Abstract
Background: The outcome of therapeutic community treatment for drug abuse has been disputed with regard to mortality and rehabilitation to school or work as compared with other treatment modalities.
Method: All patients (N = 130) admitted to a therapeutic community during 3 consecutive years (1996–1998), who had failed to stop abusing drugs after ambulatory and primary care initiatives, were assessed 1 to 4 years (mean = 36.5 months) after end of treatment. Rates of rehabilitation to school or work, changes in drug use patterns, and mortality were observed.
Results: Nine persons died during the observation period (the observation time to death seemed to be shorter in women than in men). The mortality rate per 100 observation years was 2.28. Among the surviving drug abusers, 39% were working or attending school at study endpoint. One fourth currently used drugs, and approximately 14% were enrolled in a methadone maintenance program. Another 13% were in treatment or prison.
Conclusion: Drug abuse is an activity that increases the mortality rate, but among the surviving persons, a considerable number are rehabilitated, as assessed after a longer observation period. The authors suggest that this outcome could not have been attained with ambulatory general practice–driven services, even with empathic follow-up.
Primary care practitioners are often the first to see the detrimental effects of drug abuse, but rarely are in a position to supply necessary and sufficient help.1 This is especially true today, as pressure to remain cost- effective pushes patients toward ambulatory treatment. Drug abusers run a higher risk of dying from their drug use than the age- and sex-matched nonabusing population at large.2–4 Increased mortality is probably related only to the drug abuse and is mainly due to overdoses, infections, and accidents. The death of a patient may be viewed as a failure of the treatment facility from which the incumbent was released, but as the distance in time between those 2 events might be lengthy, the question of attribution is relevant.
Third-party funding of residential treatment has been severely curtailed over the past decade in the United States and in several European countries, including Scandinavia. The care of many patients with substance abuse problems has been transferred to ambulatory programs and primary care.5 In contrast, therapeutic community treatment remains a viable option in Norway and Sweden. Understanding the long-term outcomes of therapeutic community treatment could add perspective to the treatment outcomes obtained within less intense treatment settings.
To what extent does a resident's stay at a treatment or rehabilitation facility contribute to the observed effect on behavior? Treatment counselors would only reluctantly accept that the effect of their own treatment models could be detrimental to the patient. The Project Match study did not find any differences between several accepted alcohol treatment modalities.6 In viewing the high rates of attrition, even from methadone maintenance treatment, some researchers and clinicians maintain that no intervention really helps. The general weakening of patients' symptoms over years would be the dominant factor for a healthy outcome, except for mere accidents. On the other hand, it would be tempting to argue that models such as psychotherapy, medication only, general practice handling, therapeutic community treatment, and Alcoholics Anonymous cannot be expected to give the same result in drug abusers as in alcoholics. There are, however, still several pitfalls to the discourse on effect of treatment for all types of substance abusers.
Rates of drug treatment completion are often depressingly low, as shown by Ravndal et al.7,8 from a therapeutic community in Oslo. Only 14% of an initial sample of 200 accepted patients completed a 1.5-year stay. After 5 years, a quarter of the original sample had been through 3 to 7 treatment attempts. No significant correlations were found between number of residential stays and severity of addiction or rehabilitation efforts.
The patient mix may be so diverse that no one treatment option would suffice. This assumption is used, often without any substantiation, as researchers find differences in rehabilitation effect or mortality between facilities.
There are indications that “no-shows” at follow-up among former drug abusers may be due to stable functioning. These patients would have no interest in shedding light on a turbulent past. This is in contrast to what is generally imputed in epidemiologic studies9,10 in other populations, where a no-show is taken as an indication of a bad outcome. Former drug abusers, who have managed to build a new life, have every reason to conceal their pasts. Some even change names and identity numbers. In a Norwegian 10-year follow-up study,11 1 in 4 former drug abusers refused interviews because of well-functioning lives.
The therapeutic community approach is not free from such criticisms as previously mentioned, but as an approach, it is comprehensive.12,13 Therapeutic community treatment includes learning of social skills, vocational training, group responsibility and cooperation training, and, often, external psychological counseling. A low rate of completion in many therapeutic communities has been taken as an indication of meager effect of the model, as suggested in the studies by Ravndal et al.7,8 Follow-up time has, however, been short, and we therefore wanted to look into the effect of a therapeutic community 3 years after entry. The effect measures were mortality rate and fraction entering work or school within the observation period.
METHOD
This study included all patients (N = 130) admitted to a therapeutic community, the Phoenix House in Haga, Norway, between 1996 and 1998. All patients were multiple drug users, and their main drugs of abuse were heroin, hashish, amphetamine, and alcohol. As the patients had been abusing drugs for years, they all had used, or maybe even abused, their general practitioner to an extent that the physician could not give any more advice other than a referral to a residential facility. All patients satisfied the ICD-10 definition of a dependence syndrome. The information on endpoint status was obtained from the facility staff by way of the facility's aftercare activities. Thus, a formal search of the State Death Register was not performed for this study.
There were 99 men (76.2%) and 31 women (23.8%) included in the study. Forty-nine patients entered the facility in 1996, 46 in 1997, and 35 in 1998. Some stayed for more than a year. Mean duration of stay was 8.6 months. Mean age at entry was 28.5 years (SD = 5.2) for all patients, and 29.1 and 26.6 years in men and women, respectively. The mean observation time from intake to follow-up in May 2001 was 36.5 months (SD = 18.3 months) for all patients, and 37.2 (SD = 18.1) and 34.0 (SD = 19.0) months in men and women, respectively.
RESULTS
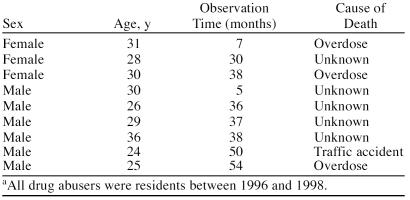
Nine persons died after the residential treatment period (Table 1). Mean age at intake of persons who died was 28.8 years, i.e., not different from the survivors. The mean observation time among the deceased was 32.8 months. The time schedule of deaths is shown in Figure 1. There were 2.28 deaths per 100 observation years. Although the first patient who died was male, the fall in the survival curve in Figure 1 indicates that the observation time before death was shorter in female patients. There was no significantly different mortality in men and women by t test (t = 1.1). Figure 2 shows the deaths according to year of referral to the therapeutic community. Five persons died in the group referred in 1996 and 4 in the 1997 group.
Table 1.
Sociodemographic Characteristics of 9 Deceased Drug Abusers From Phoenix Housea
Figure 1.
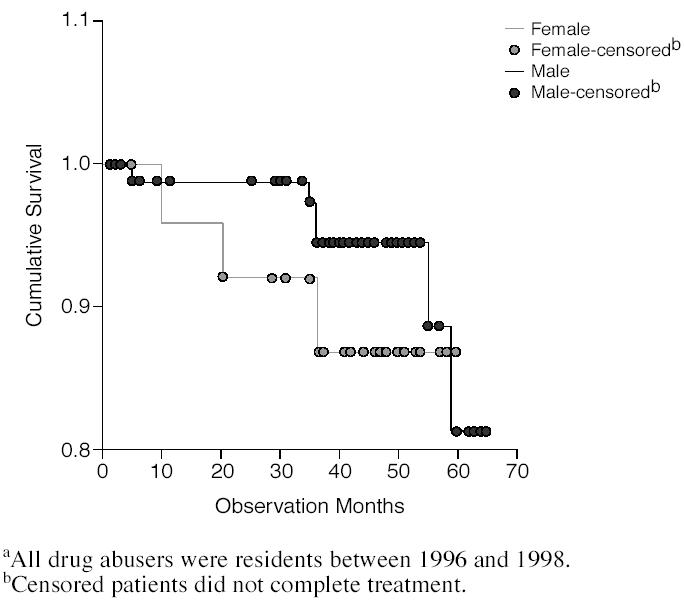
Time of Death by Sex of 130 Drug Abusers From Phoenix Housea
Figure 2.
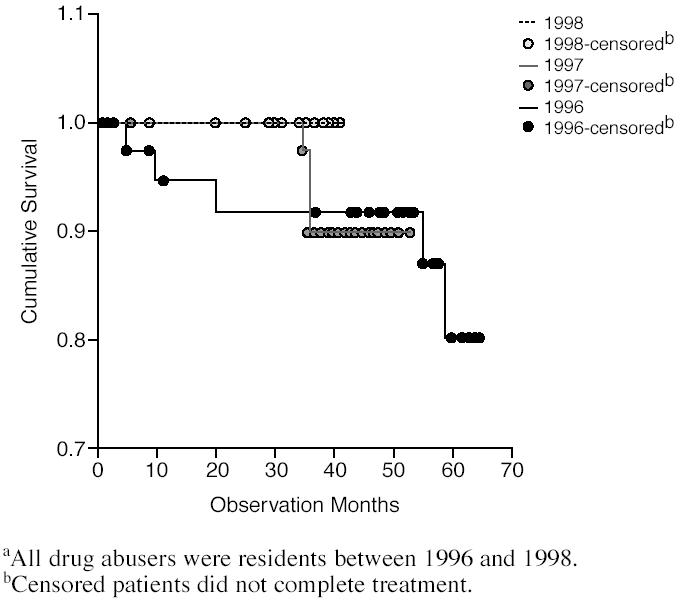
Time of Death by Year of Referral of 130 Drug Abusers From Phoenix Housea
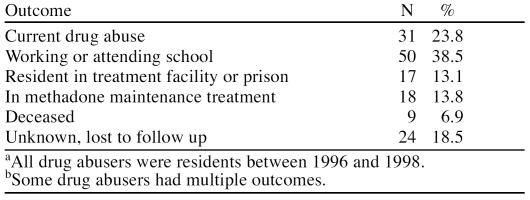
The mean observation time for all patients was 36.5 months, 37.2 months for men and 34.0 months for women. Table 2 gives the outcome at study endpoint regarding current drug use, treatment, or work status. Twenty-four residents were lost to follow-up, i.e., at study endpoint the status was unknown. For some patients, status was known 1 year after conclusion of stay at the therapeutic community, but not at the study endpoint. Patients currently working or attending school amounted to 38.5%. Thirteen percent were either in prison or again in treatment, either at the Phoenix House or another facility. Almost 14% were currently in methadone maintenance treatment, an option made available to patients during the study period.
Table 2.
Treatment Outcomes of 130 Drug Abusers From Phoenix House as of May 2001a,b
DISCUSSION
The observed mortality rate among these heavy drug abusers referred from primary care or social welfare counselors compares well with other studies of mortality among drug addicts in Norway. In a 10-year follow-up study of 482 drug addicts, the mortality rate among clients from rehabilitation-oriented facilities, comparable to therapeutic communities, was 1.6%.14 Rossow and Kielland15 found a mortality rate per year of 1.7% in a study population (N = 1491) from a Norwegian psychiatrically oriented drug treatment hospital. Findings of higher mortality rates among subgroups of drug abusers thus may hinge on other detrimental factors not present in persons leaving therapeutic communities in Norway. We have no explanation for the observed difference in time before death in women and men, but the observed group in the present study is small.
Mortality is a hard endpoint, but to be of any use in planning for future treatment and rehabilitation, a broader view of treatment efforts must be incorporated. Rehabilitation aspects often lack a focus during residential treatment.16–18 Thus, implementing a comprehensive network involving the drug abuser and the primary care setting could improve the efforts of treatment facilities.19 Innovative techniques such as videotaping for assessment and individual treatment planning may also be of help.20
Notwithstanding, in the present study, we found that almost half of the surviving group did attain working status or were engaged in vocationally oriented schooling either with or without the help of methadone maintenance treatment. Methadone maintenance treatment has not been a possibility for more than 5 years in Norway. Also, the group lost to follow-up may contain former drug abusers in a rehabilitated situation in other parts of the country, as corroborated in Andersen and Berg.11 Preparation during residential treatment seems to contribute to the stability of substance abusers entering school or work. Both halfway houses and follow-up through continued contact with the therapeutic community and regular post-release rituals may have been aspects of stabilization.
Treatment and rehabilitation for drug addiction in therapeutic communities in Norway are free of charge. As shown here, there may be a substantial benefit to be earned through the outcome shown, in which otherwise continued imputed costs of drug abuse are halted. The financial options for drug addicts in Norway may have contributed to recruitment of drug abusers who would not have been treated in payment-related facilities. It is tempting to suggest that more heavily addicted persons are recruited this way. On the other hand, the compulsory membership in the National Insurance System of all Norwegian citizens contributes to a wider range of vocational and treatment/rehabilitation possibilities even for the poorest addicts.
Footnotes
Dr. Berg reports no financial affiliation or other relationship relevant to the subject matter of this article.
REFERENCES
- Fleming MF, Barry KL, and Manwell LB. et al. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997 277:1039–1045. [PubMed] [Google Scholar]
- Fugelstad A, Annell A, and Rajs J. et al. Mortality and causes and manner of death among drug addicts in Stockholm during the period 1981–1992. Acta Psychiatr Scand. 1997 96:169–175. [DOI] [PubMed] [Google Scholar]
- Ghodse H, Oyefeso A, Kilpatrick B.. Mortality of drug addicts in the United Kingdom 1967–1993. Int J Epidemiol. 1998;27:473–478. doi: 10.1093/ije/27.3.473. [DOI] [PubMed] [Google Scholar]
- Berg JE, Andersen S.. Mortality 5 years after detoxification and counselling as indicated by psychometric tests. Subst Abus. 2001;22:1–10. doi: 10.1080/08897070109511441. [DOI] [PubMed] [Google Scholar]
- Waal H.. Overstating the case: methodological comments on “The effects of harm reduction in Amsterdam” by Buning and van Brussel. Eur Addict Res. 1997;3:199–204. [Google Scholar]
- Project Match Research Group. Matching alcoholism treatment to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Ravndal E, Vaglum P. Why do drug abusers leave the therapeutic community? problems with attachment and identification in a hierarchical therapeutic community. Nord J Psychiatry. 1994 48suppl 33. 1–55. [Google Scholar]
- Ravndal E, Vaglum P, Skjei EH.. Bruk av behandlingstiltak blant stoffmisbrukere over en 5-årsperiode: en prospektiv undersøkelse av en hjelpesøkende kohort. Nordisk Alkohol Narkotikatidskrift. 2001;18:153–162. [Google Scholar]
- Greenland S.. Response and follow-up bias in cohort studies. Am J Epidemiol. 1977;106:184–187. doi: 10.1093/oxfordjournals.aje.a112451. [DOI] [PubMed] [Google Scholar]
- Rothman KJ. Modern Epidemiology. Boston, Mass: Little, Brown and Company. 1986 [Google Scholar]
- Andersen S, Berg JE.. The use of a sense of coherence test to predict drop-out and mortality after residential treatment of substance abuse. Addict Res Theory. 2001;9:239–251. [Google Scholar]
- Leon GD, Inciardi JA, Martin SS.. Residential drug abuse treatment research: are conventional control designs appropriate for assessing treatment effectiveness? J Psychoactive Drugs. 1995;27:85–91. doi: 10.1080/02791072.1995.10471676. [DOI] [PubMed] [Google Scholar]
- Leon GD.. Residential therapeutic communities in the mainstream: diversity and issues. J Psychoactive Drugs. 1995;27:3–15. doi: 10.1080/02791072.1995.10471668. [DOI] [PubMed] [Google Scholar]
- Andersen S, Berg JE, and Bjerkedal T. et al. Norske stoffmisbrukeres dødelighet etter innleggelse i ulike typer institusjoner (Ten year mortality among Norwegian drug addicts). Tidsskr Nor Lægeforen. 1996 116:2912–2916. [PubMed] [Google Scholar]
- Rossow I, Kielland KB.. Dødelighet blant stoffmisbrukere i Norge. Tidsskr Nor Lægeforen. 1995;115:1050–1054. [PubMed] [Google Scholar]
- Anthony WA, Cohen M, Farkas M.. A psychiatric rehabilitation treatment program: can I recognize one if I see one? Community Ment Health J. 1982;18:83–96. doi: 10.1007/BF00754453. [DOI] [PubMed] [Google Scholar]
- Andersen S, Berg JE.. Rational drop-out from substance abuse treatment as a means to minimize personally felt risk. Addict Res. 1997;5:507–518. [Google Scholar]
- Berg JE, Andersen S.. Drug addict rehabilitation: a burden on society? Int J Rehabil Res. 1992;15:301–309. [PubMed] [Google Scholar]
- Kaplan C, Broekaert E, Morival M.. Improving social psychiatric treatment in residential programmes for emerging dependence groups in Europe: cross-border networking, methodological innovations and substantive discoveries. Int J Soc Welfare. 2001;10:127–133. [Google Scholar]
- Broekaert E, Soyes V, and Vanderplasschen W. et al. The videotaped addiction challenge tool: a new instrument for qualitative substance abuse assessment, treatment planning and research in therapeutic communities. Int J Soc Welfare. 2001 10:134–141. [Google Scholar]