Abstract
Patients living with HIV/AIDS face large societal and medical challenges. Inviting patients to read their doctors’ visit notes via secure electronic portals may empower patients and improve health. We investigated whether utilization and perceptions about access to doctors’ notes differed among doctors and patients in an HIV/AIDS clinic versus primary care setting. We analyzed pre- and 1-year postintervention data from 99 doctors and 3819 patients. HIV clinic patients did not report differences in perceived risks and benefits compared to primary care clinic patients, however, they were more likely to share notes with friends (33% versus 9%, P = .002), other health professionals (24% versus 8%, P = .03), or another doctor (38% versus 9%, P < .0001). HIV clinic doctors were less likely than primary care doctors to change=the level of candor in visit notes (P < .04). Our findings suggest that HIV clinic patients and doctors are ready to share visit notes online.
Keywords: human immunodeficiency virus (HIV), visit notes, electronic health records, health information technology, personal health records
Background
Patients living with HIV/AIDS face large societal and medical challenges. Inviting patients to read their doctors’ visit notes via secure electronic portals may empower patients and improve health. The availability of online electronic medical records is rapidly increasing, and has the potential to enhance patient engagement in their health care.1-4 Free, easy-to-access online medical records greatly simplify sharing health information with patients, and early reports indicate that patients want access to their medical records, including doctor's visit notes.2,5,6 Online medical records provide patients and potentially their caregivers the ability to easily view and track laboratory values, clinic notes, test results, and medication adherence. Patient–doctor communication is enhanced,4 potentially allowing earlier intervention when a problem is encountered.
Access to online medical records may be particularly advantageous for patients living with HIV/AIDS. Research has shown that active self-management and access to accurate health information improves outcomes for HIV-infected patients7,8 and that patients with chronic diseases and those with episodic needs for extensive care may benefit the most from access to medical records.6,9,10 However, few studies have explored the utilization of online medical records among patients living with HIV/AIDS. In a pioneering study, Kahn et al5 developed an Internet-based personal health record system for 211 patients at San Francisco General Hospital's HIV/AIDS clinic. More than 80% of participants reported that online access to their electronic medical record helped them better manage their medical problems, and 71% reported being satisfied or very satisfied with the online system. Another study of approximately 7000 HIV-positive adults with access to a shared online medical record portal found that slightly more than half of HIV-positive patients used at least 1 portal feature in the first 3 years after implementation.11 The most common online portal functions used by patients included communicating with providers, obtaining medication refills, scheduling appointments, and viewing medical test results.
Despite many useful features of online access to doctor's visit notes, HIV-positive patients are a potentially vulnerable population and may present specific challenges for shared notes. Adults with mental health issues and substance abuse have been disproportionately affected by the HIV/AIDS epidemic,12,13 heightening concerns about privacy and security and possible deleterious effects for patients reading notes containing such sensitive information. Although possible downsides exist, the shift toward easily accessible online medical records is ongoing and is increasing the expectation for both patients and providers, regardless of their diagnosis.
The OpenNotes study offered patients online access to their doctor's visit notes and medical records and evaluated the perceptions and opinions of patients and their doctors.1,2,14,15 In this article, we report perceptions and characteristics associated with utilization of online visit notes among HIV clinic patients and their doctors in an urban HIV/AIDS clinic compared to patients and doctors in 3 primary care practices in the United States. This is the first study to evaluate online access to full clinic visit notes, rather than visit summaries, among HIV clinic patients, and the first to report perceptions and opinions about online access to doctor's visit notes among HIV clinic patients compared to general care patients.
Methods
Setting
The study methods have been described in detail previously.15 Briefly, the OpenNotes study included primary care practices at Beth Israel Deaconess Medical Center (BIDMC) in Boston, Massachusetts; Geisinger Health Systems (GHS) in Danville, Pennsylvania; the Adult Medicine Clinic at Harborview Medical Center (Seattle, Washington); and the HIV/AIDS clinic affiliated with the University of Washington Center for AIDS Research (Seattle, Washington). The HIV clinic is managed by Harborview Medical Center, a county-owned, safety-net hospital, that provides care to a broad spectrum of patients including the county's uninsured, incarcerated, and homeless patients.16 The HIV clinic is one of 20 HIV/AIDS research centers funded by the National Institutes of Health17 and is the largest single provider of care to patients living with HIV/AIDS in the northwestern United States.18 The clinic operates as a full-service medical home for HIV-positive patients and includes psychiatric, pharmacy, nutritional, and social welfare services.
We compared the results from pre- and postintervention surveys of patients and doctors at the primary care clinics to patients and doctors at the HIV clinic. All study procedures were approved by the institutional review boards of the University of Washington, BIDMC and GHS.
The Intervention
Prior to the start of the study, patients at BIDMC and GHS had established electronic patient portals, which included access to problem lists, medication records, and laboratory and radiology reports. During the 1-year intervention, BIDMC and GHS patients of participating doctors were also given access to their full visit notes. Patients at the HIV and Adult Medicine clinics at Harborview Medical Center had no previous access to online medical records. During the study, an internally developed patient portal provided Harborview participants with access to their primary care doctor's full clinic visit notes, laboratory, pathology, radiology and cardiology test results.
Recruitment of Doctors and Patients
At BIDMC and GHS, patients of participating doctors registered on the patient portal for at least 1 year were eligible for study participation (n = 22 426). At Harborview, eligibility required that a patient could communicate in English and have a current e-mail address. At the HIV clinic, only patients currently enrolled in a clinic-managed HIV research registry were approached for the study. More than 80% of HIV clinic patients are registry members.
Pre- and Postintervention Surveys: Instrument Development and Data Collection
The pre- and postintervention surveys used standardized and verified questions15,19,20 and were selected based on themes that arose from focus group discussions.14,15 As often as possible, the patient and physician surveys used parallel questions to address issues about the anticipated (preintervention survey) and actual (postintervention survey) benefits and risks of patient access to online visit notes. After the 1-year intervention, we resurveyed patients and doctors using similar questions about their experience viewing their doctor's visit notes. We used a 4-point Likert scale (disagree/somewhat disagree/somewhat agree/agree) for most questions. The full physician and patient survey instruments are available on request.
Analysis
Patient and physician demographics and characteristics were obtained from administrative records and baseline survey responses. Pearson chi-square tests, Fisher exact test, and Freeman-Halston extension of Fisher exact tests were conducted to compare characteristics of patients and doctors from the HIV clinic and primary care clinics. Patient activity on the portal was aggregated on a per day unit. Multiple logins or views of health information on a single date were registered as 1 unit for analysis. Survey response options “Agree”/“Somewhat agree” and “Disagree”/“Somewhat disagree” were pooled for analysis. Modified Poisson regression models were performed to estimate the relative risk of the association between clinic patients (HIV clinic patients versus primary care clinic patients) in relation to survey responses, adjusted for clinic, site, age, gender, race, and education level. HIV laboratory values were based on test results closest to the patient's date of enrollment in the study. Status of AIDS was defined by International Classification of Diseases, Ninth Revision code 042.9. Statistical analysis was performed using SAS software, version 9.3 (SAS Institute, Cary, North Carolina).
Results
A total of 113 doctors enrolled in the study and 99 (88%) completed both the pre- and postintervention surveys (28 from the HIV clinic and 71 from the primary care clinics). Among the 13 564 enrolled patients at all clinics who had at least 1 doctor's note available during the intervention period, 11 155 (82%) viewed at least 1 note. A total of 3819 (34%) patients (n = 63, 72% HIV clinic patients and n = 3756, 34% primary care clinic patients) who viewed at least 1 note during the intervention period and completed a pre- and postintervention survey, and the 99 doctors who completed a pre- and postintervention survey, were selected for this analysis.
Patient Characteristics
HIV clinic patients were younger, more likely to be male, non-white, unemployed, and have fewer years of education compared to their counterparts in the primary care clinics (P < .0001; Table 1). Of the 63 HIV clinic patients, 40 (63%) had a diagnosis of AIDS. The distribution of CD4 counts among the HIV clinic patients were as follows: ≤200 cells/mm3 (52% of patients); 201 to 499 cells/mm3 (19%), and ≥500 cells/mm3 (29%). Approximately half (48%) had an RNA test for HIV viral load on record and of these, all patients had undetectable HIV RNA (<40 copies/mL), indicating likely use of antiretroviral medications.
Table 1.
Characteristics of HIV Clinic and Primary Care Clinic Patients Who Had Access to the OpenNotes Intervention.a
| Study Sites |
|||
|---|---|---|---|
| Patient Characteristics | HIV Clinic, N = 63 (%) | Primary Care Clinics, N = 3756 (%) | P b |
| Age at baselinec | |||
| 18-29 | 1 (2) | 135 (3) | <.0001 |
| 30-39 | 8 (13) | 324 (9) | |
| 40-49 | 27 (43) | 66 (18) | |
| 50-59 | 23 (36) | 1248 (33) | |
| ≥60 | 4 (6) | 1387 (37) | |
| Gender | |||
| Female | 5 (8) | 2268 (60) | <.0001 |
| Male | 58 (92) | 1488 (40) | |
| Race | |||
| White | 48 (76) | 3441 (92) | <.0001d |
| Black or African American | 5 (8) | 69 (2) | |
| Other or multiracial | 8 (13) | 188 (5) | |
| Unknown | 2 (3) | 58 (1) | |
| Currently employede | 25 (40) | 2403 (64) | <.0001 |
| Educatione | |||
| High school/GED or less | 8 (13) | 680 (18) | <.0001 |
| Some college | 35 (55) | 884 (24) | |
| College graduate | 8 (13) | 725 (19) | |
| Postcollege | 11 (17) | 1435 (38) | |
| Unknown | 1 (2) | 32 (1) | |
| Self-rated fair or poor health statuse | 12 (19) | 479 (13) | .13 |
Abbreviations: BIDMC, Beth Israel Deaconess Medical Center; GED, general equivalency diploma.
N = 3819.
P value derived from Pearson chi-square test unless otherwise noted.
One case unknown for age at BIDMC.
P value derived from Freeman-Halton extension of Fisher exact test.
Self-reported at baseline survey.
The frequency of Internet use was similar (P = .18), with 84% to 86% patients in both the HIV clinic and primary care clinics reporting that they accessed the Internet daily or almost daily. A majority (89%-95%) of patients in both clinic settings accessed the Internet from home. A higher proportion of HIV clinic participants accessed the Internet from friends’ homes (15% versus 6%, P = .008) and public libraries (22% versus 4%, P < .0001) compared to primary care patients, while a higher proportion of primary care patients accessed the Internet from computers at work (56% versus 25%, P < .0001).
Patients from the HIV clinic had lower rates of portal logins compared to patients from other clinics. The majority (78%) of patients from the HIV clinic were in the lowest quartile of portal access frequency, averaging 7 login days (standard deviation [SD] = 5) during the 1-year intervention. In comparison, the primary care patients in the lowest quartile averaged 12 login days (SD = 4) during the intervention.
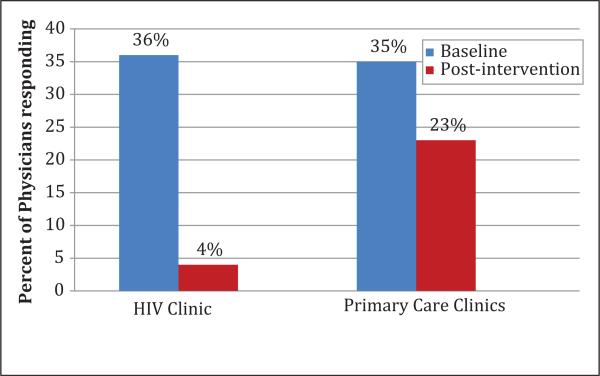
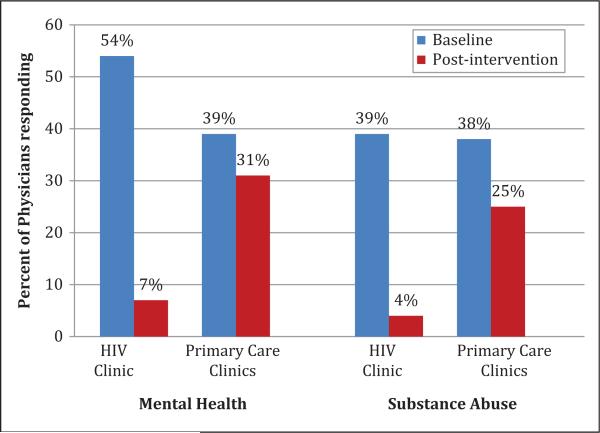
Physician Characteristics and Perceptions of Impact on Clinical Practice
Doctors at the HIV clinic were younger and more likely to provide fewer hours of direct care per week compared to their counterparts in the primary care clinics (p < .05; Table 2). Preintervention, roughly the same proportion of HIV clinic doctors and primary care clinic doctors (36% versus 35%) agreed or somewhat agreed with the statement “I will be less candid in my documentation.” However, after the 1-year intervention, a significantly lower percentage of doctors in the HIV clinic agreed with this statement (4% versus 23%, P < .04; Figure 1). After the intervention, physicians at the HIV clinic were much less likely to report that they changed the way they addressed mental health (7% versus 31%, P = .02) and substance abuse (4% versus 25%, P < .05) issues=in their notes (Figure 2).
Table 2.
Characteristics of Physicians Working at the HIV Clinic and Primary Care Clinics.
| Study Sites |
|||
|---|---|---|---|
| Physician Characteristics | HIV Clinic, N = 28 (%) | Primary Care Clinics, N = 71 (%) | P a |
| Age at baseline | |||
| 30-39 | 15 (54) | 15 (21) | .009b |
| 40-49 | 9 (32) | 26 (37) | |
| 50-59 | 4 (14) | 26 (37) | |
| ≥ 60 | 0 (0) | 4 (5) | |
| Gender | |||
| Female | 17 (61) | 30 (42) | .0976 |
| Male | 11 (39) | 41 (58) | |
| Direct care, hours per weekc | |||
| <15 | 23 (82) | 26 (37) | .0002 |
| 15-35 | 5 (18) | 34 (48) | |
| >35 | 0 (0) | 11 (15) | |
| How often doctors communicate with patients by e-mailc | |||
| Never | 0 (0) | 2 (3) | <.0001b |
| Less than once per week | 13 (46) | 7 (10) | |
| At least once per week but not daily | 15 (54) | 23 (32) | |
| At least once daily | 0 (0) | 39 (55) | |
| Percentage of entire panel with whom doctors communicate by e-mailc,d | |||
| 0-10 | 16 (57) | 17 (25) | .0246b |
| 11-25 | 7 (25) | 29 (42) | |
| 26-50 | 5 (18) | 20 (29) | |
| >50 | 0 (0) | 3 (4) | |
P values derived from Pearson chi-square test unless otherwise noted.
P value derived from Freeman-Halton extension of Fisher exact test.
Percentages displayed reflect postintervention survey responses.
No response from 2 primary care clinic physicians.
Figure 1.
Physician response to the survey question: “I will be/was less candid in Documentation.”a,b a Percentages based on doctors who completed both the baseline and postintervention survey (HIV clinic = 28; primary care clinics = 71). b Fisher exact test P < .04 for differences in postintervention survey responses between HIV clinic doctors and primary care clinic doctors.
Figure 2.
Physician response to the survey question: I will/did “change the way I address these topics in my notes.”a,b a Percentages based on doctors who completed both the baseline and postintervention survey (HIV clinic = 28; primary care clinics = 71). b Chi-square test for differences in postintervention survey responses between HIV clinic doctors and primary care clinic doctors for mental health (p = .01) and substance abuse (p = .01).
Patient Perceptions about Benefits and Risks of Access to Visit Notes
A higher proportion of HIV clinic patients reported that because of online access to their doctor's notes they would be more likely to take medications as prescribed (75% versus 67%), feel more in control of their health care (96% versus 90%), and be better prepared for visits (91% versus 80%). However, after adjusting for clinic site, age, gender, race, and education level, we observed no significant differences between HIV clinic and primary care clinic settings in regard to patients’ perceptions about potential benefits or risks of access to visit notes (Table 3). The perceived high benefit and low risk of open notes was preserved even after stratifying our results by CD4 count (ie, ≤200, 201-499, and ≥500 cells/mm; data not shown).
Table 3.
Relative Risk of HIV Clinic Patients’ Perceptions of Potential Risks and Benefits of Online Access to Doctors’ Visit Notes, Using Primary Care Patients as Reference Standard at Baseline and Postintervention.a,b
| Postintervention Surveyc |
||||
|---|---|---|---|---|
| Potential Risks and Benefits | HIV Clinic (Agree/Somewhat Agree %) | Primary Care Clinics (Agree/Somewhat Agree %) | Unadjusted RR (95% CI) | Adjusted RR (95% CI) |
| Potential Risks | ||||
| More confusing than helpful | 9 | 3 | 3.1 (1.32, 7.35) | 1.39 (0.28, 6.82) |
| Worries more | 7 | 6 | 1.22 (0.47, 3.18) | 0.46 (0.11, 1.93) |
| Concerned about privacy | 21 | 36 | 0.59 (0.35, 0.97) | 0.52 (0.26, 1.03) |
| Potential benefits | ||||
| Would take better care of self | 79 | 78 | 1.01 (0.88, 1.16) | 0.96 (0.78, 1.19) |
| Would better understand health/medical conditions | 93 | 89 | 1.04 (0.97, 1.12) | 0.98 (0.87, 1.10) |
| Would better remember plan for care | 91 | 89 | 1.02 (0.94, 1.11) | 0.98 (0.84, 1.16) |
| Would be better prepared for visits | 91 | 80 | 1.14 (1.05, 1.24) | 1.11 (0.90, 1.37) |
| Would feel more in control | 96 | 90 | 1.07 (1.02, 1.13) | 1.00 (0.90, 1.11) |
| Would be more likely to take meds as prescribedd | 75 | 67 | 1.12 (0.96, 1.31) | 1.06 (0.79, 1.43) |
Abbreviations: CI, confidence interval; RR, relative risk.
Relative risk estimates illustrate likelihood that HIV clinic patients “agreed” or “somewhat agreed” with statements regarding the potential risks and benefits of patient access to visit notes, using primary care clinic patients as the referent group.
Relative risk adjusted for the following covariates: clinic site, age, gender, race, and education level.
Patients who responded “Don't know” ranged from 3% to 7%.
Among patients who reported taking medications (n at postintervention = 3149).
The survey responses also did not reveal differences between HIV and primary care clinic participants in regard to patients’ confidence in knowing what to ask their doctor. In both settings, access to notes did not change the already-positive relationship patients had with their doctors or their sense about their overall communication with doctors. On a 10-point sliding scale, with higher scores indicating higher confidence about patient–doctor communication, the median score among patients, including those in the HIV clinic, was between 8 and 9. At baseline and postintervention, a majority of participants in both clinic settings reported that their doctor “always/almost always” explained things in a way that was easy to understand (range, 84%-93%). Likewise, most participants reported that their doctor always/almost always told them what to do about bothersome symptoms (range, 79%-94%).
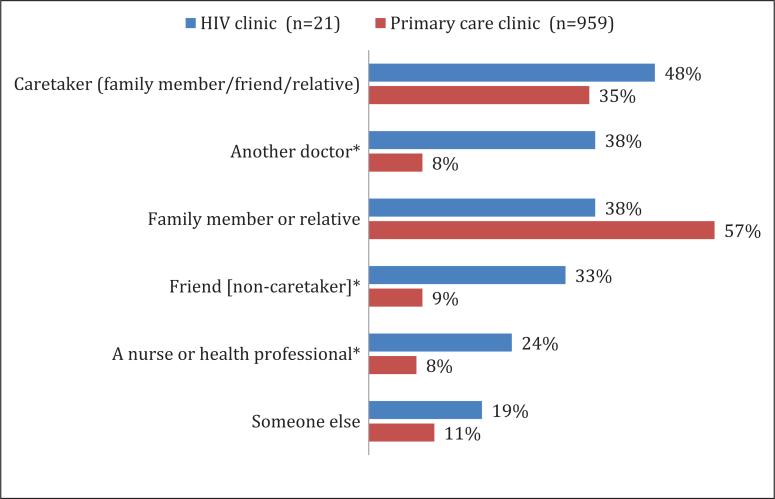
Sharing Visit Notes
HIV clinic patients were more likely than primary care clinic patients to report sharing or discussing their visit notes with a noncaretaker friend (33% versus 9%, P = .002), a nurse or health professional (24% versus 8%, P = .03), or another doctor (38% versus 8%, P < .001; Figure 3).
Figure 3.
Patient response to postintervention survey question: “With whom did you share or discuss the note?”a,b
a Figure results restricted to participants who answered the postintervention survey question “Did you show or discuss your visit notes with other people?” b Chi-square test differences between HIV clinic patients and primary care clinic patients for caretakers (p .3), family member/ relative (p = .08), “someone else” (p = 0.2, Fisher exact test). *P value <.05 (Fisher exact test).
Discussion
In our study, we found no differences between HIV clinic and primary care clinic patients in regard to patient–doctor communication or perceived benefits and risks of electronic access to doctor's visit notes. HIV-positive patients were more likely to share their visit notes with friends and health professionals. Because doctor's notes include detailed social and health histories, our a priori hypothesis was that, at baseline, HIV clinic patients would be more concerned than primary care patients about privacy and more worried about seeing their notes, but that after the 1-year intervention their concerns would decrease to the level reported by primary care patients. We were intrigued that HIV-positive patients had similar perceptions of potential risks and privacy concerns compared to primary care patients, given their historically stigmatizing condition, overall lower socioeconomic and disadvantaged backgrounds, and higher likelihood of accessing the Internet from a friend's home or public library. However, the HIV-positive patients in our population were younger and presumably more accustomed to social networking with potentially fewer boundaries on sharing what older patients may consider sensitive information. Patients from the HIV clinic had fewer portal logins compared to primary care clinic patients,but this may be due to the lower number of portal options, such as messaging features and appointment requests which were not available to patients at the HIV clinic.
Some, but not all,2 previous studies haveindicated that patients with lower socioeconomic status are less likely to engage in patient portals where electronic health records are shared20,21 and that minority patients are more concerned about the privacy of online patient portals.22 Thus, our results differed from previous reports in this regard and from our original hypothesis. Given the complexity of HIV treatment and the importance of self-management, the potential benefits of online access to visit notes may outweigh concerns about privacy or anxiety that the notes will be more confusing than helpful. This study demonstrates that even the most vulnerable patients such as those in an HIV clinic population can derive the same benefits with no increase in harm.
Our study was not designed to directly evaluate medication adherence, yet 75% of HIV-positive patients reported that they were more likely to take their medications as prescribed representing a large potential benefit. This is particularly important in the context of antiretroviral medications which historically tendto be complicated, and for which nonadherence can have particularly dire clinical and public health implications.In light of the fact that aggressive measures such as directly observed therapy and other community-based initiatives have been attempted in an effort to improve adherence, something as simple as offering electronic access to visit notes and allowing patients to share these notes with family and caretakers, offers promise. Although it is plausible that the effect is heightened by self-report, patients in focus groupscorroborated our findings, suggesting thatbeing able to read doctors’ notes provided a better understanding of what the medication was for and greatly helped with actually taking it. Focus group participants commented that reading the doctor's note was like “another person reminding you to take your meds.”2 Finally, patient satisfaction with OpenNotes was quite highand is an important aspect of patient care. Patients living with HIV/AIDS want to be involved in their care plan, and patient–provider communication and patient satisfaction are important factors in HIV medication adherence.23,24
Although patients have long had legal access to their medical charts, doctors, at least initially, are often more skeptical than patients about the potential benefits of open access.2,25-27 Some worry that providers will become more circumspect in how and what they document, thereby damaging communication among doctors and between doctors and patients. Important information such as tentative diagnoses or useful, but potentially unpleasant, descriptions of patient characteristics could be minimized. In fact, these concerns mirrored our a priori hypothesis. We hypothesized that doctors who care for HIV clinic patients would be more concerned about sharing their notes with patients compared to those in primary care clinics. Yet, in our study HIV clinic doctors were less likely than those in the primary care clinics to report that patient access to visit notes impacted their level of candor about sensitive topics, such as substance abuse and mental health. This result must be tempered by the fact that HIV clinic providers in our study reported spending fewer hours each week providing direct care, so patient responses to their visit notes would have less impact on their overall work lives.
Strengths and Limitations
The study has several limitations. First, the relatively modest numbers of HIV-positive patients were all from a single site, and we did not assess HIV status among primary care patients. The HIV prevalence rate is <1% in the general population,28 and many HIV-positive patients seek specialized care, thus we consider this limitation to be minimal. Second, the Harbor-view Medical Center HIV clinic offers comprehensive care, and many patients in this study population have comorbid psychiatric and substance issues that may be barriers to self-care. These factors may limit comparisons with HIV-positive patients who receive care in specialized clinics. The study strengths include a large, diverse population of patients and providers from different geographic locations and health care systems, detailed assessments of patient portal utilization, including access to the full clinic note, and a pre- and postintervention design.
Conclusion
Although HIV clinic patients came from more vulnerable socioeconomic backgrounds, they did not differ from primary care patients in their perception of risks and benefits of access to their doctor's full visit notes. HIV-positive patients were more likely to share their visit notes with friends and health professionals and they did not have more privacy concerns than primary care patients. At the same time, HIV providers were as receptive to shared notes as primary care providers and were less likely to change their documentation, despite writing about sensitive topics. Electronic medical records have advanced to the point where we now have the capability, and even the expectation, of offering patients access to their doctor's visit notes. Despite the stigma and confidentiality issues historically associated with HIV, our findings suggest that HIV-positive patients and doctors are ready to engage actively in sharing visit notes online.
Acknowledgments
The authors sincerely thank Andrew Markiel, PhD, for his role in developing the online patient portal. All investigators were supported by The Robert Wood Johnson Foundation's Pioneer Portfolio grant 65921. Dr Delbanco and Ms Walker were also supported by the Drane Family Fund and the Richard and Florence Koplow Charitable Foundation. Dr Elmore was supported by the National Cancer Institute (K05 CA 104699).
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121–125. doi: 10.7326/0003-4819-153-2-201007200-00008. [DOI] [PubMed] [Google Scholar]
- 2.Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intn Med. 2012;157(7):461–470. doi: 10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mador RL, Shaw NT, Cheetham S, Reid RJ. Whose record is it anyway? Putting patients’ interests at the heart of the implementation and use of electronic medical records. Healthc Q. 2008;11(4):90–92. [PubMed] [Google Scholar]
- 4.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahn JS, Hilton JF, Van Nunnery T, et al. Personal health records in a public hospital: experience at the HIV/AIDS clinic at San Francisco general hospital. J Am Med Inform Assoc. 2010;17(2):224–228. doi: 10.1136/jamia.2009.000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartlett C, Simpson K, Turner AN. Patient access to complex chronic disease records on the Internet. BMC Med Inform Decis Mak. 2012;12:87. doi: 10.1186/1472-6947-12-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalichman SC, Benotsch EG, Weinhardt LS, Austin J, Luke W. Internet use among people living with HIV/AIDS: Association of health information, health behaviors, and health status. AIDS Educ Prev. 2002;14(1):51–61. doi: 10.1521/aeap.14.1.51.24335. [DOI] [PubMed] [Google Scholar]
- 8.Gifford AL, Groessl EJ. Chronic disease self-management and adherence to HIV medications. J Acquir Immune Defic Syndr. 2002;31(suppl 3):S163–S166. doi: 10.1097/00126334-200212153-00016. [DOI] [PubMed] [Google Scholar]
- 9.Pagliari C, Detmer D, Singleton P. Potential of electronic personal health records. BMJ. 2007;335(7615):330–333. doi: 10.1136/bmj.39279.482963.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MarkleFoundation [March 2014];Americans Overwhelmingly Believe Electronic Personal Health Records Could Improve Their Health. http://www.markle.org/publications/401-americans-overwhelmingly-believe-electronic-personal-health-records-could-improve-t.
- 11.Ralston JD SM, Grothaus L, Leyden WA, et al. Use of Web-based shared medical records among patients with HIV. Am J Manag Care. 2013;19(4):e114–e124. [PMC free article] [PubMed] [Google Scholar]
- 12.Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 13.Meade CS, Sikkema KJ. HIV risk behavior among adults with severe mental illness: a systematic review. Clin Psychol Rev. 2005;25(4):433–457. doi: 10.1016/j.cpr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Dhanireddy S, Walker J, Reisch L, Oster N, Delbanco T, Elmore JG. The urban underserved: attitudes towards gaining full access to electronic medical records. Health Expect. 2012;15:1369–7625. doi: 10.1111/j.1369-7625.2012.00799.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leveille SG, Walker J, Ralston JD, Ross SE, Elmore JG, Delbanco T. Evaluating the impact of patients’ online access to doctors’ visit notes: designing and executing the opennotes project. BMC Med Inform Decis Mak. 2012;12:32. doi: 10.1186/1472-6947-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheffield JV, Young A, Goldstein EA, Logerfo JP. The public hospital mission at Seattle's Harborview medical center: high-quality care for the underserved and excellence in medical education. Acad Med. 2006;81(10):886–890. doi: 10.1097/01.ACM.0000238118.63470.5b. [DOI] [PubMed] [Google Scholar]
- 17.National Institutes of Health [March 2014];Centers for AIDS Research (CFAR) http://www.niaid.nih.gov/labsandresources/resources/cfar/Pages/default.aspx.
- 18.Fredericksen R, Tufano J, Ralston S, et al. Integrating a web-based, patient-administered assessment into primary care for HIV-infected adults. J AIDS HIV Res. 2012;4(2):47–55. doi: 10.5897/jahr11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46(7):889–894. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 20.Roblin DW, Houston TK, 2nd, Allison JJ, Joski PJ, Becker ER. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc. 2009;16(5):683–689. doi: 10.1197/jamia.M3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE). J Health Commun. 2010;15(suppl 2):183–196. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vodicka E, Leveille SG, Ralston JD, et al. Online medical records and doctors’ notes: Patient concerns about privacy. J Intern Med Res. 2013;15(9):e208. doi: 10.2196/jmir.2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roberts KJ. Physician-patient relationships, patient satisfaction, and antiretroviral medication Adherence among HIV-infected adults attending a public health clinic. AIDS Patient Care STDs. 2002;16(1):43–50. doi: 10.1089/108729102753429398. [DOI] [PubMed] [Google Scholar]
- 24.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19(11):1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorr DA, Rowan B, Weed M, James B, Clayton P. Physicians’ attitudes regarding patient access to electronic medical records. AMIA Annu Symp Proc. 2003:832. [PMC free article] [PubMed] [Google Scholar]
- 26.Ross AP. The case against showing patients their records. Br Med J. 1986;292(6520):578. doi: 10.1136/bmj.292.6520.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Earnest MA, Ross SE, Wittevrongel L, Moore LA, Lin CT. Use of a patient-accessible electronic medical record in a practice for congestive heart failure: patient and physician experiences. J Am Med Inform Assoc. 2004;11(5):410–417. doi: 10.1197/jamia.M1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Denning PDE. [March 2014];Communities in Crisis: Is There a Generalized HIV Epidemic in Impoverished Urban Areas of the United States? http://www.cdc.gov/hiv/risk/other/poverty.html.