Abstract
Purpose
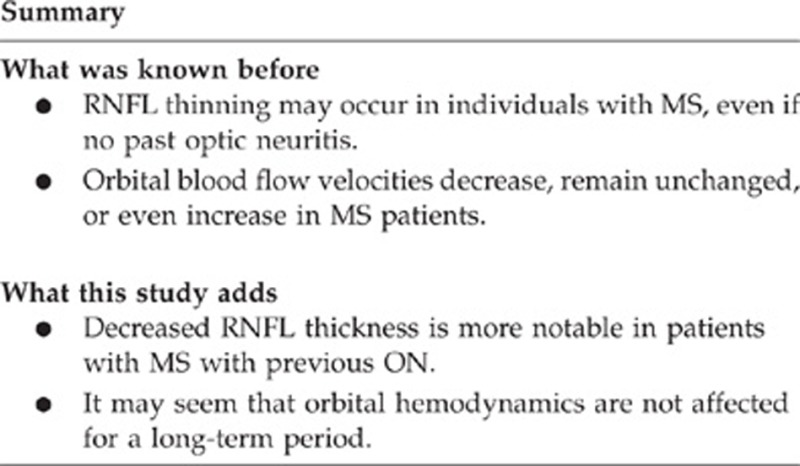
To compare both retinal nerve fiber layer thickness and orbital color Doppler ultrasonography parameters in patients with multiple sclerosis (MS) versus healthy controls.
Methods
This is an observational case–control study. Forty eyes from MS patients and twenty eyes from healthy volunteers were examined. Eyes were classified into three groups as group 1, eyes from MS patients with previous optic neuritis (n=20); group 2, eyes from MS patients without previous optic neuritis (n=20); and group 3, eyes from healthy controls (n=20). Following complete ophthalmologic examination and retinal nerve fiber layer thickness measurement for each group, blood flow velocities of posterior ciliary arteries, central retinal artery, ophthalmic artery, and superior ophthalmic vein were measured. Pourcelot index (resistive index), an indicator of peripheral vascular resistance, was also calculated. The statistical assessment was performed with the assistance of Pearson's Chi-square test, Mann–Whitney U-test, Kruskal–Wallis test, and Spearman's correlation test.
Results
The studied eyes exposed similar values in terms of intraocular pressure and central corneal thickness, implying no evidence in favor of glaucoma. All nerve fiber layer thickness values, except superior nasal quadrants, in group 1 were found to be significantly thinner than groups 2 and 3. Blood flow velocity and mean resistivity index parameters were similar in all the groups.
Conclusions
In MS patients, especially with previous optic neuritis, diminished retinal nerve fiber layer thickness was observed. Contrary to several studies in the current literature, no evidence supporting potential vascular origin of ocular involvement in MS was found.
Introduction
Multiple sclerosis (MS) is known as one of the inflammatory, degenerative central nervous system (CNS) diseases. Optic neuritis (ON), a common initial manifestation of MS, is an immune-mediated acute inflammatory disorder of the optic nerve.1 Although it is thought that primary inflammatory demyelinization is important in the pathophysiology of ON and MS, the exact underlying cause of ON in MS is still obscure.2 Sudden loss of vision is frequently a consequence of acute demyelinization of the optic nerve and nearly one half of the MS patients experience it at some point during their disease course.3 Furthermore, axonal damage may occur in some cases and this damage can be identified as a thinning of the retinal nerve fiber layer (RNFL) using computerized imaging technologies such as optical coherence tomography (OCT). OCT is a noninvasive imaging technique that enables high-resolution quantification of retinal structures and can detect subclinical changes in MS patients as well.4 However, RNFL and ganglion cell/inner plexiform layer (GCIP) thinning has been demonstrated in individuals with MS, not only in those with previous ON but also in those without it.5
In addition, vascular mechanisms such as increased plasma levels of endothelin-1 may be important for the development of axonal loss associated with ON and MS.6, 7 However, there have been conflicting reports of impaired hemodynamics in the orbital vessels of patients with ON. In some studies orbital blood flow velocities were decreased, whereas in others they remained unchanged or even increased.8, 9, 10, 11, 12
Given the conflicting results in previous studies, in the present study, we aimed to investigate the orbital blood flow velocities and RNFL thickness parameters in MS patients, with and without previous ON, and in healthy volunteers.
Materials and methods
The tenets of the Declaration of Helsinki were followed, Gazi University ethical committee approval was granted, patients were informed about the methods; and an informed consent form was signed by each participant. Forty eyes from MS patients who were being followed by Multiple Sclerosis Center at Gazi University Faculty of Medicine, Department of Neurology, and twenty eyes from healthy volunteers were recruited in the study. Eyes were divided into three groups as follows: group 1, eyes from MS patients with previous ON (P-ON); group 2, eyes from MS patients without previous ON (WP-ON); and group 3, eyes from healthy age-matched controls. None of the MS patients had clinically acute ON at the time of study. Previous ON had been diagnosed by an ophthalmologist based on its typical history and clinical findings.
To increase the statistical reliability, only one eye was included in all cases. Whereas the eyes that experienced ON were selected for P-ON group, the eyes with a higher signal strength in OCT were preferred in others. Demographic data such as age and gender were obtained during medical history questioning and the subjects had all assessments in one day. Each subject underwent a complete neurological and ophthalmic examination, including best-corrected visual acuity assessment with Snellen charts, intraocular pressure (IOP) measurement with Goldmann applanation tonometry, central corneal thickness (CCT) measurement by ultrasonic pachymeter, gonioscopy with Goldmann 3-mirror lens, slit lamp biomicroscopy, fundoscopic examination, light responses, and relative afferent pupillary defect. Eyes in P-ON and WP-ON groups were diagnosed as clinically definite MS based on McDonald's revised criteria.13 MS eyes were randomly included into the study. In each patient with MS, brain magnetic resonance imaging (MRI) was performed and Kurtzke's Expanded Disability Status Scale (EDSS) score was recorded.14
Exclusion criteria included a history of any systemic disease such as cardiovascular disease, arterial hypertension, hyperlipidemia, diabetes mellitus, refractive error of >±5.0 D spherical or ±2 D cylindrical (inability to fixate), coexisting ocular disease such as glaucoma, diabetes, or hypertensive retinopathy, compressive, toxic, or hereditary optic neuritis, history of incisional ocular surgery, and any other neurologic diseases (other than MS).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Optical coherence tomography
All OCT scans were performed on undilated pupils using the Spectralis OCT (Heidelberg Engineering, Dossenheim, Germany) for all RNFL measurements. All SD-OCT scans were performed by the same experienced technician. Peripapillary RNFL thickness was measured in central, superior temporal, temporal, inferior temporal, superior nasal, nasal, and inferior nasal quadrants of each eye.
Color Doppler imaging(CDI)
CDI of the eye was performed using an HDI 5000 SonoCT system (Philips, Bothell, WA, USA) using a 5–12-MHz multifrequency linear array transducer. The images were obtained in the supine position. Sterile coupling gel was applied to their closed eyelids, with the examiner's hand resting on the orbital margin to avoid any pressure on the eye. The average of three measurements was regarded as the final value. All individuals were evaluated by a single expert radiologist (S.O.O.). The radiologist was unaware of which side was involved for each patient. We obtained mean value±SD for the peak systolic velocity (PSV), end-diastolic velocity (EDV) and resistivity index (RI=(PSV−EDV)/PSV)15 for the ophthalmic, posterior ciliary, and central retinal arteries. Also superior ophthalmic vein (SOV) blood flow velocity was measured for all cases.
Statistical analyses
The chi-square test was used for categorical data and all of descriptive analyses results were reported as mean±SE for the groups. The Kruskal–Wallis test and Mann–Whitney U-test were conducted to determine group differences for RNFL thickness by quadrants and CDI measurements. A Spearman product moment correlation coefficient was calculated to establish the correlation between RNFL and CDI measurement. All statistical analysis was performed using the Statistical Package for the Social Sciences, version 16.0 (SPSS, Chicago, IL, USA). Statistical significance was defined as a P-value of <0.05.
Results
Twenty eyes of 20 individuals were included in each group. Mean number of ON attacks were 1.7±1.21 (1–6) in P-ON. No statistically significant differences were found among groups in terms of age, gender as well as mean IOP, mean CCT, and C/D (cup/disc) ratio. Mean elapsed time from the first symptom of ON until the admission of CDI assessment was 37.58±26.15 months (12–72 months). And the mean duration of MS was 49.95±9.41 (32–65) months in P-ON versus 44.8±8.86 (30–60) months in WP-ON (P=0.08). Mean EDSS score was 1.28±1.23 (0–3) in group 1 and 0.32±0.72 (0–2) in group 2 (P=0.13). Thereby all MS subjects had mild level of disease disability. All clinical and demographic properties of each group are shown in Table 1.
Table 1. Clinical and demographic details.
| Variables | P-ON eyes (n=20) | WP-ON eyes (n=20) | HC eyes (n=20) | P-value |
|---|---|---|---|---|
| Age (years) | 36.25±11.54 (18–61) | 37.10±10.97 (18–57) | 39.95±6.68 (23–53) | 0.40 |
| Gender | ||||
| Woman(%) | 17 (85) | 15 (75) | 11 (55) | 0.10 |
| Man(%) | 3 (15) | 5 (25) | 9 (45) | |
| BCVA(Snellen) | 0.86±0.17 (0.6–1) | 1.0 | 1.0 | 0.001 |
| IOP (mmHg) | 13.85±2.94 (10–18) | 14.35±3.42 (10–21) | 14.2±2.6 (10–19) | 0.92 |
| CCT (μm) | 546.25±34.01 (470–619) | 543.95 ±22.99 (508–595) | 547.45±26.38 (490–594) | 0.87 |
| C/D | 0.3±0.15 (0.1–0.7) | 0.28±0.12 (0.1–0.6) | 0.2±0.06 (0.1–0.3) | 0.06 |
| EDSS score | 1.28±1.23 (0–3) | 0.32±0.72 (0–2) | — | 0.13 |
Abbreviations: BCVA, best-corrected visual acuity; CCT, central corneal thickness; C/D, cup to disc ratio; EDSS, Expanded Disability Status Scale; HC, healthy age-matched control; IOP, intraocular pressure; P-ON, with previous optic neuritis; WP-ON, without previous optic neuritis. Chi-square test. Data are mean±SD (min–max). Italic entry refers to statistical significance (P<0.05).
RNFL thicknesses in all quadrants, except superior nasal quadrants, were found to be decreased in group 1 compared with group 3 (Table 2). In group 2 on the other hand, all quadrant thicknesses are similar to group 3 (Table 3). Retrobulbar blood flow velocity parameters and RIs of all eyes were comparable. Only mean EDV of the ophthalmic artery (OA) was slightly lower in group 1 (16.01±4.95 cm/s) than those of group 2 (17.82±5.83 cm/s) and group 3 (21.69±7.67 cm/s) (P=0.248 and 0.013, respectively) (Table 4). No significant correlation was found between RNFL and CDI parameters in group 1 (Table 5).
Table 2. RNFL thickness in P-ON eyes versus HC eyes.
| Quadrants (μm) | P-ON eyes | HC eyes | P-value |
|---|---|---|---|
| Central | 84.90±17.3 (48–111) | 103.10±6.64 (91–120) | 0.001 |
| Superior temporal | 118.95±25.7 (66–166) | 138.40±16.05 (107–166) | 0.009 |
| Temporal | 57.50±17.6 (28–91) | 70.35±7.35 (57–84) | 0.012 |
| Inferior temporal | 120.80±27.07 (77–157) | 149.10±17.56 (110–176) | 0.001 |
| Inferıor nasal | 98.40±2.80 (49–173) | 126.10±2.41 (93–174) | 0.002 |
| Nasal | 63.80±16.27 (32–95) | 78.75±15.80 (52–116) | 0.013 |
| Superior nasal | 96.65±35.26 (59–202) | 111.05±23.75 (73–157) | 0.372 |
Abbreviations: HC, healthy age-matched control; P-ON, with previous optic neuritis; RNFL, retinal nerve fiber layer. Mann–Whitney U-test. Data are mean±SD (min–max). Italic entries refer to statistical significance (P<0.05).
Table 3. RNFL thickness in WP-ON eyes versus HC eyes.
| Quadrants (μm) | WP-ON eyes | HC eyes | P-value |
|---|---|---|---|
| Central | 93.20±15.8 (59–117) | 103.10±6.64 (91–120) | 0.06 |
| Superior temporal | 127.65±19.27 (90–171) | 138.40±16.05 (107–166) | 0.07 |
| Temporal | 65.10±14.26 (37–89) | 70.35±7.35 (57–84) | 0.14 |
| Inferior temporal | 141.45±25.14 (89–187) | 149.10±17.56 (110–176) | 0.34 |
| Inferıor nasal | 107.65±27.66 (63–148) | 126.10±22.41 (93–174) | 0.06 |
| Nasal | 66±18.62 (40–101) | 78.75±15.80 (52–116) | 0.13 |
| Superior nasal | 103.65±21.96 (59–162) | 111.05±23.75 (73–157) | 0.16 |
Abbreviations: HC, healthy age-matched control; RNFL, retinal nerve fiber layer; WP-ON, without previous optic neuritis. Mann–Whitney U-test. Data are mean±SD (min–max).
Table 4. Doppler ultrasonography evaluation of blood flow velocities in orbital vessels.
| Orbital vessels | P-ON eyes | WP-ON eyes | HC eyes | P-value |
|---|---|---|---|---|
| CRA-PSV (cm/s) | 20.71±5.72 (12–32) | 20.18±6.07 (11–36) | 20.76±4.97 (12–31) | 0.90 |
| CRA-EDV (cm/s) | 7.89±2.34 (3.8–12.5) | 7.85±2.09 (4.8–13.5) | 8.09±2.21 (3.6–12.8) | 0.78 |
| CRA-RI | 0.63±0.07 (0.48–0.74) | 0.61±0.07 (0.5–0.78) | 0.61±0.06 (0.54– 0.78) | 0.53 |
| PCAs-PSV (cm/s) | 35.78±10.8 (23.6–57.5) | 33.76±10.42 (21.3–60.6) | 34.6 ±6.83 (26.7–48.4) | 0.68 |
| PCAs-EDV (cm/s) | 13.98±5.12 (7.6–23.6) | 13.71±5.72 (7.1–32.2) | 14.37±3.48 (6.7–21.8) | 0.41 |
| PCAs-RI | 0.61±0.06 (0.53–0.74) | 0.59±0.07 (0.48–0.75) | 0.59±0.06 (0.5–0.75) | 0.54 |
| OA-PSV (cm/s) | 56.97±13.61 (33.2–84.4) | 59.51±16.99 (33.1–104.2) | 69.39±18.76 (44.8–112.1) | 0.08 |
| OA-EDV (cm/s) | 16.01±4.95 (9.7–28.1) | 17.82±5.83 (10.5–36.3) | 21.69±7.67 (10.8–38.6) | 0.03 |
| OA-RI | 0.72±0.08 (0.57–0.84) | 0.70±0.05 (0.61–0.8) | 0.68±0.06 (0.58–0.8) | 0.19 |
| SOV (cm/s) | 15.18±6.57 (6.2–28.7) | 14.38±7.49 (6.7–37.1) | 12.67±3.39 (7.8–17.8) | 0.50 |
Abbreviations: CRA, central retinal artery; EDV, end-diastolic velocity; HC, healthy age-matched control; OA, ophthalmic artery; PCA, posterior ciliary artery; P-ON, with previous optic neuritis; PSV, peak systolic velocity, RI, resistive(resistance) index; SOV, superior ophthalmic vein; WP-ON, without previous optic neuritis. Kruskal–Wallis test. Data are mean±SD (min–max). Statistical italic entry refers to statistical significance (P<0.05).
Table 5. Correlations between CDI parameters and thickness of RNFL in P-ON eyes.
| Orbital Vessels |
RNFL quadrants |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Central |
Superior temporal |
Temporal |
Inferior temporal |
Inferior nasal |
Nasal |
Superior nasal |
||||||||
| *P | P** | *P | P** | *P | P** | *P | P** | *P | P** | *P | P** | *P | P** | |
| CRA-PSV (cm/s) | 0.09 | 0.695 | −0.57 | 0.823 | 0.279 | 0.263 | 0.156 | 0.538 | 0.039 | 0.877 | 0.063 | 0.804 | 0.054 | 0.832 |
| CRA-EDV (cm/s) | 0.09 | 0.703 | −0.08 | 0.974 | 0.101 | 0.689 | 0.039 | 0.879 | 0.117 | 0.644 | 0.130 | 0.607 | 0.109 | 0.667 |
| CRA-RI | −0.188 | 0.455 | −0.119 | 0.638 | 0.021 | 0.935 | −0.019 | 0.940 | −0.201 | 0.423 | −0.274 | 0.271 | −0.132 | 0.601 |
| PCAs-PSV (cm/s) | 0.260 | 0.298 | 0.005 | 0.820 | 0.391 | 0.108 | 0.156 | 0.536 | 0.176 | 0.485 | 0.140 | 0.581 | 0.271 | 0.276 |
| PCAs-EDV (cm/s) | 0.275 | 0.270 | 0.185 | 0.463 | 0.352 | 0.151 | 0.148 | 0.558 | 0.341 | 0.166 | 0.254 | 0.309 | 0.262 | 0.294 |
| PCAs-RI | −0.254 | 0.309 | −0.175 | 0.487 | −0.299 | 0.228 | −0.201 | 0.424 | −0.236 | 0.347 | −0.094 | 0.711 | −0.263 | 0.291 |
| OA-PSV (cm/s) | −0.153 | 0.546 | −0.277 | 0.266 | 0.073 | 0.772 | −0.128 | 0.612 | 0.039 | 0.877 | −0.126 | 0.620 | −0.012 | 0.961 |
| OA-EDV (cm/s) | −0.48 | 0.851 | −0.328 | 0.184 | −0.117 | 0.644 | −0.431 | 0.074 | 0.217 | 0.388 | 0.192 | 0.446 | −0.069 | 0.784 |
| OA-RI | 0.004 | 0.987 | 0.001 | 0.997 | 0.078 | 0.757 | 0.236 | 0.347 | −0.055 | 0.828 | −0.153 | 0.545 | 0.119 | 0.638 |
| SOV (cm/s) | −0.329 | 0.187 | 0.011 | 0.964 | −0.083 | 0.744 | −0.092 | 0.716 | −0.417 | 0.085 | −0.458 | 0.056 | −0.505 | 0.032 |
Abbreviations: CDI, color Doppler imaging; CRA, central retinal artery; EDV, end-diastolic velocity; HC, healthy age-matched control; OA, ophthalmic artery; PCA, posterior ciliary artery; P-ON, with previous optic neuritis; PSV, peak systolic velocity; RI, resistive(resistance) index; RNFL, retinal nerve fiber layer; SOV, superior ophthalmic vein. *P=rho=correlation coefficient, P**=P-value. Spearman's correlation test. All rho values are in italic to distinguish between P values and rho values.
Discussion
Optic nerve disease associated with MS results in a visual disturbance in most of the affected cases.16 Previously, MS was thought to be a disease of myelin, but in most of MS patients, neuronal and axonal loss also has been pathologically demonstrated in postmortem studies.2 Suggesting mechanisms of neuronal damage in MS other than demyelinization, Gordon-Lipkin et al17 reported the correlation between reduction of RNFL thickness and MRI-documented brain atrophy. Sepulcre et al18 demonstrated that decreased RNFL thickness, particularly in the temporal quadrant, is present in patients with MS regardless of past ON experience. Furthermore, Kurtzke et al14 reported the correlation between reduced RNFL thickness and the level of disability measured by the Kurtzke's EDSS score. Ratchford et al5 also found that in MS patients with nonocular disease activity, particularly in the early periods of disease course, accelerated GCIP thinning was exhibited.
In the current study, we found that decreased RNFL thickness is more significant in P-ON patients compared with WP-ON and healthy controls. To increase the reliability of data, only one eye of each case was evaluated in the study. Moreover, P-ON patients, WP-ON patients, and healthy controls were considered altogether. Thus, to our knowledge, this is the first well-organized study including the different groups at the same time. In accordance with the above-mentioned studies, our results demonstrated that the thinning of RNFL was observed in MS eyes. However, in contrast to the findings of Sepulcre et al,18 we found that these changes occurred nearly in all quadrants and solely in P-ON patients. The dissensus may stem from the observational approach employed in our study. It is not clear that whether findings would be different if a prospective approach had been deployed or if there were patients with longer disease course of MS and with higher EDSS score. Another important point is the differences in ON times of the P-ON eyes included in our study. However, as all MS patients have similar EDSS scores leading similar levels of disability, these differences may not be affecting the reliability of our study. Aging and interracial differences were also associated with RNFL thinning but our groups were all age matched and there were no racial differences. Furthermore, in some of the studies in literature, it has been advocated that in addition to RNFL atrophy,19 retinal periphlebitis might have a role in disease activity in MS. According to the above-mentioned studies, it is understood that retinal evaluation can be used as a surrogate marker of axonal damage in MS. However, there are some unclear points such as how often to measure the OCT parameters and how to effectively use OCT in treatment choice and follow-up activity. More detailed and comprehensive studies are needed to clarify those issues.
On the other hand, there is not sufficient research on vascular origins of ocular involvement in MS. Akarsu et al8 reported the impaired retrobulbar hemodynamics in 17 MS patients with past unilateral ON, especially in the posterior ciliary and central retinal arteries, compared with contralateral unaffected eyes as well as healthy controls. Similarly, Modrzejewska et al9 showed that significant disturbances in CDI parameters of orbital arteries exist in contralateral unaffected eyes as well compared with healthy controls. Hradílek et al10 also found pathophysiological changes during acute unilateral ON influence orbital hemodynamics in the OA in the eyes with ON; however, these changes did not persist over long periods. Karami et al11 compared orbital blood flow velocities of affected and unaffected eyes of 23 patients with acute unilateral ON. Contrary to previous studies, they concluded that orbital blood flow parameters were not related to ON. Moreover, according to other investigators, that is, Karaali et al,12 blood flow velocity increases in the OA in the initial period of acute inflammation of an optic nerve. Thus, there are conflicting results in literature about changes in orbital arterial hemodynamics in optic neuritis with MS. Recently, ‘cerebrospinal venous insufficiency' has been thought as an etiological factor in MS.20 There is no study analyzing changes for orbital venous circulation and to our knowledge this is the first study investigating this topic. In the present study, most of the retrobulbar blood flow velocity parameters and RIs, including SOV blood flow velocities, were comparable among groups. However, EDV in the OA in P-ON eyes was slightly lower than those of WP-ON eyes and healthy controls. As the vascular changes is minimal in the chronic phase after ON, slight decrease of EDV might be considered as significant data. On the other hand, we also have not found significant correlation between the reduction of RNFL thickness and ocular blood flow velocities. In our opinion, this is an insignificant finding alone by itself and should be supported by further data.
In P-ON eyes, disturbances in bulbar artery blood flow were shown using orbital Doppler ultrasound. The most reasonable theory explaining this situation is that nerve sheath thickening and inflammatory processes may cause the blood vessels within the scleral canal to be compressed and resistance in those vessels to increase.6, 10 Furthermore, in another study, it was demonstrated that increased plasma levels of endothelin-1, might have resulted in vasospasm and vascular dysregulation in MS patients.21 Therefore, vascular mechanisms may be important in the development of axonal and visual loss associated with ON and MS. One of the key issues is the duration between the appearance of symptoms of retrobulbar ON and blood flow velocity examination.12, 22 During Doppler ultrasound examinations in the study groups, patients went through remission of symptoms of ON. Disturbances of ocular blood flow might have been encountered if cases with acute ON had been included.
In conclusion, retrobulbar hemodynamics in the eyes with or without ON in MS does not change dramatically compared with healthy control eyes. Nevertheless, color Doppler should be kept in minds as a promising method of choice to follow-up the patients after ON. Thinning of the RNFL occurs particularly in eyes with P-ON. This finding might result from both disease-related neurodegeneration and direct inflammatory injury. SD-OCT offers an objective and quantitative tool that can be used for documentation of RNFL changes over time in MS. Limitations of our study include lack of cases with acute ON, lack of the prospective nature, and limited number of patients. In order to confirm the outcomes of this research, further studies with larger patient groups and prospective follow-up are still needed.
The authors declare no conflict of interest.
Footnotes
Disclaimer
The authors alone are responsible for the content and writing of the paper.
Meeting presentation: This study was presented in 46th Turkish Ophthalmology Society National Congress (17–21 October 2012, Antalya, Turkey) ‘Multiple Sklerozis'li ve Normal Sağlıklı Bireylerde Retina Sinir Lifi Tabakası ve Oftalmik Renkli Doppler Ultrasonografi Parametrelerinin Karşılaştırılması'.
References
- Cheng H, Laron M, Schiffman JS, Tang RA, Frishman LJ. The relationship between visual field and retinal nerve fiber layer measurements in patients with multiple sclerosis. Invest Ophthalmol Vis Sci. 2007;48 (12:5798–5805. doi: 10.1167/iovs.07-0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mörk S, Bö L. Axonal transection in the lesions of multiple sclerosis. N Engl J Med. 1998;338 (5:278–285. doi: 10.1056/NEJM199801293380502. [DOI] [PubMed] [Google Scholar]
- Fjeldstad C, Bemben M, Pardo G. Reduced retinal nerve fiber layer and macular thickness in patients with multiple sclerosis with no history of optic neuritis identified by the use of spectral domain high-definition optical coherence tomography. J ClinNeurosci. 2011;18 (11:1469–1472. doi: 10.1016/j.jocn.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Costello F, Hodge W, Pan YI, Eggenberger E, Coupland S, Kardon RH. Tracking retinal nerve fiber layer loss after optic neuritis: a prospective study using optical coherence tomography. Mult Scler. 2008;14 (7:893–905. doi: 10.1177/1352458508091367. [DOI] [PubMed] [Google Scholar]
- Ratchford JN, Saidha S, Sotirchos ES, Oh JA, Seigo MA, Eckstein C, et al. Active MS is associated with accelerated retinal ganglion cell/inner plexiform layer thinning. Neurology. 2013;80 (1:47–54. doi: 10.1212/WNL.0b013e31827b1a1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speciale L, Sarasella M, Ruzzante S, Caputo D, Mancuso R, Calvo MG, et al. Endothelin and nitric oxide levels in cerebrospinal fluid of patients with multiple sclerosis. J Neurovirol. 2000;6 (Suppl 2:S62–S66. [PubMed] [Google Scholar]
- Mancini M, Morra VB, Di Donato O, Maglio V, Lanzillo R, Liuzzi R, et al. Multiple sclerosis: cerebral circulation time. Radiology. 2012;262 (3:947–955. doi: 10.1148/radiol.11111239. [DOI] [PubMed] [Google Scholar]
- Akarsu C, Tan FU, Kendi T. Color Doppler imaging in optic neuritis with multiple sclerosis. Graefes Arch Clin Exp Ophthalmol. 2004;242 (12:990–994. doi: 10.1007/s00417-004-0948-1. [DOI] [PubMed] [Google Scholar]
- Modrzejewska M, Karczewicz D, Wilk G. Assessment of blood flow velocity in eyeball arteries in multiple sclerosis patients with past retrobulbar optic neuritis in color Doppler ultrasonography. Klin Oczna. 2007;109 (4–6:183–186. [PubMed] [Google Scholar]
- Hradílek P, Stourac P, Bar M, Zapletalová O, Skoloudík D. Colour Doppler imaging evaluation of blood flow parameters in the ophthalmic artery in acute and chronic phases of optic neuritis in multiple sclerosis. Acta Ophthalmol. 2009;87 (1:65–70. doi: 10.1111/j.1755-3768.2008.01195.x. [DOI] [PubMed] [Google Scholar]
- Karami M, Janghorbani M, Dehghani A, Riahinejad M. Orbital Doppler evaluation of blood flow velocities in optic neuritis. Korean J Ophthalmol. 2012;26 (2:116–122. doi: 10.3341/kjo.2012.26.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaali K, Senol U, Aydin H, Cevikol C, Apaydin A, Lüleci E. Optic neuritis: evaluation with orbital Doppler sonography. Radiology. 2003;226 (2:355–358. doi: 10.1148/radiol.2262011915. [DOI] [PubMed] [Google Scholar]
- Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005;58 (6:840–846. doi: 10.1002/ana.20703. [DOI] [PubMed] [Google Scholar]
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33 (11:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- Bude RO, Rubin JM. Relationship between the resistive index and vascular compliance and resistance. Radiology. 1999;211 (2:411–417. doi: 10.1148/radiology.211.2.r99ma48411. [DOI] [PubMed] [Google Scholar]
- Graves J, Balcer LJ. Eye disorders in patients with multiple sclerosis: natural history and management. Clin Ophthalmol. 2010;4:1409–1422. doi: 10.2147/OPTH.S6383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Lipkin E, Chodkowski B, Reich DS, Smith SA, Pulicken M, Balcer LJ, et al. Retinal nerve fiber layer is associated with brain atrophy in multiple sclerosis. Neurology. 2007;69 (16:1603–1609. doi: 10.1212/01.wnl.0000295995.46586.ae. [DOI] [PubMed] [Google Scholar]
- Sepulcre J, Murie-Fernandez M, Salinas-Alaman A, Garcia-Layana A, Bejarano B, Villoslada P. Diagnostic accuracy of retinal abnormalities in predicting disease activity in MS. Neurology. 2007;68 (18:1488–1494. doi: 10.1212/01.wnl.0000260612.51849.ed. [DOI] [PubMed] [Google Scholar]
- Ortiz-Pérez S, Martínez-Lapiscina EH, Gabilondo I, Fraga-Pumar E, Martínez-Heras E, Saiz A, et al. Retinal periphlebitis is associated with multiple sclerosis severity. Neurology. 2013;81 (10:877–881. doi: 10.1212/WNL.0b013e3182a3525e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter GM, Williamson TH. Color Doppler imaging of the eye: normal ranges, reproducibility, and observer variation. J Ultrasound Med. 1995;14 (2:91–96. doi: 10.7863/jum.1995.14.2.91. [DOI] [PubMed] [Google Scholar]
- Pache M, Kaiser HJ, Akhalbedashvili N, Lienert C, Dubler B, Kappos L, et al. Extraocular blood flow and endothelin-1 plasma levels in patients with multiple sclerosis. Eur Neurol. 2003;49 (3:164–168. doi: 10.1159/000069085. [DOI] [PubMed] [Google Scholar]
- Elvin A, Andersson T, Soderstrom M. Optic neuritis: Doppler ultrasonography compared with MR and correlated with visual evoked potential assessments. Acta Radiol. 1998;39 (3:243–248. doi: 10.1080/02841859809172188. [DOI] [PubMed] [Google Scholar]


