Abstract
Stomach cancer is one of the most common cancers in Korea. The aim of this study was to identify the association between the prevalence of cancer, particularly stomach cancer, and the amount of 24-hr urine sodium excretion estimated from spot urine specimens. The study included 19,083 subjects who took part in the Korean National Health and Nutritional Examination Survey between 2009 and 2011. The total amount of urine sodium excreted in a 24-hr period was estimated by using two equations based on the values for spot urine sodium and creatinine. In subjects who had an estimated 24-hr urine sodium excretion of more than two standard deviations above the mean (group 2), the prevalence of stomach cancer was higher than in subjects with lower 24-hr sodium excretion (group 1). By using the Tanaka equation to estimate it, the prevalence of stomach cancer was 0.6% (114/18,331) in group 1, whereas it was 1.6% (9/568) in group 2 (P=0.006). By using the Korean equation, the prevalence was 0.6% (115/18,392) in group 1, and 1.6% in group 2 (8/507) (P=0.010). By using the Tanaka equation, breast cancer in women is more prevalent in group 2 (1.9%, 6/324) than group 1 (0.8%, 78/9,985, P=0.039). Higher salt intake, as defined by the estimated amount of 24-hr urine sodium excretion, is positively correlated with a higher prevalence of stomach or breast cancer in the Korean population.
Graphical Abstract
Keywords: 24-Hour Urine Sodium, Spot Urine Sodium, Cancer
INTRODUCTION
Stomach cancer is one of the world's most common cancers, and it is also one of the major causes of cancer-related death; it is the fourth most common cancer diagnosed in men worldwide, with an expected incidence of 640,000 cases, and it is the fifth most common cancer diagnosed in women, with an expected incidence of 350,000 cases in 2011 (1). It is estimated that 464,000 men and 273,000 women will have died from stomach cancer in 2011 (1). In 2010, stomach cancer was the second most common cancer diagnosed in Korea, after thyroid cancer (2). In 2011, stomach cancer caused 9,719 deaths in Korea, and it was the second most frequent cause of cancer death (2).
There are geographic and ethnic differences in the incidence of stomach cancer around the world as well as different trends in a people over time. The changes in incidence patterns observed among immigrants indicate that stomach cancer is closely associated with modifiable factors such as diet. There are many lines of evidence suggesting that the risk of stomach cancer is associated with a high intake of salt and salt-preserved foods (3). However, while the geographic variation in stomach cancer mortality in Japan is not correlated with individual salt consumption (4), a study by Tsugane et al. (5) in Japan showed an almost linear correlation between the cumulative mortality rate of gastric cancer and 24-hr urine sodium excretion levels. Because estimating sodium intake by using dietary surveys is difficult, measuring 24-hr urine sodium excretion has become the preferred method in population surveys (6, 7). However, 24-hr urine collections are expensive and relatively tedious for study participants; estimating sodium excretion from spot urine specimens is more economical and less burdensome.
In this study, we estimated 24-hr urine sodium excretion by using spot urine specimens from a Korean study population. We also assessed the association between the estimated level of 24-hr urine sodium excretion and cancer history, including stomach cancer.
MATERIALS AND METHODS
Study population
This study was based on the Korean National Health and Nutritional Examination Survey performed between 2009 and 2011, which included individuals from all over the country. Of these survey participants, 44.9% lived in seven major cities (Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan), and the rest lived in relatively small towns. From a total of 29,235 participants, adults aged ≥20 yr and who had casual urine sodium and creatinine data were selected (n=19,132). Of these, participants without data about height, weight, or sex were excluded, and 19,083 subjects were finally assessed.
Demographic findings and nutritional information
We used a general questionnaire survey and a 24-hr dietary recall and food frequency questionnaire to obtain demographic, social, and nutritional information. The assessed general characteristics included age; sex; past and present medical history including six types of cancers, chronic kidney disease (CKD), diabetes mellitus (DM), hypertension (HTN), ischemic heart disease (IHD), cerebrovascular accident (CVA), liver cirrhosis (LC); smoking and drinking habits; occupational status; education level; marital status; residence home ownership status; household income; and health insurance type. The 24-hr recall was based on the food intake on a single weekday, and the nutrients were quantified by using the Database Management System (Korea Health Industry Development Institute). For a single 24-hr recall, supplementary tools such as food models and two-dimensional food volumes and containers were used.
Measurements
During the survey, a random urine sample (early morning, if possible) was collected. The collected urine was refrigerated and transported to the central laboratory within 24 hr. Urine sodium and potassium levels were measured by using an ion-selective electrode method. Serum and urine creatinine levels were measured by using the Jaffe reaction with an automatic analyzer (ADVIA 1650 system; Bayer Health Care, Tarrytown, NY). The estimated glomerular filtration rate (eGFR) was calculated by using the Modification of Diet in Renal Disease study equation (8). The height and weight were measured while the participant was wearing light clothing and no shoes. Body mass index (BMI) was computed as the weight (kg) divided by the square of the height (m2). Blood pressure (BP) was measured by using the standard protocol, as follows: three readings were obtained with a mercury sphygmomanometer, and the average of the second and third readings was considered as the final BP.
Definitions
HTN was defined as a systolic blood pressure (SBP) of ≥140 mmHg, diastolic blood pressure (DBP) of ≥90 mmHg, a self-reported history of HTN, or the administration of antihypertensive medications. DM was defined as a fasting glucose of ≥126 mg/dL, a self-reported history of DM, or use of hypoglycemic agents. CKD was defined as eGFR of <60 mL/min/1.73 m2 (9).
We classified the subjects into four groups according to the status of their cancer diagnosis: Present; current illness, Recent, <5 yr since diagnosis; Remote, >5 yr since diagnosis; or no diagnosis.
We classified the subjects into four groups (E24UNA_T4 or E24UNA_K4) according to their estimated level of 24-hr urine sodium excretion. On the basis of the average values estimated by using the equation described by Tanaka et al. (10) and by using Korean equation, we added and subtracted values as much as two standard deviations (SD), and we classified the subjects into four groups [24-hr urine sodium excretion by Tanaka equation (E24UNA_T4): 71.0, 144.0, 261.0 mEq/day, 24-hr urine sodium excretion by Korean equation (E24UNA_K4): 95.0, 167.0, 240.0 mEq/day]. We further reclassified the four groups into two groups (E24UNA_T2 or E24UNA_K2) as follows: groups 1-3 [lower than average + 2 standard deviations (SD)] were classified as the first group, and the fourth group (more than average + 2 SD) was classified as the second group.
We also classified the subjects into four groups according to their sodium intake, as estimated by the dietary questionnaire. On the basis of the average values and added and subtracted values as much as 2 SD, we classified the subjects into four groups (E24INTAKE4) [2.14, 4.91, 9.20 g/day=93, 213, 400 mEq/day].
Tanaka equation
Estimated 24 hr urine creatinine (E24UCR, mg/day)=-2.04×age (yr) + 14.89×weight (kg) + 16.14×height (cm) - 2,244.45
E24UNA_T=21.98×XNA0.392, XNA={spot urine sodium (mEq/L)/[10×spot urine creatinine (mg/dL)]}×E24UCR
Korean equation
E24UCR_K=-7.428×age (yr) + 10.372×weight (kg) + 15.631×height (cm)-1234.758
E24UNA_K=28.985×XNA0.346, XNA={spot urine sodium (mEq/L)/[10×spot urine creatinine (mg/dL)]}×E24UCR_K
Statistical analyses
All analyses were performed by using SPSS statistical software (SPSS version 18.0, Chicago, IL, USA). Data are presented as the mean±SD for continuous variables, and as proportions for categorical variables. Differences in the continuous variables were analyzed by performing one-way analysis of variance, and differences in categorical variables were assessed with the Pearson chi-squared tests. We analyzed the independent factors related to cancer history with multivariable logistic regression analysis. Factors that were included in the analysis were demographic data (age, sex), past or present medical history (history of one of the six cancers included in the survey, CKD, DM, HTN, IHD, CVA, and LC), social history (exercise habits, smoking, alcohol consumption, occupational status, education level, marital status, residence home ownership status, household income, health insurance type, and basic livelihood security recipient status), physical examination (SBP and DBP, weight, height, waist circumference, and BMI), estimated 24-hr urine sodium excretion. Analysis of covariance (ANCOVA) was used to adjust independent factors related to cancer history. P values of <0.05 were considered statistically significant.
Ethics statement
This study was approved by the institutional review board of Centers for Disease Control and Prevention in Korea.
RESULTS
Subject characteristics (Table 1)
Table 1.
Overall characteristics of participants in this study
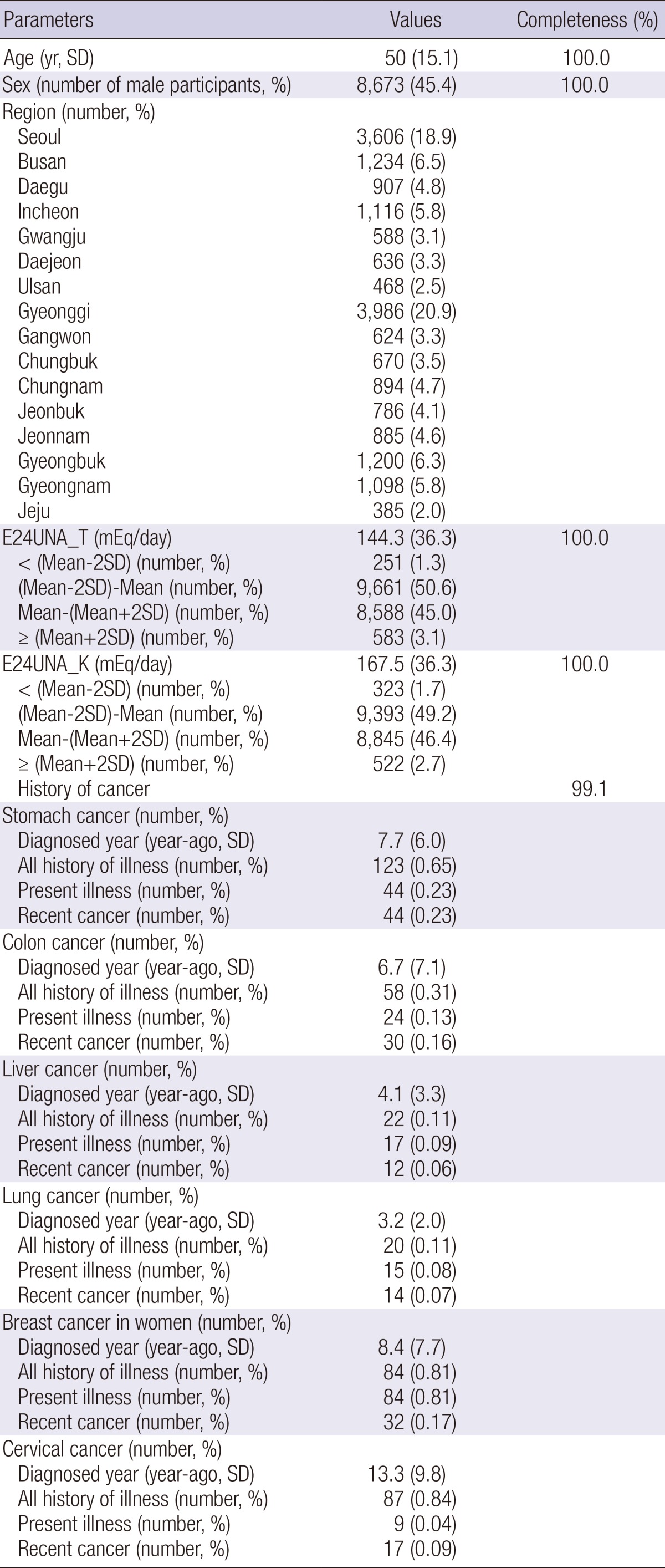
Completeness: completeness of data among participants, E24UNA_T: estimated value of 24-hr urine sodium amount with the equation proposed by Tanaka et al., E24UNA_K: estimated value of 24-hr urine sodium amount with the equation proposed by this study. Mean-2SD: value of mean of E24UNA subtracted by 2×the standard deviation of E24UNA. Mean+2SD: value of mean of E24UNA plus 2×the standard deviation of E24UNA. Diagnosed year: time difference between current age and the age at diagnosis (yr). Present illness: participants with an illness at the time of the survey. Recent cancer: participants with cancer diagnosed within 5 yr.
The mean age of the subjects was 50.0 yr (range, 20-97 yr). Among the 19,083 subjects, 45.4% were male. The estimated 24-hr urine sodium excretion for the entire study population calculated by using the Tanaka equation (10) was 144.3±36.3 mEq/day, and 1,940 (10.2%) subjects had <100 mEq/day of sodium excretion. The overall estimated amount of 24-hr urine sodium excretion calculated by using the Korean equation was 167.5±36.3 mEq/day, and 484 (2.5%) subjects had sodium excretion values of <100 mEq/day. Among the subjects, 99.1% responded the survey on cancer history including stomach cancer, colorectal cancer, liver cancer, and lung cancer in both men and women, and breast cancer and cervical cancer in women. Of these, 123 (0.65%) subjects had a history of stomach cancer; at the time of the survey, 44 (0.23%) people had stomach cancer. Overall, the subjects with history of stomach cancer were diagnosed 7.7±6.0 yr prior to the survey; 4 people were diagnosed in the same year as the survey, 9 were diagnosed the prior year, 10 were diagnosed 2 yr prior, 8 were diagnosed 3 yr prior, 13 were diagnosed 4 yr prior, and 78 patients were diagnosed >5 yr before the survey, 1 of whom did not know when they were diagnosed.
We conducted an analysis of the dietary intake of 16,878 (88.4%) subjects. The estimated sodium intake was 4.915±1.385 g/day (213.7±60.2 mEq/day), and it was higher than the estimated value of 24-hr urine sodium excretion.
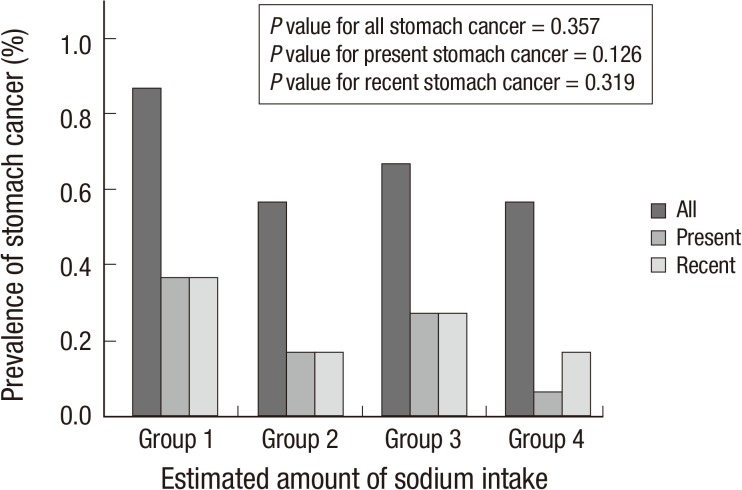
The association of cancer prevalence with sodium intake estimated by using a dietary questionnaire
We assessed the difference in cancer prevalence according to groups stratified according to their estimated dietary sodium intake (g/day). The prevalence of all cases of stomach cancer (All), current (Present) cases, and recent (Recent) cases were not significantly different among the groups stratified according to dietary sodium intake (E24INTAKE4). (Fig. 1, P>0.05). The prevalence of liver, lung, breast, and cervical cancer was not different between the dietary sodium groups.
Fig. 1.
The prevalence of stomach cancer defined by medical history according to the estimated dietary sodium intake. Group 1: dietary sodium intake of ≤ 2.140 g/day. Group 2: dietary sodium intake, 2.14-4.910 g/day. Group 3: dietary sodium intake, 4.911-9.200 g/day. Group 4: dietary sodium intake of ≥ 9.201 g/day. All: all participants with stomach cancer history. Present: participants with current stomach cancer. Recent: participants with stomach cancer diagnosed within 5 yr.
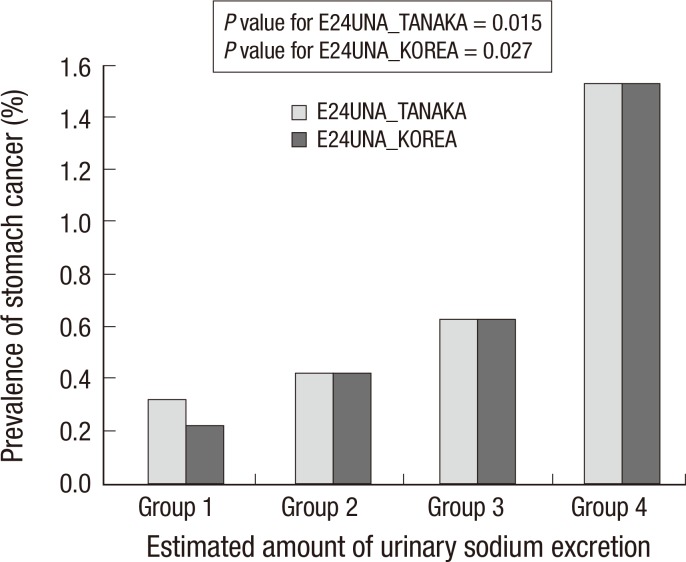
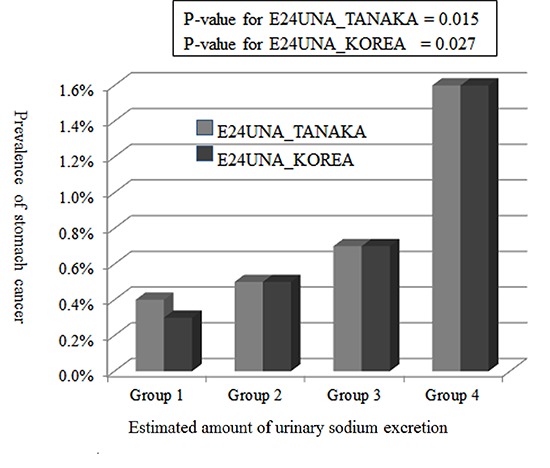
The association of cancer prevalence with estimated 24 hu Na and its groups
Univariate analysis: The Pearson Chi-squared test to determine the difference between the E24UNA and cancer groups
When we compared the differences in stomach cancer prevalence between the E24UNA_T4 and E24UNA_K4 groups, they were proportionally high according to the E24UNA level (Table 2, Fig. 2). In subjects who had an E24UNA value of 2 SD or more above the mean, the prevalence of stomach cancer increased. By using a cut-off value of 261 mEq/day of 24-hr urine sodium excretion, as estimated by using the Tanaka equation, subjects who had lower value had a cancer prevalence of 0.6% (114/18,331), whereas subjects who had higher value had a prevalence of 1.6% (9/568) (P=0.006). On the basis of the 240 mEq/day of 24-hr urine sodium estimated by using the Korean equation, the prevalence was 0.6% (115/18,392) in subjects who had lower values, whereas the prevalence was 1.6% (8/507) in subjects who had higher values (P=0.010).
Table 2.
The prevalence of stomach cancer defined by history according to the estimated 24-hr urine sodium excretion level
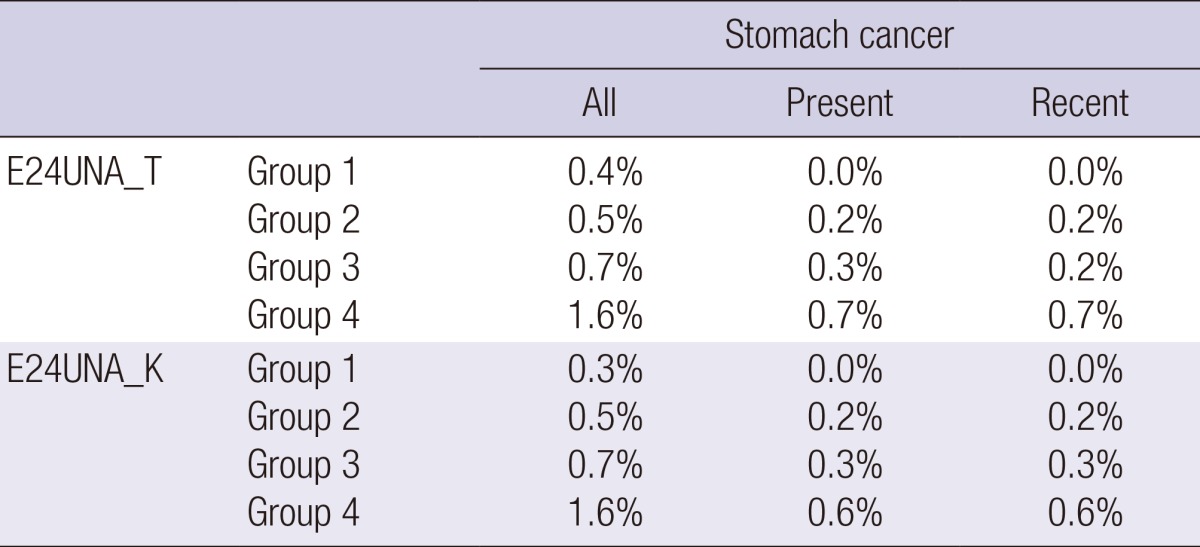
E24UNA_T: estimated 24-hr urine sodium with the equation proposed by Tanaka et al. E24UNA_K: estimated 24-hr urine sodium with the equation proposed in this study. Group 1: E24UNA of ≤71.0 mEq/day for TANAKA; E24UNA of ≤95.0 mEq/day for KOREA. Group 2: E24UNA, 71.01-144.0 mEq/day for TANAKA; E24UNA, 95.1-167.0 mEq/day for KOREA. Group 3: E24UNA, 144.1-261.0 mEq/day for TANAKA; E24UNA, 167.1-240.0 mEq/day for KOREA. Group 4: E24UNA of ≥261.1 mEq/day for TANAKA; E24UNA of ≥240.1 mEq/day for KOREA. All: all of participants with stomach cancer history. Present: participants with current stomach cancer. Recent: participants with stomach cancer diagnosed within 5 yr. P value for All stomach cancer by E24UNA_T=0.015. P value for All stomach cancer by E24UNA_K=0.027. P value for All stomach cancer between Group 1-3 and Group 4 by E24UNA_T=0.013. P value for All stomach cancer between Group 1-3 and Group 4 by E24UNA_K=0.019.
Fig. 2.
The prevalence of stomach cancer defined by medical history according to estimated 24-hr urine sodium excretion. E24UNA_TANAKA: estimated 24-hr urine sodium excretion estimated by using the equation proposed by Tanaka et al. E24UNA_KOREA: estimated 24-hr urine sodium excretion estimated by using the equation described in this study. Group 1: E24UNA of ≤ 71.0 mEq/day for TANAKA; E24UNA of ≤ 95.0 mEq/day for KOREA. Group 2: E24UNA, 71.01-144.0 mEq/day for TANAKA; E24UNA, 95.1-167.0 mEq/day for KOREA. Group 3: E24UNA, 144.1-261.0 mEq/day for TANAKA; E24UNA, 167.1-240.0 mEq/day for KOREA. Group 4: E24UNA of ≥ 261.1 mEq/day for TANAKA; E24UNA of ≥ 240.1 mEq/day for KOREA.
In addition to stomach cancer, breast cancer in women was also associated with the E24UNA groups. In the E24UNA_T4 group, the prevalence of breast cancer increased proportionally with the amount of estimated sodium excretion (Groups 1, 2, 3, and 4, were 0.0%, 0.7%, 0.9%, and 1.8%, respectively, P=0.049). In the E24UNA_T2 group, when we compared subjects who had 24-hr urine sodium excretion values of <261 mEq/day with those who had higher values, the prevalence of breast cancer was 0.8% (78/9,985) and 1.9% (6/324), respectively (P=0.039).
The prevalence of colon, liver, lung, and cervical cancer were not associated with the E24UNA groups.
Assessment of the factors associated with stomach cancer prevalence
To identify the factors related to the prevalence of stomach cancer, among the demographic data, past medical history, social history, and physical examination findings, we included only factors with more than 95% complete data in the analysis.
Univariate factors that were related to stomach cancer history included age, sex, lung cancer history, colon cancer history, 'healthcare for the poor' registration status, alcohol intake, education level, employment status, marital status, smoking history, current DM, current HTN, current CKD stage, IHD, and the E24UNA groups. On the basis of this, we configured three models and performed multivariable logistic regression analysis for the presence of stomach cancer. Among the variables, significant ones are presented in Table 3. In models adjusted for age and sex, including continuous variables, the E24UNA_K2 and E24UNA_T2 groups were significant, but in the other models, only the E24UNA_K2 group was significant. This indicates that after adjusting for all parameters that were associated with a history of stomach cancer, in subjects whose estimated level of 24-hr urine sodium excretion were determined to be >240 mEq/day by using the Korean equation, the odds ratio of the presence of stomach cancer was 2.253 (95% confidence interval [CI]: 1.028-4.939, P=0.043).
Table 3.
Multivariable logistic regression analysis for the detection of the factors related to the history of stomach cancer
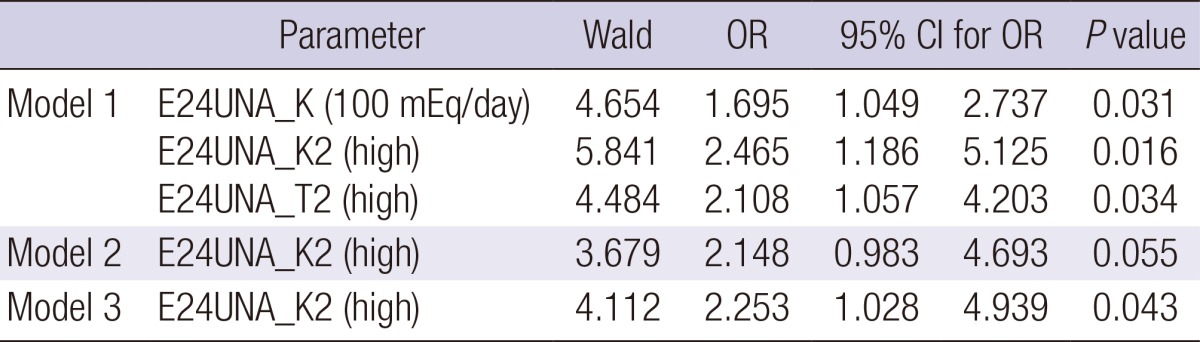
95% CI for OR: 95% confidence interval for the odds ratio. E24UNA_K: a continuous variable of the estimated 24-hr urine sodium excretion in 100 mEq/day unit, calculated with the equation created in this study. E24UNA_K2: a group of E24UNA_K stratified with a criterion of 240 mEq/day. E24UNA_K2 (high): participants with ≥241 mEq/day of E24UNA_K. E24UNA_T: a continuous variable of estimated 24-hr urine sodium in 100 mEq/day unit, calculated with the equation created by Tanaka et al. E24UNA_T2 (high): participants with ≥261 mEq/day, as calculated by using the E24UNA_T model. Model 1: logistic regression for the presence of stomach cancer adjusted for age and sex. Model 2: adjusted for age, sex, and smoking and drinking habits. Model 3: adjusted for age, sex, smoking and drinking habits, grade of household income, marital status, employment status, grade of education-year, history of ischemic heart disease, colon cancer, lung cancer, presence of diabetes mellitus, hypertension, and chronic kidney disease at the time of the survey.
Adjusted estimated 24-hr urine sodium excretion according to the presence of stomach cancer
One hundred and twenty three subjects with a history of stomach cancer were, on average, older (50.1±16.1 yr vs. 65.3±10.1 yr, P<0.001), predominantly male, with increased alcohol consumption, and a lower level of education compared to the subjects without stomach cancer history (n=18,784). There were also more subjects who were unemployed, who were recipients of basic livelihood security, and who had a lower household income. Higher number of subjects in this group had IHD, DM, and HTN, and they also had higher DBP (Table 4). In subjects with a history of stomach cancer, the estimated sodium excretion determined by using the E24UNA_T model was 153.5±41.9 mEq/day, and by using the E24UNA_ K model, it was 176.9±40.5 mEq/day; these values were higher than the values of participants without a history of stomach cancer: 144.2±36.3 and 167.5±36.2 mEq/day, respectively (P value for E24UNA_T =0.002, P value for E24UNA_K=0.005).
Table 4.
The characteristics of participants grouped according to history of stomach cancer
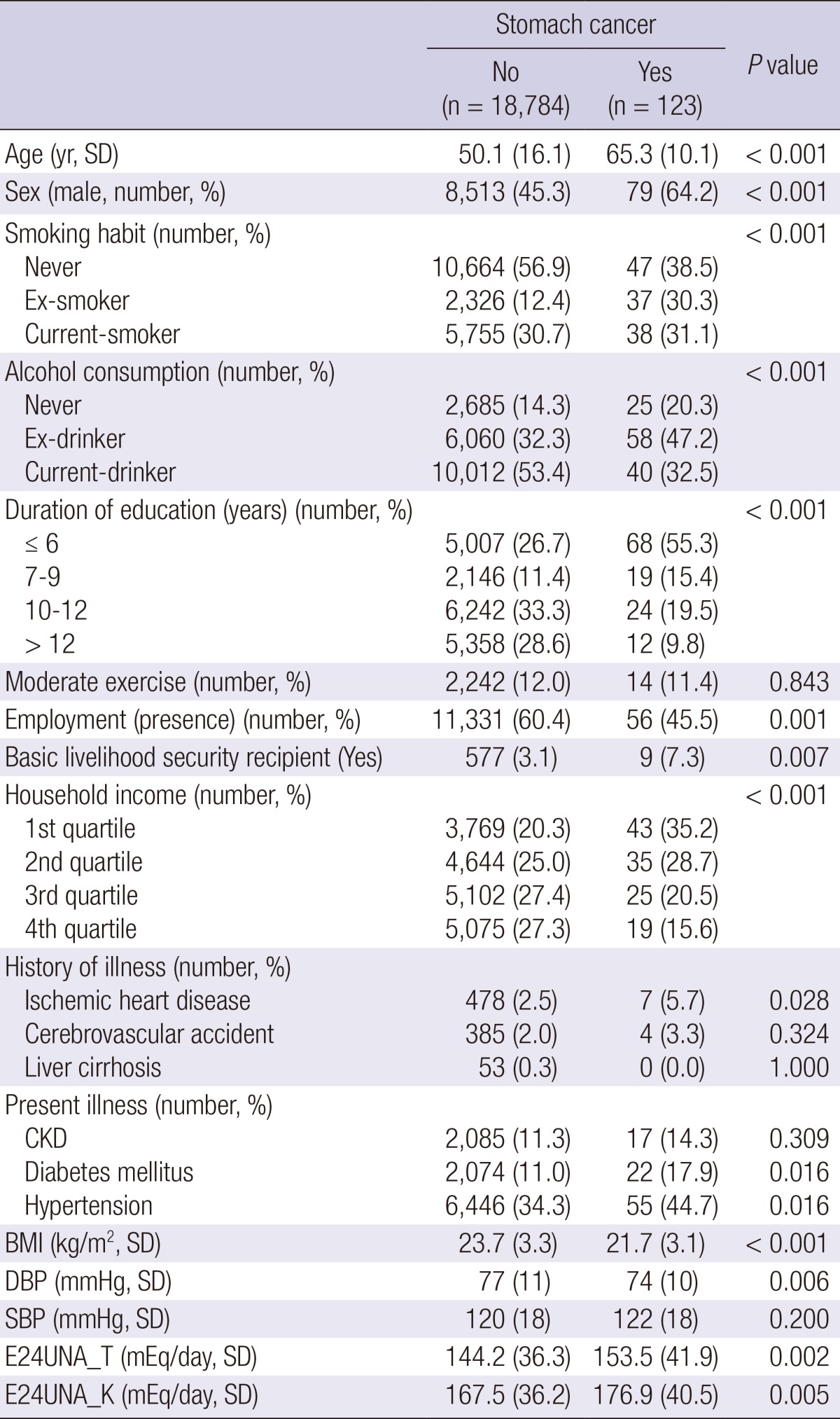
E24UNA_T: a continuous variable of estimated 24-hr urine sodium, calculated with the equation created by Tanaka et al., E24UNA_K: a continuous variable of estimated 24-hr urine sodium, calculated with the equation created in this study, Household income: Quartile group of household income defined by the Korean government according to number of household members. BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; CKD, chronic kidney disease.
Variables that were independently associated with the estimated level of 24-hr urine sodium excretion determined by using the Korean equation were age, sex, current DM, current HTN, BMI, education level, exercise ability, home ownership status, marital status, occupational status, smoking, SBP, and DBP. We adjusted the variables, and compared the estimated E24UNA_K values according to the presence or absence of a history of stomach cancer. As a result, a history of stomach cancer was significantly associated with estimated value of 24-hr urine sodium excretion (ANCOVA, P=0.004). The value of E24UNA_K was higher in subjects with a history of stomach cancer than in those without [176.6 (95% CI: 170.3-182.8) vs. 167.5 (95% CI: 167.0-168.0)]. In particular, the subjects with a present history of cancer had higher amounts of sodium excretion [185.0 (95% CI: 174.6-195.3) vs. 167.5 (95% CI: 167.0-168.0), P=0.001].
Variables that were independently associated with the estimated amount of 24-hr urine sodium excretion by using the E24UNA_ T equation also included age, sex, current DM, current HTN, BMI, education level, exercise ability, home ownership status, marital status, occupational status, smoking, SBP, and DBP. By using the same procedure, a history of stomach cancer was significantly associated with the estimated amount of 24-hr urine sodium excretion (ANCOVA, P=0.007). The E24UNA_T value was higher in subjects with a history of stomach cancer than in those without [152.8 (95% CI: 146.6-158.9) vs. 144.2 (95% CI: 143.7-144.7), P=0.001].
Assessing the probability of a history stomach cancer with the estimated amount of 24-hr urine sodium excretion by using a receiver operating characteristic curve
When we assessed the probability of stomach cancer history by using the E24UNA_K model with receiver operating characteristic analysis, the area under the curve (AUC) was 0.563 (95% CI: 0.512-0.614, P=0.016). When we assessed the probability of current history (Present) of stomach cancer, the AUC was 0.620 (95% CI: 0.540-0.700, P=0.006). When we applied the 24-hr urine sodium excretion cut-off value of ≥173.25 mEq/day as a criterion, estimated by using the E24UNA_K model, the sensitivity and specificity of predicting a current history of stomach cancer in the study subjects were 63.6% and 57.9%, respectively.
When we assessed the probability of stomach cancer history with the E24UNA_T model, the AUC was 0.561 (95% CI: 0.509-0.613, P=0.019). When we assessed the probability of a current history (Present) of stomach cancer, the AUC was 0.627 (95% CI: 0.544-0.710, P=0.004). When we applied 24-hr urine sodium excretion cut-off value of ≥153.90 mEq/day as a criterion, estimated by using the E24UNA_T model, the sensitivity and specificity of predicting a current history of stomach cancer in the study subjects were 65.9% and 62.5%, respectively.
DISCUSSION
We found that a higher rate of estimated 24-hr urine sodium excretion is associated with a history of stomach and breast cancer. Stomach and breast cancer prevalence increased proportionally with the estimated 24-hr urine sodium excretion groups.
Several studies have attempted to elucidate the association between salt consumption and stomach cancer. Honjo et al. (4) reported that there is no clear correlation between per capita salt intake and the stomach cancer mortality rate in Japan. Sjodahl et al. (11) stated that most investigations into the association between salt intake and stomach cancer have been assessed retrospectively, resulting in an inherent problem with recall bias. Few prospective studies have been undertaken, and their results are conflicting. In a U.S. cohort study, a positive association was found between salted food and the risk of stomach cancer (12). In a Japanese cohort study, a high intake of salted foods was not associated with the risk of stomach cancer (13). However, in another Japanese cohort including 93 patients with stomach cancer, a high salt intake was associated with the risk of stomach cancer (14). Tsugane et al. (15) reported that the intake of salt and salted food was dose-dependently associated with the risk of stomach cancer in a large population-based prospective study in Japan. In the Netherlands Cohort Study, 282 cases of stomach cancer were identified, and the salt intake was not associated with an increased risk for the disease (16).
One of the reasons for these controversial results may be due to the imprecise estimation of salt intake in the different studies. Rather than estimating sodium intake, measurement of 24-hr urine sodium excretion has become the preferred method for salt intake estimation in population surveys (6, 7). Although multiple 24-hr urine collections may be the ideal method to estimate salt intake, they are not feasible for large-scale prospective studies. As a result, we used spot urine specimens to estimate sodium excretion.
Tanaka et al. (10) developed a formula to estimate the 24-hr urine sodium excretion with spot urine specimens by using Japanese data from the INTERSALT study (17), and they confirmed the validity of their formula by applying the equation to an external data set. Subramanian et al. (18) also derived an equation to predict 24-hr urine sodium excretion by using spot urine specimen in a multi-ethnic Asian study population. They showed that ethnicity was an important factor for predicting the equation, indicating that prediction equations need to be derived and validated in different countries. We used our own derived equation to increase the suitability for our study population.
Ngoan et al. (13) showed that alcohol consumption and employment status are not associated with stomach cancer, but in our study, these factors were associated with a history of stomach cancer.
Other than stomach cancer, a history of breast cancer in women was associated with increased sodium excretion. Karimi et al. (19) showed that an 'unhealthy' food consumption pattern including salty foods was associated with a significantly increased risk of breast cancer.
Several mechanisms of stomach cancer pathogenesis induced by high salt intake have been suggested, although there has been no conclusive evidence. A high, intragastric salt concentration destroys the mucosal barrier and causes inflammation (20, 21). With the destruction of the mucosal barrier, high salt intake increases the susceptibility of mucosal cells to carcinogenic agents such as nitrates (22). Persistent inflammatory responses in the stomach epithelium may increase epithelial cell proliferation as part of the repair process, and it may also increase the rate of endogenous mutations (23, 24). Another explanation for the effect of high salt intake on stomach cancer pathogenesis is that the damage caused by salt may also increase gastric Helicobacter pylori colonization. H. pylori infection is one of the important known risk factors of stomach cancer. H. pylori responds to changes in the environmental salt concentration in such a way that growth, cell morphology, survival, and virulence factor expression are altered (25).
There were several limitations of the current study. First, this was not a prospective study, and cancer history was obtained by using a questionnaire; therefore, the prevalence may not be as exact as that of a prospective study. Second, we could not rule out the possible confounding factors, such as H. pylori infection, which is one of the important risk factors for stomach cancer.
In conclusion, high salt intake results in a higher rate of estimated 24-hr urine sodium excretion, which is associated with a history of stomach or breast cancer.
Footnotes
This research was supported by a grant (13162MFDS104) in 2013 from the Ministry of Food and Drug Safety, Korea.
The authors have no conflicts of interest to disclose.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45:1–14. doi: 10.4143/crt.2013.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kono S, Hirohata T. Nutrition and stomach cancer. Cancer Causes Control. 1996;7:41–55. doi: 10.1007/BF00115637. [DOI] [PubMed] [Google Scholar]
- 4.Honjo S, Kono S, Yamaguchi M. Salt and geographic variation in stomach cancer mortality in Japan. Cancer Causes Control. 1994;5:285–286. doi: 10.1007/BF01830250. [DOI] [PubMed] [Google Scholar]
- 5.Tsugane S, Tsuda M, Gey F, Watanabe S. Cross-sectional study with multiple measurements of biological markers for assessing stomach cancer risks at the population level. Environ Health Perspect. 1992;98:207–210. doi: 10.1289/ehp.9298207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bates CJ, Thurnham DI, Bingham SA, Margetts BM, Nelson M. Biochemical markers of nutrient intake. In: Margetts BM, Nelson M, editors. Design concepts in nutritional epidemiology. Oxford, New York: Oxford University Press; 1991. pp. 170–240. [Google Scholar]
- 7.Hunter D. Biochemical indicators of dietary intake. In: Willett W, editor. Nutritional epidemiology. New York: Oxford University Press; 1998. pp. 174–243. [Google Scholar]
- 8.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-hr urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103. doi: 10.1038/sj.jhh.1001307. [DOI] [PubMed] [Google Scholar]
- 11.Sjodahl K, Jia C, Vatten L, Nilsen T, Hveem K, Lagergren J. Salt and gastric adenocarcinoma: a population-based cohort study in Norway. Cancer Epidemiol Biomarkers Prev. 2008;17:1997–2001. doi: 10.1158/1055-9965.EPI-08-0238. [DOI] [PubMed] [Google Scholar]
- 12.Kneller RW, McLaughlin JK, Bjelke E, Schuman LM, Blot WJ, Wacholder S, Gridley G, CoChien HT, Fraumeni JF., Jr A cohort study of stomach cancer in a high-risk American population. Cancer. 1991;68:672–678. doi: 10.1002/1097-0142(19910801)68:3<672::aid-cncr2820680339>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 13.Ngoan LT, Mizoue T, Fujino Y, Tokui N, Yoshimura T. Dietary factors and stomach cancer mortality. Br J Cancer. 2002;87:37–42. doi: 10.1038/sj.bjc.6600415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shikata K, Kiyohara Y, Kubo M, Yonemoto K, Ninomiya T, Shirota T, Tanizaki Y, Doi Y, Tanaka K, Oishi Y, et al. A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population: the Hisayama study. Int J Cancer. 2006;119:196–201. doi: 10.1002/ijc.21822. [DOI] [PubMed] [Google Scholar]
- 15.Tsugane S, Sasazuki S, Kobayashi M, Sasaki S. Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer. 2004;90:128–134. doi: 10.1038/sj.bjc.6601511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van den Brandt PA, Botterweck AA, Goldbohm RA. Salt intake, cured meat consumption, refrigerator use and stomach cancer incidence: a prospective cohort study (Netherlands) Cancer Causes Control. 2003;14:427–438. doi: 10.1023/a:1024979314124. [DOI] [PubMed] [Google Scholar]
- 17.Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297:319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Subramanian S, Teo BW, Toh QC, Koh YY, Li J, Sethi S, Lee EJ. Spot urine tests in predicting 24-hour urine sodium excretion in Asian patients. J Ren Nutr. 2013;23:450–455. doi: 10.1053/j.jrn.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Karimi Z, Jessri M, Houshiar-Rad A, Mirzaei HR, Rashidkhani B. Dietary patterns and breast cancer risk among women. Public Health Nutr. 2014;17:1098–1106. doi: 10.1017/S1368980013001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kato S, Tsukamoto T, Mizoshita T, Tanaka H, Kumagai T, Ota H, Katsuyama T, Asaka M, Tatematsu M. High salt diets dose-dependently promote gastric chemical carcinogenesis in Helicobacter pylori-infected Mongolian gerbils associated with a shift in mucin production from glandular to surface mucous cells. Int J Cancer. 2006;119:1558–1566. doi: 10.1002/ijc.21810. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi M, Hasegawa R. Enhancing effects of dietary salt on both initiation and promotion stages of rat gastric carcinogenesis. Princess Takamatsu Symp. 1985;16:169–182. [PubMed] [Google Scholar]
- 22.Takahashi M, Kokubo T, Furukawa F, Kurokawa Y, Tatematsu M, Hayashi Y. Effect of high salt diet on rat gastric carcinogenesis induced by N-methyl-N'-nitro-N-nitrosoguanidine. Gan. 1983;74:28–34. [PubMed] [Google Scholar]
- 23.Furihata C, Ohta H, Katsuyama T. Cause and effect between concentration-dependent tissue damage and temporary cell proliferation in rat stomach mucosa by NaCl, a stomach tumor promoter. Carcinogenesis. 1996;17:401–406. doi: 10.1093/carcin/17.3.401. [DOI] [PubMed] [Google Scholar]
- 24.Charnley G, Tannenbaum SR. Flow cytometric analysis of the effect of sodium chloride on gastric cancer risk in the rat. Cancer Res. 1985;45:5608–5616. [PubMed] [Google Scholar]
- 25.Gancz H, Jones KR, Merrell DS. Sodium chloride affects Helicobacter pylori growth and gene expression. J Bacteriol. 2008;190:4100–4105. doi: 10.1128/JB.01728-07. [DOI] [PMC free article] [PubMed] [Google Scholar]