Abstract
U.S. Healthcare has developed a quality-based compensation model through which its primary care physicians, hospitals, and specialists can earn additional compensation based on the quality and cost-effectiveness of the care they provide to their patients. The model clearly delineates the expectations of U.S. Healthcare, and in contrast with traditional payment models, encourages improvement in performance. In addition, the model aligns the incentives of U.S. Healthcare purchasers, participating providers, and members in order to provide high-quality, cost-effective care that maximizes patient outcomes.
Introduction
The rapid penetration of managed care in U.S. health care markets needs to be viewed in the perspective of the past and the future. The fee-for-service (FFS) compensation model of the past, in the absence of accountability, is no longer an option. Alternative strategies of either regulation (e.g., the government, an all-payer system) or provider and consumer self-control based on incentives (i.e., measuring performance and providing incentives for superior performance) need to be carefully evaluated. The traditional systems in the United States have had an incentive to provide more care in the absence of appropriateness criteria for the majority of the health care delivered. There has been little if any incentive for preventive care and an acceleration of the maldistribution of resources. There is a reasonable body of literature that has attempted to evaluate the effect of different payment methods on the quality of care, and the overall conclusion in the majority of these studies is that the quality of care in managed care is equal to or better in health maintenance organizations (HMOs) than that in the fee-for-service sector (Udvarhelyi et al., 1991). Nevertheless, concern about incentives in managed care continues to exist. The creation of incentives for quality has not been a part of traditional systems and certainly appears to have intrinsic value.
In 1987, U.S. Healthcare introduced the concept of quality-based compensation for primary care physicians (PCPs) with the development of the Quality Care Compensation System (QCCS) for its participating PCPs. This innovative approach has facilitated the transition from the traditional incentives of FFS physician payment, communicated U.S. Healthcare's expectations to its participating providers, and helped bring accountability to physicians who care for the company's members.
U.S. Healthcare's current membership includes more than 2,250,000 fully insured members, 130,000 Medicare members, 86,000 Medicaid members, 10,000 State-sponsored uninsured children, and more than 500,000 employees of self-insured employers who contract with U.S. Healthcare for medical management services. Small and large employers, as well as government agencies, are the primary purchasers of the company's health plans. These purchasers have begun to demand value (cost and quality) for the increasingly large number of dollars they spend on health care. U.S. Healthcare's premise is that by emphasizing quality, both improved member outcomes and cost savings will follow. In this way, U.S. Healthcare has balanced the incentive for cost-effective delivery of care with the incentive to maximize quality.
U.S. Healthcare is an independent practice association (IPA) model managed-care organization that directly contracts with approximately 15,000 primary care physicians in more than 7,500 offices, 45,000 specialists, and 400 hospitals. As an IPA-model HMO, the company does not directly provide health care services; the providers with whom it contracts are in private practice. These providers also offer health care services to members of other managed-care organizations and to traditionally insured patients. For example, in primary care, U.S. Healthcare members may represent anywhere from less than 5 percent of a practice's patients to more than 50 percent.
U.S. Healthcare has contractual relationships with each of its participating providers. PCPs receive a set amount per capitated member per month, adjusted for the age and sex of the office's membership. Hospitals are typically paid through an FFS arrangement, which generally includes a per diem rate paid for each day the member spends in the hospital, but may also include case rates for the entire hospital stay; in rare instances, the payment may be based on a percentage of the actual charges. Hospital-based physicians, such as anesthesiologists and emergency department physicians, are generally paid as a component of the inpatient costs paid directly to the hospital. Many ancillary specialists, such as radiologists and clinical laboratories, are typically paid by capitation, and selection is made by the PCP. Most of the specialists who are decisionmakers in the health care process (managing specialists) are paid on an FFS basis according to U.S. Healthcare's fee schedule.
These compensation arrangements have formed the foundation upon which U.S. Healthcare has introduced its quality-based compensation models. For each provider type, U.S. Healthcare has developed a formula in which there is a base compensation and an opportunity for additional compensation based on the quality and cost-effectiveness of care provided. This added compensation is determined from measures of clinical performance, with a distinct emphasis on quality of care and service.
An overriding principle in the development of a performance-based compensation model is that it must have the support and acceptance of those being measured. In general, the approach is to utilize a guideline issued by a nationally respected organization and to allow for adaptation based on local circumstances or new medical knowledge (Brook, 1989; Eddy, 1990). The company's 35 medical directors, corporate and regionally based, evaluate evidence-based guidelines and determine their applicability to the U.S. Healthcare network. Performance measurement for the company is done by its subsidiary, U.S. Quality Algorithms, Inc. (USQA), and has benefited from the input of advisory committees composed of participating physicians. Each of U.S. Healthcare's plans has a quality-improvement committee composed of participating providers who help to define the measures to be incorporated into the compensation models.
Currently, state-of-the art measurement of performance has some limitations. Measures of process refer to whether something is done or not. They are often limited by the lack of evidence-based guidelines from which to derive performance measures. Complication rates are often the only relevant outcomes data that are routinely collected, and the reliability of these data in available administrative data sets is problematic. In addition, outcome measures generally require risk adjustment, which remains an inexact science. U.S. Healthcare's data systems use an office or a group of PCPs or specialists as the unit of analysis. The ability to determine an individual physician's performance is limited, and performance measurement at the office level allows for greater sample sizes and encourages officewide quality-improvement efforts. An additional limitation of performance measures is that they are only as good as the data upon which they are based. The company derives the raw material for most of its work from administrative data sets and supplements this material with data from abstracted medical charts, from members responding to satisfaction surveys, and increasingly, through the use of outcomes measurements (Lasker, Shapiro, and Tucker, 1992; McNeil, Pederson, and Gatsonis, 1992).
The nature of the administrative data is related to the organization of U.S. Healthcare's medical delivery system. All primary care services are capitated, and clinical data about the nature of each encounter are submitted electronically or on an encounter form. Most specialty and hospital care is paid for by some form of fee-schedule-based payment and is submitted as a claim for reimbursement. U.S. Healthcare also manages pharmacy benefits for the majority of its members and therefore has access to pharmacy-claims information. U.S. Healthcare's patient management personnel are a valuable source of clinical information based on their recording of pertinent clinical facts from inpatient, outpatient, and same-day surgery cases. Outpatient laboratory results data are also available from U.S. Healthcare's contracted clinical laboratories.
Primary Care Physician Compensation System
PCPs are paid on a capitated basis in U.S. Healthcare's medical delivery system, with rates adjusted for the age and sex of members. Each member chooses a PCP who coordinates that member's care. The PCP is expected to focus on health maintenance and early identification of disease, and to make medically indicated decisions that relate to the management of patients by the appropriate provider in the appropriate setting.
Prior to 1987, U.S. Healthcare had a “withhold” model, similar to that of many other managed-care organizations using a capitated primary model. Each PCP received 80 percent of the capitated rate on a bimonthly basis. Based on the total costs of care provided during the course of the year, a portion of the total aggregate withheld amount across all PCPs would be returned at year-end in the form of a distribution. The proportion of the distribution for which each PCP practice was eligible depended on his or her own performance in providing cost-effective care based on a measure of the total FFS costs incurred by the members within the individual PCP's practice. The withheld amount was an incentive to discourage overutilization of inappropriate medical care. One of the limitations of that model was a lack of financial accountability for the quality of medical care and services provided. In addition, the year-end distribution pool was determined by aggregate performance of all providers, diluting the individual accountability of the PCP practices (Schlackman, 1993; Franks, 1992; Hurley, Freund, and Gage, 1991; Greco and Eisenberg, 1993).
In 1987, U.S. Healthcare introduced measures of quality through its QCCS model. The introduction of this second-generation compensation model provided participating PCPs with the opportunity to increase their capitated payment and receive additional distributions based on their measured performance in providing improved quality of care and service and appropriate resource utilization for members. PCP practices were categorized into one of five performance categories. Both quality and cost-effectiveness were considered in deriving the performance levels. Quality of care was measured through focused medical chart reviews of compliance with various health-maintenance performance standards.1 Quality of service was measured through member satisfaction and rates of transfer from one PCP office to another geographically proximate office within U.S. Healthcare. Philosophy of managed care was assessed by medical directors and professional service coordinators based on the PCP's participation in various managed-care programs. Utilization was determined through hospital inpatient days, specialist FFS costs, and emergency department FFS costs (Schlackman, 1989).
The category of performance affected compensation in two ways. First, it determined the percentage of capitation that was paid (category I received 100 percent of the maximum available capitation payment, II received 90 percent, III received 80 percent, IV received 70 percent, and V received 60 percent). It should be noted that 80 percent of the maximum capitation was the prior year's rate paid to PCPs. Second, the category determined how frequently the office qualified to receive its distribution payment (I and II were monthly, III was every 2 months, and IV and V were semiannually). This model valued quality and utilization with 40 percent based on quality and 60 percent based on utilization of services. A significant defect in this model was that an office might suffer a 20-percent decrease from one year to the next if it dropped from a category I to a category III. For offices with a large number of U.S. Healthcare members, this sizable decrease in payment presented a difficult management task.
The QCCS was refined in 1992, when the present, third-generation model was introduced. Office categorization was replaced with the concept of a quality factor, which is based on a linear scale of performance allowing for less dramatic shifts in performance and compensation level. The base capitation rate is adjusted for the age, sex, plan type (commercial, Medicare, Medicaid) of the membership, and overall quality factor of the office (explained in more detail later). This provides for much more timely feedback of performance and rewards for better performance.
Distribution payments were also changed in 1992. All PCP offices meeting certain minimum member thresholds are eligible for distribution based on utilization of medical services that are paid monthly. An additional payment, based on whether the PCP office is open to new members or existing members, was incorporated as an added semiannual office-status payment. Therefore, the total compensation of a PCP accrues from three separate sources: the base capitation payment that is adjusted by the office-quality factor, quality-factored distributions, and office-status payments.
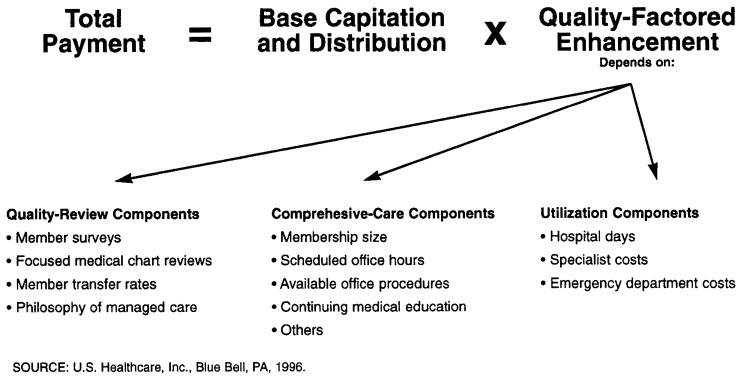
The enhancement of capitation payments and the eligibility for additional distributions is driven by the PCP office's overall quality factor, which is derived from three components on a semiannual basis: quality review, comprehensive care, and utilization (Figure 1). Although utilization of medical resources remains as a component in the QCCS model, the proportion of the additional capitation payment that is related to utilization has dropped from 60 percent to 18 percent in this model. Overall, the quality factor may add as much as 29 percent to the base capitation, with the average being approximately 12-14 percent.
Figure 1. Formula for Total Payment and Components of the Office Quality Factor for Primary Care Physicians Under the Quality Care Compensation System.
Quality review includes measures related to satisfaction from member surveys, member transfer rates, focused medical chart reviews (described in footnote 1), and the PCP office's philosophy of managed care. Approximately 85 percent of an office's members are surveyed, with a response rate of around 32 percent.
The comprehensive-care components of the quality factor relate to measures that enhance a PCP office's ability to thrive in a managed-care system and to how well their office provides optimal access and service to U.S. Healthcare members. The nine measures included under comprehensive care are: membership size, scheduled office hours, available office procedures, participation in U.S. Healthcare-sponsored continuing medical education, internal practice coverage, care provided for catastrophic cases, participation in patient management, practice growth, and the presence of a computer link to U.S. Healthcare.
Utilization measures include the use of hospitals, as measured in bed days, and the use of specialist care and emergency department services (FFS costs). Catastrophic cases, defined as those with hospital inpatient costs of more than $20,000 for adults or $10,000 for children, or those with $5,000 in specialty physician expenses, are eliminated from the determinations. Distribution tables are developed that adjust for the age and sex of the capitated membership. Performance is broken into deciles based on how an individual office compares with its peers (e.g., family practice is compared with family practice).
In addition to quality-based capitation, the office has the opportunity to receive monthly and year-end distributions. The distribution is based on a combination of the decile of performance that the office achieves, based on its distribution tables for the three utilization measures. The actual payment, however, is multiplied by the quality review and comprehensive-care components of the quality factor, thus providing a “check and balance” for any PCP offices that might be inclined to sacrifice quality and service to achieve lower utilization. The enhancement of the distribution by the quality-review and comprehensive-care components provides a strong incentive to provide quality care and earn additional percentage points to increase the utilization-performance distributions.
The office-status payment is made twice a year. The office must not only be open to new and/or existing U.S. Healthcare members but must also meet threshold quality-review and comprehensive-care scores in order to be eligible for the additional payment. If the office is presently accepting only patients who are already patients of that office but who change coverage to U.S. Healthcare, the office receives a smaller amount than an office that accepts patients who are new to the practice as well as being new U.S. Healthcare members. If the office is closed to any new U.S. Healthcare members, the office receives no status payment. The PCP office may receive up to 5 percent of the capitation payments for the previous 6 months by this status-payment methodology. This ability to earn additional monies is a strong incentive to the PCPs to remain open to new U.S. Healthcare members.
The QCCS model and the PCP office's performance are discussed with each office on a regular basis. Each PCP office is visited at least quarterly by a professional services coordinator. These visits are designed to enhance communication with the physicians and staff in each participating office and to assist U.S. Healthcare in being responsive to the PCP network and their needs. New programs, protocols, patient care issues, U.S. Healthcare service levels, physician responses, procedural changes, and other issues are discussed during these visits. In addition, each PCP office is visited yearly by a U.S. Healthcare medical director. At this visit, the QCCS scores are discussed, along with office growth and development, office performance, utilization, medical management, peer comparison, and other topics. The medical director visit serves to keep U.S. Healthcare in close communication with the PCP office and provides opportunities for PCP input into the compensation system.
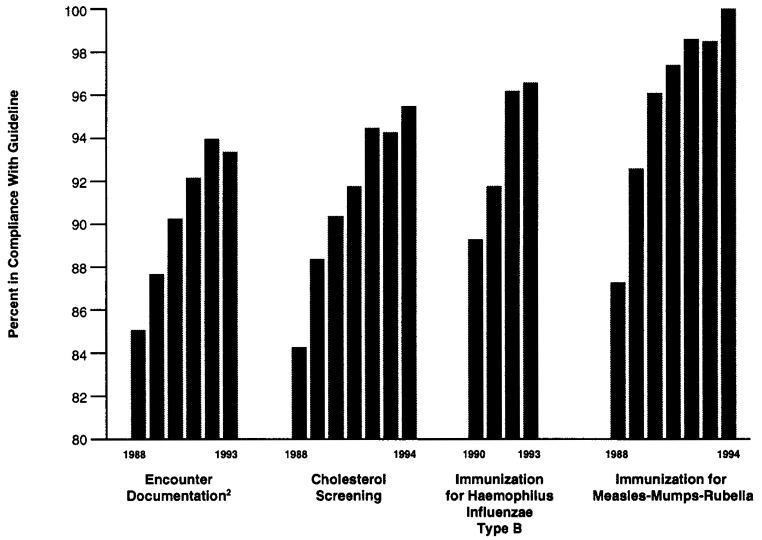
The QCCS has been successful in improving quality within U.S. Healthcare's medical delivery system. Figure 2 shows the improvement in those quality-review measures derived from the medical chart evaluations. As can be seen, there has been steady improvement in the quality of care, demonstrated by audits since the implementation of the QCCS; this improvement is further supported by a recent evaluation (Morrow, Gooding, and Clark, 1995).
Figure 2. Improvement in Quality-Review Measures1 Under the Quality Care Compensation System: Selected Years 1988-94.
1Based on compliance with established guidelines; compliance is determined from medical chart evaluations.
2Documentation criteria include: legibility, patient identification, date of visit, problem list, vital signs, chief complaint, history of illness, physician findings, impression of diagnosis, plan, and provider identification.
SOURCE: U.S. Healthcare, Inc., Blue Bell, PA, 1996.
Currently, the QCCS has limitations in offices with smaller numbers of U.S. Healthcare members. Minimum thresholds for measurement have been defined to maintain the credibility of the inferences drawn about performance. Up to the point at which minimum thresholds are met, the quality-assessment process is still operational, however, offices are assigned average scores rather than their actual scores, which would have wide confidence intervals. There is a process in place, using the regional medical directors, by which offices may question any of their performance scores.
A future enhancement of the QCCS will be the implementation of an approach to severity adjustment, based on work currently under development by USQA, U.S. Healthcare's performance-measurement subsidiary, to adjust for the burden of illness in the capitated member populations.
Captainer Hospital Compensation Model
U.S. Healthcare typically reimburses hospitals through an FFS model. In contracting with hospitals, the trend has been to move to per diem rates in which a fixed, negotiated amount is paid for each day spent in the hospital, with different rates for each level of care (e.g., intensive care, acute care) and benefit type (surgical service, medical acute care bed). Occasionally, U.S. Healthcare has also used a diagnosis-related group (DRG) type of arrangement in which a case rate is applied to hospitalization, no matter how many hospital days or other resources are consumed (Feldman et al., 1990).
The quality-based compensation model for hospital care (CapTainer) provides incentives to hospitals to improve the quality and cost-effectiveness of care provided in the inpatient setting. Through the CapTainer measurement and contracting methodology, hospitals are afforded the opportunity to share in the savings that accrue to U.S. Healthcare as hospitals provide higher quality and more efficient care. At year-end, the hospitals receive an additional distribution if they exceed previously negotiated performance measures of effectiveness, efficiency, and satisfaction. Measures of effectiveness include caesarean section rates and complication rates; average length of stay is used to measure efficiency. Service aspects of care are evaluated by the satisfaction of members admitted to the hospital and their admitting physicians (Sennett, Legorreta, and Zatz, 1993).
U.S. Healthcare has developed a case-mix and severity-adjustment approach that accounts for interhospital differences in the burden of illness of the admitted patient population. CapTainer uses UB-92 State hospital discharge data to determine expected values for the outcomes of care. Aggregate data from all hospitals within several States are obtained and compiled in a composite multistate database.
We use this large multistate database, which contains more than 2 million hospital discharge records, to develop regression models relating patient outcomes and length of stay to patient characteristics. The set of explanatory variables used to calculate expected outcomes includes age, sex, payer type, admission source, discharge type, and comorbidities. U.S. Healthcare uses principal and secondary diagnoses, available in the standard UB-92 data sets, to adjust for severity of illness in the admitted patient population. Clinical algorithms have been developed to categorize the secondary diagnoses as coexisting conditions (i.e., comorbidities) or adverse events (i.e., complications). Coexisting conditions, such as diabetes, are conditions that are highly likely to have been present upon admission to the hospital. Adverse events, such as birth canal injuries accompanying a vaginal delivery, are conditions that are highly unlikely to have been present upon admission.
CapTainer evaluates effectiveness by the adverse-event rate. These adverse events are compared with both expected and benchmark levels of performance. Efficiency is evaluated by comparing each patient's length of stay with risk-adjusted expected and benchmark lengths of stay. U.S. Healthcare's satisfaction ratings result from scoring the responses of surveys sent to members the month following their discharge from the hospital. Questions that ask if the member would recommend his or her attending physician and hospital are scored by computing the percentage of positive responses. The satisfaction of attending physicians is evaluated annually.
The expected level of performance is predicted from the regression models, adjusting for differences in patient characteristics. A benchmark level is also defined by the level of performance achieved by the top 10 percent of all hospitals. Based on a comparison of the actual to expected and benchmark levels of performance, a categorization score for each of the evaluated measures is determined. The top score is achieved by those hospitals that measure at or above the threshold that defines benchmark performance. Those hospitals that are within the 95-percent confidence intervals are considered average or expected. Hospitals that score outside the 95-percent confidence intervals are considered above average (if better than expected but below the benchmark level of performance) and below average (if worse than expected). The information is then fed back to hospitals to support the contractual agreement as well as to support hospital quality-improvement efforts.
Prior to 1995, the first-generation CapTainer model set targets of absolute levels of severity-adjusted performance to be achieved by hospitals in order to be eligible for incentive distributions. For example, if the overall surgical length of stay were 4.5 days per admission, U.S. Healthcare and the hospital would negotiate targeted levels of performance improvement (e.g., 4.3 days the following year, 4.2 the second year, and 4.0 the third year). Based on its ability to reach its preestablished goals, the hospital would either be eligible or ineligible for the agreed-upon distributions. This goal-setting methodology had several limitations. First, it did not account for underlying industry trends, which may have completely accounted for any performance improvements that were measured. Second, it limited the ability of U.S. Healthcare to advance its hospital performance measurement capabilities because of the need to remeasure against existing targets using the predetermined methodology, rather than encouraging continued enhancement of methodologies.
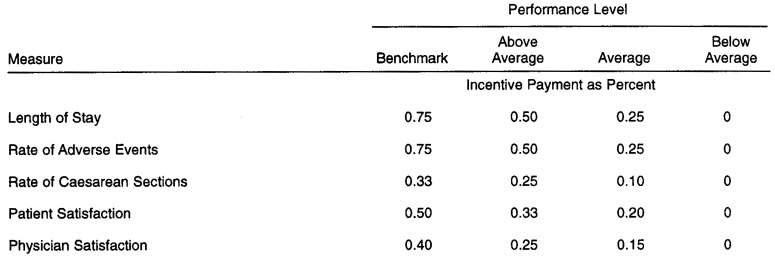
The second-generation CapTainer model allows the interhospital comparison of performance to drive the assessment process. In this way, hospitals are provided incentives to improve their performance relative to other hospitals used by the plan. Figure 3 shows an example schedule that would drive the scoring of performance for an individual hospital. In this example, five measures have been scored (length of stay, rate of adverse events, caesarean section rate, patient satisfaction, and physician satisfaction). The length of stay and adverse-event rate measures have been weighted the most heavily. In this example, if a hospital is able to perform at the benchmark level of performance, it is eligible for a 0.75-percent increase in the base payment If the level of performance is above average but below the benchmark, it earns a 0.50-percent incentive distribution. Average performance nets a 0.25-percent increase, and below-average performance does not earn any additional compensation.2 The three remaining measures (caesarean section rate, patient satisfaction, and physician satisfaction) are categorized in the same incremental levels of performance but are weighted differently.
Figure 3. Hospital Performance Incentive Payments1 Using the CapTainer Compensation Model.
1These incentive payments are based on negotiated agreements between hospitals and U.S. Healthcare.
NOTES: All figures are expressed as a percent of total base distribution. Incentive payments are additive (i.e., 0.75 is an incremental 0.75 percent above the base payment).
SOURCE: U.S. Healthcare, Inc., Blue Bell, PA, 1996.
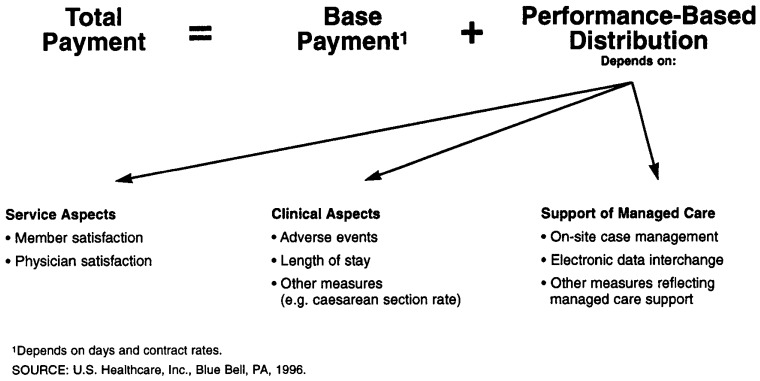
Figure 4 illustrates the basis for a hospital's total payment from U.S. Healthcare. As shown, the total payment is derived from the base payment, which depends on contracted rates and utilization, and a performance-based distribution. The latter depends on the service aspects of care (e.g., members' and physicians' satisfaction), clinical aspects of care, and various factors that support the philosophy of managed care, such as cooperation with onsite case management and electronic submission of hospital claims. This payment model aligns the incentives of hospitals and U.S. Healthcare by making explicit the goals for performance and enables the hospital to share the savings from improved efficiency. It enables hospitals to benefit from declining lengths of stay, balancing the loss of revenue based on a per diem payment methodology. Although the CapTainer methodology was developed in late 1992, U.S. Healthcare does not yet have sufficient experience to determine if the alignment of incentives through this model has improved care beyond underlying industry trends. This is an evaluation that is planned for the future.
Figure 4. Formula for Total Payment and Criteria for Performance-Based Distribution for Hospitals Under the CapTainer Hospital Compensation System.
Specialist Compensation System
Prior to 1996, most care provided by specialists in U.S. Healthcare's medical delivery system was paid on a straight FFS basis. In 1996, however, U.S. Healthcare plans to introduce a QCCS model for physicians in the top 10 specialties that gives providers the opportunity to earn compensation in addition to the base fee schedule that is determined by the quality of care and outcomes achieved in providing care to members. The specialist QCCS will help to align the incentives of U.S. Healthcare with its participating specialists in terms of both quality and cost-effectiveness. It will attempt to reward high-quality physicians who achieve good outcomes, rather than reward only the volume of services provided. FFS compensation models have a tendency to encourage the use of diagnostic testing, procedures, and high-technology care, which drives up medical costs. The specialist QCCS, however, encourages appropriate testing, the use of cognitive services, and cost-effective care.
The evaluation of PCP performance is decidedly more straightforward than the measurement of the performance of specialists. Performance measures of PCPs can be population-based because of the defined capitated relationship between members and their PCPs. PCPs are responsible for most preventive services and much of the care in managing acute and chronic diseases for their patients. Therefore, many measures of disease prevention, health maintenance, and disease management can be used to measure the performance of PCPs. The evaluation of specialists' performance must, however, be based on the population of patients referred to the specialist The focus in evaluating the quality of specialists' care often centers on evaluating their performance in diagnostic workups and procedures during an identified episode of care. Severity adjustment is especially important in measuring the performance of specialists because of differences in referral patterns and technical competencies of specialists, and because some practices are dedicated to diagnostic medicine, and others are procedure-based practices.
The specialist QCCS measures the performance of U.S. Healthcare's participating specialists in the top 10 high-volume specialties by a variety of general and specialty-specific quality indicators. The selection of these 10 was determined by ranking the FFS charges incurred by U.S. Healthcare members from care managed by providers in that specialty. These are the top 10 specialties (sorted alphabetically) that are currently evaluated by the specialist QCCS:
Cardiology
Dermatology
Gastroenterology
Neurology
Obstetrics/Gynecology (OB/GYN)
Ophthalmology and Optometry
Orthopedics
Otolaryngology
Surgery
Urology
The identification of specialty type requires designation of subgroupings of high-volume specialists. Empirical analysis has shown several distinctions in specialty subtype; for example, cardiology is adjusted for two groups of cardiologists: interventionists and noninterventionists. Eye-care professionals have also been divided into optometrists and ophthalmologists, and OB/GYNs are divided into perinatalogists and general OB/GYNs. These designations were necessary to account for the differences in referral patterns and the differential nature of cases treated by these professionals.
Various analytical methods were used in the development and reporting of performance for the specialist QCCS. Small-area analysis of variation was used to identify significant variations in practice patterns. A modification was used in which an individual specialist office was considered its own small area as a unit of analysis. Subsequent analyses were performed to determine which measures had sufficient volume and what the minimum thresholds of measurement should be to obtain stable estimates of performance for the individual specialists. Most measures required risk adjustment to account for the case mix and severity of illness of the patients treated. In some cases, risk adjustment did not change the inferences drawn from descriptive statistics and therefore was not incorporated (Salem-Schatz et al., 1994; Feinglass, Handler, and Hughes, 1987).
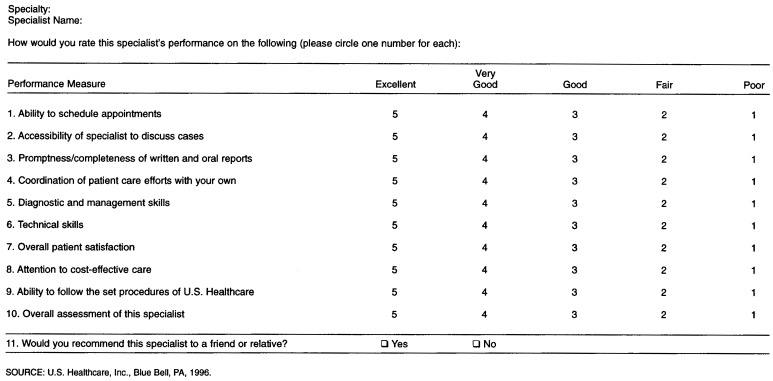
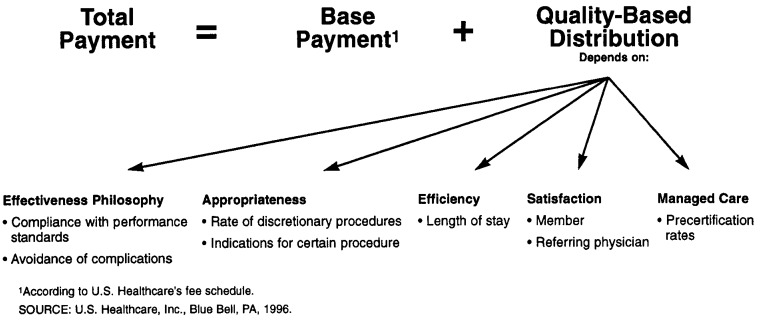
The indicators have been selected to measure quality along five dimensions: effectiveness, appropriateness, efficiency, managed-care philosophy, and satisfaction. Effectiveness of care is measured using criteria such as how well performance standards adapted from accepted practice guidelines are followed and by the avoidance of complications of care. Appropriateness is measured by the rates of performance of certain procedures and the indications for which certain procedures are performed. Length of stay is used to measure efficiency of inpatient care. Managed-care philosophy is based on how well the physician and his or her office cooperate with U.S. Healthcare and comply with administrative policies and requests for information. This dimension is measured by the percentage of elective admissions that are precertified by the specialist, allowing U.S. Healthcare to evaluate the admission for appropriateness and to provide ongoing care review. Satisfaction is measured by surveying both the members who were referred to a specialist and the PCPs who most commonly referred members to specialists. An example of the physician satisfaction survey is shown in Figure 5 (Ramsey et al., 1993).
Figure 5. Satisfaction Survey Completed by Primary Care Physicians to Assess the Performance of Specialists to Whom Patients Have Been Referred.
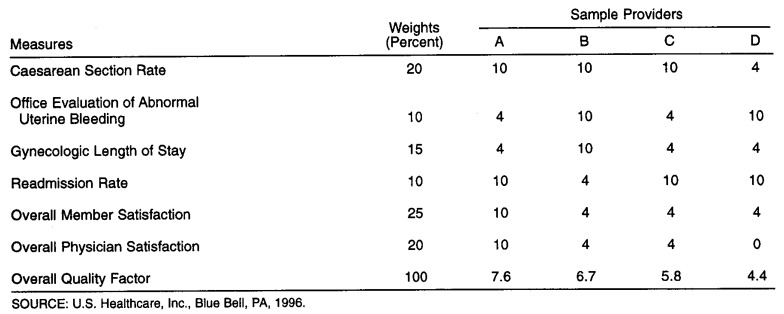
Measures of performance were divided into general and specialty-specific measures. General measures such as length of stay and readmission rate apply to all specialties; specialty-specific measures apply only to the specialty for which they were developed. These latter measures concentrate on areas of effectiveness and appropriateness. An example of such a measure is the caesarean section rate for OB/GYNs. An OB/GYN group would need to exceed the minimum case threshold of 25 deliveries to be ranked for this measure, which has been adjusted for the age of the patients being treated. The performance of an endometrial biopsy in the office setting was adopted as an appropriateness-of-site measure. The OB/GYN Quality Assessment Committee adopted this from guidelines set forth by the American College of Obstetrics and Gynecology. This measure is the rate at which patients have an elective (non-emergency) endometrial biopsy, hysteroscopy, or dilation and curettage as the first procedure in an office to evaluate the diagnosis of abnormal uterine bleeding. An example of a specialty-specific measure for cardiologists is the use of angiotensen converting enzyme (ACE) inhibitors or other afterload reduction for patients with congestive heart failure.
Each of the individual performance measures is scored on a 3-point scale. The adjusted average level of performance3 is derived for each specialty group, and the 95-percent confidence intervals are determined. Each specialty group exceeding a minimum case threshold required to obtain a stable estimate of performance for a given measure receives an ordinal rank (0 for below-average performance, 4 for average performance, and 10 for above-average performance). Each individual measure has been assigned a weight in order to derive an overall quality factor on a scale of 0-10 for the specialty group. Only groups that meet sufficient volume criteria to receive an individual rank on measures that total at least 40 percent of the overall possible weight within their specialty receive an overall quality factor. The overall quality factor is calculated by a weighted average of those measures in which a provider had a sufficient volume of cases to be ranked.
In 1994, U.S. Healthcare instituted a 2-year pilot QCCS for participating OB/GYNs for 1993 performance. The second year of this program was completed in 1995 for 1994 performance. Every participating OB/GYN specialist group that met certain minimum volume criteria was eligible for possible additional distributions in 1994 and 1995, based on the quality of care that they provided to U.S. Healthcare members. A sample of the OB/GYN performance report for 1996 for a region of U.S. Healthcare is shown in Figure 6.
Figure 6. Specialist Quality Care Compensation System Sample Performance Report for Obstetricians/Gynecologists.
Figure 7 summarizes the measures that drive the specialist QCCS model incentive distributions. As shown, the total payment first depends on the base FFS payment made to the specialist, which is determined by U.S. Healthcare's fee schedule and overall utilization of the specialist The specialist is then eligible for a quality-based distribution that depends on the five dimensions of quality that are measured. The overall specialist QCCS model is based on a budgeted allocation and is not dependent on demonstrated cost savings. A regional distribution pool will be determined by the proportionate qualifying membership. Units referred to as “specialist distribution points” will be calculated by the product of the quality factor for the group and the number of U.S. Healthcare members seen during the reporting period. The reporting period is 18 months, with a 3-month period allowed for claims lag. U.S. Healthcare plans to re-analyze the specialist QCCS on a quarterly basis. Specialists (or PCPs) will be able to address concerns about their evaluations to the 35 full-time corporate or regional medical directors for explanation and potential adjustment (Hanchak and Schlackman, 1995).
Figure 7. Total Payment and Criteria for Quality-Based Distribution for Specialists Under the Specialist Quality-Care Compensation System.
The Future of Quality-Based Compensation
The medical delivery system in the United States continues to undergo rapid, significant changes. Providers continually reorganize and move toward more vertically integrated delivery systems (IDSs). As these systems develop, the type and level of provider organizations with which payers contract and from which they expect accountability for quality and cost-effectiveness will change. An IDS that includes the continuum of providers from community-based PCPs and specialists with their community-based hospitals and extends to tertiary referral centers will begin to accept the risk for the medical costs for a population of patients. As these IDSs assume the financial risk for the medical care provided, HMOs will need to develop quality-assessment methodologies to provide valid data to ensure that quality is maintained or improved as risk is transferred. As employers and purchasers begin to develop standards of quality that must be met in order for an HMO to qualify for the employee-benefits selection menus or government contracts, HMOs will to need to develop methods to measure quality improvement with the provider organizations with whom they contract. One mechanism to maintain accountability for the quality of care and service in a risk-sharing environment would be to develop a similar quality-based compensation model directly for IDSs.
A recognized trend in the health care industry is to make purchasing decisions based on the value of the medical product offered. Value, as a quotient of quality and cost, requires that quality be measured with the same rigor with which we measure the costs of care. The field of quality measurement is still in its infancy, but important strides are being made. Although the health plan is held accountable for quality-reporting requirements to employers and purchasers, IDSs need to understand the measures selected and the methodologies employed. Because the direct-contracting IPA-model HMO is not the provider of care, provider organizations will increasingly be evaluated and held accountable in an attempt to improve performance throughout the medical delivery system.
The common theme of U.S. Healthcare's quality-based compensation model has important policy implications for the entire medical delivery system. By making explicit those aspects of care that are the focus of measurement, the expectations of any two contracting parties will be known and made public. To base compensation partly on these measures heightens the attention paid to these important issues of quality. The concept of quality- and performance-based compensation can be adapted across a broad set of circumstances. Employer groups and other purchasers, including the Health Care Financing Administration and State Medicaid agencies, can use this type of compensation model to make explicit their expectations from payers or provider organizations.
Although there is considerable cost for these methodologies and the resources required to develop and maintain the data sets, basing payments on objective performance should ultimately provide greater value. This process has been used in both our mature marketplaces with larger populations and in newer or expanding areas. Offices need to achieve a certain population before this can be used, and until that time they are valued as “average.” Because we use a combination of comparison to peers and feedback, education, and incentives, it has been difficult to extract the proportionate value of each of these activities. This model does not stand alone as a mechanism to drive quality, nor is it a means to devalue outliers. A comprehensive quality-improvement process uses the same data to identify those providers who consistently do not achieve minimal standards. However, significant timely feedback and interaction between U.S. Healthcare and physicians attempt to provide for improvement rather than penalty. Only those plans that realign themselves toward quality-based goals will likely survive as the competition within the managed-care marketplace increases (Hanchak, 1996).
Conclusions
U.S. Healthcare measures PCPs, hospitals, and specialists according to their ability to provide high-quality, cost-effective care; however, each method of measurement differs based on the role the providers play in the health care system. Information will become increasingly credible as data for valid clinical measures become more available and as better adjustment for the severity of defined patient populations can be made. We have shown how baseline performance measurement can be the starting point for quality improvement through education, peer comparison, feedback, goal-setting, and incentives. U.S. Healthcare will continue to emphasize incentives for quality in its quality-based compensation models.
Footnotes
Nicholas A Hanchak is with U.S. Quality Algorithims, Inc., a subsidiary of U.S. Healthcare, Inc. Neil Schlackman and Sandra Harmon-Weiss are with U.S. Healthcare, Inc. The views expressed in this article are those of the authors and do not necessarily reflect the views of U.S. Quality Algorithms, Inc., U.S. Healthcare, Inc., or the Health Care Financing Administration.
Medical charts are selected based on specific criteria (e.g., age, sex, length of enrollment) and are evaluated for compliance with national standards (e.g., immunizations for children, mammography, cholesterol screening of those over 40). For each practice, 30-50 charts are audited by trained personnel. Results of each audit are scored and evaluated by the quality-improvement committee, in addition to being used in the QCCS.
These incentive payments are based on negotiated agreements between hospitals and U.S. Healthcare.
The specialty group's actual level of performance is compared with U.S. Healthcare's mean level of performance but is adjusted for the characteristics of members treated by that group.
Reprint Requests: Nicholas A. Hanchak, M.D., President, U.S. Quality Algorithms, Inc., U.S. Healthcare, Inc., 980 Jolly Road, Blue Bell, Pennsylvania 19422.
References
- Brook R. Practice Guidelines and Practicing Medicine: Are They Compatible? Journal of the American Medical Association. 1989;262:3027–3030. [PubMed] [Google Scholar]
- Eddy D. Practice Policies—Where Do They Come From? Journal of the American Medical Association. 1990;263:1265–1275. [Google Scholar]
- Feinglass J, Handler I, Hughes R. Using Severity-Adjusted Physician Practice Profiles to Identify Cost-Effective Care. NLM Publications. 1987;20:99–122. [PubMed] [Google Scholar]
- Feldman R, et al. Contracts Between Hospitals and Health Maintenance Organizations. Health Care Management Review. 1990;15(1):47–60. doi: 10.1097/00004010-199001510-00009. [DOI] [PubMed] [Google Scholar]
- Franks P. Gatekeeping Revisited: Protecting Patients From Overtreatment. New England Journal of Medicine. 1992;327:424–429. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- Greco P, Eisenberg J. Changing Physician's Practices. New England Journal of Medicine. 1993;329:1271–1274. doi: 10.1056/NEJM199310213291714. [DOI] [PubMed] [Google Scholar]
- Hanchak NA. Managed Care, Accountability, and the Physician. Clinics of North America. 1996 Mar;80(2):245–261. doi: 10.1016/s0025-7125(05)70439-9. [DOI] [PubMed] [Google Scholar]
- Hanchak NA, Schlackman N. The Measurement of Physician Performance. Quality Management in Health Care. 1995;4(1):1–2. doi: 10.1097/00019514-199504010-00001. [DOI] [PubMed] [Google Scholar]
- Hurley R, Freund D, Gage B. Gatekeeper Effects on Patterns of Physician Use. Journal of Family Practice. 1991;32:167–174. [PubMed] [Google Scholar]
- Lasker RD, Shapiro DW, Tucker AM. Realizing the Potential of Practice Pattern Profiling. Inquiry. 1992;29:287–297. [PubMed] [Google Scholar]
- McNeil B, Pederson S, Gatsonis C. Current Issues in Profiling Quality of Care. Inquiry. 1992;29:298–307. [PubMed] [Google Scholar]
- Morrow RW, Gooding AD, Clark C. Improving Physicians' Preventive Health Care Behavior Through Peer Review and Financial Incentives. Archives of Family Medicine. 1995;4:165–169. doi: 10.1001/archfami.4.2.165. [DOI] [PubMed] [Google Scholar]
- Ramsey P, et al. Use of Peer Ratings to Evaluate Physician Performance. Journal of the American Medical Association. 1993;269:1655–1660. [PubMed] [Google Scholar]
- Salem-Schatz S, Moore G, Rucker M, Pearson S. The Case for Case-Mix Adjustment in Practice Profiling. Journal of the American Medical Association. 1994;272:871–874. [PubMed] [Google Scholar]
- Schlackman N. Evolution of a Quality-Based Compensation Model: The Third Generation. American Journal of Medical Quality. 1993 Summer;8:103–110. doi: 10.1177/0885713X9300800214. [DOI] [PubMed] [Google Scholar]
- Schlackman N. Integrating Quality Assessment and Physician Incentive Payment. The Joint Commission Journal on Quality Improvement. 1989;15(8):234–237. doi: 10.1016/s0097-5990(16)30301-3. [DOI] [PubMed] [Google Scholar]
- Sennett C, Legorreta AP, Zatz SL. Performance-Based Hospital Contracting for Quality Improvement. The Joint Commission Journal on Quality Improvement. 1993;19(9):374–383. doi: 10.1016/s1070-3241(16)30022-0. [DOI] [PubMed] [Google Scholar]
- Udvarhelyi IS, Jennison K, Phillips RS, et al. Comparison of the Quality of Ambulatory Care for Fee-for-Service and Prepaid Patients. Annals of Internal Medicine. 1991;115:394–400. doi: 10.7326/0003-4819-115-5-394. [DOI] [PubMed] [Google Scholar]