Abstract
The United States is typically seen as an outlier in health spending when compared with other advanced nations. Recent improvements in health accounting in lower- and middle-income countries suggest some common features with the high and pluralistic spending in the United States. The author discusses recent developments and findings in health accounting outside the Organization for Economic Cooperation and Development (OECD) and their relevance for the United States. He argues that we should expect more fruitful exchanges in the future.
Introduction
The United States has maintained detailed expenditure accounts for health care since the early 1960s and has developed a time series on health expenditure that goes back to the 1920s. So it was with some internal doubt that I agreed to write an article on what practitioners and analysts here could learn from recent experience in health accounting in the low- and middle-income countries. The World Bank recently defined high-income countries as those having a per capita gross domestic product (GDP) in 1996 greater than $9,385, middle-income countries between $766 and $9,385, and low-income countries less than $766. This grouping excludes most of the OECD member countries from the low-and middle-income groups, with the exception of Mexico and Turkey. I refer here to the low- and middle-income countries as “developing countries.” But the United States, with the developed world's most pluralistic health care system, has more in common with the majority of the world's nations than one might expect.
Defining Terms of Health Accounting
There is not yet an internationally accepted terminology for health accounting. As a result, different methods and approaches may be called by the same name. For example, “national health expenditures” (NHE) analysis refers generically to estimates of health spending that could use a variety of methods, and “national health accounts” (NHA) refers to a methodology that analyzes and displays estimates of health spending with the following characteristics:
Total national spending is estimated for a defined period of time.
The analysis presents a flow of funds from sources of spending to various uses of that spending in the form of a sources-to-uses matrix. The matrix method is used both to present data and to ensure reliability of estimates.
Both sources and uses are broken down into numerous constituent categories that do not necessarily follow the various definitions of national income accounting but rather are adapted to the policy needs of the health sector.
“Satellite health accounts” (SHA) refers to the two types of satellite accounts outlined in the 1993 revision of the United Nation's (1993) system of national accounts (SNA-93). There are some substantive methodological differences between estimates based on SNA-93 methods (which should properly refer to the value of goods and services in health) and health expenditure estimates, although these differences are sometimes modulated by data problems (Rannan-Eliya, Berman, and Somanathan, 1997). Although satellite accounts may depart from that framework in estimation and presentation, this should be done with explicit methods and tracking back to SNA-93 categories and subtotals.
Other approaches to NHE analysis discussed herein are referred to specifically according to their source. For example, the OECD health finance statistics are, strictly speaking, not compiled within an NHA framework derived from a flow-of-funds analysis in each country. Rather, statistical information on spending for a set of defined categories of uses is collected for two aggregate sources: public (including social insurance) and private.
The focus and boundaries of health accounts using these approaches differ considerably as well. In general, the term “health” accounting is misleading. Most efforts estimate expenditures for a set of economically defined activities of production and consumption that are better referred to as “health care.” There is interest in doing “health accounting,” but it is not the focus of this article. Nonetheless, in order to not add further to the confusion and in keeping with common practice, I refer to health care accounting as health accounting.
International Health Accounting
The development of internationally comparable health accounts can be traced back to two seminal studies for the World Health Organization (Abel-Smith, 1963, 1967). Both of these studies included lower- and middle-income nations along with those of higher income. Three somewhat separate lines of work emerged from this foundation.
The best known of these efforts has been organized by the OECD. Through a lengthy process of cooperation among and consultation with member countries, the OECD produced an impressive time series of health systems information, going back to the 1960s. This includes health expenditure estimates broken down by the broad categories of public and private sources and a more detailed list of specific uses. Because most OECD member countries use social insurance to finance most of their health care, more attention was given to developing feasible, useful, and comparable categories of uses than was given to disaggregating the sources of funding. Analysis of expenditures has focused on trends in the levels of total spending, spending on specific uses generally representing both types of services and the locus of provision, and the determinants of that spending in terms of volume, input prices, demography, and other factors.
A second line of work is best represented by the U.S. NHA. Although the aggregated display of the U.S. NHA looks similar to the OECD accounts in terms of the use categories (the rows), there is much more attention to disaggregating the sources of expenditure (the columns). In contrast to most other advanced nations, the United States has very pluralistic financing of health care, by which I mean that there are multiple payers on both the government/social insurance and private sector sides, and these payers finance a wide range of types of services and providers. There are several major government funding programs, involving Federal, State, and local financing, and there is a great diversity of private insurance financing. The share of government financing has increased rapidly since the 1960s. Appropriately, the system drove the accounting, and there was much more interest in analyzing the levels and composition of financing in addition to the uses of expenditures. Other advanced countries, especially those with significant private insurance sectors, have developed similarly disaggregated NHA, for example, Australia.
A third line of work grew out of national income accounting and was formalized in the 1993 revision of the United Nation's SNA-93. National income accounts already contained a number of categories that could be identified with health care, based on the classification of institutions as economic actors as well as functional breakdowns of the value of production and consumption by those institutions. SNA-93 officially encouraged the development of satellite accounts of two types (Rannan-Eliya, Berman, and Somanathan, 1997). One type of satellite account would retain the structure of the national income and product accounts but allow more flexible definitions of “health.” There are several examples of this type of satellite account, including Zaeyen et al., 1995 (Brazil), and Pommier, 1981 (France). This approach has not been widely used, perhaps because it is technically demanding and contributes more to understanding the role of the health sector in the economy than to addressing the needs of health care policymakers. The second type of satellite account allows for a much more flexible approach. This seems to be compatible in principle with NHA, but there are as yet no examples of this being done as a satellite account.
Low- and Middle-Income Countries
Since Abel-Smith's (1963) initial work, health accounting in the low- and middle-income countries could best be described as eclectic. There are many examples of country-specific accounts (Berman, 1997). Early work focused on the development of “t-style” accounts, listing revenues and expenditures in two separate tabulations. At least three manuals have been published to guide work in developing nations (Robertson, 1979; Griffiths and Mills, 1982; and Mach and Abel-Smith, 1983).
Very few countries outside of the OECD have maintained a significant time series of data on total health expenditures. Rather, there may be one or several point-in-time estimates. These were generally carried out by researchers or consultants for a specific purpose, for example, a sector or policy study, or at the request of an international organization such as the World Health Organization, as part of a comparative study. In most cases, capacity and methods for further analysis were not built up within a specific institution or government department.
There are, however, substantial time series available for government spending. The International Monetary Fund reports annual statistics on central government expenditures, which have been analyzed by Heller and Diamond (1990). Central government spending may not represent well all government health expenditures in countries where health care is primarily a State or local government function. Public finance analysts have collected more comprehensive data on central and subnational government spending and analyzed the health component (for example, Tulasidhar, Pandey, and Rey, 1992).
Many of these point-in-time studies in developing countries use some form of the NHA sources-and-uses matrix approach. Indeed, this type of analysis and presentation was highlighted in some of the manuals focusing on developing countries (several detailed examples can be found in World Health Organization, 1984). This is quite appropriate, as many lower income countries have more pluralistic structures for health care financing than those found in most OECD member nations, a characteristic shared by the United States.
Not surprisingly, the value of these individual studies has been modest. They are spread out over a variety of years for countries that experience rapid and significant economic change. Methods vary. There has been little followup within countries to track change or link it to structural differences or policy intervention. Many of the studies addressed the needs of international funders, leaving little in the country besides a summary report. Most countries still do not have national analysts permanently assigned to health expenditure estimation.
There have been several efforts to make better use of this type of information. Initially, analysts brought together a larger number of estimates from different countries into regional comparisons (McGreevey, 1990; Vogel, 1993; Griffin, 1992). Because studies for different years and employing different methods were compared, it was possible to analyze specific aspects of health spending, such as breakdowns by hospital and non-hospital service provision, line items of expenditure, and capital and recurrent spending, not simply the total and the public-private shares.
More recently, comparable estimates have been collected for the same year, using similar methods. The largest effort of this type was compiled for the World Bank's 1993 World Development Report (Murray, Govindaraj, and Musgrove, 1994). The Pan American Health Organization has also compiled estimates for Latin American countries (Suarez et al., 1995). These estimates encouraged broad comparisons across large numbers of countries. But the scope of these comparisons was limited by the data available, which were mainly total spending and the shares coming from public, insurance, and private sector sources.
The effort devoted to these global and regional cross-sectional comparisons in the developing world reflected the interest in and impact of comparative analysis by the OECD, which had been underway for more than a decade. There was also growing attention to health care financing in health policy discussions in the low- and middle-income countries. Although these large comparative analyses were promising, in fact they uncovered major problems with the data available, which raised questions about some of their basic conclusions. More careful analysis of countries covered by the World Development Report numbers (Suarez et al., 1995; Berman, 1997), in one case by the same analysts for the same years (Govindaraj, Murray, and Chellaraj, 1995), produced very different results.
Weak data can create the demand for better data, and indeed, the most recent round of work in the low- and middle-income countries reflects this. NHA has been identified as a critical basic tool for health financing policy development by a recent World Health Organization review of research priorities. Countries such as the Philippines, Mexico (a new OECD member), South Africa, and Egypt have developed repeat estimates and local capacity to sustain the work. U.S.-style NHA methods are being adapted to less data-rich environments (Berman, 1997). In 1997-1998, with support from the U.S. Agency for International Development's Partnerships for Health Reform Project and the Pan American Health Organization, 8 Latin American countries collaborated in the first of several regional networks to develop comparable methods and estimates and strengthen local teams. This year, similar networks will complete work in the Middle East and in southern Africa, covering an additional 18 countries.
NHA in the low- and middle-income countries is not yet widely accepted as essential, basic, health system information, the way it is in the OECD. Neither the supply of information nor the demand for it are well established. But three decades after Abel-Smith's (1963) initial work, momentum is building to establish this tool for health policy development among this much larger group of nations.
What we have Learned
A number of important general findings have emerged from the work to date in “the rest of the world.” The link between levels of total spending compared with GDP and average life expectancy is weak. Some of the developing countries with the best health status, such as China or Sri Lanka, are relatively low spenders as a share of income, while some of the relatively higher spending countries, such as India (which spends relatively more than other Asian countries with two to three times higher national income), have worse health status. Even among the middle-income countries, there is a wide range of relative health spending for given levels of health status. This indicates that (1) much can be done to improve health status even with more limited resources and (2) health care system performance is highly variable and can produce a wide range of efficiency outcomes.
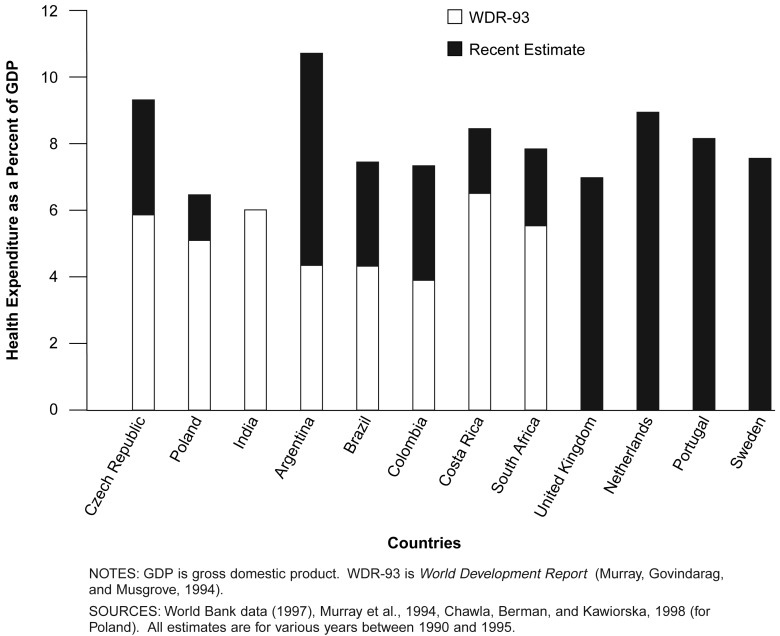
High health spending relative to national income is not exclusively a problem of rapid cost escalation in the wealthy countries. Analysis of the first round of international comparative numbers on health spending suggested an income elasticity above unity (Murray, 1994). Countries with relatively high health spending (for example, at or above the United Kingdom's level of more than 6 percent of GDP) were concentrated at the high end of the international income distribution. However, more careful analysis in the low- and middle-income countries is turning up more examples of spending at OECD levels. Recent examples include India at 6 percent of GDP, Argentina at 10.5 percent, Colombia at 7.4 percent, South Africa at 7.9 percent, the Czech Republic at 9.5 percent, and Poland at 7.3 percent. Figure 1 presents some of the striking recent examples, with comparisons to the initial World Development Report underestimates and several OECD examples. These developing countries have national incomes only a fraction (one-quarter or less) of some of the OECD examples. It is plausible that, with better estimates for more countries, analysts will need to rethink the simple linear relationship between income and health spending as a share of income. The United States may soon find company at the upper end of the spending distribution, as middle-income developing countries, such as those in South America, southeast Asia, and eastern Europe, expand insurance coverage with limited ability to control costs.
Figure 1. Estimated Health Spending in Developing Countries.
Despite the socialist rhetoric that characterized developing country governments (at least until recently), the financing of many of their health care systems may have more in common with the United States than with the western European members of the OECD. In fact, the United States looks socialist in comparison. Government and social insurance spending shares in many countries are below one-half or even below one-third of the total. Careful analysis often uncovers much higher direct spending by households and firms, even in countries such as Mexico, where social insurance coverage is around 60 percent of the population. The significant role played by multiple sources of funds and different institutional payers, often supporting the same providers, suggests that NHA-type analysis is appropriate for many developing countries. Financing reform and new financing sources will be introduced into complex payment and incentive environments and may have unforeseen effects that need to be monitored in the context of total spending and shifts in the composition of sources and uses.
NHA's strength is the ability to present a comprehensive picture of resource allocation in terms of a single measure with multiple dimensions. In the low- and middle-income countries, resource allocation has dramatic implications for national health outcomes and equity, because funds are quite limited relative to needs. Actual allocation of resources, even within government programs, has often been shown to be very different from stated priorities, whether those be emphasis on primary care services or targeting of lower income or rural populations. Inclusion of private spending can significantly change decisionmakers' long-held views about their own health care systems. In general, despite strong official statements of government support for primary care and equity in developing countries, researchers typically report:
Total spending much more skewed toward primary and ambulatory care in lower income countries than in the high-income countries.
Government funding supporting the largest share of hospital expenditures.
Private funding, mainly out-of-pocket spending, supporting the largest share of ambulatory care services.
The burden of private funding being regressively distributed relative to household income.
As in the more advanced countries, reliable NHA estimates do not come easily. There have been very significant misestimations using “quick and dirty” methods. Improving the reliability and validity of NHA will be a process of gradually identifying problems and improving the data. However, studies have shown that, for countries with even modest systems of public expenditure accounting and population and economic surveys, it is possible to assemble useful estimates at relatively low cost.
Much of the work done to date in low-and middle-income countries has been externally initiated and driven. National decisionmakers and analysts may doubt the results that emerge from the work of foreign consultants or international organizations. Often, they have done so with good reason. It is critical in future work to develop national capacity to collect and analyze NHA data on an ongoing basis.
As more complete NHA estimates become available for low- and middle-income countries, it becomes clearer that this basic tool has a variety of uses. In addition to being used as a descriptive and diagnostic methodology, there is increasing interest in basing ex ante analysis of financing reforms on simulation models building on an NHA-type framework (Solon and Tan, 1996; Australian Health Insurance Commission, 1997). As countries develop more extended time series of NHA, it will be increasingly used to monitor and evaluate financing reforms.
What can the United States Learn?
The United States and many low- and middle-income countries have developed diverse and pluralistic systems for health care financing, both for the collection and organization of financial resources as well as for the payment of providers. In the United States, expenditures from government and social insurance payers account for less than one-half of the total. Private expenditures include premiums for private insurance paid by households and firms, organized self-insurance of firms, and a significant share (17 percent in 1996) of direct household out-of-pocket expenditures. Financing by private payers includes an increasingly diverse range of institutions, including for-profit and not-for-profit indemnity insurers and various types of other health plans. Providers are mostly under private ownership, both for-profit and not-for-profit. Many elements of this description would not be unfamiliar to health system analysts in the low- and middle-income countries.
U.S.-style NHA methods are attractive in the developing countries because these methods were designed to capture important relationships in such pluralistic systems. The methods are also well suited to validity and reliability checking when data must be collected from a variety of sources, payers, and providers. This is principally achieved through the sources-and-uses matrix, with greater disaggregation for both sources and uses. In adapting these methods in other countries, several innovations have emerged that would be quite useful in the United States today.
Disaggregating Sources of Financing
One innovation that has emerged from our NHA work from the Harvard School of Public Health is the explicit breakup of sources of financing into multiple levels. The bottom level is labelled financing agents, financing intermediaries, or simply payers. These are defined as entities that receive funds from some financing source and use those funds to pay for final consumption or production of health care. These financing agents should be defined in institutional terms, that is, they capture the policy-relevant organizational structure of the payers. This representation of resource allocation across entities providing or controlling the funds for health care has useful political content—it represents an important dimension of where power lies among the institutional stakeholders.
Higher levels can be defined in terms of financing sources, typically the entities that provide the funds to the financing agents or intermediaries. Most applications to date in the developing countries have only analyzed one level above the financing agents. Typically this includes the government, international funding sources, firms, and households. One level higher, one could trace the origins of some of these funds, such as government tax revenues, to their ultimate sources, typically households and firms. This would be the procedure used to analyze the distribution of the financing burden for health care in the Nation, as part of an analysis of equity in financing (van Doerslaer, Wagstaff, and Rutten, 1993).
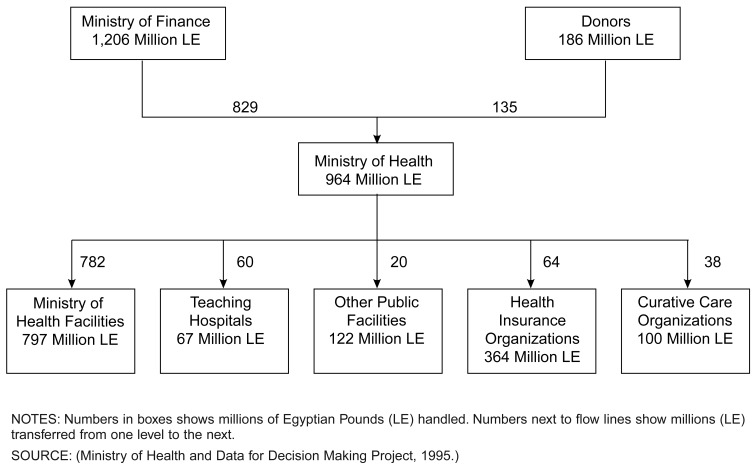
Tables 1 and 2 and Figure 2 show how this flow-of-funds approach can be presented, using data from the Egyptian NHA. The financing-agents level includes the main entities of government, social and private health insurance, and firms and households. A few conventions are important to note. First, an institutional classification of entities is used. This is compatible with the International Standard Industrial Classification (ISIC) used in the SNA-93, although the flow of funds is treated differently than in the SNA. Households are treated as a “pseudo-entity.” Second, an entity, such as households or firms, can appear at more than one level in the analysis. An entity can play more than one role in the flow of funds. A firm can pay premiums to an insurance company that pays for health care and also be a direct payer for health care services. Third, when an entity is both a payer and a provider (for example, the Ministry of Health, which pays for services in its own facilities, or a social health insurance organization, which owns and operates hospitals and clinics), this framework is useful in distinguishing between those two roles. The financing-agents breakdown focuses on the payer's role.
Table 1. Flow of Funds1 in Egypt's Health Care Financing System: Fiscal Year 1990.
| Financing Agents | Financing Source | ||||
|---|---|---|---|---|---|
|
| |||||
| All Sources | Ministry of Finance | Donors | Employers | Households | |
| All Agents | 4,166 | 1,206 | 186 | 367 | 2,407 |
| Ministry of Health | 964 | 829 | 135 | — | — |
| Ministry of Education | 270 | 270 | — | — | — |
| Ministry of Social Affairs | 7 | 7 | — | — | — |
| Other Ministries | 100 | 100 | — | — | — |
| Donors | 51 | — | 51 | — | — |
| Social Insurance Organizations | 370 | — | — | 277 | 93 |
| Private Insurance | 30 | — | — | 20 | 10 |
| Firms | 70 | — | — | 70 | — |
| Households | 2,304 | — | — | — | 2,304 |
Measured in millions of Egyptian pounds.
Table 2. Amounts1 Paid to Providers, by Financing Agents: Fiscal Year 1990.
| Provider Type | Financing Agent | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| All Agents | Ministry of Health | Ministry of Education | Ministry of Social Affairs | Other Ministries | Donors | Social Insurance Organizations | Private Insurance | Firms | Households | |
| All Providers | 4,166 | 964 | 270 | 7 | 100 | 51 | 370 | 30 | 70 | 2304 |
| Ministry of Health | 797 | 782 | — | — | — | — | — | — | — | 15 |
| Teaching Hospitals | 67 | 60 | — | — | — | 3 | — | — | — | 4 |
| University Hospitals | 342 | — | 270 | — | — | 24 | — | — | — | 48 |
| Other Public Facilities | 122 | 20 | — | — | 100 | 2 | — | — | — | — |
| Health Insurance Organization Facilities | 364 | 64 | — | — | — | — | 280 | — | 1 | 19 |
| Curative Care Organizations | 100 | 38 | — | — | — | 1 | — | 3 | 20 | 38 |
| Non-Governmental Organizations | 55 | — | — | 7 | — | 16 | — | — | 2 | 30 |
| Private Medical Sector | 955 | — | — | — | — | 5 | — | 13 | 37 | 900 |
| Pharmacies | 1,254 | — | — | — | — | — | — | 14 | 10 | 1,230 |
| Other Private | 110 | — | — | — | — | — | 90 | — | — | 20 |
Measured in millions of Egyptian pounds.
Figure 2. Partial Diagram of Flow of Funds in Egypt's Health Care Financing System: Funds to and Through the Ministry of Health: Fiscal Year 1990.
The flow of funds can be represented in a tabular form or in a diagram. Tables 1 and 2 show the tabular approach. Table 1 shows the distribution of money from the ultimate source of funds to financing agents, and Table 2 shows the subsequent distribution of money from those agents to the various entities engaged in the provision of care. Figure 2, on the other hand, shows how a portion of the flow of funds can be represented diagrammatically, focusing on the Ministry of Health in its role as financing agent and tracing the origin of the funds it handles and the disposition of those funds to the provider level.
In the United States, this approach, with U.S.-appropriate institutional classifications, would enable analysts to monitor the increasing diversity of payers as well as changes in the market share and sources of financing of different payer types. The category of private insurance is clearly insufficient to capture the rapidly changing insurance market in the United States. For example, the rapid growth of managed care includes a variety of different types of plans whose composition and characteristics are constantly changing (Weiner and de Lissavoy, 1993). There is increasing interest in government financing of social health insurance through payment of premiums to such plans. Disaggregating the side of NHA that represents collection and organization of financial resources can be done in a flexible way that would allow new classifications to be created in response to changes in the insurance industry. Would it not be useful to track the shifting composition of private payers in the health care system, in terms of both their shares of total and private spending as well as changes in the sources of their funding? Would this be feasible based on a set of measurable characteristics of health plans?
Reconstructing Classifications of Uses
Another area of innovation in international work has been in revisiting the classifications of uses of expenditure. Table 3 presents the use classifications employed in the current OECD health expenditure accounts, at the highest level of aggregation. The U.S. NHA follows most of these categories, with some variations. These categories had policy relevance and emerged from a process of adaptation to feasibility and cost. But, in reviewing these classifications and some of the manuals already cited, the logic of classification was not clear, nor were these the most policy-appropriate categories for developing countries.
Table 3. Constituent Categories1 of OECD Health Expenditure Accounts.
|
Highest level of aggregation.
NOTE: OECD is Organization for Economic Cooperation and Development.
SOURCE: (Berman, P., 1997.)
One example from Table 3 is expenditures for pharmaceuticals. Pharmaceuticals are listed as a separate expenditure category under medical goods. The same approach is used in the U.S. NHA. This category refers to expenditures for pharmaceuticals purchased directly for final consumption, for example, filling a prescription after a physician visit. Pharmaceuticals used for inpatient treatment while in a hospital or provided in a physician's office during an ambulatory care visit are counted as expenditures for inpatient care or physicians' services, respectively. The pharmaceuticals category in the accounts is largely pharmaceutical purchases from pharmacies, although one would need to read the fine print to know that. Another well-known example has to do with physician services. In the United States, a large share of physician services provided to inpatients in a hospital are billed separately by physicians, while in most other OECD member countries, these costs are included in hospital charges. This is a well-known hindrance to comparing U.S. expenditure data with that of other OECD nations. But it has also been noted at previous HCFA meetings as a problem for analyzing resource allocation within the U.S. health care system (Haber and Newhouse, 1991).
The approach now applied in many developing countries is to develop use classifications based on distinct logical categories and to use these classifications to produce multiple accounts of the same health spending total. The following five such classifications seem most useful:
Expenditures for different types of providers.
Expenditures for different types of services, diseases, or health care functions.
Expenditures for different factor inputs (line items or economic categories).
Benefit incidence of expenditure to different geographical areas.
Benefit incidence of expenditure to different socioeconomic groups.
Examples of some of the main subcategories are given in Table 4. In all of these classifications, there would also be an “other” category, which holds expenditures that cannot be classified in this way, so that the tables can maintain the same national total. For example, the administrative cost of health insurance would not appear in classifications 1, 2, 4, or 5, but could be included in 3. It is also desirable to mix the categories, but this should be done by creating new levels within one classification, for example, estimating the type-of-service or factor-input breakdown for different types of providers. It is not logically possible to mix the categories at the same level of classification.
Table 4. Typical Entities Used in National Health Accounts in Developing Countries.
|
SOURCE: (Berman, P., 1997.)
As mentioned, this issue is not new to HCFA and figured significantly in the recommendations from the 1990 Technical Advisory Panel (Haber and Newhouse, 1991). It has now also been included in recent proposals to revise and standardize the OECD classifications and to develop a combined international standard (Huber, 1999). In this regard, reference is often made to various international institutional and functional classifications used in the SNA (for example, the ISIC, the Classification of the Functions of Government, and the Classification of Individual Consumption by Purpose.)
The classifications developed for the analysis of general economic activity are not always complete enough or specific enough to satisfy the needs of health policymakers. For example, ISIC, as applied in the SNA, classifies institutions' economic activity according to their primary function. An enterprise-owned clinic or hospital may not appear in the national income accounts as health consumption but rather as a labor cost to the firm. Functional classifications of health expenditures may not distinguish between inpatient treatments in the hospital and ambulatory treatment or public health services run out of a hospital. Yet these can be important distinctions for health policymakers. There is clearly an advantage to using standard international classifications. But a strength of NHA is its policy relevance. Some further adjustments may be needed.
A more logically consistent breakdown of uses would be immensely valuable in helping us understand the shifting venues and contents of health care being driven by new payment methods, care management, technology, and consumer preferences. The relevance of these questions to the United States today is obvious. The United States has been in a period of several years in which total health spending has remained fairly stable, but the ways in which that spending is being used seem to be changing dramatically. Levit and colleagues (1998), in their recent presentation of the 1996 NHA, cite significant changes in hospital and physician practices, such as shifting services within hospitals from inpatient to outpatient procedures. But it remains very difficult to quantify the components of these changes from the available breakdowns.
The proposed new OECD (1998) system of health accounts includes categories and definitions for provider and functional breakdowns that are very compatible with the current approach in developing countries. These classifications can capture much better the shifting picture of what types of care are being provided by whom in reforming health care systems. These newly standardized classifications from OECD have been adopted and further adapted. One innovation recommended for developing countries (Berman and Thompson, 1999) is augmenting provider breakdowns with ownership classifications, for example, showing expenditure to hospitals according to government and private ownership, including for-profit and non-profit institutions. In the United States, this addition would increase ability to monitor the implications of changing provider ownership.
The nagging question is: To what extent is this feasible with the available data? Admittedly, in the developing countries, one sometimes has the luxury of initiating the data collection as well as the analysis. In Egypt, for example, Harvard worked with the Ministry of Health to develop a functional classification of its own expenditure alongside the development of NHA. Prior to this project, the central government provided block grants to the provinces with no accounting for use of funds other than the line-item categories (salaries, drugs, and supplies, etc.) accompanying the funds. The Egypt project included development of a program-budgeting type of accounting and a financial reporting system, which provide a much better picture of actual resource allocation than had been available previously (Ministry of Health and Research Triangle Institute, 1995). In the United States, where so much of the data is in the hands of private payers, there are certainly difficulties.
Equity Analysis
With limited insurance coverage and benefits and high out-of-pocket spending, there is concern in the developing countries about the distribution of the financial burden and incidence of the financial benefits of the health care system. There is growing interest in using NHA to support analyses of equity in financing.
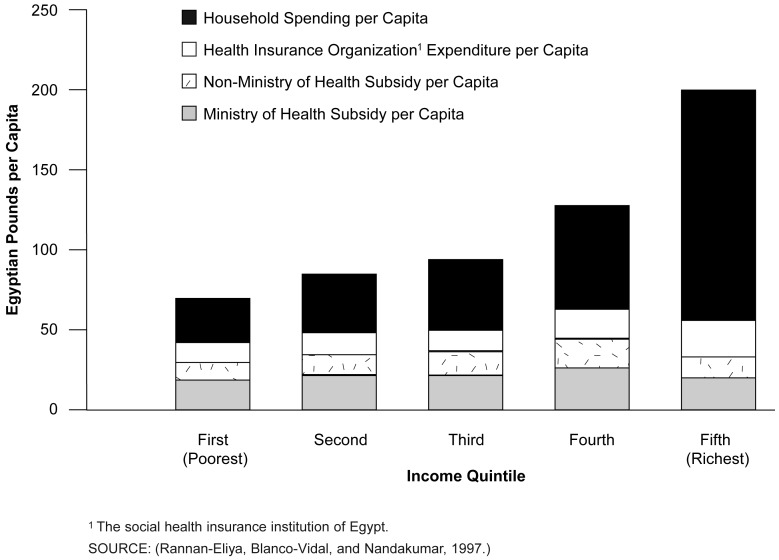
One recent example emerged from Harvard's work in Egypt (Rannan-Eliya, Blanco-Vidal, and Nandakumar, 1997). Not surprisingly, it was impossible to analyze the distribution of the tax burden on the population, given the data available there. The study, therefore, focused on a benefit-incidence analysis. As shown in Figure 3, it was possible to estimate the distribution of health expenditures by income quintiles for the country. NHA was used as the base for allocation. An innovation in this study was the use of different costs and prices for different types of providers and services in different regions of the country. These were obtained from more detailed cost studies and from a national household health care use and expenditure survey. Most previous studies of this type were not able to adjust aggregate expenditures in this way.
Figure 3. Benefit Incidence of Health Expenditure: Egypt, 1995.
The results of this study showed a relatively equitable distribution of government spending but a highly inequitable distribution of total spending. The study also highlighted a relatively high out-of-pocket spending burden borne by the lower income groups.
Data Triangulation
Estimating specific components of health spending from different and often contradictory data sources has been a topic of much discussion in the U.S. NHA and certainly affects estimation in the low-and middle-income countries. Direct household spending is especially problematic. General consumption expenditure surveys tend to underestimate household health spending, while dedicated health care expenditure surveys may overestimate it. It would be useful to try to quantify the direction and size of these effects through a meta-analysis of different sets of surveys purporting to measure the same quantity and to develop some type of standard adjustment algorithm.
Capital Investment
Treatment of capital investment is one of the basic differences between SNA and NHA methods. The former in principle takes a “value” approach, while the latter focuses on nominal expenditures. In low-and middle-income countries, most of the historical investment in hospitals came from government. The private share of hospital provision was small, in contrast to a larger role in ambulatory care. This is now rapidly changing in some countries, where private hospital investment may be rapidly increasing and government investment declining. Current expenditure estimates generally do not address capital investment in a consistent way. Public investment is treated as an expenditure fully captured in the current account, while amortized private investment (plus the cost of capital) is assumed to be included in private prices. Because public sector payment to private providers is still small in many developing countries, we have not been too concerned about the problem of public payments picking up this share of private investment.
Conclusions
The United States has usually been cast as the outlier among the other OECD-member nations in terms of the level and structure of health spending. Casting the net wider, the diversity of finance sources, payers, and providers that characterizes the U.S. health care system does not seem so unusual. Because NHA was particularly suited to capturing these characteristics and to assuring more reliable estimates in a pluralistic setting, it has been well suited to wider application in the low- and middle-income countries.
The development of NHA in the rest of the world has profited greatly from the U.S. experience. But the United States can also gain something from some of the fresh approaches being developed elsewhere. Health care, especially in the middle-income countries, is developing rapidly. We can expect to see more fruitful exchanges in terms of both substance and methods in the future.
Acknowledgments
The comments of outside reviewers and participants at the HCFA workshop in March, 1998, are gratefully acknowledged.
Footnotes
Peter Berman is director of the International Health Systems Group, the Harvard School of Public Health. Most of the work reported on in this article was financed by the U.S. Agency for International Development, through the Data for Decision Making Project (Cooperative Agreement No. DPE5991-AA-00-1052-00) and the Partnerships for Health Reform Project (Contract No. HRN-5974-C-00-5024600 with Abt Associates, Inc.). The views expressed in this article are those of the author and do not necessarily represent the views of Harvard School of Public Health, Abt Associates, Inc., or the Health Care Financing Administration (HCFA).
Reprint Requests: Dr. Peter Berman, IHSG, Bldg 1, Rm. 1210, 677 Huntington Avenue, Boston, MA 02115. Email: pberman@hsph.harvard.edu
References
- Abel-Smith B. Paying for Health Services: A Study of the Costs and Sources of Finance in Six Countries. Geneva: World Health Organization; 1963. Public Health Papers, No. 17. [Google Scholar]
- Abel-Smith B. An International Study of Health Expenditure and Its Relevance for Health Planning. Geneva: World Health Organization; 1967. Public Health Papers, No. 32. [PubMed] [Google Scholar]
- Australian Health Insurance Commission. Design of the Generic Health Financing Model. Canberra, Australia: 1997. Unpublished manuscript. [Google Scholar]
- Berman P. National Health Accounts in Developing Countries: Appropriate Methods and Recent Applications. Health Economics. 1997;6(1):11–30. doi: 10.1002/(sici)1099-1050(199701)6:1<11::aid-hec238>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Berman P, Thompson A. Developing National Health Accounts in Lower Income Countries.: Preliminary Revised Guidelines for Boundaries and Classifications to Improve Compatibility with Emerging International Standards. Boston, MA.: Harvard School of Public Health; 1999. Draft paper. Partnerships for Health Reform Project. [Google Scholar]
- Chawla M, Berman P, Kawiorska D. Financing Health Services in Poland: New Evidence on Private Expenditures. Health Economics. 1998;7:337–346. doi: 10.1002/(sici)1099-1050(199806)7:4<337::aid-hec340>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Govindaraj R, Murray CJL, Chellaraj G. Health Expenditures in Latin America. Washington, DC.: World Bank; 1995. World Bank Technical Paper No. 274. [Google Scholar]
- Griffin CC. Health Care in Asia: A Comparative Study of Cost and Financing. Washington, DC.: World Bank; 1992. World Bank Regional and Sectoral Studies. [Google Scholar]
- Griffiths A, Mills M. Money for Health: A Manual for Surveys in Developing Countries. Geneva: Sandoz Institute for Health and Socio-Economic Studies and the Ministry of Health of the Republic of Botswana (Gaborone); 1982. [Google Scholar]
- Haber S, Newhouse J. Recent Revisions to and Recommendations for National Health Expenditures Accounting. Health Care Financing Review. 1991 Fall;13:1. [PMC free article] [PubMed] [Google Scholar]
- Heller P, Diamond J. International Comparisons of Government Expenditure Revisited: The Developing Countries 1975-86. Washington, DC: International Monetary Fund; 1990. Occasional Paper No. 69. [Google Scholar]
- Huber M. Health Expenditure Trends in OECD Countries, 1970-1997. Health Care Financing Review. 1999 Winter;21(2):47–63. [PMC free article] [PubMed] [Google Scholar]
- Levit KR, Lazenby HC, Braden BR, et al. National Health Spending Trends in 1996. Health Affairs. 1998;17(1):35–51. doi: 10.1377/hlthaff.17.1.35. [DOI] [PubMed] [Google Scholar]
- Mach EP, Abel-Smith B. Planning the Finances of the Health Sector: A Manual for Developing Countries. Geneva: World Health Organization; 1983. [Google Scholar]
- McGreevey W. Social Security in Latin America: Issues and Options for the World Bank. Washington, DC.: World Bank; 1990. World Bank Discussion Paper 110. [Google Scholar]
- Ministry of Health, Arab Republic of Egypt, and Research Triangle Institute. Egypt: Budget Tracking System. Boston: Harvard School of Public Health; 1995. Data for Decision Making Project. [Google Scholar]
- Ministry of Health, Arab Republic of Egypt, and the Data for Decision Making Project: National Health Accounts for Egypt. Boston, MA.: Harvard School of Public Health; 1995. Publication No. 25. [Google Scholar]
- Murray CJL, Govindaraj R, Musgrove P. National Health Expenditures: A Global Analysis. In: Murray CJL, Lopez AD, editors. Global Comparative Assessments in the Health Sector. Geneva: World Health Organization; 1994. [PMC free article] [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development. A System of Health Accounts for International Data Collection. 4. Vol. 98. Paris: 1998. STD/NA/RD. [Google Scholar]
- Pommier P. Social Expenditure: Socialization of Expenditure? The French Experiment with Satellite Accounts. Review of Income and Wealth. 1981 Dec;27:4. [Google Scholar]
- Rannan-Eliya R, Berman P, Somanathan A. Health Accounting: A Comparison of the SNA and NHA Approaches. Bethesda, MD.: Abt Associates; 1997. Draft paper. Partnerships for Health Reform Project. [Google Scholar]
- Rannan-Eliya R, Blanco-Vidal C, Nandakumar AK. Equity in the Delivery of Health Care in Egypt: An Analysis Using a National Health Accounts Framework. Boston, MA.: Harvard School of Public Health; 1997. Data for Decision Making Project. [Google Scholar]
- Robertson RL, et al. Guidelines for Analysis of Health Sector Financing in Developing Countries. Bethesda, MD: U.S. Department of Health, Education, and Welfare; 1979. [Google Scholar]
- Solon O, Tan CR. Getting More Answers from the National Health Accounts (Through an NHA-Based Policy Simulation Model) 1996. Unpublished manuscript.
- Suarez R, Henderson P, Barillas E, Vieira C. National Health Expenditure and Financing in Latin America and the Caribbean. Washington, DC.: Pan American Health Organization; 1995. (Health Development Series No. 3). [Google Scholar]
- Tulasidhar VB, Pandey PC, Rey D. States Financing of Health Care in India: Some Recent Trends. New Delhi: National Institute of Public Finance and Policy; 1992. [Google Scholar]
- United Nations: System of National Accounts 1993. New York: 1993. [Google Scholar]
- van Doerslaer E, Wagstaff A, Rutten F. Equity in the Finance and Delivery of Health Care. Oxford: Oxford University Press; 1993. [Google Scholar]
- Vogel RJ. Financing Health Care in Sub-Saharan Africa. Westport, CT.: Greenwood Press; 1993. [Google Scholar]
- Weiner J, de Lissavoy G. Razing a Tower of Babel: A Taxonomy for Managed Care and Health Insurance Plans. Journal of Health Politics, Policy, and Law. 1993 Spring;18:1. doi: 10.1215/03616878-18-1-75. [DOI] [PubMed] [Google Scholar]
- World Bank. Health, Population, and Nutrition Data Base. 1997. Unpublished data.
- World Health Organization. World Health Statistics Quarterly. Vol. 37. Geneva: 1984. 1994. p. 4. [Google Scholar]
- Zaeyen A, Silva ABdOe, Sobral CCB, et al. Economia Politica da Saude: Uma Perspectiva Quantitativa. Pan American Health Organization. Brazil Office; Brasilia: 1995. (Serie Economia e Financiamento No. 5). [Google Scholar]