 | 10.6 |
| Florida | 4,385 | 8,404 | 13,462 | 15,992 | 17,131 | 11.1 |
| Georgia | 2,148 | 3,885 | 6,685 | 8,092 | 8,704 | 11.4 |
| Kentucky | 1,230 | 2,157 | 3,437 | 4,268 | 4,515 | 10.6 |
| Louisiana | 1,744 | 3,155 | 4,627 | 5,575 | 5,956 | 10.0 |
| Mississippi | 867 | 1,427 | 2,187 | 2,658 | 2,897 | 9.8 |
| North Carolina | 1,963 | 3,250 | 5,901 | 7,311 | 7,801 | 11.3 |
| South Carolina | 978 | 1,753 | 3,108 | 3,962 | 4,221 | 12.0 |
| Tennessee | 2,027 | 3,483 | 5,511 | 6,761 | 7,208 | 10.3 |
| Virginia | 2,077 | 3,530 | 5,661 | 6,618 | 7,031 | .9.9 |
| West Virginia | 831 | 1,219 | 1,763 | 2,190 | 2,346 | 8.4 |
| Southwest | 8,264 | 14,738 | 23,191 | 28,583 | 30,768 | 10.7 |
| Arizona | 1,093 | 2,103 | 3,218 | 3,765 | 3,999 | 10.5 |
| New Mexico | 451 | 873 | 1,364 | 1,703 | 1,848 | 11.5 |
| Oklahoma | 1,177 | 1,896 | 2,674 | 3,182 | 3,329 | 8.5 |
| Texas | 5,543 | 9,866 | 15,935 | 19,932 | 21,592 | 11.1 |
| Rocky Mountains | 2,325 | 4,010 | 6,123 | 7,488 | 7,886 | 9.9 |
| Colorado | 1,218 | 2,087 | 3,101 | 3,776 | 3,932 | 9.5 |
| Idaho | 243 | 419 | 665 | 844 | 900 | 10.7 |
| Montana | 264 | 438 | 679 | 841 | 894 | 9.9 |
| Utah | 453 | 816 | 1,325 | 1,631 | 1,743 | 11.0 |
| Wyoming | 146 | 248 | 353 | 396 | 417 | 8.5 |
| Far West | 14,901 | 24,584 | 36,955 | 43,998 | 46,621 | 9.2 |
| Alaska | 199 | 385 | 557 | 690 | 701 | 10.2 |
| California | 11,632 | 18,883 | 27,949 | 32,880 | 34,827 | 8.8 |
| Hawaii | 360 | 648 | 1,148 | 1,358 | 1,460 | 11.5 |
| Nevada | 387 | 667 | 1,043 | 1,267 | 1,362 | 10.3 |
| Oregon | 928 | 1,486 | 2,297 | 2,714 | 2,966 | 9.4 |
| Washington | 1,396 | 2,516 | 3,961 | 5,090 | 5,305 | 10.9 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 13. Physician Service Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 45,245 | 83,636 | 140,499 | 161,783 | 171,226 | 10.8 |
| New England | 2,072 | 4,010 | 7,656 | 8,678 | 9,250 | 12.2 |
| Connecticut | 589 | 1,127 | 2,185 | 2,468 | 2,587 | 12.1 |
| Maine | 142 | 275 | 480 | 570 | 601 | 11.7 |
| Massachusetts | 978 | 1,890 | 3,766 | 4,130 | 4,442 | 12.3 |
| New Hampshire | 130 | 281 | 491 | 719 | 780 | 14.8 |
| Rhode Island | 166 | 304 | 514 | 543 | 575 | 10.0 |
| Vermont | 68 | 131 | 221 | 248 | 265 | 11.1 |
| Mideast | 7,827 | 14,532 | 24,472 | 28,631 | 30,080 | 10.9 |
| Delaware | 120 | 214 | 377 | 439 | 466 | 11.0 |
| Dist. of Columbia | 237 | 362 | 657 | 651 | 672 | 8.4 |
| Maryland | 835 | 1,702 | 2,968 | 3,498 | 3,704 | 12.1 |
| New Jersey | 1,353 | 2,533 | 4,519 | 5,526 | 5,776 | 11.8 |
| New York | 3,332 | 5,822 | 9,697 | 11,287 | 12,003 | 10.4 |
| Pennsylvania | 1,950 | 3,901 | 6,254 | 7,230 | 7,460 | 10.9 |
| Great Lakes | 8,078 | 13,646 | 21,823 | 24,837 | 26,275 | 9.5 |
| Illinois | 2,118 | 3,672 | 5,864 | 6,707 | 6,970 | 9.6 |
| Indiana | 891 | 1,607 | 2,680 | 3,061 | 3,263 | 10.5 |
| Michigan | 2,002 | 3,080 | 4,668 | 5,224 | 5,562 | 8.2 |
| Ohio | 2,130 | 3,692 | 6,048 | 6,786 | 7,118 | 9.7 |
| Wisconsin | 938 | 1,595 | 2,564 | 3,059 | 3,362 | 10.3 |
| Plains | 3,286 | 5,739 | 9,125 | 10,395 | 10,987 | 9.7 |
| Iowa | 488 | 769 | 1,142 | 1,294 | 1,376 | 8.3 |
| Kansas | 461 | 774 | 1,211 | 1,362 | 1,425 | 9.1 |
| Minnesota | 944 | 1,765 | 2,957 | 3,322 | 3,617 | 10.9 |
| Missouri | 877 | 1,537 | 2,485 | 2,879 | 2,958 | 9.8 |
| Nebraska | 276 | 433 | 688 | 785 | 825 | 8.8 |
| North Dakota | 139 | 288 | 368 | 433 | 445 | 9.4 |
| South Dakota | 102 | 173 | 274 | 319 | 342 | 9.8 |
| Southeast | 9,428 | 18,184 | 32,089 | 36,086 | 37,893 | 11.3 |
| Alabama | 632 | 1,167 | 2,247 | 2,466 | 2,631 | 11.6 |
| Arkansas | 374 | 680 | 1,134 | 1,217 | 1,244 | 9.7 |
| Florida | 2,482 | 5,272 | 9,444 | 10,131 | 10,498 | 11.7 |
| Georgia | 987 | 1,930 | 3,645 | 4,321 | 4,543 | 12.5 |
| Kentucky | 562 | 955 | 1,639 | 1,950 | 2,038 | 10.4 |
| Louisiana | 743 | 1,424 | 2,129 | 2,450 | 2,537 | 9.9 |
| Mississippi | 327 | 568 | 925 | 1,015 | 1,107 | 9.8 |
| North Carolina | 866 | 1,543 | 3,005 | 3,458 | 3,717 | 11.9 |
| South Carolina | 399 | 734 | 1,325 | 1,552 | 1,685 | 11.7 |
| Tennessee | 841 | 1,499 | 2,569 | 2,988 | 3,137 | 10.7 |
| Virginia | 886 | 1,772 | 3,172 | 3,565 | 3,769 | 11.8 |
| West Virginia | 330 | 642 | 856 | 973 | 988 | 8.8 |
| Southwest | 4,350 | 8,218 | 13,377 | 15,008 | 15,680 | 10.4 |
| Arizona | 635 | 1,287 | 2,500 | 2,676 | 2,799 | 12.1 |
| New Mexico | 182 | 368 | 574 | 665 | 716 | 11.1 |
| Oklahoma | 536 | 972 | 1,382 | 1,558 | 1,640 | 9.0 |
| Texas | 2,996 | 5,590 | 8,920 | 10,108 | 10,526 | 10.1 |
| Rocky Mountains | 1,187 | 2,260 | 3,461 | 4,029 | 4,354 | 10.5 |
| Colorado | 600 | 1,230 | 1,891 | 2,242 | 2,452 | 11.4 |
| Idaho | 140 | 235 | 374 | 453 | 486 | 10.1 |
| Montana | 138 | 205 | 311 | 350 | 392 | 8.4 |
| Utah | 244 | 472 | 739 | 832 | 864 | 10.2 |
| Wyoming | 64 | 118 | 146 | 152 | 160 | 7.3 |
| Far West | 9,018 | 17,047 | 28,494 | 34,120 | 36,706 | 11.4 |
| Alaska | 97 | 214 | 258 | 276 | 301 | 9.1 |
| California | 6,959 | 13,311 | 22,365 | 26,903 | 28,981 | 11.6 |
| Hawaii | 249 | 444 | 629 | 742 | 771 | 9.1 |
| Nevada | 207 | 421 | 812 | 988 | 1,029 | 13.1 |
| Oregon | 596 | 990 | 1,597 | 1,798 | 1,904 | 9.3 |
| Washington | 909 | 1,667 | 2,834 | 3,413 | 3,720 | 11.4 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 14. Dental Service Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 13,323 | 21,650 | 30,395 | 34,719 | 37,383 | 8.3 |
| New England | 757 | 1,192 | 1,973 | 2,158 | 2,274 | 8.8 |
| Connecticut | 228 | 361 | 616 | 654 | 685 | 8.8 |
| Maine | 45 | 77 | 129 | 147 | 157 | 10.1 |
| Massachusetts | 362 | 544 | 870 | 970 | 1,022 | 8.3 |
| New Hampshire | 49 | 85 | 149 | 164 | 177 | 10.4 |
| Rhode Island | 47 | 85 | 140 | 145 | 150 | 9.3 |
| Vermont | 26 | 40 | 69 | 77 | 84 | 9.5 |
| Mideast | 2,497 | 4,036 | 5,866 | 6,533 | 6,903 | 8.1 |
| Delaware | 35 | 60 | 79 | 100 | 104 | 8.8 |
| District of Columbia | 42 | 74 | 96 | 109 | 119 | 8.4 |
| Maryland | 242 | 396 | 604 | 697 | 749 | 9.1 |
| New Jersey | 491 | 897 | 1,217 | 1,384 | 1,460 | 8.7 |
| New York | 1,081 | 1,646 | 2,407 | 2,707 | 2,837 | 7.7 |
| Pennsylvania | 606 | 964 | 1,464 | 1,536 | 1,634 | 7.9 |
| Great Lakes | 2,476 | 3,689 | 4,887 | 5,553 | 5,973 | 7.0 |
| Illinois | 662 | 962 | 1,333 | 1,476 | 1,588 | 7.0 |
| Indiana | 258 | 416 | 524 | 626 | 692 | 7.9 |
| Michigan | 682 | 996 | 1,288 | 1,442 | 1,531 | 6.4 |
| Ohio | 569 | 857 | 1,147 | 1,307 | 1,398 | 7.2 |
| Wisconsin | 306 | 458 | 595 | 702 | 765 | 7.3 |
| Plains | 918 | 1,394 | 1,906 | 2,168 | 2,366 | 7.6 |
| Iowa | 150 | 210 | 265 | 313 | 341 | 6.5 |
| Kansas | 124 | 201 | 261 | 299 | 325 | 7.7 |
| Minnesota | 274 | 426 | 608 | 671 | 741 | 7.9 |
| Missouri | 230 | 353 | 494 | 557 | 602 | 7.7 |
| Nebraska | 80 | 113 | 153 | 181 | 191 | 7.0 |
| North Dakota | 31 | 46 | 61 | 69 | 78 | 7.4 |
| South Dakota | 28 | 45 | 64 | 78 | 87 | 9.1 |
| Southeast | 2,407 | 4,101 | 5,927 | 6,859 | 7,492 | 9.1 |
| Alabama | 161 | 248 | 355 | 414 | 456 | 8.3 |
| Arkansas | 84 | 145 | 198 | 221 | 242 | 8.5 |
| Florida | 588 | 1,133 | 1,622 | 1,850 | 2,029 | 10.0 |
| Georgia | 270 | 474 | 723 | 826 | 898 | 9.7 |
| Kentucky | 128 | 195 | 270 | 331 | 369 | 8.5 |
| Louisiana | 179 | 269 | 344 | 400 | 432 | 7.0 |
| Mississippi | 80 | 120 | 167 | 194 | 214 | 7.9 |
| North Carolina | 261 | 429 | 639 | 744 | 810 | 9.1 |
| South Carolina | 114 | 209 | 308 | 356 | 387 | 9.8 |
| Tennessee | 208 | 316 | 485 | 559 | 609 | 8.6 |
| Virginia | 267 | 465 | 692 | 794 | 863 | 9.4 |
| West Virginia | 67 | 99 | 124 | 170 | 182 | 7.9 |
| Southwest | 1,061 | 1,971 | 2,449 | 2,858 | 3,164 | 8.8 |
| Arizona | 165 | 313 | 430 | 495 | 551 | 9.7 |
| New Mexico | 59 | 105 | 134 | 156 | 175 | 8.7 |
| Oklahoma | 142 | 253 | 288 | 330 | 356 | 7.3 |
| Texas | 695 | 1,301 | 1,597 | 1,876 | 2,081 | 8.8 |
| Rocky Mountains | 391 | 717 | 939 | 1,087 | 1,204 | 9.0 |
| Colorado | 192 | 375 | 470 | 543 | 605 | 9.2 |
| Idaho | 52 | 84 | 120 | 147 | 163 | 9.2 |
| Montana | 44 | 71 | 80 | 94 | 103 | 6.8 |
| Utah | 79 | 143 | 223 | 252 | 276 | 10.1 |
| Wyoming | 24 | 43 | 47 | 52 | 57 | 7.0 |
| Far West | 2,816 | 4,552 | 6,448 | 7,503 | 8,005 | 8.4 |
| Alaska | 34 | 72 | 92 | 112 | 124 | 10.6 |
| California | 2,065 | 3,299 | 4,670 | 5,399 | 5,664 | 8.1 |
| Hawaii | 80 | 129 | 188 | 215 | 235 | 8.6 |
| Nevada | 62 | 115 | 163 | 199 | 215 | 10.0 |
| Oregon | 201 | 304 | 449 | 514 | 578 | 8.5 |
| Washington | 375 | 632 | 887 | 1,064 | 1,189 | 9.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 15. Other Professional Service Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 6,353 | 16,639 | 36,010 | 46,401 | 51,220 | 17.4 |
| New England | 349 | 974 | 2,269 | 2,847 | 3,134 | 18.4 |
| Connecticut | 82 | 224 | 554 | 701 | 769 | 18.7 |
| Maine | 29 | 70 | 159 | 192 | 210 | 16.4 |
| Massachusetts | 163 | 472 | 1,096 | 1,383 | 1,524 | 18.7 |
| New Hampshire | 28 | 86 | 194 | 243 | 269 | 18.9 |
| Rhode Island | 30 | 79 | 175 | 218 | 239 | 17.3 |
| Vermont | 15 | 42 | 91 | 110 | 122 | 17.2 |
| Mideast | 1,146 | 3,087 | 6,838 | 9,044 | 9,956 | 18.1 |
| Delaware | 14 | 46 | 104 | 141 | 156 | 20.6 |
| Dist. of Columbia | 39 | 90 | 183 | 244 | 267 | 15.9 |
| Maryland | 90 | 257 | 629 | 855 | 942 | 19.8 |
| New Jersey | 186 | 542 | 1,282 | 1,701 | 1,870 | 19.4 |
| New York | 474 | 1,248 | 2,634 | 3,374 | 3,717 | 17.2 |
| Pennsylvania | 344 | 904 | 2,006 | 2,728 | 3,005 | 18.2 |
| Great Lakes | 1,176 | 2,797 | 5,481 | 7,033 | 7,744 | 15.6 |
| Illinois | 329 | 748 | 1,464 | 1,873 | 2,063 | 15.2 |
| Indiana | 149 | 349 | 728 | 899 | 993 | 15.7 |
| Michigan | 286 | 704 | 1,287 | 1,676 | 1,844 | 15.4 |
| Ohio | 299 | 718 | 1,379 | 1,790 | 1,969 | 15.6 |
| Wisconsin | 113 | 278 | 623 | 795 | 875 | 17.0 |
| Plains | 504 | 1,171 | 2,455 | 2,978 | 3,283 | 15.5 |
| Iowa | 88 | 159 | 330 | 393 | 431 | 13.0 |
| Kansas | 72 | 164 | 330 | 427 | 470 | 15.5 |
| Minnesota | 151 | 391 | 723 | 845 | 933 | 15.0 |
| Missouri | 125 | 303 | 770 | 916 | 1,013 | 17.4 |
| Nebraska | 35 | 78 | 151 | 205 | 225 | 15.5 |
| North Dakota | 15 | 31 | 63 | 85 | 93 | 14.9 |
| South Dakota | 18 | 45 | 87 | 106 | 117 | 15.6 |
| Southeast | 1,205 | 3,330 | 7,848 | 10,344 | 11,455 | 18.9 |
| Alabama | 70 | 207 | 446 | 578 | 641 | 18.6 |
| Arkansas | 52 | 120 | 230 | 301 | 332 | 15.3 |
| Florida | 343 | 998 | 2,422 | 3,163 | 3,505 | 19.6 |
| Georgia | 111 | 356 | 858 | 1,106 | 1,226 | 20.3 |
| Kentucky | 85 | 182 | 430 | 623 | 691 | 17.5 |
| Louisiana | 82 | 240 | 527 | 667 | 736 | 18.4 |
| Mississippi | 42 | 108 | 219 | 260 | 288 | 16.0 |
| North Carolina | 105 | 268 | 722 | 996 | 1,102 | 19.8 |
| South Carolina | 56 | 142 | 327 | 428 | 472 | 17.8 |
| Tennessee | 114 | 324 | 785 | 1,049 | 1,166 | 19.6 |
| Virginia | 99 | 281 | 669 | 878 | 970 | 19.2 |
| West Virginia | 46 | 105 | 213 | 295 | 326 | 16.3 |
| Southwest | 544 | 1,505 | 3,399 | 4,655 | 5,170 | 18.9 |
| Arizona | 85 | 253 | 558 | 736 | 821 | 19.1 |
| New Mexico | 36 | 88 | 178 | 230 | 254 | 16.3 |
| Oklahoma | 77 | 180 | 335 | 458 | 504 | 15.6 |
| Texas | 347 | 984 | 2,328 | 3,231 | 3,591 | 19.7 |
| Rocky Mountains | 171 | 476 | 939 | 1,199 | 1,331 | 17.1 |
| Colorado | 81 | 247 | 534 | 675 | 751 | 18.7 |
| Idaho | 26 | 59 | 92 | 115 | 126 | 13.1 |
| Montana | 25 | 63 | 108 | 149 | 166 | 15.6 |
| Utah | 25 | 75 | 156 | 198 | 220 | 18.1 |
| Wyoming | 14 | 31 | 49 | 62 | 68 | 13.2 |
| Far West | 1,259 | 3,300 | 6,781 | 8,301 | 9,147 | 16.5 |
| Alaska | 18 | 51 | 93 | 115 | 127 | 16.3 |
| California | 969 | 2,548 | 5,173 | 6,232 | 6,859 | 16.2 |
| Hawaii | 22 | 60 | 146 | 202 | 222 | 19.4 |
| Nevada | 25 | 69 | 208 | 277 | 307 | 21.3 |
| Oregon | 70 | 184 | 376 | 481 | 530 | 16.9 |
| Washington | 155 | 389 | 785 | 994 | 1,102 | 16.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 16. Home Health Care Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 2,376 | 5,642 | 13,232 | 20,348 | 22,982 | 19.1 |
| New England | 175 | 377 | 932 | 1,358 | 1,555 | 18.3 |
| Connecticut | 42 | 97 | 240 | 347 | 391 | 18.7 |
| Maine | 13 | 27 | 60 | 92 | 104 | 17.3 |
| Massachusetts | 85 | 193 | 501 | 718 | 835 | 19.2 |
| New Hampshire | 11 | 20 | 46 | 67 | 71 | 15.7 |
| Rhode Island | 16 | 29 | 58 | 90 | 103 | 15.2 |
| Vermont | 8 | 11 | 27 | 45 | 52 | 16.0 |
| Mideast | 896 | 2,041 | 4,177 | 5,141 | 5,486 | 15.0 |
| Delaware | 4 | 16 | 30 | 45 | 51 | 20.7 |
| District of Columbia | 11 | 21 | 37 | 40 | 45 | 11.7 |
| Maryland | 39 | 109 | 189 | 298 | 314 | 17.5 |
| New Jersey | 182 | 290 | 479 | 631 | 718 | 11.1 |
| New York | 536 | 1,270 | 2,937 | 3,409 | 3,562 | 15.7 |
| Pennsylvania | 124 | 334 | 505 | 718 | 796 | 15.4 |
| Great Lakes | 326 | 805 | 1,750 | 2,561 | 2,789 | 18.0 |
| Illinois | 112 | 195 | 418 | 791 | 853 | 16.9 |
| Indiana | 25 | 57 | 141 | 269 | 308 | 21.5 |
| Michigan | 73 | 268 | 562 | 638 | 714 | 19.2 |
| Ohio | 80 | 162 | 368 | 578 | 649 | 17.5 |
| Wisconsin | 37 | 123 | 261 | 286 | 265 | 16.3 |
| Plains | 114 | 267 | 644 | 1,021 | 1,155 | 19.5 |
| Iowa | 15 | 28 | 82 | 127 | 137 | 18.7 |
| Kansas | 10 | 24 | 76 | 140 | 152 | 23.3 |
| Minnesota | 27 | 79 | 243 | 369 | 414 | 23.5 |
| Missouri | 55 | 118 | 191 | 291 | 347 | 15.2 |
| Nebraska | 5 | 14 | 34 | 69 | 74 | 22.8 |
| North Dakota | 1 | 3 | 12 | 15 | 16 | 21.5 |
| South Dakota | 1 | 2 | 6 | 10 | 16 | 20.2 |
| Southeast | 409 | 1,041 | 3,336 | 6,149 | 7,042 | 24.5 |
| Alabama | 30 | 72 | 267 | 489 | 602 | 26.0 |
| Arkansas | 13 | 29 | 75 | 128 | 145 | 20.4 |
| Florida | 170 | 361 | 1,153 | 2,208 | 2,323 | 22.3 |
| Georgia | 39 | 104 | 343 | 606 | 729 | 25.2 |
| Kentucky | 16 | 44 | 183 | 326 | 357 | 26.8 |
| Louisiana | 17 | 43 | 125 | 279 | 410 | 27.7 |
| Mississippi | 21 | 48 | 168 | 262 | 300 | 22.8 |
| North Carolina | 20 | 58 | 273 | 483 | 541 | 29.1 |
| South Carolina | 18 | 43 | 83 | 175 | 216 | 21.2 |
| Tennessee | 26 | 124 | 396 | 756 | 899 | 31.2 |
| Virginia | 30 | 94 | 206 | 324 | 368 | 21.2 |
| West Virginia | 9 | 21 | 63 | 114 | 150 | 24.4 |
| Southwest | 138 | 421 | 1,035 | 1,791 | 2,234 | 23.9 |
| Arizona | 10 | 56 | 148 | 245 | 317 | 30.5 |
| New Mexico | 6 | 14 | 30 | 56 | 62 | 20.2 |
| Oklahoma | 29 | 43 | 87 | 167 | 273 | 18.7 |
| Texas | 93 | 308 | 770 | 1,323 | 1,583 | 24.3 |
| Rocky Mountains | 40 | 87 | 190 | 325 | 422 | 19.8 |
| Colorado | 25 | 47 | 105 | 156 | 195 | 17.0 |
| Idaho | 7 | 17 | 16 | 36 | 49 | 16.0 |
| Montana | 4 | 10 | 29 | 43 | 50 | 20.9 |
| Utah | 2 | 9 | 33 | 74 | 100 | 33.9 |
| Wyoming | 1 | 4 | 7 | 17 | 29 | 25.7 |
| Far West | 277 | 603 | 1,167 | 2,001 | 2,299 | 17.7 |
| Alaska | 0 | 1 | 2 | 4 | 5 | 31.8 |
| California | 200 | 449 | 847 | 1,438 | 1,640 | 17.6 |
| Hawaii | 4 | 8 | 16 | 23 | 32 | 16.7 |
| Nevada | 2 | 9 | 44 | 101 | 120 | 35.2 |
| Oregon | 19 | 39 | 52 | 105 | 122 | 15.3 |
| Washington | 52 | 98 | 207 | 329 | 380 | 16.6 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 17. Drug and Other Medical Non-Durable Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 21,621 | 37,363 | 61,217 | 70,750 | 74,956 | 10.0 |
| New England | 1,095 | 2,041 | 3,497 | 3,901 | 4,079 | 10.6 |
| Connecticut | 295 | 525 | 860 | 957 | 996 | 9.8 |
| Maine | 83 | 156 | 282 | 318 | 333 | 11.3 |
| Massachusetts | 521 | 986 | 1,682 | 1,873 | 1,961 | 10.7 |
| New Hampshire | 76 | 145 | 269 | 302 | 319 | 11.7 |
| Rhode Island | 81 | 156 | 269 | 299 | 310 | 10.9 |
| Vermont | 39 | 73 | 134 | 153 | 161 | 11.6 |
| Mideast | 3,804 | 6,776 | 11,127 | 12,583 | 13,189 | 10.0 |
| Delaware | 55 | 100 | 172 | 201 | 214 | 10.9 |
| District of Columbia | 60 | 103 | 161 | 171 | 175 | 8.6 |
| Maryland | 416 | 789 | 1,425 | 1,654 | 1,749 | 11.7 |
| New Jersey | 694 | 1,255 | 2,062 | 2,334 | 2,452 | 10.2 |
| New York | 1,503 | 2,675 | 4,337 | 4,861 | 5,081 | 9.8 |
| Pennsylvania | 1,076 | 1,854 | 2,970 | 3,361 | 3,519 | 9.5 |
| Great Lakes | 3,874 | 6,367 | 10,213 | 11,689 | 12,302 | 9.3 |
| Illinois | 1,037 | 1,718 | 2,716 | 3,102 | 3,263 | 9.2 |
| Indiana | 523 | 820 | 1,307 | 1,506 | 1,594 | 9.0 |
| Michigan | 907 | 1,490 | 2,446 | 2,799 | 2,937 | 9.5 |
| Ohio | 1,036 | 1,712 | 2,689 | 3,064 | 3,218 | 9.1 |
| Wisconsin | 371 | 628 | 1,054 | 1,218 | 1,290 | 10.1 |
| Plains | 1,532 | 2,504 | 3,941 | 4,502 | 4,746 | 9.1 |
| Iowa | 252 | 402 | 622 | 708 | 743 | 8.7 |
| Kansas | 222 | 368 | 578 | 660 | 695 | 9.2 |
| Minnesota | 341 | 575 | 939 | 1,081 | 1,146 | 9.8 |
| Missouri | 477 | 760 | 1,180 | 1,346 | 1,420 | 8.8 |
| Nebraska | 138 | 224 | 350 | 400 | 421 | 9.0 |
| North Dakota | 51 | 90 | 137 | 153 | 160 | 9.2 |
| South Dakota | 51 | 85 | 135 | 154 | 163 | 9.3 |
| Southeast | 5,136 | 8,974 | 15,193 | 17,750 | 18,912 | 10.5 |
| Alabama | 365 | 614 | 1,011 | 1,173 | 1,247 | 9.9 |
| Arkansas | 232 | 359 | 559 | 643 | 684 | 8.7 |
| Florida | 1,010 | 1,924 | 3,535 | 4,170 | 4,450 | 12.1 |
| Georgia | 523 | 940 | 1,654 | 1,967 | 2,117 | 11.4 |
| Kentucky | 357 | 612 | 978 | 1,127 | 1,196 | 9.7 |
| Louisiana | 436 | 742 | 1,059 | 1,208 | 1,269 | 8.6 |
| Mississippi | 227 | 381 | 595 | 680 | 720 | 9.3 |
| North Carolina | 565 | 939 | 1,616 | 1,892 | 2,027 | 10.3 |
| South Carolina | 274 | 454 | 786 | 922 | 978 | 10.3 |
| Tennessee | 460 | 791 | 1,308 | 1,532 | 1,635 | 10.2 |
| Virginia | 503 | 905 | 1,614 | 1,890 | 2,015 | 11.3 |
| West Virginia | 184 | 314 | 479 | 545 | 574 | 9.1 |
| Southwest | 2,194 | 3,861 | 5,954 | 7,013 | 7,538 | 10.0 |
| Arizona | 262 | 484 | 863 | 1,031 | 1,124 | 11.9 |
| New Mexico | 103 | 192 | 319 | 379 | 409 | 11.2 |
| Oklahoma | 307 | 508 | 721 | 829 | 874 | 8.4 |
| Texas | 1,522 | 2,677 | 4,052 | 4,773 | 5,131 | 9.8 |
| Rocky Mountains | 562 | 978 | 1,496 | 1,789 | 1,945 | 10.0 |
| Colorado | 255 | 459 | 704 | 843 | 919 | 10.4 |
| Idaho | 83 | 130 | 198 | 242 | 265 | 9.3 |
| Montana | 64 | 113 | 168 | 195 | 209 | 9.5 |
| Utah | 118 | 205 | 334 | 404 | 439 | 10.7 |
| Wyoming | 42 | 71 | 92 | 106 | 113 | 7.8 |
| Far West | 3,424 | 5,862 | 9,796 | 11,523 | 12,243 | 10.3 |
| Alaska | 44 | 84 | 126 | 154 | 165 | 10.8 |
| California | 2,514 | 4,341 | 7,294 | 8,527 | 9,017 | 10.3 |
| Hawaii | 109 | 211 | 339 | 393 | 416 | 10.9 |
| Nevada | 87 | 146 | 288 | 369 | 408 | 12.6 |
| Oregon | 264 | 392 | 602 | 710 | 762 | 8.5 |
| Washington | 406 | 688 | 1,146 | 1,370 | 1,474 | 10.4 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 18. Prescription Drug Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 12,049 | 21,405 | 38,198 | 45,730 | 48,840 | 11.4 |
| New England | 625 | 1,217 | 2,250 | 2,578 | 2,710 | 11.9 |
| Connecticut | 174 | 312 | 544 | 622 | 650 | 10.7 |
| Maine | 51 | 93 | 174 | 202 | 213 | 11.6 |
| Massachusetts | 290 | 596 | 1,113 | 1,270 | 1,337 | 12.5 |
| New Hampshire | 39 | 77 | 160 | 185 | 197 | 13.3 |
| Rhode Island | 48 | 96 | 174 | 198 | 206 | 11.8 |
| Vermont | 22 | 43 | 86 | 101 | 108 | 13.0 |
| Mideast | 2,100 | 3,884 | 6,990 | 8,148 | 8,590 | 11.4 |
| Delaware | 25 | 49 | 98 | 120 | 129 | 13.3 |
| District of Columbia | 32 | 57 | 93 | 101 | 103 | 9.5 |
| Maryland | 226 | 443 | 888 | 1,069 | 1,140 | 13.3 |
| New Jersey | 381 | 723 | 1,298 | 1,515 | 1,601 | 11.7 |
| New York | 820 | 1,506 | 2,665 | 3,077 | 3,232 | 11.1 |
| Pennsylvania | 616 | 1,105 | 1,948 | 2,267 | 2,386 | 11.0 |
| Great Lakes | 2,219 | 3,850 | 6,691 | 7,895 | 8,360 | 10.7 |
| Illinois | 561 | 1,006 | 1,771 | 2,084 | 2,206 | 11.1 |
| Indiana | 305 | 508 | 874 | 1,038 | 1,106 | 10.4 |
| Michigan | 527 | 939 | 1,654 | 1,947 | 2,054 | 11.0 |
| Ohio | 607 | 1,010 | 1,684 | 1,982 | 2,095 | 10.0 |
| Wisconsin | 218 | 387 | 708 | 844 | 899 | 11.5 |
| Plains | 887 | 1,495 | 2,557 | 3,012 | 3,195 | 10.4 |
| Iowa | 156 | 255 | 419 | 490 | 516 | 9.6 |
| Kansas | 128 | 218 | 373 | 439 | 465 | 10.5 |
| Minnesota | 191 | 324 | 580 | 691 | 739 | 11.0 |
| Missouri | 274 | 461 | 783 | 919 | 975 | 10.2 |
| Nebraska | 80 | 136 | 235 | 277 | 293 | 10.5 |
| North Dakota | 28 | 51 | 86 | 98 | 103 | 10.6 |
| South Dakota | 30 | 50 | 82 | 97 | 104 | 10.0 |
| Southeast | 3,011 | 5,356 | 9,811 | 11,872 | 12,759 | 11.7 |
| Alabama | 235 | 404 | 707 | 845 | 904 | 10.9 |
| Arkansas | 153 | 235 | 382 | 452 | 484 | 9.3 |
| Florida | 536 | 1,041 | 2,135 | 2,627 | 2,832 | 13.7 |
| Georgia | 294 | 540 | 1,035 | 1,283 | 1,397 | 12.7 |
| Kentucky | 225 | 392 | 667 | 791 | 846 | 10.7 |
| Louisiana | 254 | 440 | 668 | 788 | 832 | 9.5 |
| Mississippi | 142 | 241 | 399 | 468 | 499 | 10.1 |
| North Carolina | 340 | 569 | 1,061 | 1,287 | 1,392 | 11.5 |
| South Carolina | 154 | 268 | 511 | 622 | 665 | 11.9 |
| Tennessee | 288 | 500 | 886 | 1,072 | 1,153 | 11.2 |
| Virginia | 275 | 522 | 1,026 | 1,248 | 1,343 | 13.0 |
| West Virginia | 116 | 204 | 333 | 389 | 412 | 10.3 |
| Southwest | 1,198 | 2,116 | 3,512 | 4,326 | 4,709 | 11.1 |
| Arizona | 123 | 250 | 526 | 659 | 728 | 14.7 |
| New Mexico | 52 | 101 | 190 | 237 | 259 | 13.2 |
| Oklahoma | 175 | 299 | 450 | 535 | 569 | 9.5 |
| Texas | 848 | 1,467 | 2,346 | 2,896 | 3,153 | 10.6 |
| Rocky Mountains | 279 | 498 | 865 | 1,089 | 1,203 | 11.9 |
| Colorado | 127 | 223 | 379 | 481 | 534 | 11.7 |
| Idaho | 44 | 74 | 129 | 164 | 182 | 11.6 |
| Montana | 31 | 54 | 90 | 110 | 120 | 11.0 |
| Utah | 54 | 110 | 218 | 274 | 302 | 14.2 |
| Wyoming | 23 | 37 | 49 | 59 | 64 | 8.2 |
| Far West | 1,730 | 2,988 | 5,523 | 6,810 | 7,313 | 11.7 |
| Alaska | 16 | 34 | 58 | 77 | 85 | 13.7 |
| California | 1,296 | 2,274 | 4,222 | 5,155 | 5,501 | 11.8 |
| Hawaii | 44 | 87 | 148 | 184 | 197 | 12.2 |
| Nevada | 36 | 67 | 158 | 218 | 246 | 15.8 |
| Oregon | 125 | 187 | 318 | 396 | 431 | 10.0 |
| Washington | 212 | 340 | 618 | 781 | 853 | 11.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 19. Vision Products and Other Medical Durable Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 4,495 | 7,067 | 10,511 | 11,997 | 12,636 | 8.3 |
| New England | 206 | 340 | 525 | 582 | 608 | 8.7 |
| Connecticut | 67 | 107 | 165 | 184 | 192 | 8.5 |
| Maine | 16 | 26 | 40 | 44 | 46 | 8.4 |
| Massachusetts | 91 | 153 | 233 | 258 | 269 | 8.7 |
| New Hampshire | 12 | 22 | 37 | 41 | 43 | 10.3 |
| Rhode Island | 12 | 19 | 29 | 32 | 33 | 8.2 |
| Vermont | 8 | 13 | 20 | 23 | 24 | 8.9 |
| Mideast | 916 | 1,433 | 2,107 | 2,394 | 2,505 | 8.0 |
| Delaware | 14 | 19 | 28 | 33 | 35 | 7.4 |
| District of Columbia | 19 | 24 | 30 | 33 | 34 | 4.6 |
| Maryland | 95 | 147 | 226 | 259 | 272 | 8.4 |
| New Jersey | 155 | 249 | 384 | 436 | 457 | 8.7 |
| New York | 398 | 636 | 919 | 1,043 | 1,090 | 8.1 |
| Pennsylvania | 235 | 358 | 520 | 590 | 617 | 7.7 |
| Great Lakes | 818 | 1,247 | 1,790 | 2,005 | 2,103 | 7.5 |
| Illinois | 228 | 350 | 510 | 576 | 604 | 7.8 |
| Indiana | 100 | 159 | 228 | 257 | 270 | 7.9 |
| Michigan | 180 | 267 | 393 | 437 | 457 | 7.4 |
| Ohio | 223 | 328 | 455 | 507 | 531 | 6.9 |
| Wisconsin | 88 | 143 | 203 | 228 | 240 | 8.0 |
| Plains | 373 | 547 | 769 | 870 | 914 | 7.1 |
| Iowa | 61 | 93 | 127 | 141 | 148 | 7.0 |
| Kansas | 44 | 67 | 91 | 102 | 107 | 7.0 |
| Minnesota | 104 | 156 | 229 | 263 | 277 | 7.8 |
| Missouri | 100 | 144 | 205 | 232 | 244 | 7.1 |
| Nebraska | 39 | 50 | 67 | 77 | 80 | 5.7 |
| North Dakota | 12 | 19 | 25 | 27 | 28 | 7.1 |
| South Dakota | 12 | 19 | 26 | 28 | 30 | 7.0 |
| Southeast | 879 | 1,440 | 2,246 | 2,608 | 2,756 | 9.2 |
| Alabama | 52 | 82 | 125 | 147 | 155 | 8.7 |
| Arkansas | 21 | 33 | 48 | 53 | 56 | 8.0 |
| Florida | 256 | 430 | 705 | 824 | 872 | 9.9 |
| Georgia | 103 | 169 | 267 | 311 | 331 | 9.4 |
| Kentucky | 50 | 77 | 115 | 134 | 141 | 8.3 |
| Louisiana | 69 | 102 | 134 | 153 | 160 | 6.7 |
| Mississippi | 26 | 35 | 49 | 57 | 60 | 6.8 |
| North Carolina | 77 | 133 | 217 | 253 | 268 | 10.1 |
| South Carolina | 33 | 59 | 95 | 109 | 115 | 10.2 |
| Tennessee | 69 | 116 | 186 | 216 | 228 | 9.6 |
| Virginia | 98 | 160 | 244 | 280 | 295 | 8.8 |
| West Virginia | 27 | 44 | 63 | 70 | 74 | 8.1 |
| Southwest | 493 | 738 | 1,053 | 1,222 | 1,299 | 7.7 |
| Arizona | 62 | 108 | 181 | 212 | 227 | 10.5 |
| New Mexico | 22 | 37 | 56 | 65 | 69 | 9.3 |
| Oklahoma | 50 | 76 | 101 | 115 | 121 | 7.0 |
| Texas | 359 | 517 | 716 | 830 | 883 | 7.2 |
| Rocky Mountains | 149 | 239 | 341 | 402 | 430 | 8.5 |
| Colorado | 75 | 121 | 178 | 210 | 226 | 8.9 |
| Idaho | 14 | 21 | 28 | 33 | 35 | 7.1 |
| Montana | 15 | 24 | 30 | 34 | 36 | 6.8 |
| Utah | 36 | 60 | 91 | 109 | 117 | 9.4 |
| Wyoming | 9 | 13 | 14 | 16 | 17 | 5.1 |
| Far West | 660 | 1,083 | 1,679 | 1,914 | 2,021 | 9.0 |
| Alaska | 13 | 19 | 21 | 25 | 26 | 5.3 |
| California | 473 | 807 | 1,274 | 1,446 | 1,522 | 9.4 |
| Hawaii | 23 | 34 | 51 | 61 | 64 | 8.1 |
| Nevada | 21 | 34 | 58 | 70 | 76 | 10.2 |
| Oregon | 40 | 58 | 79 | 85 | 91 | 6.4 |
| Washington | 89 | 131 | 196 | 228 | 242 | 8.0 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 20. Nursing Home Care Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 17,649 | 30,679 | 50,923 | 62,297 | 66,201 | 10.7 |
| New England | 1,407 | 2,542 | 4,932 | 5,640 | 5,839 | 11.6 |
| Connecticut | 373 | 703 | 1,408 | 1,646 | 1,749 | 12.6 |
| Maine | 120 | 196 | 361 | 440 | 453 | 10.8 |
| Massachusetts | 675 | 1,208 | 2,455 | 2,716 | 2,737 | 11.4 |
| New Hampshire | 66 | 126 | 204 | 240 | 268 | 11.4 |
| Rhode Island | 124 | 246 | 376 | 456 | 485 | 11.1 |
| Vermont | 49 | 63 | 130 | 143 | 148 | 8.9 |
| Mideast | 4,818 | 8,437 | 13,269 | 15,960 | 17,021 | 10.2 |
| Delaware | 46 | 93 | 173 | 203 | 217 | 12.8 |
| District of Columbia | 26 | 73 | 142 | 213 | 231 | 18.3 |
| Maryland | 254 | 549 | 920 | 1,092 | 1,185 | 12.6 |
| New Jersey | 497 | 915 | 1,731 | 2,056 | 2,128 | 11.8 |
| New York | 2,796 | 4,677 | 7,013 | 8,502 | 9,106 | 9.5 |
| Pennsylvania | 1,200 | 2,130 | 3,289 | 3,894 | 4,153 | 10.0 |
| Great Lakes | 3,182 | 5,666 | 9,503 | 11,886 | 12,526 | 11.1 |
| Illinois | 830 | 1,480 | 2,311 | 3,006 | 3,148 | 10.8 |
| Indiana | 406 | 738 | 1,472 | 1,914 | 2,018 | 13.1 |
| Michigan | 607 | 920 | 1,502 | 1,765 | 1,849 | 8.9 |
| Ohio | 793 | 1,689 | 2,828 | 3,563 | 3,758 | 12.7 |
| Wisconsin | 545 | 840 | 1,389 | 1,639 | 1,752 | 9.4 |
| Plains | 1,816 | 3,110 | 4,632 | 5,523 | 5,844 | 9.4 |
| Iowa | 334 | 480 | 735 | 878 | 927 | 8.2 |
| Kansas | 213 | 342 | 576 | 682 | 721 | 9.8 |
| Minnesota | 589 | 1,053 | 1,477 | 1,776 | 1,884 | 9.4 |
| Missouri | 361 | 705 | 1,096 | 1,302 | 1,368 | 10.8 |
| Nebraska | 184 | 279 | 379 | 449 | 482 | 7.7 |
| North Dakota | 58 | 135 | 201 | 237 | 246 | 11.8 |
| South Dakota | 78 | 116 | 169 | 199 | 216 | 8.2 |
| Southeast | 2,746 | 5,111 | 8,988 | 11,558 | 12,509 | 12.4 |
| Alabama | 186 | 347 | 495 | 658 | 703 | 10.8 |
| Arkansas | 192 | 286 | 430 | 531 | 558 | 8.5 |
| Florida | 414 | 1,109 | 2,244 | 2,855 | 3,089 | 16.7 |
| Georgia | 285 | 448 | 776 | 961 | 1,038 | 10.5 |
| Kentucky | 243 | 421 | 623 | 782 | 850 | 10.1 |
| Louisiana | 246 | 426 | 786 | 1,070 | 1,186 | 12.9 |
| Mississippi | 134 | 192 | 310 | 419 | 460 | 10.0 |
| North Carolina | 271 | 548 | 1,080 | 1,409 | 1,562 | 14.4 |
| South Carolina | 161 | 241 | 474 | 596 | 638 | 11.2 |
| Tennessee | 258 | 453 | 768 | 1,000 | 1,085 | 11.7 |
| Virginia | 295 | 510 | 736 | 937 | 976 | 9.7 |
| West Virginia | 61 | 130 | 265 | 342 | 365 | 14.7 |
| Southwest | 1,262 | 2,063 | 3,476 | 4,321 | 4,633 | 10.5 |
| Arizona | 83 | 179 | 448 | 515 | 567 | 15.9 |
| New Mexico | 33 | 77 | 162 | 200 | 215 | 15.6 |
| Oklahoma | 218 | 365 | 593 | 713 | 748 | 10.0 |
| Texas | 929 | 1,442 | 2,273 | 2,893 | 3,104 | 9.7 |
| Rocky Mountains | 406 | 662 | 1,059 | 1,262 | 1,378 | 9.9 |
| Colorado | 210 | 338 | 513 | 614 | 661 | 9.2 |
| Idaho | 51 | 80 | 131 | 175 | 197 | 10.9 |
| Montana | 49 | 87 | 153 | 167 | 178 | 10.5 |
| Utah | 75 | 120 | 207 | 237 | 260 | 10.0 |
| Wyoming | 21 | 37 | 54 | 69 | 83 | 11.3 |
| Far West | 2,011 | 3,087 | 5,065 | 6,145 | 6,451 | 9.4 |
| Alaska | 22 | 32 | 45 | 54 | 56 | 7.3 |
| California | 1,344 | 2,014 | 3,320 | 3,939 | 4,103 | 9.0 |
| Hawaii | 46 | 95 | 139 | 174 | 181 | 11.2 |
| Nevada | 31 | 54 | 111 | 145 | 164 | 13.7 |
| Oregon | 198 | 319 | 527 | 642 | 656 | 9.7 |
| Washington | 371 | 573 | 922 | 1,192 | 1,291 | 10.1 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 21. Other Personal Health Care Expenditures and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 3,953 | 6,015 | 11,220 | 15,622 | 17,988 | 12.4 |
| New England | 276 | 406 | 958 | 1,408 | 1,654 | 14.8 |
| Connecticut | 78 | 115 | 282 | 422 | 467 | 14.7 |
| Maine | 21 | 26 | 72 | 113 | 153 | 16.7 |
| Massachusetts | 131 | 186 | 408 | 542 | 597 | 12.4 |
| New Hampshire | 17 | 33 | 77 | 108 | 136 | 17.4 |
| Rhode Island | 18 | 26 | 76 | 152 | 219 | 21.2 |
| Vermont | 12 | 19 | 43 | 70 | 82 | 15.9 |
| Mideast | 916 | 1,380 | 2,348 | 3,040 | 3,524 | 10.9 |
| Delaware | 13 | 19 | 38 | 66 | 79 | 15.2 |
| District of Columbia | 43 | 66 | 96 | 120 | 130 | 8.9 |
| Maryland | 73 | 104 | 222 | 301 | 312 | 11.9 |
| New Jersey | 137 | 208 | 420 | 504 | 570 | 11.6 |
| New York | 440 | 672 | 1,035 | 1,358 | 1,635 | 10.6 |
| Pennsylvania | 210 | 311 | 537 | 692 | 798 | 10.8 |
| Great Lakes | 665 | 895 | 1,516 | 2,138 | 2,358 | 10.2 |
| Illinois | 174 | 240 | 405 | 582 | 636 | 10.5 |
| Indiana | 91 | 133 | 181 | 254 | 264 | 8.5 |
| Michigan | 140 | 172 | 325 | 470 | 532 | 10.8 |
| Ohio | 184 | 222 | 349 | 444 | 511 | 8.2 |
| Wisconsin | 76 | 128 | 256 | 389 | 415 | 13.9 |
| Plains | 241 | 383 | 736 | 1,035 | 1,213 | 13.2 |
| Iowa | 32 | 47 | 83 | 112 | 127 | 11.3 |
| Kansas | 27 | 41 | 85 | 118 | 140 | 13.5 |
| Minnesota | 70 | 127 | 240 | 325 | 386 | 14.0 |
| Missouri | 66 | 99 | 186 | 291 | 346 | 13.6 |
| Nebraska | 22 | 28 | 68 | 88 | 99 | 12.2 |
| North Dakota | 10 | 18 | 35 | 48 | 52 | 13.6 |
| South Dakota | 15 | 24 | 38 | 53 | 63 | 11.8 |
| Southeast | 838 | 1,326 | 2,489 | 3,486 | 4,128 | 13.0 |
| Alabama | 71 | 104 | 197 | 274 | 323 | 12.4 |
| Arkansas | 31 | 39 | 66 | 111 | 127 | 11.5 |
| Florida | 146 | 265 | 540 | 764 | 912 | 15.1 |
| Georgia | 105 | 167 | 336 | 431 | 516 | 13.1 |
| Kentucky | 45 | 79 | 152 | 206 | 228 | 13.2 |
| Louisiana | 61 | 93 | 157 | 265 | 328 | 13.8 |
| Mississippi | 46 | 57 | 95 | 120 | 141 | 9.0 |
| North Carolina | 85 | 134 | 247 | 343 | 413 | 12.9 |
| South Carolina | 59 | 92 | 194 | 262 | 317 | 13.8 |
| Tennessee | 66 | 105 | 170 | 225 | 235 | 10.2 |
| Virginia | 91 | 147 | 261 | 350 | 395 | 12.0 |
| West Virginia | 31 | 45 | 77 | 133 | 192 | 15.0 |
| Southwest | 333 | 516 | 988 | 1,628 | 1,883 | 14.3 |
| Arizona | 56 | 74 | 134 | 220 | 230 | 11.4 |
| New Mexico | 29 | 38 | 78 | 113 | 131 | 12.4 |
| Oklahoma | 43 | 55 | 98 | 170 | 196 | 12.4 |
| Texas | 204 | 348 | 677 | 1,125 | 1,325 | 15.5 |
| Rocky Mountains | 142 | 225 | 402 | 552 | 610 | 11.9 |
| Colorado | 79 | 130 | 228 | 299 | 327 | 11.5 |
| Idaho | 11 | 14 | 34 | 48 | 55 | 13.2 |
| Montana | 17 | 28 | 48 | 66 | 74 | 11.7 |
| Utah | 18 | 27 | 62 | 91 | 99 | 13.8 |
| Wyoming | 16 | 26 | 31 | 48 | 55 | 10.2 |
| Far West | 543 | 884 | 1,782 | 2,335 | 2,619 | 12.9 |
| Alaska | 20 | 29 | 45 | 61 | 68 | 9.9 |
| California | 369 | 616 | 1,225 | 1,451 | 1,565 | 11.7 |
| Hawaii | 26 | 42 | 77 | 92 | 104 | 11.3 |
| Nevada | 14 | 21 | 40 | 60 | 67 | 12.9 |
| Oregon | 39 | 72 | 157 | 299 | 391 | 19.4 |
| Washington | 75 | 105 | 238 | 371 | 425 | 14.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 22. Medicare Expenditures for Personal Health Care and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 36,249 | 70,063 | 109,123 | 134,804 | 150,374 | 11.6 |
| New England | 2,195 | 4,124 | 6,162 | 7,837 | 8,829 | 11.3 |
| Connecticut | 513 | 929 | 1,550 | 1,928 | 2,134 | 11.6 |
| Maine | 177 | 301 | 442 | 533 | 605 | 9.9 |
| Massachusetts | 1,144 | 2,247 | 3,203 | 4,116 | 4,712 | 11.5 |
| New Hampshire | 113 | 209 | 329 | 435 | 473 | 11.6 |
| Rhode Island | 178 | 331 | 470 | 604 | 664 | 10.7 |
| Vermont | 71 | 108 | 168 | 220 | 241 | 9.9 |
| Mideast | 7,602 | 14,809 | 22,741 | 27,223 | 30,438 | 11.3 |
| Delaware | 86 | 155 | 268 | 333 | 377 | 12.0 |
| District of Columbia | 207 | 334 | 512 | 568 | 603 | 8.6 |
| Maryland | 555 | 1,112 | 2,024 | 2,463 | 2,692 | 12.9 |
| New Jersey | 1,075 | 2,337 | 3,365 | 4,390 | 4,838 | 12.3 |
| New York | 3,358 | 5,902 | 9,206 | 10,642 | 11,872 | 10.2 |
| Pennsylvania | 2,320 | 4,969 | 7,366 | 8,828 | 10,056 | 11.9 |
| Great Lakes | 6,740 | 12,199 | 17,702 | 21,445 | 23,508 | 10.1 |
| Illinois | 2,018 | 3,619 | 4,769 | 5,865 | 6,404 | 9.3 |
| Indiana | 682 | 1,395 | 2,232 | 2,836 | 3,126 | 12.4 |
| Michigan | 1,710 | 2,906 | 4,136 | 4,817 | 5,405 | 9.3 |
| Ohio | 1,630 | 3,018 | 4,692 | 5,758 | 6,177 | 10.8 |
| Wisconsin | 700 | 1,260 | 1,873 | 2,170 | 2,397 | 9.9 |
| Plains | 2,981 | 5,252 | 7,619 | 9,059 | 9,861 | 9.6 |
| Iowa | 458 | 772 | 1,136 | 1,310 | 1,447 | 9.3 |
| Kansas | 388 | 661 | 985 | 1,210 | 1,326 | 9.9 |
| Minnesota | 680 | 1,148 | 1,751 | 2,042 | 2,164 | 9.3 |
| Missouri | 1,006 | 1,889 | 2,595 | 3,128 | 3,439 | 9.9 |
| Nebraska | 241 | 386 | 576 | 685 | 746 | 9.1 |
| North Dakota | 115 | 216 | 304 | 351 | 374 | 9.5 |
| South Dakota | 93 | 178 | 272 | 332 | 364 | 11.0 |
| Southeast | 7,687 | 15,975 | 26,995 | 34,770 | 38,805 | 13.3 |
| Alabama | 526 | 1,048 | 1,794 | 2,354 | 2,625 | 13.2 |
| Arkansas | 326 | 656 | 1,068 | 1,347 | 1,422 | 12.0 |
| Florida | 2,416 | 5,095 | 8,728 | 10,950 | 12,484 | 13.5 |
| Georgia | 642 | 1,340 | 2,320 | 3,243 | 3,549 | 14.1 |
| Kentucky | 425 | 850 | 1,543 | 1,917 | 2,143 | 13.3 |
| Louisiana | 499 | 1,171 | 1,958 | 2,448 | 2,730 | 14.0 |
| Mississippi | 290 | 572 | 981 | 1,244 | 1,367 | 12.7 |
| North Carolina | 690 | 1,424 | 2,384 | 3,231 | 3,553 | 13.4 |
| South Carolina | 294 | 618 | 1,001 | 1,348 | 1,541 | 13.6 |
| Tennessee | 697 | 1,447 | 2,409 | 3,151 | 3,549 | 13.3 |
| Virginia | 617 | 1,207 | 1,986 | 2,483 | 2,736 | 12.1 |
| West Virginia | 266 | 547 | 824 | 1,053 | 1,106 | 11.6 |
| Southwest | 2,837 | 5,677 | 9,437 | 11,873 | 13,271 | 12.6 |
| Arizona | 424 | 985 | 1,720 | 2,134 | 2,276 | 13.8 |
| New Mexico | 128 | 277 | 442 | 514 | 565 | 12.1 |
| Oklahoma | 436 | 764 | 1,205 | 1,521 | 1,665 | 10.9 |
| Texas | 1,849 | 3,650 | 6,071 | 7,704 | 8,765 | 12.7 |
| Rocky Mountains | 683 | 1,359 | 2,134 | 2,699 | 3,104 | 12.4 |
| Colorado | 353 | 682 | 1,082 | 1,352 | 1,556 | 12.1 |
| Idaho | 85 | 173 | 246 | 340 | 384 | 12.3 |
| Montana | 91 | 172 | 279 | 346 | 391 | 11.8 |
| Utah | 117 | 261 | 421 | 532 | 624 | 13.8 |
| Wyoming | 37 | 72 | 106 | 129 | 150 | 11.4 |
| Far West | 5,525 | 10,668 | 16,332 | 19,899 | 22,558 | 11.4 |
| Alaska | 17 | 38 | 71 | 93 | 101 | 14.9 |
| California | 4,360 | 8,355 | 12,514 | 15,200 | 17,347 | 11.2 |
| Hawaii | 99 | 199 | 351 | 433 | 496 | 13.2 |
| Nevada | 136 | 278 | 499 | 605 | 732 | 13.8 |
| Oregon | 389 | 713 | 1,124 | 1,362 | 1,521 | 11.1 |
| Washington | 523 | 1,085 | 1,775 | 2,206 | 2,360 | 12.3 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 23. Medicaid Expenditures for Personal Health Care and Average Annual Percent Growth, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | Average Annual Percent Growth 1980-93 |
|---|---|---|---|---|---|---|
|
| ||||||
| Millions of Dollars | ||||||
| United States | 24,743 | 39,024 | 71,561 | 103,731 | 112,776 | 12.5 |
| New England | 1,875 | 2,884 | 6,088 | 8,068 | 7,880 | 11.9 |
| Connecticut | 346 | 626 | 1,277 | 1,857 | 1,998 | 14.7 |
| Maine | 148 | 246 | 449 | 669 | 722 | 13.1 |
| Massachusetts | 1,083 | 1,546 | 3,464 | 3,923 | 3,689 | 10.3 |
| New Hampshire | 75 | 122 | 260 | 661 | 446 | 17.0 |
| Rhode Island | 160 | 257 | 480 | 731 | 793 | 13.3 |
| Vermont | 63 | 87 | 159 | 227 | 232 | 10.9 |
| Mideast | 7,205 | 11,766 | 19,952 | 27,875 | 29,865 | 11.6 |
| Delaware | 47 | 73 | 137 | 220 | 249 | 14.2 |
| District of Columbia | 164 | 304 | 416 | 595 | 678 | 12.0 |
| Maryland | 439 | 640 | 1,199 | 1,807 | 1,924 | 12.3 |
| New Jersey | 756 | 1,178 | 2,473 | 3,555 | 3,857 | 13.6 |
| New York | 4,504 | 7,636 | 12,550 | 16,546 | 18,041 | 11.3 |
| Pennsylvania | 1,294 | 1,934 | 3,177 | 5,153 | 5,116 | 11.5 |
| Great Lakes | 4,513 | 7,010 | 11,454 | 16,693 | 18,054 | 11.4 |
| Illinois | 1,294 | 1,707 | 2,401 | 4,205 | 4,609 | 10.8 |
| Indiana | 394 | 770 | 1,525 | 2,410 | 2,777 | 16.3 |
| Michigan | 1,199 | 1,694 | 2,710 | 3,522 | 3,865 | 9.6 |
| Ohio | 873 | 1,827 | 3,326 | 4,558 | 4,665 | 14.0 |
| Wisconsin | 753 | 1,013 | 1,493 | 1,999 | 2,138 | 8.5 |
| Plains | 1,593 | 2,603 | 4,437 | 6,314 | 6,700 | 11.9 |
| Iowa | 244 | 367 | 654 | 907 | 960 | 11.3 |
| Kansas | 199 | 267 | 505 | 682 | 769 | 11.2 |
| Minnesota | 611 | 1,027 | 1,488 | 1,948 | 2,229 | 10.6 |
| Missouri | 314 | 552 | 1,087 | 1,790 | 1,648 | 14.2 |
| Nebraska | 113 | 172 | 330 | 495 | 561 | 13.3 |
| North Dakota | 51 | 123 | 201 | 253 | 269 | 14.3 |
| South Dakota | 61 | 95 | 172 | 240 | 264 | 12.1 |
| Southeast | 3,975 | 6,502 | 14,228 | 21,478 | 23,891 | 15.0 |
| Alabama | 294 | 434 | 812 | 1,201 | 1,276 | 12.6 |
| Arkansas | 249 | 376 | 612 | 919 | 1,007 | 11.6 |
| Florida | 418 | 953 | 2,576 | 4,056 | 4,697 | 20.6 |
| Georgia | 483 | 773 | 1,593 | 2,288 | 2,753 | 14.5 |
| Kentucky | 321 | 541 | 1,087 | 1,624 | 1,683 | 13.9 |
| Louisiana | 420 | 745 | 1,460 | 2,329 | 2,664 | 15.5 |
| Mississippi | 222 | 284 | 632 | 962 | 1,043 | 13.1 |
| North Carolina | 431 | 677 | 1,577 | 2,297 | 2,564 | 14.9 |
| South Carolina | 265 | 354 | 919 | 1,248 | 1,324 | 13.8 |
| Tennessee | 384 | 621 | 1,474 | 2,133 | 2,183 | 14.6 |
| Virginia | 376 | 564 | 1,047 | 1,485 | 1,621 | 12.1 |
| West Virginia | 112 | 181 | 439 | 935 | 1,075 | 19.9 |
| Southwest | 1,379 | 2,290 | 4,840 | 7,992 | 8,775 | 15.7 |
| Arizona | 0 | 101 | 568 | 1,189 | 1,270 | 51.4 |
| New Mexico | 75 | 154 | 300 | 507 | 577 | 17.3 |
| Oklahoma | 290 | 461 | 722 | 1,007 | 1,013 | 10.3 |
| Texas | 1,014 | 1,573 | 3,250 | 5,289 | 5,914 | 15.0 |
| Rocky Mountains | 406 | 667 | 1,289 | 1,897 | 2,193 | 14.1 |
| Colorado | 191 | 306 | 570 | 795 | 967 | 13.6 |
| Idaho | 53 | 75 | 164 | 270 | 290 | 14.5 |
| Montana | 69 | 104 | 198 | 279 | 322 | 13.1 |
| Utah | 78 | 152 | 285 | 431 | 477 | 15.2 |
| Wyoming | 15 | 29 | 72 | 123 | 137 | 18.9 |
| Far West | 3,797 | 5,303 | 9,273 | 13,414 | 15,418 | 11.7 |
| Alaska | 39 | 69 | 155 | 218 | 273 | 16.2 |
| California | 3,047 | 4,143 | 6,941 | 9,834 | 11,330 | 10.9 |
| Hawaii | 97 | 141 | 212 | 296 | 354 | 10.8 |
| Nevada | 49 | 70 | 153 | 329 | 344 | 17.3 |
| Oregon | 186 | 262 | 547 | 820 | 955 | 13.7 |
| Washington | 379 | 618 | 1,265 | 1,917 | 2,161 | 14.6 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 24. Number of Medicare Enrollees and Medicare Expenditures for Personal Health Care, by Type of Service, by Region and State: Calendar Year 1993.
| Region and State | Number of Enrollees1 (Thousands) |
Total Personal Health Care | Hospital Care | Physician Services | Other Professional Services | Home Health Care | Medical Durables | Nursing Home Care |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Millions of Dollars | ||||||||
| United States | 35,557 | 150,374 | 94,226 | 34,555 | 5,559 | 8,023 | 3,696 | 4,315 |
| New England | 1,988 | 8,829 | 5,559 | 1,698 | 359 | 718 | 123 | 372 |
| Connecticut | 490 | 2,134 | 1,258 | 477 | 88 | 167 | 29 | 115 |
| Maine | 194 | 605 | 391 | 116 | 22 | 58 | 12 | 7 |
| Massachusetts | 911 | 4,712 | 3,017 | 834 | 199 | 378 | 69 | 215 |
| New Hampshire | 149 | 473 | 309 | 91 | 16 | 39 | 7 | 11 |
| Rhode Island | 165 | 664 | 425 | 139 | 28 | 47 | 4 | 22 |
| Vermont | 79 | 241 | 160 | 42 | 7 | 28 | 2 | 3 |
| Mideast | 6,520 | 30,438 | 19,933 | 6,973 | 1,064 | 956 | 848 | 665 |
| Delaware | 96 | 377 | 240 | 85 | 16 | 16 | 12 | 8 |
| District of Columbia | 79 | 603 | 445 | 111 | 20 | 15 | 3 | 9 |
| Maryland | 580 | 2,692 | 1,778 | 611 | 95 | 79 | 73 | 56 |
| New Jersey | 1,142 | 4,838 | 2,944 | 1,347 | 144 | 118 | 205 | 80 |
| New York | 2,583 | 11,872 | 7,907 | 2,717 | 427 | 375 | 207 | 240 |
| Pennsylvania | 2,041 | 10,056 | 6,619 | 2,102 | 362 | 353 | 348 | 271 |
| Great Lakes | 6,071 | 23,508 | 15,441 | 4,953 | 811 | 986 | 573 | 744 |
| Illinois | 1,592 | 6,404 | 4,219 | 1,332 | 228 | 284 | 210 | 131 |
| Indiana | 803 | 3,126 | 2,105 | 601 | 70 | 147 | 41 | 162 |
| Michigan | 1,306 | 5,405 | 3,449 | 1,197 | 224 | 257 | 152 | 127 |
| Ohio | 1,626 | 6,177 | 4,066 | 1,329 | 223 | 223 | 125 | 210 |
| Wisconsin | 745 | 2,397 | 1,603 | 494 | 66 | 74 | 45 | 114 |
| Plains | 2,738 | 9,861 | 6,815 | 2,049 | 303 | 263 | 214 | 216 |
| Iowa | 469 | 1,447 | 1,043 | 287 | 47 | 33 | 29 | 8 |
| Kansas | 377 | 1,326 | 887 | 276 | 55 | 43 | 43 | 21 |
| Minnesota | 616 | 2,164 | 1,430 | 481 | 57 | 53 | 52 | 90 |
| Missouri | 815 | 3,439 | 2,395 | 691 | 105 | 113 | 64 | 71 |
| Nebraska | 245 | 746 | 527 | 159 | 20 | 13 | 16 | 11 |
| North Dakota | 102 | 374 | 269 | 81 | 10 | 5 | 4 | 6 |
| South Dakota | 114 | 364 | 264 | 75 | 8 | 2 | 7 | 8 |
| Southeast | 9,150 | 38,805 | 23,075 | 8,943 | 1,574 | 3,056 | 1,156 | 1,002 |
| Alabama | 619 | 2,625 | 1,613 | 508 | 101 | 272 | 67 | 64 |
| Arkansas | 411 | 1,422 | 962 | 281 | 53 | 64 | 40 | 22 |
| Florida | 2,519 | 12,484 | 6,438 | 3,674 | 547 | 801 | 542 | 482 |
| Georgia | 793 | 3,549 | 2,187 | 698 | 143 | 348 | 94 | 79 |
| Kentucky | 565 | 2,143 | 1,376 | 472 | 86 | 115 | 45 | 50 |
| Louisiana | 562 | 2,730 | 1,749 | 497 | 113 | 303 | 55 | 13 |
| Mississippi | 384 | 1,367 | 839 | 264 | 59 | 166 | 25 | 14 |
| North Carolina | 973 | 3,553 | 2,252 | 784 | 162 | 210 | 55 | 89 |
| South Carolina | 482 | 1,541 | 978 | 290 | 77 | 110 | 50 | 36 |
| Tennessee | 739 | 3,549 | 2,107 | 618 | 100 | 528 | 113 | 82 |
| Virginia | 781 | 2,736 | 1,817 | 609 | 101 | 101 | 52 | 55 |
| West Virginia | 322 | 1,106 | 756 | 247 | 33 | 37 | 17 | 15 |
| Southwest | 3,211 | 13,271 | 8,318 | 2,888 | 541 | 949 | 307 | 268 |
| Arizona | 561 | 2,276 | 1,298 | 664 | 99 | 94 | 44 | 78 |
| New Mexico | 199 | 565 | 354 | 130 | 23 | 29 | 13 | 16 |
| Oklahoma | 474 | 1,665 | 1,108 | 317 | 49 | 146 | 30 | 16 |
| Texas | 1,977 | 8,765 | 5,558 | 1,777 | 371 | 681 | 220 | 158 |
| Rocky Mountains | 898 | 3,104 | 2,042 | 615 | 82 | 156 | 87 | 123 |
| Colorado | 396 | 1,556 | 1,013 | 319 | 49 | 63 | 50 | 61 |
| Idaho | 143 | 384 | 257 | 73 | 10 | 17 | 8 | 19 |
| Montana | 125 | 391 | 271 | 78 | 8 | 13 | 9 | 11 |
| Utah | 177 | 624 | 399 | 119 | 13 | 55 | 13 | 26 |
| Wyoming | 57 | 150 | 101 | 25 | 3 | 9 | 6 | 5 |
| Far West | 4,955 | 22,558 | 13,044 | 6,437 | 824 | 940 | 389 | 924 |
| Alaska | 30 | 101 | 76 | 17 | 3 | 2 | 2 | 1 |
| California | 3,499 | 17,347 | 9,895 | 5,093 | 641 | 735 | 292 | 691 |
| Hawaii | 141 | 496 | 306 | 156 | 11 | 12 | 6 | 6 |
| Nevada | 172 | 732 | 411 | 215 | 22 | 44 | 18 | 22 |
| Oregon | 454 | 1,521 | 932 | 392 | 50 | 50 | 27 | 70 |
| Washington | 659 | 2,360 | 1,425 | 563 | 97 | 97 | 44 | 134 |
Number of aged and disabled persons enrolled in the Hospital and/or Supplementary Medical Insurance programs as of July 1, 1993, by State of residence. U.S. total includes enrollees with unknown State of residence.
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 25. Medicaid Recipients and Expenditures for Personal Health Care, by Type of Service, by Region and State: 1993.
| Region and State | Number of Medicaid Recipients1 (Thousands) |
Total Personal Health Care | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Prescription Drugs | Nursing Home Care | Other Personal Health Care |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Millions of Dollars | ||||||||||
| United States | 32,664 | 112,776 | 46,108 | 12,471 | 1,541 | 1,320 | 3,166 | 7,647 | 32,427 | 8,096 |
| New England | 1,618 | 7,880 | 2,431 | 555 | 72 | 35 | 276 | 419 | 3,139 | 953 |
| Connecticut | 334 | 1,998 | 546 | 102 | 13 | 10 | 64 | 97 | 929 | 238 |
| Maine | 169 | 722 | 204 | 54 | 6 | 6 | 14 | 50 | 284 | 104 |
| Massachusetts | 765 | 3,689 | 1,308 | 297 | 40 | 13 | 187 | 195 | 1,354 | 294 |
| New Hampshire | 79 | 446 | 85 | 57 | 4 | 3 | 4 | 26 | 173 | 93 |
| Rhode Island | 191 | 793 | 240 | 16 | 4 | 2 | 3 | 31 | 327 | 170 |
| Vermont | 81 | 232 | 48 | 28 | 4 | 1 | 4 | 19 | 72 | 54 |
| Mideast | 5,393 | 29,865 | 12,320 | 2,090 | 177 | 544 | 1,803 | 1,525 | 9,776 | 1,631 |
| Delaware | 69 | 249 | 84 | 17 | 1 | 2 | 10 | 13 | 83 | 40 |
| District of Columbia | 120 | 678 | 337 | 67 | 2 | 2 | 18 | 23 | 213 | 17 |
| Maryland | 445 | 1,924 | 935 | 227 | 4 | 2 | 47 | 110 | 473 | 126 |
| New Jersey | 794 | 3,857 | 1,719 | 198 | 35 | 11 | 107 | 262 | 1,266 | 260 |
| New York | 2,742 | 18,041 | 7,298 | 1,273 | 103 | 512 | 1,587 | 709 | 5,701 | 859 |
| Pennsylvania | 1,223 | 5,116 | 1,948 | 308 | 33 | 16 | 35 | 408 | 2,040 | 328 |
| Great Lakes | 5,094 | 18,054 | 7,244 | 1,900 | 167 | 158 | 315 | 1,276 | 5,873 | 1,120 |
| Illinois | 1,396 | 4,609 | 2,165 | 347 | 36 | 35 | 8 | 299 | 1,431 | 289 |
| Indiana | 565 | 2,777 | 1,024 | 384 | 35 | 38 | 34 | 229 | 937 | 95 |
| Michigan | 1,172 | 3,865 | 1,559 | 555 | 41 | 16 | 173 | 227 | 1,023 | 271 |
| Ohio | 1,491 | 4,665 | 1,967 | 430 | 40 | 54 | 23 | 333 | 1,639 | 178 |
| Wisconsin | 471 | 2,138 | 529 | 183 | 16 | 15 | 77 | 188 | 843 | 286 |
| Plains | 1,863 | 6,700 | 2,429 | 615 | 83 | 54 | 136 | 491 | 2,293 | 599 |
| Iowa | 289 | 960 | 392 | 106 | 21 | 9 | 14 | 78 | 304 | 37 |
| Kansas | 243 | 769 | 289 | 93 | 8 | 5 | 8 | 55 | 246 | 64 |
| Minnesota | 425 | 2,229 | 758 | 171 | 25 | 22 | 91 | 112 | 821 | 228 |
| Missouri | 609 | 1,648 | 640 | 116 | 15 | 9 | 16 | 176 | 517 | 160 |
| Nebraska | 165 | 561 | 188 | 73 | 8 | 4 | 6 | 44 | 191 | 48 |
| North Dakota | 62 | 269 | 86 | 26 | 4 | 3 | 1 | 13 | 106 | 31 |
| South Dakota | 70 | 264 | 76 | 30 | 3 | 2 | 1 | 14 | 109 | 30 |
| Southeast | 8,635 | 23,891 | 9,188 | 3,815 | 306 | 183 | 371 | 1,965 | 6,361 | 1,700 |
| Alabama | 522 | 1,276 | 393 | 157 | 8 | 10 | 17 | 125 | 408 | 159 |
| Arkansas | 339 | 1,007 | 410 | 183 | 7 | 8 | 32 | 65 | 245 | 56 |
| Florida | 1,745 | 4,697 | 1,875 | 631 | 46 | 55 | 73 | 414 | 1,217 | 387 |
| Georgia | 955 | 2,753 | 1,153 | 478 | 32 | 29 | 33 | 212 | 633 | 183 |
| Kentucky | 618 | 1,683 | 590 | 361 | 40 | 20 | 47 | 163 | 369 | 94 |
| Louisiana | 751 | 2,664 | 1,077 | 323 | 23 | 0 | 17 | 196 | 832 | 195 |
| Mississippi | 504 | 1,043 | 449 | 173 | 2 | 1 | 7 | 115 | 249 | 47 |
| North Carolina | 898 | 2,564 | 954 | 382 | 37 | 18 | 76 | 163 | 806 | 130 |
| South Carolina | 470 | 1,324 | 495 | 210 | 13 | 8 | 7 | 91 | 358 | 142 |
| Tennessee | 909 | 2,183 | 858 | 404 | 23 | 12 | 15 | 193 | 612 | 66 |
| Virginia | 576 | 1,621 | 643 | 242 | 12 | 9 | 6 | 155 | 429 | 125 |
| West Virginia | 347 | 1,075 | 292 | 271 | 62 | 14 | 42 | 74 | 202 | 117 |
| Southwest | 3,340 | 8,775 | 4,044 | 1,043 | 77 | 102 | 186 | 491 | 1,987 | 845 |
| Arizona | 404 | 1,270 | 1,035 | 171 | 1 | 2 | 3 | 7 | 8 | 44 |
| New Mexico | 241 | 577 | 259 | 89 | 6 | 27 | 4 | 31 | 103 | 58 |
| Oklahoma | 387 | 1,013 | 350 | 101 | 8 | 7 | 20 | 75 | 362 | 90 |
| Texas | 2,308 | 5,914 | 2,401 | 683 | 62 | 66 | 159 | 378 | 1,513 | 652 |
| Rocky Mountains | 664 | 2,193 | 863 | 332 | 27 | 19 | 26 | 132 | 545 | 249 |
| Colorado | 281 | 967 | 426 | 144 | 5 | 1 | 6 | 51 | 213 | 120 |
| Idaho | 100 | 290 | 103 | 38 | 7 | 7 | 7 | 20 | 82 | 25 |
| Montana | 89 | 322 | 100 | 40 | 5 | 6 | 9 | 21 | 102 | 40 |
| Utah | 148 | 477 | 179 | 90 | 7 | 5 | 3 | 32 | 116 | 45 |
| Wyoming | 46 | 137 | 54 | 20 | 2 | 0 | 1 | 8 | 32 | 19 |
| Far West | 6,056 | 15,418 | 7,589 | 2,120 | 632 | 224 | 52 | 1,348 | 2,453 | 999 |
| Alaska | 65 | 273 | 125 | 56 | 8 | 2 | 1 | 12 | 48 | 21 |
| California | 4,834 | 11,330 | 6,300 | 1,503 | 555 | 143 | 15 | 1,096 | 1,316 | 402 |
| Hawaii | 110 | 354 | 141 | 49 | 10 | 3 | 1 | 25 | 99 | 27 |
| Nevada | 88 | 344 | 143 | 52 | 7 | 5 | 6 | 13 | 97 | 21 |
| Oregon | 325 | 955 | 243 | 87 | 7 | 3 | 8 | 72 | 239 | 297 |
| Washington | 633 | 2,161 | 638 | 373 | 46 | 69 | 21 | 130 | 654 | 231 |
Medicaid recipient data from the Health Care Financing Administration, Medicaid Bureau, as reported on HCFA Form-2082 for fiscal year 1993.
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 26. Medicare and Medicaid Personal Health Care Expenditures as a Share of Total Personal Health Care Expenditures, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 | |
|---|---|---|---|---|---|---|
|
| ||||||
| Percent | ||||||
| United States | 28.2 | 29.1 | 29.7 | 32.8 | 33.8 | |
| New England | 31.8 | 31.5 | 32.0 | 35.8 | 35.2 | |
| Connecticut | 27.3 | 27.8 | 28.3 | 32.7 | 33.8 | |
| Maine | 35.0 | 34.4 | 33.0 | 37.6 | 38.6 | |
| Massachusetts | 33.5 | 33.7 | 34.8 | 36.6 | 35.9 | |
| New Hampshire | 26.9 | 23.8 | 23.4 | 35.2 | 26.6 | |
| Rhode Island | 34.6 | 34.5 | 34.8 | 42.1 | 42.5 | |
| Vermont | 33.6 | 28.6 | 27.7 | 32.0 | 31.6 | |
| Mideast | 33.4 | 34.9 | 34.7 | 37.8 | 38.7 | |
| Delaware | 23.9 | 22.8 | 23.7 | 26.5 | 27.7 | |
| District of Columbia | 26.7 | 27.9 | 26.3 | 28.9 | 29.9 | |
| Maryland | 24.4 | 24.9 | 27.2 | 30.1 | 30.5 | |
| New Jersey | 28.4 | 30.2 | 29.3 | 33.1 | 33.8 | |
| New York | 39.0 | 40.7 | 40.5 | 43.2 | 44.6 | |
| Pennsylvania | 30.7 | 33.1 | 32.5 | 36.1 | 36.5 | |
| Great Lakes | 28.0 | 29.5 | 29.2 | 32.2 | 32.9 | |
| Illinois | 28.3 | 29.0 | 26.1 | 30.6 | 31.7 | |
| Indiana | 23.5 | 28.2 | 29.9 | 34.4 | 36.0 | |
| Michigan | 31.1 | 31.1 | 31.2 | 32.8 | 34.2 | |
| Ohio | 24.7 | 27.8 | 30.0 | 32.8 | 32.4 | |
| Wisconsin | 32.8 | 32.6 | 29.7 | 30.8 | 31.3 | |
| Plains | 27.6 | 28.7 | 28.6 | 31.0 | 31.4 | |
| Iowa | 27.0 | 29.1 | 29.7 | 31.8 | 32.8 | |
| Kansas | 25.9 | 25.9 | 27.0 | 28.8 | 30.4 | |
| Minnesota | 30.5 | 29.8 | 28.1 | 29.9 | 31.0 | |
| Missouri | 27.4 | 29.8 | 29.2 | 33.0 | 31.9 | |
| Nebraska | 24.2 | 24.5 | 26.1 | 28.5 | 29.7 | |
| North Dakota | 26.4 | 29.4 | 31.2 | 31.4 | 31.8 | |
| South Dakota | 26.5 | 28.5 | 29.8 | 31.6 | 32.1 | |
| Southeast | 26.7 | 28.2 | 30.2 | 33.9 | 35.2 | |
| Alabama | 26.0 | 27.2 | 28.5 | 31.7 | 32.3 | |
| Arkansas | 32.9 | 34.4 | 34.7 | 39.4 | 39.7 | |
| Florida | 28.9 | 30.4 | 32.2 | 35.8 | 38.3 | |
| Georgia | 24.6 | 24.9 | 25.6 | 29.7 | 31.3 | |
| Kentucky | 27.5 | 29.5 | 33.6 | 36.3 | 36.8 | |
| Louisiana | 25.7 | 29.5 | 34.6 | 39.6 | 41.4 | |
| Mississippi | 29.0 | 29.2 | 34.2 | 39.0 | 39.0 | |
| North Carolina | 26.6 | 28.8 | 28.9 | 32.7 | 33.5 | |
| South Carolina | 26.7 | 26.1 | 28.7 | 31.0 | 31.7 | |
| Tennessee | 26.6 | 28.7 | 31.9 | 35.0 | 35.4 | |
| Virginia | 22.9 | 22.5 | 22.9 | 25.4 | 26.1 | |
| West Virginia | 23.8 | 27.8 | 32.4 | 41.1 | 42.0 | |
| Southwest | 22.6 | 23.4 | 26.0 | 29.6 | 30.5 | |
| Arizona | 17.3 | 22.4 | 27.0 | 33.6 | 33.3 | |
| New Mexico | 22.1 | 24.1 | 25.6 | 28.6 | 29.4 | |
| Oklahoma | 28.1 | 28.2 | 30.7 | 33.6 | 33.3 | |
| Texas | 22.6 | 22.7 | 25.0 | 28.2 | 29.5 | |
| Rocky Mountains | 20.3 | 21.0 | 22.9 | 25.3 | 27.1 | |
| Colorado | 19.9 | 19.6 | 21.4 | 22.9 | 25.1 | |
| Idaho | 21.9 | 23.4 | 24.8 | 29.1 | 29.6 | |
| Montana | 25.7 | 26.5 | 29.7 | 32.3 | 33.9 | |
| Utah | 18.6 | 21.4 | 22.3 | 25.2 | 26.7 | |
| Wyoming | 15.4 | 17.1 | 22.4 | 27.4 | 28.7 | |
| Far West | 26.7 | 26.2 | 26.1 | 28.3 | 30.1 | |
| Alaska | 12.6 | 12.1 | 18.3 | 20.9 | 23.8 | |
| California | 27.9 | 27.0 | 26.2 | 28.4 | 30.4 | |
| Hawaii | 21.4 | 20.4 | 20.6 | 22.4 | 24.4 | |
| Nevada | 22.1 | 22.6 | 23.5 | 26.9 | 28.7 | |
| Oregon | 24.4 | 25.4 | 27.2 | 29.7 | 31.0 | |
| Washington | 23.6 | 25.0 | 27.2 | 29.3 | 29.9 | |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Table 27. Medicare Personal Health Care Expenditures as a Share of Total Personal Health Care Expenditures, by Region and State: Selected Calendar Years 1980-93.
| Region and State of Provider | 1980 | 1985 | 1990 | 1992 | 1993 |
|---|---|---|---|---|---|
|
| |||||
| Percent | |||||
| United States | 16.7 | 18.7 | 17.9 | 18.5 | 19.3 |
| New England | 17.1 | 18.6 | 16.1 | 17.6 | 18.6 |
| Connecticut | 16.3 | 16.6 | 15.5 | 16.7 | 17.5 |
| Maine | 19.0 | 18.9 | 16.4 | 16.7 | 17.6 |
| Massachusetts | 17.2 | 20.0 | 16.7 | 18.7 | 20.1 |
| New Hampshire | 16.2 | 15.0 | 13.0 | 14.0 | 13.7 |
| Rhode Island | 18.2 | 19.4 | 17.2 | 19.0 | 19.4 |
| Vermont | 17.9 | 15.8 | 14.2 | 15.8 | 16.1 |
| Mideast | 17.1 | 19.5 | 18.5 | 18.7 | 19.5 |
| Delaware | 15.5 | 15.5 | 15.7 | 16.0 | 16.7 |
| District of Columbia | 14.9 | 14.6 | 14.5 | 14.1 | 14.1 |
| Maryland | 13.6 | 15.8 | 17.1 | 17.4 | 17.8 |
| New Jersey | 16.6 | 20.1 | 16.9 | 18.3 | 18.8 |
| New York | 16.7 | 17.8 | 17.1 | 16.9 | 17.7 |
| Pennsylvania | 19.7 | 23.8 | 22.7 | 22.8 | 24.2 |
| Great Lakes | 16.8 | 18.7 | 17.7 | 18.1 | 18.6 |
| Illinois | 17.2 | 19.7 | 17.4 | 17.8 | 18.4 |
| Indiana | 14.9 | 18.2 | 17.8 | 18.6 | 19.1 |
| Michigan | 18.3 | 19.7 | 18.8 | 18.9 | 19.9 |
| Ohio | 16.1 | 17.3 | 17.6 | 18.3 | 18.5 |
| Wisconsin | 15.8 | 18.1 | 16.5 | 16.0 | 16.5 |
| Plains | 18.0 | 19.2 | 18.0 | 18.3 | 18.7 |
| Iowa | 17.6 | 19.7 | 18.9 | 18.8 | 19.7 |
| Kansas | 17.2 | 18.4 | 17.9 | 18.4 | 19.2 |
| Minnesota | 16.0 | 15.8 | 15.2 | 15.3 | 15.2 |
| Missouri | 20.9 | 23.1 | 20.6 | 21.0 | 21.6 |
| Nebraska | 16.5 | 17.0 | 16.6 | 16.6 | 17.0 |
| North Dakota | 18.3 | 18.7 | 18.8 | 18.3 | 18.5 |
| South Dakota | 16.1 | 18.6 | 18.2 | 18.4 | 18.6 |
| Southeast | 17.6 | 20.0 | 19.8 | 21.0 | 21.8 |
| Alabama | 16.7 | 19.2 | 19.6 | 21.0 | 21.8 |
| Arkansas | 18.7 | 21.8 | 22.0 | 23.4 | 23.3 |
| Florida | 24.7 | 25.6 | 24.8 | 26.1 | 27.9 |
| Georgia | 14.0 | 15.8 | 15.2 | 17.4 | 17.7 |
| Kentucky | 15.6 | 18.0 | 19.7 | 19.7 | 20.6 |
| Louisiana | 13.9 | 18.0 | 19.8 | 20.3 | 21.0 |
| Mississippi | 16.4 | 19.5 | 20.8 | 22.0 | 22.1 |
| North Carolina | 16.4 | 19.5 | 17.4 | 19.1 | 19.5 |
| South Carolina | 14.1 | 16.6 | 14.9 | 16.1 | 17.1 |
| Tennessee | 17.1 | 20.1 | 19.8 | 20.9 | 21.9 |
| Virginia | 14.2 | 15.3 | 15.0 | 15.9 | 16.4 |
| West Virginia | 16.8 | 20.9 | 21.1 | 21.8 | 21.3 |
| Southwest | 15.2 | 16.7 | 17.2 | 17.7 | 18.3 |
| Arizona | 17.3 | 20.3 | 20.3 | 21.6 | 21.4 |
| New Mexico | 13.9 | 15.5 | 15.3 | 14.4 | 14.6 |
| Oklahoma | 16.9 | 17.6 | 19.2 | 20.2 | 20.7 |
| Texas | 14.6 | 15.8 | 16.3 | 16.7 | 17.6 |
| Rocky Mountains | 12.7 | 14.1 | 14.3 | 14.9 | 15.9 |
| Colorado | 12.9 | 13.5 | 14.0 | 14.5 | 15.5 |
| Idaho | 13.6 | 16.4 | 14.9 | 16.2 | 16.9 |
| Montana | 14.7 | 16.5 | 17.4 | 17.9 | 18.6 |
| Utah | 11.1 | 13.5 | 13.3 | 13.9 | 15.2 |
| Wyoming | 10.9 | 12.1 | 13.4 | 14.0 | 15.0 |
| Far West | 15.8 | 17.5 | 16.6 | 16.9 | 17.9 |
| Alaska | 3.7 | 4.3 | 5.7 | 6.3 | 6.4 |
| California | 16.4 | 18.1 | 16.9 | 17.2 | 18.4 |
| Hawaii | 10.8 | 11.9 | 12.8 | 13.3 | 14.2 |
| Nevada | 16.2 | 18.1 | 18.0 | 17.4 | 19.5 |
| Oregon | 16.5 | 18.6 | 18.3 | 18.5 | 19.0 |
| Washington | 13.7 | 16.0 | 15.9 | 15.7 | 15.6 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Estimates prepared by the Office of National Health Statistics.
Acknowledgments
Estimates for the SHEA are prepared in the Office of National Health Statistics under the general direction of Daniel Waldo, Office Director, and Mark Freeland, Director of the Division of Health Cost Analysis. Other staff members were instrumental in the preparation of SHEA estimates: C. Sue Donham and Arthur Sensenig prepared estimates, Charles Fisher and David Gibson prepared tabulations and offered advice on Medicare program data, John Klemm provided guidance on Medicaid data, and Anna Long assembled this manuscript. Charles Helbing and Wilson Kirby of the Office of Research and Demonstrations also contributed to this effort by preparing special tabulations of Medicare data.
Footnotes
The authors are with the Office of the Actuary, Health Care Financing Administration (HCFA). The opinions expressed are those of the authors and do not necessarily reflect those of HCFA.
For example, spending estimates are presented for the District of Columbia, but many residents of Maryland and Virginia come to District of Columbia providers for health care services. Spending for District of Columbia residents is overstated in aggregate by this measure, and division by resident population would produce exaggerated per capita spending estimates.
Latest year for which GSP is available.
Under the Standard Industrial Classification, revenues received for physician services are captured under the category “offices and clinics of physicians.” These revenues include those billed and received for services delivered by physicians based within that establishment, including revenues received from affiliations with HMOs. Staff-model HMOs employ physicians and other medical personnel who deliver a wider variety of services than those provided in an office or clinic of physicians. The revenues received by staff-model HMOs for services delivered at those establishments are also included with expenditures for physician services.
HMOs include plans that offer prepaid comprehensive health coverage for both hospital and physician services, in which members are usually required to use participating providers, and in which members are enrolled for specific periods of time.
Additional long-term care services may be purchased in hospital-based nursing homes, hospital swing beds, and from hospital-based home health agencies. Expenditures for these services are counted with hospital expenditures.
Reprint Requests: Anna Long, Office of National Health Statistics, 7500 Security Boulevard, N-3-02-02, Baltimore, Maryland 21244-1850. Address requests for diskette copy of State health expenditure accounts to the same address. Enclose one blank formatted diskette.
References
- Actuarial Research Corporation. National Health Accounts Drug Study. Annandale, VA.: 1994. Health Care Financing Administration Contract Number 500-94-0004. [Google Scholar]
- Agency for Health Care Policy and Research. Rockville, MD.: 1987. Data from the National Medical Expenditures Survey. Unpublished. [Google Scholar]
- American Dental Association. Distribution of Dentists in the United States by Region and State, 1991. Chicago: Feb, 1993. [Google Scholar]
- American Hospital Association. Hospital Statistics. Chicago: 1993. [Google Scholar]
- American Nurses' Association. Inventory of Registered Nurses for 1977-78. Kansas City: 1979. [Google Scholar]
- Beemiller RM, Dunbar AE. Survey of Current Business. 8. Vol. 74. Washington: U.S. Government Printing Office; Aug, 1994. Gross State Product, 1977-91; pp. 80–97. [Google Scholar]
- Emmons DW, Simon CJ. Socioeconomic Characteristics of Medical Practice 1994. Chicago: American Medical Association; 1994. Recent Trends in Managed Care. [Google Scholar]
- Executive Office of the President. Standard Industrial Classification Manual, 1987. Washington: U.S. Government Printing Office; 1987. [Google Scholar]
- Harrington C, Swan JH, Grant LA. Nursing Home Bed Capacity in the States, 1978-86. Health Care Financing Review. 1988 Fall;10(1):33–53. [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Estes CL. Health Policy and Nursing: Crisis and Reform in the US Health Care Delivery System. Boston: Jones and Bartlett; 1994. [Google Scholar]
- Helbing C, Sangl JA, Silverman HA. Home Health Agency Benefits. Health Care Financing Review 1992 Annual Supplement. 1993 Oct;:125–148. [PubMed] [Google Scholar]
- InterStudy. The Competitive Edge. Excelsior, MN.: 1991-95. [Google Scholar]
- InterStudy. Managed Care: A Decade in Review 1980-1990. Excelsior, MN.: 1991. [Google Scholar]
- Kenney GM. Rural and Urban Differentials in Medicare Home Health Use. Health Care Financing Review. 1993 Summer;14(4):39–57. [PMC free article] [PubMed] [Google Scholar]
- Lazenby HC, Levit KR, Waldo DR, et al. National Health Accounts: Lessons From the U.S. Experience. Health Care Financing Review. 1992 Summer;13(4):89–104. [PMC free article] [PubMed] [Google Scholar]
- Levit KR. Personal Health Care Expenditures, by State: 1966-82. Health Care Financing Review. 1985 Summer;6(4):1–49. [PMC free article] [PubMed] [Google Scholar]
- Levit KR, Lazenby HC, Cowan CA, et al. Health Spending by State: New Estimates for Policy Making. Health Affairs. 1993 Fall;12(3):7–26. doi: 10.1377/hlthaff.12.3.7. [DOI] [PubMed] [Google Scholar]
- Levit KR, Sensenig AL, Cowan CA, et al. National Health Expenditures, 1993. Health Care Financing Review. 1994 Fall;16(1):247–294. [PMC free article] [PubMed] [Google Scholar]
- Lewin-VHI Inc. The States as Payers: Managed Care for Medicaid Populations. Feb, 1995. Prepared for the National Institute for Health Care Management. [Google Scholar]
- Prospective Payment Assessment Commission. Medicare and the American Health Care System: Report to Congress. Washington: Prospective Payment Assessment Commission; Jun, 1995. [Google Scholar]
- U.S. Bureau of the Census. Census of Service Industries. Washington: U.S. Government Printing Office; 1977, 1982, 1987, 1992. [Google Scholar]
- U.S. Bureau of the Census. Texas Now Second Largest State, Nevada Fastest Growing, District of Columbia Fastest Loser, Census Bureau Says, CB94-204 1990-93. Washington: U.S. Department of Commerce; Dec, 1994. Press Release. [Google Scholar]
- U.S. Bureau of the Census. Census of Retail Trade, Merchandise Line Sales Report. Washington: U.S. Government Printing Office; 1977, 1982, 1987. [Google Scholar]
- U.S. Bureau of Economic Analysis. Survey of Current Business. 8. Vol. 74. Washington: U.S. Government Printing Office; Aug, 1994. State Personal Income, Revised Estimates for 1991-93; pp. 64–79. [Google Scholar]
- U.S. Bureau of Economic Analysis. Wage and Salary Disbursements. Washington: U.S. Department of Commerce; 1969-93. Unpublished. [Google Scholar]
- U.S. Bureau of Labor Statistics. Employment and Wages Annual Averages, 1993. Washington: U.S. Government Printing Office; 1994. [Google Scholar]
- U.S. Internal Revenue Service. Business Master File. Washington: U.S. Department of the Treasury; 1977-92. Unpublished. [Google Scholar]
- U.S. Public Health Service. The Registered Nurse Population, National Sample Survey of Registered Nurses, 1984 and 1992. Washington: U.S. Government Printing Office; 1986, 1994. [Google Scholar]
- Vladeck BC, Miller NA. The Medicare Home Health Initiative. Health Care Financing Review. 1994 Fall;16(1):7–16. [PMC free article] [PubMed] [Google Scholar]
- Waldo DR, Sonnefeld ST, McKusick DR, Arnett RH. Health Expenditures by Age Group, 1977 and 1987. Health Care Financing Review. 1989 Summer;10(4):111–120. [PMC free article] [PubMed] [Google Scholar]