Abstract
This article presents data on health care spending for the United States, covering expenditures for various types of medical services and products and their sources of funding from 1960 to 1994. Although these statistics for 1994 show the slowest growth in more than three decades, health spending continued to grow faster than the overall economy. The Federal Government continued to fund an increasing share of health care expenditures in 1994, offset by a falling share from out-of-pocket sources. Shares paid by State and local governments and by other private payers including private health insurance remained unchanged from 1993.
1994 health spending at a glance
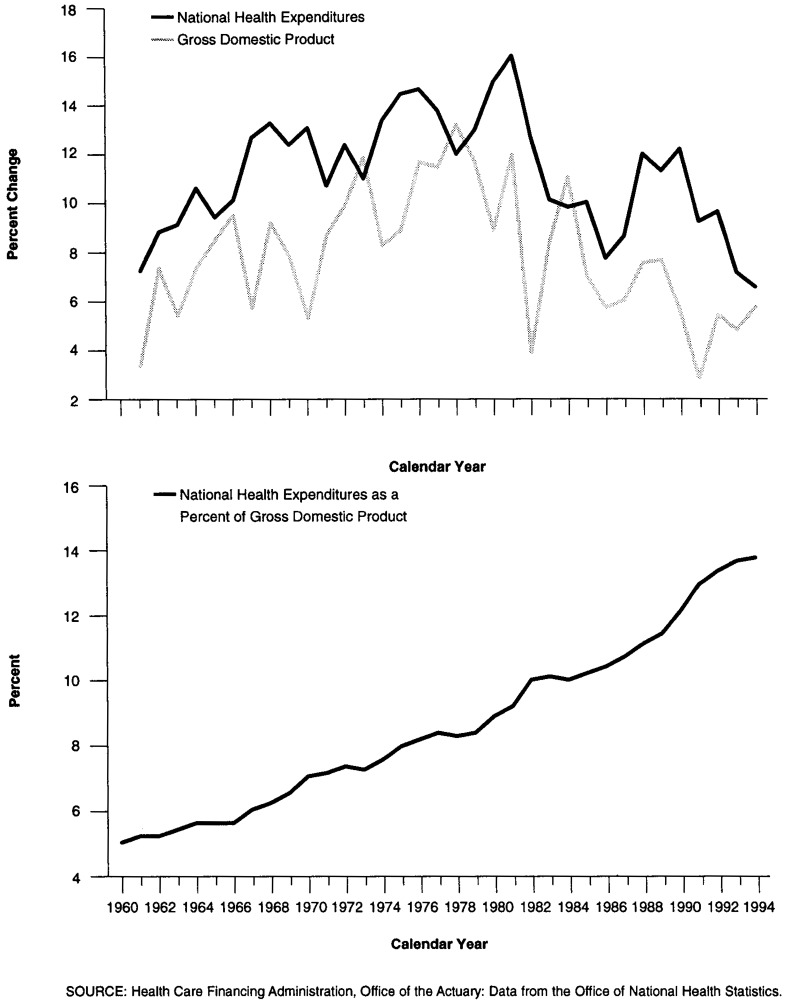
National health expenditures (NHE) reached $949.4 billion in 1994. The 6.4-percent increase in 1994 marked the slowest growth rate recorded in more than three decades. Slower-than-average growth in health spending, combined with healthy growth in the gross domestic product (GDP), led to only a small increase in health care spending as a share of GDP; from 13.6 percent in 1993 to 13.7 percent in 19941 (Figure 1).
Figure 1. Percent Growth in National Health Expenditures and Gross Domestic Product, and National Health Expenditures as a Percent of Gross Domestic Product: Calendar Years 1960-94.
The public share of health spending rose from 43.4 percent in 1993 to 44.3 percent in 1994, the highest level recorded in the NHE time series. Medicare's share was 17.8 percent of NHE in 1994, and Medicaid's share (including State funds) was 13.6 percent. Together, spending by HCFA programs represented more than 70 percent of all public funding for health care.
Growth in private health expenditures (including private health insurance premiums and out-of-pocket spending) dipped to 4.7 percent, about one-half the 8.7-percent spending growth registered by the public sector. Private sector insurance, sponsored principally through employers, has been increasingly dominated by managed-care plans. These plans achieved cost savings through negotiated price discounts with providers and the use of gatekeepers to control utilization, while maintaining relatively little change in privately paid out-of-pocket deductibles and copayments for services delivered.
The temptation is to use aggregate figures to infer that Medicare is less able than private health insurance to control costs. From 1969 to 1993, growth in Medicare and private health insurance benefits was comparable, increasing at average annual rates of 13.7 and 13.4 percent, respectively. In 1994 however, growth in spending diverged dramatically: Medicare spending grew 11.8 percent, almost 3 times the 4.0-percent growth experienced by private health insurance. But aggregate figures mask important underlying factors. Differences in services covered by the two insurers and differences in enrollment growth contributed to this differential. In addition, Medicare volume performance standards (MVPS), set up to slow Medicare growth, paid bonuses to physicians in 1994 for restraint in volume growth exhibited in 1992; MVPS will also extract a penalty from physicians in 1996 for volume growth above the 1994 target These factors have little to do with insurer performance. However, they are responsible for one-half of Medicare's 1994 growth.
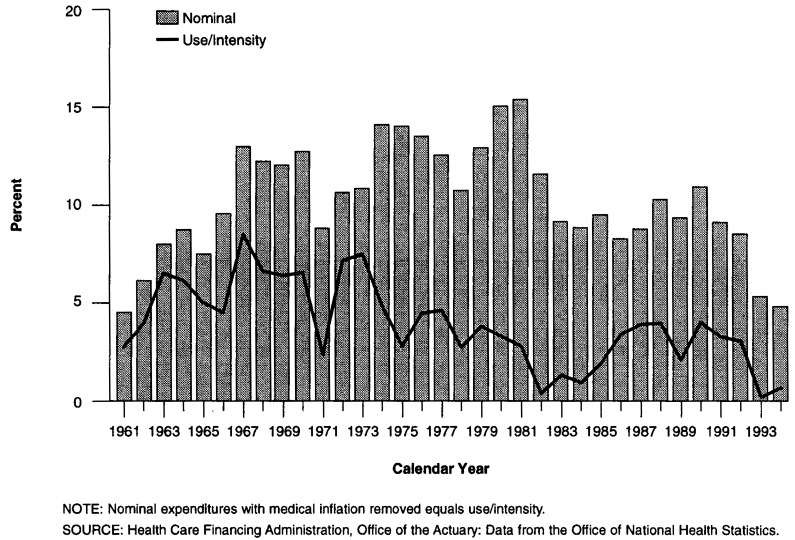
Personal health care expenditures (PHCE) grew 6.3 percent in 1993 and 5.7 percent in 1994 (Table 1). After removing the effects of medical price inflation and population growth, the quantity and intensity of personal health care per person increased only 0.5 percent in 1993 and 0.9 percent in 1994, among the slowest growth years recorded since 1960 (Figure 2). Slow growth suggests that insurer incentives at work within the health care system constrained the use of services.
Table 1. Personal Health Care Expenditures in Current and Constant Dollars and Associated Price Indexes, by Type of Expenditure: Selected Years 1960-94.
| Type of Expenditure | 1960 | 1970 | 1975 | 1980 | 1985 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|---|---|
| Current Dollars in Billions | ||||||||||
| Personal Health Care | $23.6 | $63.8 | $114.5 | $217.0 | $376.4 | $614.7 | $676.2 | $739.8 | $786.5 | $831.7 |
| Hospital Care | 9.3 | 28.0 | 52.6 | 102.7 | 168.3 | 256.4 | 282.3 | 305.3 | 324.2 | 338.5 |
| Physician Services | 5.3 | 13.6 | 23.9 | 45.2 | 83.6 | 146.3 | 158.6 | 174.7 | 181.1 | 189.4 |
| Dental Services | 2.0 | 4.7 | 8.0 | 13.3 | 21.7 | 31.6 | 33.3 | 37.0 | 39.2 | 42.2 |
| Other Professional Services and Home Health Care | 0.7 | 1.6 | 3.4 | 8.7 | 22.3 | 47.8 | 54.3 | 61.7 | 69.3 | 75.8 |
| Drugs and Other Medical Non-Durables | 4.2 | 8.8 | 13.0 | 21.6 | 37.1 | 59.9 | 65.6 | 71.3 | 75.2 | 78.6 |
| Vision Products and Other Medical Durables | 0.6 | 1.6 | 2.5 | 3.8 | 6.7 | 10.5 | 11.2 | 11.9 | 12.6 | 13.1 |
| Nursing Home Care | 0.8 | 4.2 | 8.7 | 17.6 | 30.7 | 50.9 | 57.2 | 62.3 | 67.0 | 72.3 |
| Other Personal Health Care | 0.7 | 1.3 | 2.5 | 4.0 | 6.1 | 11.2 | 13.6 | 15.6 | 17.8 | 21.8 |
| Price Indexes1 | ||||||||||
| Hospital Care | 11.60 | 19.32 | 28.42 | 44.27 | 71.74 | 91.40 | 95.79 | 100.00 | 104.50 | 108.26 |
| Physician Services | 12.06 | 19.02 | 26.54 | 42.20 | 62.49 | 88.75 | 94.07 | 100.00 | 105.60 | 110.25 |
| Dental Services | 15.09 | 21.93 | 29.76 | 44.15 | 63.95 | 87.18 | 93.72 | 100.00 | 105.30 | 110.35 |
| Other Professional Services and Home Health Care | 13.51 | 21.05 | 28.93 | 44.32 | 64.65 | 88.75 | 94.25 | 100.00 | 105.10 | 109.62 |
| Drugs and Other Medical Non-Durables | 24.90 | 24.66 | 28.31 | 40.06 | 61.17 | 86.86 | 93.98 | 100.00 | 103.70 | 106.71 |
| Vision Products and Other Medical Durables | 22.41 | 29.89 | 39.40 | 55.81 | 75.06 | 92.46 | 96.06 | 100.00 | 102.70 | 104.75 |
| Nursing Home Care | 15.35 | 24.62 | 34.77 | 52.20 | 71.78 | 91.57 | 96.04 | 100.00 | 104.12 | 107.87 |
| Other Personal Health Care | 11.71 | 17.86 | 24.97 | 39.38 | 59.70 | 85.66 | 93.11 | 100.00 | 106.00 | 111.09 |
| Constant (1992) Dollars in Billions | ||||||||||
| Personal Health Care | $173.1 | $310.9 | $400.7 | $493.8 | $559.3 | $684.5 | $712.2 | $739.8 | $750.9 | $764.6 |
| Hospital Care | 80.0 | 144.9 | 185.0 | 232.0 | 234.6 | 280.6 | 294.7 | 305.3 | 310.3 | 312.7 |
| Physician Services | 43.8 | 71.4 | 90.1 | 107.2 | 133.8 | 164.9 | 168.6 | 174.7 | 171.5 | 171.8 |
| Dental Services | 13.0 | 21.3 | 26.7 | 30.2 | 33.9 | 36.2 | 35.6 | 37.0 | 37.3 | 38.2 |
| Other Professional Services and Home Health Care | 4.9 | 7.7 | 11.6 | 19.7 | 34.5 | 53.8 | 57.6 | 61.7 | 65.9 | 69.1 |
| Drugs and Other Medical Non-Durables | 17.1 | 35.7 | 46.0 | 54.0 | 60.6 | 69.0 | 69.8 | 71.3 | 72.5 | 73.6 |
| Vision Products and Other Medical Durables | 2.9 | 5.4 | 6.5 | 6.8 | 9.0 | 11.3 | 11.6 | 11.9 | 12.2 | 12.5 |
| Nursing Home Care | 5.5 | 17.1 | 24.9 | 33.8 | 42.7 | 55.6 | 59.5 | 62.3 | 64.4 | 67.0 |
| Other Personal Health Care | 5.9 | 7.3 | 9.9 | 10.2 | 10.2 | 13.1 | 14.6 | 15.6 | 16.8 | 19.7 |
| Personal Health Care Price Indexes | ||||||||||
| Chain-Weighted Index | 13.89 | 20.55 | 28.56 | 43.87 | 67.34 | 89.81 | 94.95 | 100.00 | 104.74 | 108.77 |
| Fixed-Weight Index | 13.82 | 20.62 | 28.71 | 44.12 | 67.36 | 89.82 | 94.95 | 100.00 | 104.74 | 108.77 |
| Implicit Price Deflator | 13.65 | 20.53 | 28.58 | 43.95 | 67.31 | 89.79 | 94.95 | 100.00 | 104.74 | 108.77 |
| Growth from Previous Period | Average Annual Growth | |||||||||
| Based on Current Dollars | — | 10.5 | 12.4 | 13.6 | 11.6 | 10.3 | 10.0 | 9.4 | 6.3 | 5.7 |
| In Constant (1992) Dollars | — | 6.0 | 5.2 | 4.3 | 2.5 | 4.1 | 4.0 | 3.9 | 1.5 | 1.8 |
Each component of personal health care is deflated by a Laspeyres (fixed-weight) index, with a 1987 base year rescaled to 1992 to be consistent with the gross domestic product. Input prices from the Consumer Price Index (CPI) are used to deflate nominal expenditures for physician services, dental services, other professional services (including home health care), and vision products and other durable medical products. CPIs for medical care and medical care commodities are used as price proxies for other personal health care and other non-durables. Output or transaction prices measured historically by the Health Care Financing Administration's transaction price index and currently by the producer price index are used to deflate hospital care expenditures. The price proxy for nursing home care is the national nursing home input price index.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Figure 2. Growth in Nominal Expenditures and Use/Intensity of Personal Health Care per Capita: 1961-94.
Slowest Growth in Decades
NHE as a share of GDP measures the impact of health spending on the economy by quantifying the proportion of national resources devoted to health care. From 1960 to 1994, this measure grew from 5.1 to 13.7 percent. On average, this means that the economy sustained an increase in the share of expenditures devoted to health care of 0.2-0.3 percentage points per year. From 1988 to 1992, health care expenditures as a share of GDP grew at an average rate of more than 0.5 percentage points annually. This 5-year period was the only time since 1960 that an increase in the NHE share of GDP of more than 0.3 percentage points was sustained for 2 or more consecutive years. The enormous pressure that health care exerted on the Nation's economic resources provided a backdrop for the health reform debate of 1993-94. By the time the debate began in late 1993, this pressure had begun to subside, as the increase in the NHE share of GDP slowed to the average rate of 0.3 percentage points. In 1994, the share increased only 0.1 percentage point to 13.7 percent—the direct result of slowing health care and accelerating GDP growth rates.
After 5 years of double-digit and near-double-digit growth in aggregate health care spending from 1988 to 1992, growth slowed to 7.0 percent in 1993 and 6.4 percent in 1994. The 6.4-percent rate in 1994 was the slowest recorded in more than three decades.
One way to interpret the slow growth in health expenditures is with real or inflation-adjusted NHE. When economywide inflation2 is removed from NHE, the results measure the value of health care purchases in terms of the foregone opportunity to purchase other goods and services. In 1994, real NHE grew 4.0 percent, as additional purchases of health care were substituted for the purchase of other goods and services. However, this rate also matched the slowest real growth rates for health care spending recorded over the last three decades. The trend for 1993-94 shows that the runaway health care expenditures experienced for most of the 1988-92 period have subsided. However, history warns that a 2-year observation does not necessarily constitute the beginning of a long-run trend. Real growth rates identical to those measured for 1993 and 1994 were also recorded for 1978 and 1979 during the Voluntary Effort. During this period, the threat of explicit government cost controls provided incentives for the private sector to voluntarily exercise restraint on increases in hospital costs and physician fees. As the threat subsided, real growth escalated to higher levels. The threat of health care reform during 1993 and 1994 may be having a similar, possibly short-lived, effect (Aaron, 1994).
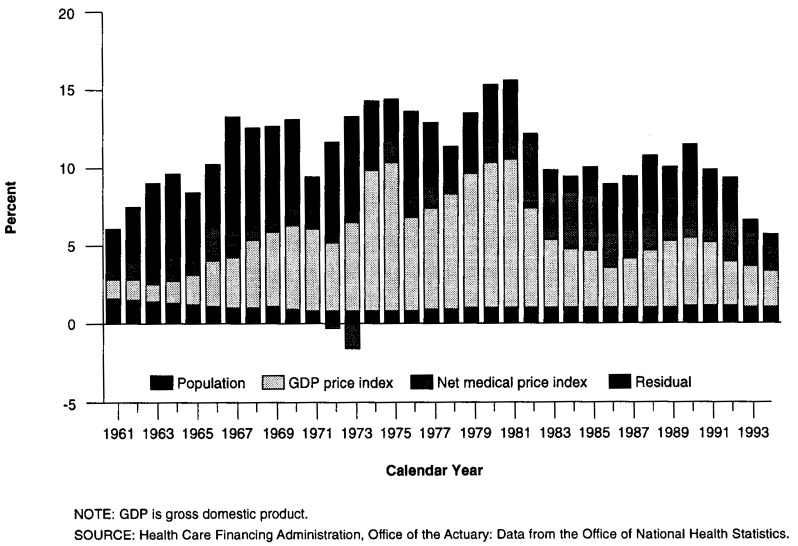
Spending for PHCE decelerated sharply in 1993 to 6.3 percent and less sharply again in 1994 to 5.7 percent. Growth in PHCE can be attributed to four factors: population growth, economywide inflation, medical inflation in excess of economywide inflation, and a residual (Figure 3). In 1994, population growth accounted for 17.5 percent of PHCE growth. Economywide inflation as measured by the GDP chain-type annual-weighted price index (Landefeld and Parker, 1995) accounted for 41.5 percent, and medical inflation above and beyond that recorded in economywide inflation accounted for 26.1 percent. The residual measures change in intensity per person, including quantity of services delivered, age/sex composition of the population, and technological developments. It also includes the net effect of any error in the measurement of medical prices or medical expenditures. In 1994, this residual accounted for 15.0 percent of PHCE growth. After removing the effects of general and medical price inflation and population growth, use and intensity of personal health care per person grew 0.5 percent in 1993 and 0.9 percent in 1994.3
Figure 3. Factors Accounting for Growth in Personal Health Care Expenditures: Calendar Years 1960-94.
Slow growth in personal health care use and intensity per person over the last 2 years suggests that insurer incentives at work within the health care system were successful in curbing utilization. Community hospital admission rates per capita for the population under 65 years of age continued to decline in 1993 and 1994, at rates of-1.5 and -0.8 percent, respectively. Admission declines were accompanied by declines in length of stay for the same age cohort (Sensenig, Heffler, and Donham, 1996). The mean number of hours worked by physicians in patient care activities has remained stable or declined since 1989 (American Medical Association, 1996), and the number of physician contacts per person remained unchanged from 1993 to 1994, following steady increases since 1988 (National Center for Health Statistics, 1996).
Despite slow nominal health expenditure growth overall, some categories of spending still exhibited double-digit increases. Spending for the PHCE category of other personal health care (dominated by Medicaid waivers) and for home health care services experienced double-digit increases (22.5 and 13.8 percent, respectively). Other spending for services grew modestly: Expenditures for hospital care; physician services; drugs and other non-durable medical products including prescription drugs; and durable medical products including vision products and hearing aids, all increased by less than 5 percent in 1994. Expenditures for dental services; other professional services such as those furnished by optometrists, chiropractors, and podiatrists; and nursing home care grew slightly faster, between 7 and 8 percent.
Medicare And Private Health Insurance—A Comparison
Comparing Unadjusted Growth Rates
Figures for 1994 show a striking break in the traditional relationship between growth in Medicare benefits and that in private health insurance benefits. Both payers encountered rapid benefit payment increases between 19694 and 1993 (at average annual rates of 13.7 percent for Medicare and 13.4 percent for private health insurance). But as previously mentioned, in 1994 growth patterns diverged: Spending for benefits increased 11.8 percent for Medicare but only 4.0 percent for private health insurance.
Although benefit growth rates in 1994 appear unusually far apart, it is important to understand the underlying reasons for differential growth. Certain factors tended to exaggerate the growth rate of Medicare benefits, especially in 1994. These factors include enrollment growth, benefit coverage, and government regulatory and policy effects. These have little to do with insurer performance in providing benefits to enrollees.
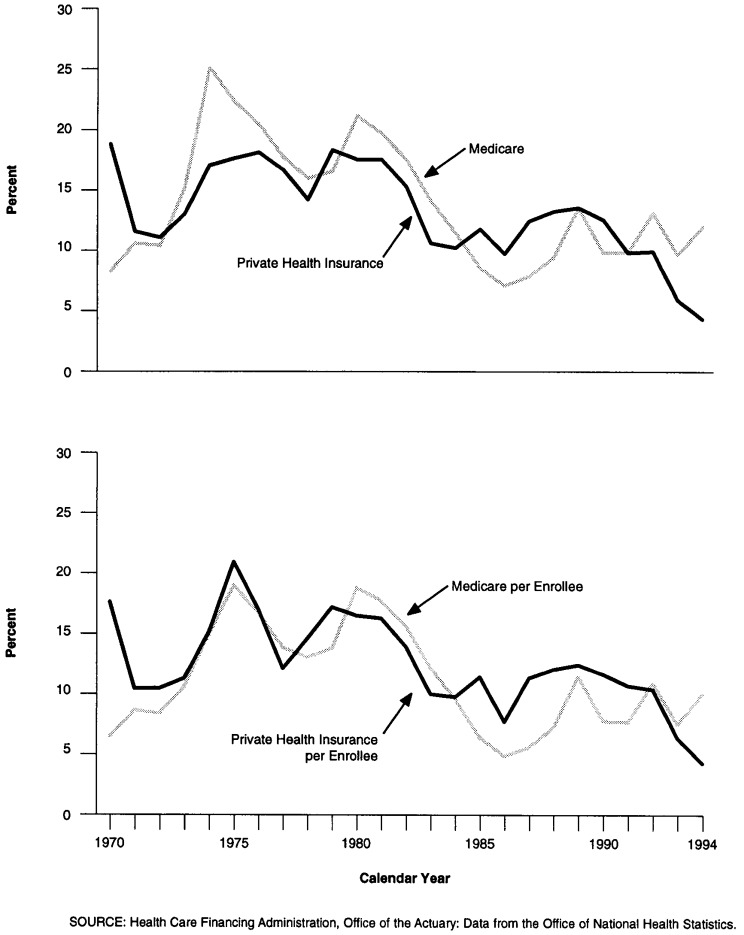
Sources of Differential Growth
A substantial part of the difference between aggregate Medicare growth and private insurance growth is attributable to enrollment. The number of aged and disabled Medicare beneficiaries increased at an average annual rate of 2.5 percent from 1969 to 1990 and has increased 1.9 percent annually since 1991. Enrollment in private health insurance has grown more slowly, averaging 0.7 percent annually from 1969 to 1990; since 1991 enrollment has actually declined an average of 0.3 percent annually. Thus, one would expect Medicare benefits in aggregate to grow more rapidly than private insurance benefits (Figure 4).
Figure 4. Growth in Medicare and Private Health Insurance Aggregate and per Enrollee Benefits: Calendar Years 1970-94.
On a per enrollee basis, however, Medicare benefits grew more slowly than private health insurance benefits from 1969 to 1993. Medicare increased at average annual rates of 10.9 percent, compared with 12.6 percent for private health insurance. Prior to 1984, growth rates were generally similar. During 1984-91, Medicare increased more slowly than private health insurance. For 1992 and 1993, growth rates were similar again. In 1994 however, spending changed dramatically. Medicare benefit expenditures per enrollee increased 9.8 percent, and those for private health insurance only 4.1 percent (Table 2). Even enrollment growth differentials do not explain the wide gap in expenditure growth in 1994.
Table 2. Medicare and Private Health Insurance Expenditures per Enrollee for Personal Health Care: Selected Years 1969-94.
| Source of Funding and Year | Personal Health Care Expenditures per Enrollee | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Freestanding-Home Health Care | Drugs and Other Medical Non-Durables | Vision Products Medical Durables | Freestanding Nursing Home Care | |
| Medicare | Expenditures in Dollars | ||||||||
| 1969 | $338 | $241 | $79 | — | $2 | $4 | — | $2 | $11 |
| 1974 | 535 | 394 | 118 | — | 5 | 5 | — | 4 | 8 |
| 1979 | 1,079 | 784 | 236 | — | 18 | 20 | — | 12 | 10 |
| 1984 | 2,127 | 1,502 | 484 | — | 39 | 51 | — | 36 | 14 |
| 1989 | 2,971 | 1,904 | 799 | — | 76 | 59 | — | 62 | 72 |
| 1991 | 3,436 | 2,175 | 881 | — | 117 | 121 | — | 86 | 56 |
| 1993 | 4,083 | 2,550 | 930 | — | 159 | 214 | — | 104 | 126 |
| 1994 | 4,484 | 2,743 | 1,028 | — | 184 | 258 | — | 111 | 160 |
| Average Annual Percent Growth | |||||||||
| 1969-74 | 9.6 | 10.3 | 8.3 | — | 27.4 | 7.3 | — | 19.3 | −4.9 |
| 1974-79 | 15.1 | 14.7 | 14.9 | — | 27.6 | 29.4 | — | 24.3 | 3.9 |
| 1979-84 | 14.5 | 13.9 | 15.4 | — | 16.9 | 21.1 | — | 25.7 | 6.3 |
| 1984-89 | 6.9 | 4.9 | 10.5 | — | 14.0 | 2.7 | — | 11.2 | 39.1 |
| 1989-91 | 7.5 | 6.9 | 5.0 | — | 24.2 | 43.5 | — | 18.0 | −11.7 |
| 1991-94 | 9.3 | 8.0 | 5.3 | — | 16.4 | 28.6 | — | 8.7 | 41.9 |
| 1969-93 | 10.9 | 10.3 | 10.8 | — | 21.2 | 18.3 | — | 19.0 | 10.8 |
| 1993-94 | 9.8 | 7.6 | 10.5 | — | 16.0 | 20.1 | — | 6.1 | 27.0 |
| Private Health Insurance | Expenditures in Dollars | ||||||||
| 1969 | $82 | $50 | $26 | $1 | $1 | $0 | $3 | $1 | $0 |
| 1974 | 149 | 91 | 46 | 3 | 2 | 0 | 5 | 1 | 0 |
| 1979 | 314 | 188 | 86 | 18 | 6 | 2 | 11 | 2 | 1 |
| 1984 | 580 | 317 | 161 | 43 | 18 | 4 | 29 | 3 | 4 |
| 1989 | 969 | 461 | 297 | 76 | 52 | 10 | 57 | 5 | 9 |
| 1991 | 1,193 | 540 | 385 | 86 | 70 | 14 | 82 | 5 | 11 |
| 1993 | 1,395 | 615 | 464 | 99 | 80 | 17 | 104 | 5 | 11 |
| 1994 | 1,453 | 630 | 488 | 108 | 83 | 18 | 109 | 5 | 12 |
| Average Annual Percent Growth | |||||||||
| 1969-74 | 12.8 | 12.5 | 12.0 | 23.5 | 25.4 | 29.0 | 15.1 | 11.2 | 32.2 |
| 1974-79 | 16.1 | 15.7 | 13.2 | 40.1 | 25.1 | 54.2 | 16.8 | 18.0 | 24.2 |
| 1979-84 | 13.1 | 11.0 | 13.4 | 18.9 | 26.0 | 17.3 | 20.6 | 10.6 | 30.9 |
| 1984-89 | 10.8 | 7.8 | 13.0 | 11.9 | 23.2 | 20.8 | 14.3 | 7.6 | 19.5 |
| 1989-91 | 11.0 | 8.2 | 13.7 | 5.9 | 16.1 | 15.3 | 19.7 | −1.8 | 12.7 |
| 1991-94 | 6.8 | 5.3 | 8.2 | 7.9 | 5.6 | 10.7 | 9.8 | −1.5 | 2.7 |
| 1969-93 | 12.6 | 11.0 | 12.7 | 20.3 | 22.5 | 26.7 | 16.6 | 9.5 | 23.0 |
| 1993-94 | 4.1 | 2.4 | 5.2 | 8.4 | 3.7 | 9.4 | 4.7 | −2.4 | 6.7 |
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
In addition to differences in enrollment growth, coverage of services and products by these two insurers also differs. The function of Medicare is to fund health care services for the aged and disabled. The target population for private health insurance is primarily the working-age population and their families. As a result of the different needs of these two insured groups, coverage of health care services by Medicare and private health insurance differs substantially. Per enrollee, Medicare funded 14 times the home health care and 13 times the nursing home care funded by private health insurance in 1994. These differences are fundamental to serving the health care needs of the aged and disabled population, services that are needed less often by the non-aged. On the other hand, private health insurance covered almost two-fifths of all outpatient prescription drug expenditures and almost one-half of all expenditures for dental services, benefits that Medicare does not cover. Although both insurers paid benefits for durable medical equipment, the composition of these benefits differed: Medicare paid for oxygen and oxygen-related equipment, prosthetics and orthotics, and rental and purchase of durable products such as wheelchairs and walkers; the majority of private health insurance durable medical spending purchased vision products. Medicare also provides the majority of payments for end stage renal disease (ESRD) treatments and hospice care, two benefits that are less frequently funded by private health insurance.
Comparison of expenditure growth rates is complicated by yet another factor— changes in benefit coverages over time. In particular, government laws, regulations, and policies affected growth in Medicare benefit expenditures by abruptly altering coverage, eligibility, and reimbursement. Examples include the introduction of the Medicare Catastrophic Coverage Act of 1989 (MCCA), the clarification of skilled nursing home conditions for payment (1988), and the clarification of home health coverage criteria (1988). These policies produced major expansions in eligibility and benefit payments for home health and skilled nursing home services. These actions and their residual effects produced average annual expenditure increases in home health care and skilled nursing home care of 35 and 44 percent, respectively, from 1988 to 1994.
For private health insurance, the breadth of services covered by employer-sponsored private health insurance5 increased gradually from 1980 to 1994. During the early to mid-1980s, coverage for full-time workers participating in employer-sponsored plans expanded in the areas of mental health and substance abuse treatment. In the late 1980s and early 1990s, coverage expansions have focused on preventive services, such as routine physicals, well-baby and well-child care, and immunizations and inoculations (U.S. Bureau of Labor Statistics, 1994; KPMG Peat Mar wick, 1992-94). Part of this expansion was the result of increased breadth of coverage by conventional, fee-for-service plans. Part was also the result of the changing mix of plans in which employees enroll. HMO and other managed-care plans typically emphasize preventive services. As these plans have become increasingly popular in recent years, they have contributed to the overall expansion of benefit coverage for preventive services.
Government introduced another source of differential growth in spending, the MVPS, in 1990 and incorporated it into the physician fee schedule in 1992. These regulations were designed to control growth in the volume of Medicare physician and other professional services. The MVPS penalizes physicians and other professionals for volume-of-service increases that exceed a predetermined target. A penalty for overshooting the target is imposed by reducing fee increases 2 years later. Similarly, when the volume of services increases less than targeted amounts, bonuses are paid through higher fee increases in a subsequent year.
In 1994, physicians and other professionals received higher Medicare payment rates (bonuses) as a reward for limiting volume increases in the first year (1992) of the Medicare physician fee schedule. The large growth in Medicare physician expenditures in 1994 was partly the result of an increase in the volume of physician and other professional services. This increase exceeded the MVPS target for 1994 by 1.2 percentage points and will result in a fee schedule penalty in 1996.
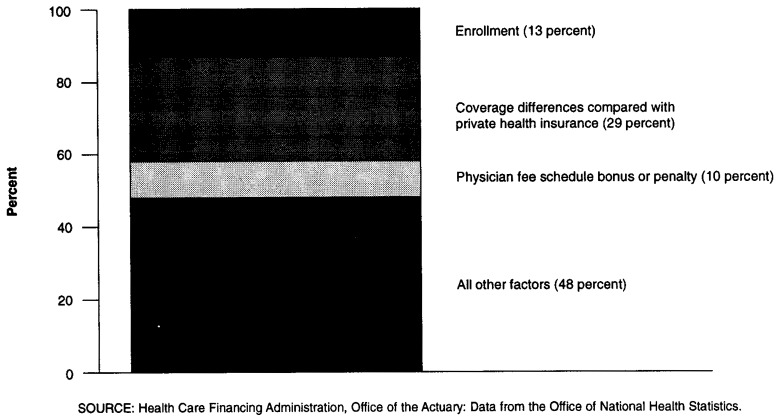
Comparing Adjusted Growth Rates
To make more meaningful comparisons between Medicare and private health insurance experience, it is important to make the two series as comparable as possible. Enrollment growth accounted for 13 percent of the 1994 increase in Medicare benefits. Services not traditionally covered by private health insurance (home health care, skilled nursing home care, ESRD treatment, durable medical products, and hospice care) accounted for another 29 percent of the increase. MVPS bonuses for 1992 and the 1994 penalty to be imposed in 1996 accounted for 10 percent of the increase. Adjusting for these three factors, which accounted for 52 percent of Medicare's increase (Figure 5), reduces the 1994 growth rate to 5.6 percent per enrollee.
Figure 5. Factors Accounting for Growth in Medicare Expenditures: Calendar Year 1994.
A comparable analysis of private health insurance requires the removal of spending associated with enrollment increases and coverage differences. In 1994, private health insurance benefits grew 4.0 percent, and enrollment declined 0.1 percent. Creating a benefit package comparable to Medicare's stripped-down package already described requires the removal of spending for prescription drugs, home health care, skilled nursing home care, dental services, and durable medical products (Table 2). These changes result in private health insurance benefit growth per enrollee of 3.6 percent.
Comparing the adjusted figures shows much less divergence between Medicare and private insurance. The gap is narrowed from 7.8 percentage points on an unadjusted basis to 2.0 points on an adjusted basis.
Highlights: Service Expenditures
The Nation's health care bill totaled $949.4 billion in 1994 for the 271 million persons residing in the United States. Spending per person amounted to $3,510 in 1994, 5.4 percent higher than the 1993 level. Data cited in the remaining discussion can be found in Tables 9-18 at the end of this article.
Table 9. National Health Expenditures Aggregate and Per Capita Amounts, Percent Distribution, and Average Annual Percent Growth, by Source of Funds: Selected Years 1960–94.
| Item | 1960 | 1970 | 1975 | 1980 | 1985 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Billions | ||||||||||
| National Health Expenditures | $26.9 | $73.2 | $130.7 | $247.2 | $428.2 | $697.5 | $761.3 | $833.6 | $892.3 | $949.4 |
| Private | 20.2 | 45.5 | 75.7 | 142.5 | 253.9 | 413.1 | 441.0 | 477.0 | 505.1 | 528.6 |
| Public | 6.6 | 27.7 | 55.0 | 104.8 | 174.3 | 284.3 | 320.3 | 356.5 | 387.2 | 420.8 |
| Federal | 2.9 | 17.8 | 36.4 | 72.0 | 123.3 | 195.8 | 224.4 | 254.8 | 278.5 | 303.6 |
| State and Local | 3.7 | 9.9 | 18.6 | 32.8 | 51.0 | 88.5 | 95.8 | 101.8 | 108.6 | 117.2 |
| Number in Millions | ||||||||||
| U.S. Population1 | 190.1 | 214.8 | 224.5 | 235.1 | 246.9 | 259.5 | 262.3 | 265.1 | 267.9 | 270.5 |
| Amount in Billions | ||||||||||
| Gross Domestic Product | $527 | $1,036 | $1,631 | $2,784 | $4,181 | $5,744 | $5,917 | $6,244 | $6,550 | $6,931 |
| Per Capita Amount | ||||||||||
| National Health Expenditures | $141 | $341 | $582 | $1,052 | $1,735 | $2,688 | $2,902 | $3,144 | $3,331 | $3,510 |
| Private | 106 | 212 | 337 | 606 | 1,029 | 1,592 | 1,681 | 1,799 | 1,886 | 1,954 |
| Public | 35 | 129 | 245 | 446 | 706 | 1,096 | 1,221 | 1,345 | 1,445 | 1,556 |
| Federal | 15 | 83 | 162 | 306 | 499 | 754 | 856 | 961 | 1,040 | 1,122 |
| State and Local | 20 | 46 | 83 | 140 | 207 | 341 | 365 | 384 | 406 | 433 |
| Percent Distribution | ||||||||||
| National Health Expenditures | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private | 75.2 | 62.2 | 57.9 | 57.6 | 59.3 | 59.2 | 57.9 | 57.2 | 56.6 | 55.7 |
| Public | 24.8 | 37.8 | 42.1 | 42.4 | 40.7 | 40.8 | 42.1 | 42.8 | 43.4 | 44.3 |
| Federal | 10.9 | 24.3 | 27.8 | 29.1 | 28.8 | 28.1 | 29.5 | 30.6 | 31.2 | 32.0 |
| State and Local | 13.9 | 13.5 | 14.2 | 13.3 | 11.9 | 12.7 | 12.6 | 12.2 | 12.2 | 12.3 |
| Percent of Gross Domestic Product | ||||||||||
| National Health Expenditures | 5.1 | 7.1 | 8.0 | 8.9 | 10.2 | 12.1 | 12.9 | 13.3 | 13.6 | 13.7 |
| Average Annual Percent Growth From Previous Year Shown | ||||||||||
| National Health Expenditures | — | 10.6 | 12.3 | 13.6 | 11.6 | 10.2 | 9.1 | 9.5 | 7.0 | 6.4 |
| Private | — | 8.5 | 10.7 | 13.5 | 12.3 | 10.2 | 6.7 | 8.2 | 5.9 | 4.7 |
| Public | — | 15.3 | 14.7 | 13.7 | 10.7 | 10.3 | 12.7 | 11.3 | 8.6 | 8.7 |
| Federal | — | 19.8 | 15.4 | 14.6 | 11.4 | 9.7 | 14.6 | 13.5 | 9.3 | 9.0 |
| State and Local | — | 10.2 | 13.5 | 12.0 | 9.2 | 11.6 | 8.3 | 6.2 | 6.7 | 7.9 |
| U.S. Population | — | 1.2 | 0.9 | 0.9 | 1.0 | 1.0 | 1.1 | 1.1 | 1.0 | 1.0 |
| Gross Domestic Product | — | 7.0 | 9.5 | 11.3 | 8.5 | 6.6 | 3.0 | 5.5 | 4.9 | 5.8 |
July 1 Social Security area population estimates for each year, 1960–94.
NOTE: Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 18. Expenditures for Health Services and Supplies Under Public Programs, by Type of Expenditure and Program: 1994.
| Program Area | All Expenditures | Personal Health Care | Administration | Public Health Activities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Drugs and Other Medical Non-Durables | Vision Products and Other Medical Durables | Nursing Home Care | Other | ||||
|
| |||||||||||||
| Amount in Billions | |||||||||||||
| Public and Private Spending | $919.2 | $831.7 | $338.5 | $189.4 | $42.2 | $49.6 | $26.2 | $78.6 | $13.1 | $72.3 | $21.8 | $58.7 | $28.8 |
| All Public Programs | 402.2 | 361.8 | 199.6 | 60.9 | 1.8 | 11.2 | 13.2 | 10.0 | 4.5 | 41.8 | 18.8 | 11.5 | 28.8 |
| Federal Funds | 290.3 | 280.0 | 162.7 | 48.6 | 1.0 | 8.3 | 11.4 | 5.2 | 4.4 | 27.0 | 11.4 | 6.6 | 3.7 |
| State and Local Funds | 111.8 | 81.8 | 36.8 | 12.3 | 0.8 | 2.9 | 1.7 | 4.8 | 0.1 | 14.9 | 7.4 | 4.9 | 25.1 |
| Medicare | 169.2 | 166.1 | 101.6 | 38.1 | — | 6.8 | 9.5 | — | 4.1 | 5.9 | — | 3.1 | — |
| Medicaid1 | 129.3 | 122.9 | 49.4 | 13.4 | 1.6 | 1.2 | 3.5 | 8.4 | — | 34.3 | 11.1 | 6.4 | — |
| Federal | 81.5 | 78.4 | 36.1 | 8.0 | 0.9 | 0.7 | 1.9 | 4.9 | — | 19.5 | 6.4 | 3.1 | — |
| State and Local | 47.8 | 44.5 | 13.3 | 5.4 | 0.7 | 0.5 | 1.6 | 3.5 | — | 14.8 | 4.7 | 3.3 | — |
| Other State and Local Public Assistance Programs | 5.5 | 5.5 | 3.3 | 0.4 | 0.1 | 0.3 | 0.1 | 1.0 | 0.0 | 0.1 | 0.2 | — | — |
| Department of Veterans Affairs | 15.1 | 15.1 | 12.4 | 0.1 | 0.0 | — | — | 0.0 | 0.2 | 1.5 | 0.7 | 0.1 | — |
| Department of Defense2 | 13.2 | 13.0 | 10.3 | 1.6 | 0.0 | — | — | 0.2 | — | — | 0.8 | 0.2 | — |
| Workers' Compensation | 18.9 | 17.4 | 8.4 | 6.4 | — | 2.1 | — | 0.3 | 0.1 | — | — | 1.5 | — |
| Federal | 0.6 | 0.6 | 0.3 | 0.1 | — | 0.1 | — | 0.0 | 0.0 | — | — | 0.0 | — |
| State and Local | 18.3 | 16.8 | 8.1 | 6.3 | — | 1.9 | — | 0.3 | 0.1 | — | — | 1.5 | — |
| State and Local Hospitals3 | 11.8 | 11.8 | 11.8 | — | — | — | — | — | — | — | — | — | — |
| Other Public Programs for Personal Health Care4 | 10.3 | 10.1 | 2.2 | 0.8 | 0.1 | 0.9 | — | 0.0 | 0.1 | — | 5.9 | 0.3 | — |
| Federal | 6.9 | 6.8 | 1.9 | 0.6 | 0.1 | 0.7 | — | 0.0 | 0.1 | — | 3.4 | 0.1 | — |
| State and Local | 3.4 | 3.3 | 0.3 | 0.2 | 0.0 | 0.2 | — | 0.0 | 0.0 | — | 2.5 | 0.2 | — |
| Government Public Health Activities | 28.8 | — | — | — | — | — | — | — | — | — | — | — | 28.8 |
| Federal | 3.7 | — | — | — | — | — | — | — | — | — | — | — | 3.7 |
| State and Local | 25.1 | — | — | — | — | — | — | — | — | — | — | — | 25.1 |
| Medicare and Medicaid | 298.5 | 289.1 | 51.1 | 51.5 | 1.6 | 8.1 | 13.1 | 8.4 | 4.1 | 40.2 | 11.1 | 9.5 | — |
Excludes funds paid into the Medicare trust funds by States under buy-in agreements to cover premiums for Medicaid recipients.
Includes care for retirees and military dependents.
Expenditures not offset by revenues.
lncludes program spending for maternal and child health; vocational rehabilitation medical payments; temporary disability insurance medical payments; Public Health Service and other Federal hospitals; Indian health services; alcoholism, drug abuse, and mental health; and school health.
NOTES: 0.0 denotes amounts less than $50 million. Numbers may not add to total because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Hospital Care
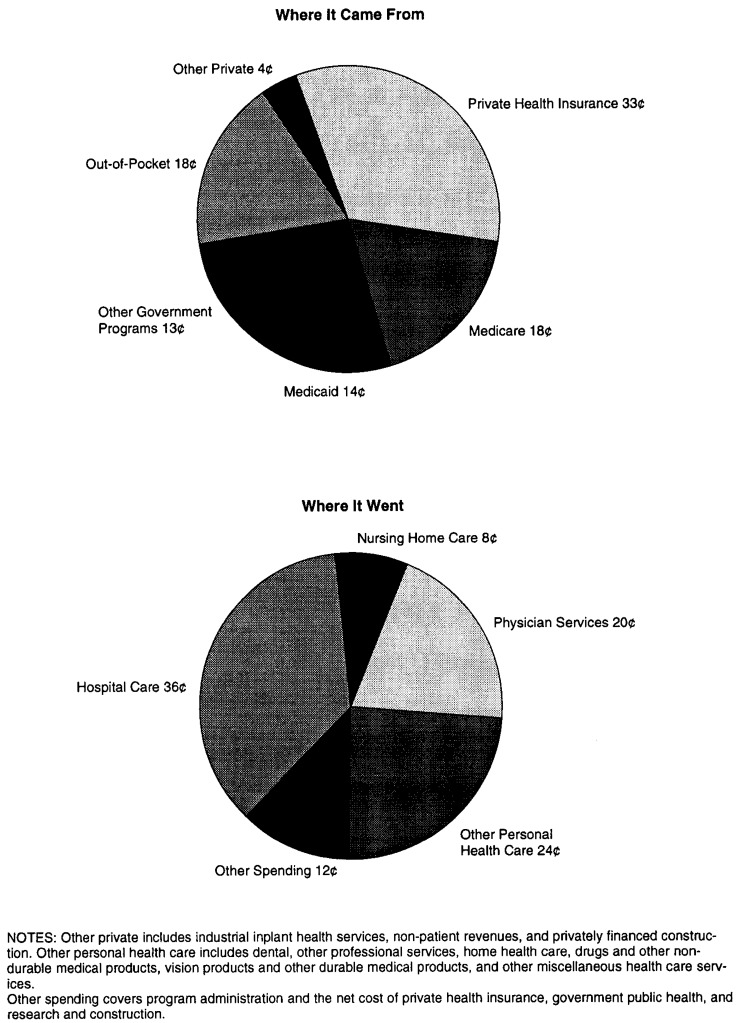
The largest single component of NHE is hospital care (Figure 6). With spending of $338.5 billion in 1994, this sector accounted for 35.7 percent of NHE. Eighty-eight percent of all hospital care in 1994 was delivered in short-term, acute-care community hospitals, 63 percent for inpatient services alone (Table 3). The remaining hospital services were provided in Federal facilities such as Department of Veterans Affairs hospitals and military facilities, or in non-Federal, non-community institutions, such as psychiatric hospitals.
Figure 6. The Nation's Health Dollar: 1994.
Table 3. Hospital Revenues, Percent Distribution, and Annual Percent Growth: Calendar Years 1985-94.
| Type of Hospital | 1985 | 1986 | 1987 | 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|---|---|
| Revenues in Millions | ||||||||||
| Total | $168,290 | $179,825 | $194,099 | $211,585 | $231,603 | $256,447 | $282,323 | $305,255 | $324,218 | $338,511 |
| Non-Federal | 155,036 | 165,829 | 179,378 | 196,360 | 215,190 | 238,570 | 262,586 | 284,659 | 302,112 | 316,121 |
| Community | 143,375 | 153,245 | 165,758 | 181,639 | 199,130 | 221,604 | 245,171 | 267,499 | 285,238 | 299,081 |
| Inpatient | 119,173 | 125,179 | 133,393 | 143,539 | 155,069 | 169,221 | 183,288 | 196,171 | 206,662 | 212,378 |
| Outpatient | 24,202 | 28,066 | 32,365 | 38,100 | 44,061 | 52,383 | 61,883 | 71,328 | 78,576 | 86,704 |
| Non-Community | 11,661 | 12,584 | 13,620 | 14,721 | 16,060 | 16,966 | 17,415 | 17,160 | 16,874 | 17,040 |
| Federal | 13,254 | 13,996 | 14,721 | 15,225 | 16,413 | 17,877 | 19,737 | 20,596 | 22,106 | 22,389 |
| Percent Distribution | ||||||||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Non-Federal | 92 | 92 | 92 | 93 | 93 | 93 | 93 | 93 | 93 | 93 |
| Community | 85 | 85 | 85 | 86 | 86 | 86 | 87 | 88 | 88 | 88 |
| Inpatient | 71 | 70 | 69 | 68 | 67 | 66 | 65 | 64 | 64 | 63 |
| Outpatient | 14 | 16 | 17 | 18 | 19 | 20 | 22 | 23 | 24 | 26 |
| Non-Community | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 6 | 5 | 5 |
| Federal | 8 | 8 | 8 | 7 | 7 | 7 | 7 | 7 | 7 | 7 |
| Annual Percent Growth | ||||||||||
| Total | 6.8 | 6.9 | 7.9 | 9.0 | 9.5 | 10.7 | 10.1 | 8.1 | 6.2 | 4.4 |
| Non-Federal | 6.7 | 7.0 | 8.2 | 9.5 | 9.6 | 10.9 | 10.1 | 8.4 | 6.1 | 4.6 |
| Community | 6.7 | 6.9 | 8.2 | 9.6 | 9.6 | 11.3 | 10.6 | 9.1 | 6.6 | 4.9 |
| Inpatient | 4.5 | 5.0 | 6.6 | 7.6 | 8.0 | 9.1 | 8.3 | 7.0 | 5.3 | 2.8 |
| Outpatient | 19.3 | 16.0 | 15.3 | 17.7 | 15.6 | 18.9 | 18.1 | 15.3 | 10.2 | 10.3 |
| Non-Community | 6.8 | 7.9 | 8.2 | 8.1 | 9.1 | 5.6 | 2.6 | −1.5 | −1.7 | 1.0 |
| Federal | 7.5 | 5.6 | 5.2 | 3.4 | 7.8 | 8.9 | 10.4 | 4.4 | 7.3 | 1.3 |
NOTE: Non-community non-Federal hospitals include long-term care hospitals (where the average length of stay is 30 days or longer), psychiatric hospitals, alcohol- and chemical-dependency hospitals, units of institutions such as prison hospitals or college infirmaries, chronic disease hospitals, and some institutions for the mentally retarded.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Hospital expenditures experienced the fourth consecutive year of decelerated growth, increasing only 4.4 percent in 1994. Price inflation accounted for 3.6 percentage points of this increase, and 1.0 percentage point was accounted for by population increases. Removing price and population increases from hospital growth produced a decline in real hospital expenditures per person in 1994 (-0.2 percent), the first time since the introduction of Medicare's prospective payment system that such a decline occurred.
Since the early 1980s, admissions per capita have been declining. In recent years, this decline almost halted, as admissions per population changed by only -0.3 percent in 1993 and -0.1 percent in 1994 (Table 4). The slowing decline in admissions combined with the negative real growth in hospital expenditures suggests that the severity of illness and use of services for each admission in 1994 may be less than in previous years. This may be particularly true for the population 65 years of age or over, for whom admissions per capita in this age group have been rising every year since 1991.
Table 4. Admissions, Inpatient Days, and Length of Stay in Community Hospitals, by Age Group: Selected Calendar Years 1983–94.
| Age Group and Statistic | 1983 | 1984 | 1985 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|
| All Ages | ||||||||
| Admissions in Thousands | 37,692 | 36,305 | 34,535 | 33,017 | 32,670 | 32,411 | 32,652 | 32,938 |
| Admissions per 1,000 Population | 156 | 149 | 140 | 127 | 125 | 122 | 122 | 122 |
| Inpatient Days in Thousands | 264,504 | 241,780 | 226,129 | 216,836 | 211,475 | 206,440 | 202,078 | 196,117 |
| Length of Stay in Days | 7.0 | 6.7 | 6.5 | 6.6 | 6.5 | 6.4 | 6.2 | 6.0 |
| Average Annual Percent Growth From Previous Year Shown | ||||||||
| Admissions | — | -3.7 | -4.9 | -0.9 | -1.1 | -0.8 | 0.7 | 0.9 |
| Admissions per 1,000 Population | — | -4.6 | -5.8 | -1.9 | -2.1 | -1.8 | -0.3 | -0.1 |
| Inpatient Days | — | -8.6 | -6.5 | -0.8 | -2.5 | -2.4 | -2.1 | -2.9 |
| Change in Length of Stay in Days From Previous Year Shown | — | -0.4 | -0.1 | 0.0 | -0.1 | -0.1 | -0.2 | -0.2 |
| Age 65 or Over | ||||||||
| Admissions in Thousands | 11,812 | 11,508 | 10,904 | 11,379 | 11,659 | 11,860 | 12,209 | 12,456 |
| Admissions per 1,000 Population | 425 | 406 | 377 | 357 | 360 | 360 | 366 | 369 |
| Inpatient Days in Thousands | 114,313 | 102,971 | 95,510 | 99,056 | 99,468 | 98,920 | 97,042 | 94,877 |
| Length of Stay in Days | 9.7 | 8.9 | 8.8 | 8.7 | 8.5 | 8.3 | 7.9 | 7.6 |
| Average Annual Percent Growth From Previous Year Shown | ||||||||
| Admissions | — | -2.6 | -5.2 | 0.9 | 2.5 | 1.7 | 2.9 | 2.0 |
| Admissions per 1,000 Population | — | -4.5 | -7.1 | -1.1 | 0.7 | 0.1 | 1.5 | 0.8 |
| Inpatient Days | — | -9.9 | -7.2 | 0.7 | 0.4 | -0.6 | -1.9 | -2.2 |
| Change in Length of Stay in Days From Previous Year Shown | — | -0.7 | -0.2 | -0.1 | -0.2 | -0.2 | -0.4 | -0.3 |
| Under Age 65 | ||||||||
| Admissions in Thousands | 25,880 | 24,797 | 23,631 | 21,638 | 21,011 | 20,551 | 20,443 | 20,483 |
| Admissions per 1,000 Population | 121 | 115 | 109 | 95 | 92 | 89 | 87 | 87 |
| Inpatient Days in Thousands | 150,191 | 138,809 | 130,619 | 117,781 | 112,007 | 107,520 | 105,036 | 101,240 |
| Length of Stay in Days | 5.8 | 5.6 | 5.5 | 5.4 | 5.3 | 5.2 | 5.1 | 4.9 |
| Average Annual Percent Growth From Previous Year Shown | ||||||||
| Admissions | — | -4.2 | -4.7 | -1.7 | -2.9 | -2.2 | -0.5 | 0.2 |
| Admissions per 1,000 Population | — | -5.0 | -5.5 | -2.6 | -3.8 | -3.2 | -1.5 | -0.8 |
| Inpatient Days | — | -7.6 | -5.9 | -2.0 | -4.9 | -4.0 | -2.3 | -3.6 |
| Change in Length of Stay in Days From Previous Year Shown | — | -0.2 | -0.1 | -0.1 | -0.1 | -0.1 | -0.1 | -0.2 |
SOURCE: American Hospital Association: Data from the National Hospital Panel Survey, 1983-94.
Nearly all hospital care was financed by third parties, with only 2.9 percent paid by consumers through out-of-pocket expenditures. Private health insurance financed 34.2 percent of hospital care, while Medicare paid for 30.0 percent, and Medicaid for another 14.6 percent.
Professional Services
Expenditures for physician services grew to $189.4 billion in 1994, accounting for almost 20 percent of all NHE. Similar to hospital care expenditures, expenditures for physician services increased modestly in 1993 (3.7 percent) and 1994 (4.6 percent). Net income per physician as recorded by the American Medical Association experienced only a modest increase in 1993 and a first-time decline in 1994 (Moser, 1996) resulting, at least in part, from the effect of managed-care arrangements. For 1994, AMA reported that 77 percent of physicians participated in one or more managed-care arrangements, up from 61 percent in 1990 (Emmons and Simon, 1995). These trends in physician expenditures reflect the growing numbers of physician practices with managed-care arrangements (Terry, 1995; Arnold and Dobosenski, 1995). These arrangements accept negotiated fee reductions for access to a pool of insured patients and may use gatekeepers as a way to limit referrals to specialists.
Two-thirds of all funding for physician services came from private sources in 1994. Out-of-pocket expenditures accounted for 18.9 percent, and private health insurance for 47.3 percent. The share of spending from out-of-pocket sources continued to fall, as the growth in aggregate copayments and deductibles required by third-party payers (KPMG Peat Marwick, 1992-94) failed to keep pace with third-party reimbursement. As more privately insured persons moved from traditional fee-for-service to managed-care plans, they faced flat out-of-pocket charges per visit or copayment rates that were frequently smaller than a percentage copayment required by conventional insurance plans. Similarly, slow growth in cost-sharing liability for Medicare beneficiaries resulted in out-of-pocket expenditures accounting for a smaller share of Medicare benefits (Health Care Financing Administration, 1995).
Spending for dentist services increased slightly faster than spending for most other health goods and services. In part, this is because third-party payments play a smaller role in the market for dental services than elsewhere; almost one-half of all dental spending was paid out of pocket. Growth in 1993 (6.0 percent) and 1994 (7.5 percent) was slower than that experienced in 1992 (11.0 percent), when dentist offices raised fees to cover costs associated with the Occupational Safety and Health Administration's standard on occupational exposure to blood-borne pathogens such as acquired immunodeficiency syndrome (AIDS) (American Dental Association, 1994). Overall, the $42.2 billion spent on dental care accounted for 4.4 percent of NHE.
Other professional services include those provided by such licensed medical professionals as chiropractors, psychologists, optometrists, podiatrists, and private duty nurses; by kidney dialysis centers and freestanding specialty outpatient clinics, such as those for substance abuse, rehabilitation, and mental health; by ambulances paid under Medicare; and by miscellaneous health and allied services not elsewhere classified. This category accounted for 5.2 percent of NHE in 1994. Expenditures in 1994 amounted to $49.6 billion, an increase of 7.1 percent over the 1993 level. Although expenditure growth in this sector exceeded that of NHE overall, spending for other professional services in 1994 represented the slowest expenditure growth in this sector since 1968.
Expenditures for freestanding private and public home health agencies6 amounted to $26.2 billion in 1994, a 13.8-percent increase over 1993 expenditure levels. Home health care expenditures were the second-fastest growing component of PHCE in 1994, although the 13.8-percent growth is substantially slower than the 20-30 percent growth rates experienced in the late 1980s and early 1990s. Expenditures for services and products provided by these agencies were 2.8 percent of NHE, a small but rapidly growing share. In 1994 Medicare and Medicaid financed more than one-half of all home health care expenditures. This share continues to rise, despite the deceleration in Medicare expenditure growth from the 40-50 percent range in 1990-92 to 22.3 percent in 1994.
Non-Durable and Durable Medical Products
Expenditures for drugs and other non-durable medical products amounted to $78.6 billion in 1994 (Table 5). Spending for these products has decelerated steadily since 1990, from a growth rate of 11.5 percent in 1990 to 4.5 percent in 1994. More than 60 percent of spending for non-durable medical products came from out-of-pocket sources. This category is composed of two parts: (1) prescription drugs, and (2) over-the-counter medicines and medical sundries. Since 1987, the share of NHE attributable to spending for non-durable medical products has shrunk from 9.0 percent to 8.3 percent.
Table 5. Expenditures for Drugs and Other Medical Non-Durables,1 by Source of Funds: Selected Years 1960-94.
| Source of Funds | 1960 | 1970 | 1975 | 1980 | 1985 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|---|---|
| Drugs and Non-Durable | Amount in Billions | |||||||||
| Medical Products | $4.2 | $8.8 | $13.0 | $21.6 | $37.1 | $59.9 | $65.6 | $71.3 | $75.2 | $78.6 |
| Prescription Drugs | 2.7 | 5.5 | 8.1 | 12.0 | 21.2 | 37.7 | 42.1 | 46.6 | 49.4 | 51.9 |
| Out-of-Pocket Payments | 2.6 | 4.5 | 6.1 | 7.9 | 11.7 | 18.2 | 19.3 | 20.4 | 21.2 | 22.0 |
| Third-Party Payments | 0.1 | 1.0 | 2.0 | 4.1 | 9.4 | 19.5 | 22.9 | 26.2 | 28.2 | 30.0 |
| Private Health Insurance | 0.0 | 0.5 | 1.0 | 2.4 | 6.3 | 13.0 | 15.2 | 18.0 | 19.1 | 20.0 |
| Medicaid | — | 0.4 | 0.9 | 1.4 | 2.5 | 5.1 | 6.2 | 6.7 | 7.7 | 8.4 |
| General Assistance | 0.0 | 0.0 | 0.1 | 0.1 | 0.4 | 0.9 | 0.9 | 0.9 | 0.9 | 1.0 |
| Other Government | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 0.4 | 0.5 | 0.5 | 0.6 | 0.6 |
| Non-Prescription Drugs and Other Medical Non-Durables2 | 1.6 | 3.3 | 5.0 | 9.6 | 15.9 | 22.2 | 23.5 | 24.7 | 25.7 | 26.6 |
| Out-of-Pocket Payments | 1.6 | 3.3 | 5.0 | 9.6 | 15.9 | 22.2 | 23.5 | 24.7 | 25.7 | 26.6 |
| Percentage Distribution by Source of Funds Within Each Category | ||||||||||
| Prescription Drugs | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Out-of-Pocket Payments | 96 | 82 | 75 | 66 | 55 | 48 | 46 | 44 | 43 | 42 |
| Third-Party Payments | 2 | 18 | 25 | 34 | 45 | 52 | 54 | 56 | 57 | 58 |
| Private Health Insurance | 1 | 9 | 12 | 20 | 30 | 35 | 36 | 39 | 39 | 38 |
| Medicaid | — | 8 | 11 | 12 | 12 | 14 | 15 | 14 | 16 | 16 |
| General Assistance | 0 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 |
| Other Government | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Non-Prescription Drugs and Other Medical Non-Durables2 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Out-of-Pocket Payments | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
This class of expenditure is limited to spending for products purchased in retail outlets. The value of drugs and other products provided by hospitals, nursing homes, or health professionals is implicit in estimates of spending for these providers' services.
Assumes no third-party payments for non-prescription drugs and other medical non-durables.
NOTES: Numbers and percentages may not add to totals because of rounding. The figure 0.0 denotes less than $50 million.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Two-thirds of all non-durable product expenditures, $51.9 billion, went for purchases of prescription drugs. Spending rose 5.1 percent in 1994, having steadily decelerated from 14.6 percent in 1990. During this period, prescription drug price increases, as measured by the Consumer Price Index (CPI), tumbled from 10 percent in 1990 to 3.4 percent in 1994. Price competition precipitated by an increase in the number of available generic drugs, the rise of pharmaceutical benefit managers, and the emergence of alternative pharmacy sites forced consumer prices to fall (Genuardi, Stiller, and Trapnell, 1996). Through 1989, out-of-pocket expenditures paid for the majority of prescription drugs. By 1994, the share financed by this source fell to 42.3 percent. Private health insurance financed 38.5 percent in that year, with Medicaid and State-funded general assistance paying for 18.1 percent.
Spending for durable medical products totaled $13.1 billion in 1994. Spending grew a modest 4.6 percent in 1994 for purchases such as vision products, hearing aids, wheelchairs, crutches, and artificial limbs. Almost two-thirds of all spending for durable products comes from private sources: 59.0 percent from out-of-pocket expenditures and 6.5 percent from private health insurance. Medicare paid for 31.2 percent of durable products in 1994, and the Department of Veterans Affairs for another 1.7 percent.
Nursing Home Care
Expenditures for nursing home care rose to $72.3 billion in 1994, a 7.8-percent increase from the 1993 level of $67.0 billion. This estimate covers expenditures in three facility types: (1) private and State and local government nursing home facilities; (2) Department of Veterans Affairs facilities; and (3) intermediate care facilities for the mentally retarded (ICFs/MR). The fastest growing component was spending in private, and State and local government facilities (9.0 percent); the slowest growing component was spending in ICFs/MR (-0.7 percent). Expenditures by the Department of Veterans Affairs in their own facilities grew 6.9 percent.
In 1994 Medicaid funded a slightly smaller share (47.4 percent) of all nursing home care than in 1993 (48.4 percent). This share decline was offset by an increased share funded by Medicare (8.2 percent in 1994, compared with 6.8 percent in 1993). Private funding, mostly through out-of-pocket spending, amounted to 42.1 percent of the total nursing home bill.
Other Personal Health Care
In this fastest growing PHCE category, governments and businesses spent $21.8 billion in 1994 to purchase services from establishments not usually recognized as medical care providers. In that year, businesses spent $3.0 billion for inplant health services, and government programs spent $18.8 billion for services in schools, military facilities, and other non-medical locations. More than one-half of all purchases for other personal health care came from the Medicaid program, mostly through waivers received by States for services not usually covered by that program.
Highlights: Source of Funding Expenditures
Of the $949.4 billion spent for health care in 1994, $528.6 billion (55.7 percent) resulted from private sector expenditures, mostly through private health insurance (33.0 percent) and out-of-pocket spending (18.4 percent). Another $420.8 billion (44.3 percent) came from government expenditures. Medicare and Medicaid alone accounted for more than 70 percent of all public expenditures on health care.
Spending shares have shifted between the Federal Government and private sector since 1990, with the Federal Government assuming a larger share of total spending. From 1990 to 1994, the Federal share of spending rose from 28.1 to 32.0 percent, and the private share fell from 59.2 to 55.7 percent. The increase in the Federal share results from growth in Medicare spending (from 16.1 in 1990 to 17.8 in 1994) and in Federal Medicaid payments (from 6.1 percent in 1990 to 8.6 percent in 1994). State and local governments were responsible for 12.3 percent of health expenditures, approximately the same proportion that they paid in 1990. Private health insurance funded about 33 percent of NHE in both years, and the amount funded from out-of-pocket sources dropped from 21.3 percent in 1990 to 18.4 percent in 1994.
Private Health Insurance
In 1994 private health insurance premiums equaled $313.3 billion, up 5.7 percent from 1993. This is the second consecutive year of decelerating growth and the fourth of single-digit growth. In large measure, the slower growth exhibited by private health insurance resulted from a shift by employees to lower cost managed-care plans offered through the workplace (Foster Higgins, 1994; KPMG Peat Marwick, 1992-94). These plans tended to restrict use to a preapproved list of providers in return for smaller premiums, copayments, and deductibles. An increasingly popular type of managed-care plan, known as a point-of-service (POS) plan, offers the option to go outside the plan provider list, but only by incurring larger out-of-pocket costs. Within various plan types, surveys note that premiums continued to increase in 1994.7 This suggests that a portion of the slow growth in private health insurance premiums resulted from the change in mix of plans toward lower cost plans. It also fuels speculation about the insurance industry's ability to maintain slow growth in the future once the shift to managed care is completed.
In 1994, private health insurance paid $266.8 billion in benefits. In general, the breadth of insurance coverage widened as more people enrolled in managed-care plans that more fully cover preventive services. The distribution of benefits paid by private health insurance for personal health care reflected this change. A smaller share of benefits went for hospital care between 1990 and 1994, offset by larger shares for physician services and prescription drugs. In response to increasing costs for prescription drugs, many employers switched to “carve-out plans,” including prescription card plans and mail-order drug plans (Foster Higgins, 1994). Carve-out plans, such as those for prescription drugs or mental health, are offered by private insurers who specialize in the management of a specific part of a health benefit package. These private insurers promise to deliver effective and efficient care at a lower price.
The net cost of private health insurance rose 16.0 percent in 1994, to $46.5 billion. This amount, 14.8 percent of total premiums, includes the administrative costs faced by private health insurers and self-insurers, insurer's net additions to reserves, rate credits and dividends, premium taxes, and profits and losses. From the late 1980s through 1994, the insurance industry maintained a net underwriting gain, rather than following the historical pattern of 3 years of gain followed by 3 years of loss. The stability of the underwriting cycle in recent years contributed to the slow growth in premiums (Gabel et al., 1991; KPMG Peat Marwick, 1992-94).
Medicare
Medicare expenditures for personal health care amounted to $166.1 billion in 1994 (Table 6), an increase of 11.8 percent over spending incurred in 1993. Medicare provided health care coverage for 36.9 million aged and disabled enrollees in 1994. More than four-fifths of these enrollees, 30.1 million, incurred expenses resulting in program payments. However, the distribution of benefits among enrollees was skewed: An estimated 11 percent of enrollees accounted for 73 percent of program payments in 1994.
Table 6. Personal Health Care Expenditures Under Medicare and Medicaid and Sources of Medicare Financing: Selected Calendar Years 1966-94.
| Year | Personal Health Care Expenditures | Population | Medicare Financing | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Inpatient Hospital Deductible6 | Supplementary Medical Insurance Monthly Premium7 | Annual Maximum Taxable Earnings | Contribution Rate 8,9 | |||||||
|
| ||||||||||
| Medicare and Medicaid1 | Medicare | Medicaid | ||||||||
|
| ||||||||||
| Medicare2 | Medicaid Recipients5 | |||||||||
|
| ||||||||||
| Enrollees3 | Users4 | |||||||||
|
| ||||||||||
| Amount In Billions | Number in Millions | Amount in Dollars | Percent | |||||||
| 1966 | $3.0 | $1.7 | $1.3 | 19.1 | 3.7 | — | $40 | $3.00 | $6,600 | 0.35 |
| 1967 | 7.8 | 4.7 | 3.0 | 19.5 | 7.2 | — | 40 | 3.00 | 6,600 | 0.50 |
| 1972 | 16.9 | 8.9 | 8.0 | 21.3 | 10.0 | 17.6 | 68 | 5.80 | 9,000 | 0.60 |
| 1973 | 19.3 | 10.2 | 9.1 | 23.5 | 10.2 | 19.6 | 72 | 106.30 | 10,800 | 1.00 |
| 1975 | 28.6 | 15.7 | 12.9 | 25.0 | 13.0 | 22.0 | 92 | 6.70 | 14,100 | 0.90 |
| 1980 | 61.2 | 36.4 | 24.8 | 28.5 | 18.0 | 21.6 | 180 | 9.60 | 25,900 | 1.05 |
| 1985 | 109.4 | 70.3 | 39.2 | 31.1 | 22.3 | 21.8 | 400 | 15.50 | 39,600 | 1.35 |
| 1989 | 159.1 | 100.0 | 59.1 | 33.6 | 26.1 | 23.5 | 560 | 1131.90 | 48,000 | 1.45 |
| 1990 | 181.3 | 109.6 | 71.7 | 34.2 | 27.1 | 25.3 | 592 | 28.60 | 51,300 | 1.45 |
| 1991 | 210.2 | 120.2 | 90.1 | 34.9 | 27.6 | 28.3 | 628 | 29.90 | 125,000 | 1.45 |
| 1992 | 238.4 | 135.9 | 102.5 | 35.6 | 27.9 | 30.9 | 652 | 31.80 | 130,200 | 1.45 |
| 1993 | 262.7 | 148.6 | 114.1 | 36.3 | 29.5 | 33.4 | 676 | 36.60 | 135,000 | 1.45 |
| 1994 | 289.1 | 166.1 | 122.9 | 36.9 | 30.1 | 35.1 | 696 | 41.10 | (12) | 1.45 |
Excludes “buy-in” premiums paid by Medicaid for SMI coverage of aged and disabled Medicaid recipients eligible for coverage.
Hospital insurance (HI) and/or supplementary medical insurance (SMI).
Enrollees as of July 1 of specified year.
Enrollees with some provider payment under Medicare during calendar year. Data through 1973 reflect aged users only. Data for 1974 and later include aged and disabled users.
Unduplicated count of Medicaid recipients during fiscal year.
As of January of specified year with the exception of 1966, for which July data are used.
As of July for 1966-83 and as of January for 1984 and later.
Employer and employee (each) and self-employed people through 1983.
Effective in 1984, self-employed people pay double this rate, the equivalent of both the employer and the employee share.
Monthly premium for July and August 1973 was reduced to $5.80 and $6.10, respectively, by the Cost of Living Council.
Includes $27.90 SMI monthly premium and $4 catastrophic coverage monthly premium.
The limit on earnings subject to the HI contribution rate was repealed, effective January 1, 1994.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Medicare is the largest public payer for total PHCE and for each of the service components covered by the program except nursing home care. In 1994 Medicare financed 20.0 percent of total spending for PHCE, 30.0 percent of spending for hospital care, 20.1 percent for physician services, 13.7 percent for other professional services, 36.5 percent for home health care, 31.2 percent for medical durables, and 8.2 percent for nursing home care. Medicare's shares have increased each year since 1991 (earlier for some services), except for physician services. Faster growth in the Medicare population, compared with the general population, and the aging of frail elderly Medicare enrollees are contributing factors to these increasing funding shares.
In 1994, expenditures by Medicare for a broad range of services continued to exhibit strong growth. Medicare expenditures for hospital care reached $101.6 billion, 9.6 percent higher than the $92.8 billion spent in 1993. These expenditures for hospital care services include inpatient, outpatient, and hospital-based home health agency and skilled nursing facility services. Medicare spending for physician services increased 12.6 percent from $33.9 billion in 1993 to $38.1 billion in 1994. A portion of the growth in 1994 is the result of bonuses paid to physicians for restraining growth in volume below designated levels established for 1992; another portion represents increases in volume above the specified target that will be penalized in 1996.8 Medicare paid $5.9 billion for nursing home care provided in freestanding skilled nursing facilities in 1994. Growth in these expenditures decelerated for the second consecutive year. Between 1993 and 1994, spending for nursing home care grew 29.3 percent. Other Medicare expenditures in 1994 included $6.8 billion for other professional services, $4.1 billion for medical durable products, and $9.5 billion for home health care furnished by non-facility-based home health agencies.
Unlike other Federal programs, Medicare is not financed solely by appropriations from general tax receipts. Medicare has two parts, each with its own trust fund. The hospital insurance (HI) program pays for inpatient hospital services, post-hospital skilled nursing services, home health services, and hospice care. The supplementary medical insurance (SMI) program covers physician services, outpatient hospital services and therapy, and other services. In 1994 87.3 percent of income for the HI program came from a 1.45-percent payroll tax levied on employers and employees for all taxable earnings. (Self-employed persons were required to contribute 2.9 percent, the equivalent of both the employer's and employee's share of the HI tax.) Beginning in 1994, the HI program received revenue attributable to income taxes imposed on a portion of Social Security benefits paid to individuals or couples whose total income exceeded prescribed amounts. In 1994 1.5 percent of HI program income was derived from taxation of Social Security benefits (Table 7).9
Table 7. Payments Into Medicare Trust Funds and Percent Distribution, by Type of Fund and Source of Income: Selected Calendar Years, 1967–94.
| Year and Source of Income | Total | Hospital Insurance Trust Fund | Supplementary Medical Insurance (SMI) Trust Fund | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Amount in Billions | Percent Distribution | Amount in Billions | Percent Distribution | Amount in Billions | Percent Distribution | |
| 1967 | ||||||
| Total | $5.2 | 100.0 | $3.6 | 100.0 | $1.6 | 100.0 |
| Payroll Taxes | 3.2 | 62.0 | 3.2 | 89.8 | — | — |
| General Revenues | 1.2 | 24.1 | 0.3 | 8.8 | 0.9 | 58.4 |
| Premiums | 0.6 | 12.4 | — | — | 0.6 | 40.1 |
| Interest | 0.1 | 1.5 | 0.1 | 1.4 | 0.0 | 1.5 |
| 1972 | ||||||
| Total | 9.2 | 100.0 | 6.4 | 100.0 | 2.8 | 100.0 |
| Payroll Taxes | 5.8 | 62.9 | 5.8 | 90.5 | — | — |
| General Revenues | 1.8 | 19.7 | 0.4 | 6.7 | 1.4 | 49.5 |
| Premiums | 1.4 | 15.0 | — | — | 1.4 | 49.2 |
| Interest | 0.2 | 2.4 | 0.2 | 2.8 | 0.0 | 1.3 |
| 1993 | ||||||
| Total | 155.9 | 100.0 | 98.2 | 100.0 | 57.7 | 100.0 |
| Payroll Taxes | 84.5 | 54.2 | 84.5 | 86.1 | — | — |
| General Revenues | 41.9 | 26.9 | 0.4 | 0.5 | 41.5 | 71.9 |
| Premiums | 14.9 | 9.5 | 0.7 | 0.7 | 14.2 | 24.6 |
| Interest | 14.6 | 9.3 | 212.5 | 12.8 | 2.0 | 3.5 |
| 1994 | ||||||
| Total | 165.2 | 100.0 | 109.6 | 100.0 | 55.6 | 100.0 |
| Payroll Taxes | 95.7 | 57.9 | 95.7 | 87.3 | — | — |
| Taxation of Benefits1 | 1.6 | 1.0 | 1.6 | 1.5 | — | — |
| General Revenues | 36.8 | 22.3 | 0.6 | 0.5 | 36.2 | 65.1 |
| Premiums | 18.3 | 11.1 | 0.9 | 0.8 | 17.4 | 31.3 |
| Interest | 12.8 | 7.7 | 10.7 | 9.8 | 2.0 | 3.6 |
Income taxes on Social Security benefits.
Includes a $1.8 billion transfer from the SMI catastrophic coverage fund.
NOTES: The figure 0.0 denotes less than $50 million. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
The SMI program was financed through monthly premiums of $41.10 per enrollee in 1994 and through general revenue. The general revenue share of SMI receipts declined from 71.9 percent in 1993 to 65.1 percent in 1994. This in the lowest share from general revenues since 1976. Increases in the SMI premium share offset general revenue declines.
Medicaid
Combined Federal and State Medicaid spending for personal health care accounted for 14.8 percent of total PHCE in 1994. Since 1992 growth in Medicaid spending has been decelerating, slowing to 7.7 percent in 1994. Legislation that imposed State limits on disproportionate share hospital (DSH) payments (Levit et al., 1994) seems to have had an effect on controlling growth in program expenditures.
Medicaid largely funds institutional services. In 1994, hospital and nursing home care consumed 68.1 percent of the $122.9 billion in PHCE funded by Medicaid. Medicaid is the largest third-party payer of long-term care. In 1994, Medicaid financed $34.3 billion, 47.4 percent of total expenditures for care provided in freestanding nursing facilities. The Medicaid share of total spending for nursing home care has fluctuated between 45 percent and 51 percent since the mid-1970s.
Medicaid is funded jointly by Federal and by State and local governments. For States to receive Federal matching funds, they must adhere to minimum requirements for eligibility and services set by the Federal Government. Within this broad framework, State governments are afforded considerable flexibility in designing the total scope of the program within the constraints of the State budgetary process.
In fiscal year 1994, 35.1 million people received some type of Medicaid benefit. Children and adults in families with dependent children represented 70.7 percent of all recipients, yet consumed only 28.5 percent of program payments. Conversely, the aged, blind, and disabled represented just over one-quarter of all recipients but consumed nearly three-quarters of program payments. Annual growth in the number of recipients has decelerated in each fiscal year, from 12.0 percent in 1991 to 4.8 percent in 1994.
Revisions to NHE
This section contains information on revisions in concept, method, and data sources introduced in expenditure estimates presented in this article. Detailed information on definitions, data sources, and methods can be found in previously published articles (Lazenby et al., 1992; Levit et al., 1994).
Conceptual and Methodological Revisions
The NHE have been revised to remove the double-counting of hospital-based nursing homes. In the data sources previously used to estimate nursing home expenditures, hospital-based nursing homes could not be separately identified from freestanding nursing homes. Current NHE estimates for nursing homes are based on information from the Census Bureau's Service Annual Survey and the Census of Service Industries that includes only freestanding nursing homes. This correction resulted in a downward revision in nursing home expenditures and no change in the hospital expenditures. It also prompted a transfer of expenditures for Medicare and Medicaid hospital-based nursing homes from the nursing home category to the hospital category.
In a major revision to home health care and government public health expenditures, home health services delivered by government agencies was transferred from government public health to home health services. The amount of the transfer was estimated using Medicare information on the proportion of total Medicare home health services delivered by government agencies. Home health care expenditures were revised upward because of this change, with an equal reduction in government public health spending (Table 8).
Table 8. Total National Health Expenditures (NHE), Medicare, Medicaid, and Other Spending for Both Hospital-Based and Non-Hospital-Based Home Health Care: Selected Calendar Years 1960–94.
| Year | NHE for Home Health Care | Medicare | Medicaid | Other Sources Total2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Total | Hospital-Based HHA1 | Non-Hospital-Based HHA2 | Total | Hospital-Based HHA1 | Non-Hospital-Based HHA2 | Total | Hospital-Based HHA1 | Non-Hospital-Based HHA2,3 | ||
|
| ||||||||||
| Amount in Millions | ||||||||||
| 1960 | $56 | $0 | $56 | — | — | — | — | — | — | $56 |
| 1970 | 231 | 11 | 219 | $69 | $9 | $60 | $17 | $2 | $15 | 145 |
| 1975 | 664 | 42 | 622 | 221 | 29 | 192 | 99 | 13 | 86 | 344 |
| 1980 | 2,583 | 207 | 2,376 | 754 | 102 | 652 | 401 | 106 | 295 | 1,428 |
| 1985 | 6,283 | 641 | 5,642 | 1,943 | 360 | 1,583 | 1,151 | 280 | 871 | 3,188 |
| 1990 | 14,933 | 1,816 | 13,117 | 3,951 | 957 | 2,994 | 2,911 | 859 | 2,052 | 8,070 |
| 1991 | 18,464 | 2,414 | 16,050 | 5,684 | 1,450 | 4,233 | 3,386 | 964 | 2,422 | 9,395 |
| 1992 | 22,735 | 3,111 | 19,624 | 7,983 | 2,053 | 5,930 | 3,885 | 1,058 | 2,827 | 10,867 |
| 1993 | 26,930 | 3,948 | 22,982 | 10,516 | 2,710 | 7,805 | 4,452 | 1,238 | 3,214 | 11,962 |
| 1994 | 30,932 | 4,774 | 26,158 | 12,944 | 3,401 | 9,543 | 4,907 | 1,373 | 3,534 | 13,081 |
Included in the hospital spending category of the National Health Accounts (NHA).
Estimated spending reported in the home health care category of the NHA.
Medicaid spending for home health care delivered by non-hospital-based HHAs and providers not affiliated with a formal HHA.
NOTES: HHA is home health agency. Figures may not add to totals shown because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Revisions in the estimates of retail spending for prescription drugs were mainly the result of the introduction of new methodologies and data sources that better capture expenditures for prescription drugs in retail outlets (Genuardi, Stiller, and Trapnell, 1996). Expenditures for vision and other durable medical products changed for two reasons. First, the concept was revised to better reflect the full range of durable medical products recorded in various categories of personal consumption expenditures. Second, sun or glare glasses and magnifying non-focus lenses (non-health-related items) were removed from the durable medical expenditure category.
In January 1996 the U.S. Bureau of Economic Analysis (BEA) (1996) introduced revisions to the estimation of GDP. These revisions increased the size of GDP in 1993 by $207 billion. In addition, BEA introduced its GDP chain-type annual-weighted index to measure economywide inflation (Landefeld and Parker, 1995). This index was incorporated into the calculation of HCFA's PHCE index, which was also changed from a fixed-weight index to a chain-type annual-weighted index.
Revisions Because of Data Sources
Many of the expenditure estimates in NHE are based on data collected by the U.S. Bureau of the Census. Every 5 years (years ending in 2 and 7), economic data on the health care industry are collected in the Census of Service Industries; for intervening years, the Bureau provides estimates based on responses from sample establishments in the Service Annual Survey. When data from a new economic census become available, revisions to the annual estimates for years between the current and previous censuses are made. The estimates presented in this article incorporate new information from the 1992 Census of Service Industries and associated revisions back to 1988 from Census Bureau's Service Annual Survey. The new and revised information affected estimates for physician, dental, other professional, nursing home care, and home health care expenditures. Similarly, the value of new construction put in place, estimated by the U.S. Bureau of the Census (U.S. Bureau of the Census, 1995), was revised from 1982 forward and the changes incorporated into NHE.
The private sources of funding include out-of-pocket spending, private health insurance expenditures, and non-patient revenues. Estimates of private sources of funding were developed for each type of service by subtracting total public sources of funding from each of the independently derived service expenditure totals. Most of the revisions to private health insurance premiums were the result of changes in benefits, mainly from hospital and physician estimates.
Table 10. National Health Expenditures Aggregate Amounts and Average Annual Percent Change, by Type of Expenditure: Selected Years 1960–94.
| Type of Expenditure | 1960 | 1970 | 1975 | 1980 | 1985 | 1990 | 1991 | 1992 | 1993 | 1994 |
|---|---|---|---|---|---|---|---|---|---|---|
| Amount in Billions | ||||||||||
| National Health Expenditures | $26.9 | $73.2 | $130.7 | $247.2 | $428.2 | $697.5 | $761.3 | $833.6 | $892.3 | $949.4 |
| Health Services and Supplies | 25.2 | 67.9 | 122.3 | 235.6 | 411.8 | 672.9 | 736.3 | 806.0 | 863.1 | 919.2 |
| Personal Health Care | 23.6 | 63.8 | 114.5 | 217.0 | 376.4 | 614.7 | 676.2 | 739.8 | 786.5 | 831.7 |
| Hospital Care | 9.3 | 28.0 | 52.6 | 102.7 | 168.3 | 256.4 | 282.3 | 305.3 | 324.2 | 338.5 |
| Physician Services | 5.3 | 13.6 | 23.9 | 45.2 | 83.6 | 146.3 | 158.6 | 174.7 | 181.1 | 189.4 |
| Dental Services | 2.0 | 4.7 | 8.0 | 13.3 | 21.7 | 31.6 | 33.3 | 37.0 | 39.2 | 42.2 |
| Other Professional Services | 0.6 | 1.4 | 2.7 | 6.4 | 16.6 | 34.7 | 38.3 | 42.1 | 46.3 | 49.6 |
| Home Health Care | 0.1 | 0.2 | 0.6 | 2.4 | 5.6 | 13.1 | 16.1 | 19.6 | 23.0 | 26.2 |
| Drugs and Other Medical Non-Durables | 4.2 | 8.8 | 13.0 | 21.6 | 37.1 | 59.9 | 65.6 | 71.3 | 75.2 | 78.6 |
| Vision Products and Other Medical Durables | 0.6 | 1.6 | 2.5 | 3.8 | 6.7 | 10.5 | 11.2 | 11.9 | 12.6 | 13.1 |
| Nursing Home Care | 0.8 | 4.2 | 8.7 | 17.6 | 30.7 | 50.9 | 57.2 | 62.3 | 67.0 | 72.3 |
| Other Personal Health Care | 0.7 | 1.3 | 2.5 | 4.0 | 6.1 | 11.2 | 13.6 | 15.6 | 17.8 | 21.8 |
| Program Administration and Net Cost of Private Health Insurance | 1.2 | 2.7 | 4.9 | 11.8 | 23.8 | 38.6 | 38.7 | 42.8 | 51.0 | 58.7 |
| Government Public Health Activities | 0.4 | 1.3 | 2.9 | 6.7 | 11.6 | 19.6 | 21.4 | 23.4 | 25.7 | 28.8 |
| Research and Construction | 1.7 | 5.3 | 8.4 | 11.6 | 16.4 | 24.5 | 24.9 | 27.6 | 29.2 | 30.2 |
| Research1 | 0.7 | 2.0 | 3.3 | 5.5 | 7.8 | 12.2 | 12.9 | 14.2 | 14.5 | 15.9 |
| Construction | 1.0 | 3.4 | 5.1 | 6.2 | 8.5 | 12.3 | 12.0 | 13.4 | 14.7 | 14.3 |
| Average Annual Percent Change From Previous Year Shown | ||||||||||
| National Health Expenditures | — | 10.6 | 12.3 | 13.6 | 11.6 | 10.2 | 9.1 | 9.5 | 7.0 | 6.4 |
| Health Services and Supplies | — | 10.4 | 12.5 | 14.0 | 11.8 | 10.3 | 9.4 | 9.5 | 7.1 | 6.5 |
| Personal Health Care | — | 10.5 | 12.4 | 13.6 | 11.6 | 10.3 | 10.0 | 9.4 | 6.3 | 5.7 |
| Hospital Care | — | 11.7 | 13.4 | 14.3 | 10.4 | 8.8 | 10.1 | 8.1 | 6.2 | 4.4 |
| Physician Services | — | 9.9 | 12.0 | 13.6 | 13.1 | 11.8 | 8.4 | 10.1 | 3.7 | 4.6 |
| Dental Services | — | 9.1 | 11.2 | 10.9 | 10.2 | 7.8 | 5.6 | 11.0 | 6.0 | 7.5 |
| Other Professional Services | — | 8.8 | 14.2 | 18.4 | 21.2 | 15.8 | 10.4 | 10.0 | 10.0 | 7.1 |
| Home Health Care | — | 14.5 | 23.2 | 30.7 | 18.9 | 18.4 | 22.4 | 22.3 | 17.1 | 13.8 |
| Drugs and Other Medical Non-Durables | — | 7.6 | 8.1 | 10.7 | 11.4 | 10.1 | 9.5 | 8.6 | 5.4 | 4.5 |
| Vision Products and Other Medical Durables | — | 9.6 | 9.5 | 8.1 | 12.4 | 9.2 | 6.8 | 6.9 | 5.1 | 4.6 |
| Nursing Home Care | — | 17.4 | 15.5 | 15.3 | 11.7 | 10.7 | 12.2 | 9.0 | 7.6 | 7.8 |
| Other Personal Health Care | — | 6.5 | 13.8 | 10.2 | 8.8 | 12.9 | 21.1 | 14.7 | 14.3 | 22.5 |
| Program Administration and Net Cost of Private Health Insurance | — | 8.9 | 12.5 | 19.2 | 15.0 | 10.2 | 0.2 | 10.5 | 19.1 | 15.2 |
| Government Public Health Activities | — | 13.9 | 16.8 | 18.1 | 11.5 | 11.0 | 9.1 | 9.4 | 9.6 | 12.4 |
| Research and Construction | — | 12.2 | 9.4 | 6.8 | 7.1 | 8.4 | 1.7 | 10.5 | 5.9 | 3.5 |
| Research1 | — | 10.9 | 11.2 | 10.4 | 7.5 | 9.3 | 5.8 | 9.8 | 2.2 | 9.9 |
| Construction | — | 12.9 | 8.3 | 4.1 | 6.7 | 7.6 | -2.4 | 11.4 | 9.7 | -2.8 |
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from research expenditures but are included in the expenditure class in which the product falls.
NOTE: Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 11. National Health Expenditures, by Source of Funds and Type of Expenditure: Selected Calendar Years 1960–94.
| Year and Type of Expenditure | Total | Private | Government | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| All Private Funds | Consumer | Other | Total | Federal | State and Local | ||||
|
| |||||||||
| Total | Out of Pocket | Private Insurance | |||||||
|
| |||||||||
| Amount in Billions | |||||||||
| 1960 | |||||||||
| National Health Expenditures | $26.9 | $20.2 | $18.9 | $13.1 | $5.9 | $1.3 | $6.6 | $2.9 | $3.7 |
| Health Services and Supplies | 25.2 | 19.5 | 18.9 | 13.1 | 5.9 | 0.6 | 5.7 | 2.3 | 3.4 |
| Personal Health Care | 23.6 | 18.5 | 18.1 | 13.1 | 5.0 | 0.4 | 5.1 | 2.1 | 3.0 |
| Hospital Care | 9.3 | 5.3 | 5.2 | 1.9 | 3.3 | 0.1 | 3.9 | 1.6 | 2.3 |
| Physician Services | 5.3 | 4.9 | 4.9 | 3.3 | 1.6 | 0.0 | 0.4 | 0.1 | 0.3 |
| Dental Services | 2.0 | 1.9 | 1.9 | 1.9 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Other Professional Services | 0.6 | 0.6 | 0.5 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Home Health Care | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | — | 0.0 |
| Drugs and Other Medical Non-Durables | 4.2 | 4.2 | 4.2 | 4.1 | 0.0 | — | 0.1 | 0.0 | 0.0 |
| Vision Products and Other Medical Durables | 0.6 | 0.6 | 0.6 | 0.6 | 0.0 | — | 0.0 | 0.0 | 0.0 |
| Nursing Home Care | 0.8 | 0.7 | 0.7 | 0.7 | — | 0.1 | 0.1 | 0.1 | 0.1 |
| Other Personal Health Care | 0.7 | 0.2 | — | — | — | 0.2 | 0.5 | 0.3 | 0.2 |
| Program Administration and Net Cost of Private Health Insurance | 1.2 | 1.0 | 0.9 | — | 0.9 | 0.1 | 0.2 | 0.0 | 0.1 |
| Government Public Health Activities | 0.4 | — | — | — | — | — | 0.4 | 0.1 | 0.3 |
| Research and Construction | 1.7 | 0.7 | — | — | — | 0.7 | 1.0 | 0.7 | 0.3 |
| Research | 0.7 | 0.1 | — | — | — | 0.1 | 0.6 | 0.5 | 0.0 |
| Construction | 1.0 | 0.6 | — | — | — | 0.6 | 0.4 | 0.2 | 0.3 |
| 1980 | |||||||||
| National Health Expenditures | 247.2 | 142.5 | 130.0 | 60.3 | 69.7 | 12.5 | 104.8 | 72.0 | 32.8 |
| Health Services and Supplies | 235.6 | 138.0 | 130.0 | 60.3 | 69.7 | 8.0 | 97.6 | 66.7 | 30.9 |
| Personal Health Care | 217.0 | 130.0 | 122.2 | 60.3 | 62.0 | 7.8 | 87.0 | 63.4 | 23.6 |
| Hospital Care | 102.7 | 46.8 | 41.8 | 5.3 | 36.4 | 5.0 | 55.9 | 42.2 | 13.8 |
| Physician Services | 45.2 | 32.1 | 31.8 | 14.6 | 17.1 | 0.4 | 13.1 | 10.0 | 3.1 |
| Dental Services | 13.3 | 12.7 | 12.7 | 8.8 | 3.8 | 0.0 | 0.6 | 0.4 | 0.3 |
| Other Professional Services | 6.4 | 4.9 | 4.4 | 3.3 | 1.1 | 0.5 | 1.5 | 1.1 | 0.4 |
| Home Health Care | 2.4 | 1.4 | 0.9 | 0.5 | 0.4 | 0.5 | 1.0 | 0.8 | 0.1 |
| Drugs and Other Medical Non-Durables | 21.6 | 19.9 | 19.9 | 17.5 | 2.4 | — | 1.7 | 0.9 | 0.8 |
| Vision Products and Other Medical Durables | 3.8 | 3.2 | 3.2 | 2.7 | 0.4 | — | 0.6 | 0.5 | 0.1 |
| Nursing Home Care | 17.6 | 8.1 | 7.6 | 7.4 | 0.2 | 0.5 | 9.5 | 5.6 | 3.9 |
| Other Personal Health Care | 4.0 | 0.9 | — | — | — | 0.9 | 3.1 | 2.0 | 1.1 |
| Program Administration and Net Cost of Private Health Insurance | 11.8 | 8.0 | 7.7 | — | 7.7 | 0.2 | 3.9 | 2.1 | 1.8 |
| Government Public Health Activities | 6.7 | — | — | — | — | — | 6.7 | 1.2 | 5.5 |
| Research and Construction | 11.6 | 4.5 | — | — | — | 4.5 | 7.2 | 5.2 | 2.0 |
| Research | 5.5 | 0.3 | — | — | — | 0.3 | 5.2 | 4.7 | 0.5 |
| Construction | 6.2 | 4.2 | — | — | — | 4.2 | 2.0 | 0.6 | 1.5 |
| 1990 | |||||||||
| National Health Expenditures | $697.5 | $413.1 | $380.8 | $148.4 | $232.4 | $32.3 | $284.3 | $195.8 | $88.5 |
| Health Services and Supplies | 672.9 | 402.9 | 380.8 | 148.4 | 232.4 | 22.1 | 270.0 | 185.4 | 84.6 |
| Personal Health Care | 614.7 | 371.7 | 350.2 | 148.4 | 201.8 | 21.5 | 243.0 | 178.1 | 64.9 |
| Hospital Care | 256.4 | 115.0 | 104.3 | 10.3 | 94.0 | 10.7 | 141.5 | 106.6 | 34.9 |
| Physician Services | 146.3 | 101.4 | 98.7 | 35.4 | 63.3 | 2.7 | 45.0 | 35.9 | 9.1 |
| Dental Services | 31.6 | 30.7 | 30.6 | 15.4 | 15.1 | 0.1 | 0.9 | 0.5 | 0.4 |
| Other Professional Services | 34.7 | 28.2 | 25.6 | 14.2 | 11.4 | 2.6 | 6.5 | 4.3 | 2.2 |
| Home Health Care | 13.1 | 8.0 | 5.9 | 3.6 | 2.3 | 2.2 | 5.1 | 4.1 | 1.0 |
| Drugs and Other Medical Non-Durables | 59.9 | 53.5 | 53.5 | 40.4 | 13.0 | — | 6.5 | 3.1 | 3.4 |
| Vision Products and Other Medical Durables | 10.5 | 7.7 | 7.7 | 6.7 | 0.9 | — | 2.8 | 2.6 | 0.1 |
| Nursing Home Care | 50.9 | 25.0 | 24.1 | 22.2 | 1.9 | 0.9 | 25.9 | 15.7 | 10.2 |
| Other Personal Health Care | 11.2 | 2.2 | — | — | — | 2.2 | 9.0 | 5.4 | 3.6 |
| Program Administration and Net Cost of Private Health Insurance | 38.6 | 31.2 | 30.6 | — | 30.6 | 0.6 | 7.4 | 4.9 | 2.5 |
| Government Public Health Activities | 19.6 | — | — | — | — | — | 19.6 | 2.4 | 17.2 |
| Research and Construction | 24.5 | 10.2 | — | — | — | 10.2 | 14.3 | 10.4 | 3.9 |
| Research | 12.2 | 1.0 | — | — | — | 1.0 | 11.3 | 9.5 | 1.7 |
| Construction | 12.3 | 9.3 | — | — | — | 9.3 | 3.0 | 0.8 | 2.2 |
| 1992 | |||||||||
| National Health Expenditures | 833.6 | 477.0 | 441.0 | 164.4 | 276.6 | 36.0 | 356.5 | 254.8 | 101.8 |
| Health Services and Supplies | 806.0 | 465.9 | 441.0 | 164.4 | 276.6 | 24.9 | 340.1 | 243.0 | 97.1 |
| Personal Health Care | 739.8 | 431.5 | 407.1 | 164.4 | 242.7 | 24.3 | 308.3 | 234.4 | 73.9 |
| Hospital Care | 305.3 | 128.5 | 116.5 | 10.6 | 105.9 | 12.0 | 176.7 | 141.9 | 34.9 |
| Physician Services | 174.7 | 121.9 | 119.4 | 37.9 | 81.5 | 2.5 | 52.7 | 40.9 | 11.8 |
| Dental Services | 37.0 | 35.7 | 35.5 | 18.2 | 17.3 | 0.1 | 1.3 | 0.8 | 0.6 |
| Other Professional Services | 42.1 | 33.1 | 30.1 | 16.0 | 14.2 | 2.9 | 9.0 | 6.3 | 2.8 |
| Home Health Care | 19.6 | 10.8 | 7.9 | 5.0 | 2.9 | 2.9 | 8.8 | 7.4 | 1.4 |
| Drugs and Other Medical Non-Durables | 71.3 | 63.1 | 63.1 | 45.1 | 18.0 | — | 8.2 | 4.1 | 4.1 |
| Vision Products and Other Medical Durables | 11.9 | 8.1 | 8.1 | 7.3 | 0.9 | — | 3.8 | 3.7 | 0.1 |
| Nursing Home Care | 62.3 | 27.6 | 26.4 | 24.3 | 2.1 | 1.2 | 34.7 | 21.5 | 13.2 |
| Other Personal Health Care | 15.6 | 2.6 | — | — | — | 2.6 | 13.0 | 8.0 | 5.0 |
| Program Administration and Net Cost of Private Health Insurance | 42.8 | 34.4 | 33.9 | — | 33.9 | 0.6 | 8.3 | 5.5 | 2.8 |
| Government Public Health Activities | 23.4 | — | — | — | — | — | 23.4 | 3.0 | 20.4 |
| Research and Construction | 27.6 | 11.1 | — | — | — | 11.1 | 16.4 | 11.8 | 4.6 |
| Research | 14.2 | 1.2 | — | — | — | 1.2 | 13.0 | 11.0 | 2.0 |
| Construction | 13.4 | 9.9 | — | — | — | 9.9 | 3.4 | 0.8 | 2.7 |
| 1993 | |||||||||
| National Health Expenditures | $892.3 | $505.1 | $465.8 | $169.4 | $296.5 | $39.2 | $387.2 | $278.5 | $108.6 |
| Health Services and Supplies | 863.1 | 493.1 | 465.8 | 169.4 | 296.5 | 27.2 | 370.0 | 266.5 | 103.6 |
| Personal Health Care | 786.5 | 452.3 | 425.8 | 169.4 | 256.4 | 26.6 | 334.1 | 256.8 | 77.3 |
| Hospital Care | 324.2 | 136.2 | 123.0 | 10.0 | 113.0 | 13.2 | 188.0 | 152.2 | 35.8 |
| Physician Services | 181.1 | 125.1 | 122.3 | 37.0 | 85.3 | 2.7 | 56.0 | 44.0 | 12.0 |
| Dental Services | 39.2 | 37.5 | 37.3 | 19.1 | 18.3 | 0.2 | 1.7 | 1.0 | 0.8 |
| Other Professional Services | 46.3 | 36.0 | 32.8 | 18.1 | 14.7 | 3.3 | 10.3 | 7.4 | 3.0 |
| Home Health Care | 23.0 | 11.9 | 8.7 | 5.6 | 3.1 | 3.2 | 11.1 | 9.6 | 1.5 |
| Drugs and Other Medical Non-Durables | 75.2 | 66.0 | 66.0 | 46.9 | 19.1 | — | 9.2 | 4.7 | 4.4 |
| Vision Products and Other Medical Durables | 12.6 | 8.4 | 8.4 | 7.5 | 0.9 | — | 4.2 | 4.1 | 0.1 |
| Nursing Home Care | 67.0 | 28.5 | 27.3 | 25.2 | 2.1 | 1.2 | 38.5 | 24.7 | 13.8 |
| Other Personal Health Care | 17.8 | 2.8 | — | — | — | 2.8 | 15.0 | 9.2 | 5.8 |
| Program Administration and Net Cost of Private Health Insurance | 51.0 | 40.7 | 40.1 | — | 40.1 | 0.6 | 10.3 | 6.4 | 3.9 |
| Government Public Health Activities | 29.0 | 25.7 | 22.4 | — | — | — | 3.3 | 3.3 | 22.4 |
| Research and Construction | 29.2 | 12.0 | — | — | — | 12.0 | 17.1 | 12.1 | 5.1 |
| Research | 14.5 | 1.2 | — | — | — | 1.2 | 13.3 | 11.2 | 2.1 |
| Construction | 14.7 | 10.8 | — | — | — | 10.8 | 3.9 | 0.9 | 2.9 |
| 1994 | |||||||||
| National Health Expenditures | 949.4 | 528.6 | 488.1 | 174.9 | 313.3 | 40.4 | 420.8 | 303.6 | 117.2 |
| Health Services and Supplies | 919.2 | 517.1 | 488.1 | 174.9 | 313.3 | 28.9 | 402.2 | 290.3 | 111.8 |
| Personal Health Care | 831.7 | 469.9 | 441.6 | 174.9 | 266.8 | 28.2 | 361.8 | 280.0 | 81.8 |
| Hospital Care | 338.5 | 138.9 | 125.5 | 9.8 | 115.7 | 13.4 | 199.6 | 162.7 | 36.8 |
| Physician Services | 189.4 | 128.5 | 125.5 | 35.8 | 89.6 | 3.0 | 60.9 | 48.6 | 12.3 |
| Dental Services | 42.2 | 40.4 | 40.3 | 20.5 | 19.8 | 0.2 | 1.8 | 1.0 | 0.8 |
| Other Professional Services | 49.6 | 38.4 | 34.7 | 19.5 | 15.2 | 3.7 | 11.2 | 8.3 | 2.9 |
| Home Health Care | 26.2 | 13.0 | 9.5 | 6.1 | 3.4 | 3.5 | 13.2 | 11.4 | 1.7 |
| Drugs and Other Medical Non-Durables | 78.6 | 68.6 | 68.6 | 48.6 | 20.0 | — | 10.0 | 5.2 | 4.8 |
| Vision Products and Other Medical Durables | 13.1 | 8.6 | 8.6 | 7.7 | 0.9 | — | 4.5 | 4.4 | 0.1 |
| Nursing Home Care | 72.3 | 30.4 | 29.0 | 26.8 | 2.2 | 1.4 | 41.8 | 27.0 | 14.9 |
| Other Personal Health Care | 21.8 | 3.0 | — | — | — | 3.0 | 18.8 | 11.4 | 7.4 |
| Program Administration and Net Cost of Private Health Insurance | 58.7 | 47.2 | 46.5 | — | 46.5 | 0.7 | 11.5 | 6.6 | 4.9 |
| Government Public Health Activities | 28.8 | — | — | — | — | — | 28.8 | 3.7 | 25.1 |
| Research and Construction | 30.2 | 11.5 | — | — | — | 11.5 | 18.7 | 13.3 | 5.4 |
| Research | 15.9 | 1.3 | — | — | — | 1.3 | 14.7 | 12.4 | 2.3 |
| Construction | 14.3 | 10.3 | — | — | — | 10.3 | 4.0 | 0.9 | 3.1 |
NOTES: The figure 0.0 denotes less than $50 million. Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from research expenditures but are included in the expenditure class in which the product falls. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 12. Personal Health Care Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960–94.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $23.6 | $13.1 | $10.6 | $5.0 | $0.4 | $5.1 | $2.1 | $3.0 | — | — |
| 1970 | 63.8 | 24.9 | 38.9 | 14.8 | 1.6 | 22.5 | 14.7 | 7.8 | $7.3 | $5.1 |
| 1975 | 114.5 | 38.1 | 76.4 | 28.4 | 2.7 | 45.3 | 30.9 | 14.4 | 15.7 | 12.9 |
| 1980 | 217.0 | 60.3 | 156.8 | 62.0 | 7.8 | 87.0 | 63.4 | 23.6 | 36.4 | 24.8 |
| 1985 | 376.4 | 100.6 | 275.8 | 113.8 | 14.1 | 148.0 | 111.3 | 36.7 | 70.3 | 39.2 |
| 1990 | 614.7 | 148.4 | 466.3 | 201.8 | 21.5 | 243.0 | 178.1 | 64.9 | 109.6 | 71.7 |
| 1991 | 676.2 | 155.1 | 521.1 | 221.2 | 23.3 | 276.6 | 205.7 | 70.8 | 120.2 | 90.1 |
| 1992 | 739.8 | 164.4 | 575.4 | 242.7 | 24.3 | 308.3 | 234.4 | 73.9 | 135.9 | 102.5 |
| 1993 | 786.5 | 169.4 | 617.1 | 256.4 | 26.6 | 334.1 | 256.8 | 77.3 | 148.6 | 114.1 |
| 1994 | 831.7 | 174.9 | 656.8 | 266.8 | 28.2 | 361.8 | 280.0 | 81.8 | 166.1 | 122.9 |
| Per Capita Amount | ||||||||||
| 1960 | $124 | $69 | $56 | $26 | $2 | $27 | $11 | $16 | — | — |
| 1970 | 297 | 116 | 181 | 69 | 8 | 105 | 68 | 36 | (3) | (3) |
| 1975 | 510 | 170 | 340 | 126 | 12 | 202 | 138 | 64 | (3) | (3) |
| 1980 | 923 | 256 | 667 | 264 | 33 | 370 | 270 | 100 | (3) | (3) |
| 1985 | 1,525 | 407 | 1,117 | 461 | 57 | 599 | 451 | 149 | (3) | (3) |
| 1990 | 2,369 | 572 | 1,797 | 778 | 83 | 936 | 686 | 250 | (3) | (3) |
| 1991 | 2,578 | 591 | 1,987 | 843 | 89 | 1,054 | 784 | 270 | (3) | (3) |
| 1992 | 2,790 | 620 | 2,170 | 916 | 92 | 1,163 | 884 | 279 | (3) | (3) |
| 1993 | 2,936 | 632 | 2,304 | 957 | 99 | 1,247 | 959 | 289 | (3) | (3) |
| 1994 | 3,074 | 646 | 2,428 | 986 | 104 | 1,337 | 1,035 | 302 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 55.3 | 44.7 | 21.2 | 1.8 | 21.7 | 9.0 | 12.6 | — | — |
| 1970 | 100.0 | 39.0 | 61.0 | 23.2 | 2.6 | 35.3 | 23.0 | 12.2 | 11.4 | 7.9 |
| 1975 | 100.0 | 33.3 | 66.7 | 24.8 | 2.4 | 39.6 | 27.0 | 12.5 | 13.7 | 11.3 |
| 1980 | 100.0 | 27.8 | 72.2 | 28.6 | 3.6 | 40.1 | 29.2 | 10.9 | 16.8 | 11.4 |
| 1985 | 100.0 | 26.7 | 73.3 | 30.2 | 3.7 | 39.3 | 29.6 | 9.7 | 18.7 | 10.4 |
| 1990 | 100.0 | 24.1 | 75.9 | 32.8 | 3.5 | 39.5 | 29.0 | 10.6 | 17.8 | 11.7 |
| 1991 | 100.0 | 22.9 | 77.1 | 32.7 | 3.4 | 40.9 | 30.4 | 10.5 | 17.8 | 13.3 |
| 1992 | 100.0 | 22.2 | 77.8 | 32.8 | 3.3 | 41.7 | 31.7 | 10.0 | 18.4 | 13.9 |
| 1993 | 100.0 | 21.5 | 78.5 | 32.6 | 3.4 | 42.5 | 32.7 | 9.8 | 18.9 | 14.5 |
| 1994 | 100.0 | 21.0 | 79.0 | 32.1 | 3.4 | 43.5 | 33.7 | 9.8 | 20.0 | 14.8 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-94. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 13. Hospital Care Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960–94.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $9.3 | $1.9 | $7.4 | $3.3 | $0.1 | $3.9 | $1.6 | $2.3 | — | — |
| 1970 | 28.0 | 2.5 | 25.5 | 9.1 | 0.9 | 15.5 | 10.2 | 5.3 | $5.4 | $2.7 |
| 1975 | 52.6 | 4.4 | 48.2 | 17.3 | 1.4 | 29.4 | 20.4 | 9.0 | 11.6 | 5.2 |
| 1980 | 102.7 | 5.3 | 97.4 | 36.4 | 5.0 | 55.9 | 42.2 | 13.8 | 26.4 | 10.6 |
| 1985 | 168.3 | 8.8 | 159.5 | 58.7 | 8.3 | 92.5 | 72.5 | 20.0 | 49.1 | 15.8 |
| 1990 | 256.4 | 10.3 | 246.2 | 94.0 | 10.7 | 141.5 | 106.6 | 34.9 | 69.7 | 29.7 |
| 1991 | 282.3 | 11.3 | 271.0 | 100.2 | 11.7 | 159.1 | 123.8 | 35.3 | 76.1 | 38.2 |
| 1992 | 305.3 | 10.6 | 294.7 | 105.9 | 12.0 | 176.7 | 141.9 | 34.9 | 86.5 | 43.4 |
| 1993 | 324.2 | 10.0 | 314.2 | 113.0 | 13.2 | 188.0 | 152.2 | 35.8 | 92.8 | 47.1 |
| 1994 | 338.5 | 9.8 | 328.7 | 115.7 | 13.4 | 199.6 | 162.7 | 36.8 | 101.6 | 49.4 |
| Per Capita Amount | ||||||||||
| 1960 | $49 | $10 | $39 | $17 | $1 | $21 | $8 | $12 | — | — |
| 1970 | 130 | 12 | 119 | 42 | 4 | 72 | 47 | 25 | (3) | (3) |
| 1975 | 234 | 20 | 215 | 77 | 6 | 131 | 91 | 40 | (3) | (3) |
| 1980 | 437 | 23 | 414 | 155 | 21 | 238 | 179 | 59 | (3) | (3) |
| 1985 | 682 | 36 | 646 | 238 | 34 | 375 | 294 | 81 | (3) | (3) |
| 1990 | 988 | 40 | 948 | 362 | 41 | 545 | 411 | 134 | (3) | (3) |
| 1991 | 1,076 | 43 | 1,033 | 382 | 45 | 607 | 472 | 135 | (3) | (3) |
| 1992 | 1,151 | 40 | 1,111 | 400 | 45 | 667 | 535 | 132 | (3) | (3) |
| 1993 | 1,210 | 37 | 1,173 | 422 | 49 | 702 | 568 | 134 | (3) | (3) |
| 1994 | 1,251 | 36 | 1,215 | 428 | 50 | 738 | 602 | 136 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 20.7 | 79.3 | 35.6 | 1.2 | 42.5 | 17.3 | 25.2 | — | — |
| 1970 | 100.0 | 9.0 | 91.0 | 32.4 | 3.2 | 55.4 | 36.4 | 19.0 | 19.2 | 9.5 |
| 1975 | 100.0 | 8.3 | 91.7 | 32.9 | 2.7 | 56.0 | 38.9 | 17.1 | 22.0 | 10.0 |
| 1980 | 100.0 | 5.2 | 94.8 | 35.5 | 4.9 | 54.4 | 41.0 | 13.4 | 25.8 | 10.4 |
| 1985 | 100.0 | 5.2 | 94.8 | 34.9 | 4.9 | 54.9 | 43.1 | 11.9 | 29.2 | 9.4 |
| 1990 | 100.0 | 4.0 | 96.0 | 36.6 | 4.2 | 55.2 | 41.6 | 13.6 | 27.2 | 11.6 |
| 1991 | 100.0 | 4.0 | 96.0 | 35.5 | 4.1 | 56.4 | 43.8 | 12.5 | 27.0 | 13.5 |
| 1992 | 100.0 | 3.5 | 96.5 | 34.7 | 3.9 | 57.9 | 46.5 | 11.4 | 28.4 | 14.2 |
| 1993 | 100.0 | 3.1 | 96.9 | 34.9 | 4.1 | 58.0 | 46.9 | 11.0 | 28.6 | 14.5 |
| 1994 | 100.0 | 2.9 | 97.1 | 34.2 | 4.0 | 59.0 | 48.1 | 10.9 | 30.0 | 14.6 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: Per capita amounts based on July 1 Social Security area population estimates for each year, 1960–94. Numbers and percents may not add to totals because of rounding.
Table 14. Physician Services Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960–94.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $5.3 | $3.3 | $2.0 | $1.6 | $0.0 | $0.4 | $0.1 | $0.3 | — | — |
| 1970 | 13.6 | 5.7 | 7.8 | 4.8 | 0.0 | 3.1 | 2.2 | 0.8 | $1.7 | $0.6 |
| 1975 | 23.9 | 8.8 | 15.1 | 8.4 | 0.1 | 6.6 | 4.8 | 1.9 | 3.4 | 1.8 |
| 1980 | 45.2 | 14.6 | 30.6 | 17.1 | 0.4 | 13.1 | 10.0 | 3.1 | 8.0 | 2.5 |
| 1985 | 83.6 | 24.4 | 59.3 | 33.4 | 1.4 | 24.5 | 19.6 | 4.9 | 16.5 | 3.5 |
| 1990 | 146.3 | 35.4 | 110.9 | 63.3 | 2.7 | 45.0 | 35.9 | 9.1 | 29.5 | 7.1 |
| 1991 | 158.6 | 35.6 | 123.1 | 71.4 | 2.5 | 49.2 | 38.6 | 10.6 | 30.8 | 9.2 |
| 1992 | 174.7 | 37.9 | 136.7 | 81.5 | 2.5 | 52.7 | 40.9 | 11.8 | 31.7 | 11.2 |
| 1993 | 181.1 | 37.0 | 144.1 | 85.3 | 2.7 | 56.0 | 44.0 | 12.0 | 33.9 | 12.6 |
| 1994 | 189.4 | 35.8 | 153.5 | 89.6 | 3.0 | 60.9 | 48.6 | 12.3 | 38.1 | 13.4 |
| Per Capita Amount | ||||||||||
| 1960 | $28 | $17 | $10 | $8 | $0 | $2 | $0 | $2 | — | — |
| 1970 | 63 | 27 | 37 | 22 | 0 | 14 | 10 | 4 | (3) | (3) |
| 1975 | 106 | 39 | 67 | 38 | 0 | 30 | 21 | 8 | (3) | (3) |
| 1980 | 192 | 62 | 130 | 73 | 2 | 56 | 43 | 13 | (3) | (3) |
| 1985 | 339 | 99 | 240 | 135 | 6 | 99 | 79 | 20 | (3) | (3) |
| 1990 | 564 | 137 | 427 | 244 | 10 | 173 | 138 | 35 | (3) | (3) |
| 1991 | 605 | 136 | 469 | 272 | 10 | 188 | 147 | 40 | (3) | (3) |
| 1992 | 659 | 143 | 516 | 307 | 10 | 199 | 154 | 45 | (3) | (3) |
| 1993 | 676 | 138 | 538 | 318 | 10 | 209 | 164 | 45 | (3) | (3) |
| 1994 | 700 | 133 | 568 | 331 | 11 | 225 | 180 | 45 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 62.7 | 37.3 | 30.2 | 0.1 | 7.1 | 1.4 | 5.7 | — | — |
| 1970 | 100.0 | 42.2 | 57.8 | 35.2 | 0.1 | 22.5 | 16.3 | 6.2 | 12.2 | 4.8 |
| 1975 | 100.0 | 36.7 | 63.3 | 35.3 | 0.2 | 27.7 | 19.9 | 7.8 | 14.1 | 7.5 |
| 1980 | 100.0 | 32.4 | 67.6 | 37.9 | 0.8 | 28.9 | 22.1 | 6.8 | 17.6 | 5.6 |
| 1985 | 100.0 | 29.1 | 70.9 | 39.9 | 1.6 | 29.3 | 23.4 | 5.9 | 19.7 | 4.2 |
| 1990 | 100.0 | 24.2 | 75.8 | 43.2 | 1.8 | 30.7 | 24.5 | 6.2 | 20.2 | 4.8 |
| 1991 | 100.0 | 22.4 | 77.6 | 45.0 | 1.6 | 31.0 | 24.3 | 6.7 | 19.4 | 5.8 |
| 1992 | 100.0 | 21.7 | 78.3 | 46.6 | 1.5 | 30.2 | 23.4 | 6.8 | 18.2 | 6.4 |
| 1993 | 100.0 | 20.4 | 79.6 | 47.1 | 1.5 | 30.9 | 24.3 | 6.6 | 18.7 | 7.0 |
| 1994 | 100.0 | 18.9 | 81.1 | 47.3 | 1.6 | 32.1 | 25.7 | 6.5 | 20.1 | 7.1 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: The figure 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $0.50 for per capita amounts. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960–94. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 15. Nursing Home Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960–94.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $0.8 | $0.7 | $0.2 | $0.0 | $0.1 | $0.1 | $0.1 | $0.1 | — | — |
| 1970 | 4.2 | 2.3 | 2.0 | 0.0 | 0.2 | 1.7 | 1.0 | 0.7 | 0.1 | 0.9 |
| 1975 | 8.7 | 3.7 | 5.0 | 0.1 | 0.4 | 4.5 | 2.6 | 1.9 | 0.2 | 4.1 |
| 1980 | 17.6 | 7.4 | 10.3 | 0.2 | 0.5 | 9.5 | 5.6 | 3.9 | 0.3 | 8.8 |
| 1985 | 30.7 | 13.6 | 17.1 | 0.8 | 0.6 | 15.7 | 9.2 | 6.5 | 0.4 | 14.5 |
| 1990 | 50.9 | 22.2 | 28.7 | 1.9 | 0.9 | 25.9 | 15.7 | 10.2 | 1.7 | 23.1 |
| 1991 | 57.2 | 23.4 | 33.8 | 2.1 | 1.1 | 30.7 | 18.4 | 12.3 | 2.0 | 27.5 |
| 1992 | 62.3 | 24.3 | 38.0 | 2.1 | 1.2 | 34.7 | 21.5 | 13.2 | 3.2 | 30.2 |
| 1993 | 67.0 | 25.2 | 41.8 | 2.1 | 1.2 | 38.5 | 24.7 | 13.8 | 4.6 | 32.4 |
| 1994 | 72.3 | 26.8 | 45.4 | 2.2 | 1.4 | 41.8 | 27.0 | 14.9 | 5.9 | 34.3 |
| Per Capita Amount | ||||||||||
| 1960 | $4 | $3 | $1 | $0 | $0 | $1 | $0 | $0 | — | — |
| 1970 | 20 | 11 | 9 | 0 | 1 | 8 | 5 | 3 | (3) | (3) |
| 1975 | 39 | 16 | 22 | 0 | 2 | 20 | 12 | 8 | (3) | (3) |
| 1980 | 75 | 31 | 44 | 1 | 2 | 41 | 24 | 17 | (3) | (3) |
| 1985 | 124 | 55 | 69 | 3 | 2 | 63 | 37 | 26 | (3) | (3) |
| 1990 | 196 | 86 | 111 | 7 | 4 | 100 | 61 | 39 | (3) | (3) |
| 1991 | 218 | 89 | 129 | 8 | 4 | 117 | 70 | 47 | (3) | (3) |
| 1992 | 235 | 92 | 143 | 8 | 4 | 131 | 81 | 50 | (3) | (3) |
| 1993 | 250 | 94 | 156 | 8 | 5 | 144 | 92 | 52 | (3) | (3) |
| 1994 | 267 | 99 | 168 | 8 | 5 | 155 | 100 | 55 | (3) | (3) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 77.9 | 22.1 | 0.0 | 6.3 | 15.7 | 7.9 | 7.8 | — | — |
| 1970 | 100.0 | 53.5 | 46.5 | 0.4 | 4.9 | 41.2 | 24.8 | 16.4 | 3.4 | 22.3 |
| 1975 | 100.0 | 42.6 | 57.4 | 0.8 | 4.8 | 51.9 | 30.5 | 21.3 | 2.5 | 47.1 |
| 1980 | 100.0 | 41.8 | 58.2 | 1.2 | 3.0 | 54.0 | 31.8 | 22.2 | 1.7 | 50.0 |
| 1985 | 100.0 | 44.4 | 55.6 | 2.7 | 1.8 | 51.1 | 29.8 | 21.2 | 1.4 | 47.2 |
| 1990 | 100.0 | 43.6 | 56.4 | 3.7 | 1.9 | 50.8 | 30.8 | 20.0 | 3.3 | 45.4 |
| 1991 | 100.0 | 40.9 | 59.1 | 3.6 | 1.8 | 53.6 | 32.2 | 21.5 | 3.4 | 48.1 |
| 1992 | 100.0 | 39.0 | 61.0 | 3.4 | 1.9 | 55.7 | 34.5 | 21.2 | 5.1 | 48.5 |
| 1993 | 100.0 | 37.6 | 62.4 | 3.1 | 1.9 | 57.5 | 36.8 | 20.7 | 6.8 | 48.4 |
| 1994 | 100.0 | 37.2 | 62.8 | 3.0 | 1.9 | 57.9 | 37.3 | 20.6 | 8.2 | 47.4 |
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: The figure 0.0 denotes less than $50 million for aggregate amounts, and 0 denotes less than $0.50 for per capita amounts. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960–94. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 16. Other Personal Health Care Expenditures1 Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Years 1960–94.
| Year | Total | Out-of-Pocket Payments | Third-Party Payments | Medicare1 | Medicaid2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Private Health Insurance | Other Private Funds | Government | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
| Amount in Billions | ||||||||||
| 1960 | $8.2 | $7.2 | $1.0 | $0.1 | $0.2 | $0.7 | $0.4 | $0.3 | — | — |
| 1970 | 18.0 | 14.4 | 3.6 | 0.9 | 0.5 | 2.2 | 1.2 | 1.0 | NA | NA |
| 1975 | 29.4 | 21.2 | 8.1 | 2.6 | 0.8 | 4.7 | 3.1 | 1.6 | NA | NA |
| 1980 | 51.5 | 32.9 | 18.6 | 8.2 | 1.9 | 8.5 | 5.6 | 2.8 | NA | NA |
| 1985 | 93.9 | 53.8 | 40.1 | 20.8 | 3.9 | 15.4 | 10.1 | 5.3 | NA | NA |
| 1990 | 161.0 | 80.4 | 80.5 | 42.7 | 7.2 | 30.6 | 20.0 | 10.7 | NA | NA |
| 1991 | 178.1 | 84.9 | 93.2 | 47.6 | 8.0 | 37.6 | 24.9 | 12.7 | NA | NA |
| 1992 | 197.6 | 91.5 | 106.0 | 53.3 | 8.6 | 44.1 | 30.2 | 14.0 | NA | NA |
| 1993 | 214.1 | 97.1 | 116.9 | 56.0 | 9.4 | 51.5 | 35.9 | 15.7 | NA | NA |
| 1994 | 231.5 | 102.4 | 129.1 | 59.2 | 10.4 | 59.5 | 41.7 | 17.8 | NA | NA |
| Per Capita Amount | ||||||||||
| 1960 | $43 | $38 | $5 | $1 | $1 | $4 | $2 | $1 | — | — |
| 1970 | 84 | 67 | 17 | 4 | 2 | 10 | 6 | 4 | (4) | (4) |
| 1975 | 131 | 95 | 36 | 11 | 4 | 21 | 14 | 7 | (4) | (4) |
| 1980 | 219 | 140 | 79 | 35 | 8 | 36 | 24 | 12 | (4) | (4) |
| 1985 | 380 | 218 | 162 | 84 | 16 | 62 | 41 | 21 | (4) | (4) |
| 1990 | 620 | 310 | 310 | 165 | 28 | 118 | 77 | 41 | (4) | (4) |
| 1991 | 679 | 324 | 355 | 181 | 31 | 143 | 95 | 48 | (4) | (4) |
| 1992 | 745 | 345 | 400 | 201 | 32 | 167 | 114 | 53 | (4) | (4) |
| 1993 | 799 | 363 | 437 | 209 | 35 | 192 | 134 | 58 | (4) | (4) |
| 1994 | 856 | 379 | 477 | 219 | 39 | 220 | 154 | 66 | (4) | (4) |
| Percent Distribution | ||||||||||
| 1960 | 100.0 | 87.4 | 12.6 | 1.5 | 3.0 | 8.1 | 4.8 | 3.4 | — | — |
| 1970 | 100.0 | 79.9 | 20.1 | 5.0 | 2.8 | 12.3 | 6.9 | 5.3 | NA | NA |
| 1975 | 100.0 | 72.4 | 27.6 | 8.7 | 2.9 | 16.1 | 10.5 | 5.6 | NA | NA |
| 1980 | 100.0 | 63.9 | 36.1 | 16.0 | 3.6 | 16.5 | 11.0 | 5.5 | NA | NA |
| 1985 | 100.0 | 57.3 | 42.7 | 22.2 | 4.1 | 16.4 | 10.8 | 5.6 | NA | NA |
| 1990 | 100.0 | 50.0 | 50.0 | 26.5 | 4.5 | 19.0 | 12.4 | 6.6 | NA | NA |
| 1991 | 100.0 | 47.7 | 52.3 | 26.7 | 4.5 | 21.1 | 14.0 | 7.1 | NA | NA |
| 1992 | 100.0 | 46.3 | 53.7 | 27.0 | 4.4 | 22.3 | 15.3 | 7.1 | NA | NA |
| 1993 | 100.0 | 45.4 | 54.6 | 26.2 | 4.4 | 24.1 | 16.8 | 7.3 | NA | NA |
| 1994 | 100.0 | 44.2 | 55.8 | 25.6 | 4.5 | 25.7 | 18.0 | 7.7 | NA | NA |
Personal health care expenditures other than those for hospital care, physician services, and nursing home care.
Subset of Federal funds.
Subset of Federal and State and local funds.
Calculation of per capita estimates is inappropriate.
NOTES: NA is not available. Per capita amounts based on July 1 Social Security area population estimates for each year, 1960-94. Numbers and percents may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Table 17. Personal Health Care Expenditures, by Type of Expenditure and Source of Funds: Selected Years 1980–94.
| Source of Funds | Total | Hospital Care | Physician Services | Dental Services | Other Professional Services | Home Health Care | Drugs and Other Medical Non-Durables | Vision Products and Other Medical Durables | Nursing Home Care | Other Personal Care |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Amount in Billions | ||||||||||
| 1980 | ||||||||||
| Personal Health Care Expenditures | $217.0 | $102.7 | $45.2 | $13.3 | $6.4 | $2.4 | $21.6 | $3.8 | $17.6 | $4.0 |
| Out-of-Pocket Payments | 60.3 | 5.3 | 14.6 | 8.8 | 3.3 | 0.5 | 17.5 | 2.7 | 7.4 | — |
| Third-Party Payments | 156.8 | 97.4 | 30.6 | 4.5 | 3.1 | 1.9 | 4.1 | 1.0 | 10.3 | 4.0 |
| Private Health Insurance | 62.0 | 36.4 | 17.1 | 3.8 | 1.1 | 0.4 | 2.4 | 0.4 | 0.2 | — |
| Other Private | 7.8 | 5.0 | 0.4 | 0.0 | 0.5 | 0.5 | — | — | 0.5 | 0.9 |
| Government | 87.0 | 55.9 | 13.1 | 0.6 | 1.5 | 1.0 | 1.7 | 0.6 | 9.5 | 3.1 |
| Federal | 63.4 | 42.2 | 10.0 | 0.4 | 1.1 | 0.8 | 0.9 | 0.5 | 5.6 | 2.0 |
| Medicare | 36.4 | 26.4 | 8.0 | — | 0.6 | 0.7 | — | 0.4 | 0.3 | — |
| Medicaid | 13.7 | 5.8 | 1.4 | 0.3 | 0.1 | 0.2 | 0.8 | — | 4.9 | 0.2 |
| Other | 13.3 | 9.9 | 0.6 | 0.1 | 0.4 | 0.0 | 0.0 | 0.1 | 0.4 | 1.8 |
| State and Local | 23.6 | 13.8 | 3.1 | 0.3 | 0.4 | 0.1 | 0.8 | 0.1 | 3.9 | 1.1 |
| Medicaid | 11.1 | 4.9 | 1.1 | 0.2 | 0.1 | 0.1 | 0.6 | — | 3.9 | 0.2 |
| Other | 12.5 | 8.9 | 2.0 | 0.1 | 0.3 | 0.0 | 0.2 | 0.1 | 0.0 | 0.9 |
| Total Medicaid | 24.8 | 10.6 | 2.5 | 0.5 | 0.2 | 0.3 | 1.4 | — | 8.8 | 0.4 |
| 1990 | ||||||||||
| Personal Health Care Expenditures | 614.7 | 256.4 | 146.3 | 31.6 | 34.7 | 13.1 | 59.9 | 10.5 | 50.9 | 11.2 |
| Out-of-Pocket Payments | 148.4 | 10.3 | 35.4 | 15.4 | 14.2 | 3.6 | 40.4 | 6.7 | 22.2 | — |
| Third-Party Payments | 466.3 | 246.2 | 110.9 | 16.1 | 20.5 | 9.5 | 19.5 | 3.7 | 28.7 | 11.2 |
| Private Health Insurance | 201.8 | 94.0 | 63.3 | 15.1 | 11.4 | 2.3 | 13.0 | 0.9 | 1.9 | — |
| Other Private | 21.5 | 10.7 | 2.7 | 0.1 | 2.6 | 2.2 | — | — | 0.9 | 2.2 |
| Government | 243.0 | 141.5 | 45.0 | 0.9 | 6.5 | 5.1 | 6.5 | 2.8 | 25.9 | 9.0 |
| Federal | 178.1 | 106.6 | 35.9 | 0.5 | 4.3 | 4.1 | 3.1 | 2.6 | 15.7 | 5.4 |
| Medicare | 109.6 | 69.7 | 29.5 | — | 3.3 | 3.0 | — | 2.5 | 1.7 | — |
| Medicaid | 40.5 | 16.7 | 4.2 | 0.4 | 0.3 | 1.1 | 2.9 | — | 13.0 | 2.0 |
| Other | 28.0 | 20.1 | 2.2 | 0.1 | 0.7 | 0.0 | 0.1 | 0.2 | 1.0 | 3.5 |
| State and Local | 64.9 | 34.9 | 9.1 | 0.4 | 2.2 | 1.0 | 3.4 | 0.1 | 10.2 | 3.6 |
| Medicaid | 31.1 | 13.0 | 2.9 | 0.3 | 0.2 | 1.0 | 2.2 | — | 10.1 | 1.5 |
| Other | 33.7 | 21.9 | 6.2 | 0.1 | 2.0 | 0.0 | 1.2 | 0.1 | 0.1 | 2.1 |
| Total Medicaid | 71.7 | 29.7 | 7.1 | 0.7 | 0.5 | 2.1 | 5.1 | — | 23.1 | 3.5 |
| 1992 | ||||||||||
| Personal Health Care Expenditures | 739.8 | 305.3 | 174.7 | 37.0 | 42.1 | 19.6 | 71.3 | 11.9 | 62.3 | 15.6 |
| Out-of-Pocket Payments | 164.4 | 10.6 | 37.9 | 18.2 | 16.0 | 5.0 | 45.1 | 7.3 | 24.3 | — |
| Third-Party Payments | 575.4 | 294.7 | 136.7 | 18.8 | 26.1 | 14.6 | 26.2 | 4.7 | 38.0 | 15.6 |
| Private Health Insurance | 242.7 | 105.9 | 81.5 | 17.3 | 14.2 | 2.9 | 18.0 | 0.9 | 2.1 | — |
| Other Private | 24.3 | 12.0 | 2.5 | 0.1 | 2.9 | 2.9 | — | — | 1.2 | 2.6 |
| Government | 308.3 | 176.7 | 52.7 | 1.3 | 9.0 | 8.8 | 8.2 | 3.8 | 34.7 | 13.0 |
| Federal | 234.4 | 141.9 | 40.9 | 0.8 | 6.3 | 7.4 | 4.1 | 3.7 | 21.5 | 8.0 |
| Medicare | 135.9 | 86.5 | 31.7 | — | 5.0 | 5.9 | — | 3.4 | 3.2 | — |
| Medicaid | 65.9 | 32.1 | 6.6 | 0.6 | 0.4 | 1.5 | 3.9 | — | 17.1 | 3.7 |
| Other | 32.6 | 23.2 | 2.5 | 0.1 | 0.8 | 0.0 | 0.2 | 0.2 | 1.3 | 4.3 |
| State and Local | 73.9 | 34.9 | 11.8 | 0.6 | 2.8 | 1.4 | 4.1 | 0.1 | 13.2 | 5.0 |
| Medicaid | 36.6 | 11.3 | 4.5 | 0.5 | 0.3 | 1.3 | 2.8 | — | 13.1 | 2.7 |
| Other | 37.3 | 23.6 | 7.3 | 0.1 | 2.4 | 0.1 | 1.3 | 0.1 | 0.1 | 2.3 |
| Total Medicaid | 102.5 | 43.4 | 11.2 | 1.1 | 0.8 | 2.8 | 6.7 | — | 30.2 | 6.3 |
| 1993 | ||||||||||
| Personal Health Care Expenditures | $786.5 | $324.2 | $181.1 | $39.2 | $46.3 | $23.0 | $75.2 | $12.6 | $67.0 | $17.8 |
| Out-of-Pocket Payments | 169.4 | 10.0 | 37.0 | 19.1 | 18.1 | 5.6 | 46.9 | 7.5 | 25.2 | — |
| Third-Party Payments | 617.1 | 314.2 | 144.1 | 20.2 | 28.2 | 17.4 | 28.2 | 5.1 | 41.8 | 17.8 |
| Private Health Insurance | 256.4 | 113.0 | 85.3 | 18.3 | 14.7 | 3.1 | 19.1 | 0.9 | 2.1 | — |
| Other Private | 26.6 | 13.2 | 2.7 | 0.2 | 3.3 | 3.2 | — | — | 1.2 | 2.8 |
| Government | 334.1 | 188.0 | 56.0 | 1.7 | 10.3 | 11.1 | 9.2 | 4.2 | 38.5 | 15.0 |
| Federal | 256.8 | 152.2 | 44.0 | 1.0 | 7.4 | 9.6 | 4.7 | 4.1 | 24.7 | 9.2 |
| Medicare | 148.6 | 92.8 | 33.9 | — | 5.8 | 7.8 | — | 3.8 | 4.6 | — |
| Medicaid | 73.7 | 34.7 | 7.6 | 0.9 | 0.8 | 1.8 | 4.5 | — | 18.7 | 4.8 |
| Other | 34.5 | 24.7 | 2.6 | 0.1 | 0.8 | 0.0 | 0.2 | 0.3 | 1.4 | 4.4 |
| State and Local | 77.3 | 35.8 | 12.0 | 0.8 | 3.0 | 1.5 | 4.4 | 0.1 | 13.8 | 5.8 |
| Medicaid | 40.4 | 12.4 | 5.0 | 0.7 | 0.6 | 1.5 | 3.2 | — | 13.8 | 3.4 |
| Other | 36.9 | 23.4 | 7.0 | 0.1 | 2.4 | 0.1 | 1.3 | 0.1 | 0.1 | 2.5 |
| Total Medicaid | 114.1 | 47.1 | 12.6 | 1.5 | 1.4 | 3.2 | 7.7 | — | 32.4 | 8.1 |
| 1994 | ||||||||||
| Personal Health Care Expenditures | 831.7 | 338.5 | 189.4 | 42.2 | 49.6 | 26.2 | 78.6 | 13.1 | 72.3 | 21.8 |
| Out-of-Pocket Payments | 174.9 | 9.8 | 35.8 | 20.5 | 19.5 | 6.1 | 48.6 | 7.7 | 26.8 | — |
| Third-Party Payments | 656.8 | 328.7 | 153.5 | 21.7 | 30.2 | 20.1 | 30.0 | 5.4 | 45.4 | 21.8 |
| Private Health Insurance | 266.8 | 115.7 | 89.6 | 19.8 | 15.2 | 3.4 | 20.0 | 0.9 | 2.2 | — |
| Other Private | 28.2 | 13.4 | 3.0 | 0.2 | 3.7 | 3.5 | — | — | 1.4 | 3.0 |
| Government | 361.8 | 199.6 | 60.9 | 1.8 | 11.2 | 13.2 | 10.0 | 4.5 | 41.8 | 18.8 |
| Federal | 280.0 | 162.7 | 48.6 | 1.0 | 8.3 | 11.4 | 5.2 | 4.4 | 27.0 | 11.4 |
| Medicare | 166.1 | 101.6 | 38.1 | — | 6.8 | 9.5 | — | 4.1 | 5.9 | — |
| Medicaid | 78.4 | 36.1 | 8.0 | 0.9 | 0.7 | 1.9 | 4.9 | — | 19.5 | 6.4 |
| Other | 35.4 | 25.0 | 2.5 | 0.1 | 0.8 | 0.0 | 0.2 | 0.3 | 1.5 | 5.0 |
| State and Local | 81.8 | 36.8 | 12.3 | 0.8 | 2.9 | 1.7 | 4.8 | 0.1 | 14.9 | 7.4 |
| Medicaid | 44.5 | 13.3 | 5.4 | 0.7 | 0.5 | 1.6 | 3.5 | — | 14.8 | 4.7 |
| Other | 37.3 | 23.5 | 6.9 | 0.1 | 2.4 | 0.1 | 1.3 | 0.1 | 0.1 | 2.7 |
| Total Medicaid | 122.9 | 49.4 | 13.4 | 1.6 | 1.2 | 3.5 | 8.4 | — | 34.3 | 11.1 |
NOTES: 0.0 denotes amounts less than $50 million. Medicaid expenditures exclude Part B premium payments to Medicare by States under buy-in agreements to cover premiums for eligible Medicaid recipients. Numbers may not add to totals because of rounding.
SOURCE: Health Care Financing Administration, Office of the Actuary: Data from the Office of National Health Statistics.
Footnotes
The authors are with the Office of the Actuary, Health Care Financing Administration (HCFA). The opinions expressed are those of the authors and do not necessarily reflect those of HCFA.
Benchmark revisions to estimates of GDP were introduced in January 1996 and have been included here. The substantial upward revision to GDP is the major reason why NHE fell as a share of GDP from the 13.9 percent reported last year for 1993 to the 13.6 percent recorded in this set of estimates for the same year.
In this report, the new GDP chain-type annual-weighted price index is used to measure economywide inflation (Landefeld and Parker, 1995).
Caution should be used in interpreting real expenditure growth. With the expansion of managed care and increased use of negotiated price discounts, indices used to deflate nominal expenditures for some components of personal health care spending became less effective in measuring actual transaction prices or amounts paid. For that reason, we use a HCFA-developed hospital transaction price index (Fisher, 1992) instead of the consumer price index (CPI) for years 1960-92. The U.S. Bureau of Labor Statistics began publishing a producer price index (PPI) for hospital services in 1993 and for physician services in 1994. PPIs are designed to measure transaction prices rather than full charge or list prices. As PPIs are incorporated in the calculation of the PHCE chain-weighted price index, our ability to measure medical price inflation will improve.
Medicare began in 1966. During the first 3 years of Medicare, the enrollment of new program beneficiaries and the accompanying pent-up demand for services created enormous growth rates in expenditures of up to 175 percent. Therefore, the first year used in this analysis is 1969, after the initial influx of aged beneficiaries but before the inclusion of the disabled population.
Employer-sponsored private health insurance covers six out of every seven privately insured persons.
Home health agencies also operate out of hospitals and other medical facilities. In these cases, expenditures for those services are included in the NHE category of the sponsoring establishment. Estimates shown for this category contain a conceptual revision: They now include home health services delivered by government agencies. In 1994, this adjustment added $3 billion to home health agency expenditures, amounts that would otherwise have been included in State and local government public health expenditures.
Foster Higgins (1994) reported 1994 premium increases of 2.1 percent in preferred provider organization (PPO) plans and 10.5 percent in POS plans, and KPMG Peat Marwick (1992-94) reported premium increases of 3.2 percent in PPO plans and 5.9 percent in POS plans.
See previous section on Medicare and Private Health Insurance—A Comparison.
Annual reports on the status and operations of the trust funds are published by the Board of Trustees, Federal Hospital Insurance and Supplementary Medical Insurance Trust Funds. These reports are available from the Office of the Actuary, Health Care Financing Administration.
Reprint Requests: Office of National Health Statistics, Health Care Financing Administration, 7500 Security Boulevard, N3-02-02, Baltimore, Maryland 21244-1850.
References
- Aaron H. Thinking Straight About Medical Costs. Health Affairs. 1994;13(5):8–13. doi: 10.1377/hlthaff.13.5.7. [DOI] [PubMed] [Google Scholar]
- American Dental Association. 1993 Survey of Infection Control and OSHA Compliance Costs. Chicago: Sep, 1994. [Google Scholar]
- American Medical Association. Socioeconomic Characteristics of Medical Practice, 1996. Chicago: 1996. [Google Scholar]
- Arnold W, Dobosenski T. Are Physician Compensation Trends as Predicted? Group Practice Journal. 1995 Sep-Oct;:14–16. [Google Scholar]
- Emmons DW, Simon CJ. Socioeconomic Characteristics of Medical Practice, 1995. Chicago: American Medical Association; 1995. Managed Care: Participation, Revenues, and Risk. [Google Scholar]
- Fisher CR. Trends in Total Hospital Financial Performance Under the Prospective Payment System. Health Care Financing Review. 1992 Spring;13(4):1–16. [PMC free article] [PubMed] [Google Scholar]
- Foster Higgins. National Survey of Employer-Sponsored Health Plans, 1994: Report. New York: Foster Higgins Survey and Research Services; 1994. [Google Scholar]
- Gabel J, Formisano R, Lohr B, DiCarlo S. Tracing the Cycle of Health Insurance. Health Affairs. 1991 Winter;10(4):48–61. doi: 10.1377/hlthaff.10.4.48. [DOI] [PubMed] [Google Scholar]
- Genuardi JS, Stiller JM, Trapnell GR. Changing Prescription Drug Sector: New Expenditure Methodologies. Health Care Financing Review. 1996 Spring;17(3):XX–XX. [PMC free article] [PubMed] [Google Scholar]
- Health Care Financing Administration. Total Cost-Sharing Liability of Medicare Beneficiaries by Type of Coverage. Health Care Financing Review Statistical Supplement: 43 and 190. 1995 [Google Scholar]
- KPMG Peat Marwick. Health Benefits in 1994 (Also 1992 and 1993 ed) Newark, NJ.: 1992-94. [Google Scholar]
- Landefeld JS, Parker RP. Survey of Current Business. Washington: U.S. Government Printing Office; Jul, 1995. Preview of the Comprehensive Revision of the National Income and Product Accounts: BEA's New Featured Measures of Output and Prices. [Google Scholar]
- Lazenby HC, Levit KR, Waldo DR, et al. National Health Accounts: Lessons From the U.S. Experience. Health Care Financing Review. 1992 Summer;13(4):89–104. [PMC free article] [PubMed] [Google Scholar]
- Levit KR, Sensenig AL, Cowan CA, et al. National Health Expenditures, 1993. Health Care Financing Review. 1994 Fall;16(1):247–294. [PMC free article] [PubMed] [Google Scholar]
- Moser JW. Socioeconomic Characteristics of Medical Practice, 1996. Chicago: American Medical Association; 1996. Trends and Patterns in Physician Income. [Google Scholar]
- National Center for Health Statistics. Health, United States, 1995. Hyattsville, MD.: Public Health Service; 1996. [Google Scholar]
- Sensenig AL, Heffler SK, Donham CS. Health Care Indicators: Hospital, Employment, and Price Indicators for the Health Care Industry: Third Quarter 1995. Health Care Financing Review. 1996 Spring;17(3):XX–XX. [PMC free article] [PubMed] [Google Scholar]
- Terry K. Forecast for Doctors: Stronger Winds of Change. Medical Economics. 1995 Dec 11;72(23):160–171. [PubMed] [Google Scholar]
- U.S. Bureau of the Census. Current Construction Reports—Value of New Construction Put in Place. Washington: U.S. Government Printing Office; 1995. [Google Scholar]
- US Bureau of Economic Analysis. Gross Domestic Product: Third Quarter 1995 (Preliminary); Corporate Profits: Third Quarter 1995 (Preliminary; Revised Estimates, 1993-95. Washington: Jan 19, 1996. Press release from the U.S. Department of Commerce. [Google Scholar]
- U.S. Bureau of Labor Statistics. Employee Benefits in Medium and Large Firms, 1993. Washington: U.S. Government Printing Office; Nov, 1994. Bulletin 2456. U.S. Department of Labor. [Google Scholar]