Abstract
Background: In the early course of schizophrenia, premorbid functioning, negative symptoms, and neurocognition have been robustly associated with several domains of daily functioning. Research with chronic schizophrenia patients suggests that attitudinal beliefs may influence daily functioning. However, these relationships have not been examined in recent-onset schizophrenia patients. Methods: The sample consisted of recent-onset schizophrenia outpatients (n = 71) who were on average 21.7 (SD = 3.3) years old, had 12.5 (SD = 1.8) years of education, and 5.9 (SD = 6.3) months since psychosis onset. Patients were assessed for premorbid adjustment, positive and negative symptoms, neurocognition, attitudinal beliefs, and daily functioning. Normal controls (n = 20) were screened for psychopathology and demographically matched to the patients. Results: Comparisons indicated that recent-onset patients had higher levels of dysfunctional attitudes and lower self-efficacy compared to healthy controls (t = 3.35, P < .01; t = −4.1, P < .01, respectively). Dysfunctional attitudes (r = −.34) and self-efficacy (r = .36) were significantly correlated with daily functioning. Negative symptoms were found to mediate the relationship between self-efficacy and daily functioning (Sobel test, P < .01), as well as between dysfunctional attitudes and daily functioning (Sobel test, P < .05). Neurocognition was a significant mediator of the relationship between self-efficacy and daily functioning (Sobel test, P < .05). Discussion: Early course schizophrenia patients have significantly more dysfunctional attitudes and lower self-efficacy than healthy subjects. Both self-efficacy and dysfunctional attitudes partially contribute to negative symptoms, which in turn influence daily functioning. In addition, self-efficacy partially contributes to neurocognition, which in turn influences daily functioning.
Key words: recent-onset schizophrenia, dysfunctional attitudes, self-efficacy, negative symptoms, neurocognition, daily functioning, mediation models, premorbid history
Introduction
The predictors and determinants of daily functioning and, ultimately, recovery from schizophrenia are of substantial current interest to patients and clinical researchers. A number of key factors have been identified as meaningful predictors of functioning in the early course of schizophrenia, which generally parallel the factors found to predict functioning in chronic schizophrenia patients.1,2 Among the First-Episode Psychosis (FEP) studies reporting on 1–2-year outcomes, 3 factors stand out as consistent predictors of functioning: premorbid history, neurocognition, and negative symptoms3–10 (for reviews see: Allott et al.; Lin et al.; MacBeth and Gumley11–13). Poor premorbid adjustment has been inversely associated with good role functioning, quality of life, and has been linked to the severity of negative symptoms.13 This is especially important because studies have suggested that persistent negative symptoms are displayed by 20%–25% of FEP patients.14,15 In addition to premorbid history, the severity of negative symptoms has also been consistently associated with several domains of functioning in FEP.16–20 Considering another relevant domain, extensive research on cognition in schizophrenia has shown that individuals suffer a broad range of characteristic impairments that are related to deficits in various domains of daily functioning. However, there appears to be some lack of consistency across studies regarding the relationship between neurocognition and daily functioning in the early course.11 Yet, Nuechterlein and colleagues6 reported that 52% of the variance in work functioning for first-episode patients was explained by neurocognitive predictors. These findings provide strong evidence for the role of premorbid history, negative symptoms, and neurocognition in predicting daily functioning in schizophrenia patients.
Although there is much less research on attitudinal beliefs such as dysfunctional attitudes and self-efficacy, findings from studies in chronic patients indicate the promise of these factors for understanding functioning in the early course of schizophrenia. Chronic patients have documented dysfunctional attitudes compared with healthy controls.21,22 In addition, these attitudinal beliefs have been found to predict daily functioning in chronic patients. Beck and colleagues have proposed a model in schizophrenia patients suggesting that negative symptoms develop as a consequence of dysfunctional attitudes, such as anticipated failure in goal-directed tasks and low expectancies for pleasure or success in social activities.23,24 Support was found for these hypotheses indicating that dysfunctional attitudes, such as “If you cannot do something well, there is little point in doing it at all” and “People will think less of me if I make mistakes and fail,” were associated with the development of negative symptoms.21,22 In addition, recent path analyses demonstrated that negative symptoms mediated the relationship between dysfunctional attitudes and daily functioning.9,21
One question of interest is the developmental course of attitudinal beliefs in schizophrenia patients. The period during and shortly after a first psychotic episode is considered a critical transitional period psychosocially. Sorting out whether these maladaptive attitudes are present in the early phase of illness tells us whether they may be trait-like characteristics or vulnerability markers. In contrast, perhaps these attitudes could be the consequences of the long-term presence of illness factors that increase in severity as the condition worsens. In the early phase of illness, there is an absence of influences of chronic illness (eg, chronic disability patterns, social alienation, and gray and white matter volume loss). Furthermore, evidence of a role for attitudinal beliefs early in the illness would have implications for early intervention targets that might help prevent chronic disability. Thus, the early course is an opportune time to examine potential psychological contributors to functioning, before factors associated with chronic illness dominate functional outcomes.
Some investigators have suggested that another attitudinal belief, self-efficacy, may be associated with negative symptoms and neurocognition in schizophrenia patients.25,26 Perceived self-efficacy concerns an individual’s belief in his or her ability to influence events that affect the outcome of his or her life. According to Bandura,21,27 this core belief is the foundation of human motivation, performance, accomplishments, and emotional well-being. Unless people believe they can produce a desired effect by their actions, they may have little incentive to initiate activities or persevere in the face of challenges or obstacles. People with a low sense of efficacy in a given domain of functioning will shy away from difficult tasks they perceive as personally threatening. They tend to have low aspirations and waver in their commitment to achieving life’s goals. This research has direct applicability to schizophrenia patients because, as Bandura28 theorized, a person’s success at handling tasks such as performance on neurocognitive tests is directly linked to skill and ability as well as one’s belief about the success of the outcome. Thus, the presence of low self-efficacy in schizophrenia patients suggests that they may be unsuccessful in everyday life partially due to a perception that they lack the ability to succeed. A self-efficacy questionnaire may ask: How confident are you in your ability to: go out on a date, go on a job interview, or concentrate on your work?8,27 Interestingly, self-efficacy has been hypothesized to influence the type of coping efforts that have been associated with successful psychosocial functioning.29 In addition, self-efficacy was highly correlated with the number of strategies used to cope with negative symptoms and with personally experienced stressful life events.30,31 Given these findings, the door is open for further exploration of attitudinal beliefs as potential contributors to established predictors of daily functioning, such as negative symptoms and neurocognition.
In a contrasting model, dysfunctional attitudes were found to be mediators of the relationship between neurocognition and functioning (defined as quality of life) in chronic patients.22 Beck and colleagues proposed that defeatist beliefs, assessed with a subscale of dysfunctional attitudes, is a mediating variable between neurocognition (predictor) and negative symptoms (outcome), and between neurocognition (predictor) and quality of life (outcome).22–24,32 Further work has suggested that a reduction in dysfunctional attitudes was related to success in a skills training cognitive behavioral therapy intervention.8 In fact, a reduction in the degree of dysfunctional attitudes during the intervention was significantly correlated with improvement in functioning at follow-up. Another attitudinal belief, self-efficacy, has been shown to be a moderator, rather than a mediator, in relationship to functioning.25,33,34 For example, when self-efficacy was high, functional capacity scores were significantly related to functioning, but not when self-efficacy was low.25 Although weaker than expected results were found in studies after examining mediating effects of self-efficacy on daily functioning, further exploration in FEP is warranted.33,35 High levels of self-efficacy in chronic schizophrenia patients were associated with social participation and being employed,36 and thus they may play a role in functioning. Researchers have postulated that high self-efficacy is not simply a correlate of good functioning, but actually contributes directly by mediating the impact of other variables in predicting functioning. Indeed, direct attempts at increasing self-efficacy have been suggested as targets for treatment.37
There appear to be 2 competing models regarding attitudinal beliefs. One model for which there is fairly consistent evidence in chronic patients proposes neurocognition and negative symptoms as mediators of the relationship between attitudinal beliefs (predictor) and daily functioning (outcome). Another model, for which the evidence is mixed, proposes that attitudinal beliefs (dysfunctional attitudes and self-efficacy) are mediators between established predictors (neurocognition or negative symptoms) and daily functioning (outcome). These 2 models have not been tested on the same sample of chronic patients, or more specifically, on recent-onset patients. Examining empirically based predictors along with hypothesized mediators during this early phase of illness is critically important to understanding outcome. Identifying mediators might help to identify additional treatment targets in the early phase where interventions can pay big dividends.
This study aimed: (1) to determine if more dysfunctional attitudes and lower self-efficacy are present in recent-onset patients compared with normal controls, and (2) to test competing models previously proposed in chronic patients hypothesizing that dysfunctional attitudes and self-efficacy are either primary or indirect contributors to daily functioning.25,33,35 Based on a review of the literature, we hypothesize that in the early course of schizophrenia, dysfunctional attitudes and low self-efficacy: (1) are present in patients compared with healthy controls, (2) are correlated with poor premorbid functioning, neurocognition, negative symptoms, and daily functioning, and (3) are contributors to neurocognitive deficits and negative symptoms, which in turn contribute to daily functioning.
Methods
Subjects
The sample consisted of 71 recent-onset schizophrenia patients and 20 demographically matched healthy controls participating in the fourth phase of an National Institute of Mental Health-funded project focusing on the early course of schizophrenia [for additional sample details, see Nuechterlein et al.38; (table 1)]. Although patients were enrolled within 2 years of the beginning of their first psychotic episode, they were psychotic on average for about 5 months. Healthy controls were screened with the Structured Clinical Interview for DSM-IV for absence of major Axis I diagnoses and absence of schizophrenia spectrum personality disorders. Patients were enrolled in the Aftercare Research Program, an outpatient clinic that provides medication and offers individual case management, group therapy focused on practical life skills, and family education for all research subjects diagnosed with schizophrenia. The present study was approved by the University of California Los Angeles Institutional Review Board. All participants were provided with oral and written information about the research procedures involved in the study and gave written informed consent prior to data collection.
Table 1.
Sample Characteristics at Study Entry for Recent-Onset Schizophrenia Patients (n = 71) and Age-Matched Controls (n = 20)
| Patients | Controls | Test Statistics | P Value | |
|---|---|---|---|---|
| Age | 21.68 (3.29) | 21.80 (1.96) | t = 0.2 | .87 |
| Education | 12.49 (1.82) | 13.30 (1.22) | t = 1.9 | .06 |
| Parental education | 14.05 (3.79) | 14.50 (1.88) | t = 0.4 | .10 |
| Male | 56 (80%) | 9 (75%) | χ 2(1) = 0.1 | .70 |
| Marital status | χ 2(1) = 1.0 | .32 | ||
| Single | 95% | 100% | ||
| Married | 5% | |||
| Race | χ 2(5) = 8.3 | .14 | ||
| Caucasian | 38 (54%) | 9 (75%) | ||
| African American | 17 (21%) | 1 (8%) | ||
| Asian | 6 (9%) | 0 | ||
| Pacific Islander | 2 (3%) | 1 (8%) | ||
| Native American | 4 (6%) | 0 | ||
| Mixed/Other | 3 (4%) | 1 (8%) | ||
| Ethnicity | ||||
| Hispanic | 29 (41%) | 4 (33%) | χ 2(1) = 0.3 | .59 |
| Diagnosis | — | — | — | |
| Schizophrenia | 51% | |||
| Schizoaffective | 11% | |||
| Schizophreniform | 38% | |||
| Mean number of months since psychosis onset | 5.92 (6.27) | — | — | — |
| Premorbid history | 2.13 (1.71) | — | — | — |
| SANS | — | — | — | |
| Total SANS | 1.98 (1.02) | |||
| Experiential symptoms | 2.32 (1.31) | |||
| Expressive symptoms | 1.63 (1.17) | |||
| MCCB composite score | 31.81 (12.84) | 43.5 (7.21) | t = −3.7 | < .01 |
| RFS Global Role Functioning Index | 16.35 (5.26) | 24.05 (3.08) | t = −6.1 | < .01 |
Note : MCCB, MATRICS Consensus Cognitive Battery; RFS, Role Functioning Scale; SANS, Scale for the Assessment of Negative Symptoms.
Procedures
All patient participants received outpatient psychiatric treatment as part of the program, including regular psychiatrist visits, as well as individual case management and therapy by Master’s and Doctoral level therapists. All participants were considered eligible to enter the study when they were on a stable outpatient dose of oral or long-acting injectable risperidone for at least 3 weeks prior to data collection as part of a randomized controlled trial of these antipsychotic medications. The outpatient psychiatric treatment involved a similar frequency of weekly clinic visits in which the various psychosocial interventions and psychiatric care were provided to all patients. Cognitive behavior therapy, which is known to impact dysfunctional attitudes, was not part of the psychosocial intervention package. The Aftercare Research Program was the participants’ primary source of mental health care.
Measures
Psychiatric and Social History Schedule38 was used to gather demographic, patient education, gender, and premorbid history data at intake by trained raters using a form created by the study team. Data included age, patient level of education, gender, first appearance of psychotic and prodromal symptoms, and prior psychiatric treatments, including antipsychotic medications and hospitalizations.
Premorbid Adjustment Scale (PAS)39 was selected as a well-validated measure of premorbid functioning used in research on schizophrenia patients. The PAS is rated on a Likert scale from 0 (least healthy) to 4 (most healthy). The PAS assesses work functioning, social functioning, dating relationships, treatment and hospitalization history, family psychiatric history, age of onset, symptom items, independence, and fullness of life. A global score was used for these analyses.
Scale for the Assessment of Negative Symptoms Raters who were trained to criterion levels40 administered the Scale for the Assessment of Negative Symptoms (SANS), a 25-item measure, ie, widely used to assess 2 negative symptom domains: (1) Expressive symptoms, which consists of affective flattening (blunted affect) and alogia, and (2) Experiential symptoms, which consists of avolition and apathy, and asociality. The global ratings for each of these 2 negative symptom domains were combined to create the SANS composite score (excluding attention). The Attention subscale was not included in these analyses due to the strong correlational relationship to cognitive functioning, which raises questions about whether the SANS attention item is actually a core negative symptom (see Andreasen et al.41 for a discussion).
Neurocognition.
Neurocognition was assessed using the MATRICS Consensus Cognitive Battery.42 The current study included the 7 MATRICS domains of cognitive functioning43: speed of processing, attention/vigilance, working memory, verbal learning, visual learning, reasoning and problem solving, and social cognition. The primary variable of interest was the composite score.
Dysfunctional Attitudes and Revised Self-efficacy Scale
The Dysfunctional Attitudes Scale (DAS) and Self-efficacy Scale (SES) were administered as a pencil-and-paper measure, after an interviewer provided detailed directions and an example item.
The DAS44 is a 40-item instrument based on Beck’s Cognitive Therapy Model that contains items related to the 7 major value systems: approval, love, achievement, perfectionism, entitlement, omnipotence, and autonomy. The Defeatist Performance Attitudes Subscale (DPAS) consists of 15 statements describing overgeneralized conclusions about one’s ability to perform tasks (eg, “If you cannot do something well, there is little point in doing it at all”). The Dysfunctional Need for Acceptance Subscale (DNAS) consists of 10 statements that exaggerate the importance of being accepted by other people (eg, “I cannot be happy unless most people I know admire me”).
The SES45 is comprised of 57 statements that require respondents to rate their confidence in their ability to perform social behaviors, school and work tasks, engage in self-care, and manage symptoms (scale from 0 to 100, with 0 referring to “not at all able” and 100 being “totally able”). McDermott45 administered the SES to 62 participants with schizophrenia and found high internal consistency and test-retest reliability over 2 weeks.
Psychosocial Functioning.
The Role Functioning Scale (RFS)46,47 was used as the functional outcome measure of the following domains: independent living, work productivity, family relationships, and social relationships. We used specific probes to cover multiple areas of community functioning. The items on the RFS are anchored 1–6, so that higher scores reflect decreasing reliance on agency-related support and increasing independence in community functioning. A composite score, the Global Role Functioning Index, the sum of the 4 domains, was used (see Goodman et al.46).
Results
Comparisons of Patients and Controls on Dysfunctional Attitudes and Self-efficacy
We conducted t tests to examine whether patients showed significantly more dysfunctional attitudes and lower self-efficacy than age- and gender-matched controls. The mean level of self-efficacy was significantly lower for patients than for controls (M = 73.54 vs 90.74, P < .01, respectively). In particular, patients indicated asking someone out on a date as the behavior they felt least capable of performing (M = 51.95), considerably lower than any other item (nearest item was scored as M = 67.18). Similarly, patients had significantly higher levels of dysfunctional attitudes compared with controls (dysfunctional attitudes total score M = 132.13 vs 108.30, P < .01, respectively) and higher scores on the subscale, DPAS, compared with controls (M = 46.8 vs 36.0, P < .01, respectively). The difference for the other subscale, DNAS, although higher in patients, was not statistically significant (M = 35.3 vs 31.7, P = .13, respectively). For the DAS, no single item stood out as patients scored equally low on most items, but 2 particularly low scoring items pertained to dysfunctional attitudes about asking for help (M’s = 2.16 and 2.21).
Bivariate Correlations Among Premorbid History, Neurocognition, Negative Symptoms, Dysfunctional Attitudes, Self-efficacy, and Daily Functioning
We found that premorbid functioning, neurocognition, negative symptoms, dysfunctional attitudes, and self-efficacy were all significantly related to the Global Role Functioning Index (table 2). Self-efficacy was also significantly related to premorbid functioning, neurocognition, and negative symptoms. In addition, self-efficacy was significantly related to the individual domains of daily functioning, including independent living (r = .31, P = .01), work/school productivity (r = .43, P < .01), social functioning (r = .38, P < .01), and family relationships (r = .25, P = .05).
Table 2.
Correlations Between Attitudinal Beliefs, Neurocognition, Negative Symptoms, and Daily Functioning (n = 71)
| Variable Name | Negative Symptoms (SANS) |
Experiential Symptoms | Expressive Symptoms | Neurocognition (MCCB) | Dysfunctional Attitudes (DAS) | DPAS | DNAS | Self-efficacy (SES) | Global Role Functioning Index (RFS) |
|---|---|---|---|---|---|---|---|---|---|
| Premorbid functioning | −0.45** | −0.57** | −0.15 | 0.30* | −0.22† | −0.19 | −0.02 | 0.45** | 0.62** |
| Negative symptoms (SANS) | — | 0.84** | 0.80** | −0.42** | 0.28* | 0.33** | 0.10 | −0.58** | −0.68** |
| Experiential symptoms | — | 0.35** | −0.33** | 0.23* | 0.28* | 0.03 | −0.53** | −0.68** | |
| Expressive symptoms | — | −0.36** | 0.23 | 0.26* | 0.13 | −0.43** | −0.41** | ||
| Neurocognition (MCCB) |
— | −0.14 | −0.12 | −0.01 | 0.29* | 0.49** | |||
| Dysfunctional attitudes (DAS) | — | 0.93** | 0.83** | −0.38** | −0.34** | ||||
| DPAS | — | 0.69** | −0.38** | −0.31* | |||||
| DNAS | — | −0.23* | −0.10 | ||||||
| Self-efficacy Scale (SES) | — | 0.45** |
Notes: DAS, Dysfunctional Attitudes Scale; DNAS, Dysfunctional Need for Acceptance Subscale; DPAS, Defeatist Performance Attitudes Subscale; MCCB, MATRICS Consensus Cognitive Battery; RFS, Role Functioning Scale; SANS, Scale for the Assessment of Negative Symptoms.
*P < .05, **P < .01, † P < .10.
Dysfunctional beliefs (total score) were significantly related to negative symptoms (composite). Correlational relationships between Defeatist Performance Attitudes (DPAS) and both experiential and expressive negative symptoms were stronger than the relationship of the DNAS with either experiential or expressive negative symptoms. Furthermore, the total score for dysfunctional attitudes was significantly related to the individual domains of daily functioning including: independent living (r = −.31, P = .01), family relationships (r = −.34, P < .01), work or school functioning (r = −.31, P = .02), and social functioning (r = −.25, P = .05).
Testing Competing Models of Mediation
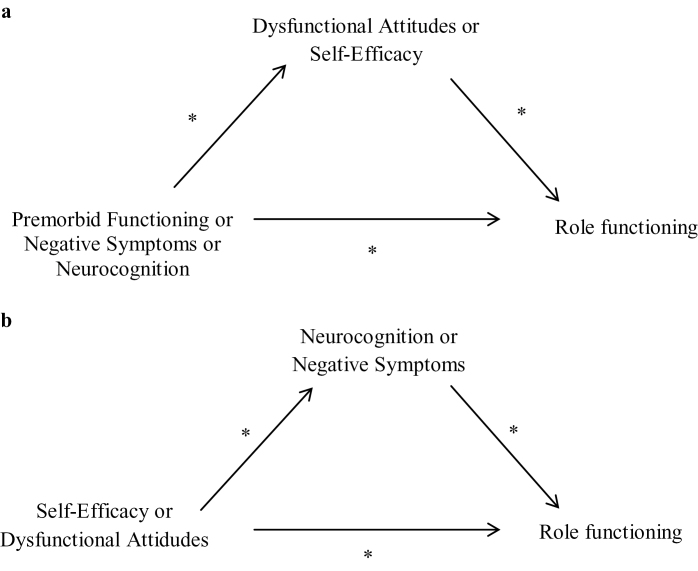
For testing mediation, we used the Sobel test48 to determine the significance of the indirect effect through the mediator for 2 competing models (figures 1a and 1b). We do not present statistics for mediation tests if there was an absence of a significant correlation for any relevent path (indicated by an asterisk in figures 1a and 1b), including between the predictor and the outcome (path A–C), the predictor and the hypothesized mediator (path A–B), and the mediator and the outcome (path B–C). In the absence of a relevant significant correlation, the indirect path cannot be significant. A significant Sobel test is evidence of partial mediation and does not make any claims about the absence or presence of complete mediation.
Fig. 1.
(a) Examination of self-efficacy and dysfunctional attitudes as potential mediators of the relationship between premorbid functioning, negative symptoms, neurocognition, and functioning in the early course of schizophrenia as evaluated using the Sobel test. (b) Examination of negative symptoms and neurocognition as potential mediators of the relationship between self-efficacy and dysfunctional attitudes, and daily functioning in the early course of schizophrenia as evaluated using the Sobel test.
We tested 2 mediation models, one in which dysfunctional attitudes and self-efficacy are the mediators (figure 1a) and one in negative symptoms and neurocognition are the mediators (figure 1b). We found evidence consistent with a model of self-efficacy and dysfunctional attitudes as partial influences on negative symptom level (figure 1b), which in turn was a significant influence on daily functioning (Sobel test, P < .01, for both predictors, table 3). In addition, evidence supported a model in which self-efficacy is a partial contributor to neurocognition (figure 1b), which in turn contributes to daily functioning (Sobel test, P < .01). Also, we note that analyses with experiential negative symptoms as the mediator and Defeatist Performance Attitudes (DPAS) as the predictor were stronger than analyses with expressive negative symptoms as the mediator and DNAS as the predictor.
Table 3.
Results from Sobel Tests of Mediation with Predictors and Potential Mediators (n = 71)
Tests of Mediation With Established Predictors and Attitudinal Beliefs as Potential Mediators Using the Sobel Test (Standardized Values)
| Predictor | Mediator | Outcome | C | c′ | a × b | P Value |
|---|---|---|---|---|---|---|
| Negative symptoms | Dysfunctional attitudes | Role functioning | −0.68 | −0.64 | 0.04 | .35, NS |
| Negative symptoms | Self-efficacy | Role functioning | −0.68 | −0.70 | 0.03 | .74, NS |
| Experiential negative symptoms | Dysfunctional attitudes | Role functioning | −0.68 | −0.63 | −0.03 | .23, NS |
| Experiential negative symptoms | Self-efficacy | Role functioning | −0.68 | −0.65 | −0.03 | .62, NS |
| Expressive negative symptoms | Dysfunctional attitudes | Role functioning | −0.41 | −0.34 | −0.05 | .16, NS |
| Expressive negative symptoms | Self-efficacy | Role functioning | −0.41 | −0.31 | −0.09 | .12, NS |
| Neurocognition | Dysfunctional attitudes | Role functioning | 0.49 | 0.46 | 0.03 | .24, NS |
| Neurocognition | Self-efficacy | Role functioning | 0.49 | 0.24 | 0.25 | .06, NS |
| Premorbid history | Dysfunctional attitudes | Role functioning | 0.62 | 0.58 | 0.04 | .26, NS |
| Premorbid history | Self-efficacy | Role functioning | 0.62 | 0.39 | 0.23 | .28, NS |
| Tests of Mediation with Attitudinal Beliefs as the Predictors and the Established Predictors as Potential Mediators Using the Sobel Test (Standardized Values) | ||||||
| Predictor | Mediator | Outcome | C | c′ | a × b | P Value |
| Dysfunctional attitudes | Negative symptoms | Role functioning | −0.34 | −0.09 | 0.24 | .03 |
| Self-efficacy | Negative symptoms | Role functioning | 0.36 | −0.04 | 0.40 | <.01 |
| Dysfunctional attitudes | Experiential negative symptoms | Role functioning | −0.34 | −0.14 | 0.19 | .06, NS |
| Self-efficacy | Experiential symptoms | Role functioning | 0.36 | 0.05 | 0.31 | <.01 |
| Dysfunctional attitudes | Expressive negative symptoms | Role functioning | −0.34 | −0.23 | 0.11 | .08, NS |
| Self-efficacy | Expressive negative symptoms | Role functioning | 0.36 | 0.22 | 0.14 | .04 |
| Dysfunctional attitudes | Neurocognition | Role functioning | −0.34 | −0.25 | 0.09 | .26, NS |
| Self-efficacy | Neurocognition | Role functioning | 0.36 | 0.22 | 0.14 | .04 |
Note: a × b, indirect path; C, predictor relationship; c′, predictor relationship after controlling for moderator; NS, not significant.
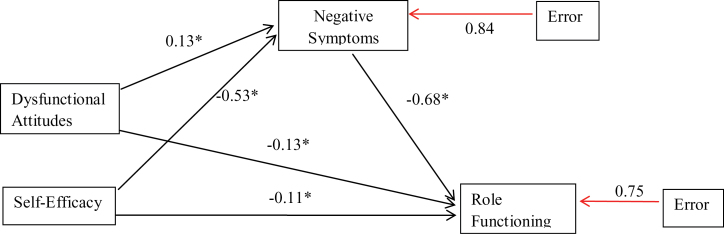
Combined Mediational Analysis
Additionally, we tested a combined mediation model that showed indirect paths for both DAS and SES through negative symptoms as influences on role functioning (figure 2). In this model, there was a significant indirect effect of SES (z = 3.57, P < .01), while the indirect effect of DAS was not significant (z = −1.11, P = .27). These variables were chosen because all pathways in the bivariate associations were statistically significant. For expressive negative symptoms, neither the indirect effect of SES (z = 1.83, P = .07) nor the indirect effect of DAS was significant (z = −.81, P = .42), while for experiential negative symptoms the indirect effect of SES (z = 3.13, P < .01) was significant, while the indirect effect for DAS was not (z = −.71, P = .48).
Fig. 2.
Model that examines the combined effects of self-efficacy and dysfunctional attitudes on daily functioning as mediated through negative symptoms.
Discussion
As far as we are aware, this is the first study to conduct a comprehensive examination of both dysfunctional attitudes and self-efficacy on the same sample, as well as the first study to examine these attitudinal beliefs within recent-onset schizophrenia patients and normal control subjects. We found support for our hypothesis that more dysfunctional attitudes and lower self-efficacy are present in FEP compared with healthy controls. Further, we found significant associations between premorbid functioning, neurocognition, negative symptoms, attitudinal beliefs, and daily functioning. The model proposing that self-efficacy and dysfunctional attitudes appear to make moderately significant, direct contributions to negative symptoms, which in turn act as a mediator contributing to daily functioning was supported. This finding supports Beck and colleagues’ contention that dysfunctional beliefs contribute to the severity of negative symptoms and thus poor outcomes.23,24 We found support for our previous finding that self-efficacy,49 but not dysfunctional attitudes,22 was related to neurocognition in patients. In addition, there was evidence supporting a model in which self-efficacy influences neurocognition, which in turn influences daily functioning.25,36 Self-efficacy and dysfunctional attitudes appear to be moderately related (r = −.38), yet separable constructs. Our findings support the hypotheses previously validated in chronic schizophrenia samples that self-efficacy is not a mediator of the relationship between negative symptoms and daily functioning.33,35 These findings are consistent with research on chronic patients showing that low self-efficacy or dysfunctional beliefs are related in indirect ways through negative symptoms and neurocognition to poor functioning.25,33,35
Consistent with models proposed by Beck and colleagues in chronic patients, our findings suggest that recent-onset patients have higher levels of dysfunctional attitudes compared with healthy controls. On the other hand, we did not find any evidence for the hypothesis that dysfunctional attitudes are mediators of the relationship between negative symptoms and functioning, or between neurocognition and functioning.8,21,22 In addition, our findings did not provide specific support for Grant and Beck’s22 hypothesis that dysfunctional attitudes are related to poor neurocognition. We believe that one of the reasons for these discrepancies is that Grant and Beck (2009) used an abbreviated 10-item Quality of Life measure to define functioning in schizophrenia, ie, based on the patient’s report. This 10-item version was derived from the Quality of Life Scale (QLS; Henrichs et al., 1984), a 21-item scale. According to the authors of the original scale, the QLS balances subjective questions regarding life satisfaction and objective indicators of social and occupational role functioning. The 10-item measure used by Grant and Beck is likely to be assessing to some extent the person’s attitudes and beliefs about the quality of his or her life and as such may be quite proximal to the DAS. In contrast, our measure of functioning was the Global Index from the RFS, which uses behavioral anchor points to measure objective aspects of level of functioning in schizophrenia patients. Thus, our measure of functioning is more objective and does not overlap with attitudes as much as the measure used by Grant and Beck. In addition, Grant and Beck focused on a chronic schizophrenia sample, unlike our recent-onset schizophrenia emphasis. In comparisons with chronic patients (published literature), we noted that the Dysfunctional Need for Acceptance is actually higher in these early course patients, thereby appearing to decrease as the illness progresses. This change may impact relationships of dysfunctional attitudes to other constructs.
Our findings do extend to the early course of schizophrenia the observation that dysfunctional attitudes partially contribute to negative symptoms, which in turn contribute to poor daily functioning.21,50 We agree that negative expectancies regarding positive outcomes may contribute to negative symptoms (eg, lack of motivation), which reduces attempts to engage in daily activities.51 Another interpretation is that the lower levels of dysfunctional attitudes contribute to absence of negative symptoms, which in turn leads to better functioning.
Our findings provide the first evidence that self-efficacy is on average lower in schizophrenia patients (specifically in first-episode patients) than in healthy controls and is related to several domains of daily functioning, such as family and social relationships, and work or school. We extend to the early course of schizophrenia the previous work on chronic patients indicating that high self-efficacy is linked to better functioning. As Bandura (1993) suggested, the mechanism of action is likely to be that a belief in one’s ability to succeed, eg, on a cognitive task, translates to greater cognitive effort, which in turn translates to improved performance. Patients with higher levels of self-efficacy are thus more motivated to put effort into cognitive tasks, which could be especially important during the premorbid phase of illness. This is consistent with the idea that a person’s level of confidence is linked to the achievement of personal goals.52–54 Our findings also support previous work indicating that self-efficacy influences negative symptoms, which in turn has an impact on functional outcome in chronic schizophrenia patients.25,36 Specifically in chronic patients, there is a link between self-efficacy, self-confidence, functional capacity, and increased motivation that could explain successful functioning in daily living.25 The number and magnitude of relationships we found between self-efficacy and premorbid history, negative symptoms, and neurocognition suggest closer interrelationships than is the case for dysfunctional attitudes. This suggests that level of self-efficacy might be the core feature from which dysfunctional attitudes are generated and thus has a greater impact on some aspects of the illness.
The presence of lowered self-efficacy early in the course of illness suggests that these beliefs may be enduring, core features of schizophrenia. If present at early stages such as when symptoms are forming, low self-efficacy can influence the early course of the illness. Further, comparisons with chronic patients (published literature; see table 4) suggest that self-efficacy might continue to decrease with chronicity. Lowered self-efficacy with illness chronicity might be explained by the discouragement associated with continued failure to cope successfully with the challenges of daily living.
Table 4.
Comparisons of Dysfunctional Attitudes and Self-efficacy in First-Episode and Chronic Schizophrenia Patients Means and SDs
| Attitudinal Beliefs | First-Episode | Chronic | t(df) = P Value | |
|---|---|---|---|---|
| Current Study (n = 71) | Horan et al., 2010 (n = 111) | Cardenas et al., 2012 (n = 97) | ||
| Dysfunctional Attitudes Scale Factors | ||||
| DNAS | 35.39 (9.53) | 30.7 (12.1) | — | t(180) = 2.76, P < .01 |
| DPAS | 46.57 (16.52) | 51.2 (18.0) | — | t(180) = −1.75, P = .08 |
| Self-efficacy | 74.12 (18.3) | — | 61.0 (14.1) | t(166) = 5.25, P < .01 |
Note: DNAS, Dysfunctional Need for Acceptance Subscale; DPAS, Defeatist Performance Attitudes Subscale.
Several of the study limitations have been discussed in our prior work on related topics so will only be briefly reviewed.55,56 The primary limitation is that this cross-sectional study cannot make conclusions about the longitudinal nature of these relationships. Furthermore, directional hypotheses are not testable. The selection of variables as “cause” and “effect” is purely theoretical. Future research should be directed at clarifying the longitudinal nature of these relationships and experimentally manipulating the variables through interventions. A second limitation is the moderate sample size of patients. The sample was large enough to successfully detect mediating relationships of moderate strength, but not large enough to detect mediating relationships that are present, but quite weak. Third, as is the case with most studies of schizophrenia patients, the sample is predominately male. Sample size was too small for separate analyses of female patients. Finally, the results would have been strengthened with the administration of identical measures to a chronic sample of individuals with schizophrenia to provide direct comparisons of the effects of chronicity on these observed relationships. Despite these limitations, the study results do have important implications for understanding how impairments in dysfunctional attitudes and self-efficacy contribute to functioning in schizophrenia.
These findings have potential implications for implementing effective interventions that aim to improve daily functioning in early course schizophrenia patients. We provide evidence that supports attempts to reduce negative symptoms and improve cognitive functions, as they are proximal influences on daily functioning. Pharmacological interventions have thus far had limited effectiveness for improving negative symptoms or cognitive deficits. However, cognitive enhancement approaches have been effective in improving cognition to a moderate degree.57 In addition, dysfunctional attitudes and low self-efficacy were present in the early course and therefore may be additional, but less proximal targets for intervention. Using this approach within a Cognitive Behavioral Therapy paradigm would be an indirect way to improve functioning by reducing negative symptoms. Another implication is that increasing self-efficacy might lead to improved cognitive functioning and, in turn, better functional outcome.
Funding
National Institute of Mental Health Grants (MH37705, P50 MH066286 to Principal Investigator K.H.N., PhD). An investigator-initiated grant from Janssen Scientific Affairs, LLC, provided the antipsychotic medication and supplemental funding. Pfizer, Inc. and Genentech, Inc. (J.V.); Janssen Scientific Affairs, LLC, Brain Plasticity, Inc., and Genentech, Inc. (K.H.N.); Otsuka America Pharmaceutical, Inc. (K.L.S.).
Acknowledgments
We would like to thank Julie Bullock for her assistance in data collection, Jacqueline Hayata and Lilian Medina for conducting neurocognitive assessments, and Luana Turner and Nicole DeTore for providing patient case management and conducting symptom assessments. J.V., PhD, has served as a consultant to Brain Plasticity, Inc. and Boehringer-Ingelheim. K.H.N., PhD, has served as a consultant to Genentech, Inc. and Otsuka America Pharmaceutical, Inc. K.L.S., PhD, has served as a consultant to Otsuka America Pharmaceutical, Inc. A.E., BA; D.G.-D., PhD; G.S.H., PhD; and A.V., PhD, have no financial conflicts of interest to disclose.
References
- 1. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330 [DOI] [PubMed] [Google Scholar]
- 2. Mueser KT, Bellack AS, Douglas MS, Wade JH. Prediction of social skill acquisition in schizophrenic and major affective disorder patients from memory and symptomatology. Psychiatry Res. 1991;37:281–296 [DOI] [PubMed] [Google Scholar]
- 3. Albert N, Bertelsen M, Thorup A, et al. Predictors of recovery from psychosis: analyses of clinical and social factors associated with recovery among patients with first-episode psychosis after 5 years. Schizophr Res. 2011;125:257–266 [DOI] [PubMed] [Google Scholar]
- 4. Álvarez-Jiménez M, Gleeson JF, Henry LP, et al. Road to full recovery: longitudinal relationship between symptomatic remission and psychosocial recovery in first-episode psychosis over 7.5 years. Psychol Med. 2012;42:595–606 [DOI] [PubMed] [Google Scholar]
- 5. Couture SM, Granholm EL, Fish SC. A path model investigation of neurocognition, theory of mind, social competence, negative symptoms and real-world functioning in schizophrenia. Schizophr Res. 2011;125:152–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nuechterlein KH, Subotnik KL, Green MF, et al. Neurocognitive predictors of work outcome in recent-onset schizophrenia. Schizophr Bull. 2011;37(s uppl 2):S33–S40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crespo-Facorro B, Ortiz-García de la Foz V, Mata I, et al. Aripiprazole, ziprasidone and quetiapine in the treatment of first-episode nonaffective psychosis: a 12-week randomized, flexible-dose, open-label trial. Schizophr Res. 2013;147:375–382 [DOI] [PubMed] [Google Scholar]
- 8. Leeson V, Joyce EM, Harrison I, Barnes TR. Does the early course of cognitive function in first-episode schizophrenia predict functional outcome? Schizophr Res. 2010;117:280 [Google Scholar]
- 9. Ventura J, Subotnik KL, Guzik LH, et al. Remission and recovery during the first outpatient year of the early course of schizophrenia. Schizophr Res. 2011;132:18–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams LM, Whitford TJ, Flynn G, et al. General and social cognition in first episode schizophrenia: identification of separable factors and prediction of functional outcome using the IntegNeuro test battery. Schizophr Res. 2008;99:182–191 [DOI] [PubMed] [Google Scholar]
- 11. Allott K, Liu P, Proffitt TM, Killackey E. Cognition at illness onset as a predictor of later functional outcome in early psychosis: systematic review and methodological critique. Schizophr Res. 2011;125:221–235 [DOI] [PubMed] [Google Scholar]
- 12. Lin A, Wood SJ, Yung AR. Measuring psychosocial outcome is good. Curr Opin Psychiatry. 2013;26:138–143 [DOI] [PubMed] [Google Scholar]
- 13. MacBeth A, Gumley A. Premorbid adjustment, symptom development and quality of life in first episode psychosis: a systematic review and critical reappraisal. Acta Psychiatr Scand. 2008;117:85–99 [DOI] [PubMed] [Google Scholar]
- 14. Malla AK, Norman RM, Takhar J, et al. Can patients at risk for persistent negative symptoms be identified during their first episode of psychosis? J Nerv Ment Dis. 2004;192:455–463 [DOI] [PubMed] [Google Scholar]
- 15. Kern RS, Glynn SM, Horan WP, Marder SR. Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull. 2009;35:347–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. González-Ortega I, de Los Mozos V, Echeburúa E, et al. Working memory as a predictor of negative symptoms and functional outcome in first episode psychosis. Psychiatry Res. 2013;206:8–16 [DOI] [PubMed] [Google Scholar]
- 17. Ventura J, Tom SR, Jetton C, Kern RS. Memory functioning and negative symptoms as differential predictors of social problem solving skills in schizophrenia. Schizophr Res. 2013;143:307–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Faerden A, Barrett EA, Nesvåg R, et al. Apathy, poor verbal memory and male gender predict lower psychosocial functioning one year after the first treatment of psychosis. Psychiatry Res. 2013;210:55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chang WC, Yee Man Tang J, Lai Ming Hui C, et al. The relationship of early premorbid adjustment with negative symptoms and cognitive functions in first-episode schizophrenia: a prospective three-year follow-up study. Psychiatry Res. 2013;209:353–360 [DOI] [PubMed] [Google Scholar]
- 20. Peña J, Segarra R, Ojeda N, García J, Eguiluz JI, Gutiérrez M. Do the same factors predict outcome in schizophrenia and non-schizophrenia syndromes after first-episode psychosis? A two-year follow-up study. J Psychiatr Res. 2012;46:774–781 [DOI] [PubMed] [Google Scholar]
- 21. Horan WP, Rassovsky Y, Kern RS, Lee J, Wynn JK, Green MF. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. J Psychiatr Res. 2010;44:499–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rector NA. Dysfunctional attitudes and symptom expression in schizophrenia: differential associations with paranoid delusions and negative symptoms. JCognPsychother. 2004;18:163–173 [Google Scholar]
- 24. Rector NA, Beck AT, Stolar N. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. 2005;50:247–257 [DOI] [PubMed] [Google Scholar]
- 25. Cardenas V, Abel S, Bowie CR, et al. When functional capacity and real-world functioning converge: the role of self-efficacy. Schizophr Bull. 2013;39:908–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163:418–425 [DOI] [PubMed] [Google Scholar]
- 27. Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Worth Publishers; 1997 [Google Scholar]
- 28. Ventura J, Reise SP, Keefe RS, et al. The Cognitive Assessment Interview (CAI): development and validation of an empirically derived, brief interview-based measure of cognition. Schizophr Res. 2010;121:24–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nuechterlein KH, Dawson ME. Vulnerability models for schizophrenia: state of the art. In: Hafner H, Gattaz WF, Janzarik W, eds. Search for the Causes of Schizophrenia. Berlin: Springer-Verlag; 1987:297–316 [Google Scholar]
- 30. Mueser KT, Curran PJ, McHugo GJ. Factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol Assess. 1997;9:196–204 [Google Scholar]
- 31. Ventura J, Nuechterlein KH, Green MF, Horan WP, Subotnik KL, Mintz J. The timing of negative symptom exacerbations in relationship to positive symptom exacerbations in the early course of schizophrenia. Schizophr Res. 2004;69:333–342 [DOI] [PubMed] [Google Scholar]
- 32. Beck AT, Grant PM, Huh GA, Perivoliotis D, Chang NA. Dysfunctional attitudes and expectancies in deficit syndrome schizophrenia. Schizophr Bull. 2013;39:43–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kurtz MM, Olfson RH, Rose J. Self-efficacy and functional status in schizophrenia: relationship to insight, cognition and negative symptoms. Schizophr Res. 2013;145:69–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hill K, Startup M. The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: the mediating role of self-efficacy. Psychiatry Res. 2013;206:151–157 [DOI] [PubMed] [Google Scholar]
- 35. Pratt SI, Mueser KT, Smith TE, Lu W. Self-efficacy and psychosocial functioning in schizophrenia: a mediational analysis. Schizophr Res. 2005;78:187–197 [DOI] [PubMed] [Google Scholar]
- 36. Suzuki M, Amagai M, Shibata F, Tsai J. Factors related to self-efficacy for social participation of people with mental illness. Arch Psychiatr Nurs. 2011;25:359–365 [DOI] [PubMed] [Google Scholar]
- 37. Granholm E, Holden J, Link PC, McQuaid JR, Jeste DV. Randomized controlled trial of cognitive behavioral social skills training for older consumers with schizophrenia: defeatist performance attitudes and functional outcome. Am J Geriat Psychiat. 2013;21:251–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nuechterlein KH, Dawson ME, Gitlin M, et al. Developmental processes in schizophrenic disorders: longitudinal studies of vulnerability and stress. Schizophr Bull. 1992;18:387–425 [DOI] [PubMed] [Google Scholar]
- 39. Carpenter BN, Chapman LJ. Premorbid status in schizophrenia and abstract, literal, or autistic proverb interpretation. J Abnorm Psychol. 1982;91:151–156 [DOI] [PubMed] [Google Scholar]
- 40. Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “The drift busters.” Int J Method Psychiat Res. 1993;3:221–244 [Google Scholar]
- 41. Horan WP, Kern RS, Tripp C, et al. Efficacy and specificity of social cognitive skills training for outpatients with psychotic disorders. J Psychiatr Res. 2011;45:1113–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–213 [DOI] [PubMed] [Google Scholar]
- 43. Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72:29–39 [DOI] [PubMed] [Google Scholar]
- 44. Weissman AN, Beck AT. Development and validation of the dysfunctional attitude scale: apreliminary investigation. Paper presented at the 62nd Annual Meeting of the American Educational Research Association; March 27–31, 1978; Toronto, Ontario, Canada.
- 45. McDermott BE. Development of an instrument for assessing self-efficacy in schizophrenic spectrum disorders. J Clin Psychol. 1995;51:320–331 [PubMed] [Google Scholar]
- 46. Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment Health J. 1993;29:119–131 [DOI] [PubMed] [Google Scholar]
- 47. Green RS, Gracely EJ. Selecting a rating scale for evaluating services to the chronically mentally ill. Community Ment Health J. 1987;23:91–102 [DOI] [PubMed] [Google Scholar]
- 48. Sobel M. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, ed. Sociological Methodology 1982. San Francisco: Jossey-Bass; 1982:290–312 [Google Scholar]
- 49. Ventura J, Nuechterlein KH, Subotnik KL, Green MF, Gitlin MJ. Self-efficacy and neurocognition may be related to coping responses in recent-onset schizophrenia. Schizophr Res. 2004;69:343–352 [DOI] [PubMed] [Google Scholar]
- 50. Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry. 2012;69:1216–1224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Horan WP, Green MF, Kring AM, Nuechterlein KH. Does anhedonia in schizophrenia reflect faulty memory for subjectively experienced emotions? J Abnorm Psychol. 2006;115:496–508 [DOI] [PubMed] [Google Scholar]
- 52. Bandura A, Locke EA. Negative self-efficacy and goal effects revisited. J Appl Psychol. 2003;88:87–99 [DOI] [PubMed] [Google Scholar]
- 53. Schnoll RA, James C, Malstrom M, et al. Longitudinal predictors of continued tobacco use among patients diagnosed with cancer. Ann Behav Med. 2003;25:214–222 [DOI] [PubMed] [Google Scholar]
- 54. O’Brien KM. Measuring career self-efficacy: promoting confidence and happiness at work. In: Lopez, S. J., Snyder, C. R., eds. Positive psychological assessment: A handbook of models and measures (pp. 109-126). Washington, DC: American Psychological Association; 2003: xvii, 495.
- 55. Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113:189–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ventura J, Thames AD, Wood RC, Guzik LH, Hellemann GS. Disorganization and reality distortion in schizophrenia: a meta-analysis of the relationship between positive symptoms and neurocognitive deficits. Schizophr Res. 2010;121:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472–485 [DOI] [PubMed] [Google Scholar]