Abstract
Gastric antral vascular ectasia (GAVE) is an uncommon and often neglected cause of gastric hemorrhage. The treatments for GAVE include surgery, endoscopy and medical therapies. Here, we report an unusual case of GAVE. A 72-year-old man with a three-month history of recurrent melena was diagnosed with GAVE. Endoscopy revealed the classical “watermelon stomach” appearance of GAVE and complete pyloric involvement. Melena reoccurred three days after argon plasma coagulation treatment, and the level of hemoglobin dropped to 47 g/L. The patient was then successfully treated with distal gastrectomy with Billroth II anastomosis. We propose that surgery should be considered as an effective option for GAVE patients with extensive and severe lesions upon deterioration of general conditions and hemodynamic instability.
Keywords: Gastric antral vascular ectasia, Melena, Distal gastrectomy, Argon plasma coagulation, Endoscopic band ligation
Core tip: Gastric antral vascular ectasia (GAVE) is still an uncommon and often neglected cause of gastric hemorrhage and surgery for treatment is not often reported in the literature. This case report represents that a GAVE patient who had recurrent melena successfully treated with distal gastrectomy. When clinical condition of GAVE patients deteriorate, surgery should be considered.
INTRODUCTION
Gastric antral vascular ectasia (GAVE) was first described in 1953 by Rider et al[1] as a cause of massive gastric hemorrhage. GAVE is an uncommon and often neglected cause of upper gastrointestinal (GI) bleeding. Endoscopic findings demonstrated that GAVE was limited almost exclusively to the antrum, and red spots were either aggregated in linear stripes (watermelon stomach) or diffusely spread[2]. Treatments include endoscopic therapy, surgery and pharmacotherapies, such as hormones, tranexamic acid and somatostatin analogues. For intractable cases, surgery is the last resort[3] because this approach has significant mortality and morbidity risks, especially in the setting of portal hypertension and liver cirrhosis[4]. Here, we report a case of recurrent GAVE refractory to argon plasma coagulation (APC) and successfully controlled by distal gastrectomy.
CASE REPORT
A 72-year-old man presented with a three-month history of recurrent melena. He described three episodes of melena with dizziness. His past medical history in a community hospital included necessary transfusion and acid suppression therapy, such as the administration of a proton pump inhibitor. The past two gastrointestinal endoscopies indicated a diagnosis of hemorrhagic erosive gastritis and chronic superficial gastritis with gastric antral erosion. His social history was significant for hypertension, which he controls well with Norvasc (10 mg, qd), and gout, which is treated with aspirin and discontinued after the first bleeding. Cirrhosis, renal failure, and connective tissue diseases were excluded.
The most recent episode occurred three days before being admitted to the hospital. Initial laboratory studies were significant for 66 g/L hemoglobin (reference range 129-173 g/L). Colonoscopy was negative. The capsule endoscopy indicated a diagnosis of hemorrhagic gastritis. Repeated endoscopy revealed the classical “watermelon stomach” appearance of GAVE and complete pyloric involvement (Figure 1). The lesion was so extensive and severe that it made it difficult for the endoscope to pass through the pylorus. After a successful pass, the friction between the endoscope and the lesions caused bleeding. Then, the patient was treated with APC (Erbe ICC200 high-frequency electrotome, 40 W) primarily for the bleeding areas. The melena recurred three days after APC, and the level of hemoglobin dropped to 47 g/L. He was then transferred to have an open surgery consisting of distal gastrectomy with Billroth II anastomosis. The operation was successful without any postoperative complication except tolerable pain. Surgical specimens revealed that the lesion was extensive and severe and that the pylorus was completely involved (Figure 2). Specimen histology revealed gastric antral mucosal erosion with bleeding from mesenchymal dilated vessels (Figure 3). Over a 12-mo follow-up period, the patient has experienced no further episodes of bleeding. His hemoglobin levels are stabilized at normal levels.
Figure 1.
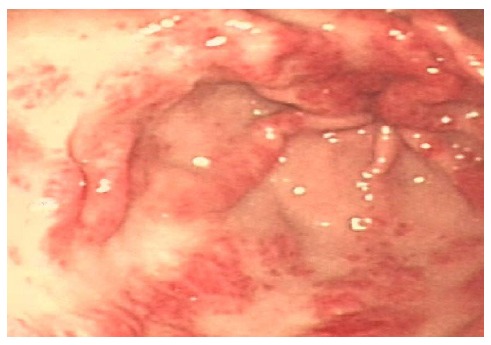
Endoscopy revealed striped lesion radially departing from the pylorus.
Figure 2.
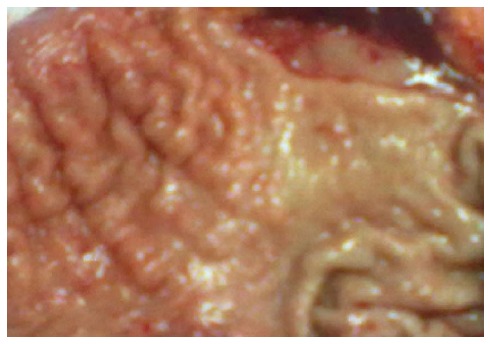
Pathological specimen revealed that lesion is extensive and serious and that the pylorus was completely involved.
Figure 3.
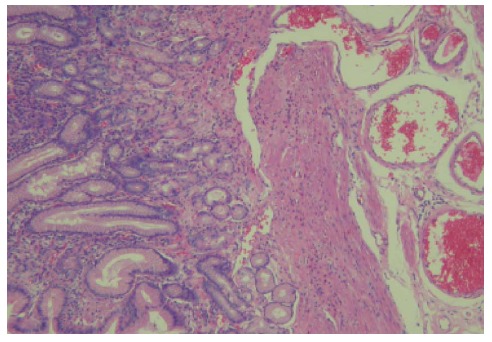
Surgical pathologic specimens indicated gastric antral mucosal erosion with bleeding from mesenchymal dilated vessels.
DISCUSSION
GAVE is an uncommon but severe cause of upper GI bleeding, and evidence suggests that GAVE is identified in 26 of 744 (4%) consecutive endoscopies for non-variceal upper GI bleeding[5]. Clinically, GAVE often coexists with other disorders. Most GAVE patients are thought to have GAVE-related comorbid conditions. Cirrhosis is observed in 30% of GAVE patients[6]. In noncirrhotic patients, autoimmune disorders are the most common; the majority of GAVE-associated disorders are connective tissue diseases, with an incidence as high as 62%[7].
Currently, many therapeutic options are available, including surgical, endoscopic and medical choices. Drug therapies, such as hormones, octreotide, and tranexamic acid, have no definite role in the cure of GAVE-related bleeding and should be considered an experimental therapeutic approach[4]. Endoscopic therapy, particularly APC treatment, has shown to be as effective as and also safer than surgery, and this therapeutic option should always be considered as the first-line treatment for patients with GAVE-related bleeding. In recent years, another endoscopic treatment, endoscopic band ligation, appeared; endoscopic band ligation was firstly reported by Sinha et al[8] as a treatment for refractory GAVE in the patients who failed other treatment modalities, such as APC or hormonal therapy. However, its utilization is still sparse, and future randomized multicenter prospective studies are necessary to conclusively establish the superiority of EBL over conventional methods for the treatment of GAVE[7].
In this case, the patient was firstly advised to have APC treatment after being diagnosed with GAVE. However, given the limited depth of thermal injury, APC treatment might not be effective in some cases[9]. In this patient, the extensive and serious area of involvement might have affected the treatment-resistant hemorrhage. Given the deteriorating clinical condition of the patient, distal gastrectomy was performed.
Surgery for GAVE treatment is not often reported in the literature. Although surgical resection is associated with a high rate of morbidity and mortality (the postoperative mortality rate was 6.6% to 7.4%) when attempted in patients with GAVE especially those with combined liver cirrhosis and other serious concomitant diseases, this treatment modality remains the only reliable method and often the last resort for refractory cases or recurrent GI bleeding[10]. Here, we propose that surgery should be considered as an effective option for GAVE patients with extensive and severe lesions upon deterioration of general conditions and hemodynamic instability.
COMMENTS
Case characteristics
A 72-year-old man with a three-month history of recurrent melena was diagnosed with Gastric antral vascular ectasia (GAVE), and three days after argon plasma coagulation (APC) treatment which primarily for the bleeding areas ,the melena recurred.
Clinical diagnosis
Gastric antral vascular ectasia was diagnosed.
Differential diagnosis
Acute hemorrhagic erosive gastritis, protal hypertensive gastropathy, peptic ulcer, small intestinal bleeding, ischemic bowel disease.
Laboratory diagnosis
On admission, the level of hemoglobin was 66 g/L; however three days after APC treatment it decreased to 47 g/L; fecal occult blood was positive.
Imaging diagnosis
Endoscopy revealed the classical “watermelon stomach” appearance of GAVE and complete pyloric involvement, and the colonoscopy was negative.
Pathological diagnosis
Specimen histology revealed gastric antral mucosal erosion with bleeding from mesenchymal dilated vessels.
Treatment
The patient was successfully treated with distal gastrectomy with Billroth IIanastomosis after failure of argon plasma coagulation (APC) treatment.
Related reports
Endoscopic therapy, particularly APC treatment always be considered as the first-line treatment for patients with GAVE-elated bleeding, while surgery the last resort for its high rate of morbidity and mortality.
Term explanation
APC which can be applied through a flexible endoscope, involves the passing of inert argon gas through a probe at a preset flow rate. The energy released by ionized gas heats the surface to a depth of 0.5 mm to 3 mm, coagulating the superficial blood vessels.
Experiences and lessons
APC treatment may not be effective in some GAVE patients and when their clinical condition deteriorate, surgery should be considered.
Peer review
This special case reminds us that surgery definitely has a place in the treatment of GAVE patients.
Footnotes
P- Reviewer: Beales ILP, Manner H, Marrelli D, Stanciu C S- Editor: Ma N L- Editor: A E- Editor: Du P
References
- 1.Rider JA, Klotz AP, Kirsner JB. Gastritis with veno-capillary ectasia as a source of massive gastric hemorrhage. Gastroenterology. 1953;24:118–123. [PubMed] [Google Scholar]
- 2.Sato T, Yamazaki K, Akaike J. Endoscopic band ligation versus argon plasma coagulation for gastric antral vascular ectasia associated with liver diseases. Dig Endosc. 2012;24:237–242. doi: 10.1111/j.1443-1661.2011.01221.x. [DOI] [PubMed] [Google Scholar]
- 3.Saad Aldin E, Mourad F, Tfayli A. Gastric antral vascular ectasia in a patient with GIST after treatment with imatinib: case report and literature review. Jpn J Clin Oncol. 2012;42:447–450. doi: 10.1093/jjco/hys032. [DOI] [PubMed] [Google Scholar]
- 4.Fuccio L, Mussetto A, Laterza L, Eusebi LH, Bazzoli F. Diagnosis and management of gastric antral vascular ectasia. World J Gastrointest Endosc. 2013;5:6–13. doi: 10.4253/wjge.v5.i1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dulai GS, Jensen DM, Kovacs TO, Gralnek IM, Jutabha R. Endoscopic treatment outcomes in watermelon stomach patients with and without portal hypertension. Endoscopy. 2004;36:68–72. doi: 10.1055/s-2004-814112. [DOI] [PubMed] [Google Scholar]
- 6.Ward EM, Raimondo M, Rosser BG, Wallace MB, Dickson RD. Prevalence and natural history of gastric antral vascular ectasia in patients undergoing orthotopic liver transplantation. J Clin Gastroenterol. 2004;38:898–900. doi: 10.1097/00004836-200411000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Keohane J, Berro W, Harewood GC, Murray FE, Patchett SE. Band ligation of gastric antral vascular ectasia is a safe and effective endoscopic treatment. Dig Endosc. 2013;25:392–396. doi: 10.1111/j.1443-1661.2012.01410.x. [DOI] [PubMed] [Google Scholar]
- 8.Sinha SK, Udawat HP, Varma S, Lal A, Rana SS, Bhasin DK. Watermelon stomach treated with endoscopic band ligation. Gastrointest Endosc. 2006;64:1028–1031. doi: 10.1016/j.gie.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Yoshida H, Takahashi H, Akoshima H, Chida N, Noguchi K, Tanabe N, Yutaka Mano, Ukai K, Tadokoro K. Successful treatment of refractory gastric antral vascular ectasia using transcatheter arterial embolization. Clin J Gastroenterol. 2013;6:231–236. doi: 10.1007/s12328-013-0385-y. [DOI] [PubMed] [Google Scholar]
- 10.Liu F, Ji F, Jin X, Du Y. Gastric antral vascular ectasia (GAVE) in two non-cirrhotic patients involved large area of stomach: case report and literature review. J Interv Gastroenterol. 2013;3:107–110. [Google Scholar]


