Abstract
During the 1970s and 1980s, a new approach to the integration of acute and long-term care(LTC) services was conceived and refined at On Lok, an organization in the Chinese community of San Francisco. Since then, On Lok and 10 Federal demonstration sites have tested this model which is today called the Program of All-inclusive Care for the Elderly (PACE). This program has gained considerable political support and as a result, the 1997 Balanced Budget Agreement establishes PACE as a permanent provider under Medicare. The Federal demonstration of PACE was designed as a voluntary program. By exploiting its voluntary enrollment design, this study analyzes the determinants of program participation within a group of screened applicants. Findings of this study support the theory that the capitated payment structure of PACE creates incentives for program staff to avoid costly individuals. However, home ownership and provider attachment also act as important and significant barriers to enrollment.
Introduction
PACE is an innovative program that provides acute and LTC services in a day-care setting for frail elders. During the 1970s and 1980s, the PACE approach was conceived and refined at On Lok, an organization in the Chinese community of San Francisco. In 1986, legislation was passed to support the replication of On Lok's model through Federal demonstration sites. The first of 10 such sites began operating in 1987. As of June 30, 1997, enrollment at these sites, as well as On Lok, had reached 3,524 persons. Today, 29 organizations in 16 States are operating under a Medicaid capitation waiver, or dual waivers for Medicaid and Medicare capitated payments, and another 38 are expected to be delivering services or exploring the feasibility of operation as PACE sites in the near future (National PACE Association, 1998). The 1997 Balanced Budget Agreement establishes PACE as a permanent provider under Medicare and allows States the option to pay for PACE services under Medicaid. The passage of this legislation tells of its political support because little evidence-based research regarding the program is available in the literature.
This study begins to address the paucity of research by analyzing the determinants of program participation within a group of program applicants. The PACE demonstration was designed as a voluntary program, and therefore the design presents the research opportunity of determining who is likely to participate in such a program. Such understanding is an important first step to understanding program impacts.
PACE seeks to insure the needs of elders who wish to continue to live at home and avoid nursing home placement but have health conditions that interfere with their ability to live independently. These programs seek to maintain an elder's health and functioning by integrating a range of preventive, acute, and LTC services. The distinguishing features of the PACE approach are:
A clientele consisting of impaired and frail elders who, despite living at home, are nursing-home eligible and likely to require care for the rest of their lives.
Provision of comprehensive medical and social services by a group of specialists (physicians, nurses, therapists, and social workers) working together as an interdisciplinary team.
The use of an adult day health center.
Continued community residence for most participants.
Capitation of Medicare and Medicaid payments at a fixed amount per client; individual PACE programs face the risk for the costs of participants' care, but are free of any service-by-service restrictions (Zimmerman et al., 1996).
The anticipated benefits of PACE are the avoidance of functional decline and costly nursing home services.
Although these distinguishing features create a unifying concept for PACE, there is variability among programs. Catchment and targeted populations vary, but programs also vary with regard to their attendance requirements at the day-health center and whether the program offers some type of housing arrangement.
Each program structures the provision of care around an interdisciplinary team. The team approach is used to facilitate the program's ability to address simultaneously the individual's medical, functional, and social needs. As a unit, the team is able to focus attention on the whole individual and reduce the fragmentation that exists among health care providers and between the health and social service delivery systems. Typically, teams meet daily to discuss cases, monitor, and adjust treatment plans. The average size of a PACE interdisciplinary team is 15 (ranging from 8 to 23) and consists of a center supervisor or center director who typically works as the team facilitator, social work staff, registered nurse or nurse practitioner, physician, home care personnel, personal care aide, recreation specialist, occupational and physical therapists, and, in most cases, a dietician. In some cases a chaplain, transportation specialist, or pharmacist may also participate in the team (Eng et al., 1997; Zimmerman et al., 1998).
These interdisciplinary teams provide care in the program's adult day-health center and as needed in the individual's home and inpatient facility. PACE participants attend these centers at least periodically throughout the week (on average 2-3 days per week), though some attend daily. A PACE center serves two functions. First, through its full-service medical clinic, it is the location of the participant's medical home. While at the center, the participant receives medical attention as necessary which may include the administration of medications, various forms of therapy, visits with any member of the individual's interdisciplinary medical team, and transportation to and from home and to off-site medical appointments. Second, the center also serves a social function. Many participants spend the entire day at the center socializing with other attendees and eating meals.
As described, the structure of PACE provides intensive monitoring of a participant's condition. More importantly, it provides ongoing care that allows participants to remain in the community. Costs within this system are managed through capitated reimbursement. During developmental stages, all sites receive capitated Medicaid payments. Those receiving Medicaid and Medicare capitated payments are considered fully developed PACE sites.
Capitated payments typically create incentives for programs to reach out and enroll the least costly members of a given population, while avoiding the most costly. This type of payment system may also induce a provider to trade off care that is cost-effective in the long term, for short-term cost considerations. However, capitated payments allow flexibility in the design of treatment plans, an extremely important consideration for a chronically ill population with complex needs. In interviews and observation-based studies of the interdisciplinary teams, Zimmerman et al. (1998) have found that service provision through the team is typically based on the team's understanding of long-term effectiveness of a given service. However, when a program faces financial difficulties, there is some evidence that short-term cost considerations may impinge on the team's decisions.
To date, little evidence-based research on the PACE program has been available. One early study compared PACE participants with a sample of elders in the 1985 National Nursing Home Survey (On Lok, 1993). This early study suggests that PACE participants were less dependent in the activities of daily living (ADLs) relative to individuals in nursing homes. Unfortunately, a nursing home population is not an ideal comparison group. Wiener and Skaggs (1995) suggest that the differences found in this study may only reflect systematic differences between PACE participants and nursing home residents, such as their motivation or ability to remain living in the community.
The following research addresses some of the limitations in this previous study of PACE participants by using a group of applicants who do not enroll as a comparison group. The data include all those who are eligible, but exclude those who do not apply or those whose application did not progress much beyond the referral stage. As a result, the current work is restricted to looking at the determinants of program participation within a sample of screened applicants.
Conceptual Framework
Although enrollment into a voluntary program might be treated as a consumer-choice problem, a program such as PACE has a relatively complex enrollment process which is managed by staff at each PACE site. The design of the program and its payment structure, coupled with application, assessment, and enrollment processes that are controlled by PACE program staff, open up the possibility for selection effects — systematic enrollment patterns that result in differences between participants and non-participants with regard to case mix and medical expenditures. In the following study, the analysis of selection effects is restricted. This study analyzes those effects that occur after the initial referral to the program.
Enrollment into a PACE program involves a sequential process. The individual is referred to the program, and if willing, he or she enters a process of learning about the program and its services. Simultaneously, program staff determine eligibility and assess service needs. Referrals come from a variety of sources such as providers, including the medical organization sponsoring the program, and family and friends.1 In 1995, when the 11 programs in the study were asked to rank referral sources by number of referrals, 4 programs cited family, friends, and self referrals as providing the most referrals; the sponsoring organization was cited by 4 other programs (Zimmerman et al., 1997). Other data compiled by Clark et al. (1996) indicate that in 1995, more than one-fourth of all referrals were made by family, friends, or oneself. Social service agencies accounted for 16 percent of all referrals, and home health agencies accounted for another 12 percent.
Local program staff followup on all referrals and determine eligibility, need, and interest in the program. During this follow-up period, the individual and his or her family are encouraged to visit the PACE facilities and meet staff and other participants. Program staff will also conduct one or two in-home assessments.
Because the marketing, assessment, and enrollment processes are operated by the individual PACE programs, the opportunity exists for program staff to encourage or discourage enrollment. Theory would suggest that the capitated payment mechanism would encourage staff to seek out the least costly applicants while avoiding the most costly. Also, capacity constraints may be an issue at some sites. PACE programs vary widely in the number of individuals they serve at a given point. The data used in this study cover a period when census numbers for programs grew from an average of about 214 (ranging from 101 to 404 individuals) to 314 individuals (ranging from 140 to 634). At no time during the data collection period did a PACE program maintain a waiting list.2 However, the absence of a waiting list does not necessarily mean that sites did not manage their participant census through other methods such as reduced or expanded referral and marketing efforts.
The data available for this study do not provide any information or evidence regarding the extent to which program staff may have influenced enrollment among particular types of applicants. Discussion therefore concentrates on the relationship between program enrollment and measurable characteristics of the individual.
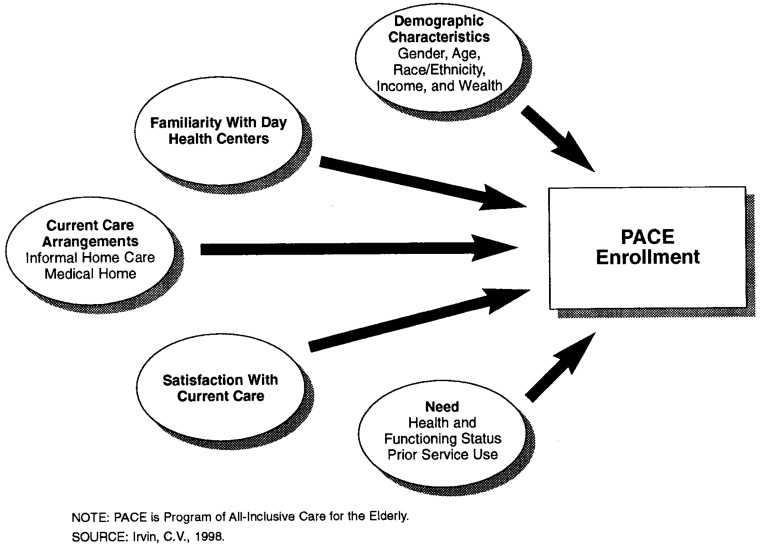
Five areas affect the individual's enrollment status: demographic background, familiarity with the day-health center concept, make-up of community-based assistance available to the individual, satisfaction, and need (Figure 1). In this study, demographic characteristics of the individual include such measures as gender, race or ethnicity, age, and schooling. Indicators of income and wealth are measured by home ownership and receipt of Medicaid benefits.
Figure 1. Conceptual Framework of PACE Enrollment.
Familiarity with the day-health center concept is also likely to influence an individual's enrollment decision. Those unfamiliar with a service are less likely to use it or purchase it, particularly one that involves a dramatic change in their medical-care arrangements. During the application process individuals are exposed to various forms of marketing including visits to the PACE site to see the facilities and meet current participants. However, individuals considering these programs are also likely to be influenced by any prior experiences they may have had with the day-center concept, either through direct participation or through friends who have used other similar types of centers.
Because PACE is a community-based service system, an individual's community-based arrangements at the time of the application represents an alternative service system to the PACE program. Individuals who can obtain care through a variety of home-care arrangements and a community-based medical home, are likely to be less willing to change those arrangements (particularly if they are satisfactory arrangements) for a program such as PACE.
Although all individuals have some system of care available to them, their level of satisfaction with their current arrangements is likely to influence the likelihood of entering a program like PACE. Those who are satisfied with their current medical care arrangements can be expected to see little reason to make dramatic changes in those arrangements.
Lastly, the needs of an individual are likely to influence enrollment. Individuals eligible for PACE must be certified by the State as meeting care requirements for skilled nursing facilities (SNF). These requirements vary by State, but generally imply that the eligible population is frail and has complex and LTC requirements. Within the eligible population, needs will vary as conditions and functioning status vary in type and acuity. As a result, need in this framework is a complex concept that covers measures of health and functioning status. Functioning status is an important inclusion because frailty is closely associated with an individual's ability to carry out routine activities. Also, as functioning declines, the need for more intensive and ongoing care increases. Prior use of medical-care services is also included in this part of the model. They are a direct measure of need, and prior service use is a predictor of future use. How the various measures of need are related to enrollment will indicate the nature of selection effects that PACE programs experience after an individual has progressed past the initial referral stage.
Study Sample
A survey of PACE applicants at On Lok and 10 dually capitated3 PACE demonstration sites began in early January 1995. The survey was administered as an in-person interview in the applicant's home. Although the desired respondent was the applicant, not all applicants could complete the interview. The interview began with a 10-question Mental Status Questionnaire, and if the applicant was unable to answer at least 5 questions accurately, the interview would proceed with a proxy, typically the applicant's primary caregiver. Approximately one-fourth of the surveys were completed in their entirety by proxies. Because a caregiver was frequently in the room during the interview, it was not uncommon for him or her to answer at least a portion of the questions, particularly when the applicant was having difficulties answering a question. Interviewers were asked to record the proportion of questions answered by proxies and, according to these interviewer notes, in approximately 45 percent of interviews, proxies answered 50 percent or more of the questions.4
This study uses data from the baseline survey which was administered early in the application process. Individuals who were asked to participate in the baseline survey had been referred to the program and passed the site's initial eligibility determination process. If the referred person appeared to be eligible and interested in the program, PACE staff would arrange for an initial in-home assessment. As previously noted, eligibility is based on the following elements: The individual is at least 55 years of age, resides in the catchment area, is eligible for Medicare and Medicaid benefits or for Medicare and willing to pay the monthly costs of participation for those not eligible for Medicaid, certified by the State as meeting the SNF level of care requirements, and has the potential to remain in the community with assistance. After making an initial determination of eligibility and to see if the individual would be willing to consider the program further, PACE staff conducting the home assessment would ask the applicant to participate in the baseline survey. As a result, the baseline survey occurred near the time of the initial in-home assessment.
From January 1, 1995 through February 28, 1997, 3,009 individuals were recorded as having been referred, determined to be eligible, and expressed an interest in considering the program across the 10 PACE sites and On Lok (Table 1). Within this sample, 44 percent completed the baseline interview. The rate of completed surveys varied considerably over the 11 sites from a low of 10 percent to a high of 91 percent (Technical Note). The low response rate and variation in response rates across the sites are likely a result of certain population characteristics and the survey's reliance on local program staff to encourage participation in the survey. As at any medical facility, PACE program staff face considerable burdens and soliciting participants for a survey only increases that burden.
Table 1. PACE Enrollment, by Survey Response: January 1,1995 Through February 28,1997.
| Status | Survey Respondents | Percent | Survey Non-Respondents | Percent | All Applicants | Percent |
|---|---|---|---|---|---|---|
| PACE Enrollees | 909 | 68 | 1,019 | 61 | 1,928 | 64 |
| PACE Decliners | 399 | 30 | 573 | 34 | 972 | 32 |
| Status Unknown1 | 28 | 2 | 81 | 5 | 109 | 4 |
| All Applicants2 | 1,336 | 100 | 1,673 | 100 | 3,009 | 100 |
Some PACE applicants have unknown status because of incomplete information received from sites or because they died within 3 months of the home visit date and possibly did not have enough time to make an enrollment decision.
Applicants are those individuals who receive the initial home visit and are deemed eligible for PACE by February 28, 1997.
NOTE: PACE is Program of All-inclusive Care for the Elderly.
SOURCE: PACE Tracking File, Abt Associates Inc., 1997.
Limitations of the Data
As a result of the referral and determination processes, the sample of individuals asked to participate in the survey is likely to include a number of biases. First, the individual was necessarily referred to the program. No information is available on those who were eligible during this period but not referred. Those not referred may include individuals who have satisfactory and stable care arrangements and may be less likely to enroll, those who have providers and caregivers who are unaware of the program, or those with minimal access to care who may be more likely to enroll.
After the referral, program staff would attempt to determine eligibility immediately. It is a relatively straightforward process to determine age, Medicare and Medicaid eligibility, and SNF certification. All individuals in the sample meet these eligibility criteria. However, the assessment of needs and the potential to remain in the community with assistance may be difficult and subjective. The point at which a site determines need and the appropriateness of an individual's community-based assistance may vary across sites, and probably varies by the individual. Some portion of the sample may include individuals determined to be ineligible on a basis of need, if that determination were made late in the application and enrollment process. However, sites were asked to identify such cases regardless of the individual's survey participation status, and those identified were eliminated from the study.
As program staff were determining eligibility, they were also determining whether the individual was interested in considering PACE. Those turning down program services before or during the initial in-home assessment were not asked to participate in the survey and are therefore excluded from the sample. It is not necessarily clear how this exclusion biases the data. Clearly, this group represents part of the non-participant population. However, because program staff did not have the opportunity to conduct a full eligibility determination, some proportion would have been found ineligible.
As a result of these sample selection issues, our analysis is restricted to one that looks at the determinants of program enrollment among applicants who have been initially screened by the program and who were willing to consider program services after the initial referral. Had PACE been subject to an experimental design, an enrollment study would not have been possible and policymakers would not understand who would enter PACE in practice. Given that PACE is voluntary, the construction of a reasonable comparison group is required to analyze selection and impacts. Screened applicants who do not enroll represent the comparison group in this study. Although the ideal comparison group would have been a random sample of eligibles not participating in PACE, a sample of screened applicants who do not enroll represents those individuals in the eligible population who are likely to be most similar to PACE participants. If the comparison group in this sample is more similar to PACE participants than the general population of non-participating eligibles, then it will be more difficult to detect differences in this sample when differences exist in the entire eligible population.
Nevertheless, the overall response rate causes questions to arise regarding the generalizability of the survey data. Of the 3,009 persons in the initial sample, 64 percent joined the PACE program and 32 percent did not (Table l).5 Among those applicants completing the survey, 68 percent enrolled compared with 61 percent of non-respondents. Higher enrollment rates among survey respondents were seen at all but one site (Technical Note).
The disparity in enrollment rates between survey respondents and non-respondents suggests potential biases associated with completion of the survey. Using data from the Medicare eligibility database and Medicare claims, we are able to measure differences between survey respondents and non-respondents in regard to gender, age, participation in a risk-based or cost-based group health plan, the death rate within the 3 months following the initial home visit, and total Medicare reimbursements during the 6 months prior to the individual's application to the program.6 Respondents are substantially more likely to be female (70 percent compared with 59 percent), 1 year younger on average, and are less likely to have been in a group health plan prior to their application to PACE (Table 2). Survey respondents had a 3-month death rate of 41 per 1,000, a rate that is not statistically different from the rate among non-respondents, which is 52 per 1,000. Reimbursements during the prior 6 months, which averaged between $11,304-$11,491, also are not statistically different across the two groups.7
Table 2. Characteristics and Medicare Reimbursements, by Survey Response.
| Characteristics | Survey Respondents | Survey Non-Respondents | Difference |
|---|---|---|---|
| Percent | |||
| Female | 69.8 | 59.2 | *10.6 |
| Age at Home Visit | |||
| Under 75 Years | 36.6 | 24.5 | — |
| 75-84 Years | 38 | 37.1 | — |
| 85 Years or Over | 25.4 | 26.4 | — |
| Missing | 0.1 | 12.1 | — |
| Mean Years | 78 | 79 | *-1 year |
| Percent | |||
| Participation in Group Health Plan 6 Months Prior to Application | |||
| Risk-Based | 7.5 | 13.9 | *-6.4 |
| Cost-Based | 1.5 | 4.4 | *-2.9 |
| Death Rate Within 3 Months of Home Visit | 41/1,000 | 52/1,000 | -11/1,000 |
| Average Medicare Reimbursements 6 Months Prior to Application1 | $11,304 | $11,491 | -$187 |
| Number of Observations | 1,289 | 1,423 | — |
Statistically significantly different from 0 at *p=0.001.
Reimbursements exclude those in risk- or cost-based group health plans.
NOTE: PACE is Program of All-Inclusive Care for the Elderly.
SOURCE: Merged PACE Tracking File and Medicare claims, Abt Associates Inc., 1997.
These few measures of characteristics indicate some differences. Also, the study sample is likely to underrepresent men and those in group health plans. Although the following analysis attempts to address these issues in a variety of ways, we have no reason to believe that the conceptual framework would differ if the response rate had been greater. In addition, it is not clear how an individual's decision to respond to the survey is related to his or her decision to enroll. It is likely that the relationships estimated using the sample are at least reflective of the true relationships in the population, but that the estimated magnitudes of these relationships are biased by some factor.
Respondent Characteristics
Based on our conceptual framework, the study focuses on the relationship between enrollment and demographic characteristics, familiarity with day-health centers, current community-based care arrangements, and need (as defined by health and functioning status and prior use of services) among survey respondents. The measures for these characteristics are described below. Response frequencies for these characteristics are presented in Table 3. These frequencies not only profile the individuals in the sample, but also allow comparisons between this sample and other samples of frail elders discussed and described in the literature.
Table 3. Respondent Characteristics.
| Variables | Survey Respondents1 |
|---|---|
|
| |
| Percent | |
| Sociodemographics | |
| Gender | |
| Female | 69.7 |
| Race or Ethnicity | 38.6 |
| White (Not Hispanic) | 33.1 |
| Black (Not Hispanic) | 19.8 |
| Hispanic | 7.0 |
| Other | 1.5 |
| Missing | |
| Average Age | 77.8 years |
| Income and Wealth | |
| Owns Home | 24.7 |
| Medicaid Beneficiary | 80.3 |
| Familiar With Day Health Centers | 15.3 |
| Regularly Attends Senior Center | |
| Community-Based Assistance | |
| Informal Caregiver | |
| Residential | 64.8 |
| Non-Residential | 47.9 |
| Person Who Shares the Most Responsibilities for Overall Care | |
| Spouse | 13.4 |
| Daughter or Daughter-in-Law | 36.5 |
| Son or Son-in-Law | 10.4 |
| Sibling | 4.0 |
| Other | 14.8 |
| No one | 18 |
| Missing | 2.1 |
| Has Usual Doctor | 80.4 |
| Satisfaction | |
| If you could enroll in a health program that provided for all your health care needs, how likely would you be to change to another doctor or medical professional? | |
| Likely | 75.0 |
| Unlikely | 14.3 |
| Missing | 10.7 |
| Indicators of Service Needs | |
| Current Health Status2 | |
| Excellent/Very Good | 14.4 |
| Good | 26.2 |
| Fair | 33.0 |
| Poor | 23.2 |
| Missing | 3.2 |
| Utilization In Prior 6 Months | |
| Hospitalized | 45.3 |
| Nursing Home Admission | 14.7 |
| Average Number of Dependencies3 | |
| Activities of Daily Living4 | 2.7 |
| Instrumental Activities of Daily Living5 | 5.7 |
| Cognitive Impairment6 | 25.3 |
N=1,308
Proxy assessment if survey answered by proxy.
Usually requires that either someone assist in the activity or that someone be in the room to provide assistance.
Includes: bathing, dressing, grooming, walking, toileting, transferring, and eating.
lncludes: shopping, housework, transportation, laundry, meal preparation, money management, and medication.
Scored 5 or more incorrect responses, out of 10, on Mental Status Questionnaire (MSQ).
NOTE: PACE is Program of All-Inclusive Care for the Elderly.
SOURCE: PACE Applicant Survey, January 1995 - February 1997.
The majority of survey respondents are women and from minority groups (Table 3). It is not surprising that survey respondents are predominately women; disability is more prevalent among women, they are disabled for longer periods, and widowhood increases the need for non-family care options (Manton et al., 1993). However, respondents appear to be unique compared with other samples of the frail elderly regarding their racial and ethnic background. Kemper (1992) and Applebaum (1988) found that among elders applying to the Channeling Demonstration, 72 percent were female and slightly more than one-fourth were minorities. In addition, only 22 percent were Medicaid beneficiaries and 57 percent reported their only asset as their house. Bauer (1996), in a recent study of the Arizona Long-Term Care System (ALTCS), drew a sample of beneficiaries where 33 percent were minorities and nearly one-fourth owned their homes.
In an article by PACE physicians (Eng et al., 1997), the authors note that currently PACE has primarily attracted low-income individuals. The data here confirm that understanding. Approximately 80 percent of these applicants were Medicaid beneficiaries and only one-fourth own their home at the time of application.
The data contain little information on the individual's or family's familiarity with day-health centers in general and PACE in particular. Although respondents completed the baseline survey at approximately the same point in the assessment and enrollment process, sites varied in their strategies for marketing and dissemination of information about the program. The little information available is unreliable and not a direct measure of understanding. Respondents were asked to cite the five most positive aspects of PACE, as well as the five most negative aspects. Approximately 29 percent did not provide an answer when asked about the positive aspects; the most common answer among responders was “medical services.” When asked about negative aspects, 80 percent did not or could not cite a reason; among responders the most common response was “inadequate services or benefits.” The one aspect of familiarity that can be measured in these data is whether the individual had previous experience with day centers. Among survey respondents, approximately 15 percent were usually attending a senior day center, day-health center, or some other type of social center at the time of the survey. Individuals who are familiar with various aspects of center-based services may view PACE as a familiar concept.
As mentioned previously, one aspect of eligibility for PACE is that the individual has the potential to remain in the community with assistance. Approximately 65 percent of the sample rely on informal caregivers who live with the respondent, 48 percent have informal caregivers who live elsewhere.8 When asked about the person who shares the most responsibilities for the respondent's care, approximately 37 percent cited a daughter or daughter-in-law whereas 13 percent said a spouse was the person.
Alternatively, community-based assistance can be measured by whether the individual is attached to a medical home, i.e., has an established relationship with a physician. For those without a medical home, entrance into PACE would address a fundamental barrier to care. Those with an established medical home are usually required to end that relationship upon entrance into the program. Once in PACE, their care is managed by the interdisciplinary team who only serve PACE participants. The physician on the team provides primary care services including inpatient services as appropriate. Specialty physician services are supplied through physicians who contract with the programs (Eng et al., 1997). 9 Although many individuals may be reluctant to make this type of change in their care and 80 percent of survey respondents have a usual physician, 75 percent of the study sample indicated they would be likely to change to another doctor or medical professional if they could enroll in a health program that provided for all their health care needs.
The data available for this study are particularly rich in measures of service needs. Current health status is a self-assessment of current health. Only 14 percent report excellent and very good health, 26 percent report good health, and 33 percent and 23 percent report fair to poor health respectively. An alternative way of measuring health-care needs or the severity of clinical conditions is to examine medical care utilization patterns. Prior utilization patterns are also good predictors of current and short-term future patterns. The frailty of the survey respondents is shown by the relatively common occurrence of hospital and nursing home admissions (45 percent and 15 percent respectively). In more general samples of the elderly, between 23 percent (Manton et al., 1993) and 39 percent (Harrington et al., 1993) are hospitalized in a given 12-month period. In Kemper's (1992) sample from the Channeling experiment, 48 percent had a previous hospitalization, whereas Bauer (1996) found a 6-month hospitalization rate of 53 percent among ALTCS beneficiaries.
Functioning is measured by dependencies in the activities of daily living (ADL) and instrumental activities of daily living (IADL). Each category contains seven activities: eating, toileting, dressing, bathing, grooming, transferring, and walking. The IADLs include shopping, housework, transportation, laundry, meal preparation, money management, and medication. Dependency in this instance is defined to reflect those individuals who usually require that either someone assist in the activity or that someone be in the room to provide assistance if required.10 Of the seven activities measured, the average respondent has approximately three dependencies in the ADLs (2.7). Slightly more than one-fourth of respondents have five or more dependencies in these activities. In the sample that Bauer (1996) used to analyze the ALTCS program, the average number of ADL dependencies was three. Within the sample of applicants to the Channeling Demonstration, approximately 54 percent had three or fewer dependencies out of the five activities measured. Among PACE applicants, dependencies in the seven IADLs is more common. On average, respondents report close to six dependencies (5.7) and 80 percent have five or more.
Cognitive impairment is also relatively common at one-fourth of the sample. In this instance impairment is defined as scoring at least 5 incorrect responses out of 10 on a Mental Status Questionnaire that was administered at the beginning of the interview. When an individual failed to answer at least five questions correctly, the interviewer asked to interview a knowledgeable proxy respondent. Even though only 25 percent of the sample answered at least five questions incorrectly, approximately 45 percent of the interviews were completed by proxies or proxies answered more than 50 percent of the survey questions.
Characteristics Associated with Enrollment
Logistic regression modeling was used to analyze the relationships between enrollment in PACE and an individual's demographic characteristics, familiarity with day health centers, current care arrangements, satisfaction, and need. Two estimated models are presented in Table 4. The first and third columns present estimated coefficients and their standard errors for each model. The second and fourth columns translate the estimated coefficient into their marginal effects.11 The first set of estimated coefficients and marginal effects is the unweighted variant of the model. In the second model, the data are weighted to account for the different response rates across the 11 programs (Appendix). In this second model, observations from sites with below-average response rates receive greater weight relative to those from sites with above-average response rates. As a result, the data in the weighted model are transformed such that the proportional representation of each site in the data is equivalent to its proportion of total applicants eligible for the survey during the survey period. This weighting methodology therefore only addresses the differences in response rates across the sites, but does not address the overall low response rate.12
Table 4. Logistic Model of PACE Enrollment.
| Variable | Unweighted Estimated Coefficient Marginal | Weighted Estimated Coefficient Marginal | ||
|---|---|---|---|---|
| (Standard Error) | Effects1 | (Standard Error) | Effects1 | |
| Sociodemographics | ||||
| Female | 0.233 (0.156) |
0.047 | 0.168 (0.158) |
0.033 |
| Black | -0.026 (0.179) |
-0.005 | 0.166 (0.193) |
0.033 |
| Hispanic | -0.21 (0.252) |
-0.042 | 0.003 (0.27) |
0.00 |
| 85 Years of Age or Older | -0.074 (0.16) |
-0.015 | -0.083 (0.163) |
-0.016 |
| Widowed | 0.23 (0.154) |
0.046 |
**0.349 (0.158) |
0.069 |
| Fewer Than 12 Years of School |
*0.275 (0.15) |
0.055 | 0.242 (0.149) |
0.048 |
| Household Size | 0.077 (0.057) |
0.015 | 0.053 (0.06) |
0.01 |
| Own Home |
**0.353 (0.158) |
-0.071 |
***-0.616 (0.165) |
-0.122 |
| Medicaid Beneficiary | 0.199 (0.171) |
0.04 |
***0.473 (0.182) |
0.094 |
| Familiar with Day Health Centers | ||||
| Usually Attends a Senior Day Center |
***1.363 (0.25) |
0.275 |
***1.063 (0.201) |
0.211 |
| Current Care Arrangements | ||||
| Residential Informal Home Care | -0.212 (0.203) |
-0.043 |
*-0.337 (0.202) |
0.067 |
| Non-Residential Informal Home Care | -0.032 (0.142) |
-0.006 | -0.239 (0.147) |
-0.047 |
| Daughter Shares Most Responsibilities | -0.026 (0.151) |
-0.005 | -0.059 (0.157) |
-0.012 |
| Has usual physician |
*-0.334 (0.179) |
-0.067 | -0.071 (0.175) |
0.014 |
| Satisfaction | ||||
| Dissatisfied with Quality of Medical Care | 0.157 (0.229) |
0.032 | 0.215 (0.237) |
0.043 |
| Unlikely to be Willing to Change Providers |
***-0.798 (0.187) |
-0.161 |
***-0.723 (0.178) |
-0.143 |
| Health and Functioning | ||||
| Report at least Good Health | -0.13 (0.141) |
-0.026 | -0.059 (0.145) |
-0.012 |
| Died Within 3 Months of Interview |
***-1.070 (0.37) |
-0.216 |
***-1.296 (0.387) |
-0.257 |
| Number of ADL Dependencies | 0.00 (0.036) |
0.00 | -0.045 (0.038) |
-0.009 |
| Number of IADL Dependencies |
**0.114 (0.045) |
0.023 |
***0.151 (0.045) |
0.03 |
| Cognitively Impaired | 0.016 (0.167) |
0.003 | -0.153 (0.18) |
-0.03 |
| Prior Utilization of Medical Care Services2 | ||||
| Hospital Admission | 0.043 (0.163) |
-0.009 | 0.203 (0.167) |
0.04 |
| Nursing Home Admission | 0.139 (0.207) |
0.028 | -0.017 (0.205) |
-0.003 |
| Medicare Reimbursements3 | ||||
| Second Quartile | -0.166 (0.203) |
0.033 | -0.17 (0.208) |
-0.034 |
| Third Quartile | -0.231 (0.216) |
-0.047 |
*-0.402 (0.232) |
-0.08 |
| Fourth Quartile |
**-0.591 (0.234) |
-0.119 |
**-0.587 (0.246) |
-0.116 |
| In a Group Health Plan | 0.254 (0.276) |
-0.051 | -0.234 (0.229) |
-0.046 |
| Time Trend |
**0.024 (0.01) |
0.005 | -0.00 (0.009) |
-0.00 |
| Site Effects | ||||
| Site 2 | -0.402 (0.516) |
-0.081 | 0.194 (0.38) |
0.038 |
| Site 3 | -0.519 (0.564) |
-0.105 | -0.305 (0.347) |
-0.06 |
| Site 4 | -0.254 (0.484) |
-0.051 | 0.007 (0.356) |
0.001 |
| Site 5 |
**-1.118 (0.478) |
-0.226 |
***-0.978 (0.333) |
0.194 |
| Site 6 |
**-1.089 (0.487) |
-0.22 |
***-1.046 (0.323) |
-0.208 |
| Site 7 | -0.378 (0.531) |
-0.076 | -0.435 (0.406) |
-0.086 |
| Site 8 | -0.32 (0.601) |
-0.065 | -0.254 (0.333) |
-0.05 |
| Site 9 | -0.574 (0.528) |
-0.116 | -0.482 (0.367) |
-0.096 |
| Site 10 | -0.201 (0.503) |
-0.04 | -0.072 (0.387) |
-0.014 |
| Site 11 | -0.023 (0.566) |
-0.005 | -0.045 (0.449) |
-0.009 |
| Intercept | 0.415 (0.572) |
0.319 (0.451) |
||
| Log-Likelihood | -696.987 | -680.88 | ||
| Number of Observations | 1,261 | 1,261 | ||
| Mean of Dependent Variable | 0.693 | 0.693 | ||
Statistically significantly different from 0 at the 0.10 level.
Statistically significantly different from 0 at the 0.05 level.
Statistically significantly different from 0 at the 0.01 level.
The marginal effect for characteristic i is δi = Λ(β'x)(1-Λ(β'x))βi where Λ is the logistic cumulative distribution function and βi, is the estimated coefficient for characteristic i.
AII measures are based in the 6-month period prior to the interview. Service use is self-reported. Medicare reimbursements are from Medicare claims files.
First Quartile: $0 to $255.19. Second Quartile: $255.20 to $3,365.90. Third Quartile: $3,365.91 to $14,349.40. Fourth Quartile: $14,349.41 to $138,115.51.
NOTE: PACE is Program of All-Inclusive Care for the Elderly.
SOURCE: PACE Applicant Survey, January 1995 - February 1997.
The models indicate that the demographic background of an individual demonstrates few relationships to enrollment. The results showing that those slightly more likely to enroll had lost a spouse, had fewer than 12 years of school, or received Medicaid benefits at the time of application are suggestive but not robust. The one robust finding is that home ownership is a significant predictor of enrollment. The percent of home owners who enroll in PACE is between 7-12 percentage points less than those who do not own a home, all else equal.
Familiarity with the concept of a day-health center is also a significant and robust predictor of enrollment. Those reporting that they regularly attended a senior center or a day-health center have a rate of enrollment that is 21-28 percentage points greater than those not regularly attending.
The characteristics of an individual's current care arrangements are not predictive of enrollment. The results are suggestive which show that having an informal live-in caregiver or having an established relationship with a physician before application reduces the probability that an individual will enroll. However, these results are sensitive to model specification. The data are relatively rich in the number of different measures that might be used to characterize care arrangements. Different measures of informal and formal home care were constructed and tested in the model (e.g., number of hours of care in total and by type), but none was found to be predictive.
One aspect of satisfaction is associated with enrollment. Individuals who indicate that they are unlikely to enroll in a health program that provides for all their healthcare needs if they are required to change to another doctor or medical professional have a rate of enrollment that is 14-16 percentage points less than others, all else equal. For most individuals, entrance into PACE requires them to leave an established relationship with a primary-care physician, and these results indicate that individuals can be reluctant to make that type of change, despite the promise of more comprehensive, better coordinated care.
The models contain a number of measures of need, including those of health and functioning status, and use of services and Medicare reimbursements prior to application to the program. One measure of health status is whether the individual died within 3 months of the interview. Although a few of these individuals may have died because of an accident or a sudden and dramatic change in health, we theorize that most were declining in health in the months before death and that this indicator is a proxy measure for that decline. This measure is a robust predictor of enrollment. Those who died within this period have a rate of enrollment that is 22-26 percentage points less than survivors.13 Functioning status with regard to the IADLs is also a robust predictor; individuals with more dependencies in the seven IADLs are significantly more likely to enroll.
Service utilization in the 6 months before the interview are not predictive of enrollment, except as this utilization relates to Medicare payments during this period. Individuals in the top quartile of Medicare payments (ranging from $14,349 to $138,116 over 6 months) are significantly less likely to enroll. Those with payments in this range have a rate of enrollment that is 12 percentage points less than those with payments in the first quartile (payments ranging from $0 to $255). When the data are weighted, the relationship between prior payments and enrollment becomes somewhat more distinct as those with payments in the third quartile (ranging from $3,366 to $14,349) are shown to be less likely to enroll relative to individuals in the first quartile.
The models also include a time trend. As previously noted, the sample was accumulated over a 2-year period, from January 1995 through the end of February 1997. In the data it is apparent that enrollment rates within the sample increased over time, though it is not clear why this happened. The time trend controls for this pattern in the data. When the unweighted model is estimated, the trend is a positive and significant predictor of enrollment; in the weighted model the sign on the estimated coefficient changes and it is not predictive of enrollment. Because the weights change the proportional representations of the sites in the data, it is likely that the time trend reflects site-specific effects that are not otherwise controlled for in the model.
Lastly, site-specific differences in enrollment only appear at two sites, sites 5 and 6. This result confirms what was seen in the data (Technical Note). It is interesting to note that when the unweighted model was estimated without the site-specific controls, the results associated with the remaining variables did not qualitatively change.
Conclusions
It would appear that PACE is experiencing favorable selection effects, at least among those individuals who are referred, screened, and willing to consider program services. Within this group of applicants, those with the greatest Medicare expenditures and in the last months of life are the least likely to enroll. This finding supports the theory that capitated payments induce the avoidance of the costliest individuals.
This study also highlights three other important findings. First, home ownership is an important signal that an individual will be significantly less likely to enroll in PACE. In the conceptual framework, ownership of a home is treated as a measure of wealth and this finding suggests that higher-income individuals are relatively less likely to enter PACE. Prior qualitative analyses of PACE discuss how it has primarily served low-income individuals (Eng, et al., 1997, and Kane et al., 1992). This is partly because of the design of the program, an integration of Medicare and Medicaid benefits. The pattern of attracting low-income frail elders continues to be confirmed in this study sample where 80 percent are Medicaid beneficiaries and only one-fourth own their home.
Second, prior attendance at a senior day center or other type of day-health center is a significant signal that an individual will enroll in PACE. These individuals are familiar with the day-health center concept and are likely to quickly understand and appreciate the PACE concept. It is likely that PACE provides a competitive alternative to other types of day-health centers. However, because PACE has the ability to offer a more complete range of services, and the capitated payment structure allows flexibility in treatment plans, it may be the case that as an individual's functioning and health status declines, it is appropriate to move to a more comprehensive program.
Third, attachment to an established provider-patient relationship would appear to be an important barrier to enrollment in PACE. From the very beginning of the 10 Federal demonstrations, PACE had anecdotal information from numerous applicants that this barrier existed (Kane et al., 1992). The findings here support that early anecdotal evidence. This finding is not surprising given the complexity of an applicant's medical needs and the time and effort required for a provider to understand this complexity. It is likely to be the case that PACE will continue to a face this barrier to enrollment into the future. As increasing proportions of the elderly experience capitated health services programs, either through Medicaid managed-care programs or increasing prevalence of Medicare managed-care contracts, it is unclear how the relationship between provider attachment and PACE enrollment will be affected. If these programs are more likely to disrupt established patient-physician relationships, then the issue of provider attachment is likely to become less important However, if Medicaid and Medicare capitated programs create barriers to disen-rollment from these plans, then provider attachment will continue to be an important barrier to PACE enrollment and may actually become more important over time.
It would be incorrect to consider this study as definitive. Prior medical costs only reflect Medicare spending. In the study sample, 80 percent of applicants are Medicaid beneficiaries. Although Medicare costs may dominate total spending for those dually eligible for Medicare and Medicaid, the omission of prior Medicaid spending means the data do not offer a complete picture of medical spending just prior to the application to PACE. Also, the finding that those with high levels of dependency in the IADLs are relatively more likely to enroll, offers some contradictory evidence. This finding suggests that the need for assistive services and ongoing monitoring of daily activities among PACE enrollees may be considerable. Although needs for assistance in the IADLs may be considerable and long-term, these are not particularly costly services when compared with a hospitalization or nursing-home admission.
Lastly, the comparison between program participants and non-participants is only one aspect of selection. Another involves determining which individuals are long-term participants (Riley et al., 1989 is an example of such a study). Voluntary capitated programs are not only interested in determining which individuals enroll, but also which individuals become long-term participants. The daily census of PACE will be dominated by long-term participants, and if these individuals have particular health characteristics (e.g., more likely to be cognitively impaired), over time program services may be structured to better meet the needs of these individuals. A full study of selection would look not only at the determinants of enrollment, but include an analysis of duration of participation.
Technical Note
Survey Response Rates by Site.
| Site | Number of Applicants (Percent of Total) |
Number of Survey Respondents (Percent of Total) |
Response Rate | Enrollment Rate | |
|---|---|---|---|---|---|
|
| |||||
| Respondents | Non-Respondents | ||||
|
| |||||
| In Percent | |||||
| 1 | 300 (10.0) |
42 (3.1) |
14.0 | 78.6 | 74.8 |
| 2 | 194 (6.4) |
94 (7.0) |
48.5 | 73.4 | 57.0 |
| 3 | 367 (12.2) |
57 (4.3) |
15.5 | 71.9 | 64.2 |
| 4 | 383 (12.7) |
349 (26.1) |
91.1 | 73.1 | 41.2 |
| 5 | 303 (10.0) |
196 (14.7) |
64.7 | 56.6 | 47.7 |
| 6 | 272 (9.0) |
104 (7.8) |
38.2 | 53.8 | 45.8 |
| 7 | 150 (5.0) |
75 (5.6) |
50.0 | 74.7 | 84.0 |
| 8 | 394 (13.1) |
39 (2.9) |
10.0 | 69.2 | 64.2 |
| 9 | 236 (7.8) |
80 (6.0) |
33.9 | 66.3 | 46.8 |
| 10 | 286 (9.5) |
241 (18.0) |
84.3 | 66.8 | 48.9 |
| 11 | 124 (4.1) |
59 (4.4) |
47.6 | 79.7 | 64.6 |
|
| |||||
| Total | 3,009 (100.0) |
1,336 (100.0) |
44.4 | 68.0 | 60.9 |
Acknowledgments
Helpful comments were received from Gary Gaumer, David Kidder, Robert Schmitz, Nancy Burstein, Nancy Miller, Yvonne Zimmerman, Alan White, and Elizabeth Goldstein. Louise Hadden and Elizabeth Axelrod provided expert programming.
Footnotes
The authors are with Abt Associates. This research was funded by the Health Care Financing Administration (HCFA) under Contract Number 500-91-0027. The statements contained herein are those of the authors and do not necessarily reflect the views or policies of HCFA.
Of the 11 programs in this study, 7 are sponsored by a medical organization such as an acute-care hospital or a community-based provider.
Some programs maintain waiting lists of program participants for housing slots. In one instance, individuals waited up to 2 years for a slot.
These sites receive capitated payments for Medicaid and Medicare.
The data do not indicate which questions were answered by a proxy and which by the applicant.
The status of 4 percent of all individuals in this sample is unknown. In approximately one-half of these cases, the individual died within 3 months of the home visit.
Because of an inability to match the sample of 3,009 individuals with the Medicare files, 297 individuals were lost from this analysis. Matching involved using Medicare identification number, date of birth, social security number, and name.
Reimbursements are compared only among those in the fee-for-service system, whereas those in group health plans do not have equivalent reimbursement information.
Formal home care, unskilled care provided by an agency or voluntary organization, was used by 46 percent of the respondents, whereas 39 percent said they received skilled nursing care in the home. Altogether, 94 percent used at least one type of home care (skilled nursing, formal, or informal).
PACE will, in certain situations, contract with a specialist of choice for a participant.
If a person answered no to the following question, he or she was defined as having a dependency in eating (an example of an ADL dependency): “Do you usually eat without any help from another person or is someone usually present to give help if needed?” If a person answered no to the following question, he or she was defined as having a dependency in housework (an example of an IADL dependency): “Do you usually do routine housework such as dusting, vacuuming, cleaning the kitchen and bathroom, and changing linens without any help from another person?”
Each marginal effect is computed in the following manner: The marginal effect for characteristic i is δi = Λ(β'x) (1-Λ(β'x))βi where Λ is the logistic cumulative distribution function and βi is the estimated coefficient for characteristic i. The marginal effect measures the difference in the predicted probabilities of enrollment when an indicator is either present or not and all other variables in the model are set equal to their mean values. For example, the percent of home owners who enrolled is 7.1 percentage points less than non-home owners when all other variables are equal to their mean values.
The unweighted model was also estimated using only those observations from the three sites with the greatest response rates: sites 4, 5, and 10. The conclusions drawn did not change from those when the full sample was used. Consequently, the estimated model based on the full sample is the only one presented.
Because of the imprecise nature of this measure, models that excluded this variable were also estimated. The results associated with the other variables in the model did not qualitatively change.
Reprint Requests: Carol V. Irvin, Ph.D., Abt Associates Inc. 55 Wheeler Street, Cambridge, MA 02138. E-Mail: Carol_Irvin @abtassoc.com.
References
- Applebaum RA. The Evaluation of the National Long Term Care Demonstration: 3. Recruitment and Characteristics of Channeling Clients. Health Services Research. 1988;23(1):51–66. [PMC free article] [PubMed] [Google Scholar]
- Bauer EJ. Transitions from Home to Nursing Home in a Capitated Long-Term Care Program: The Role of Individual Support Systems. Health Services Research. 1996;31(3):309–326. [PMC free article] [PubMed] [Google Scholar]
- Clark ML, Rice-Trumble K, Cheng DP, Turchie CD. PACE Fact Book: Information about the Program of All-inclusive Care for the Elderly. On Lok; San Francisco, CA: 1996. [Google Scholar]
- Eng C, Pedulla J, Eleazer GP, et al. Program of All-inclusive Care for the Elderly (PACE): An Innovative Model of Integrated Geriatric Care and Financing. Journal of the American Geriatrics Society. 1997;45(2):223–232. doi: 10.1111/j.1532-5415.1997.tb04513.x. [DOI] [PubMed] [Google Scholar]
- Harrington C, Newcomer RJ, Preston S. A Comparison of S/HMO Disenrollees and Continuing Members. Inquiry. 1993;30:429–440. [PubMed] [Google Scholar]
- Kane RL, Illston LH, Miller NA. Qualitative Analysis of the Program of All-inclusive Care for the Elderly (PACE) The Gerontologist. 1992;32(6):771–780. doi: 10.1093/geront/32.6.771. [DOI] [PubMed] [Google Scholar]
- Kemper P. The Use of Formal and Informal Home Care by the Disabled Elderly. Health Services Research. 1992;27(4):421–451. [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Newcomer R, Lowrimore GR, et al. Social/Health Maintenance Organizations and Fee-for-Service Health Outcomes Over Time. Health Care Financing Review. 1993;30:173–202. [PMC free article] [PubMed] [Google Scholar]
- National PACE Association: Personal communication, 1998.
- On Lok. Inc. PACE: Who is Served and What Services are Used? PACE: Progress Report on the Replication of the On Lok Model. San Francisco, CA: On Lok, Inc.; 1993. [Google Scholar]
- Riley G, Rabey E, Kasper J. Biased Selection and Regression Toward the Mean in Three Medicare HMO Demonstrations: A Survival Analysis of Enrollees and Disenrollees. Medical Care. 1989;27:337–351. doi: 10.1097/00005650-198904000-00002. [DOI] [PubMed] [Google Scholar]
- Wiener JM, Skaggs J. Current Approaches to Integrating Acute and Long-Term Care Financing and Services. Public Policy Institute of the American Association of Retired Persons; 1995. 9516. [Google Scholar]
- Zimmerman YA, Maher RJ, Pemberton DA, et al. Evaluation of the Program of All-inclusive Care for the Elderly (PACE) Demonstration Annual Site Visit Report: Calendar Year 1994. Abt Associates Inc.; Cambridge, MA: 1996. [Google Scholar]
- Zimmerman YA, Pemberton DA, Dorsey TA, et al. Annual Site Visit Report: Calendar Year 1995. Abt Associates Inc.; Cambridge, MA.: 1997. Report submitted to HCFA under contract No. HCFA 500-91-0027. [Google Scholar]
- Zimmerman YA, Pemberton DA, Thomas L. Factors Contributing to Care Management and Decision Making in the PACE Model. Abt Associates Inc.; Cambridge, MA: 1998. Report submitted to HCFA under contract No. HCFA 500-91-0027. [Google Scholar]