Introduction
Medicare reimburses about one-half of the health care goods and services used by the eligible population (Laschober and Olin, 1996). Medicare beneficiaries usually find it desirable to hold supplementary health insurance to cover the cost sharing and services that Medicare does not cover. A previous report described the distribution of supplementary insurance in 1991, the first year the Medicare Current Beneficiary Survey (MCBS) was in the field (Chulis et al., 1993). That report focused on the elderly population living in the community who received care in the fee-for-service sector.
The distribution of supplementary insurance has been changing rapidly in recent years in response to increased managed care options under Medicare, additional legislated ways to qualify under Medicaid, a lessening in support from employers toward retirement benefits, and increasing costs of individually purchased medigap policies. This report brings the supplementary insurance distribution up to date through 1996, and analyzes gains and losses in the insurance shares from 1992-96. Expanding on earlier reports, the entire Medicare population (aged, disabled, living in the community, living in institutions) is included. We present more detailed categories than previous reports, including breakouts of qualified Medicare beneficiaries (QMBs) and special low income Medicare beneficiaries (SLMBs) under Medicaid. The report also shows separate distributions of supplementary insurance for persons in the fee-for-service and managed care sectors.
The earlier report used the MCBS Access to Care file which (of necessity) included only people continuously enrolled in Medicare for the entire year. Persons who began their Medicare coverage during the year, or who died during the year, were not included in that report. The data in this report are from the 1992 MCBS Cost and Use file and the 1996 Access to Care file, which has been adjusted to reflect the 1996 ever-enrolled population. Thus the data for both years includes all Medicare beneficiaries enrolled at any time in those years. To the degree that changes in the supplementary insurance distribution are being spearheaded by newer enrollees migrating toward the newer forms of insurance while the older beneficiaries (who die at higher rates) are leaving the more traditional forms of insurance, including these groups adds more than just cosmetic value. (For a description of the MCBS design and methods, see Adler, 1994).
1996 Distribution Overview
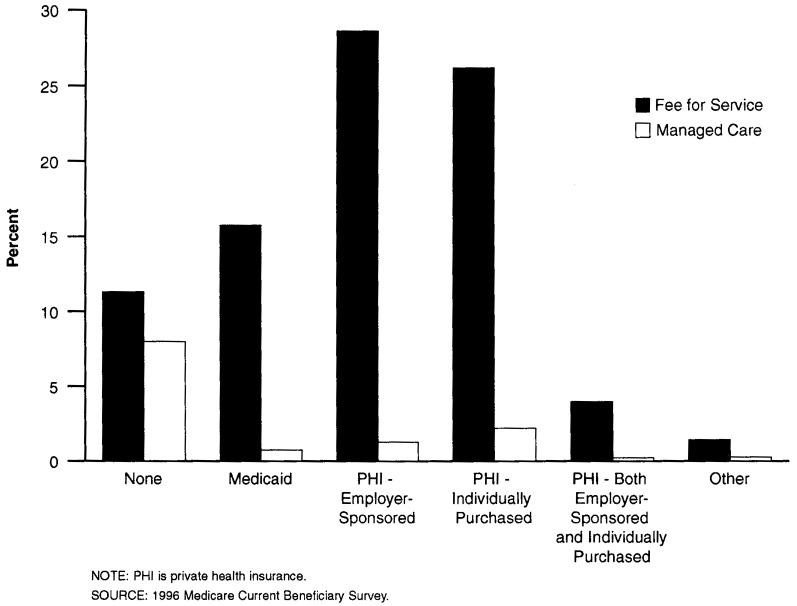
Over 87 percent of the Medicare population receive their care in the fee-for-service sector, and 13 percent are enrolled in Medicare managed care plans (Table 1 and Figure 1). Over 19 percent of the Medicare population have no supplementary insurance. However, there is a large difference between the fee-for-service sector, where 13 percent have no supplement, and the managed care sector, where 63 percent have no supplement. One of the main attractions of managed care is that many plans offer lower cost-sharing and services in addition to the traditional Medicare benefit package. The extra benefits offered in 1996 appear to have been generous enough that almost two-thirds of those enrolled in managed care plans no longer felt it necessary to hold supplementary insurance.
Table 1. Distribution of Supplementary Health Insurance for the Medicare Population: 1996.
| All Enrollees | Fee-For-Service | Managed Care | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Type of Insurance | Number | Percent | Number | Percent of Total | Percent of FFS | Number | Percent of Total | Percent of MC |
| Total | 39,385.1 | 100.0 | 34,401.5 | 87.3 | 100.0 | 4,983.6 | 12.7 | 100.0 |
| Medicare Only | 7,609.0 | 19.3 | 4,462.3 | 11.3 | 13.0 | 3,146.7 | 8.0 | 63.1 |
| Individual Medigap | 11,180.4 | 28.4 | 10,317.8 | 26.2 | 30.0 | 862.6 | 2.2 | 17.3 |
| Employer-Sponsored | 11,768.3 | 29.9 | 11,271.8 | 28.6 | 32.8 | 496.5 | 1.3 | 10.0 |
| Both Private Types | 1,667.9 | 4.2 | 1,583.3 | 4.0 | 4.6 | 84.61 | 0.21 | 1.71 |
| Medicaid, Total | 6,494.1 | 16.5 | 6,207.8 | 15.8 | 18.0 | 286.3 | 0.7 | 5.7 |
| Full Coverage | 3,268.6 | 8.3 | 3,147.1 | 8.0 | 9.1 | 121.4 | 0.3 | 2.4 |
| QMBs | 2,925.7 | 7.4 | 2,793.7 | 7.1 | 8.1 | 132.0 | 0.3 | 2.6 |
| SLMBs | 299.9 | 0.8 | 267.0 | 0.7 | 0.8 | 32.91 | 0.11 | 0.71 |
| Other | 665.4 | 1.7 | 558.5 | 1.4 | 1.6 | 106.9 | 0.3 | 2.1 |
Numbers shown are included for completeness, but are considered too small to be reliable because they are based on weighted counts of less than 100,000 (approximately 50 cases).
NOTES: FFS is fee-for-service. MC is managed care. QMBs are qualified Medicare Beneficiaries. SLMBs are Special Low-income Medicare Beneficiaries. Percent columns will add to more than total line because persons with Medicaid are shown twice, in Medicaid Total and in Medicaid Subcategories - Full Coverage, QMBs, SLMBs. Weighted counts between 100,000 and 200,000 should be interpreted carefully because they have relatively high statistical variances.
SOURCE: 1996 Medicare Current Beneficiary Survey.
Figure 1. Secondary Health Insurance Distribution of the Medicare Population in 1996.
Adding together the private insurance categories (individual medigap, employer-sponsored, both), 63 percent of the Medicare population had private supplementary insurance in 1996. Again, however, there is a large difference between the fee-for-service sector, where 67 percent held private plans, and the managed care sector, where only 29 percent held private supplements. The largest difference was for employer-sponsored insurance, where 37 percent of fee-for-service persons held policies, compared with only 12 percent of managed care persons (adding employer-sponsored and both). This difference may reflect the recent trend by employers to stop offering supplementary policies to retirees that wrap around Medicare fee-for-service coverage, and instead encouraging their former employees to enroll in Medicare health maintenance organizations (HMOs) (McArdle and Yamamoto, 1997).
In 1996, persons dually eligible for Medicare and Medicaid were nearly 17 percent of the total Medicare population. This included 8 percent entitled to full Medicaid benefits, 7 percent entitled under the Qualified Medicare Beneficiary (QMB) program where they are exempt from Medicare premiums and cost sharing, and 1 percent entitled under the Special Low Income Medicare Beneficiary (SLMB) program who are exempt from Medicare premiums only. Persons dually eligible to Medicare and Medicaid were more heavily represented in the fee-for-service sector (18 percent) than in managed care (6 percent). In fact, only 1 percent of dually eligible Medicare beneficiaries were enrolled in managed care in 1996. (Note: Under Medicare regulations, States are not allowed to compel dually eligible beneficiaries to join Medicare HMOs.)
The next two sections examine the changes in insurance distributions in fee-for-service and managed care, respectively, from 1992-96.
Fee-For-Service Insurance Trends: 1992-96
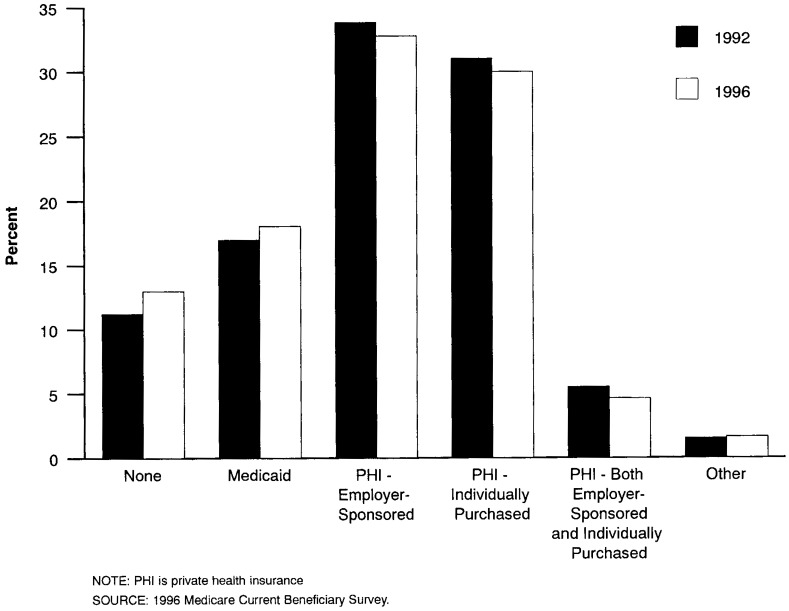
The total Medicare population increased just over 7 percent from 1992-96 (Table 2 and Figure 2). At the same time, the share of Medicare enrollees in the fee-for-service sector declined 6 percent from 94 percent in 1992 to 87 percent in 1996. The net result of these nearly offsetting effects was that there were 34.4 million beneficiaries in the fee-for-service sector in both 1992 and 1996. There was a 2-percent increase in share of fee-for-service persons with no supplementary insurance from 1992 (11 percent) through 1996 (13 percent), an increase of over 610,000 persons. Since Medicare enrollees were being drawn from fee-for-service to managed care in this period, this suggests that the managed care gains came from those with some supplementary insurance, not those with Medicare only.
Table 2. Changes Between 1992 and 1996 in Medicare Fee-for-Service and Managed Care Supplementary Insurance Distributions.
| Type of Insurance | 1992 | 1996 | Difference | |||
|---|---|---|---|---|---|---|
| Number in Thousands | Percent Share | Number in Thousands | Percent Share | Number in Thousands | Percent Change | |
| Total Medicare | 36,786.5 | – | 39,385.1 | – | 2,598.6 | 7.1 |
| Fee-for-Service | ||||||
| Total | 34,422.4 | 100.0 | 34,401.5 | 100.0 | -20.9 | -0.1 |
| Medicare Only | 3,851.6 | 11.2 | 4,462.3 | 13.0 | 610.7 | 15.9 |
| Individual Medigap | 10,676.3 | 31.0 | 10,317.8 | 30.0 | -358.5 | -3.4 |
| Employer-Sponsored | 11,642.4 | 33.8 | 11,271.8 | 32.8 | -370.6 | -3.2 |
| Both Private Types | 1,894.4 | 5.5 | 1,583.3 | 4.6 | -311.1 | -16.4 |
| Medicaid, Total | 5,843.8 | 17.0 | 6,207.8 | 18.0 | 364.0 | 6.2 |
| Other | 513.9 | 1.5 | 558.5 | 1.6 | 44.6 | 8.7 |
| Managed Care | ||||||
| Total | 2,362.1 | 100.0 | 4,983.6 | 100.0 | 2,621.5 | 111.0 |
| Medicare Only | 1,609.8 | 68.1 | 3,146.7 | 63.1 | 1,536.9 | 95.5 |
| Individual Medigap | 196.5 | 8.3 | 862.6 | 17.3 | 666.1 | 338.9 |
| Employer-Sponsored | 321.7 | 13.6 | 496.5 | 10.0 | 174.8 | 54.4 |
| Both Private Types | 12.21 | 0.51 | 84.61 | 1.71 | 72.41 | 594.21 |
| Medicaid, Total | 142.4 | 6.0 | 286.3 | 5.7 | 143.9 | 101.1 |
| Other | 79.51 | 3.41 | 106.9 | 2.1 | 27.3 | 34.4 |
Numbers shown are included for completeness, but are considered too small to be reliable because they are based on weighted counts of less than 100,000 (approximately 50 cases).
NOTE: Weighted counts between 100,000 and 200,000 should be interpreted carefully because they have relatively high statistical variances.
SOURCE: 1992 and 1996 Medicare Current Beneficiary Survey.
Figure 2. Comparison of the Secondary Health Insurance Distribution of the Medicare Fee-For-Service Population: 1992 and 1996.
The largest decreases in the fee-for-service sector from 1992-96 came from the private supplementary insurance categories. Specifically, there were over 1 million fewer persons with individual medigap-gap insurance (359,000), employer-sponsored insurance (371,000), or both individual and employer-sponsored insurance (311,000), in 1996. This suggests that persons holding private health insurance were the insurance group most attracted to Medicare's managed care program during that 4-year period. The share of persons in the fee-for-service sector with individual medigap insurance declined from 31 percent to 30 percent, the share with employer- sponsored insurance declined from 34 percent to 33 percent, and the share with both declined from 6 percent to 5 percent.
The number of fee-for-service persons dually eligible for Medicare and Medicaid increased by 364,000 persons from 1992-96, and the share increased from 17 percent to 18 percent. This increase is not reflected in the overall Medicaid share, which stayed constant at 16 percent; rather, it is an artifact of the small number of dually eligible persons enrolled in Medicare managed care plans.
Managed Care Insurance Trends: 1992-96
The number of persons enrolled in Medicare managed care plans more than doubled from 1992 (2.3 million) to 1996 (5.0 million). The largest increase, 1.5 million persons, was for persons who have no supplementary insurance in addition to Medicare. It appears that the more generous cost sharing and expanded benefits offered by Medicare HMOs allowed many persons who previously carried private supplemental insurance to drop that coverage when they switched from the fee-for-service sector to managed care. Even though the Medicare-only category showed the largest increase in absolute number terms, its rate of increase (96 percent) was among the slowest. As a result, the share of managed care persons with Medicare-only dropped from 68 percent in 1992 to 63 percent in 1996. insurance increased from 8 percent in 1992 to 17 percent in 1996. This implies that many persons who join managed care organizations continue to hold their individually purchased private policies; however, sometimes the reported individual insurance consists of additional HMO premiums the Medicare beneficiary pays to obtain coverage for services not covered by the Medicare HMO premium. The picture is different for persons with employer-sponsored insurance, where the share of Medicare managed care enrollees reporting employer-sponsored insurance decreased from 14 percent in 1992 to 10 percent in 1996. This decrease is puzzling in light of the recent reports that employers are encouraging their retirees to join Medicare HMOs to decrease their financial liability.
The number of Medicare managed care persons who are dually entitled to Medicaid increased at about the same rate (101 percent) from 1992-96 as the entire managed care population (111 percent). While nearly 144,000 additional dual eligibles (net) joined Medicare managed care organizations in that period, the share of dual eligibles stayed about the same, near 6 percent.
Footnotes
The authors are with the Office of Strategic Planning, Health Care Financing Administration (HCFA). The views and opinions expressed are those of the author and do not necessarily reflect those of HCFA.
Reprint Requests: Franklin J. Eppig, J.D., Office of Strategic Planning, Health Care Financing Administration, 7500 Security Boulevard, N3-02-02 Baltimore, Maryland 21244-1850. e-mail feppig@HCFA.gov
References
- Adler GS. A Profile of the Medicare Current Beneficiary Survey. Health Care Financing Review. 1994 Summer;15(4):153–163. [PMC free article] [PubMed] [Google Scholar]
- Chulis GS, Eppig FJ, Hogan MO, et al. Health Insurance and the Elderly: Data From the MCBS. Health Care Financing Review. 1993 Spring;14(3):163–181. [PMC free article] [PubMed] [Google Scholar]
- Laschober MA, Olin GL. Health and Health Care of the Medicare Population: Data From the 1992 Medicare Current Beneficiary Survey. Rockville, MD.: Westat, Inc.; Nov, 1996. [Google Scholar]
- McArdle FB, Yamamoto DH. Retiree Health Trends and Implications of Possible Medicare Reforms. Washington D.C.: Hewitt Associates; Sep, 1997. [Google Scholar]