Abstract
Primary splenic epithelial cyst is an unusual event in everyday surgical practice with about 800 cases reported until date in the English literature. Splenic cysts may be parasitic or non-parasitic in origin. Nonparasitic cysts are either primary or secondary. Primary cysts are also called true, congenital, epidermoid or epithelial cysts. Primary splenic cysts account for 10% of all benign non-parasitic splenic cysts and are the most frequent type of splenic cysts in children. Usually, splenic cysts are asymptomatic and can be found incidentally during imaging techniques or on laprotomy. The symptoms are related to the size of cysts. When they assume large sizes, they may present with fullness in the left abdomen, local or referred pain, symptoms due to compression of adjacent structures (like nausea, vomiting, flatulence, diarrhoea) or rarely thrombocytopenia, and occasionally complications such as infection, rupture and/or haemorrhage. The preoperative diagnosis of primary splenic cysts can be ascertained by ultrasonography (USG), computed tomography or magnetic resonance imaging, although the wide use of USG today has led to an increase in the incidence of splenic cysts by 1%. However, careful histopathological evaluation along with immunostaining for presence of epithelial lining is mandatory to arrive at the diagnosis. The treatment has changed drastically from total splenectomy in the past to splenic preservation methods recently.
Keywords: Epithelial cyst, Spleen, Diagnosis, Splenectomy, Laporoscopy
Core tip: Accurate preoperative diagnosis of primary epithelial cysts is difficult; the occurrence of a cystic lesion that is either unilocular or multilocular in the absence of previous trauma, infection or exposure to hydatid disease may help to arrive at the diagnosis. However, careful histopathological evaluation along with immunostaining is important to arrive at correct diagnosis. The treatment has changed drastically from total splenectomy in the past to splenic preservation methods recently. The rationale behind conservative management is to preserve the splenic function in order to avoid untoward complications related to historical treatment.
INTRODUCTION
Primary splenic cysts are unusual and often an incidental finding in surgical practice. As per the existing literature, since the first case was reported in 1929 by Andral, the classification of these lesions has evolved into the present system[1].
CLASSIFICATION
Splenic cysts have been classified based on the presence or absence of an epithelial lining, etiology, pathogenesis, etc. Martin classified splenic cysts as type 1 cysts, which are true cysts having lining epithelium, and type 2 cysts, which are false cysts without lining epithelium[2,3]. Pseudocysts are usually posttraumatic, due to failure of organization of hematomas located beneath the capsule or in the splenic parenchyma, and rarely they may occur in splenic abscess or splenic infarction[1,4,5]. Depending on the causative agent splenic cysts can be divided into two types: parasitic cysts and non-parasitic cysts. Parasitic cysts are usually seen in endemic areas and are caused mainly by Echinococcus granulosus infestation[1,6,7]. A new classification based on the true pathogenesis of cyst divides non-parasitic splenic cysts as congenital, neoplastic, traumatic, and degenerative[8]. Primary splenic cysts constitute 10% of all nonparasitic cysts of the spleen. These cysts are predominantly seen in paediatric and adolescent age groups[2,9]. Usually they are asymptomatic and found incidentally on ultrasound examination of the abdomen[2]. The clinical significance is attributed mainly because of their potential to rupture, to infect or to bleed, and due to the potential of a serious differential diagnosis of a neoplastic lesion in the left hypochondrium[10].
Recently, treatment of choice is open partial splenectomy as it preserves the splenic functions and there is no recurrence of the lesion due to complete removal[11]. Histopathological evaluation along with immunohistochemistry is the mainstay to confirm the subtype of splenic cyst and to rule out the rare possibility of malignant transformation in the pluripotent epithelial lining[12].
EPIDEMIOLOGY
Primary splenic epithelial cyst is a rare condition with an incidence rate of 0.07% as reported in a review of 42327 autopsies[13-16]. Primary splenic cysts are seen mostly in children, adolescents and young adults[13]. Congenital type is common in girls[17,18]. Non-parasitic splenic cysts are common in Europe and North America, while parasitic cysts are common in Africa and Central America[19]. The prevalence rate of splenic cysts has been increased nowadays due to increased use of non-invasive diagnostic modalities, i.e., ultrasonography (USG) and computed tomography (CT)[20].
PATHOPHYSIOLOGY
The pathogenesis of primary splenic cysts is not clear. In view of this, many hypotheses were proposed.
Mesothelial invagination theory
In case of congenital cysts, it is postulated that during development there is invasion of mesothelial lining along with the capsule. As the lining has pluripotent nature, it has propensity to undergo metaplasia and secretion of fluid, leading to the formation of cysts[1,5].
The congenital cyst lining is postulated to arise from invasion of the peritoneum along with its mesothelial lining after rupture of the splenic capsule or due to trapping of mesothelial cells in splenic sulci.
Lymph space theory
According to this theory the cysts may arise from the normal lymph spaces in the spleen[16].
Endodermal inclusion theory
Endodermal inclusion theory proposes that epithelial splenic cysts develop by true metaplasia of a heterotopic endodermal inclusion within the spleen[21-23]. Due to pluripotent nature of the mesothelium, there seems to be metaplasia in the lining leading to formation of cysts with various types of epithelial lining, i.e., squamous, columnar, etc.[12]. According to some studies the epidermoid nature is due to teratomatous differentiation or to inclusion of fetal squamous lining instead of metaplasia.
CLINICAL FEATURES
Age
Splenic cysts are predominantly seen in the second and third decades; however, they can be seen in paediatric age group[24].
Sex
Splenic cysts are common in females as compared to males[18].
Signs and symptoms
Usually small cysts are symptomless. A painless mass in the left hypochondriac region is the main presentation in 30%-40% cases. There may be localized pain or referred pain due to mass effect[25]. Occasionally the patients may present with thrombocytopenia[1,26]. The initial symptoms are mainly due to pressure effect, including nausea and belching pain in the abdomen[25]. Pleuritic pain and persistent cough are also the presenting features[27]. Occasionally they present with complications, like infection, rupture and haemorrhage[25,28]. Physical examination often reveals a left hypochondriac mass. The routine haematological and biochemical investigations are within normal limits.
Tumour markers
The serum tumour markers carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA 19-9) may be raised and so checked[29].
DIAGNOSIS
Clinical diagnosis
Most of primary cysts are clinically silent and are diagnosed incidentally on USG. Nowadays, the prevalence is increased because of the increased use of non-invasive imaging techniques, i.e., USG and CT[30].
Whenever there is a lump in the left hypochondriac region, the clinician should exclude other causes of splenomegaly, i.e., infectious mononucleosis, fever of unknown origin, haemolytic anaemia, chronic leukaemias, collagen vascular disease, and liver diseases. Serological markers play key role in such circumstances[31].
USG
USG is a good non-invasive tool for screening and confirming the cystic nature of a mass[2]. Ultrasound can differentiate solid and cystic lesions in most cases[32]. Characteristically, on USG the cyst appears as an anechoic mass with thin walls and septations or irregular walls. There are calcific foci in case of complex cysts. Calcifications are useful to differentiate cysts from other causes of splenomegaly[27,30,10].
CT and magnetic resonance imaging
CT and magnetic resonance imaging (MRI) may give guidelines, with regard to the morphology of cyst, the nature of fluid, the exact location and its relationship with adjacent structures[10,27,30]. On T1-weighted MRI images, the cyst is hypointense while on T2, it is hyperintense, with intensity of signal equal to water without reinforcement after contrast injection. However, the signal intensity may be elevated according to contents in the cyst, e.g., signal intensity on T1 can be increased in case of a hemorrhagic cyst[33].
Accurate clinical diagnosis
Accurate clinical diagnosis of primary epithelial cysts is difficult; the occurrence of a unilocular cyst in the absence of previous trauma, infection or exposure to hydatid disease may help to arrive at the diagnosis[1]. The diagnosis of pseudocyst should be suspected in cases with a history of trauma, elder age along with evidence of hematoma in the organ parenchyma and calcification in the cyst wall. The diagnosis of hydatid cyst is done by detailed clinical history, the evidence of calcification in the wall, and presence of daughter cysts with multiple organ involvement[34,35].
Other techniques
Other techniques such as 99m technetium sulphur colloid scintigraphy and 67-gallium citrate also prove the diagnostic utility[2]. The inner cyst wall is immunoreactive to anti-CA 19-9 antibodies[36]. Serum levels of the markers may be low as compared to actual elevations within the cystic cavity.
Angiography is helpful in differentiating a splenic cyst, which is usually an avascular lesion, while the malignant tumours (lymphoma, sarcoma) usually have a disarranged vascular pattern[27,13].
However, definite diagnosis is possible only after splenectomy when epithelial lining is confirmed by histopathology along with immunohistochemistry. Primary epithelial cysts are usually solitary, but can be multiple. Cases have also been described in accessory spleens[37,38].
The cysts are either unilocular/multilocular with occasional calcific foci. Figure 1 shows an example of a unilocular cyst with smooth glistening inner wall surface.
Figure 1.

Huge primary splenic cyst with glistening smooth inner wall.
A case of multilocular primary epithelial cyst of the spleen in a postmenopausal women presenting as splenomegaly was reported (Figure 2)[12].
Figure 2.
Multiloculated primary splenic cyst.
Histologically, primary splenic cysts have epithelial lining, i.e., flattened, low cuboidal, low columnar or squamous type and unilayered or multilayered with benign nuclear features[1]. Epidermoid cysts have stratified squamous epithelium with a fibrocollagenous cyst wall (Figure 3). Immunohistochemically, the epithelial cells are positive for pan-cytokeratin and negative for CD240 (a lymphatic epithelial marker) and CD34 (an endothelial cell marker). Figure 4 shows an example of primary splenic cyst lined with cuboidal to flattened epithelium.
Figure 3.
Epidermoid cyst of the spleen (Hematoxylin and eosin staining, × 10).
Figure 4.
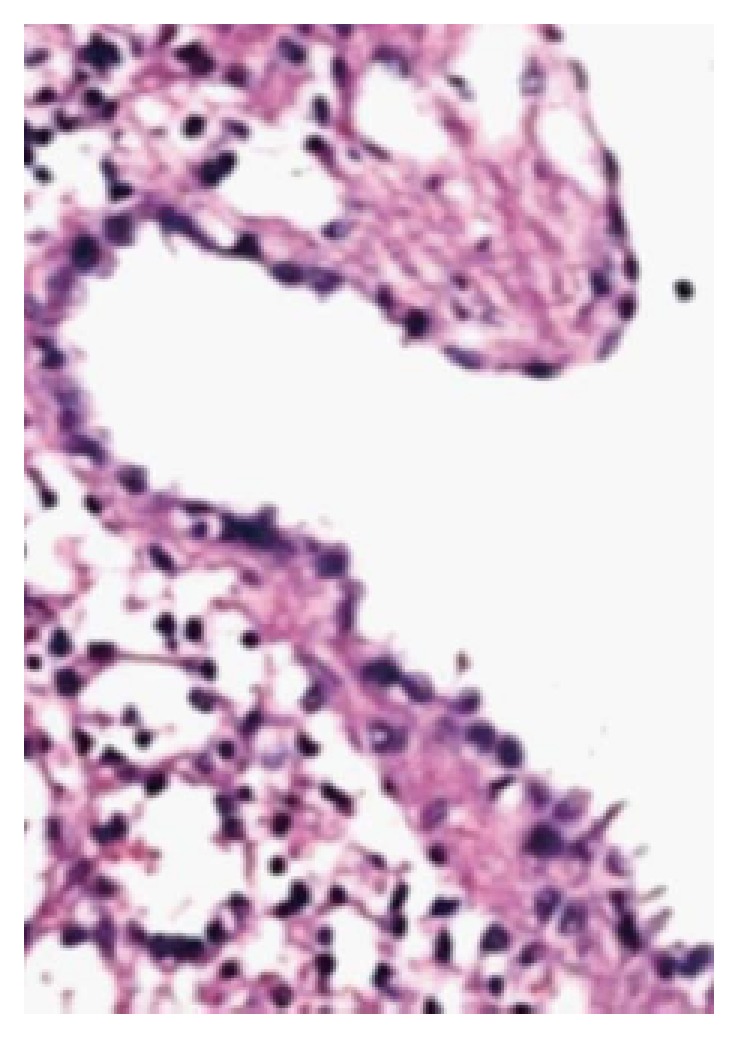
Primary splenic cyst lined with cuboidal to flattened epithelium (Hematoxylin and eosin staining, × 10).
The differential diagnoses for a cysts in the spleen include parasitic echinococcal disease, congenital cyst, posttraumatic pseudocyst, infarction, infection, pyogenic splenic abscess, pancreatic pseudocyst, metastatic disease, and cystic neoplasms like haemangioma/lymphangioma (diffuse lymphangiomatosis of spleen) (Figure 5).
Figure 5.
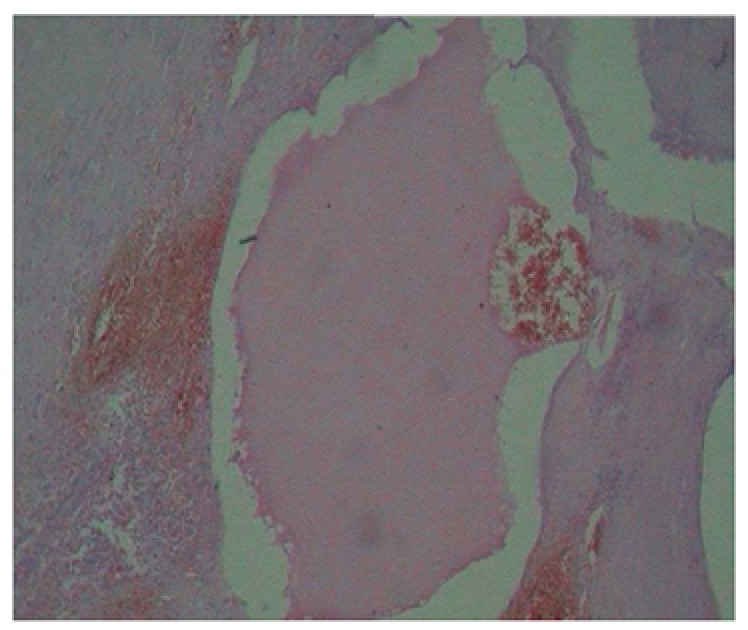
Diffuse lymphangiomatosis of the spleen (Hematoxylin and eosin staining, × 10).
TREATMENT
Previously, splenectomy was the treatment of choice for splenic cysts. Recently, the approach is changed towards conservative surgery in view of overwhelming sepsis after splenectomy leading to raised mortality. The splenic cysts with a diameter more than 4 cm should be treated surgically[11]. Traditionally the cysts have been treated either by partial or total splenectomy. However, there are chances of overwhelming sepsis after splenectomy. In the modern era of laparoscopic surgery, more interest in conservative surgery like percutaneous aspiration and sclerosis is documented to prevent post splenectomy complications. Marsupialisation is very much effective in small cysts.
There are different types of surgical modalities according to the clinical situation.
Today, there are different conservative treatment modalities, including percutaneous drainage, partial splenectomy with a stapler or harmonic scalpel, total cystectomy, marsupialisation or cyst unroofing. Laparoscopic puncture and creation of a cyst peritoneal window are also an effective conservative treatment modality. The aim of partial splenectomy is to retain the immunological protection of patient by preserving more than 25% of the splenic parenchyma, which is the optimum splenic tissue to preserve immunologic efficiency without increasing the risk of recurrence[28].
Any type of conservative surgical treatment modality has little value in cases such as a very large cyst in the hilum of the spleen, an intrasplenic cyst almost surrounded by splenic parenchyma, with dense vascular adhesions to surrounding structures, and multiple cysts. In such circumstances, splenectomy either by open approach or by laparoscopic approach is the treatment of choice.
PROGNOSIS
The clinical importance of splenic cysts is due to their potential to rupture, to be infected or to bleed. Cysts with a diameter > 5 cm are more likely to rupture resulting in life threatening haemoperitoneum. Two rare cases of patients with epithelial splenic cysts as an incidental finding during emergency laprotomy for splenic rupture were reported[39]. The most common infection is caused by Salmonella bacteria[13]. A 12-year-old prepubertal gir presenting with a large congenital splenic cyst complicated by Salmonella infection was documented[18]. Pregnancy associated splenic cysts are extremely rare and only five cases were described[40]. A case of squamous cell carcinoma in an epidermoid cyst was reported in a pregnant woman[4].
Footnotes
P- Reviewer: Kamocki Z, Liu PP, Murakami M, Schrittwieser R S- Editor: Ding Y L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Ingle SB, Hinge CR, Jatal SN. An interesting case of primary epithelial cyst of spleen. Indian J Pathol Microbiol. 2013;56:181–182. doi: 10.4103/0377-4929.118700. [DOI] [PubMed] [Google Scholar]
- 2.Garg M, Kataria SP, Sethi D, Mathur SK. Epidermoid cyst of spleen mimicking splenic lymphangioma. Adv Biomed Res. 2013;2:49. doi: 10.4103/2277-9175.114190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin JW. Congenital splenic cysts. Am J Surg. 1958;96:302–308. doi: 10.1016/0002-9610(58)90916-4. [DOI] [PubMed] [Google Scholar]
- 4.Schwarts SI. The spleen. In: Schwartz SI, Harold E, editors. Maingot’s Abdominal Operations. 9th edition. USA: Appleton and Lange; 1990. p. 80. [Google Scholar]
- 5.Valente AP, Barrabin H, Jorge RV, Paes MC, Scofano HM. Isolation and characterization of the Mg2(+)-ATPase from rabbit skeletal muscle sarcoplasmic reticulum membrane preparations. Biochim Biophys Acta. 1990;1039:297–304. doi: 10.1016/0167-4838(90)90262-e. [DOI] [PubMed] [Google Scholar]
- 6.Avital S, Kashtan H. A large epithelial splenic cyst. N Engl J Med. 2003;349:2173–2174. doi: 10.1056/NEJM200311273492222. [DOI] [PubMed] [Google Scholar]
- 7.Kalinova K. Giant pseudocyst of the spleen: A case report and review of the literature. J Indian Assoc Pediatr Surg. 2005;10:176–178. [Google Scholar]
- 8.Morgenstern L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg. 2002;194:306–314. doi: 10.1016/s1072-7515(01)01178-4. [DOI] [PubMed] [Google Scholar]
- 9.Belekar D, Desai A, Dewoolkar A, Dewoolkar V, Bhutala U. Splenic epithelial cyst: A rare entity. Int J Surg. 2010;22:1–18. [Google Scholar]
- 10.Hansen MB, Moller AC. Splenic cysts. Surg Laparosc Endosc Percutan Tech. 2004;14:316–322. doi: 10.1097/01.sle.0000148463.24028.0c. [DOI] [PubMed] [Google Scholar]
- 11.Szczepanik AB, Meissner AJ. Partial splenectomy in the management of nonparasitic splenic cysts. World J Surg. 2009;33:852–856. doi: 10.1007/s00268-008-9868-2. [DOI] [PubMed] [Google Scholar]
- 12.Manoj MG, Misra P, Kakkar S. Multilocular epithelial cyst of spleen: a rare occurrence. Indian J Pathol Microbiol. 2012;55:602–604. doi: 10.4103/0377-4929.107850. [DOI] [PubMed] [Google Scholar]
- 13.Macheras A, Misiakos EP, Liakakos T, Mpistarakis D, Fotiadis C, Karatzas G. Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol. 2005;11:6884–6887. doi: 10.3748/wjg.v11.i43.6884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doolas A, Nolte M, McDonald OG, Economou SG. Splenic cysts. J Surg Oncol. 1978;10:369–387. doi: 10.1002/jso.2930100502. [DOI] [PubMed] [Google Scholar]
- 15.Geraghty M, Khan IZ, Conlon KC. [In Process Citation] J Minim Access Surg. 2009;5:14–16. doi: 10.4103/0972-9941.51315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robbins FG, Yellin AE, Lingua RW, Craig JR, Turrill FL, Mikkelsen WP. Splenic epidermoid cysts. Ann Surg. 1978;187:231–235. doi: 10.1097/00000658-197803000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilmes MA, Strouse PJ. The pediatric spleen. Semin Ultrasound CT MR. 2007;28:3–11. doi: 10.1053/j.sult.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Karia N, Lakhoo K. Complicated congenital splenic cyst: saved by a splenunculus. Afr J Paediatr Surg. 2011;8:98–100. doi: 10.4103/0189-6725.79068. [DOI] [PubMed] [Google Scholar]
- 19.Sellers GJ, Starker PM. Laparoscopic treatment of a benign splenic cyst. Surg Endosc. 1997;11:766–768. doi: 10.1007/s004649900446. [DOI] [PubMed] [Google Scholar]
- 20.Wu HM, Kortbeek JB. Management of splenic pseudocysts following trauma: a retrospective case series. Am J Surg. 2006;191:631–634. doi: 10.1016/j.amjsurg.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 21.Kundal VK, Gajdhar M, Kundal R, Sharma C, Agrawal D, Meena A. Giant Epithelial Non-Parasitic Splenic Cyst. J Case Rep. 2013;3:106–109. [Google Scholar]
- 22.Harding HE. A large inclusion cyst in a spleen. J Path. 1933;36:485. [Google Scholar]
- 23.Touloukian RJ, Maharaj A, Ghoussoub R, Reyes M. Partial decapsulation of splenic epithelial cysts: studies on etiology and outcome. J Pediatr Surg. 1997;32:272–274. doi: 10.1016/s0022-3468(97)90193-7. [DOI] [PubMed] [Google Scholar]
- 24.Sakamoto Y, Yunotani S, Edakuni G, Mori M, Iyama A, Miyazaki K. Laparoscopic splenectomy for a giant splenic epidermoid cyst: report of a case. Surg Today. 1999;29:1268–1272. doi: 10.1007/BF02482221. [DOI] [PubMed] [Google Scholar]
- 25.Trompetas V, Panagopoulos E, Priovolou-Papaevangelou M, Ramantanis G. Giant benign true cyst of the spleen with high serum level of CA 19-9. Eur J Gastroenterol Hepatol. 2002;14:85–88. doi: 10.1097/00042737-200201000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Tsakraklides V, Hadley TW. Epidermoid cysts of the spleen. A report of five cases. Arch Pathol. 1973;96:251–254. [PubMed] [Google Scholar]
- 27.Labruzzo C, Haritopoulos KN, El Tayar AR, Hakim NS. Posttraumatic cyst of the spleen: a case report and review of the literature. Int Surg. 2002;87:152–156. [PubMed] [Google Scholar]
- 28.Till H, Schaarschmidt K. Partial laparoscopic decapsulation of congenital splenic cysts. A medium-term evaluation proves the efficiency in children. Surg Endosc. 2004;18:626–628. doi: 10.1007/s00464-003-9046-4. [DOI] [PubMed] [Google Scholar]
- 29.Walz MK, Metz KA, Sastry M, Eigler FW, Leder LD. Benign mesothelial splenic cyst may cause high serum concentration of CA 19-9. Eur J Surg. 1994;160:389–391. [PubMed] [Google Scholar]
- 30.Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol. 2001;11:80–95. doi: 10.1007/s003300000528. [DOI] [PubMed] [Google Scholar]
- 31.Knudson P, Coon W, Schnitzer B, Liepman M. Splenomegaly without an apparent cause. Surg Gynecol Obstet. 1982;155:705–708. [PubMed] [Google Scholar]
- 32.Siniluoto TM, Päivänsalo MJ, Lähde ST, Alavaikko MJ, Lohela PK, Typpö AB, Suramo IJ. Nonparasitic splenic cysts. Ultrasonographic features and follow-up. Acta Radiol. 1994;35:447–451. [PubMed] [Google Scholar]
- 33.Ramani M, Reinhold C, Semelka RC, Siegelman ES, Liang L, Ascher SM, Brown JJ, Eisen RN, Bret PM. Splenic hemangiomas and hamartomas: MR imaging characteristics of 28 lesions. Radiology. 1997;202:166–172. doi: 10.1148/radiology.202.1.8988207. [DOI] [PubMed] [Google Scholar]
- 34.Fernández-Ruiz M, Guerra-Vales JM, Enguita-Valls AB, Vila-Santos J, García-Borda FJ, Morales-Gutiérrez C. Splenic hydatid cyst, a rare location of extrahepatic echinococcosis: Report of six cases. Eur J Intern Med. 2008;19:e51–e53. doi: 10.1016/j.ejim.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 35.Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003;23:475–494; quiz 536-537. doi: 10.1148/rg.232025704. [DOI] [PubMed] [Google Scholar]
- 36.Madia C, Lumachi F, Veroux M, Fiamingo P, Gringeri E, Brolese A, Zanus G, Cillo U, D’Amico DF. Giant splenic epithelial cyst with elevated serum markers CEA and CA 19-9 levels: an incidental association? Anticancer Res. 2003;23:773–776. [PubMed] [Google Scholar]
- 37.Morohoshi T, Hamamoto T, Kunimura T, Yoshida E, Kanda M, Funo K, Nagayama T, Maeda M, Araki S. Epidermoid cyst derived from an accessory spleen in the pancreas. A case report with literature survey. Acta Pathol Jpn. 1991;41:916–921. doi: 10.1111/j.1440-1827.1991.tb01639.x. [DOI] [PubMed] [Google Scholar]
- 38.Tateyama H, Tada T, Murase T, Fujitake S, Eimoto T. Lymphoepithelial cyst and epidermoid cyst of the accessory spleen in the pancreas. Mod Pathol. 1998;11:1171–1177. [PubMed] [Google Scholar]
- 39.Fragandreas G, Papadopoulos S, Gerogiannis I, Spyridis C, Tsantilas D, Venizelos I, Gerasimidis T. Epithelial splenic cysts and life-threatening splenic rupture. Chirurgia (Bucur) 2011;106:519–522. [PubMed] [Google Scholar]
- 40.Rotas M, Ossowski R, Lutchman G, Levgur M. Pregnancy complicated with a giant splenic cyst: a case report and review of the literature. Arch Gynecol Obstet. 2007;275:301–305. doi: 10.1007/s00404-006-0229-9. [DOI] [PubMed] [Google Scholar]


