Abstract
Background: The introduction of selective serotonin reuptake inhibitors (SSRIs) represented a breakthrough in depression treatment due to their safety and ease of use. The purpose of this study was to extend previous work on trends in antidepressant use to include recent data and to provide more detailed analysis of prescribing trends for SSRIs and newer non-SSRI antidepressants, specifically in adult primary care practice.
Method: Adult primary care visits from the National Ambulatory Medical Care Survey (NAMCS) between 1989 and 2000 were analyzed. Chi-square tests for trend and multivariable logistic regression models were utilized to examine patterns of antidepressant use over time. SSRIs (citalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) and newer non-SSRI antidepressants (bupropion, mirtazapine, nefazodone, venlafaxine) were classified as newer agents.
Results: 89,424 adult primary care visits were recorded in the NAMCS during the period studied. Antidepressant use increased in primary care from 2.6% (∼ 6 million visits) in 1989 to 7.1% (∼ 20.5 million) in 2000 (p < .001). SSRI and newer non-SSRI use increased linearly from 1989 to 2000 (p < .001), with an adjusted odds ratio for use of 1.27 per year (95% confidence interval = 1.25 to 1.29). The increase in antidepressant use was due to these newer agents (13.5% of all antidepressant use in 1989 to 82.3% in 2000) with each new agent adding to a stable base of previously introduced newer antidepressant agents.
Conclusions: The prevalence of antidepressant use in adult primary care has risen dramatically since 1989, largely reflecting use of newer agents. The detailed pattern of increased use of these medications is striking, with each new agent adding to aggregate use without concomitant decrease in previously introduced newer agents. Such trends reflect more widespread pharmacologic treatment of depressed primary care patients.
The advent of selective serotonin reuptake inhibitors (SSRIs) in 1988 represented a turning point in the treatment of depression. SSRIs and subsequently introduced non-SSRI (atypical) antidepressants have a more favorable safety profile and are easier to use than older agents. Antidepressant prescribing reported in primary care visits has increased1 and appears to reflect increased prescribing of these new agents.2–4
Better understanding of the prescribing of antidepressant medications in primary care is essential. Studies have reported that 23% of primary care patients have a depressive disorder5 and that 6.6%6 to 13.5%5 have a major depressive illness; prescribing of antidepressants would most likely be appropriate in these patients. Furthermore, guidelines stress the importance of primary care physicians in the diagnosis and treatment of depression,7,8 and over half of patients with major depression seeking help are seen in the general medical sector.9
By using data from the National Ambulatory Medical Care Survey (NAMCS) during the period January 1989 to December 2000, our aim was to extend previous work on trends in depression diagnosis and antidepressant prescribing to more recently acquired data, and to focus exclusively on these trends in primary care. We expected that examination of the 12-year period following the introduction of SSRIs would demonstrate a sustained increase in overall antidepressant medication prescribing in primary care attributable to increased prescribing of SSRIs and newer non-SSRI antidepressant agents. We sought to link upward trends in antidepressant prescribing to increasing diagnosis of depression, as these medications may result in a lower threshold for diagnosis. Lastly, we used these data to examine the impact of serial introduction of SSRIs and newer non-SSRI antidepressant agents.
METHOD
The NAMCS is a national probability survey of outpatient practices administered by the National Center for Health Statistics (Hyattsville, Md.), an organizational component of the Centers for Disease Control and Prevention (CDC). Randomly selected office-based practitioners complete the surveys for 1 week on a systematic sample of their outpatient visits. The unit of measurement is patient visits. The NAMCS participation rate for general practitioners, family practitioners, and internists combined was 70% in 1989 and 69% in 2000.10 NAMCS data and a detailed description of the survey methodology are publicly available through the CDC Web site.11
The NAMCS was utilized for the years 1989 through 2000 to provide estimates of antidepressant prescribing in ambulatory medical care visits in the United States since the introduction of SSRIs. Primary care physicians were defined as family practitioners, general practitioners, and internists, and analysis was limited to patients aged 18 years and older. The NAMCS instructs practitioners to list medications that were “ordered, supplied, administered, or continued”10 at that visit. The number of medications that could be listed was not consistent year to year, so while up to 6 medications were listed for 1995 to 2000, a maximum of 5 medications were listed for 1989 to 1994. Therefore, our analysis included the first 5 medications listed across all years examined.
Medication entries are listed in the databases by drug entry codes developed by the National Center for Health Statistics. We classified tricyclic and tetracyclic antidepressants, tricyclic and tetracyclic antidepressant combination products, monoamine oxidase inhibitors (MAOIs), and trazodone as older antidepressant agents. SSRIs (citalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) and newer non-SSRI antidepressants (bupropion, mirtazapine, nefazodone, venlafaxine) were classified as newer agents. When prescribed, antidepressants were among the top 3 listed medications in 90% of visits. When an antidepressant was not listed, 5 other medications were listed in 7% of visits. The number of visits in the NAMCS in which antidepressant prescribing occurred but was not reported is unknown.
The NAMCS records up to 3 diagnoses coded according to the International Classification of Diseases, Clinical Modification, Ninth Revision (ICD-9-CM).12 We searched for ICD-9-CM codes corresponding to a diagnosis of depression (296.20, 296.30, 300.40, 309.10, and 311.00) for any of 3 possible diagnostic entities that could be listed on the NAMCS form. When depression was diagnosed, it was listed as the primary diagnosis in 50.5% of visits. Among primary care visits where a depression diagnosis was not listed, 18.7% used the 3 available entries for other diagnoses, which indicates some diagnoses of depression may not have been reported in the NAMCS.
Statistical Analysis
Our primary outcome was newer antidepressant prescribing, but we also examined older antidepressant prescribing and overall antidepressant medication prescribing, as well as whether depression was listed as a diagnosis. Sampling variables used to account for the complex design of the NAMCS were not available for all years of interest. We therefore adjusted the sample weights in all analyses according to the method of Potthoff et al.13 which provides estimates of standard errors. Chi-square tests for trends were used to examine the relationship of year with categorical variables and univariate regressions for the relationship of year with continuous variables. Multivariable logistic regression models were used to analyze yearly trends over time adjusted for available potential confounders (i.e., patient age, duration of visit, gender, and race/ethnicity). These factors were included in each model. We performed a subset analysis of only those visits for which depression was listed as a diagnosis.
Starting with 1991, NAMCS data include a physician-specific identifier, which we used to determine whether accounting for clustering effects by physician would be necessary in the logistic models. Using 1991 to 2000 data, results for models that accounted for physician clustering were very similar to models that did not account for clustering. We therefore used models that did not account for clustering, so that the years proximate to the introduction of SSRIs could be included in the analysis. All analyses were performed using SAS software, version 8.2 (SAS Institute, Cary, N.C.).
RESULTS
89,424 adult primary care visits were recorded in the NAMCS between 1989 and 2000, representing approximately 260 million annual visits. Over the period studied, the average age of patients seen in primary care visits increased from 51.6 to 53.3 years (p < .001). There were modest changes in other sociodemographic visit characteristics as well. The proportion of males increased from 33.8% to 40.2% (p < .001). Race/ethnicity changed (p < .0001), with the proportion of Hispanics increasing from 5.2% to 8.8% and black non-Hispanics declining from 11.2% to 9.7%.
Newer Antidepressant Prescribing
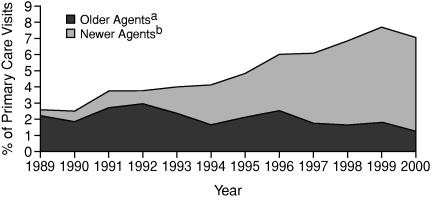
The proportion of visits for which an older antidepressant was listed declined modestly over the period studied (adjusted odds ratio [OR] = 0.97 per year, 95% confidence interval [CI] = 0.95 to 0.99). In contrast, there was a striking linear increase in the odds that newer antidepressants would be used (OR = 1.27 per year, 95% CI = 1.25 to 1.29). This increase of 27% per year outpaced the decline in the prescribing of older antidepressants (Figure 1). Because bupropion can be prescribed for smoking cessation, we repeated the analyses without this medication, and the point estimates did not change.
Figure 1.
Use of Older and Newer Antidepressants in Adult Primary Care Visits
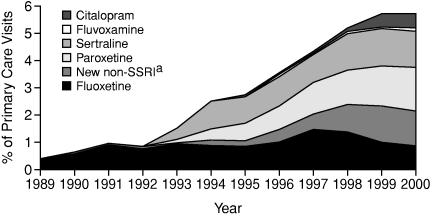
We examined the contribution over time of individual SSRIs and the newer non-SSRI antidepressants. Because of the relatively smaller numbers for the individual newer non-SSRI antidepressants, these were collapsed into a single category. Figure 2 illustrates how each new agent added to total newer antidepressant prescribing. Prescribing of each agent tended to increase after its introduction and then level off. Interestingly, there appears to be little to no diminution in the aggregate prescribing of each agent after other newer agents were introduced.
Figure 2.
Use of Individual SSRIs and Newer Non-SSRIs in Adult Primary Care Visits
Overall Antidepressant Prescribing
Reporting of antidepressant medication prescribing among all primary care visits increased significantly over the 12-year period, from 2.6% of visits (corresponding to an estimated 6.3 million visits) in 1989 to 7.1% of visits (∼ 20.5 million visits) in 2000 (p < .001). In a multivariable model that adjusted for patient age, duration of visit, gender, and race/ethnicity, the likelihood of the prescribing of antidepressant medication among all adult primary care visits increased dramatically over time (OR = 1.12 per year, 95% CI = 1.10 to 1.13).
Tricyclic and tetracyclic antidepressant prescribing was reported in 1.73% of primary care visits in 1989 and 1.03% in 2000, but the test for trend was not significant. Tricyclic and tetracyclic antidepressant combination preparations and MAOIs were rarely prescribed. Trazodone prescribing increased from 0.38% in 1989 to 0.54% in 2000 (p < .008 for trend). SSRI prescribing dominated the increase in prescribing of antidepressants. By 1994, SSRIs accounted for the majority of antidepressants listed, and in 2000, SSRIs comprised 65% of all antidepressants prescribed in primary care. Similarly, prescribing of the newer non-SSRIs grew to account for 17% of all antidepressant prescribing reported in 2000. In total, of antidepressant prescribing reported in primary care visits in 2000, 82% were newer antidepressants.
Depression Diagnosis in Primary Care
In parallel with increasing prescribing of newer antidepressant agents in primary care, the yearly prevalence of the diagnosis of depression increased significantly (p < .001), from 2.0% (∼ 4.8 million visits) in 1989 to 3.3% (∼ 9.5 million visits) in 2000. The adjusted OR for the diagnosis of depression was 1.07 per year (95% CI = 1.06 to 1.09).
Antidepressant Prescribing in Visits With a Depression Diagnosis
Overall prescribing of antidepressants increased among visits in which depression was a diagnosis (OR = 1.07, 95% CI = 1.04 to 1.10). Prescribing of older antidepressants declined by 20% per year (OR = 0.80 per year, 95% CI = 0.77 to 0.83), whereas prescribing of newer antidepressants increased by 26% per year (OR = 1.26 per year, 95% CI = 1.22 to 1.31). In this population, the replacement of older with newer agents is more obvious, but again, there is increased prescribing beyond that of simple replacement. The pattern for individual newer agents among visits with a depression diagnosis is similar to that found for the general primary care population, with each agent adding to aggregate prescribing with little to no decline in the other newer agents.
DISCUSSION
Our results document that antidepressant prescribing in primary care has increased since the introduction of SSRIs and that this increase is composed of SSRI and newer non-SSRI agents rather than older antidepressants. By 1994, SSRI prescribing eclipsed that for all other antidepressants combined. With increased prescribing of newer agents, there has been a parallel increase in the frequency of the diagnosis of depression in primary care visits. It is likely that the popularity of newer antidepressant agents has prompted a lower threshold for making a diagnosis of depression.
We have also observed a remarkable pattern of each newly introduced, and potentially competitive, agent adding to aggregate prescribing of antidepressants without a net reduction in the prescribing of previously introduced agents. This expansion in the prescribing of newer medications may reflect broadened indications for these medications, although the same pattern held when we restricted our analysis to visits for which depression was explicitly listed as a diagnosis. Newer agents have somewhat different patterns of efficacy and side effects, providing the physician with added therapeutic flexibility and expanding the pool of treatable patients.
Finally, our results likely reflect, in part, aggressive marketing by pharmaceutical companies. Recent work by Zachry and colleagues14 found that direct-to-consumer advertising increased diagnosis and treatment of some conditions, although depression was not among the conditions they examined. It will be interesting to see if the pattern we describe persists with the introduction of more new branded agents or changes after addition of generic formulations.
There have been several prior studies of patterns of antidepressant prescribing.2–4,15–17 Our work confirms previous reports on national trends, and it extends beyond previous studies of primary care by encompassing a longer, continuous period of analysis. In particular, ours is the first study to highlight the distinctive pattern of increasing aggregate prescribing of antidepressants following the introduction of each new agent.
The NAMCS encompasses a large scope of outpatient care visits but lacks detailed clinical information. It does not include medication dose or duration of treatment, so treatment adequacy or adherence cannot be evaluated. Other medical illnesses may well supersede depression for inclusion among the 3 diagnoses listed. The observation that the proportion of visits with antidepressant prescribing exceeds that for depression diagnosis may reflect prescribing of these medications for indications other than that of depression, or could reflect underreporting of depression, even when treated. Since the unit of measurement in the NAMCS is visits, not patients, our results could be influenced by shorter intervals between visits by depressed patients over time. Nonetheless, our results reflect trends from the perspective of primary care practice.
Depression is a common, serious illness seen in primary care practice. The advent of SSRIs and newer non-SSRI antidepressants has revolutionized depression management. We have demonstrated a clear trend of increasing antidepressant prescribing and of increasing prevalence of depression diagnoses in primary care practice. Newer antidepressant agents appear to be the driving force in these trends. Our findings suggest that the addition of newer antidepressant agents is central to the expansion in aggregate prescribing of these medications. The mechanism for this pattern is not clear. Likely components include broadening of indications for these agents, greater flexibility afforded by additional agents with somewhat different efficacy and side-effect profiles, increased comfort among primary care physicians with prescribing these agents, and aggressive marketing of new antidepressant medications. Depression has been reported to be underrecognized and undertreated in primary care.18 By contrast, our findings show positive trends toward more frequent diagnosis of depression and more widespread pharmacologic intervention for depression in primary care visits.
Drug names:bupropion (Wellbutrin and others), citalopram (Celexa), fluoxetine (Prozac and others), mirtazapine (Remeron and others), nefazodone (Serzone), paroxetine (Paxil), setraline (Zoloft), trazodone (Desyrel and others), venlafaxine (Effexor).
Footnotes
This work was supported by National Research Service Award grant number 5 T32 PE 11001-14 (Dr. Pirraglia) and the Donald W. Reynolds Cardiovascular Clinical Research Center (Dr. Stafford), Stanford University, Calif.
Presented at the New England Regional Society of General Internal Medicine Meeting, March 14, 2003, Storrs, Conn., and the National Society of General Internal Medicine Meeting, April 30–May 3, 2003, Vancouver, British Columbia.
REFERENCES
- Pincus HA, Tanielian TL, and Marcus SC. et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998 279:526–531. [DOI] [PubMed] [Google Scholar]
- Sclar DA, Robison LM, and Skaer TL. et al. Trends in prescribing of antidepressant pharmacotherapy: office-based visits, 1990–1995. Clin Ther. 1998 20:871–884. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, and Druss B. et al. National trends in the outpatient treatment of depression. JAMA. 2002 287:203–209. [DOI] [PubMed] [Google Scholar]
- Stafford RS, MacDonald EA, Finkelstein SN.. National patterns of medication treatment for depression, 1987 to 2001. Primary Care Companion J Clin Psychiatry. 2001;3:232–235. doi: 10.4088/pcc.v03n0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC, Fechner-Bates S, Schwenk TL.. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16:267–276. doi: 10.1016/0163-8343(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M.. Recognition, management, and outcomes of depression in primary care. Arch Fam Med. 1995;4:99–105. doi: 10.1001/archfami.4.2.99. [DOI] [PubMed] [Google Scholar]
- Clinical Practice Guideline, Number 5: Depression in Primary Care, vol 1. Diagnosis and Detection. Rockville, Md: US Dept Health Human Services, Agency for Health Care Policy and Research. 1993 AHCPR publication 93-0550. [Google Scholar]
- Clinical Practice Guideline, Number 5. Depression in Primary Care, vol 2. Treatment of Major Depression. Rockville, Md: US Dept Health Human Services, Agency for Health Care Policy and Research. 1993 AHCPR publication 93-0551. [Google Scholar]
- Regier DA, Narrow WE, and Rae DS. et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993 50:85–94. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Public Use Data Files (Micro Data). National Ambulatory Medical Care Survey, 1989 to 2000. Available at: http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm#Micro-data. Accessed May 15, 2003. [Google Scholar]
- National Center for Health Statistics. National Ambulatory Medical Care Survey (NAMCS). Available at: http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm. Accessed May 15, 2003. [Google Scholar]
- American Medical Association. ICD-9-CM: International Classification of Diseases, 9th Revision, Clinical Modification. Dover, Del: American Medical Association. 1998 [Google Scholar]
- Potthoff RF, Woodbury MA, Manton KG.. “Equivalent sample size” and “equivalent degrees of freedom” refinements for inference using survey weights under superpopulation models. J Am Stat Assoc. 1992;87:383–396. [Google Scholar]
- Zachry WM, Shepherd MD, and Hinich MJ. et al. Relationship between direct-to-consumer advertising and physician diagnosing and prescribing. Am J Health Syst Pharm. 2002 59:42–49. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Kessler RC, and Lin E. et al. Medication management of depression in the United States and Ontario. J Gen Intern Med. 1998 13:77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Hoff RA, Rosenheck RA.. Underuse of antidepressants in major depression: prevalence and correlates in a national sample of young adults. J Clin Psychiatry. 2000;61:234–237. [PubMed] [Google Scholar]
- Stafford RS, Ausiello JC, and Misra B. et al. National patterns of depression treatment in primary care. Primary Care Companion J Clin Psychiatry. 2000 2:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JR., Meltzer-Brody SE. The underrecognition and undertreatment of depression: what is the breadth and depth of the problem? J Clin Psychiatry. 1999 60suppl 7. 4–9. [PubMed] [Google Scholar]