Abstract
Theoretical models postulate an important role of attributional style (AS) in the formation and maintenance of persecutory delusions and other positive symptoms of schizophrenia. However, current research has gathered conflicting findings. In a cross-sectional design, patients with persistent positive symptoms of schizophrenia (n = 258) and healthy controls (n = 51) completed a revised version of the Internal, Personal and Situational Attributions Questionnaire (IPSAQ-R) and assessments of psychopathology. In comparison to controls, neither patients with schizophrenia in general nor patients with persecutory delusions (n = 142) in particular presented an externalizing and personalizing AS. Rather, both groups showed a “self-blaming” AS and attributed negative events more toward themselves. Persecutory delusions were independently predicted by a personalizing bias for negative events (beta = 0.197, P = .001) and by depression (beta = 0.152, P = .013), but only 5% of the variance in persecutory delusions could be explained. Cluster analysis of IPSAQ-R scores identified a “personalizing” (n = 70) and a “self-blaming” subgroup (n = 188), with the former showing slightly more pronounced persecutory delusions (P = .021). Results indicate that patients with schizophrenia and patients with persecutory delusions both mostly blamed themselves for negative events. Nevertheless, still a subgroup of patients could be identified who presented a more pronounced personalizing bias and more severe persecutory delusions. Thus, AS in patients with schizophrenia might be less stable but more determined by individual and situational characteristics that need further elucidation.
Key words: schizophrenia, persecutory delusions, positive symptoms, attributional style, depression, negative emotions
Attributional style (AS) is defined as the way of inferring a causal explanation for important life events,1,2 either toward oneself (internal), toward other persons (personal), or toward circumstances or fate (situational). For example, if “a friend starts a fight with me,” it is possible to attribute this event to internal factors (“I am a bad person”), to personal factors (“He is annoyed quite quickly”), or to situational factors (“We lived in different parts of the country”).
Analysis of AS in schizophrenia derived from the clinical insight that persecutory delusions can be viewed as an excessive tendency to attribute negative events toward other persons. Initial studies used the Attributional Style Questionnaire (ASQ),3 an instrument originally developed for the assessment of AS in depression. These studies found that patients with persecutory delusions showed more internal attributions for positive events and less internal attributions for negative events, compared with controls. This AS has been termed self-serving bias or externalizing bias (EB). 4–6 Because the ASQ showed quite low reliability indices (Cronbach’s alpha between .39 and .52)7 and cannot differentiate between external attributions toward other persons (personal attributions) and toward circumstances (situational attributions), Kinderman and Bentall7 developed the Internal, Personal and Situational Attributions Questionnaire (IPSAQ) and found that patients with persecutory delusions blamed other persons more often than circumstances for negative events, which supports the personalizing bias (PB) hypothesis.8,9
Due to these findings, EB and PB were incorporated into theoretical models as cognitive biases triggering the development and maintenance of persecutory delusions10–12 and positive symptoms in schizophrenia.13–15
However, recent research has questioned these assumptions because several studies that used the IPSAQ and compared patients with persecutory delusions and controls did not find the hypothesized EB and PB 16–21 or even found a less pronounced EB. 11 Studies that compared patients with schizophrenia and controls found a more pronounced EB but an equivalent level of PB in patients5,22 or no differences between patients and controls.23 Even in a recent meta-analysis, neither a pronounced EB nor a pronounced PB could be identified in patients with schizophrenia (n = 212) in comparison to controls.24
These inconsistent results could be explained by a number of factors: First, previous studies in patients with persecutory delusions were mostly of small sample size (between 14 and 40 patients:),6,9 which may have obscured or even exaggerated results with a medium or minor effect size.25 The problem of small sample sizes is aggravated by patients’ heterogenity with regard to psychopathology. Consequently, a large-scale study is necessary in order to address the question of whether EB and PB are associated with persecutory delusions and schizophrenia.
Second, some inconsistent results could be explained by specific features of the questionnaires used. While the IPSAQ by Kinderman and Bentall9 introduced the important discrimination between personal and situational external attributions, it is not without problems either, with regard to its limited reliability (0.61–0.76)7,26 and also with regard to its demand characteristics. The IPSAQ forces a person to make a clear choice whether an event is caused exclusively by internal, personal, or situational factors even if a person (realistically) assumes that an event is caused by multiple factors. Patients with schizophrenia might have particular problems in making such a decision because they often tend to decide spontaneously, without gathering a sufficient amount of information (jumping to conclusions bias).27,28 Thus, the use of the original IPSAQ might lead to a distorted view of AS in patients with schizophrenia, and possibly to inconsistent findings as well.
Rather than enforcing respondents to choose between 3 attributional alternatives by method, it is interesting to study whether patients with schizophrenia and persecutory delusions indeed present a more “monocausal” AS in comparison to controls who might present a more balanced and “multifactorial” view. Finally, in light of patients’ heterogeneity with regard to psychopathology, it is interesting to assess whether there are distinct subgroups of patients who might differ with regard to their AS.
In order to derive clear-cut evidence about the presence and clinical correlations of AS, we conducted a large multicenter study with patients with positive symptoms of schizophrenia and controls, employing a revised version of the IPSAQ that allows the subject to rate the relative degree of the contribution of internal, personal, and situational factors toward important life events (IPSAQ-R).29,30 We hypothesize (1) that patients with persistent positive symptoms and (2) especially patients with persecutory delusions show a more pronounced EB, PB, and mono causality bias in comparison to controls. Furthermore, (3) we assumed that externalizing, personalizing, and monocausal AS are associated with delusions of persecution and (4) that distinct subgroups of patients who differ in their AS can be identified empirically.
Method
Participants
Participants were 258 patients with schizophrenia and 51 healthy controls from the “Cognitive behavioural therapy for persistent positive symptoms (CBTp) in psychotic disorders” Trial31 (ISRCTN29242879), a multicentered randomized controlled trial investigating the efficacy of CBTp for patients with schizophrenia in comparison to supportive therapy. Patients were recruited from 6 different psychiatric settings; healthy controls were recruited via press releases and matched with regard to age, gender, and education to the first 51 patients that were already recruited.
From the study sample (n = 330), several patients (n = 57) did not participate at this ancillary study: 9 patients dropped out before they were asked to participate, 48 patients refused to be tested for the ancillary study. From the remaining sample (n = 273), several patients (n = 15) were excluded because they did not understand the instructions of the IPSAQ-R: They presented no causal explanation for more than 3 items (n = 12), they stated “I don’t know” as a causal explanation for more than 3 situations (n = 2), or they wrote down the same causal explanation for more than 3 situations (n = 1). There were no statistically significant differences between patients who refused to be tested and those who endorsed testing with regard to sociodemographic and clinical variables (all P > .10).
Patients were diagnosed with a schizophrenia spectrum disorder (schizophrenia [n = 201], schizophreniform disorder [n = 5], schizoaffective disorder [n = 33], delusional disorder [n = 17]) as assessed with the Structured Clinical Interview for DSM-IV32 according to DSM-IV-TR.33 Further inclusion criteria were persistent positive symptoms for at least the last 3 months and a minimum score of 4 in the item P1 (delusions in general: n = 219) or in the item P3 (hallucinations: n = 39) of the Positive and Negative Syndrome scale (PANSS),34 age between 18 and 59, adequate language fluency and a verbal intelligence quotient (IQ) > 80 in the German vocabulary IQ test MWT-B.35 In line with other studies,9,17,18 exclusion criteria for controls were mental disorders in their lifetime. Most of the patients (n = 142, 64.8%) presented delusions of persecution (defined as a minimum score of 4 in the PANSS item P6). All participants were informed about the assessment and gave written informed consent. The ethics committees at the 6 centers’ medical faculties approved the study.
Measures
The IPSAQ-R29,30 consists of 16 items describing 8 positive and 8 negative situations. For each item, subjects are asked to put themselves in the position of someone experiencing the particular situation and to infer and write down the most probable causal explanation for it. They are then asked to estimate in percent whether their causal explanation is due to internal, personal, or situational factors. For example, if a person interprets the item “A friend says that he does not respect you” in the sense of “I am a bad person,” an estimation of the causal explanation as 80% internal, 20% personal, and 20% situational would be consistent. If the percentage estimations do not add up to 100%, they are rescaled so that their sum equals 100%. First, for every item, the sum of percentage estimations for internal, personal, and situational attributions is computed (eg, 40% internal + 50% personal + 70% situational = 180%). In the next step, the rescaled percentage estimations are computed as follows: rescaled percentage estimation = (former percentage estimation × 100)/former sum of percentage estimations (eg, rescaled percentage estimation = (40 × 100)/180 = 22.22%).
Six attributional scores are calculated by adding up the rescaled percent ratings of internal, personal, and situational attributions for positive and negative events. Moreover, several biases are computed according to previous studies.7 EB only regards internal attributions and is present when a person attributes more positive than negative events toward internal causes, hence to himself/herself. It is computed by subtracting the internal negative score from the internal positive score. The PB only regards negative events and is present when a person attributes negative events rather to personal than to situational factors. It is calculated by dividing the personal negative score by the sum of personal negative score and situational negative score. Moreover, in accordance to Moritz et al,30 a mono causality bias was present if a person at least in 1 situation estimates that an event is caused by 1 attributional factor by a minimum score of 80%. It was computed by counting the items that were rated in this way. Range of Cronbach’s alpha for attributional scores indicated sufficient to good internal consistency (between .71 and .81 [mean = .79] in patients and between .75 and .83 [mean = .79] in controls).
The PANSS34 is a semistructured interview assessing 30 symptoms divided into 3 standard scales (positive symptoms, negative symptoms, general psychopathology) using a 7-point Likert scale. PANSS rating was performed by trained raters, interrater reliability (correlation R 2) was satisfactory to high (.92 for the PANSS positive scale and .86 for the PANSS negative scale).31
The Calgary Depression Rating Scale for Schizophrenia (CDSS)36 was used in order to assess observer-rated depressive symptoms.
Analysis
First, we used Fisher’s exact tests, Chi-square tests, t tests, and ANOVAs in order to compare patients with schizophrenia and controls and patients with persecutory delusions (PD), patients without persecutory delusions (Non-PD), and controls in sociodemographic and clinical variables. In case of group differences in specific variables, it was analyzed whether these variables are related to AS, using Pearson’s 2-tailed correlations. If these variables were related to AS, they were included as covariates in all statistical analyses.
All IPSAQ-R scores were normally distributed within all groups with the exception of EB and mono causality bias, and inspection of the data revealed no outliers. In order to investigate differences in AS and attributional biases between patients with schizophrenia and controls (Hypothesis 1), ANOVAs were performed using attributional scores and biases as dependent variables if Levene tests indicated homogeneous variances, even if variables were not normally distributed, because parametric tests show higher statistical power compared with nonparametric tests.37,38 In case of heterogeneous variances (mono causality bias), nonparametric tests were used (Mann-Whitney U test, Kruskal-Wallis test). We controlled these tests for important covariates by performing a linear regression analysis using the covariate as predictor and mono causality bias as criterion and saved the standardized residuum scores. These scores were included as dependent variables in nonparametric tests. In order to prevent alpha inflation, Bonferroni corrections were performed for each event type (eg, for positive events: P = .05/3 attributional loci = 0.017). The same procedure was used in order to assess differences between patients with persecutory delusions and controls in attribution biases (Hypothesis 2).
In order to investigate whether attribution biases are associated with delusions of persecution (Hypothesis 3), we first examined bivariate relations between sociodemographic variables, delusions of persecution (PANSS item P6), and attribution biases using Pearson’s 2-tailed correlations. Second, all variables that showed a statistically significant association with persecutory delusions were included into the multivariate regression analysis (ENTER method) predictors and persecutory delusions were included as criterion. Multivariate regression analysis was controlled for multicollinearity by investigating the variance inflation factors and tolerance statistics. Finally, we analyzed whether there are distinct subgroups of patients with a comparable AS who could be identified empirically by a hierarchical cluster analysis (Hypothesis 4). The Ward’s method was used, and the 6 IPSAQ-R scores in the patient sample were included as cluster variables and squared Euclidian distance as distance measure.
Results
Table 1 shows sociodemographic and clinical data of patients with schizophrenia, patients with persecutory delusions (PD), patients without persecutory delusions (Non-PD), and healthy controls. There were no statistically significant differences between patients with schizophrenia and controls and between PD, Non-PD, and controls in terms of age, gender, or education. Compared with controls, patients with schizophrenia showed significantly lower verbal intelligence scores (MWT-B). Moreover, both PD and Non-PD showed a lower verbal intelligence score in comparison to controls. In comparison to Non-PD, PD presented a more pronounced level of positive symptoms and depressive symptoms, while both groups were comparable in terms of negative symptoms.
Table 1.
Means, Standard Ddeviations, and Comparisons of Patients With Sschizophrenia and Controls Regarding Sociodemographic and Clinical Variables
| Patients With Schizophrenia (n = 258); n (%)/M (SD) | Healthy Controls (HC) (n = 51); n (%)/M (SD) | Test Statistics | Patients With Persecutory Delusions (PD) (n = 142); n (%)/M (SD) | Patients Without Persecutory Delusions (Non-PD) (n = 116); n (%)/M (SD) | Test Statistics | |
|---|---|---|---|---|---|---|
| Gender (female) | 107 (41.5%) | 21 (41.2%) | P = .969a | 58 (40.85%) | 49 (42.24%) | X 2 (2) = .158, P = .924 |
| Education grade completedb | 13 y: 135, 10 y: 74, 9 y: 48, none: 3 | 13 y: 26, 10 y: 23, 9 y: 2 | Χ 2 (5) = 10.223, P = .069 | High: 75, medium: 40, low: 30, none: 2 | High: 61, medium: 35, low: 18 2 | Χ 2 (10) = 16.119, P = .096 |
| Age (y) | 37.44 (9.54) | 35.77 (9.47) | F(1,307) = 0.152, P = .284 | 37.75 (9.6) | 37.32 (9.62) | F(2,306) = 0.742, P = .477 |
| Verbal IQ | 107.29 (14.88) | 114.88 (15.38) | F(1,307) = 11.053, P ≤ .001 | 105.98 (15.57) | 107.13 (14.49) | F(2,306) = 5.511, P = .004; PD, Non-PD < HC |
| Duration of illness | 15.03 (9.97) | 14.50 (9.51) | 15.44 (10.14) | F(1,256) = .617, P = .433 | ||
| PANSS POS | 17.44 (3.50) | 18.50 (3.30) | 15.94 (3.33) | F(1,256) = 38.550, P ≤ .001 | ||
| PANSS NEG | 13.90 (4.21) | 14.19 (4.23) | 13.56 (3.95) | F(1,256) = 1.538, P = .216 | ||
| PANSS GEN | 32.94 (6.94) | 34.01 (7.12) | 31.70 (6.64) | F(1,256) = 7.141, P = .008 | ||
| PANSS P1 | 4.21 (1.18) | 4.57 (.81) | 3.74 (1.36) | F(1,256) = 37.840, P ≤ .001 | ||
| PANSS P6 | 3.52 (1.46) | 4.56 (.71) | 2.11 (.82) | F(1,256) = 591.897, P ≤ .001 | ||
| CDSS | 5.47 (4.66) | 6.22 (5.00) | 4.58 (3.90) | F(1,256) = 8.372, P = .004 |
Note: MWT-B = Mehrfachwahl-Wortschatz-Intelligenztest-B (MWT-B), a German vocabulary IQ test; PANSS = Positive and Negative Syndrome scale; PANSS POS = PANSS positive scale sum score; PANSS NEG = negative scale sum score; PANSS GEN = PANSS general psychopathology sum score; PANSS P1 = item delusions in general mean score; PANSS P6 = item persecution/suspiciousness mean score; CDSS: Calgary Depression Scale for Schizophrenia sum score.
aFishers exact test.
beducation grade completed after 9 years = “Hauptschulabschluss,” education grade completed after 10 years = “Realschulabschluss,” education grade completed after 13 years = “Abitur” (A-level or high school equivalent).
As only the mono causality bias was related to verbal intelligence (patient group: r = −.215, P = .004; controls: r = −.338, P = .018), all group comparisons in mono causality bias were controlled for verbal intelligence.
Group Comparisons in AS
Results of comparisons between patients and controls in AS are depicted in table 2. Because most Levene tests indicated homogeneous variances (all P > .05), groups were compared in their AS with ANOVAs. With regard to mono causality bias, we used a Mann-Whitney U tests because the Levene test indicated heterogeneous variances. In comparison to controls, patients with schizophrenia presented more internal attributions and less personal attributions for negative events and a reduced EB. With regard to other attributional scores, there were no statistically significant differences between the 2 groups. The observed effect sizes (partial eta)2 indicated large effects.
Table 2.
Comparisons Between Patients and Controls in the Scores of the Internal, Personal and Situational Attributions Questionnaire Revised Version
| Patients With Positive Symptoms (n = 258) | Healthy Controls (n = 51) | Statistics | |
|---|---|---|---|
| Internal positive scorea | 53.58 (15.10) | 54.50 (13.69) | F(1,307) = .972, P = .325, partial eta2 = .003 |
| Personal positive scorea | 28.22 (12.84) | 30.86 (11.64) | F(1,307) = 2.842, P = .093, partial eta2 = .009 |
| Situational positive scorea | 18.20 (11.75) | 14.64 (9.86) | F(1,307) = 2.919, P = .089, partial eta2 = .009 |
| Internal negative scoreb | 43.33 (16.05) | 36.43 (11.46) | F(1,307) = 5.857, P = .016, partial eta2 = .019 |
| Personal negative scoreb | 36.18 (14.69) | 43.68 (15.63) | F(1,307) = 14.911, P ≤ .001, partial eta2 = .047 |
| Situational negative scoreb | 20.49 (12.97) | 19.89 (13.17) | F(1,307) = .000, P = .983, partial eta2 = .000 |
| Externalizing bias c | 10.25 (17.64) | 18.07 (15.77) | F(1,307) = 8.284, P = .004, partial eta2 = .026 |
| Personalizing bias c | .64 (.20) | .69 (.18) | F(1,307) = 2.649, P = .105, partial eta2 = .009 |
| Monocausality bias d | 2.20 (3.45) | 1.59 (2.30) | U = 5626.000, P = .367 |
aANOVA with Bonferroni corrections for all positive events: P = .05/3 = .17.
bANOVA with Bonferroni corrections for all negative events: P = .05/3 = .17.
cSeparate ANOVAs
dMann-Whitney U tests using residual scores of mono causality bias (controlled for the influence of verbal intelligence [MWT-B]).
In the next step, patients with persecutory delusions (PD: n = 142) were compared with controls. Again, because all Levene tests (with the exception of the mono causality bias) indicated homogeneous variances (all P > .05), groups were compared in their AS with ANOVAs. With regard to mono causality bias, we used Mann-Whitney U tests because the Levene test indicated heterogeneous variances. As depicted in table 3, results were largely comparable to those in the full sample; in comparison to controls, patients showed fewer personal attributions for negative events and a reduced EB. The observed effect sizes indicated large effects. With regard to other attributional scores, there were no statistically significant differences between the 2 groups.
Table 3.
Comparisons Between Patients With Persecutory Delusions and Controls in the Scores of the Internal, Personal and Situational Attributions Questionnaire Revised Version
| Patients with persecutory delusions (n = 142) | Healthy controls (n=51) | Statistics | |
|---|---|---|---|
| Internal positive scorea | 52.54 (14.39) | 54.50 (13.69) | F(1,195) = 1.793, P = .182, partial eta2 = .009 |
| Personal positive scorea | 29.77 (13.09) | 30.86 (11.64) | F(1,195) = .692, P = .407, partial eta2 = .004 |
| Situational positive scorea | 17.69 (11.24) | 14.64 (9.86) | F(1,195) = 2.141, P = .145, partial eta2 = .011 |
| Internal negative scoreb | 42.77 (15.13) | 36.43 (11.46) | F(1,195) = 5.301, P = .022, partial eta2 = .026 |
| Personal negative scoreb | 37.65 (14.18) | 43.68 (15.63) | F(1,195) = 9.147, P = .003, partial eta2 = .045 |
| Situational negative scoreb | 19.58 (12.67) | 19.89 (13.17) | F(1,195) = .162, P = .688, partial eta2 = .001 |
| Externalizing bias c | 9.77 (16.64) | 18.07 (15.77) | F(1,195) = 9.993, P = .002, partial eta2 = .049 |
| Personalizing bias c | .66 (.19) | .69 (.18) | F(1,195) = .837, P = .361, partial eta2 = .004 |
| Monocausality bias d | 1.86 (3.06) | 1.59 (2.30) | U = 2966.500, P = .180 |
aANOVA with Bonferroni corrections for all positive events: P = .05/3 = .17.
bANOVA with Bonferroni corrections for all negative events: P = .05/3 = .17.
cSeparate ANOVAs.
dMann-Whitney U tests using residual scores of mono causality bias (controlled for the influence of verbal intelligence [MWT-B]).
Associations Between AS and Delusions of Persecution
First, bivariate correlation analysis revealed that persecutory delusions were associated with a pronounced PB (r = .164, P = .008) and with more severe depression (CDSS sum: r = .130, P = .037). Sociodemographic and other clinical variables were not related to persecutory delusions. In the next step, we performed a multivariate regression analysis using PB and depression as predictors and persecutory delusions as criterion variable. The model was statistically significant [F(2,254) = 8.013, P ≤ .001, adjusted R 2 = .052)], and both depression (β = .152; P = .013) and PB (β =.197; P = .001) were significant predictors, the amount of explained variance in delusions of persecution indicated a small effect size. Including the interaction between PB and depression as predictor did not explain a significant amount of variance (P > .10), in comparison to the first model.
Cluster Analyses
Finally, a hierarchical cluster analysis was performed. Inspection of squared Euclidian distance led to a plausible 2-cluster solution (Cluster 1: 188 patients, Cluster 2: 70 patients). As depicted in table 4, patients in the first cluster presented a less pronounced PB, compared with controls. In comparison to controls and patients in the first cluster, patients in the second cluster presented a more pronounced PB.
Table 4.
Comparisons of the 2 Clusters and Controls in Their Attributional Style in the Internal, Personal and Situational Attributions Questionnaire, Revised Version
| Patients in Cluster 1 (C1) (n = 188) | Patients in Cluster 2 (C2) (n = 70) | Healthy Controls (n = 51) | Statistics | |
|---|---|---|---|---|
| Internal positive scorea,b | 54.70 (16.0) | 49.61 (12.50) | 54.50 (13.69) | F(2,306) = 3.856, P = .022, partial eta2 = .025 |
| Personal positive scorea,b | 23.45 (10.44) | 41.07 (10.87) | 30.86 (11.64) | F(2,306) = 61.083, P ≤ .001, partial eta2 = .287, C2 > C1, HC, HC > C1 |
| Situational positive scoreb,c | 21.85 (11.56) | 9.32 (6.20) | 14.64 (9.86) | Chi2 = 75.469, P ≤ .001, C1> C2,HC, HC > C1 |
| Internal negative scorec,d | 46.59 (16.59) | 40.87 (14.19) | 36.43 (11.46) | Chi2= 10.100, P = .006, C1 > HC |
| Personal negative scorec,d | 29.02 (11.15) | 49.19 (12.47) | 43.68 (15.63) | Chi2 = 118.981, P ≤ .001, C2 > C1, HC, HC > C1 |
| Situational negative scorec,d | 24.09 (12.68) | 9.94 (6.49) | 19.89 (13.17) | Chi2 = 73.769, P ≤ .001, C1 > C2, HC > C2 |
| Externalizing bias a | 8.11 (17.32) | 8.74 (18.50) | 18.07 (15.77) | F(2,306) = 4.147, P = .017, partial eta2 = .027, C1 < HC |
| Personalizing bias c | .57 (.17) | .84 (09) | .69 (.18) | Chi2 = 118.396, P ≤ .001, C2 > C1, HC, HC > C1 |
| Monocausality bias d,e | 1.78 (2.97) | 4.94 (4.40) | 1.52 (2.27) | Chi2 = 3.993, P = .136 |
aANOVA.
bBonferroni corrections for all positive events: P = .05/3 = .17.
cKruskal-Wallis test.
dANOVA with Bonferroni corrections for all negative events: P = .05/3 = .17.
eKruskal-Wallis test using residual scores of mono causality bias (controlled for the influence of verbal intelligence [MWT-B]).
In the next step, clusters were compared with regard to sociodemographic and clinical variables using t tests (2-tailed). There was only 1 statistically significant difference between the 2 clusters: Patients in the second cluster showed more pronounced delusions of persecution [PANSS P6: Cluster 1: mean = 3.40 (SD = 1.48), Cluster 2: mean = 3.87 (SD = 1.31); F(1,256) = 5.462, P = .02, partial eta2 =.021); group differences were of medium effect size.
Discussion
In comparison to controls, patients with schizophrenia and patients with persecutory delusions showed a “self-blaming” AS and attributed negative events more toward themselves in comparison to positive events. Nevertheless, persecutory delusions were independently predicted by a pronounced PB and by depression. Finally, in a cluster analysis of IPSAQ-R scores, a “personalizing” and a “self-blaming” subgroup could be identified, with the former showing slightly more severe persecutory delusions.
With regard to a “self-blaming” AS, our results are in striking contrast to previous studies that used the classic IPSAQ and reported a comparable23 or even more pronounced EB in patients with schizophrenia5,22 or in patients with persecutory delusions.16–20 Nevertheless, our results are in line with 1 previous study that used the classic IPSAQ and reported a self-blaming AS in patients with persecutory delusions.9 Moreover, in concordance with our results, patients with schizophrenia belonging to a black ethnic group blamed themselves more for social disadvantages, whereas other patients attributed them toward other persons.39
Several points should be made regarding these results: Because the internal consistency scores in our study are quite satisfactory and our patient sample is more than 4 times larger than previous studies, measure errors are less likely to occur.
One explanation for these inconsistent results might lie in different demand characteristics of the measures used. The forced choice that is required in the classic IPSAQ could induce an exaggerated externalizing and personalizing AS in patients with schizophrenia: Because they are asked to decide between internal, personal, and situational causes for important life events, they might be overstrained, show their well-known jumping to conclusions bias,28 and make their decision based on intuitive and heuristic judgements associated with the faster but more error-prone System 1 according to Kahneman and Fredericks’ dual-process theory of judgments40–42 or the intuitive route of thinking according to Nelson’s 2 routes model of responding to a situation for patients with schizophrenia.43 This might be reflected in the low internal consistency scores of the classic IPSAQ (between .61 and.76).7,26
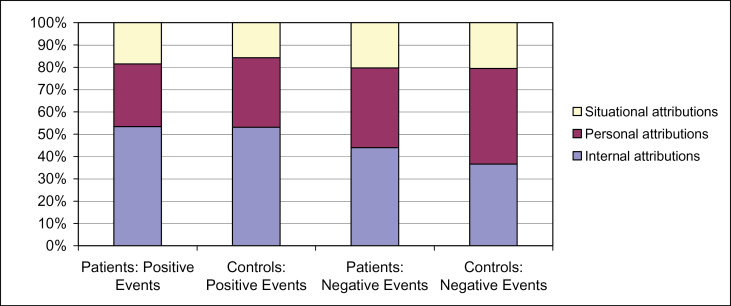
Fig. 1.
Proportional attributions of causes for positive and negative events in patients with schizophrenia and controls.
In contrast, we used the IPSAQ-R, so our patients were not forced to choose among internal, personal, and situational causes but were asked to rate the probability of these causes. It is likely that this kind of probability judgement might require more analytic reasoning and the use of higher cognitive capacities that are linked to the less error-prone System 2 of Kahneman and Fredericks’ dual-process theory.40–42 Moreover, it might activate the more rational route of thinking according to Nelson’s model.43
Thus, if our hypothesis of 2 different causal attribution processes, a rational and an intuitive process is correct and the IPSAQ-R activates a more rational process, the assessment with the IPSAQ-R sheds light on the presence of a self-blaming AS for negative events in patients with schizophrenia/persecutory delusions. Moreover, we assessed a population of psychological help seekers who might present a pronounced level of insight that is often linked to depression and self-stigmatization.44,45 Thus, these patients might truly blame mostly themselves for negative life events.
Nevertheless, a second subgroup of patients could be identified by cluster analysis. These patients presented a more pronounced PB and more severe persecutory delusions. Moreover, multivariate regression analysis indicated that patients who presented a PB and depression are more likely to show more severe persecutory delusions as well. On the one hand, the IPSAQ-R might not trigger a more rational attribution process in all patients, thus, a small subgroup performed causal attributions in a more intuitive way and presented a pronounced PB. On the other hand, these patients might correctly assume that other persons are often responsible for negative events in their life and feel depressed as a consequence. Given the less supportive social network of patients with schizophrenia,46 this assumption might be plausible.
If our hypothesis of 2 different attribution processes , a more intuitive and a more rational process, is correct, AS should not be viewed as a stable trait but as depending on individual and situational characteristics that might activate either a more intuitive or a more rational attribution process. This assumption fits well with the finding of an increased PB in patients with schizophrenia after induction of social stress. In order to test our hypothesis further, experimental studies are highly necessary in order to elucidate individual and situational conditions that might activate different attribution processes (eg, negative emotions, interpersonal threat).
At present, theoretical models of CBTp assume an important role of AS in the formation and maintenance of persecutory delusions15 and positive symptoms of schizophrenia.13,14 In light of our results, it might not be an exaggerated AS that enhances patients’ personal risk, but a more pronounced individual susceptibility toward situational characteristics that activate a more intuitive attribution process. With regard to CBTp, our study brings forward the positive message that patients with schizophrenia are able to adapt their attributions to the present situation. Thus, they might be able to learn strategies in order to activate more rational attribution processes in difficult social situations as well.
In interpreting the findings of our study, some limitations should be considered. The IPSAQ-R is a new assessment that has not been investigated with regard to its reliability and validity in a large sample of controls. Moreover, the mode of assessment that forces persons to perform percentage estimations could be criticized. But as discussed above, while not ideal, the IPSAQ-R presents several advantages in comparison to the classic IPSAQ: Patients are not required to decide between different attributional loci; thus, reliability indices are quite sufficient, and assessment of AS might be more accurate as it activates more rational attribution processes. Furthermore, although our control group is quite small, we carefully checked for violation of assumptions for statistical analyses. Investigation of monocausality bias revealed no significant differences between patients with schizophrenia and controls and between patients with persecutory delusions and controls. However, it should be noted that patients with schizophrenia presented a more pronounced monocausality bias, if intelligence was not controlled. Moreover, if a higher treshold (90%) was used to assess monocausality, patients with schizophrenia (P = .015) and patients with persecutory delusions presented a more monocausal attribution style in parametric tests (P = .003), if intelligence was not controlled. These results suggest that general intelligence helps to reach a balanced interpretation of reality. Finally, although regression analysis seems to imply that PB is causal to delusions of persecution or involved in their etiology, it must be noted that all analyses are based on cross-sectional associations. Hence, it can be assumed that a PB could follow from delusions of persecution or merely be an attribute of them as well.
Several important conclusions can be drawn from our results. In comparison to controls, patients with schizophrenia in general and patients with persecutory delusions in particular showed a “self-blaming” AS for negative events. Nevertheless, a subgroup of patients could be identified who presented a more pronounced PB and more severe persecutory delusions as well. Thus, AS in patients with schizophrenia might be less stable but more determined by individual and situational characteristics that need further elucidation.
Funding
German Federal Ministry of Education and Research (BMBF: 01GV0618, 01GV0620).
Acknowledgments
We thank all members of the POSITIVE study: S. Baal, J. Berning, S. Beulen, G. Buchkremer, A. Büch, B. Conradt, Y. Eikenbusch, W. Gaebel, A. Gawronski, J. Güttgermans, A. Herold, U. Jakobi-Malterre, I.. Lengsfeld, W. Maier, K. Platt, B. Pohlmann, A. Rotarska-Jagiela, S. Sickinger, H. Smoltczyk, S. Unsöld, A. Vogeley, A. Witt, and L. Zipp. The study was part of the BMBF research program “Research Networks on Psychotherapy.” The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Heider F. The Psychology of Interpersonal Relations. New York, NY: Wiley; 1958:162 [Google Scholar]
- 2. Kelley HH. Attribution theory in social psychology. In: Levin D, ed. Nebraska Symposium on Motivation. Vol 15 Lincoln, NE: University of Nebraska Press; 1967:192–240 [Google Scholar]
- 3. Peterson C, Semmel A, Von Baeyer C, et al. The attributional style questionnaire. Cogn Ther Res. 1992;3:287−–300 [Google Scholar]
- 4. Kaney S, Bentall RP. Persecutory delusions and attributional style. Br J Med Psychol. 1989;62(Pt 2):191–198 [DOI] [PubMed] [Google Scholar]
- 5. Janssen I, Versmissen D, Campo JA, Myin-Germeys I, van Os J, Krabbendam L. Attribution style and psychosis: evidence for an externalizing bias in patients but not in individuals at high risk. Psychol Med. 2006;36:771–778 [DOI] [PubMed] [Google Scholar]
- 6. Lyon HM, Kaney S, Bentall RP. The defensive function of persecutory delusions. Evidence from attribution tasks. Br J Psychiatry. 1994;164:637–646 [DOI] [PubMed] [Google Scholar]
- 7. Kinderman P, Bentall RP. A new measure of causal locus: The Internal, Personal and Situational Attributions Questionnaire. Pers Indiv Differ. 1996;20:261–264 [Google Scholar]
- 8. Kinderman P, Bentall RP. Self-discrepancies and persecutory delusions: evidence for a model of paranoid ideation. J Abnorm Psychol. 1996;105:106–113 [DOI] [PubMed] [Google Scholar]
- 9. Diez-Alegría C, Vázquez C, Nieto-Moreno M, Valiente C, Fuentenebro F. Personalizing and externalizing biases in deluded and depressed patients: are attributional biases a stable and specific characteristic of delusions? Br J Clin Psychol. 2006;45:531–544 [DOI] [PubMed] [Google Scholar]
- 10. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347 [DOI] [PubMed] [Google Scholar]
- 11. Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192 [DOI] [PubMed] [Google Scholar]
- 12. Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27:425–457 [DOI] [PubMed] [Google Scholar]
- 13. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195 [DOI] [PubMed] [Google Scholar]
- 14. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391 [DOI] [PubMed] [Google Scholar]
- 15. Bentall RP, Fernyhough C. Social predictors of psychotic experiences: specificity and psychological mechanisms. Periodical. 2008;34:1012–1020. 10.1093/schbul/sbn103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Randall F, Corcoran R, Day JC, Bentall RP. Attention, theory of mind, and causal attributions in people with persecutory delusions: A preliminary investigation. Cogn Neuropsychiatry. 2003;8:287–294 [DOI] [PubMed] [Google Scholar]
- 17. McKay R, Langdon R, Coltheart M. Paranoia, persecutory delusions and attributional biases. Psychiatry Res. 2005;136:233–245 [DOI] [PubMed] [Google Scholar]
- 18. Martin JA, Penn DL. Attributional style in schizophrenia: an investigation in outpatients with and without persecutory delusions. Schizophr Bull. 2002;28:131–141 [DOI] [PubMed] [Google Scholar]
- 19. Wittorf A, Giel KE, Hautzinger M, et al. Specificity of jumping to conclusions and attributional biases: a comparison between patients with schizophrenia, depression, and anorexia nervosa. Cogn Neuropsychiatry. 2012;17:262–286 [DOI] [PubMed] [Google Scholar]
- 20. Mehl S, Rief W, Lüllmann E, Ziegler M, Kesting ML, Lincoln TM. Are theory of mind deficits in understanding intentions of others associated with persecutory delusions? J Nerv Ment Dis. 2010;198:516–519 [DOI] [PubMed] [Google Scholar]
- 21. Mehl S, Rief W, Lüllmann E, Ziegler M, Müller MJ, Lincoln TM. Implicit attributional style revisited: evidence for a state-specific “self-decreasing” implicit attributional style in patients with persecutory delusions. Cogn Neuropsychiatry. 2010;15:451–476 [DOI] [PubMed] [Google Scholar]
- 22. Langdon R, Ward PB, Coltheart M. Reasoning anomalies associated with delusions in schizophrenia. Schizophr Bull. 2010;36:321–330. 310.1093/schbul/sbn1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Donohoe G, Spoletini I, McGlade N, et al. Are relational style and neuropsychological performance predictors of social attributions in chronic schizophrenia? Psychiatry Res. 2008;161:19–27 [DOI] [PubMed] [Google Scholar]
- 24. Savla GN, Vella L, Armstrong CC, Penn DL, Twamley EW. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical evidence. Schizophr Bull. 2013;39:979–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Button KS, Ioannidis JP, Mokrysz C, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–376 [DOI] [PubMed] [Google Scholar]
- 26. Randjibar S, Veckenstedt R, Vitzthum F, Hottenrott B, Moritz S. Further evidence for a decreased sense of self-causation in paranoia. Psychosis. 2010;3:74–85 [Google Scholar]
- 27. Huq SF, Garety PA, Hemsley DR. Probabilistic judgements in deluded and non-deluded subjects. Q J Exp Psychol A. 1988;40:801–812 [DOI] [PubMed] [Google Scholar]
- 28. Fine C, Gardner M, Craigie J, Gold I. Hopping, skipping or jumping to conclusions? Clarifying the role of the JTC bias in delusions. Cogn Neuropsychiatry. 2007;12:46–77 [DOI] [PubMed] [Google Scholar]
- 29. Moritz S, Burnette P, Sperber S, et al. Elucidating the black box from stress to paranoia. Schizophr Bull. 2011;37:1311–1317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Moritz S, Schilling L, Wingenfeld K, et al. Psychotic-like cognitive biases in borderline personality disorder. J Behav Ther Exp Psychiatry. 2011;42:349–354 [DOI] [PubMed] [Google Scholar]
- 31. Klingberg S, Wittorf A, Meisner C, et al. Cognitive behavioural therapy versus supportive therapy for persistent positive symptoms in psychotic disorders: the POSITIVE Study, a multicenter, prospective, single-blind, randomised controlled clinical trial. Trials. 2010;11:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wittchen HU, Wunderlich U, Gruschwitz S, Zaudig M. Strukturiertes Klinisches Interview fuer DSM-VI (SKID). Göttingen, Germany: Hogrefe; 1997 [Google Scholar]
- 33. APA. Diagnostic and Statistical Manual of Mental Disorders, Text Revision. 4th ed. 2004 [Google Scholar]
- 34. Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS). New York: Multi Health Systems Inc; 1992 [Google Scholar]
- 35. Lehrl S. Mehrfachwahl-Wortschatz-Intelligenztest MWT-B. Fünfte unveränderte Auflage. Balingen, Germany: Spitta Verlag; 2005 [Google Scholar]
- 36. Mueller MJ, Marx-Dannigkeit P, Schlösser R, et al. The Calgary Depression Rating scale for schizophrenia: development and interrater reliability of a German version (CDSS-G). J Psychiatr Res. 1999;10:799–812 [DOI] [PubMed] [Google Scholar]
- 37. Finch H. Comparison of the Performance of Nonparametric and Parametric MANOVA test statistics when assumptions are violated. Methodology. 2005;1:27–38 [Google Scholar]
- 38. Bortz J, Schuster C. Statistik für Sozialwissenschaftler. Berlin, Germany: Springer; 2010 [Google Scholar]
- 39. Cooper C, Morgan C, Byrne M, et al. Perceptions of disadvantage, ethnicity and psychosis. Br J Psychiatry. 2008;192:185–190 [DOI] [PubMed] [Google Scholar]
- 40. Kahneman D, Frederick S. Representativeness revisited: attribute substitution in intuitive judgement. In: Gilovich T, Griffin D, Kahneman D, eds. Heuristics and Biases: The Psychology of Intuitive Judgement. Cambridge, UK: Cambridge University Press; 2002:49–81 [Google Scholar]
- 41. Kahneman D, Frederick S. A model of heuristic judgement. In: Holyoak K, Morrison RG, eds. The Cambridge Handbook of Thinking and Reasoning. Cambridge, UK: Cambridge University Press; 2005:267–294 [Google Scholar]
- 42. Evans JS. Dual-processing accounts of reasoning, judgment, and social cognition. Annu Rev Psychol. 2008;59:255–278 [DOI] [PubMed] [Google Scholar]
- 43. Nelson HE. Cognitive-Behavioural Therapy with Delusions and Hallucinations. Cheltenham, UK: Nelson Thornes; 2005 [Google Scholar]
- 44. Lincoln TM, Lüllmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull. 2007;33:1324–1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Staring APB, Van der Gaag M, Van den Berge M, Duivenvoorden HJ, Mulder CL. Stigma moderates the associations of insight with depressed mood, low self-esteem, and low quality of life in patients with schizophrenia spectrum disorders. Schizophr Res. 2009;115:363–369 [DOI] [PubMed] [Google Scholar]
- 46. Gregory HN, Ponzoha CA, Cutler DL, Weigel RM. Social networks and negative versus positive symptoms of schizophrenia. Schizophr Bull. 1989;15:625–633 [DOI] [PubMed] [Google Scholar]