Abstract
Objective
Studies examining the association between prenatal cocaine exposure (PCE) and child behavior problems have yielded mixed results, suggesting a need to identify additional mediating and moderating influences. We hypothesized that the relation between PCE and behavior problems at kindergarten would be mediated/moderated by child exposure to violence; and that maternal warmth/sensitivity and harshness would moderate the association between violence exposure and behavior problems.
Methods
Participants consisted of 216 (116 cocaine-exposed, 100 non-cocaine exposed (NCE) mother-child dyads participating in an ongoing longitudinal study of PCE.
Results
Results yielded no direct or mediated/moderated association between PCE and child behavior problems, and no significant interaction effects between PCE and parenting quality. However, higher exposure to violence in kindergarten was significantly associated with higher child behavior problems. This association was moderated by maternal warmth/sensitivity and harshness. High maternal warmth/sensitivity buffered the association between violence exposure and behavior problems while high maternal harshness exacerbated this association.
Conclusion
This study highlights the role of violence exposure in the development of behavior problems among high-risk children, and emphasizes the significance of parenting quality in buffering or exacerbating this risk among these children. Implications for prevention include targeting the potential role of maternal warmth/sensitivity as a protective influence among children exposed to violence.
Keywords: community and family violence, cocaine exposure, child, behavior problems, parenting
Multiple risk and protective factors may influence the emergence of externalizing behavior problems. One possible developmental influence is prenatal exposure to substances such as cocaine (PCE). Children prenatally exposed to cocaine are at a greater risk for behavior problems due to the impact of cocaine on brain regions involved in regulation of affect and behavior (Li et al., 2011; Lester et al., 2009). However, results from existing research have been mixed with some studies indicating no associations between PCE and externalizing problems (Accornero, Morrow, Bandstra, Johnson, & Anthony, 2002; Warner et al., 2006), others indicating significant direct associations (Bada et al., 2007; Lester et al., 2009), and yet others indicating associations mediated or moderated by other variables (Bailey et al., 2005; Delaney-Black et al., 2004), or predicted by environmental factors. In one of the few prospective analyses of behavior problems in cocaine-exposed children, Bada et al. (2007) found higher PCE was associated with higher behavior problems compared to some or no cocaine exposure with consistent effects from 7 to 11 years. These results indicated a dose-response relationship between exposure and a higher trajectory of behavior problems. In addition, community violence was a significant predictor of parent reported behavior problems. Contrary to these findings, Accornero and colleagues (2002) found that recent caregiver drug use and psychological symptoms, not PCE, were predictors of behavior problems among PCE children. There may be several reasons for these differences in findings. These include variations in timing, dose of exposure, sampling, and sample sizes across studies, the extent of comorbidity with other substances (i.e., alcohol, cigarettes, and marijuana), and the possibility that associations between PCE and behavior problems may occur through indirect pathways or due to the role of moderating variables.
Exposure to Violence as Mediator/Moderator
In addition to the potential for direct associations, PCE may be indirectly associated with higher child behavior problems via children’s exposure to violence. Large numbers of young children from high-risk neighborhoods common to drug using parents are exposed to violence. Among children 5 years of age and younger, 10% had witnessed a knifing or shooting, 18% had witnessed shoving, kicking, or punching, and 47% had heard gunshots (Taylor, Zuckerman, Harik, & McAlister, 1994). Both victimization and indirect exposure such as witnessing violent acts may have harmful effects on young children’s development (Shahinfar et al., 2000), especially when combined with the biological vulnerability posed by PCE. Indeed, studies have indicated that environmental risk in general and exposure to violence in particular may play a critical role in predicting behavior problems among substance exposed children (Bada et al., 2011; Bennett, Bendersky, & Lewis, 2007; Singer et al., 2004; Yumoto, Jacobson & Jacobson, 2008). However, given variations in caregiving situations of PCE children with significant numbers residing with foster parents or relatives, not all may experience high levels of violence. Thus, we hypothesized that exposure to violence may be an important mediator or moderator of the association between PCE and child behavior problems.
Parenting Quality as a Moderator
The potential effects of biological or environmental risk on child adjustment may be moderated by proximal caregiving experiences within the family (Lynch, 2006). In one of the few studies of the potential moderating role of parenting among substance exposed children, Wakschlag and Hans (2002) reported significant moderation by parenting in infancy on the association between prenatal cigarette exposure and conduct disorder at 10 years of age for boys. Results indicated that the association between cigarette exposure and conduct disorder was significant only when children experienced maternal unresponsiveness in infancy. These results were supportive of theoretical models suggesting that the effects of biological vulnerability may be moderated by quality of parenting in early childhood (Mayes & Bornstein, 1997). Similarly, the important role of parenting quality in potentially moderating the effects of environmental risk such as problematic neighborhood characteristics has been long recognized (Duncan, Connell, & Klebanov, 1997). For instance, in a study of adolescents, Salzinger et al. (2011) reported that among children experiencing high levels of community violence, positive attachment to parents was associated with lower behavior problems, thus having a protective effect. Several studies reported that parental warmth, praise, and low derogation in parenting buffer young children exposed to high family conflict from negative outcomes on emotional regulation and behavior problems (e.g., Katz & Gottman, 1997). However, the role of maternal warm/sensitive parenting (marked by high levels of warmth, positive affect, connectedness, and sensitivity to child cues during interactions) in the context of high levels of violence exposure or prenatal cocaine exposure has seldom been examined at younger ages. In addition to maternal warmth/sensitivity, harsh parenting (marked by high verbal or physical threats and negative affect) may exacerbate the association between prenatal cocaine or to violence exposure and child behavior problems. This is supported by evidence from interventions designed to reduce behavior problems among children exposed to violence indicating that decreases in harsh maternal parenting accounted for significant decreases in children’s behavior problems (Jouriles et al., 2009; McCart, Priester, Davies, & Azen, 2006).
Purpose of the Current Study
The current study is guided by ecological models that highlight the role of interacting risk and protective factors within different systems such as individual, family, community, and the larger society (Bronfenbrenner, 1979). Thus, biological vulnerability due to prenatal substance exposure may be associated with child adjustment via variables such as exposure to community and family violence or be exacerbated by exposure to violence. However, proximal family influences such as the experience of maternal warmth/sensitivity may act as a protective influence (Luthar & Cicchetti, 2000) and lead to resilience as defined by low behavior problems in the context of high risk due to exposure to PCE or community and family violence. In contrast, the experience of maternal harshness may exacerbate the potential influence of PCE or community and family violence on children’s adjustment. Thus, we hypothesized that (1) cocaine exposed children would exhibit higher behavior problems in kindergarten; (2) this association would be mediated/moderated by child exposure to violence; and (3) maternal warmth/sensitivity and harshness would moderate the association between PCE/violence exposure and child behavior problems. More specifically, we hypothesized that maternal warmth/sensitivity would serve as a protective factor, such that among PCE children or those with high violence exposure, high maternal warmth/sensitivity would be associated with lower behavior problems compared to those with low maternal warmth/sensitivity. We expected maternal harshness to exacerbate risk such that among PCE children or those with high violence exposure, high maternal harshness would be associated with higher behavior problems compared to low maternal harshness.
Finally, it is important to note that maternal cocaine use is a polydrug issue. The majority of mothers using cocaine also use other substances such as alcohol, cigarettes, and marijuana (Lester et al., 2003). All of these substances have the potential to alter developmental outcomes (see Irner, 2012, review). Thus, the potential effects of cocaine use can only be examined in the context of other substance use during pregnancy. Given that the majority of mothers using cocaine also use other substances such as alcohol, marijuana, and cigarettes, prenatal exposure to these substances were used as covariates in analyses examining direct and indirect associations between PCE and behavior problems.
Methods
The sample consisted of 216 mother-child dyads participating in an ongoing longitudinal study of PCE, (116 PCE, 100 NCE). Of the 216 children, 106 (49%) were male. Participants were recruited after delivery from two local area hospitals. Mothers ranged in age from 18 to 42 years (M =29.78, SD =5.46). The majority of the mothers were African American (74%), were receiving Temporary Assistance for Needy Families (71%) at the time of their first laboratory visit and were single (60%). Once a family was recruited into the cocaine group, the closest matching comparison family was recruited matched on maternal education, maternal race/ethnicity, and infant gender (see Eiden et al., 2011 for sampling details).
Procedure
Mother-child dyads were assessed 4-8 weeks, 7, 13, 24, 36 months and 5 years old (kindergarten assessment). All visits consisted of a combination of maternal interviews, observations of mother-child interactions, and child assessments. With regard to change in custody arrangements, the legal guardian of the child was contacted and asked to participate. In these circumstances, biological mothers were interviewed in addition to the foster mother at the first assessment in order to obtain accurate information about prenatal substance use.
Identification of Substance Use
Cocaine status was determined by a combination of maternal report, chart review, maternal hair and urine analysis. Mothers were included in the cocaine group if self-reports, urine toxicology or hair sample results were positive. Mothers were included in the control group if they did not test positive on urine or hair, and denied using cocaine during pregnancy based on self-report. Exclusion criteria included mothers who had other major confounding conditions including diagnosed psychiatric disorder, used illicit substances other than cocaine or marijuana, age < 18, positive for HIV status, or children with fetal alcohol syndrome or other serious birth defects.
Urine toxicology consisted of standard urine screening for drug level or metabolites of cocaine, opiates, benzodiazepines, and tetrahydrocannabinol. Urine was rated positive if the quantity of drug or metabolite was >300g/ml. Urine toxicology results were available for 90% of the families in the control group and 92% of the families in the cocaine group. Hair samples were collected from the mothers at the first laboratory visit and sent to Psychemedics Corporation for Radioimmunoanalyses (RIAH), which is the most well established hair analysis technique (see Magura, Freeman, Siddiqi, & Lipton, 1992). Hair samples were screened for cocaine followed by gas chromatography/mass spectrometry confirmations for positive cocaine screens. About 98% of the mothers in the cocaine group had positive hair sample results, and 2% of mothers admitted having used cocaine in the brief self-report screening instrument administered after delivery, but did not have positive hair results. Mothers in the comparison group reported not having used any illicit substances other than marijuana and did not test positive for cocaine in hair results.
The Timeline Follow-Back Interview (TLFB; Sobell, Sobell, Klajmer, Pavan, & Basian, 1986) was used to assess maternal substance use during pregnancy and postnatally. The TLFB yields data about the average number of joints smoked per week, average number of cigarettes smoked per week, and average number of standard drinks per week during pregnancy. Postnatal substance use was an average across 6 postpartum phases (1, 7, 13, 24, 36, and Kindergarten), as such the average number of days used cocaine, number of cigarettes per week, number of standard drinks per week, and number of joints per week across the six time points were used in final analyses. Composites across phases were calculated as variables reflecting cumulative exposure across early childhood were considered a conceptually stronger predictor of child outcomes given that there was no conceptual rationale for hypothesizing that postnatal exposure at any particular age would be more strongly associated with outcomes. Moreover, the stability for some postnatal exposure variables such as cigarettes and cocaine across adjacent time points were quite high ranging from .73 to .86 for cigarettes and from .70 to .90 for cocaine. The stability for marijuana and alcohol was lower. However, all these variables within each time point were extremely skewed and kurtotic. A composite measure over time had better distribution and was transformed using square root transformations before being used in analysis. Thus, the cumulative measure was conceptually and statistically better justified than exposure at particular time points.
Maternal Warmth/Sensitivity and Harshness
Maternal warmth/sensitivity was assessed using behavioral observations during a free-play task during infant-toddler period (e.g. 7, 13, and 24 months). Mothers were asked to interact with their infants as they normally would at home for 10 minutes in a room filled with toys. These interactions were coded using a collection of global 5-point rating scales developed by Clark, Musick, Scott, and Klehr (1980), with higher scores indicating more positive affect or behavior. The scale for maternal warmth/sensitivity consisted of items such as warm tone of voice, expressed positive affect, enthusiastic, cheerful mood, and connectedness with the child. Maternal warmth/sensitivity across the three assessment points was significantly correlated with correlations ranging from r = .22 to r = .32, p < .01. The final variable for maternal sensitivity measure consisted of the averages across the three time points, with higher scores indicating more positive affect or behavior. This composite scale had high internal consistency (Cronbach’s α = .90).
As children move into early childhood, testing of limits emerges which elicits maternal discipline and directives. Consequently, maternal harshness was assessed during a variety of tasks at 24 and 36 months of age. Maternal harshness was coded during specific segments of the 24 and 36-month observational assessments. These included a 10-minute mother-child free play paradigm, 10-minute clean up, 8-minute structured play, 10-minute snack, and 5-minute emotion regulation paradigm. Harshness was coded using codes developed in previous studies (Cummings et al., 1989; Keenan and Shaw, 1994). This included physical harshness (hitting, threatening bodily gestures, grabbing and pushing) directed toward a person, toward an object (e.g., hard banging and throwing toys); or verbal harshness that consisted of and threats (angry tone, yelling, verbal attacks, or threats of harm). Event coding of each episode was triggered by the mother or the child displaying of any of these behaviors. The final variable for maternal harshness consisted of the average intensity of overall harshness across 24 and 36 months, with higher scores indicating higher intensity of harshness. The correlation between maternal harshness variables at 24 and 36 months was r = .48, p < .01.
Inter-rater reliability for maternal harshness was conducted on a random selection of tapes at 24 (n = 32) and 36 months (n = 20). Inter-rater reliability on average intensity of maternal harshness was high (Intra-class correlation coefficient of .87 at 36 months to .91 at 24 months). Similarly, inter-rater reliability for maternal warmth/sensitivity was conducted on a random selection of tapes at 7 (n = 23), 13 (n = 15) and 24 months (n = 17). Inter-rater reliability on maternal sensitivity at each age was high (Intra-class coefficient of .99 at 7 months, .83 at 13 months, and .98 at 24 months).
Child Behavior Problem
The Child Behavior Checklist (CBCL; Achenbach, 2000) was used as a measure of child behavioral/emotional problems. Maternal reports were obtained during kindergarten assessment using the 1.5 – 5 year version of the CBCL. Raw scores were used and behavior ratings yield both internalizing and externalizing behavior problems as well as a total score. Higher scores indicate more behavior problems. The correlation between internalizing and externalizing subscales was r = .70. Thus, the total child behavior problems score was used as the dependent measure in the model testing. The internal consistency reliability Cronbach’s α =.92 for total behavior problems on the CBCL.
Child Exposure to Violence
Mothers completed the Survey of Exposure to Community Violence (Richters & Saltzman, 1990) for their children during the kindergarten assessment. The measure evaluated child exposure to severe violence (e.g., shooting and rape), moderately severe violence (e.g., threats and drug deals), and less severe violence (e.g., beating and chasing). For each violent event, mothers reported “true” or “false” if their child had witnessed (19 items; e.g., “seen someone getting beaten up”) or been the victim (7 items; e.g., “child has been threatened with serious physical harm by someone”) of a violent act. The sum of all items was computed. Approximately 33% of the children in this sample experienced some level of violence exposure. However, this continuous measure was extremely skewed and kurtotic with a large number (67%) of mothers reporting no violence exposure for their children. Thus, this measure was dichotomized (no vs. some violence exposure). The internal consistency reliability Cronbach’s α = .83 for maternal report of child exposure to community violence.
Previous studies of young children indicate that they are likely to witness violent events experienced by their mothers because of the likelihood of close proximity to the mother (e.g., Linares et al., 2001). Thus, young children’s exposure to violence may be closely associated with maternal exposure to violence. Thus, maternal exposure to violence was assessed using the TLFB (Sobell & Sobell, 1996) and the Conflict Tactics Scale (CTS, Straus, 1979). The TLFB has been used to measure episodes of intimate partner violence and other exposure to violence in various studies (e.g., Mignone, Klostermann, & Chen, 2009). The total number of days women reported witnessing, experiencing, or perpetrating violence was summed. Given the apparent bimodal distribution with only 7% of women reporting any violent event the variable was dummy-coded (i.e., 0, 1). Maternal experience of physical aggression from their intimate partners was assessed using maternal reports on the CTS for women with intimate partners (n = 117). The prevalence of physical violence was summed to create a composite measure of maternal experience of physical violence from their partners. This measure was quite skewed and kurtotic and was dummy coded. About 30% of mothers reported intimate partner violence on the CTS. Maternal reports of child exposure to violence and/or own exposure to violence based on the TLFB and CTS were combined into a single composite dummy coded measure reflecting no vs. any experience of violence by mothers or children. In this sample, 36% of the children experienced violence based on this final composite measure.
Data Analytic Strategy
ANOVAs were used to examine group differences (cocaine vs. control) in demographics, perinatal risk characteristics, maternal substance use variables, child exposure to violence, and child behavior problems at kindergarten age and to guide the selection of potential covariates. Demographic or perinatal risk variables that were associated with both the predictors and outcomes at p < .10 were used as covariates in subsequent analyses. To test the primary hypotheses, Hierarchical Linear Regression was used to examine the association between child exposure to community violence and child behavior problems, as well as the hypotheses that maternal warmth/sensitivity may buffer, while maternal harshness may exacerbate this relationship.
Missing Data
As with any longitudinal study, there were incomplete data for some of the participants at one or more of the several assessment points included in this study. Of the 216 mother-child dyads who completed the 4-week laboratory visit, 189 completed the 7-month assessment, 177 completed the 24-month assessment, 165 completed the 36-month assessment, and 164 completed the kindergarten age assessment. There were no significant differences between families with complete vs. missing at any age until the kindergarten assessment. Families with missing data at kindergarten had lower maternal education, F (1, 213) = 4.82, p < .05 (M = 11.89 and 11.26 for those with complete vs. missing data respectively, SD = 1.73 and 2.06). Mothers with missing data at the kindergarten assessment also were more likely to smoke marijuana in pregnancy compared to those with complete data, F (1, 213) = 5.24, p < .05 (M = .87 and 3.01 joints/week for those with complete and missing data respectively, SD = 4.50 and 8.82). There was no association between cocaine group status and attrition. Approximately, 25% of participants in the control group had missing data in kindergarten compared to 23% in the cocaine group. Finally, 36.5% of children with missing data at kindergarten were in foster care compared to 22% of those with complete data, Pearson χ2 = 4.02, p < .05. Data were thus determined to fit criteria for missing at random (MAR). We used model based multiple imputation methods to iteratively estimate values for missing data based on non-missing data given the specified model (Schafer & Graham, 2002; Jansen & Oud, 1995; Royston, 2005). This strategy has the net effect of minimally altering effects that involve variables on which there are missing data, and more importantly, keeping the maximum number of participants in the analysis for effects that involve variables on which there are no missing data. Prenatal and postnatal substance exposure variables, demographic covariates, child exposure to violence, maternal warmth and sensitivity, and the centered product terms for the hypothesized interaction effects were included as variables for model based imputation. We used SAS PROC MI (SAS, 1999) to impute missing data and create 5 data sets. We then fitted each regression model to the 5 imputed data sets and pooled the parameter estimates and standard errors using SAS PROC MIANALYZE.
Results
Demographics and Perinatal Risk: Analyses for Potential Covariates
Results from ANOVA with the demographic variables as the dependent measures and cocaine status indicated that control group mothers were younger, had lower parity (number of children), and higher occupational status compared to those in the cocaine group (see Table 1). Correlational analyses with these demographic variables and child behavior problems indicated that higher parity was associated with lower child behavior problems (r = -.15, p < .05). Thus, parity was included as a covariate in model testing. ANOVA with child gender as the independent variable and child behavior problems as the dependent variable indicated no gender difference in behavior problems. Child age in kindergarten was not associated with behavior problems.
Table 1.
Group Differences in Study Variables
| Exposure Group | Non-Cocaine | Cocaine | F-value | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Demographics | |||||
| BM age | 27.7 | 5.6 | 31.0 | 6.0 | 16.5** |
| BM parity | 3.2 | 1.6 | 4.2 | 2.4 | 12.02** |
| Years education | 12.0 | 1.9 | 11.6 | 1.9 | 2.12 |
| Maternal Occupational Status |
3.4 | 1.8 | 2.8 | 1.3 | 7.9** |
| Prenatal Substance Use | |||||
| Cigarettes/week | 12.9 | 25.8 | 37.2 | 43.7 | 23.6** |
| Drinks/week | 0.2 | 0.8 | 3.8 | 11.4 | 9.9** |
| Joints/week | 1.5 | 7.4 | 1.3 | 4.2 | 0.04 |
| Days cocaine/week | 0 | 0 | 0.9 | 1.6 | |
| Postnatal Substance Use | |||||
| Cigarettes/week | 14.6 | 28.9 | 26.6 | 36.6 | 7.1** |
| Drinks/week | 0.4 | 0.9 | 1.9 | 4.0 | 3.8* |
| Joints/week | 0.6 | 2.3 | 1.3 | 5.5 | 1.1 |
| Days cocaine/week | 0 | 0 | 0.1 | 0.2 | |
| Postnatal Outcomes | |||||
| % Exposed to Violence | 32 | 39 | |||
| Maternal Sensitivity | 3.8 | 0.6 | 3.7 | 0.7 | 1.8 |
| Maternal Harshness | 1.4 | 0.9 | 1.7 | 1.2 | 3.9* |
| Child Behavior Problems | 27.3 | 22.6 | 27.0 | 23.9 | 0.2 |
Note. BM = biological mother; Maternal Occupational status was measured using the Hollingshead Occupational Scale (Hollingshead, 1975); Child Behavior Problems were the raw scores obtained from the CBCL.
p<.05.
p<.01
Maternal Substance Use and Foster Care Status
Results from ANOVA with prenatal substance use variables as the dependent measures and group status as the independent variable were as expected. Mothers in the cocaine group were heavier users of cigarettes and alcohol, during pregnancy (see Table 1). There was no group difference in marijuana use. These results remained unchanged when the 56 foster care mothers were excluded from analyses. ANOVA with foster care status as the independent variable and child behavior problems as the dependent variable indicated no significant effect of foster care status on child behavior problems. There were no significant differences on maternal warmth/sensitivity and harshness or on child exposure to violence as a function of foster care status.
Associations between Maternal Substance Use and Child Behavior Problems
ANCOVA with parity, number of drinks per week during pregnancy, and number of cigarettes smoked per week during pregnancy, and number of joints per week in pregnancy as covariates, cocaine group status as the independent variable, and child behavior problems as the dependent measure indicated no significant group differences in child behavior problems. Next, we examined if there was an indirect association via exposure to violence. Chi-square analysis yielded no significant association between cocaine group status and exposure to violence. Approximately 39% of mothers in the PCE group reported child or maternal exposure to violence compared to 36% of mothers in the NCE group. Thus, no further analyses were conducted to examine if there was an indirect association between PCE and behavior problems via exposure to violence. Although PCE was not associated with violence exposure, higher exposure to violence was associated with higher behavior problems. Correlational analyses (see Table 2) indicated that at the bivariate level, higher maternal postnatal cigarette, alcohol, and marijuana use were associated with higher child behavior problems in kindergarten.
Table 2.
Correlations Among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parity | ||||||||||||
| 2. #Drinks/Week Preg. | .06 | |||||||||||
| 3. #Joints/Week Preg. | .01 | .01 | ||||||||||
| 4. #Cigarettes/Week Preg. | .11 | .34 | .01 | |||||||||
| 5. Cocaine Group Status | .23 | 21 | −.02 | .32 | ||||||||
| 6. #Drinks/Week Postnatal | −.03 | .12 | .01 | .12 | .08 | |||||||
| 7. #Joints/Week Postnatal | −.05 | .01 | .27 | .03 | .00 | .32 | ||||||
| 8. #Cigs/Week Postnatal | .07 | .15 | .01 | .63 | .24 | .18 | .19 | |||||
| 9. # Days Used Cocaine Postnatal |
.00 | .36 | .02 | .16 | .28 | .29 | .10 | .18 | ||||
| 10. Child Exposure to Violence |
.02 | .00 | .05 | .03 | −.02 | .22 | .05 | .02 | .12 | |||
| 11. Maternal Sensitivity | −.01 | −.12 | −.03 | −.06 | −.09 | .06 | −.01 | −.18 | −.06 | − .12 | ||
| 12. Maternal Harshness | −.07 | .09 | .03 | .15 | .12 | .05 | .19 | .25 | .13 | .11 | − .35 | |
| 13. Child Behavior Problems |
− .16 | −.03 | −.04 | .15 | .02 | .20 | .22 | .25 | .04 | .30 | −.18 | .26 |
Note. # = number; Preg = pregnancy.
p<.05 in bold face.
Moderation by Maternal Warmth/Sensitivity and Harshness
Two separate regression models were used to test the hypotheses that maternal warmth/sensitivity and/or maternal harshness may moderate the association between PCE and behavior problems. Parity was entered in the first step as a control variable, followed by prenatal substance exposure variables (number of drinks/week, number of cigarettes/week, number of joints/week, cocaine group status) in step 2, postnatal substance exposure variables, exposure to violence, and maternal warmth/sensitivity or harshness in step 3, and the product term of PCE and maternal warmth/sensitivity or harshness in step 4. Among first order effects, parity and exposure to violence were significantly associated with child behavior problems (see Table 3). Lower parity and higher exposure to violence were associated with higher child behavior problems. However, there were no significant interaction effects between PCE and parenting quality.
Table 3.
Regression Analysis: DV: Child Behavior Problems
| Maternal Sensitivity | Maternal Harshness | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Coefficient | SE | tvalue | Coefficient | SE | tvalue | |
| Parity | −3.94* | 1.46 | −2.69 | −4.75* | 1.46 | −3.26 |
| Prenatal Substance Use: | ||||||
| Number of Drinks/Week | −0.11 | 1.74 | − 0.06 | −0.50 | 1.65 | −0.30 |
| Number of Joints/Week | −2.93 | 1.95 | −1.51 | −1.32 | 1.70 | −0.78 |
| Number of Cigs/Week | −0.91 | 2.32 | −0.39 | 0.46 | 1.93 | 0.24 |
| Cocaine Group Status | 1.28 | 3.73 | 0.34 | 0.74 | 4.07 | 0.18 |
| Postnatal Substance Use: | ||||||
| Number of Drinks/Week | 1.92 | 1.49 | 1.28 | 0.74 | 1.55 | 0.48 |
| Number of Joints/Week | 3.51 | 2.68 | 1.31 | 1.75 | 2.79 | 0.63 |
| Number of Cigs/Week | 7.26 | 3.26 | 2.23 | 7.93 | 4.05 | 1.96 |
| Days Used Cocaine/Week | −2.14 | 2.08 | −1.03 | −1.32 | 1.86 | −0.71 |
| Exposure to Violence | 13.76** | 3.40 | 4.05 | 14.50** | 3.44 | 4.21** |
| Maternal Sensitivity | 4.01 | 2.77 | 1.45 | |||
| Maternal Harshness | −1.59 | 2.27 | −0.70 | |||
| Interaction of Violence and Sensitivity | −17.03** | 4.84 | −3.52 | |||
| Interaction of Violence and Harshness | 12.26** | 4.55 | 2.70 | |||
| Interaction of PCE and Sensitivity | −4.30 | 3.24 | −1.33 | |||
| Interaction of PCE and Harshness | 5.71 | 4.27 | 1.34 | |||
Note: DV = dependent variable
p< .05.
p< .01.
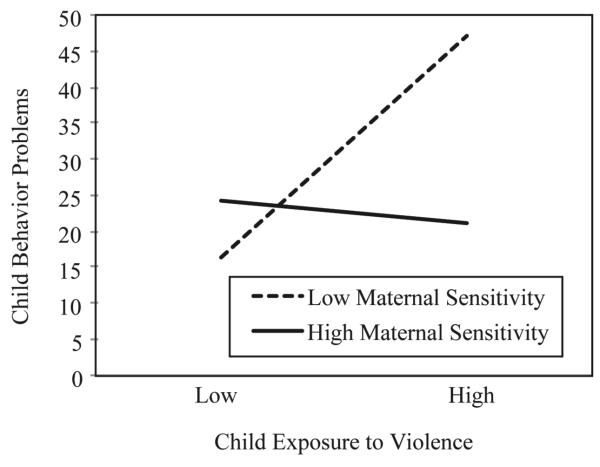
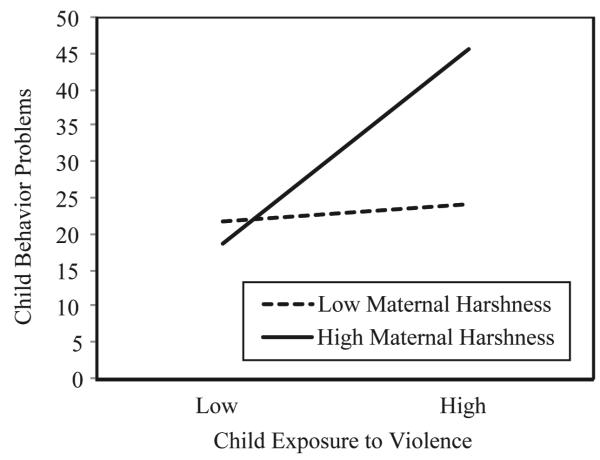
Two separate regression models were examined to test the hypotheses that maternal warmth/sensitivity and/or maternal harshness may moderate the association between exposure to violence and behavior problems. Parity was entered in the first step as a control variable, followed by prenatal substance exposure variables (number of drinks/week, number of cigarettes/week, number of joints/week, cocaine group status) in step 2, postnatal substance exposure variables, exposure to violence, and maternal warmth/sensitivity or harshness in step 3, and the product term of exposure to violence and maternal warmth/sensitivity or harshness in step 4. Results with maternal warmth/sensitivity as the moderator indicated that the model explained 34% of the variance in child behavior problems. As before, lower parity and higher exposure to violence were associated with higher child behavior problems. There was also a significant interaction effect of exposure to violence and maternal warmth/sensitivity on child behavior problems. As depicted in Figure 1, there was a significant association between exposure to violence and behavior problems at low levels of maternal warmth/sensitivity (−1 SD below the mean), but not at high levels of maternal warmth/sensitivity (+1 SD above the mean). Results with maternal harshness as the moderator indicated that the model explained 35% of the variance in child behavior problems (see Table 3). In addition to the first order effects of lower parity and exposure to violence, there was a significant interaction effect of exposure to violence and maternal harshness on child behavior problems. As depicted in Figure 2, there was a significant association between exposure to violence and child behavior problems at high (+1 SD above the mean) but not at low levels of maternal harshness (−1 SD below the mean).
Figure 1.
Maternal sensitivity moderating the association between exposure to violence and child behavior problems in kindergarten
Figure 2.
Maternal harshness moderating the association between exposure to violence and child behavior problems in kindergarten
Discussion
Our goal was to provide some clarity to the mixed literature on association between PCE and child behavior problems by examining potential moderators and mediators. Results from the current study indicated that there were no direct or indirect associations between PCE and child behavior problems. Although PCE was not associated with child exposure to violence, thus indicating no indirect association between PCE and violence exposure, we did find that child exposure to violence was a significant predictor of behavior problems. Moreover, this association was moderated by maternal warmth/sensitivity and harshness in theoretically predictable ways. We consider these findings in turn.
We hypothesized that PCE would be associated with behavior problems. Contrary to our hypothesis, results revealed no significant direct or indirect associations between PCE and child behavior problems, suggesting that cocaine exposure was not associated with maternal reports of child behavior problems as the children entered kindergarten. This finding was inconsistent with previous results of Bada et al. (2007; 2011), but the current study did not examine levels of cocaine exposure (i.e., dose-response), the sample size in the current study was smaller, and age of children in current study were younger. The lack of significant difference between exposed and matched controls may be due in part to the high-risk nature of the sample. Similar to previous research (Tronick & Beeghly, 1999), cocaine effects in this sample may not be visible in the face of cumulative risk factors. However, results of the present study are consistent with those of Accornero et al. (2002), who found no significant relationship between PCE and behavior problems in a sample of cocaine-exposed 5-year-olds.
Inconsistencies in the link between PCE and child behavior problems may also be due to unmeasured mediators or moderators. We proposed that one such mediator/moderator would be child exposure to violence. However, our results did not support this hypothesis because we found that PCE was not associated with violence exposure and the association between PCE and behavior problems did not vary across levels of violence exposure. These findings may indicate that violence exposure was more strongly related to demographic risk than cocaine use as our NCE group was carefully matched according to demographic data. Thus, PCE itself may not present a substantial risk for violence exposure within the context of a high-risk environment.
Contrary to hypotheses, parenting quality did not moderate the association between PCE and behavior problems. Only one previous study has examined parenting as a moderator of the association between prenatal exposure and child behavior problems (Wakschlag & Hans, 2002). Results from this study indicated that this moderation occurred only for boys with prenatal cigarette exposure. We did not examine three way interactions in the current study due to limitations of sample size and the children were younger compared to the previous study of 10 year olds. It is possible that there may be cumulative effects of warm/sensitive vs. harsh parenting across early childhood and the risk or protection conferred by parenting in the context of biological vulnerability associated with PCE may not be apparent until the children are older. Prospective studies of PCE cohorts with detailed assessments of parenting quality in early childhood are needed to address this issue.
Consistent with previous findings (e.g., Bada et al., 2011), results supported our hypothesis that violence exposure would be associated with behavior problems. These results are similar to those of Bada et al. (2011). In this study, exposure to violence accounted for significant variance in behavior problems at 7 years of age and was a more significant predictor of behavior problems than PCE. Findings were also supportive of our hypothesis that maternal warmth/sensitivity would be associated with lower behavior problems and that maternal harshness would be associated with higher behavior problems in the context of higher violence exposure, thus indicating that parenting behavior presents an important proximal risk and protective factor among children residing in high-risk homes and neighborhoods. These results are similar to those obtained by Ceballo et al. (2003) who reported that positive parenting served to protect children living in highly stressed environments. There may be a variety of ways that parenting behavior moderated exposure to violence for children. Krenichyn, Saegert, and Evans (2001), for instance, proposed that parents may respond to living in violent homes and communities by becoming emotionally distressed and, consequently, less emotionally available to their children. Conversely, some parents may provide needed social support to compensate for what they believe their children’s experience to be in order to minimize children’s potential exposure to violence. Some have argued that high maternal warmth and support promotes children’s adjustment regardless of the context of violence (Katz & Gottman, 1997). Our results indicate that this association may be particularly important in the context of high-risk environment and serve to buffer children from the potential negative consequences of living in high-risk homes and neighborhoods.
In addition to those findings directly related to our primary hypotheses, additional results are worth noting. Perhaps, most significant is the role of various covariates. Prenatal cigarette exposure was a significant predictor of child behavior problems, thus suggesting that comorbid prenatal cigarette use may partially account for elevated behavior problems reported among PCE children. This interpretation is supported by previous studies among NCE children indicating that prenatal tobacco exposure is associated with behavior problems (e.g., Day, Richardson, Goldschmidt, & Cornelius, 2000; Orlebeke, Knol, & Verhulst, 1997). The effects of prenatal tobacco exposure presents an important topic for future research involving PCE children as these children are disproportionately likely to be exposed to tobacco (Minnes et al., 2010).
Results also indicate that higher maternal postnatal cigarette, alcohol and marijuana use which were averaged across all postnatal phases were predictive of behavior problems in kindergarten and add to a growing body of evidence reporting significant associations between postnatal substance use and child behavior problems (Accornero et al., 2002; Bada et al., 2007). This finding suggests that postnatal substance use presents an important topic of treatment among mothers of PCE children.
Limitations
There are several limitations to this study. First, accurate measure of prenatal and postnatal substance use is difficult to obtain, as participants are often reluctant to divulge accurate information, particularly with regard to illicit substances such as cocaine. A strength of this study is the use of multiple methods to ascertain prenatal substance use, which partially mitigated this limitation. However, measures of prenatal use were retrospective. This has some advantages as well as limitations. One advantage is that cocaine-using women are less likely to present for prenatal care and may be missed in prenatal recruitment (Brady et al., 2003). Another advantage is that some women are more likely to acknowledge drug use postnatally after a successful delivery than in the prenatal period (Pickett et al., 2009). The primary disadvantage of recruitment at delivery is the retrospective recall of drug use data. We attempted to limit this problem by including well-validated measures for retrospective recall such as the TLFB and collection of hair samples that would yield data over a longer period of time. Second, is the lack of biological assays for measurement of postnatal substance use. Third, our measure of child behavior problems was derived solely from maternal report using CBCL. Previous research has shown that caregiver reports are only moderately correlated with alternative measures of behavior problems and are subject to rater bias. Future studies incorporating parental report, teacher report (see Delaney-Black et al., 2000) and observational measures of behavior problems are needed to extend this area of inquiry. Similarly, our exposure to violence measure was also limited to maternal reports. According to Farver et al. (2005), maternal report data are difficult to verify and are subject to recall bias. Mothers’ may not be fully aware of their young children’s experience or level of awareness and may inaccurately report the level of their children’s exposure. However, our prevalence rates for exposure to specific types of violence were similar to those reported in previous studies of young children. For instance, the current study found that 18% of the children had witnessed physical violence (i.e. someone being beaten up), and 7% had witnessed a stabbing or shooting. These results are similar to one study among children 5 years of age and younger found that 18% had witnessed a beating and 10% had witnessed a stabbing or shooting (Taylor et al., 1994). However, mothers may have found it emotionally difficult to report on aversive experiences of children’s violence exposure. Thus, our data could represent an underreporting of children’s experiences. Moreover, our final measure of violence included the CTS and only women with intimate partners completed this measure. Fourth, while our measures of parenting are objective and based on observations as opposed to parent reports, they are also limited to brief lab based interactions and subject to effects of being observed. Finally, we did not assess child IQ and this may have been an important covariate. In addition to these measurement issues, the generalizability of this study is limited to children of low-income predominantly African American mothers who used primarily crack cocaine throughout pregnancy, postnatal period, or both, and demographically matched controls.
Implications
In spite of these limitations, this study extends the literature on developmental outcomes among PCE children, as well as identifies risk and protective factors among children residing in high-risk environments. This is important because previous research has shown that early experiences may have long-lasting implications for developmental outcomes (Guerra, Huesmann, & Spindler, 2003). This study covers new ground by suggesting that exposure to violence and quality of parenting play an important role in the development of behavior problems during early childhood among PCE and non-PCE children experiencing high demographic risk. Results indicate that high maternal warmth/sensitivity may buffer children from the potential effects of exposure to violence, while maternal harshness may exacerbate these associations. Given the current findings, the role of risk and protective factors that may affect young children’s resiliency in challenging environment represents an important area of future research.
Acknowledgments
Brent Finger is now at Department of Psychology, Montana State University Billings. The study was supported by Award R01DA013190 from the National Institute on Drug Abuse. Special thanks to Dr. Claire Coles for collaboration on the larger study, Dr. Amol Lele for collaboration on data collection at Women and Children’s Hospital of Buffalo, and Dr. Michael Ray for his collaboration on data collection at Sisters of Charity Hospital of Buffalo. The authors thank the families who participated in this study and the research staff responsible for data collection.
Footnotes
Author Note Yvette Veira, Research Institute on Addictions, State University of New York at Buffalo; Brent Finger, Research Institute on Addictions, State University of New York at Buffalo; Rina D. Eiden, Research Institute on Addictions, State University of New York at Buffalo; Pamela Schuetze, Psychology Department, Buffalo State College; Craig R. Colder, Psychology Department, State University of New York at Buffalo; Stephanie Godleski, Research Institute on Addictions, State University of New York at Buffalo.
References
- Accornero VH, Morrow CE, Bandstra ES, Johnson AL, Anthony JC. Behavioral outcome of preschoolers exposed prenatally to cocaine: Role of maternal behavioral health. Journal of Pediatric Psychology. 2002;27(3):259–269. doi: 10.1093/jpepsy/27.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM. Manual for the child behavior checklist. University of Vermont Department of Psychiatry; Burlington: 2000. [Google Scholar]
- Bada HS, Bann CM, Bauer CR, Shankaran S, Lester B, LaGasse L, Higgins R. Preadolescent behavior problems after prenatal cocaine exposure: Relationship between teacher and caretaker ratings (Maternal Lifestyle Study). [Multicenter Study Research Support, N.I.H., Extramural] Neurotoxicology and Teratology. 2011;33(1):78–87. doi: 10.1016/j.ntt.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bada HS, Das A, Bauer CR, Shankaran S, Lester B, LaGasse L, et al. Impact of prenatal cocaine exposure on child behavior problems through school age. Journal of the American Academy of Pediatrics. 2007;119:348–359. doi: 10.1542/peds.2006-1404. [DOI] [PubMed] [Google Scholar]
- Bailey BN, Sood BG, Sokol RJ, Ager J, Janisse J, Hannigan JH, Delaney-Black V. Gender and alcohol moderate prenatal cocaine effects on teacher-report of child behavior. Neurotoxicology and Teratology. 2005;27:181–189. doi: 10.1016/j.ntt.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Bennett D, Bendersky M, Lewis M. Preadolescent health risk behavior as a function of prenatal cocaine exposure and gender. Journal of Development Behavioral Pediatric. 2007;28:467–472. doi: 10.1097/DBP.0b013e31811320d8. [DOI] [PubMed] [Google Scholar]
- Brady TM, Visscher W, Feder M, Burns AM. Maternal drug use and the timing of prenatal care. Journal of Health Care Poor Underserved. 2003;14:588–607. doi: 10.1353/hpu.2010.0700. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiment by nature and design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Ceballo R, Ramires L, Hearn KD, Maltese KL. Community violence and children’s psychological well-being: Does parental monitoring matter. Journal of Clinical Child & Adolescent Psychology. 2003;32:586–592. doi: 10.1207/S15374424JCCP3204_11. [DOI] [PubMed] [Google Scholar]
- Clark R, Musick J, Scott F, Klehr K. The mother’s project rating scale of mother-child intervention. 1980 Unpublished manuscript. [Google Scholar]
- Cummings JS, Pellegrini DS, Notarius CI, Cummings EM. Children’s responses to angry adult behavior as a function of marital distress and history of interparent hostility. Child Development. 1989;60:1035–1043. doi: 10.1111/j.1467-8624.1989.tb03534.x. [DOI] [PubMed] [Google Scholar]
- Day N, Richardson G, Goldschmidt L, Cornelius M. Prenatal tobacco exposure and preschooler behaviour. Journal of Behavioral and Developmental Pediatrics. 2000;21:180–188. [PubMed] [Google Scholar]
- Delaney-Black V, Covington C, Nordstrom B, Ager J, Janisse J, Hannigan JH, Sokol RJ. Prenatal cocaine: Quantity of exposure and gender moderation. Development and Behavioral Pediatric. 2004;25(4):254–263. doi: 10.1097/00004703-200408000-00005. [DOI] [PubMed] [Google Scholar]
- Delaney-Black V, Covington C, Templin T, Ager J, Nordstrom-Klee B, Martier S, Sokol RJ. Teacher-assessed behavior of children prenatally exposed to cocaine. Pediatrics. 2000;106:782–791. doi: 10.1542/peds.106.4.782. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Connell JP, Klebanov EK. Are neighborhood effects really causal? In: Duncan G, Brooks-Gunn J, Aber L, editors. Neighborhood poverty: Context and consequences for children. Russell Sage Foundation; New York: 1997. [Google Scholar]
- Farver J, Xu Y, Eppe S, Fernandez A, Schwartz D. Community violence, family conflict and preschoolers’ socioemotional function. Developmental Psychology. 2005;41:160–170. doi: 10.1037/0012-1649.41.1.160. [DOI] [PubMed] [Google Scholar]
- Eiden RD, Granger DA, Schuetze P, Veira Y. Child behavior problems among cocaine-exposed toddlers: Indirect and interactive effects. Development and Psychopathology. 2011;23:539–550. doi: 10.1017/S0954579411000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra NG, Huesmann LR, Spindler A. Community violence exposure, social cognition, and aggression among urban elementary school children. Child Development. 2003;74:1561–1576. doi: 10.1111/1467-8624.00623. [DOI] [PubMed] [Google Scholar]
- Irner TB. Substance exposure in utero and developmental consequences in adolescence: A systematic review. Child Neuropsychology. 2012;18(6):521–549. doi: 10.1080/09297049.2011.628309. [DOI] [PubMed] [Google Scholar]
- Jansen R, Oud JHL. Longitudinal LISREL model estimation from incomplete panel using and EM algorithm and the Kalman smoother. Statistica Neerlandica. 1995;49:362–377. [Google Scholar]
- Jouriles EN, McDonald R, Rosenfield D, Stephens N, Corbitt-Shindler D, Miller PC. Reducing conduct problems among children exposed to intimate partner violence: A randomized clinical trial examining effects of project support. Journal of Consulting and Clinical Psychology. 2009;77(4):705–717. doi: 10.1037/a0015994. [DOI] [PubMed] [Google Scholar]
- Katz LF, Gottman JM. Buffering children from marital conflict and dissolution. Journal of Clinical Child Psychology. 1997;26:157–171. doi: 10.1207/s15374424jccp2602_4. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. The development of aggression in toddlers: a study of low-income families. Journal of Abnormal Child Psychology. 1994;22:53–77. doi: 10.1007/BF02169256. [DOI] [PubMed] [Google Scholar]
- Krenichyn K, Saegert S, Evans GW. Parents as moderators of psychological and physiological correlates of inner-city children’s exposure to violence. Journal of Applied Development Psychology. 2001;22:581–602. [Google Scholar]
- Lester BM, Bagner DM, Liu J, LaGasse LL, Seifer R, Bauer CR, Das A. Infant neurobehavioral dysregulation: Behavior problems in children with prenatal substance exposure. Pediatrics. 2009;124(5):1355–1362. doi: 10.1542/peds.2008-2898. doi: 10.1542/peds.2008-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, LaGasse L, Seifer R, Tronick EZ, Bauer CR, Shankaran S, Bada HS, Wright LL, Smeriglio VL, Liu J, Finnegan LP, Maza PL. The maternal lifestyle study (MlS): Effects of prenatal cocaine and/or opiate exposure on auditory brain response at one month. Journal of Pediatrics. 2003;142(3):279–285. doi: 10.1067/mpd.2003.112. [DOI] [PubMed] [Google Scholar]
- Li Z, Santhanam P, Coles CD, Lynch ME, Hamann S, Peltier S, Hu X. Increased ‘default mode’ activity in adolescents prenatally exposed to cocaine. Human Brain Mapping. 2011;32(5):759–770. doi: 10.1002/hbm.21059. doi: 10.1002/hbm.21059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares LO, Heeren T, Bronfman E, Zuckerman B, Augustyn M, Tronick E. A mediational model for the impact of exposure to community violence on early child Behavior problems. Child Development. 2001;72(2):639–652. doi: 10.1111/1467-8624.00302. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D. The construct of resilience: implications for interventions and social policies. Development and Psychopathology. 2000;12(4):857–885. doi: 10.1017/s0954579400004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch M. Children exposed to community violence. In: Feerick M, Silverman G, editors. Children Exposed to Violence. Paul H. Brookes; Baltimore, MD: 2006. pp. 29–52. [Google Scholar]
- Magura S, Freeman RC, Siddiqi Q, Lipton DD. The validity of hair analysis for detecting cocaine and heroin use among addicts. International Journal of Addiction. 1992;27:51–69. doi: 10.3109/10826089109063462. [DOI] [PubMed] [Google Scholar]
- Mayes L, Bornstein M. The development of children exposed to cocaine. In: Luthar S, Burack J, Cicchetti D, Weisz J, editors. Developmental psychopathology: Perspectives on adjustment risk and disorder. Cambridge University Press; New York: 1997. pp. 166–188. [Google Scholar]
- McCart MR, Priester PE, Davies WH, Azen R. Differential effectiveness of behavioral parent-training and cognitive-behavioral therapy for antisocial youth: A meta-analysis. Journal of Abnormal Child Psychology. 2006;34(4):527–543. doi: 10.1007/s10802-006-9031-1. [DOI] [PubMed] [Google Scholar]
- Mignone T, Klostermann K, Chen R. The relationship between relapse to alcohol and relapse to violence. Journal of Family Violence. 2009;24:497–505. [Google Scholar]
- Minnes S, Singer LT, Kirchner HL, Short E, Lewis B, Satayathom S, Queh D. The effects of prenatal cocaine exposure on problem behavior in children 4 -10 years. Neurotoxicology and Teratology. 2010;32:443–451. doi: 10.1016/j.ntt.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlebeke JF, Knol DL, Verhulst FC. Increase in child behavior problems resulting from maternal smoking during pregnancy. Archive Environmental Health. 1997;52:317–321. doi: 10.1080/00039899709602205. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Kasza K, Biesecker G, Wright RJ, Wakschlag LS. Women who remember, women who do not: A methodological study of maternal recall of smoking in pregnancy. Nicotine & Tobacco Research. 2009;11:1166–1174. doi: 10.1093/ntr/ntp117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Saltzman W. Survey of exposure to community violence: Self-report version. National Institute of Mental Health; Rockville, MD: 1990. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update of ice. The Stata Journal. 2005;5:527–536. [Google Scholar]
- Salzinger S, Feldman RS, Rosario M, Ng-Mak DS. Role of parent and peer relationships and individual characteristics in middle school children’s behavioral outcomes in the face of community violence. Journal of Research on Adolescence. 2011;21(2):395–407. doi: 10.1111/j.1532-7795.2010.00677.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of art. Psychology Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Shahinfar A, Fox N, Leavitt L. Preschool children’s exposure to violence: Relation of behavior problems to parent and children reports. American Journal of Orthopsychiatry. 2000;70:115–125. doi: 10.1037/h0087690. [DOI] [PubMed] [Google Scholar]
- Singer LT, Minnes S, Short E, Arendt R, Farkas K, Lewis B, et al. Cognitive outcomes of preschool children with prenatal cocaine exposure. Journal of the American Medical Association. 2004;291:2448–3456. doi: 10.1001/jama.291.20.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajmer F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students’ recent. 1986 doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol timeline followback (TLFB) users’ manual. Addiction Research Foundation; Toronto, Canada: 1996. [Google Scholar]
- Straus MA. Measuring intra family conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Taylor L, Zuckerman B, Harik V, McAlister Groves B. Witnessing violence during pregnancy and substance use. American Journal of Public Health. 1994;80(5):575–579. doi: 10.2105/ajph.80.5.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tronick EZ, Beeghly M. Prenatal cocaine exposure, child development, and the compromising effects of cumulative risk. Clinical Perinatology. 1999;26:151–171. [PubMed] [Google Scholar]
- Wakschlag LS, Hans SL. Maternal smoking during pregnancy and conduct problems in high-risk youth: A developmental framework. Development and Psychopathology. 2002;14:351–369. doi: 10.1017/s0954579402002092. [DOI] [PubMed] [Google Scholar]
- Warner TD, Behnke M, Hou W, Garvan CW, Wobie K, Eyler FD. Predicting caregiver-reported behavior problems in cocaine-exposed children at 3 years. Development and Behavioral Pediatrics. 2006;27:83–92. doi: 10.1097/00004703-200604000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yutomo C, Jacobson SW, Jacobson JC. Fetal substance exposure and cumulative environmental risk in an African-American cohort. Child Development. 2008;76:1761–1776. doi: 10.1111/j.1467-8624.2008.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]