Abstract
This article captures some key trends in Medicare managed care. The figures which accompany this article explore, among other issues: enrollment; numbers of participating plans; demographic characteristics such as geographic location, age, and income; and premium and benefit comparisons.
Introduction
Managed care options have been incorporated as a feature of Medicare since the inception of the program in 1965. The Tax Equity and Fiscal Responsibility Act of 1982 introduced a full-risk health maintenance organization (HMO) option available to Medicare beneficiaries beginning in 1985. Since 1985, there has been a steady increase in enrollment in full-risk HMOs and similar competitive medical plans (CMPs), with rates of enrollment accelerating in the last few years. In 1996, nearly 1 in 10 Medicare beneficiaries was enrolled in a risk HMO or CMP. An additional 2 percent of Medicare beneficiaries were enrolled in cost-reimbursed HMOs or other cost-reimbursed prepaid plans.
Medicare beneficiaries enrolled in most risk HMOs have reduced out-of-pocket expenses for covered services and receive benefits not otherwise covered by Medicare, including, in many cases, prescription drug coverage. Medicare beneficiaries are “locked in” to risk HMOs, but as of 1996 some Medicare HMOs are beginning to offer “point-of-service” options permitting the use of non-network providers.
Interest among HMOs in Medicare risk contracts has increased significantly in the last several years. As of April 1996, there were 202 risk contractors and 52 pending applications for risk contracts, representing about 45 percent of the Nation's HMOs. According to the American Association of Health Plans, 70 percent of its members have or expect to have Medicare risk contracts by 1997.
Medicare HMO contracting has become a significant market segment for many HMOs. In 1986, none of the 5 largest Medicare risk plans was among the 5 largest HMOs in the Nation, and only 1 Medicare risk HMO was among the largest 15 HMOs in the country. As of 1994, three of the five largest HMOs in the Nation were also among the five largest Medicare risk contractors.
Enrollment in Medicare risk HMOs continues to be concentrated in certain regions of the country. As of December 1995, 5 counties had 25 percent of total risk enrollment: Los Angeles, Orange, and San Diego Counties in California; Maricopa County, Arizona (Phoenix); and Dade County, Florida (Miami). The Los Angeles area, including the preceding California counties and the counties of San Bernardino, Riverside, Ventura, and Kern, had over 25 percent of total risk enrollment in 1995. Although the highest numbers of enrollees are in areas with relatively high Medicare HMO payment rates (which are based on historical fee-for-service rates in each county), there are a number of relatively low payment areas where substantial percentages of Medicare beneficiaries are enrolled in risk HMOs.
Medicare risk HMO enrollees are less likely to be 85 years of age or over, institutionalized, on Medicaid, or entitled to Medicare on the basis of disability (i.e., under 65 years of age). Results of the 1993 Medicare Current Beneficiary Survey (MCBS) indicate that HMO enrollees tend to be healthier than non-enrollees. Enrollees are particularly satisfied with their costs of health care in an HMO.
Enrollment has increased every year since the beginning of the program.
Medicare risk enrollment in recent years has increased at an accelerated rate. Although Medicare HMO enrollment is less than one-half the level of the non-Medicare sector, where over one-third of the non-Medicare insured population is enrolled in HMOs,1 the rate of growth in Medicare HMO enrollment has far exceeded non-Medicare growth rates over the past several years.
From December 1994 through April 1996, Medicare risk HMO enrollment grew 53 percent. Between December 1993 and December 1994, Medicare risk enrollment grew 25 percent, while in the non-Medicare sector, HMO enrollment grew 13.1 percent in the same time period.
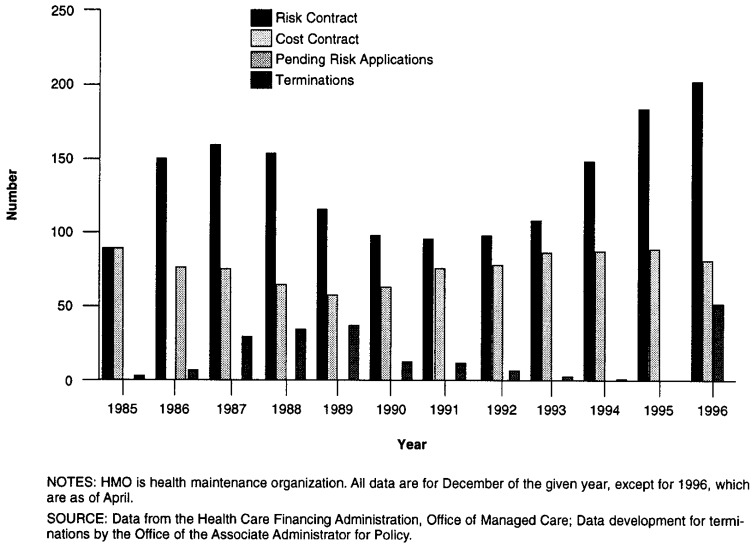
Risk contracts are at their highest historic levels and terminations are becoming rare. The early years of the risk program saw the quick entry and exit of a number of HMOs as Medicare contractors. At the end of 1987, there were 161 Medicare risk contractors. Beginning in 1988, the number of risk HMO contracts began to decline. From 1988 to 1991, the number declined by 40 percent.
Renewed HMO interest in Medicare contracting resulted in dramatic increases in the number of contractors in the mid-1990s. The number of risk contracts doubled between 1990 and 1996. During the 12-month period ending January 1996, there was a 24-percent increase in the number of risk contractors.
As of the beginning of 1996, several States that had not previously had Medicare risk contractors have such HMOs, including Arkansas, South Carolina, and Utah (as well as Georgia, where a risk plan had been terminated several years ago). As of the beginning of 1996, only nine States have no Medicare risk HMOs (and two States are served only by out-of-state risk HMOs).
The level of concentration in larger plans is declining, though Medicare risk HMO enrollment continues to be concentrated in the largest plans. Seven of the 15 largest plans were in California, and all but 1 of the 5 largest plans is in California. In 1986, 33 percent of Medicare risk HMO enrollment was in the largest 5 contractors, all but 1 of which had participated in a Medicare HMO demonstration project in the early 1980s.
New plans have a significant proportion of the enrollment, as do the oldest plans.
Risk enrollment is highly concentrated in certain geographic areas. California, Florida, and Arizona account for about 60 percent of all risk enrollment but only 19 percent of total Medicare beneficiaries.
There is wide access to managed care plans for Medicare beneficiaries. In 1994, 74 percent of Medicare beneficiaries lived in areas served by a Medicare managed care plan (risk or cost), and 56 percent of beneficiaries had 2 or more plans available to them. Multiple risk plans are available in many metropolitan areas. The highest number is in Los Angeles County, where 15 Medicare risk HMOs were available in March 1995. Adjacent Orange County had 14 plans, and Dade County, Florida (Miami) had 8 risk plans available to Medicare beneficiaries.
Non-Medicare penetration exceeds Medicare HMO penetration in almost all States.
Counties with the highest Medicare risk HMO penetration levels do not necessarily have the highest payment levels. The 10 highest payment rates in 1996 (for aged beneficiaries, for the District of Columbia and the 50 States) included only 1 county with high Medicare risk HMO penetration (20 percent or greater): Dade County, Florida (Miami). The highest adjusted average per capita cost (AAPCC) rates in urban areas are in the New York City area and Philadelphia.
Payments to risk HMOs for the month of December 1995 totaled $1.3 billion, or about 9 percent of total monthly program outlays for Medicare. For 1996, county standardized risk HMO monthly payments for aged beneficiaries in counties where an HMO is available range from $250-760. For January 1996, the average monthly per enrollee payment to Medicare risk HMOs was $440.
As of February 1996, 63 percent of risk plans offered a basic package with no member premium in at least part of their service area. The basic premium includes both the amounts risk HMOs are permitted to charge Medicare beneficiaries for cost-sharing for Medicare covered services, representing Medicare's coinsurance and deductible amounts not included in AAPCC payments to HMOs, and the cost of any non-covered benefits that beneficiaries are required to purchase as part of the basic package offered by the HMO (such as preventive care that Medicare does not cover and which HMOs traditionally cover).
In 1987, zero-premium plans were available in only four metropolitan areas. In 1991, in addition to these areas, six more areas had zero-premium plans. In 1995, 38 metropolitan areas had zero-premium HMOs. In 1995, in only six States where there were risk contractors was a zero-premium plan not available (in at least part of the State). Each of those six States had, at most, two risk HMOs.
The majority of Medicare risk HMOs use savings to finance reduced premiums and/or additional benefits for their members. For 1996, 20 percent of projected Medicare payments will be returned to beneficiaries in the form of reduced premiums and/or additional benefits.2 Expressed in dollars, $4 billion of $20 billion in projected annual Medicare payments to risk HMOs will be used for enhanced benefits.
As of February 1996, 60 percent of plans offered prescription drug benefits in their basic benefit package in at least part of their service area. This number includes 94 plans that included drug coverage as part of a zero-premium package in at least part of their service area.2
In some States, all risk HMOs include drug coverage. Note, however, that for Maryland, Nevada, New Mexico, Pennsylvania, Minnesota, Massachusetts, Illinois, and Oregon, not all beneficiaries in each plan have drug coverage. Residents of some counties do not have drugs included in basic coverage, even though the HMO in which they are enrolled includes drugs in some of the counties included in the plan's service area.
Except for those under 65 years of age (the disabled) and the oldest old (85 years of age or over), HMOs have a fairly representative age distribution.
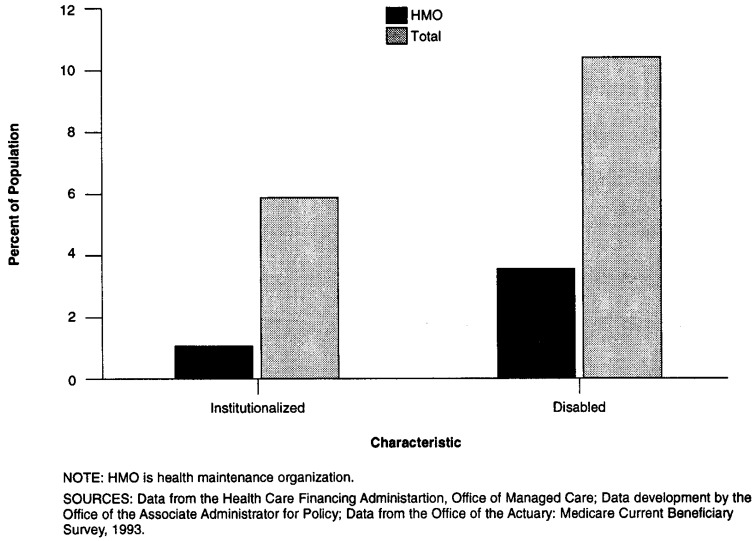
The institutionalized and beneficiaries entitled to Medicare on the basis of disability are less likely to be risk HMO enrollees. In December 1995, 1.06 percent3 of risk HMO enrollees were institutionalized (residing in a nursing home or similar institutional arrangement), while MCBS data indicate that 5-6 percent of the general Medicare population is institutionalized.
According to a recent study, “Beneficiaries who are dually eligible [have both Medicare and Medicaid coverage] are two-thirds less likely to enroll in HMOs than are other Medicare beneficiaries as a group—less likely to enroll even than the under-65 group” (Welch, 1996).
A number of barriers exist that prevent greater enrollment of dual eligibles in Medicare risk HMOs (Saucier, 1995). Similarly, for the institutionalized, their enrollment is low in risk HMOs because many are eligible for Medicaid, are 85 years of age or over, or are less likely to change providers in order to enroll in a managed care plan.4
In terms of income, the MCBS shows that there is a mix of distribution of HMO enrollment in relation to income. The very poor are less likely to be enrolled in HMOs (reflecting their status as dual eligibles), and the very wealthy are also less likely to be HMO enrollees.
Survey results for a sample of risk HMO enrollees from MCBS data for September 1993 indicate that HMO enrollees enjoy better health than non-HMO enrollees. This may reflect a variety of factors, including the types of Medicare beneficiaries who are likely to enroll in HMOs, and improved access to care among HMO enrollees.
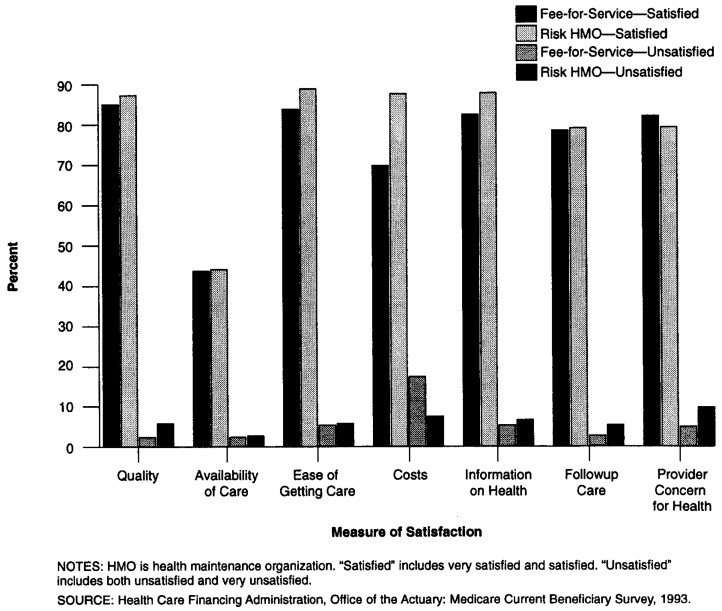
In their attitudes towards their health plans, MCBS data indicate that risk HMO enrollees are most satisfied with HMO costs. The September 1993 MCBS survey of a sample of Medicare beneficiaries found that HMO enrollees were significantly more satisfied with out-of-pocket costs for medical care, compared with beneficiaries in fee-for-service Medicare.
Each category of beneficiaries (HMO enrollees and non-enrollees) had similar attitudes in terms of availability of care, and the ease of getting care. Impressions of the quality of care varied from one group to the other: 37 percent of risk HMO enrollees were very satisfied with their care while only 30 percent of fee-for-service beneficiaries said they were very satisfied. Those “satisfied” with their care included 55 percent in fee-for-service and 52 percent in HMOs. Fewer than 1 percent of beneficiaries in either category were very unsatisfied with their care, but 5.5 percent of HMO enrollees were unsatisfied with their care versus 2.9 percent of fee-for-service beneficiaries.
Figure 1. Medicare HMO Enrollment: 1985-96.
Figure 2. Relative Growth in HMO Enrollment: 1988-94.
Figure 3. Medicare HMO Contracts and Terminations: 1985-96.
Figure 4. Enrollment Concentration in the Largest Risk HMOs: 1986, 1994, and 1995.
Figure 5. Enrollment Distribution by Length of Medicare Risk Contract: December 1995.
Figure 6. Distribution of Medicare Risk Enrollees Among Selected States: 1994-95.
Figure 7. Medicare and Non-Medicare HMO Penetration in Selected States: 1993-95.
Figure 8. Risk HMO Monthly Premium Levels: 1995 and 1996.
Figure 9. Risk HMO Additional Benefits: 1995 and 1996.
Figure 10. Percent of Risk Plans With Drug Coverage in Basic Plan, for Selected States: January 1996.
Figure 11. Age Distribution of HMO Enrollees: 1995.
Figure 12. Characteristics of Medicare Risk HMO Enrollees: 1995.
Figure 13. Income Distribution of HMO Enrollees Versus Non-HMO Enrollees: 1993.
Figure 14. Relative Health Status of HMO Enrollees: 1993.
Figure 15. Beneficiary Attitudes Towards HMOs and Fee-for-Service: 1993.
Table 1. Medicare Risk HMO Penetration in Selected High and Low Payment Areas: December 1995.
| County | Medicare Risk HMO Penetration (Percent) |
Number of Risk Plans Available | 1994 Percent of Commercially Insured in HMO for MSA | 1996 Aged AAPCC | Percent 1996 U.S Per Capita Costs |
|---|---|---|---|---|---|
| High Payment Areas | |||||
| Dade, FL (Miami) | 33 | 8 | 45 | $687 | 162 |
| Los Angeles, CA | 34 | 15 | 64 | 587 | 133 |
| Richmond, NY | 18 | 3 | 45 | 759 | 172 |
| New York, NY | 5 | 3 | 45 | 715 | 162 |
| Queens, NY | 10 | 5 | 45 | 652 | 147 |
| Wayne, MI (Detroit) | 1 | 1 | 35 | 628 | 142 |
| Baltimore City, MD | 2 | 4 | 44 | 614 | 139 |
| Low Payment Areas | |||||
| Clackamas, OR (Portland) | 44 | 5 | 54 | 368 | 83 |
| Multnomah, OR | 44 | 5 | 54 | 385 | 87 |
| Washington, OR | 44 | 5 | 54 | 395 | 90 |
| Hennnepin, MN (Minneapolis) | 20 | 3 | 59 | 387 | 82 |
| Ramsey, MN (St. Paul) | 23 | 3 | 59 | 411 | 93 |
NOTES: HMO is health maintenance organization. MSA is metropolitan statistical area. AAPCC is adjusted average per capita cost.
SOURCES: Data from the Health Care Financing Administration, Office of the Actuary and Office of Managed Care; (Group Health Association of
Footnotes
Carlos Zarabozo is with the Special Analysis Staff, Office of the Associate Administrator for Policy, Health Care Financing Administration (HCFA). Charles Taylor is a Commander in the U.S. Naval Nurse Corps. He was serving as a U.S Army Baylor University Administrative Resident at HCFA when this research was performed. Jarret Hicks is with the Office of Managed Care, HCFA. The opinions expressed are those of the authors and do not necessarily reflect those of the U.S. Navy or HCFA.
Number derived from Group Health Association of America (1995) figures for December 1994 HMO enrollment by State, less August 1994 Medicare HMO enrollment Privately insured numbers computed using State populations as of July 1994, less Medicare population, less uninsured for 1993 (Employee Benefits Research Institute, 1995).
Data based on an Office of Managed Care analysis of premium rate submissions to HCFA.
Data based on Office of Managed Care Monthly Report for February 1996. Although the report shows that there were 194 risk contractors at the time, premium and benefit information is displayed for only 162 risk plans, 115 of which had zero-premium plans.
Based on HCFA Office of the Associate Administrator for Policy data development of weighted averages based on HMO reporting of institutionalized enrollees. HMOs report the number of institutionalized enrollees on a monthly basis.
Medicare payments to risk HMOs are adjusted at the individual beneficiary level, with adjustments for various demographic factors, including institutional and Medicaid status. If an HMO has a smaller share of institutionalized members compared with the local Medicare population, the HMO's overall payments will be less than if the HMO's share of institutionalized members mirrored their number in the community, because Medicare's payments for institutionalized individuals are higher, generally, than for the non-institutionalized.
Reprint Requests: Carlos Zarabozo, Special Analysis Staff, Office of the Associate Administrator for Policy, Health Care Financing Administration, 325H Hubert H. Humphrey Building, 200 Independence Avenue, SW, Washington, DC 20201.
References
- Employee Benefits Research Institute. Data Book on Employee Benefits, 3rd Edition. Washington, DC.: 1995. [Google Scholar]
- Group Health Association of America. Patterns of Enrollment: 1995 Edition. Washington, DC.: Jun, 1995. [Google Scholar]
- Saucier P. Federal Barriers to Managed Care for Dually Eligible Persons. Portland, ME.: National Academy for State Health Policy; Aug, 1995. [Google Scholar]
- Welch WP. Growth in HMO Share of the Medicare Market Unpublished manuscript. Washington, DC.: The Urban Institute; Jan, 1996. [Google Scholar]