Abstract
Excessive dietary salt intake is related to cardiovascular morbidity and mortality. Although dietary salt restriction is essential, it is difficult to achieve because of salt palatability. However, the association between salt perception or salt eating habit and actual salt intake remains uncertain. In this study, we recruited 74 healthy young individuals. We investigated their salt-eating habits by questionnaire and salt taste threshold through a rating scale that used serial dilution of a sodium chloride solution. Predicted 24-hr urinary salt excretions using Kawasaki's and Tanaka's equations estimated dietary salt intake. Participants' mean age was 35 yr, and 59.5% were male. Salt sense threshold did not show any relationship with actual salt intake and a salt-eating habit. However, those eating "salty" foods showed higher blood pressure (P for trend=0.048) and higher body mass index (BMI; P for trend=0.043). Moreover, a salty eating habit was a significant predictor for actual salt intake (regression coefficient [β] for Kawasaki's equation 1.35, 95% confidence interval [CI] 10-2.69, P=0.048; β for Tanaka's equation 0.66, 95% CI 0.01-1.31, P=0.047). In conclusion, a self-reported salt-eating habit, not salt taste threshold predicts actual salt intake.
Graphical Abstract
Keywords: Salt-Eating Habit, Salt Taste Threshold, Salt Intake
INTRODUCTION
Higher salt intake is a well-known risk factor for hypertension, stroke, and cardiovascular disease (1). Previous studies showed that a high-salt diet is believed to be responsible for up to 40% of all cases of hypertension and 6% of myocardial infarction and stroke annually (2). Moreover, salt reduction can substantially reduce future cardiovascular events; therefore, it is probably one of the most cost-effective strategies to prevent cardiovascular disease (1, 3). Unfortunately, however, most individuals prefer to consume substantially more salt than is necessary to maintain normal physiology and that is recommended by major health organizations (4). According to the results of the Korean National Health and Nutritional Examination Survey, salt intake in Korea was 11.0 to 14.0 g/day, which is 40% to 56% in excess of the Ministry of Health and Welfare's recommendation (5).
Behavioral changes are notoriously difficult to achieve in terms of reducing salt intake. Because low-salt foods are considered by some to lack taste, many salt-restriction programs encountered difficulties in both initiating and maintaining compliance. Because a hedonic response to salt preference results from a complex interplay of physiologic, genetic, psychological, and developmental factors, high salt intake could explain sensory and behavioral factors (6, 7). Previous studies showed that the preference for salty taste can be decreased by long-term adherence to salt restriction (8). In this regard, individual attempts to lower dietary salt intake have largely proved to be ineffective (9). A national regulation to reduce salt intake would be cost-saving and effective (3, 10), with the food industry bearing some of the costs. Individuals appear to prefer less salty food as salt intake is reduced (11).
These statements can be determined by the assumption that elevated salt preference leads to higher salt intakes. However, there is little evidence about whether salt taste perception is associated with actual salt intake. Moreover, several previous studies have shown controversial results (12, 13). Another simple method to measure salt preference is a person's subjective salt-eating habit. Studies to explore the association between a salt-eating habit and real salt intake are also scarce and discrepant (14, 15). Therefore, we proposed to demonstrate the association between salt preference represented by salt taste threshold, self-reported salt-eating habit, and real salt intake.
MATERIALS AND METHODS
Study subjects and clinical parameters
We surveyed 79 young healthy adults who had visited the "Salt and Health" between January 2013 and February 2014. They participated in a detailed e-mail questionnaire, underwent standardized physical examinations and anthropometric measures, and provided urine samples. Blood pressure was measured by a specified automatic blood pressure monitor after a minimum of 5 min of rest while sitting in a chair. The average of 3 measurements was recorded. Body mass index (BMI) was calculated based on weight and height (weight [kg]/height [m2]). From the fasting morning urine samples, we measured the concentration of urine sodium, potassium, chloride, and creatinine and performed a simple urinalysis by microscopic examination that was sent to the Green Cross Corporation. We collected multiple urine samples from most subjects. More than 90% of subjects provided samples for spot urine analysis 10 times, others 9 times. Subjects who refused the salt taste threshold test, provided inadequate questionnaire replies, or collected their urine samples less than 5 times were excluded.
Self-reported salt preference
We surveyed the subject's self-reported salt-eating habit by using a self-administered questionnaire on dietary habits. To the question "How salty do you usually eat your food?" participants could select from these answers: "eat salty," "on average, eat salty," and "eat sparingly." We checked the responses repeatedly during the study interval.
Salt taste threshold measurement
Salt taste threshold was measured in each subject by the ability to discern the taste of salt in graded solution of a sodium chloride concentration. The salt taste threshold was graded in 0.0625%, 0.125%, 0.25%, 0.5%, 1%, 2%, 4%, and 5% of salt solution prepared by weighing the amount of sterilized salt and dissolving it in distilled and deionized water. Each bottle was coded to prevent bias from the examiner and each had a separate pipette to prevent admixture of the different solutions. Three drops of salt solution at room temperature were placed on the tongue of each subject, starting with the lowest concentration, 0.0625%, and increasing incrementally. The minimum concentration of solution at which the subject was able to discern the taste of salt was taken as his or her salt taste threshold.
Estimation of 24-hr salt excretion from spot urine
Based on spot urinary sodium to creatinine ratios, we predicted 24-hr urinary salt excretion using the Kawasaki (16) and Tanaka (17) estimation equations. Both formulas were developed for a Japanese population (18), but also have been validated in Western populations (19). Only the Kawasaki formula had sex-specific predictions of creatinine. The Kawasaki equation estimated 24-hr urinary sodium excretion as follows: predicted 24-hr urinary sodium excretion=23 * (16.3 * XNa0.5), where XNa= (spot sodium concentration [mM/L]/spot creatinine concentration [mg/dL] * 10) * (predicted 24-hr creatinine [mg/d]). For men, the predicted 24-hr creatinine (mg/d)=(-12.63 * age [yr]) + (15.12 * weight [kg]) + (7.39 * height [cm])-79.9. For women, the predicted 24-hr creatinine (mg/d)=(-4.72 * age [yr]) + (8.58 * weight [kg]) + (5.09 * height [cm])-74.5. The Tanaka equation estimated 24-hr urinary sodium excretion as follows: 23 * (21.98 * XNa0.392), where XNa is the same as in the Kawasaki equation. As we collected repetitive spot urine samples, we determined the mean value of repetitively predicted 24-hr urinary salt excretion levels from each participant.
Statistical analysis
All data are presented as frequencies and percentages of categorical variables. Before further statistical analysis, continuous variables were tested for normality with the Kolmogorov-Smirnov test. Variables without a normal distribution were analyzed by nonparametric tests. The values with normal distribution are indicated as mean±standard deviation (spot urine sodium/potassium and predicted 24-hr urine salt excretions), whereas those without normal distribution (age, systolic blood pressure, diastolic blood pressure, BMI, and salt taste threshold) are shown as the median and interquartile range. Differences in demographic factors, salt taste thresholds, and predicted 24-hr urinary salt excretions across the salt-eating groups were compared using the chi-square test for trend (linear-by-linear association). Similarly, one way analysis of variance test was applied to demonstrate linearity of continuous variables across the salt-eating groups.
To assess the relationship between predicted 24-hr urine salt excretion and a salt-eating habit, salt taste, and other clinical parameters, univariate and multivariable linear regression analyses were performed. Variables that showed a significant association (P<0.10) in the univariate analysis or were of considerable theoretical relevance were entered into the multivariate stepwise linear regression models. Analyses were performed using the SPSS software package (version 21.0, Chicago, IL, USA). All tests were two-tailed, with P<0.05 considered statistically significant.
Ethics statement
To ensure that the participants' rights were protected, this investigation was approved by the institutional review board of the Seoul National University Hospital and was operated in accordance with the principles of the Helsinki Declaration II (H-1205-121-411). The primary investigator explained the purposes and procedures for this study to the board before data collection. Then, written informed consent was obtained from the participants. Potential subjects understood that their participation was voluntary. If they declined to participate, they were excluded. Ethical principles and standards of human rights protection were adhered to during the entire research process.
RESULTS
Study population characteristics according to self-reported salt preference
After exclusion, 74 participants and their 732 urine samples were included in our final analysis. The median age of the study subjects was 35 (31-38) yr (median [interquartile range]); 59.5% of the subjects were male. We measured salt-eating habits twice. The first question the subjects answered had 3 categories: "insipid", "average", and "salty." The second question had 4 categories: "very insipid", "insipid", "salty", and "very salty"; the "average" category was removed. In the first question, 8 subjects reported that they usually ate thinly, 44 participants said that they ate salty on average, and 22 declared that they ate salty. In the second question, 1 subject answered as very insipid, 24 insipid, 48 salty, and only 1 subject reported that he or she ate very salty. Interestingly, participants who responded that they ate both "insipid" and "salty" showed consistent replies for the 2 separate questions. However, subjects who answered that they ate an average amount of salt were divided into "insipid" and "salty" responses. Because average salt intake is ambiguous, we decided to discriminate salt-eating habits. In other words, we regarded participants with average salt intake as a gray zone.
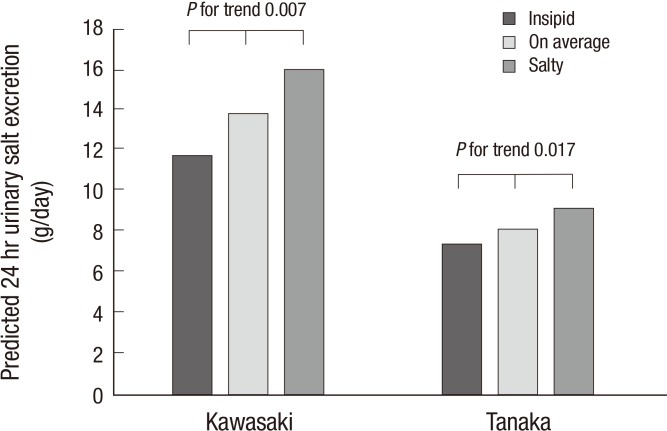
The demographic and clinical characteristics of the subjects stratified by self-reported salt-eating habits are shown in Table 1. Age distribution did not differ across the salt-eating group. However, the salty-eating group was relatively older, predominantly male, and had higher systolic and diastolic blood pressure and higher BMI. In terms of a salt taste threshold, there was no difference among the 3 salt-eating groups. However, salt intake, determined by 2 estimated 24-hr urinary salt excretions, was significantly increased with a higher self-reported salt eating habit (Kawasaki's estimation, P for trend 0.007; Tanaka's estimation, P for trend 0.017; Fig. 1).
Table 1.
Baseline characteristics according to self-reported salt eating habit
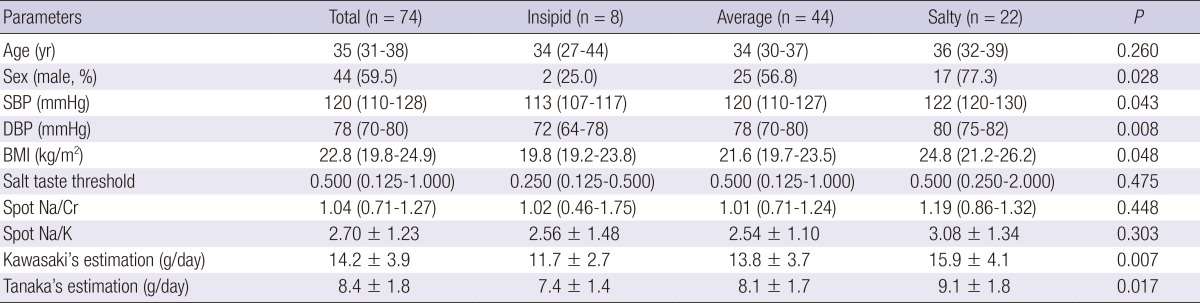
SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index.
Fig. 1.
Estimated 24-hr urinary salt excretion according to self-reported salt eating habit.
Salt taste threshold and salt preference
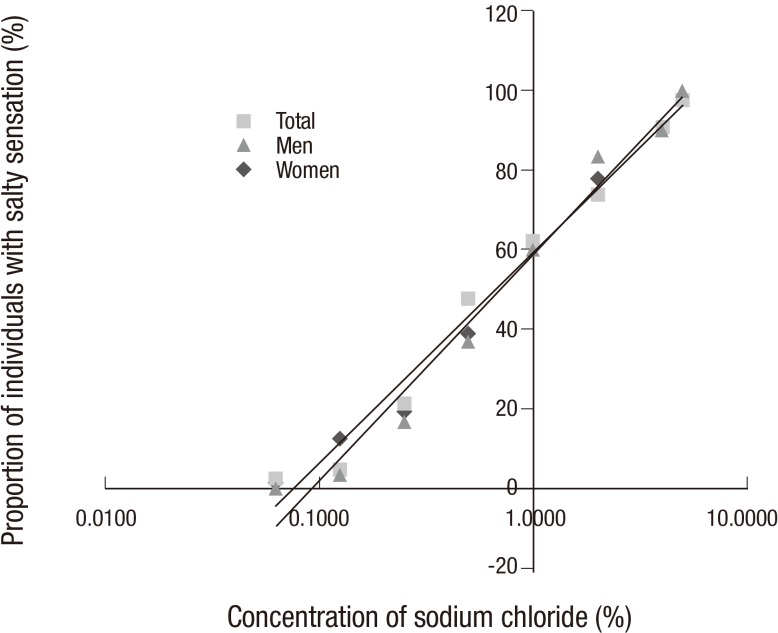
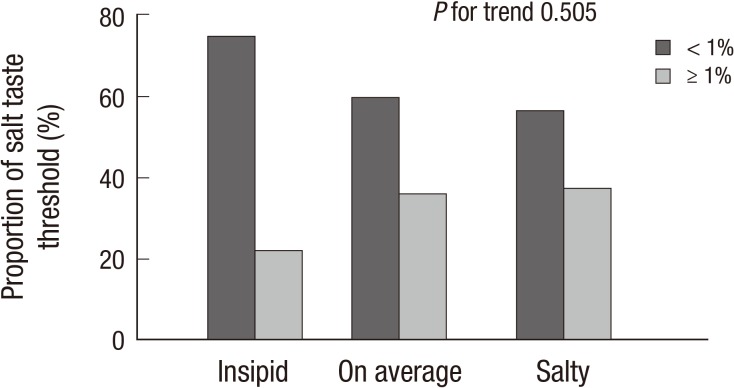
A salt taste threshold result was available for 72 participants. Fig. 2 shows the overall distribution of salt taste threshold in this population. All of the subjects tasted "salty" in the 5% sodium chloride solution. More than 20% of subjects tasted "salty" with the isotonic saline. Salt taste threshold did not differ according to sex. As shown in Fig. 2, the proportion of individuals who tasted "salty" was related linearly with sodium chloride concentration presented on a log scale. Subjects who reported that they ate thinly tended to have a lower salt taste threshold, although the association between salt taste threshold and salt-eating habit was insignificant (P for trend 0.505, Fig. 3).
Fig. 2.
Salt taste threshold according to sex.
Fig. 3.
Proportion of salt taste threshold according to self-reported salt eating habit.
Predictors of estimated 24-hr urinary salt excretion
The Kawasaki and Tanaka equations correlated well (r2=0.988, P<0.001). In the univariate linear regression analysis, increased predicted 24-hr urinary salt excretion was associated with older age, male gender, higher systolic and diastolic blood pressure, higher BMI, and self-reported a salt-eating habit. The salt taste threshold failed to prove any association with both predicted 24-hr urinary salt excretions. Although sex was one of strongest determinants of estimated salt intake, it showed significant colinearity in the multivariate analysis. Therefore, we excluded sex in the final multivariate analysis. Even after full adjustment, a self-reported salt-eating habit (adjusted regression coefficient [β] [95% confidence interval] for Kawasaki's estimation: 1.35 [0.10-2.69], P=0.048; β for Tanaka's estimation =0.66 [0.01-1.31], P=0.047) remained a significant predictor for estimated 24-hr urinary salt excretion (Table 2). When we performed subgroup analysis for sex, these findings were reproduced in men, but not in women. In men, a self-reported salt-eating habit was a risk factor for daily urinary salt excretion even after adjustment (adjusted β for Kawasaki's estimation: 1.87 [0.18-3.56], P=0.031; adjusted β for Tanaka's estimation= 0.88 [0.11-1.66], P=0.027). In women, the multivariate modeling could not be constructed because of the low number of subjects.
Table 2.
Linear regression analysis for predicted 24 hr urinary salt excretion
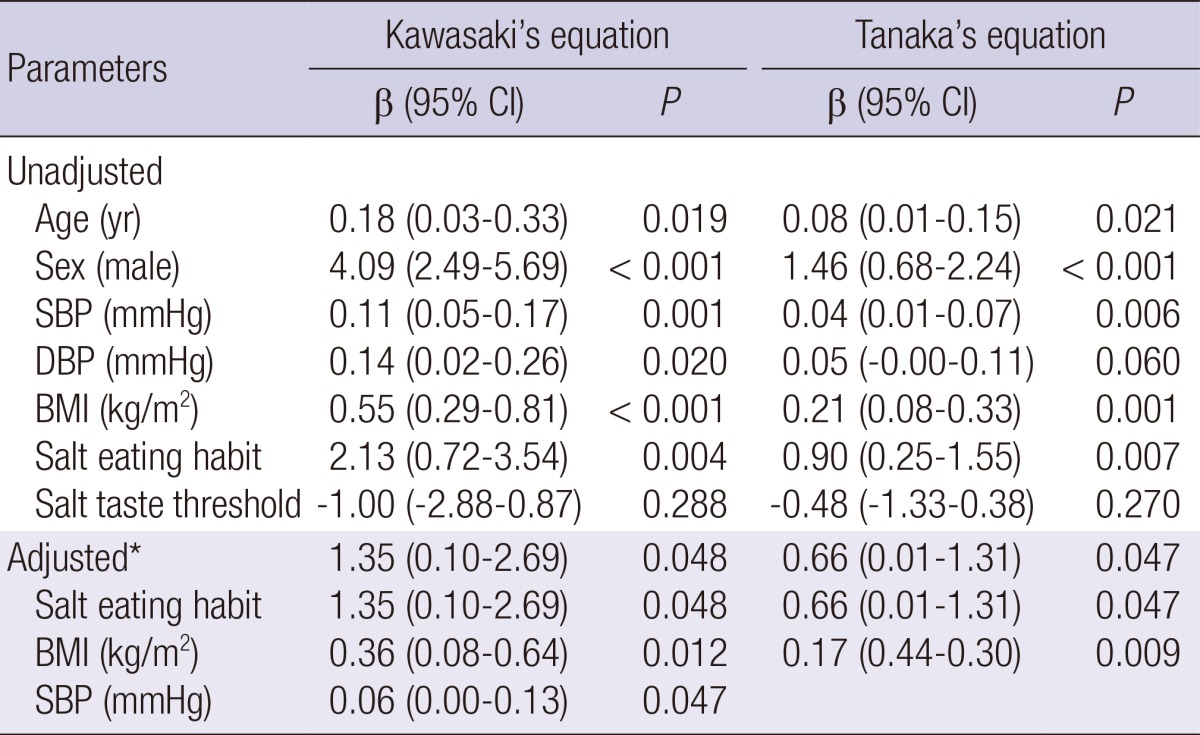
*Adjusted by age, body mass index, systolic blood pressure, and taste perception. SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index.
DISCUSSION
In this study, we demonstrated that a self-reported salt-eating habit is associated with elevated blood pressure and higher BMI. Moreover, a self-reported salt-eating habit proved to independently predict estimated salt intake from spot urine sodium analysis. On the other hand, salt taste perception fails to prove an association with either clinical parameter such as blood pressure and BMI or estimated salt intake. This study was conducted in a relatively healthy, young population, not in older or hypertensive patients. These findings suggest that the idea of following a low-salt diet can be a link between having the will and the ongoing behavior for dietary salt reduction.
One important finding of this study is that hedonic responses to salt are not directly related with actual salt intake. Previous studies showed that manipulation of salt intake could change salt preference (20, 21); however, the association between hedonic rating and salt intake with a stable intake remains unclear. Several studies noted a significant association (22, 23); others observed no relation (24). These discrepancies might be due to inconsistent quantification of both salt perception and salt intake. Salt taste perception was measured variously, including by a 9-category, fully anchored hedonic rating scale (22, 25) and preferred concentration of salt in food (23, 24). Preference is a multidimensional factor and threshold determination is more difficult to achieve in taste because of what taste receptors do. Therefore, hedonic ratings of salt in food may be insensitive and poorly characterized (26). These different and insensitive methods of salt perception measurement may hinder using salt taste as a prediction of real salt intake.
In the present study, we used a rating scale method for determining "absolute" taste threshold (27, 28). As shown in Fig. 2, serial dilution of sodium chloride in tap water appears to reflect the population's salt taste perception, irrespective of sex. Moreover, individuals perceive only the salt taste, not food flavors or other tastes; therefore, absolute salt taste threshold can be measured. Unexpectedly, salt taste sensitivity was not related to real salt intake; rather, a self-reported eating habit was associated with actual salt intake. These results support that it is possible to limit salt intake effectively by educating and training individuals. Moreover, such findings have also proposed that the food industry would be affected only slightly by reducing salt in their products during manufacturing. In other words, manufacturers may not need to produce their product with as much salt just to satisfy as many as possible people's salt hedonia. Maintaining food palatability with less salt is possible. In this regard, our findings are important for long-term adherence to lower dietary salt intake by both individuals and the food industry.
Another unprecedented finding in the present study is that a self-reported salt-eating habit can be a simple and useful method to predict actual dietary salt intake. Although a self-reported salt-eating habit is a subjective attribute, it is simply and easy to obtain. Moreover, self-adherence to a dietary salt restriction is an important part of preventing hypertension and other cardiovascular disease. However, there was little evidence whether it can reflect actual salt intake or clinical outcome. Previous studies were performed in patients with heart failure, and the results are inconsistent. One study showed that self-adherence to a low-salt diet was associated with symptom relief and decreased cardiac events in patients with heart failure (29). Other articles showed that a self-reported eating habit is not reliable method for estimating salt intake (30). Characteristically, our study population was composed of relatively young and healthy subjects, and they had a limited experience of salt restriction. In this population, salt-eating habits are not only related to higher blood pressure and higher BMI, but also to actual salt intake. To clarify this finding, further well-designed, large-scale studies are warranted.
The present study has some limitations. First, we could not standardize or scale participants' salt-eating habits; therefore, it is difficult to ensure reproducibility. Although we asked the participants twice about their salt intake, they did not provide the same answers. To guarantee objectivity, further confirmation should be determined at a regular interval. Second, to estimate actual daily salt intake, we used derivation equations from spot urine sodium and creatinine, not 24-hr urine sodium excretion. Actually, 24-hr urine sodium excretion is the gold standard for monitoring sodium intake; however, it is difficult, inconvenient, and cumbersome, particularly for women. Therefore, many subjects cannot accurately collect their specimen. Dietary recall is another main method for accessing salt intake; however, it is also inaccurate. To overcome such limitations, we used 2 representative predictive equations. They estimated 24-hr urinary sodium excretion by using spot urine sodium excretion. All of them were validated for their predictability (19). Our study could not adopt a gold standard method, but we applied acceptable derivation equations for estimation of dietary salt intake. Third, the sample size was relatively small and clinical attributes were limited. Further well-designed trials may be helpful to clarify these study findings.
In conclusion, a self-reported salt-eating habit, not a salt taste threshold is associated with elevated blood pressure, higher BMI, and finally higher salt intake. Moreover, it independently predicts actual dietary salt intake. These findings have crucial clinical implications that accentuate the importance of individual education for behavioral change.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. doi: 10.1136/bmjopen-2013-003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee SW, Kim YC, Oh SW, Koo HS, Na KY, Chae DW, Kim S, Chin HJ. Trends in the prevalence of chronic kidney disease, other chronic diseases and health-related behaviors in an adult Korean population: data from the Korean National Health and Nutrition Examination Survey (KNHANES) Nephrol Dial Transplant. 2011;26:3975–3980. doi: 10.1093/ndt/gfr154. [DOI] [PubMed] [Google Scholar]
- 6.Beauchamp GK, Engelman K. High salt intake. Sensory and behavioral factors. Hypertension. 1991;17:I176–I181. doi: 10.1161/01.hyp.17.1_suppl.i176. [DOI] [PubMed] [Google Scholar]
- 7.Leshem M. Biobehavior of the human love of salt. Neurosci Biobehav Rev. 2009;33:1–17. doi: 10.1016/j.neubiorev.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Coldwell SE, Tordoff MG. Learned preferences for the flavor of salted food. Physiol Behav. 1993;54:999–1004. doi: 10.1016/0031-9384(93)90314-6. [DOI] [PubMed] [Google Scholar]
- 9.Hooper L, Bartlett C, Davey SG, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database Syst Rev. 2004:CD003656. doi: 10.1002/14651858.CD003656.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Martikainen JA, Soini EJ, Laaksonen DE, Niskanen L. Health economic consequences of reducing salt intake and replacing saturated fat with polyunsaturated fat in the adult Finnish population: estimates based on the FINRISK and FINDIET studies. Eur J Clin Nutr. 2011;65:1148–1155. doi: 10.1038/ejcn.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension. 2003;42:1093–1099. doi: 10.1161/01.HYP.0000102864.05174.E8. [DOI] [PubMed] [Google Scholar]
- 12.Shim E, Ryu HJ, Hwang J, Kim SY, Chung EJ. Dietary sodium intake in young Korean adults and its relationship with eating frequency and taste preference. Nutr Res Pract. 2013;7:192–198. doi: 10.4162/nrp.2013.7.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drewnowski A, Henderson SA, Driscoll A, Rolls BJ. Salt taste perceptions and preferences are unrelated to sodium consumption in healthy older adults. J Am Diet Assoc. 1996;96:471–474. doi: 10.1016/S0002-8223(96)00131-9. [DOI] [PubMed] [Google Scholar]
- 14.Chang Y, Park MS, Chung SY, Lee SY, Kwon HT, Lee JU. Lack of association between self-reported saltiness of eating and actual salt intake. Korean J Fam Med. 2012;33:94–104. doi: 10.4082/kjfm.2012.33.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radimer KL, Harvey PW. Comparison of self-report of reduced fat and salt foods with sales and supply data. Eur J Clin Nutr. 1998;52:380–382. doi: 10.1038/sj.ejcn.1600557. [DOI] [PubMed] [Google Scholar]
- 16.Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20:7–14. doi: 10.1111/j.1440-1681.1993.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 17.Kamata K, Tochikubo O. Estimation of 24-h urinary sodium excretion using lean body mass and overnight urine collected by a pipe-sampling method. J Hypertens. 2002;20:2191–2197. doi: 10.1097/00004872-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Iseki K, Iseki C, Itoh K, Uezono K, Sanefuji M, Ikemiya Y, Fukiyama K, Kawasaki T. Urinary excretion of sodium and potassium in a screened cohort in Okinawa, Japan. Hypertens Res. 2002;25:731–736. doi: 10.1291/hypres.25.731. [DOI] [PubMed] [Google Scholar]
- 19.Cogswell ME, Wang CY, Chen TC, Pfeiffer CM, Elliott P, Gillespie CD, Carriquiry AL, Sempos CT, Liu K, Perrine CG, et al. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18-39 y. Am J Clin Nutr. 2013;98:1502–1513. doi: 10.3945/ajcn.113.059436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beauchamp GK, Bertino M, Engelman K. Failure to compensate decreased dietary sodium with increased table salt usage. JAMA. 1987;258:3275–3278. [PubMed] [Google Scholar]
- 21.Jeffery RW, Pirie PL, Elmer PJ, Bjornson-Benson WM, Mullenbach VA, Kurth CL, Johnson SL. Low-sodium, high-potassium diet: feasibility and acceptability in a normotensive population. Am J Public Health. 1984;74:492–494. doi: 10.2105/ajph.74.5.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shepherd R, Farleigh CA, Land DG. The relationship between salt intake and preferences for different salt levels in soup. Appetite. 1984;5:281–290. doi: 10.1016/s0195-6663(84)80001-x. [DOI] [PubMed] [Google Scholar]
- 23.Pangborn RM, Pecore SD. Taste perception of sodium chloride in relation to dietary intake of salt. Am J Clin Nutr. 1982;35:510–520. doi: 10.1093/ajcn/35.3.510. [DOI] [PubMed] [Google Scholar]
- 24.Mattes RD. Gustation as a determinant of ingestion: methodological issues. Am J Clin Nutr. 1985;41:672–683. doi: 10.1093/ajcn/41.4.672. [DOI] [PubMed] [Google Scholar]
- 25.David R, Peryam FJP. Hedonic scale method of measuring food preferences. Food Technol. 1957;11:9–14. [Google Scholar]
- 26.Mattes RD. The taste for salt in humans. Am J Clin Nutr. 1997;65:692s–697s. doi: 10.1093/ajcn/65.2.692S. [DOI] [PubMed] [Google Scholar]
- 27.Gregson RAM. A rating scale method for determining absolute taste threshold. J Food Sci. 1962;27:376–380. [Google Scholar]
- 28.Wise PM, Breslin PAS. Individual Differences in Sour and Salt Sensitivity: Detection and Quality Recognition Thresholds for Citric Acid and Sodium Chloride. Chem Senses. 2013 doi: 10.1093/chemse/bjt003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Son YJ, Lee Y, Song EK. Adherence to a sodium-restricted diet is associated with lower symptom burden and longer cardiac event-free survival in patients with heart failure. J Clin Nurs. 2011;20:3029–3038. doi: 10.1111/j.1365-2702.2011.03755.x. [DOI] [PubMed] [Google Scholar]
- 30.Colin-Ramirez E, McAlister FA, Woo E, Wong N, Ezekowitz JA. Association between self-reported adherence to a low-sodium diet and dietary habits related to sodium intake in heart failure patients. J Cardiovasc Nurs. 2014 doi: 10.1097/JCN.0000000000000124. DOI: 10.1097/JCN.0000000000000124. [DOI] [PubMed] [Google Scholar]