Abstract
The Transtheoretical Model (TTM, the “stage model”) can guide development of programs to increase Medicare beneficiaries' readiness to make informed health plan choices. In this study, TTM staging algorithms were developed to assess readiness to engage in three types of informed choice: (1) learning about the Medicare program; (2) learning about Medicare health maintenance organizations (HMOs); and (3) reviewing different plan options. Stage of change based on all three algorithms is related to knowledge about the Medicare program and information-seeking. Findings provide evidence for the construct validity of the stage measures and for the applicability of the TTM to informed choice among beneficiaries.
Introduction
The Balanced Budget Act (BBA) of 1997 authorized a number of new health plan options under the Medicare+Choice program. CMS has launched a comprehensive campaign, the National Medicare Education Program (NMEP), to raise awareness among Medicare beneficiaries about their options, educate beneficiaries about the characteristics of different plan types, and help beneficiaries assess the advantages and disadvantages each choice holds for them, among other things. A primary goal of the NMEP is to ensure that beneficiaries make informed choices, regardless of whether they stay with Original Medicare or choose one of the new options. CMS is responsible for demonstrating improvement over time in the level of awareness and understanding beneficiaries have about their health plan options.
The CMS campaign can benefit from empirically validated conceptual models that can (1) explain and facilitate movement from one level of awareness about choice to another, (2) provide reliable methods of identifying groups of beneficiaries who may be more or less receptive to messages and information about informed choice, and (3) provide guidance in the targeting and tailoring of messages for different groups. Based on qualitative research, CMS has recently adopted an information-seeking model that segments beneficiaries into three groups, according to information-seeking behaviors:
Passive information-seekers, who lack specific strategies for gathering information they need. They may make poor decisions or fail to obtain valuable services due to lack of information. This is the largest segment of beneficiaries.
Proactive information-seekers, who seek information in advance of needing the information.
Reactive information-seekers, who seek information only in response to developmental or environmental events, such as the onset of a new illness or change in financial situation.
Although this approach provides a useful description of individual differences in beneficiaries' attitudes and habitual ways of responding to information, it lacks an empirically validated framework and the tools necessary to help beneficiaries change their information-seeking behavior.
The TTM, one of the leading models of health behavior change, offers an alternative approach to market segmentation. Briefly, the TTM understands change as progress over time through a series of stages: precontemplation, contemplation, preparation, action, and maintenance. Passive information-seekers in the CMS current CMS model might be conceptualized as precontemplators; proactive information-seekers as individuals in the action stage; and reactive information-seekers as individuals who are spurred into action unintentionally and perhaps without adequate preparation.
Unlike sociodemographic variables (e.g., income, education) often examined in Medicare audience research, stage of change is not static, but dynamic and modifiable. Nearly 20 years of quantitative research on a variety of health behaviors has identified the principles and processes of change that work best in each stage to facilitate progression through the stages. For example, increasing the pros (perceived advantages) of engaging in a new behavior facilitates movement from the precontemplation stage, and reducing the cons (perceived disadvantages) facilitates movement from the contemplation stage. This research can serve as a foundation on which to build stage-matched interventions to increase participation in informed health plan choice among Medicare beneficiaries. The TTM can provide intervention tools to help beneficiaries progress from passive acceptance of their current plan to more active participation in informed choice based on an understanding of the Medicare program and available health plan options. It can also provide sensitive measurement tools to monitor change over time.
TTM
The TTM systematically integrates four theoretical constructs central to change:
Stages of Change—Readiness to take action.
Decisional Balance—Pros and cons associated with a behavior's consequences.
Self-Efficacy—Confidence to make and sustain changes in difficult situations, and temptation to slip back into old patterns.
Processes of Change—Ten cognitive, affective, and behavioral activities that facilitate change.
Stage of change, the central organizing construct of the model, represents the temporal and motivational dimensions of the change process. Longitudinal studies of change have found that people move through a series of five stages when modifying behavior on their own or with the help of formal intervention (DiClemente and Prochaska, 1982; Prochaska and DiClemente, 1983). In the first stage of change, the precontemplation stage, individuals deny they have a problem and thus are resistant to change, are unaware of the negative consequences of their behavior, believe the consequences are insignificant, or have given up the thought of changing because they are demoralized. They are not intending to change in the next 6 months. Individuals in the contemplation stage are more likely to recognize the benefits of changing. However, they continue to overestimate the costs of changing and, therefore, are ambivalent and not quite ready to change. They are intending to make a change within the next 6 months. Individuals in the preparation stage have decided to make a change in the next 30 days and have already begun to take small steps toward that goal. People in the action stage are overtly engaged in modifying their problem behaviors or acquiring new, healthy behaviors. Individuals in the maintenance stage have been able to sustain change for at least 6 months and are actively striving to prevent relapse.
The stage construct has received empirical support across a broad range of health-related behaviors (Prochaska et al., 1994). These include daily behaviors, such as eating a low-fat diet (Greene et al., 1999), and yearly behaviors, such as mammography screening (Rakowski et al., 1996). These behaviors include acquisition behaviors, such as exercise (Marcus et al., 1992), and cessation behaviors, such as quitting smoking (Prochaska and DiClemente, 1983). Stage assessments also have been validated for professional practices, such as collaborative service delivery (Levesque, Prochaska, and Prochaska, 1999) and for decisionmaking among families faced with the choice to donate a loved one's organs (Robbins et al., 2001). Given the broad applicability of the stage construct, we hypothesized that the stage model could be applied to informed choice in the Medicare population. The present study is a preliminary test of that hypothesis.
Research comparing stage distributions across behaviors and populations found that about 40 percent of pre-action individuals were in precontemplation, 40 percent in contemplation, and only 20 percent in preparation (Laforge et al., 1999; Velicer et al., 1995). These data suggest that if we offer all beneficiaries action-oriented interventions that assume readiness to participate in informed choice, we are mis-serving the majority who are not prepared to take action.
Stage of change is generally assessed using a staging algorithm, a set of decision rules that place individuals in one of five mutually exclusive stage categories based on their responses to a few questions about their intentions, past behavior, and present behavior. This approach to staging is robust across behaviors and populations (DiClemente et al., 1991; Prochaska et al., 1994).
Stage-Matched Interventions
In a comparative analysis of 24 major systems of psychotherapy, Prochaska (1984) distilled a set of 10 fundamental processes by which people change. The set was refined following further theoretical analyses (Prochaska and DiClemente, 1984) and empirical studies (Prochaska and DiClemente, 1985; 1986). These processes describe the basic patterns of activity therapists try to encourage or elicit to help clients change problem behaviors, affects, cognitions, or interpersonal relationships. The 10 processes applied to informed choice are defined here:
Consciousness Raising—Increasing awareness and information about making an informed choice or its benefits.
Dramatic Relief—Experiencing strong negative emotions that go along with not making an informed choice.
Environmental Re-Evaluation—Realizing the impact of making or not making an informed choice on other people.
Self-Re-Evaluation—Emotional and cognitive reappraisal of values related to informed choice.
Self-Liberation—Making or demonstrating a firm commitment to making an informed choice.
Reinforcement Management—Increasing intrinsic and extrinsic rewards for making an informed choice.
Helping Relationships—Seeking and using social support to encourage or help with informed choice.
Counter-Conditioning—Substituting new behaviors and cognitions for old responses.
Stimulus Control—Adding cues or reminders to make an informed choice.
Social Liberation—Realizing that society is changing to support informed choice.
Nearly 20 years of research on a variety of health behaviors has identified processes of change that work best in each stage to facilitate change. For example, the data show that individuals in the precontemplation stage rely on consciousness raising, dramatic relief, and environmental re-evaluation; individuals in action rely more on reinforcement management, helping relationships, and stimulus control (DiClemente et al., 1991; Prochaska and DiClemente, 1983; 1984; Prochaska, DiClemente, and Norcross, 1992). Stage-matched interventions can have a greater impact than action-oriented, one-size-fits-all programs by increasing participation and increasing the likelihood that individuals will take action. Stage-matched interventions for smokers more than double the smoking-cessation rates of the best traditional interventions available (Prochaska et al., 1993; Strecher et al., 1994). Stage-matched interventions have outperformed one-size-fits-all interventions for exercise acquisition (Marcus et al., 1998), dietary behavior (Campbell et al., 1994), mammography screening (Rakowski et al., 1998), and other health behaviors in 20 population-based studies.
TTM research provides a scheme for tailoring population-based education programs by matching them to the needs of people at each stage of change. It can serve as a scientific framework for integrating and coordinating diverse components of an educational campaign, such as Web sites, mailings, hotlines, counselors, and health fairs. Each component can be evaluated and enhanced to maximize stage appropriateness for the target population.
The TTM assessments also can be used to provide individually tailored educational materials. For example, stage-matched interventions for Medicare beneficiaries could be administered by means of informed-choice booklets, by State Health Insurance Assistance Program (SHIP) counselors, or by computerized expert systems accessed by the Internet, desktop computers, or kiosks. Once education programs are in place, stage assessments can identify segments of the population that are progressing toward action and segments that are stalled in the early stages. Such sensitive assessments can help program leaders understand how ready the population is to make informed choices. These assessments also allow programs to meet the challenge of assisting individuals in the early stages to move forward by enhancing communications to match the needs of those who are not progressing.
Assessing Readiness
The first step in the application of the TTM to a new area is the development of valid measures of stage and other dimensions of the model. Early on, we recognized that informed choice had not been defined in the BBA, and that the concept is multifaceted and fluid and may depend somewhat on the characteristics of beneficiaries and the Medicare health plan choices available to them.
In a subsequent project, we worked with CMS research and program operations staff to develop a consensus definition of informed choice and gold-standard measures of stage of change and other TTM dimensions (Levesque, Cummins, and Prochaska, 2000). Based on interviews with CMS staff, informed choice was defined as a two-step process. Step I involves an annual review, much like an annual checkup, to ensure that all is in working order. Beneficiaries would review their current plan to determine if it still meets their needs. Beneficiaries who find that their plan does not meet their needs (and new enrollees) would move to Step II and compare different plans. Annual review was further defined as checking on costs, benefits covered, doctors and hospitals that can be used, and rules that must be followed to get care, and considering whether or not a plan still meets the beneficiaries' needs, given their health and financial situation. Comparing different plans was defined as finding out what the Medicare health plan choices are, gathering information on different Medicare health plans, comparing the advantages and disadvantages of the available choices, such as costs, benefits covered, doctors and hospitals that can be used, rules that must be followed to get care, and quality of the health care provided, and using this information to choose the plan that best meets the beneficiaries' needs, given their health and financial situation. CMS staff found this approach to informed choice to be non-threatening, supportive, and appropriate for beneficiaries with varying degrees of choice (Levesque, Cummins, and Prochaska, 2000).
However, in the present project, the goal was to conduct a preliminary test of the applicability of the TTM to informed choice by developing and validating stage measures constructed from data collected in CMS's 1996, 1997, and 1998 Medicare Current Beneficiary Survey (MCBS) administered between 1997 and 1999. The MCBS is an excellent source of empirical data on beneficiary knowledge, information-seeking behavior, and other dimensions that represent CMS's increasing concern about and conceptualization of informed choice at the time. This project had three objectives:
To determine if staging algorithms assessing readiness to learn about the Medicare program and about Medicare HMOs, two components of informed choice, could be created from questions currently included in the MCBS.
To develop, for inclusion in upcoming beneficiary assessments, a new TTM measure assessing stage of change for a third component of informed choice, reviewing health plan options.
To test the construct validity of these new measures.
This preliminary research provided measurement tools for assessing the efficacy of CMS's communication and education campaigns and laid the foundation for other work underway to develop more refined TTM assessments and stage-matched programs.
MCBS
The MCBS, conducted by CMS's Office of Strategic Planning and administered by Westat, is designed to provide longitudinal data on Medicare beneficiaries' health care utilization and expenditures, health status, and demographic and behavioral characteristics. The survey contains periodic supplements to address pressing policy issues (e.g., assessments of beneficiaries' experiences with and attitudes about HMOs, assessments of knowledge about the Medicare program). The MCBS has been administered three times annually since 1991 and now utilizes a rotating panel design. Each year, more than 3,000 beneficiaries drawn from CMS's Medicare enrollment file are recruited into the survey and invited to participate for up to 4 years before being rotated out and replaced by new participants. Stratified random sampling techniques are used to ensure adequate representation of beneficiaries from targeted geographical areas throughout the Nation and the overrepresentation of beneficiaries who are under age 65 or over age 85. The MCBS oversamples Medicare HMO enrollees periodically. Surveys are administered in person to beneficiaries or designated proxies.
The current study involves cross-sectional and longitudinal analyses of data from Rounds 18, 19, 20, 23, and 24 of the MCBS administered in 1997, 1998, and 1999. The new stage-of-change measure developed specifically for this study was included in Round 23 of the MCBS.
Development of TTM Readiness Measures
Learning About the Medicare Program
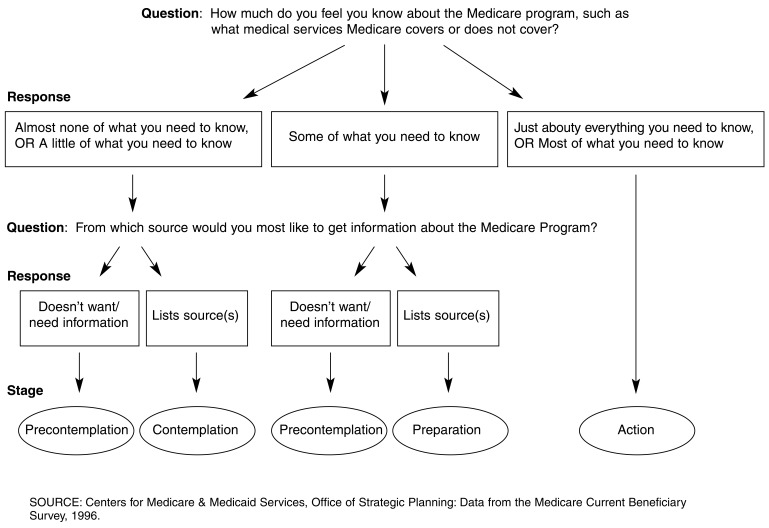
Survey items in the MCBS Round 18 supplement were used to construct two staging algorithms to assess beneficiaries' readiness to make informed health plan choices. The first staging algorithm, which classifies beneficiaries into one of four stages representing readiness to learn about the Medicare program, uses the two following questions from the Round 18 MCBS:
How much do you feel you know about the Medicare program, such as what medical services Medicare covers or does not cover?
From which source would you most like to get information about the Medicare program?
Figure 1 illustrates the decision rules for the Medicare program algorithm. Beneficiaries who reported that they knew “almost none,” “a little,” or “some” of what they needed to know and stated that they did not want or need additional information were classified in the precontemplation stage. Beneficiaries who knew “almost none” or “a little” of what they needed to know and listed sources from which they would like to get information were classified in the contemplation stage.Beneficiaries who knew “some” of what they needed to know and listed additional information sources were classified in the preparation stage. Finally, individuals who reported that they knew “most” or “just about everything” they needed to know were classified in the action stage. The MCBS did not include questions that might differentiate between beneficiaries in the action and maintenance stage (e.g., questions about how long individuals had been seeking information or been at their current knowledge level). Thus, the maintenance stage was not identified using this staging algorithm.
Figure 1. Proxy-Staging Algorithm Assessing Readiness to Learn About the Medicare Program.
Learning About Medicare HMOs
The second staging algorithm, which classifies beneficiaries into one of four stages representing readiness to learn about Medicare HMOs, utilized the following two questions from the MCBS:
How much do you feel you know about the availability and benefits of Medicare health maintenance organizations (Medicare HMOs)?
From which source would you most like to get information about Medicare HMOs?
Decision rules for classifying individuals into the precontemplation, contemplation, preparation, and action stages for learning about Medicare HMOs are identical to the rules previously outlined and illustrated in Figure 1.
Reviewing Health Plan Options
Although knowledge about the Medicare program and Medicare HMOs is necessary for informed choice, a major goal of the NMEP is to increase beneficiaries' awareness about different health plan options. Thus, a third staging algorithm was developed to assess beneficiaries' readiness to review their options. Pro-Change staff and research and operations staff from CMS's Office of Strategic Planning and Center for Beneficiary Services jointly developed the following staging questions for the MCBS Round 23 Supplement:
Starting in 1999, Medicare will offer new health plan choices. You may want to review these choices. Have you reviewed information about different Medicare health plan choices?
How long have you been reviewing information about different Medicare health plan choices?
Do you intend to review information about your Medicare health plan choices in the next year?
Do you intend to review information in the next 3 months?
Beneficiaries were classified into stages based on the following rules:
Precontemplation—Has not reviewed health plan options and has no intention of reviewing in the next year.
Contemplation—Has not reviewed options but intends to review in the next year.
Preparation—Has not reviewed options but intends to review in the next 3 months.
Action—Has been reviewing options for 1 year or less.
Maintenance—Has been reviewing options for more than 1 year.
Similar decision rules have been used in TTM staging algorithms for a wide range of behaviors, from smoking cessation to seatbelt use (Nigg et al., 1999). However, in most algorithms, contemplation and preparation are defined by intention to make a change in the next 6 months and in the next 30 days, respectively, rather than the 12 months and 3 months used here; maintenance is generally defined by engagement in the new behavior for at least 6 months, not the 12 months used here. We reasoned that the 12-month time-frame was more appropriate for informed choice, given the annual publication of the Medicare & You handbook, annual enrollment period in November, and the potential lock-in provision.
Stage Distributions
Learning About the Medicare Program
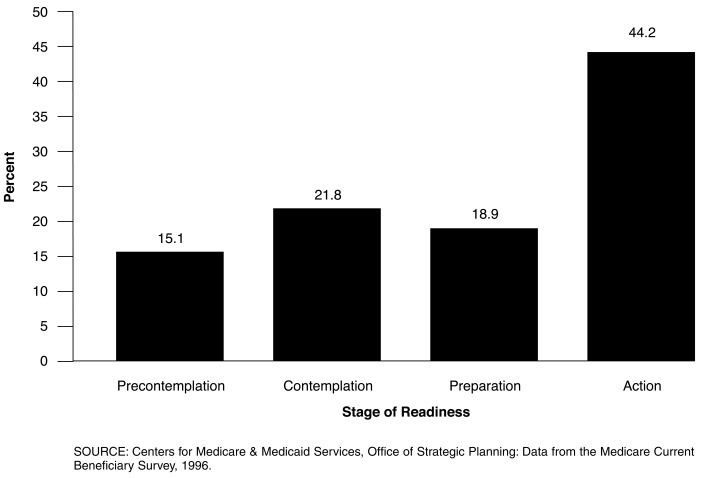
The 12,621 beneficiaries who completed the Round 18 staging algorithm questions were classified into stages. Figure 2 illustrates the percentage of Medicare beneficiaries in each of the stages of change for learning about the Medicare program. Among surveyed beneficiaries, 15.1 percent were in the precontemplation stage, 21.8 percent in contemplation, 18.9 percent in preparation, and 44.2 percent in action, indicating that a majority of beneficiaries considered themselves to be knowledgeable about the Medicare program or were prepared to become more informed. There were no differences in the stage distributions for beneficiaries who completed the measures on their own or through a designated proxy respondent.
Figure 2. Medicare Beneficiaries' Stage of Readiness to Learn About the Medicare Program: 1997.
Learning About Medicare HMOs
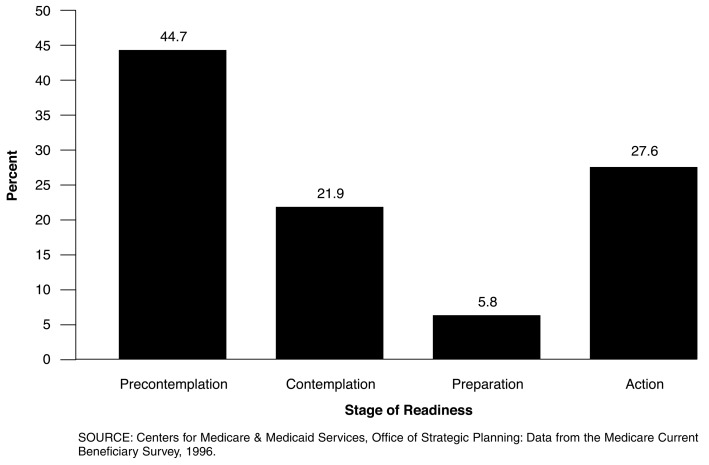
As illustrated in Figure 3, beneficiaries, as a group, were far less ready to learn about the availability and benefits of Medicare HMOs. Based on the second algorithm, 44.7 percent of the 12,480 beneficiaries who completed the staging questions were classified in the precontemplation stage. These beneficiaries, who have no intention of seeking additional information about Medicare HMOs, are unlikely to benefit from traditional action-oriented educational materials. In addition, 21.9 percent were classified in the contemplation stage for learning about Medicare HMOs, 5.8 percent in the preparation stage, and 27.6 percent in the action stage. Stage distributions were the same for beneficiaries who completed the measures on their own or through a designated proxy respondent.
Figure 3. Medicare Beneficiaries' Stage of Readiness to Learn About Medicare Health Maintenance Organizations: 1997.
Reviewing Health Plan Options
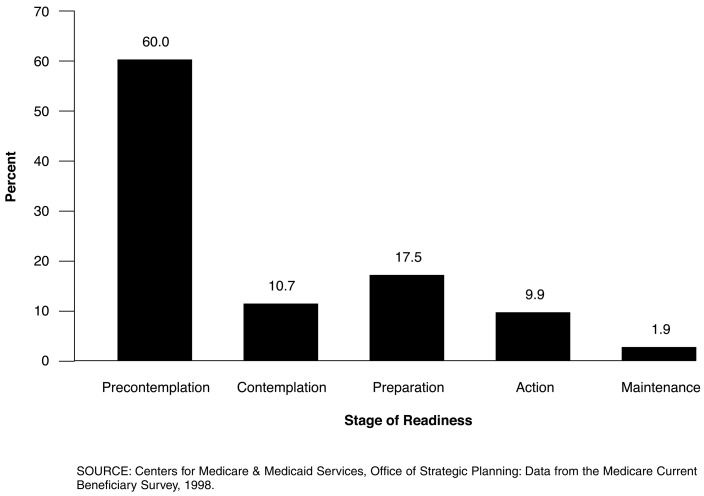
As illustrated in Figure 4, beneficiaries were even less ready to review their health plan options. Among the 12,862 beneficiaries who answered the new staging questions included in the MCBS 1998 Access and Use file Round 23 Supplement, 60.0 percent were in the precontemplation stage for review. There were 10.7 percent classified in the contemplation stage, 17.5 percent in the preparation stage, 9.9 percent in the action stage, and 1.9 percent in the maintenance stage. Once again, stage distributions were the same for beneficiaries who completed the measures on their own or through a designated proxy respondent.
Figure 4. Medicare Beneficiaries' Stage of Readiness to Review Different Health Plan Options: 1999.
Construct Validity of The Staging Algorithms
To assess the construct validity of the three staging algorithms, we determined whether stage of change for informed choice was related to knowledge about the Medicare program and information seeking.
Knowledge
It was hypothesized that beneficiaries in the later stages of change for informed choice would have greater knowledge of the Medicare program than beneficiaries in the earlier stages. To test this hypothesis, we used the following five measures of Medicare knowledge constructed from MCBS items for CMS by the Center for Health Systems Research and Analysis and the Research Triangle (Bann et al., 2000):
Medicare Understandability Question—This single-item measure, drawn from the Round 20 MCBS, asks, “In general, do you think the Medicare program is understandable?” Response options are 0=No and 1=Yes.
Global Know-All-Need-to-Know Question—This single-item measure, drawn from the Round 23 MCBS, asks, “How much do you think you know about the Medicare program?” Response options range from 1=Almost none of what you need to know, to 5=Just about everything you need to know.
Three-Item Quiz—This measure, drawn from the Round 24 MCBS, is composed of three true/false questions about the Medicare program (e.g., “Medicare covers an annual flu shot”). The scale score, which ranges from 0 to 3, is calculated by summing the number of correct responses. The scale has low internal reliability, with a Cronbach's alpha of 0.46.
Four-Item Quiz—This measure is composed of four true/false questions drawn from the Round 18 MCBS. The scale score is calculated by summing the number of correct responses. Cronbach's alpha is 0.52.
Eight-Item Quiz—This measure, drawn from the Round 23 MCBS, is composed of eight true/false questions about Medicare HMOs (e.g., “If someone joins a Medicare HMO that covers people on Medicare, they can change or drop the plan and still be covered by Medicare”). The scale score is calculated by summing the number of correct responses. Cronbach's alpha is 0.76.
A sixth MCBS knowledge measure, the Know-All-Need-to-Know Index from the Round 18 MCBS, is comprised of several of the same items used in the staging algorithms and thus cannot be considered an independent measure of knowledge. Refer to Bann et al. (2000) for a detailed description of the development and validation of these six knowledge measures.
Learning About the Medicare Program
Because it is unclear whether proxy respondents can accurately answer knowledge questions on behalf of beneficiaries, cases relying on proxies were excluded from the following analyses.
A multivariate analysis of variance (MANOVA) was conducted in which the independent variable was stage of change based on the staging algorithm assessing readiness to learn about the Medicare program; the dependent variables were the five knowledge measures already listed. The results of the MANOVA, followup univariate tests, and post-hoc tests, summarized in Table 1, show that beneficiaries in different stages of change differed significantly on all five knowledge measures. In general, beneficiaries in the later stages of change had significantly higher knowledge scores than beneficiaries in the middle stages, who in turn had higher knowledge scores than beneficiaries in the earlier stages. Effect sizes ranged from η2 = 0.046 to η2 = 0.125. The strongest relationship was found between stage of change and the Global Know-All-Need-to-Know question, perhaps because of the similarity in wording of the questions used in the two measures. However, the staging algorithm was created from questions from the Round 18 MCBS and the global-knowledge measure from a question from the Round 23 MCBS.
Table 1. Knowledge Scores Among Beneficiaries in Different Stages of Readiness to Learn About the Medicare Program.
| Univariate Followup Tests | Stage of Readiness | F (3,5628) | Effect Size1 | Post-Hoc Comparisons | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Precontemplation (PC) (n = 844) |
Contemplation (C) (n = 1,278) |
Preparation (PR) (n = 1,095) |
Action (A) (n = 2,415) |
||||||||
|
|
|
|
|
||||||||
| Mean | Standard Deviation | Mean | Standard Deviation | Mean | Standard Deviation | Mean | Standard Deviation | ||||
| Medicare Understandability Question | 0.64 | 0.48 | 0.68 | 0.47 | 0.78 | 0.41 | 0.86 | 0.35 | *89.96 | 0.046 | PC<C<PR<A |
| Global Know-All-Need-to-Know Question | 2.60 | 1.18 | 2.48 | 1.13 | 3.10 | 1.03 | 3.45 | 1.11 | *264.97 | 0.124 | C<PC<PR<A |
| 3-Item Quiz | 1.52 | 0.94 | 1.54 | 0.92 | 1.84 | 0.91 | 2.01 | 0.89 | *103.91 | 0.052 | PC,C<PR<A |
| 4-Item Quiz | 2.04 | 1.27 | 2.17 | 1.18 | 2.61 | 1.02 | 2.78 | 1.00 | *145.38 | 0.072 | PC<C<PR<A |
| 8-Item Quiz | 3.55 | 2.53 | 4.06 | 2.37 | 4.79 | 2.13 | 5.11 | 2.17 | *127.42 | 0.064 | PC<C<PR<A |
p < 0.01.
To assess whether significant findings can be attributed to effect size, and not just large sample size, a measure of effect size, η2, is provided. A small effect is defined as η2 = 0.01, medium effect as η2 = 0.06, and a large effect as η2 = 0.14 (Cohen, 1988).
NOTES: Wilks' Λ = 0.805, approximate F(15,15526) = 84.36, p < 0.001, η2 = 0.070.
SOURCE: Centers for Medicare & Medicaid Services, Office of Strategic Planning: Data from the Medicare Current Beneficiary Survey, 1996-1998.
Learning About Medicare HMOs
A second MANOVA was conducted to assess the relationship between stage of change based on the Medicare HMO algorithm and the five knowledge measures. Once again, results (which are not displayed here; for a full report, refer to Levesque et al., 2000) show that beneficiaries in the various stages of change differed significantly on all five knowledge measures. Beneficiaries in the later stages of change tended to have significantly higher knowledge scores than beneficiaries in the middle stages, who in turn had higher scores than beneficiaries in the earlier stages. Effect sizes ranged from η2 = 0.014 to η2 = 0.052. As further evidence of the validity of this measure, stage of change for learning about Medicare HMOs was most strongly related to the eight-item knowledge measure assessing knowledge about HMOs.
Reviewing Health Plan Options
A final MANOVA was conducted to assess the relationship between stage of change based on the Review algorithm specifically developed for and administered in the Round 23 MCBS and the three knowledge measures administered during or after Round 23. Individuals in the Action and Maintenance stages were combined into a single group for analyses. Once again, beneficiaries in the later stages had significantly greater knowledge than beneficiaries in the earlier stages. Effect sizes ranged from η2 = 0.016 to η2 = 0.068. Stage of change for reviewing options was most strongly associated with the 8-item knowledge measure focusing on Medicare HMOs.
Relative Contribution of Stage
Extensive research on smoking cessation has shown that stage of change is a better predictor of future behavior than demographic variables (Prochaska et al., 1985). Such findings have important implications for intervention: First, unlike many demographic variables such as race and gender, stage of change is not static, but dynamic and modifiable. Second, stage-matched interventions that facilitate progression through the stages can increase the likelihood of successful behavior change.
In the present study, multiple regression analyses were conducted to determine if stage of change is a better predictor of beneficiary knowledge than 13 demographic, health-status, and health plan variables. An additional variable, years of participation in the survey, was also included as a predictor to account for any increase in knowledge that might be attributable to experience with the MCBS. Knowledge measures were the five MCBS knowledge scales used in the validity analyses already discussed.
Separate multiple regression analyses were conducted in which the independent variables were the predictor variables, and the dependent variables were the five knowledge measures. Aged and disabled beneficiaries were analyzed separately, given possible differences in their information needs. Cases relying on proxy respondents in the MCBS were excluded from analyses because it is unclear whether proxies can accurately answer knowledge questions on behalf of beneficiaries. Data on the predictor variables were taken from the Round 19 MCBS.
Stage of change for learning about the Medicare program was a better predictor of knowledge about the Medicare program than all demographic, health-status, and health plan variables examined, even education. Stage of change for learning about Medicare HMOs and for reviewing different health plan options were the best predictors of knowledge about Medicare HMOs (for a full report, refer to Levesque et al., 2000).
Information Seeking
To assess the construct validity of the staging algorithms, an additional set of analyses was conducted to examine the relationship between stage of change for informed choice and information-seeking behavior. Compared with individuals in the earlier stages of change, it was hypothesized that individuals in the later stages would be more likely to seek and utilize information about the Medicare program and their health plan options.
Learning About the Medicare Program
Chi-square tests were conducted to assess the relationship between stage of change for learning about the Medicare program and seven self-report measures of information-seeking taken from Rounds 18 and 20 of the MCBS (e.g., ever used Medicare & You handbook; if needed, found information on changes in benefits; was very satisfied with information on the Medicare program).
Results, summarized in Table 2, show significant relationships between stage of change and all indicators of information seeking. Effect sizes ranged from Cohen's h=0.26 to Cohen's h=0.55. Individuals who reported using the handbook and/or being very satisfied with their efforts or available materials were more likely to be in the action stage than individuals who did not seek information or who were less satisfied.
Table 2. Information Seeking and Stage of Change for Learning about the Medicare Program.
| Information-Seeking Activity | Stage of Change | Chi-squared1 | Cohen's h‡ | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | Precontemplation | Contemplation | Preparation | Action | |||
|
| |||||||
| Percent | |||||||
| Ever Used Handbook | |||||||
| Yes | 6,506 | 9.6 | 15.5 | 20.4 | 54.4 | *841.67 | 0.43 |
| No | 5,999 | 20.8 | 28.7 | 17.2 | 33.3 | ||
| Found Handbook Very Useful | |||||||
| Yes | 2,570 | 6.6 | 12.1 | 18.4 | 63.0 | *542.91 | 0.48 |
| No | 9,544 | 17.1 | 24.2 | 19.2 | 39.4 | ||
| Received Handbook in Last Year | |||||||
| Yes | 5,757 | 11.3 | 18.2 | 19.2 | 51.3 | *248.00 | 0.26 |
| No | 5,849 | 17.7 | 24.9 | 18.7 | 38.6 | ||
| If Needed, Found Information on Changes in Benefits | |||||||
| Yes | 487 | 8.0 | 20.1 | 27.3 | 44.6 | *33.17 | 0.45 |
| No | 89 | 12.4 | 46.1 | 18.0 | 23.6 | ||
| If Needed, Found Information on Services Covered | |||||||
| Yes | 606 | 7.3 | 23.9 | 24.1 | 44.7 | *29.69 | 0.54 |
| No | 127 | 9.4 | 40.9 | 29.9 | 19.7 | ||
| If Needed, Found Information on Availability and Benefits of HMOs | |||||||
| Yes | 626 | 10.9 | 21.1 | 19.2 | 48.9 | *13.27 | 0.55 |
| No | 52 | 13.5 | 32.7 | 30.8 | 23.1 | ||
| Very Satisfied with Availability of Information on Medicare | |||||||
| Yes | 1,331 | 9.0 | 12.9 | 17.9 | 60.2 | *166.97 | 0.35 |
| No | 11,134 | 15.5 | 22.7 | 19.0 | 42.7 | ||
p < 0.01.
To assess whether significant findings can be attributed to effect size, and not just large sample size, a measure of effect size, Cohen's h based on the arcsine transformation of proportions, is provided. Measures represent the magnitude of the difference in percentages for action versus pre-action (Precontemplation, Contemplation, and Preparation combined). A small effect is defined as h = 0.20, medium effect as h = 0.50, and a large effect as h = 0.80 (Cohen, 1988).
Degrees of freedom = 3.
SOURCE: Centers for Medicare & Medicaid Services, Office of Strategic Planning: Data from the Medicare Current Beneficiary Survey, 1996.
Learning About Medicare HMOs
Chi-square tests revealed statistically significant relationships between stage of change for learning about the availability and benefits of Medicare HMOs and the same seven measures of information seeking, with one exception: there were no differences among the stages in ability to find needed information on changes in benefits. Effect sizes for statistically significant effects ranged from h=0.10 to h=0.49. For detailed results, refer to Levesque et al. (2000).
Reviewing Health Plan Options
Chi-square tests were conducted to assess the relationship between stage of change for reviewing different health plan options and 10 measures of information-seeking drawn from the Round 23 MCBS (e.g., read Medicare & You handbook thoroughly; used a health plan comparison chart; and was very satisfied with availability of information). Stage of change was significantly related to all measures of information-seeking examined. Effect sizes ranged from h=0.22 to h=0.78. Individuals who had read their handbook thoroughly or had used it to look up a telephone number or to learn about different options or compare plans, were more than three times as likely to be in the action/maintenance stage as those who had not read the handbook thoroughly or used it as a resource. Once again, individuals who were very satisfied with the availability of information about the Medicare program were more likely to be in the action/maintenance stage. For detailed results, refer to Levesque et al. (2000).
Summary and Future Directions
In the initial step in the application of TTM to facilitate informed choice in the Medicare population, staging algorithms were developed to assess readiness to engage in three types of informed choice: (1) learning about the Medicare program; (2) learning about Medicare HMOs; and (3) reviewing different health plan options. The first two algorithms were constructed from existing items from the Round 18 MCBS; the third algorithm was constructed from questions developed specifically for this study and included in the Round 23 MCBS. As a group, beneficiaries were most prepared to learn about the Medicare program (44.2 percent of respondents in the action stage [Figure 2]) and least prepared to review different health plan options (11.8 percent in action or maintenance [Figure 4]).
Analyses examining construct validity found that stage of change based on all three algorithms was related to knowledge about the Medicare program and information seeking. Compared with beneficiaries in the earlier stages of change, beneficiaries in the later stages scored significantly higher on five measures of Medicare knowledge and were more likely to seek out or find information on new benefits, services covered, and HMOs. They were more likely to report receiving and using their Medicare & You handbook and to be satisfied with information available on the Medicare program. Stage of change for learning about the Medicare program was a better predictor of knowledge about the Medicare program than all demographic, health-status, and health plan variables examined. Stage of change for learning about Medicare HMOs and for reviewing different health plan options were the best predictors of knowledge about Medicare HMOs.
One of the most difficult problems in measure-development research is identifying satisfactory measures to assess construct validity. Such measures must be related to the construct being measured, be free of bias, and have high face validity. We are fortunate that the MCBS included direct measures of knowledge and information seeking that allowed us to validate the new staging algorithms. Elsewhere, we have reported the results of additional analyses examining the relationship between the algorithms and a range of other MCBS variables expected to vary systematically with stage of change, including demographics, health and cognitive functioning, health care utilization, and health insurance characteristics (refer to Levesque et al., 2000, for the full report). As hypothesized, stage of change was related to race, age, marital status, income, health status, and most other variables expected to vary with stage.
Results provide evidence for the construct validity of the stage-of-change measures, and an impetus for continued work in this area. There are four steps in the future application of the TTM to facilitate informed choice in the Medicare population:
Development of a definition of “informed choice.”
Customization of TTM measures.
Model testing.
Development and testing of TTM-based interventions.
In a separate CMS project, work is underway in Phase I to develop and refine gold-standard measures of stage of change and other dimensions of the TTM (refer to Levesque, Cummins, and Prochaska, 2000, for a description of the procedures followed—and the challenges encountered—in the development of a definition of informed choice and the customization of TTM measures).
In Phase II of the project, the goal is to develop prototypes of TTM-based interventions that might be administered to beneficiaries to accelerate progress through the stages of change for informed choice. A Technical Expert Panel was convened to identify segments of the Medicare population that could benefit most from stage-matched interventions (e.g., beneficiaries with skill deficits, vulnerable populations, new enrollees, individuals living in market “hot spots”), and the best intervention channels for reaching different segments (e.g., the Medicare & You handbook, mass media, SHIP counselors, the initial enrollment package for new enrollees). Based on the recommendations of the panel and available resources, we are developing TTM-based interventions for new enrollees. The intervention materials include counselor protocols, a stage-matched manual, and a multimedia expert system program that delivers an assessment and individualized feedback. Possible channels for dissemination include SHIP counselors, the initial enrollment package for new enrollees and the 1-800-Medicare helpline.
In Phase III, the final phase of the project, a randomized clinical trial may be conducted to assess the efficacy of the stage-matched interventions. Outcome measures would include knowledge, information-seeking, and satisfaction with health plan choice.
Footnotes
Deborah Levesque, James Prochaska, and Carol Cummins are with Pro-Change Behavior Systems. Sherry Terrell and David Miranda are with the Centers for Medicare & Medicaid Services (CMS). Research for this article was performed under CMS Cooperative Agreement Number 17-C-90950/1 and CMS Contract Number 500-97-0040, Subcontract Number 20036-3.1. The views expressed in this article are those of the authors and do not necessarily reflect the views of Pro-Change Behavior Systems or CMS.
Reprint Requests: Deborah A. Levesque, Ph.D., Pro-Change Behavior Systems, Inc., P.O. Box 755, W. Kingston, RI 02892. E-mail: levesque@etal.uri.edu
References
- Bann C, Lissy KS, Keller S, et al. Analysis of Medicare Beneficiary Baseline Knowledge Data from the Medicare Current Beneficiary Survey. Center for Health Systems Research and Analysis and Research Triangle Institute; Madison, WI.: 2000. Centers for Medicare & Medicaid Services Knowledge Technical Note, Contract Number 500-95-0061/004. [Google Scholar]
- Campbell MK, DeVellis BM, Strecher VJ, et al. Improving Dietary Behavior: The Effectiveness of Tailored Messages in Primary Care Settings. American Journal of Public Health. 1994;84(5):783–787. doi: 10.2105/ajph.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Second Edition. Erlbaum; Hillsdale, NJ.: 1988. [Google Scholar]
- DiClemente CC, Prochaska JO. Self-Change and Therapy Change of Smoking Behavior: A Comparison of Processes of Change in Cessation and Maintenance. Addictive Behaviors. 1982;7(2):133–142. doi: 10.1016/0306-4603(82)90038-7. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, et al. The Process of Smoking Cessation: An Analysis of Precontemplation, Contemplation, and Preparation Stages of Change. Journal of Consulting and Clinical Psychology. 1991;59(2):295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Greene GW, Rossi SR, Rossi JS, et al. Dietary Applications of the Stages of Change Model. Journal of the American Dietetic Association. 1999;99(6):673–678. doi: 10.1016/S0002-8223(99)00164-9. [DOI] [PubMed] [Google Scholar]
- Laforge RG, Velicer WF, Richmond RL, Owen N. Stage Distributions for Five Health Behaviors in the United States and Australia. Preventive Medicine. 1999;28(1):61–74. doi: 10.1006/pmed.1998.0384. [DOI] [PubMed] [Google Scholar]
- Levesque DA, Cummins CO, Prochaska JO. Application of the Transtheoretical Model to Informed Choice in the Medicare Population. Pro-Change Behavior Systems; Kingston, RI.: 2000. Centers for Medicare & Medicaid Services Qualitative Report, Contract Number 500-97-0040, Subcontract Number 20036-3.1. [Google Scholar]
- Levesque DA, Prochaska JO, Cummins CO, Evans JL. Assessing Readiness of Medicare Beneficiaries to Participate in Informed Health Care Choices. Pro-Change Behavior Systems; Kingston, RI.: 2000. Centers for Medicare & Medicaid Services Final Report, Contract Number 17-C-90950/1-01. [Google Scholar]
- Levesque DA, Prochaska JM, Prochaska JO. Stages of Change and Integrated Service Delivery. Consulting Psychology Journal: Practice and Research. 1999;51(4):226–241. [Google Scholar]
- Marcus BH, Rossi JS, Selby VC, et al. The Stages and Processes of Exercise Adoption and Maintenance in a Worksite Sample. Health Psychology. 1992;11(6):386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Bock BC, Pinto BM, et al. Efficacy of an Individualized, Motivationally Tailored Physical Activity Intervention. Annals of Behavioral Medicine. 1998;20(3):174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- Nigg CR, Burbank PM, Padula C, et al. Stages of Change Across Ten Health Risk Behaviors for Older Adults. The Gerontologist. 1999;39(4):473–482. doi: 10.1093/geront/39.4.473. [DOI] [PubMed] [Google Scholar]
- Prochaska JO. Systems of Psychotherapy: A Transtheoretical Analysis. Brooks/Cole; Pacific Grove, CA.: 1984. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and Processes of Self-Change of Smoking: Toward an Integrative Model of Change. Journal of Consulting and Clinical Psychology. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy. Dow Jones-Irwin; Homewood, IL.: 1984. [Google Scholar]
- Prochaska JO, DiClemente CC. Common Processes of Change in Smoking, Weight Control, and Psychological Distress. In: Shiffman S, Wills T, editors. Coping and Substance Use: A Conceptual Framework. Academic Press; New York: 1985. [Google Scholar]
- Prochaska JO, DiClemente CC. Toward a Comprehensive Model of Behavior Change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of Change. Plenum Press; New York: 1986. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In Search of How People Change: Applications to Addictive Behaviors. American Psychologist. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Velicer WF, et al. Predicting Change in Smoking Status for Self-Changers. Addictive Behavior. 1985;10(4):395–406. doi: 10.1016/0306-4603(85)90036-x. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, Individualized, Interactive, and Personalized Self-Help Programs for Smoking Cessation. Health Psychology. 1993;12(5):399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, et al. Stages of Change and Decisional Balance for Twelve Problem Behaviors. Health Psychology. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Ehrich B, Dube CE, et al. Screening Mammography and Constructs from the Transtheoretical Model: Associations Using Two Definitions of the Stages-of-Adoption. Society of Behavioral Medicine. 1996;18(2):91–100. doi: 10.1007/BF02909581. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Ehrich B, Goldstein MG, et al. Increasing Mammography Among Women Aged 40-74 by Use of a Stage-Matched, Tailored Intervention. Preventive Medicine. 1998;27(5):748–756. doi: 10.1006/pmed.1998.0354. [DOI] [PubMed] [Google Scholar]
- Robbins ML, Levesque DA, Redding CA, et al. Assessing Family Members' Motivational Readiness and Decision Making for Consenting to Cadaveric Organ Donation. Journal of Health Psychology. 2001;6(5):523–535. doi: 10.1177/135910530100600506. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, Kreuter M, Den Boer DD, et al. The Effects of Computer-Tailored Smoking Cessation Messages in Family Practice Settings. Journal of Family Practice. 1994;39:262–270. [PubMed] [Google Scholar]
- Velicer WF, Fava JL, Prochaska JO, et al. Distribution of Smokers by Stage in Three Representative Samples. Preventive Medicine. 1995;24(4):401–411. doi: 10.1006/pmed.1995.1065. [DOI] [PubMed] [Google Scholar]