Abstract
Despite being a vulnerable and costly population, little is known about disabled Medicaid beneficiaries. Using data from a 1999-2000 survey, we describe the population and their health care experiences in terms of access, use, and satisfaction with care. Results indicate that disabled beneficiaries are a unique population with wide-ranging circumstances and health conditions. Our results on access to care were indeterminate: by some measures, they had good access, but by others they did not. Beneficiaries' assessments of their health care were more clear: The bulk of the sample rated one or more area of care as being fair or poor.
Introduction
Medicaid provides health care coverage to more than 40 million people (Bruen and Holahan, 2001). In providing this coverage, the program serves a highly diverse population that includes low-income females and children, the elderly, and disabled. Each of these groups has distinct health care needs with their use of health care services reflecting these underlying health care needs: adults and children in low-income families rely on Medicaid largely for ambulatory and preventative care whereas disabled persons rely on Medicaid for ambulatory care as well as acute and long-term care services.
While considerable research has been done on health care access, use and satisfaction among low-income families and elderly Medicaid beneficiaries (Stein, 1997; Sisk et al., 1996; Rosenbach, 1995; Gold et al., 1997), less work has been completed on the non-elderly disabled Medicaid beneficiary (Davis and O'Brien, 1996; Hagglund et al., 1999; Meyer and Zeller, 1999; Hill and Wooldridge, 2000; Allen and Croke, 2000). The purpose of this article is to add to the limited baseline knowledge on working-age disabled Medicaid beneficiaries by providing descriptive information on the popula-tion—who they are, what types of services they use, and their satisfaction with the health care they receive under Medicaid.
Having such information on the disabled Medicaid population is important. The disabled Medicaid population is a vulnerable group, having very complex medical and health conditions. Developmental disabilities, serious mental illness, and acquired immunodeficiency syndrome (AIDS) are some of the conditions among the disabled Medicaid population. Given their typically low health and functional status, persons with disabilities are heavy users of health care and thus are costly to serve: While disabled Medicaid beneficiaries constitute only 17 percent of the Medicaid caseload, they accounted for approximately 43 percent of program spending in 1998 (Bruen and Holahan, 2001). Moreover, the disabled, with an average annual growth rate of 7.1 percent, was the fastest growing subgroup in the Medicaid population between 1990 and 1998 (Bruen and Holahan, 2001).
Having a clear understanding of the non-elderly disabled Medicaid beneficiaries has become especially important recently as many States have moved (or are considering moving) the disabled into managed care (Allen and Croke, 2000). Most States have limited experience in designing managed care programs that meet the specialized needs of persons with disabilities (U.S. General Accounting Office, 1996; Center for Health Care Strategies, 2000). Structuring high quality managed care programs for the disabled Medicaid population and—after the programs have been implement-ed—determining program impacts on beneficiaries, requires information on how the population is currently faring under the Medicaid fee-for-service (FFS) system. Further, having some knowledge about the population would be most helpful to States in setting appropriate capitation rates.
In a step toward filling this information gap, we present findings from a 1999-2000 survey of working-age disabled Medicaid beneficiaries living in two areas in New York State—New York City (NYC) and Westchester County (WC). The survey collected information on a range of topics including socioeconomic circumstances, health status and disability, as well as information on health care access, use, and satisfaction. The survey was conducted in the period proceeding New York's planned switch to mandatory Medicaid managed care for disabled beneficiaries and was designed to provide baseline information for future work which will assess how managed care affects care for disabled Medicaid recipients.
Analytical Approach
This article relies on a traditional analytic framework to examine health care access, use, and satisfaction within the working-age disabled Medicaid population (Andersen, 1968, 1995; Andersen and Aday, 1978; Andersen and Newman 1973). Using this framework, we define two broad categories of access to care: potential and realized access (that is, service use). Potential access measures characteristics that might affect the demand for and supply of health care services. In this analysis we focus on the presence of a usual source of care, continuity of care, and convenience of care. Realized access reflects the outcomes of a person's experience with the health care system. Here, we examine several measures of realized access—service use, satisfaction with care, and the extent of and reasons for unmet need.
Our analysis builds on Andersen's Behavioral Model (1968) which describes health care service use as a function of the predisposition of a individual to use services, factors that enable or impede use, and an individual's need for services. Predisposing factors include demographic and social characteristics such as age, sex, education, and race. Enabling characteristics reflect both family and personal resources (for example, income and social support) as well as availability of health care services. Lastly, a person's need for services is measured by their type of disability, level of functional impairment measured by activities of daily living (ADLs), instrumental activities of daily living (IADLs), and their perceived overall health status.
Beyond these measures we also consider whether the survey response was obtained from a proxy respondent for the sample member. This was done to control for the possibility that responses from a proxy may have differed from those that would have been reported by the sample member.
Data and Methods
Data Source
This analysis is based on data obtained from the New York Survey of Working-Age Disabled Medicaid Beneficiaries, which was conducted by Mathematica Policy Research, Inc. in New York City in 1999-2000 and in Westchester County in 1999. The two sites for the survey were independently selected because of plans by the State to implement mandatory Medicaid managed care for the disabled in those areas in the near future.1 For the most part, we view NYC and WC as two data points and thus present, for the most part, the survey data separately for the two areas. The survey provided the baseline for evaluation of the impacts of the shift to managed care on disabled enrollees.2 Survey information on access to, use of, and satisfaction with care, along with socioeconomic, health status, and disability information was collected.
We acknowledge that survey data obtained from two sites are not generaliz-able to all of New York or to the Nation. The survey was intended to provide important information about how working-age disabled Medicaid beneficiaries are faring in two distinct geographic settings—one urban and one suburban. We also acknowledge that New York, with its longstanding tradition of funding one of the Nation's most comprehensive Medicaid Programs, is not representative of many other States' programs. However, the survey data should detail disabled beneficiaries' health care experiences when enrolled in a comprehensive, well-funded Medicaid Program.
Sample
The sample members for the survey were identified through New York State Medicaid enrollment records of its SSI disabled beneficiaries who were active in the Medicaid Program as of July 1998. Information on the primary disabling condition under SSI was obtained through a match with Social Security Administration (SSA) records for the SSI Program. (For individuals with multiple disabling conditions, the primary disabling condition represents the disabling condition that most readily qualified the individual for the SSI Program.3) The sample excluded SSI beneficiaries age 65 or over and those under age 18. It also excluded SSI beneficiaries who were eligible for Medicare, those residing in institutions, and those receiving long-term care services in the community. In order to obtain estimates for key subgroups of the adult disabled population in each of the two survey areas, SSA data were used to stratify the sample by four groups: physically disabled adults, adults with mental illness, mentally retarded/ developmentally disabled (MR/DD) adults, and adults for whom the disabling condition was unknown.4 Random samples of disabled adults were selected within each strata. Variations in the distribution of the population across the subgroups between the two survey areas reflects underlying population differences.
Before conducting the interviews, letters (written in English and Spanish) were mailed to potential respondents describing the survey and seeking their participation. Mathematica Policy Research, Inc., conducted the interviews by telephone using computer-assisted telephone interviewing (CATI).5 Interviews were conducted by telephone in English and Spanish.6 Telephones with amplifiers and TTY services were used for respondents with hearing limitations.
As shown in Table 1, the overall response rate for the survey was 56 percent in NYC and 59 percent in WC. The single biggest reason for non-response was that a telephone number was not available. In NYC, 33 percent of the sample did not have valid telephone numbers; in WC, it was 34 percent. However, once a sample person was located, the cooperation rate was very high: 94 percent in NYC and 92 percent in WC. Most of the surveys were conducted in English—91percent in NYC and 96 percent in WC.
Table 1. Selected Sample Statistics from the New York Survey of Working-Age Disabled Medicaid Beneficiaries: 1999-2000.
| Response | Beneficiaries | |
|---|---|---|
|
| ||
| New York City | Westchester County | |
| Sample Size | 840 | 957 |
| Final Distribution of Cases | Percent | |
| Response Rate | 56.0 | 59.0 |
| Non-locatable Rate | 33.0 | 34.0 |
| Cooperation Rate | 94.0 | 92.0 |
| Conducted In | ||
| English | 91.0 | 96.0 |
| Spanish1 or Other Language | 7.0 | 4.0 |
| Self-Response Rate | ||
| Total | 82.3 | 77.8 |
| Physically Disabled | 86.6 | 86.8 |
| Mentally Ill | 85.1 | 87.2 |
| Mentally Retarded/Developmentally Disabled | 63.3 | 38.4 |
| Reason for Proxy Use | ||
| Mentally Incapable | 46.5 | 68.3 |
| Language Issue | 39.6 | 14.3 |
| Sample Person Ill | 5.1 | 3.4 |
| Hearing Problem | 4.6 | 2.4 |
| Other | 4.1 | 9.0 |
In New York City, interviews were conducted in languages other than English or Spanish for approximately 1.5 percent of the sample and in Westchester County 0.2 percent.
NOTE: Survey responses provided the baseline information needed to evaluate the impacts of the shift to managed care on disabled enrollees.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
Our response rates are comparable to those achieved in other social science surveys (Massey et al., 1997). In a recent review of social science surveys, for example, Massey and colleagues found that the median response rate across the studies was between 60 and 64 percent. Our response rates are also in keeping with other recent health surveys of disabled Medicaid enrollees (e.g., a 65-percent response rate among SSI enrollees in Tennessee [Hill and Woolridge, 2000]), other recent surveys of the overall Medicaid population (e.g., a 52-percent response rate among welfare recipients in NYC [Sisk et al.,1996]), and recent surveys of the population in general (e.g., a 62-percent response rate for a national survey of families [Kenney, Scheuren, and Wang, 1999]).
As previously mentioned, interviewing was done by telephone (as opposed to in-person), one of the first telephone surveys of people with disabilities (Cybulski and Ciemnecki, 2000). To accommodate the special needs of the population, several special features were incorporated into both the design and fielding of the survey, including eliminating soft consonant sounds to overcome high-frequency sounds that are sometimes difficult to hear over the telephone, internal consistency checks for unexpected response, and building in breaks for respondents. (Cybulski and Ciemnecki, 2000).
A principal goal of the survey was to minimize proxy response. The overall self-response rate was 82.3 percent in NYC and 77.8 percent in WC (Table 1). The ability to self-respond varied by subgroup: In both locations, approximately 86 percent of those with physical and mental disabilities were able to self-respond. Self-response was lower among individuals with MR/ DD—63 percent in NYC and 38 percent in WC. The most common reason for relying on a proxy was to overcome cognitive challenges. Proxies were also used to address language issues and when the sample person was too ill to respond. Although not shown in the table, the reason for proxy use varied by the disabling condition of the sample person: Sample members with physical disabilities were more likely to rely on proxies because of illness or hearing problems, whereas those with mental retardation or mental illness relied on proxies because of cognitive impairment. However, after controlling for a range of personal, health, and situational factors, whether a sample person relied on proxy respondent had no significant effect on key outcome variables.
Followup in-person and family member interviewing, reliability, and validity testing of persons with mental illness and mental retardation who self-responded has been conducted with other samples using the same survey instrument used in our study (Ciemnecki et al., 2000). Overall, these fol-lowup interviews revealed that the information collected by telephone from persons with mental illness and those with mental retardation was both consistent and reliable.
Sample weights were developed to compensate for the different probabilities of selection for each individual to reduce biases occurring because non-respondents have different characteristics than respondents. The adjustments for non-response were based on the administrative data available for both respondents and non-respondents, which included basic demographic information along with primary disabling condition and geographic location. The analyses reported here have been weighted using these sample weights. Missing data were a relatively minor problem for the explanatory variables included in our regression analysis: less than 3 percent of the individuals had missing values. We used hot-deck imputation procedures to assign values for observations with missing data for the explanatory variables (Ford, 1980).
Our measures of potential access were whether the person had a usual source of care and convenience of getting care. For realized access we use both subjective and actual measures. Subjective measures asked respondents about their extent of unmet need for various services such as medical care or surgery, mental health care, and dental care. In our analysis we also included measures of actual service use including outpatient care, emergency room (ER) and inpatient hospital care, and preventative care. Finally, in assessing satisfaction with care, we asked respondents to rate various aspects of their health care as excellent, very good, good, fair, or poor. We consider five areas: overall quality of care, ease of finding a doctor who will accept Medicaid, ease of getting specialist care, ease of getting mental health care, and ease of getting ER care.
For the descriptive analysis we looked at a range of access, use, and satisfaction variables. For the multivariate analysis we looked at selected measures within each of these three categories. Specifically, we examined whether a person had: a usual source of care, a hospital stay or an ER visit in the last 12 months, a doctor visit in the last 3 months, reported an unmet need for medical care or surgery, rated overall quality of care as fair or poor, and rated the ease of finding a doctor who accepts Medicaid as fair or poor.
Independent Variables
In this section we describe the independent variables, grouped in the three domains set out in the behavioral model.7 Predisposing factors include age, sex, race and ethnicity, first spoken language, education level, and living arrangement. For the descriptive analysis we show both the mean age as well as three age categories—18-30 years, 31-45 years, and 46-64 years, whereas in the multivariate analysis we use a continuous age variable. We classified race and ethnicity into four groups—Hispanic; white, non-Hispanic; black, non-Hispanic; and other non-Hispanic. Educational level is grouped into three categories—less than high school or ungraded, high school graduate, and some college or college graduate. Language is also grouped into three categories—English, Spanish, and other. Living arrangement, a proxy for social support, was broken out as follows: alone, with spouse, with parent(s), with other family member, and other.
Enabling factors include income and availability of community health care resources. Income is measured as total annual family income and is broken out into four groups—less than $5000, $5000-$9,999, $10,000-$19,999, and $20,000 or up. For availability of health care providers, we included a measure of how far a respondent lived from the closest hospital.
We looked at several measures of need. One was the primary disabling condition as determined by SSA. Three categories were used—physical or sensory impairment, mental illness, and MR/DD impairment. Another measure was the level of functional impairment based on ADLs and IADLs. For ADLs, we included six activities—bathing, dressing, toileting, transferring, getting around the home, and eating. Six activities were also included in the IADL variable—shopping, money management, preparing meals, using the telephone, doing light housework, and managing medications. Another measure of need is self-reported health status which was divided into three categories—fair or poor, good, and very good or excellent.
Methods
We conduct both descriptive and multi-variate analyses. In the descriptive analysis, we present basic statistics on health care access, use, and satisfaction among working-age Medicaid SSI beneficiaries who reside in two areas—NYC and WC. For the multivariate analysis, our goal was to examine whether the health care experiences of SSI beneficiaries varied across different subgroups and to identify characteristics of the study population that are associated with greater difficulties in obtaining care. In addressing these issues, we estimate multivariate models of access, use, and satisfaction as a function of the predisposing, enabling, and need factors.8 Since all the outcome measures are binary variables we estimate logit regression models. For ease of presentation, the WC and NYC samples were combined for the multivariate analy-sis.9 To account for a possible location effect, we included a variable indicating whether the respondent lived in WC.
Results
Health and Disability Status
Although the entire sample is disabled, we found substantial variation in disabling condition, functional status, and general health status among respondents. As to primary disabling condition, they varied somewhat between NYC and WC. In NYC, 48 percent of the SSI enrollees qualified because of a physical or sensory impairment, 35 percent because of a psychiatric illness, and 16 percent because of MR/DD impairment. In contrast, approximately equal shares (40 percent) of SSI enrollees in WC have a physical or sensory impairment and psychiatric illness, while MR/DD enrollees account for approximately 20 percent of that sample. Nationally, 41 percent of non-aged adult SSI recipients have physical or sensory disabilities, 31 percent have mental illness, and 28 percent mental retardation.
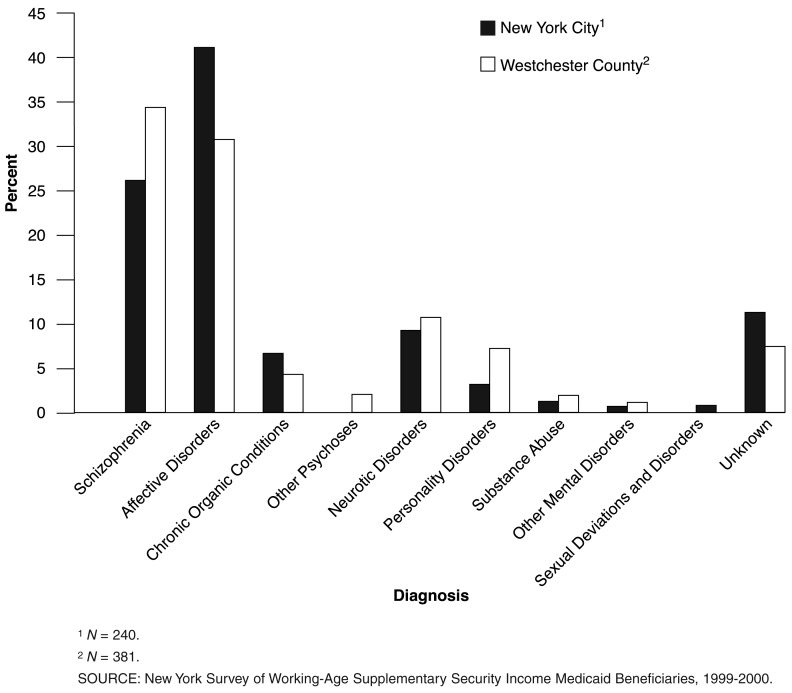
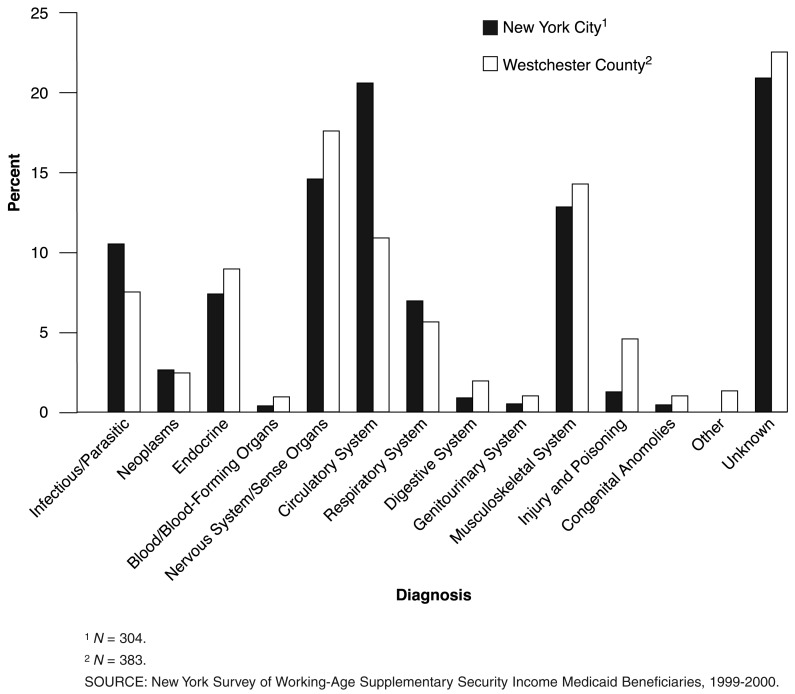
Among the SSI recipients with a primary diagnosis of mental illness, the specific types of diseases and disorders are roughly comparable in NYC and WC (Figure 1). The primary difference is in the share of people with affective disorders which is higher in NYC than in WC (41 versus 32 percent). Likewise, among enrollees with a primary diagnosis of a physical or sensory disability, the types of diseases and disorders are comparable between the two locations (Figure 2). One exception is in the share of the sample with diseases of the circulatory system which is approximately twice as high in NYC as in WC (21 versus 11 percent).
Figure 1. Summary of Specific Mental Disorders Among Working-Age Supplementary Security Income Beneficiaries with Mental Disabilities: New York, 1999-2000.
Figure 2. Summary of Specific Diseases Among Working-Age Supplementary Security Income Beneficiaries with Physical and Sensory Disabilities: New York, 1999-2000.
Consistent with the greater share of physical and sensory impairments in the NYC sample, SSI enrollees in NYC are more likely than those in WC to report that they need assistance with ADLs and IADLs. Nevertheless, the pattern of ADL limitations (needing help with bathing, dressing, eating, transferring, toileting, and getting around in their home) is very similar between NYC and WC. Of particular importance in the context of access to care, more than 20 percent of both groups of SSI enrollees reported needing help getting around their homes, raising the possibility of barriers to care due to mobility limitations. There are more differences between NYC and WC in IADL limitations (needing help with meal preparation, shopping, finances, telephone, housework, and medications), with approximately 70 percent of SSI enrollees in NYC reporting that they need IADL assistance as compared with 62 percent of the WC enrollees. Overall, three-quarters of SSI enrollees in NYC needed help with ADLs and/or IADLS, as compared with two-thirds of the WC sample. While the bulk of the sample reported some functional limitations, a substantial minority (26 percent in NYC and 33 percent in WC) reported no limitations.
Perhaps also reflecting the greater share of physical/sensory impairments in the NYC sample, SSI enrollees in NYC are much more likely than those in WC to report that they are in fair or poor health (61 versus 49 percent), that their health has gotten worse over the past year (25 versus 18 percent), and that they are not able to stay home alone for more than 2 hours (30 versus 24 percent). (Additional information on the health and disability status of the working age SSI beneficiaries is available on request from the authors.)
Demographic and Socioeconomic Characteristics
The average age of the SSI enrollees was slightly older in NYC compared with WC—45 versus 41 years. In NYC, 60 percent of enrollees are female, compared with 54 percent in WC. The dominant ethnic group in NYC was Hispanic; 45 percent of the sample identified themselves as being Hispanic. Another 27 percent reported being black, 23 percent white (non-Hispanic), and 5 percent fell into other racial groups (non-Hispanic). By contrast, WC recipients were more likely to be white (42 percent) and less likely to be Hispanic (24 percent). Consistent with the differences in ethnic and racial composition, 50 percent of SSI enrollees in NYC, as compared with 25 percent in WC, reported that English was not their first language. While the majority of both the NYC and WC enrollees were living with others (most often family members), nearly one-third reported that they lived alone. Enrollees reported limited formal education. Approximately 60 percent of NYC respondents and 50 percent of WC respondents had not completed high school. As would be expected given SSI Program financial limitations, family income was very low across both samples with most enrollees in NYC and WC reporting living in families with annual income of less than $10,000.
Finally, nearly all of the SSI enrollees had been enrolled in Medicaid for the full 12 months of the last year. Since the survey asked questions about recipients' health care experiences in the prior year, what was reported by respondents was generally encountered while being on Medicaid. In the NYC sample, where a voluntary managed care program was available for SSI recipients at the time of our survey, 11 percent of enrollees were in Medicaid managed care.10 (Additional information on demographic and sociodemographic characteristics on adult SSI beneficiaries is available on request from the authors.)
Potential Access to Care
Usual Source of Care
Having a usual source of care is often interpreted as an indicator of a greater likelihood of continuity of care. As shown in Table 2, 90 percent or more of the SSI recipients in both NYC and WC reported having a usual source of care (other than an ER) for their physical (somatic) health, a level in keeping with what has been reported for Medicaid enrollees nationally (Berk and Schur, 1998; Schoen et al., 1997; Cornelius, Beaureguard, and Cohen, 1991).
Table 2. Characteristics of Usual Source of Care, Continuity of Care, and Barriers to Care for Adult Supplementary Security Income Beneficiaries: New York, 1992-2000.
| Measure | Beneficiaries | |
|---|---|---|
|
| ||
| New York City | Westchester County | |
| Sample Size | 837 | 957 |
| Usual Source of Care (other than ER) for Physical Health | Percent | |
| Yes | 93.3 | 90.0 |
| Those with Usual Source of Care | ||
| Doctor's Office | 18.3 | 31.5 |
| Health Clinic | 42.0 | 37.3 |
| Outpatient Department (or Rehabilitation Hospital) | 37.5 | 28.0 |
| Other | 2.2 | 3.3 |
| Share Who See Same Provider at All or Most Visits | 82.4 | 81.1 |
| Length of Wait for Non-Emergency Appointment | ||
| More than 4 Days | 24.9 | 22.1 |
| More than 1 Week | 14.6 | 11.7 |
| Length of Wait in Office to See Provider | ||
| More than 30 Minutes | 70.1 | 59.1 |
| More than 60 Minutes | 45.5 | 30.7 |
| Travel Time to Usual Source of Care | ||
| More than 30 Minutes | 41.3 | 28.2 |
| More than 1 Hour | 13.0 | 9.8 |
| Difficulty Communicating with Medical Professional | ||
| Language Problem | 23.3 | 15.1 |
NOTE: ER is emergency room.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
For NYC respondents with a usual source of care, 42 percent reported a health clinic as their usual source of care, and another 37 percent reported using the outpatient department as their usual source of care. Only 18 percent reported a doctor's office as their usual source of care. The distribution was somewhat different in WC: Thirty-seven percent reported a health clinic as being their usual source of care, followed by a doctor's office (31 percent), and an outpatient department (28 percent). Finally, among those with usual source of care, more than 80 percent of both samples reported that they see the same provider at all or most visits. These findings suggest continuity of care for a large share of SSI enrollees under the current Medicaid FFS system. Even so, a substantial minority—approximately one in five—appear to lack some continuity of care as they report not seeing the same provider at all or most visits.
Convenience of Care
While most SSI recipients have a usual source of care, they reported long travel to appointments and wait times in the office—much higher than national estimates for the general Medicaid and uninsured populations (Cornelius, Beaureguard, and Cohen 1991). Nearly one-quarter of SSI recipients in both NYC and WC, for example, wait for more than 4 days for an appointment; one-half of those wait more than 1 week. Office wait times were also high. Waits of more than 30 minutes are the norm for 70 percent of NYC enrollees and 60 percent of those in WC. Moreover, almost one-half of the NYC enrollees wait longer than 1 hour and nearly one-quarter wait more than 2 hours (not shown). Enrollees also reported lengthy travel times to their usual source of care. Travel times of more than 30 minutes are reported by 41 percent of SSI recipients in NYC, and 28 percent of those in WC. Ten percent or more of both groups are traveling more than an hour to reach their usual source of care. While the survey did not ask respondents whether they chose to travel comparatively long distances or chose long appointment wait times, we did find that respondents indicating long travel or wait times were also more likely to report having more difficulty finding a doctor who accepts Medicaid than those who reported shorter travel and wait times.
As another measure of access to care we asked respondents whether they had difficulty communicating with health care providers because of a language problem. A large minority of recipients reported having communication difficulties with health care providers—23 percent of the NYC sample, and 15 percent of the WC sample. Since English is not the first language of one-half of the NYC population and 25 percent of the WC population, this result is not surprising. Some of the language problem may also be attributed to speech impediments that some disabled persons possess or a reliance on sign language.
Realized Access to Care
Health Care Use
Given that SSI enrollees are eligible for Medicaid because of a severe and chronic disability, they are heavy users of health care services. More than 90 percent of both the NYC and WC samples reported an outpatient visit for physical health in the last 12 months (Table 3). Within the last 3 months, the majority (more than 75 percent) of both NYC and WC sample members reported a doctor visit, almost one-half reported a visit to a specialist, and approximately one-third reported a mental health visit.
Table 3. Health Care Service Use for Adult Supplementary Security Income Beneficiaries: New York, 1999-2000.
| Type of Service | Beneficiaries | |
|---|---|---|
|
| ||
| New York City | Westchester County | |
| Sample Size | 839 | 956 |
| Percent | ||
| Outpatient Care | ||
| Outpatient Visits1 | 94.9 | 92.6 |
| Doctor Visits2 | 81.1 | 73.3 |
| Multiple Doctor Visits | 64.3 | 57.9 |
| Specialist Visits2 | 47.7 | 43.0 |
| Multiple Specialist Visits2 | 33.8 | 30.6 |
| Mental Health Visit2 | 32.0 | 33.0 |
| Multiple Mental Health Visits2 | 26.5 | 28.6 |
| Emergency Room or Hospital Care1 | ||
| Hospital Stays | 26.9 | 23.9 |
| Multiple Hospital Stays | 12.4 | 11.1 |
| Emergency Room | 48.3 | 45.7 |
| Multiple Visits | 26.5 | 28.2 |
| Preventative Care1 | ||
| Dental Visits | 69.6 | 68.4 |
| Blood Pressure Checks | 98.4 | 95.1 |
| Flu Shot | 38.0 | 35.7 |
| Pap Smear (Females Only) | 71.4 | 63.6 |
Last 12 months.
Last 3 months.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
In addition to the high levels of use of outpatient care, the NYC and WC SSI enrollees are frequent users of ERs and inpatient hospital care. Nearly one-half of the SSI recipients in NYC and WC reported an ER visit in the last 12 months and approximately one-quarter reported a hospital stay. Moreover, for those with ER visits and hospital stays, multiple visits and stays were quite common: More than 25 percent of the SSI enrollees reported multiple ER visits and more than 10 percent reported multiple hospital stays in the last year. While we are not able to identify ambulatory care-sensitive ER visits and hospital stays, the high levels of ER and hospital use suggest that there may be opportunities to improve SSI recipients' access to primary care and, in turn, lower health care costs.
The survey also asked respondents about their use of preventative care—dental care visits, blood pressure checks, flu shots, and Pap smears. Overall, the sample reported receiving preventative care at levels in keeping with or approximate the goals set out in Healthy People 2000 (U.S. Department of Health and Human Services, 1991). For example, approximately 70 percent of the sample both in NYC and WC had: a dental visit in the past 12 months, nearly all a blood pressure check in the last year, and 71 percent of the females in NYC and 64 percent in WC had a Pap smear in the last year. Getting a flu shot was the one preventative service that fell short of targeted goals: Less than 40 percent of the samples in NYC and WC reported getting immunized in the last year; the Healthy People 2000 goal for high-risk groups such as persons with disabilities is 60 percent (U.S. Department of Health and Human Services, 1991).
Unmet Need
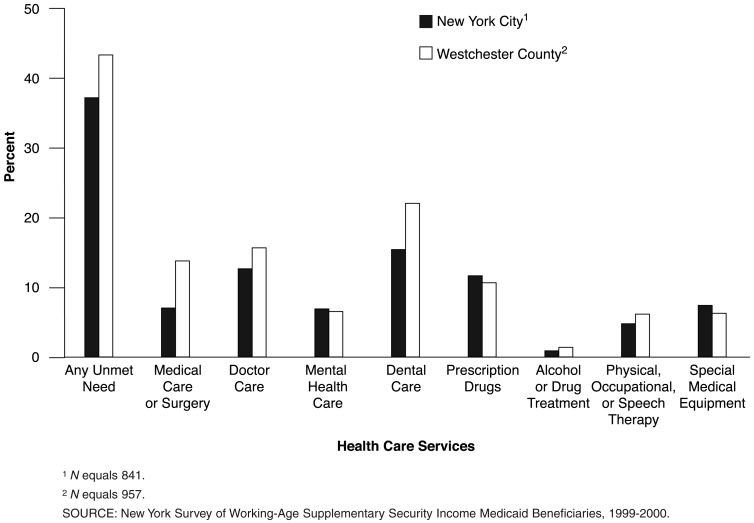
Despite being frequent users of health care services and most reporting have a usual source of care, substantial shares of SSI enrollees report not getting all the care they felt they needed (Figure 3). Approximately 38 percent of NYC enrollees and 43 percent of WC enrollees report some type of unmet need as measured across five services—medical care or surgery, doctor care, mental health care, dental care, and prescription drugs. The most common sources of unmet need in the two samples are dental care (16 percent in NYC to 21 percent in WC) and doctor care (13 percent in NYC to 15 percent in WC). The biggest difference between NYC and WC was in the reported unmet need levels for medical care or surgery: The level in WC was twice that of NYC (14 versus 7 percent).
Figure 3. Unmet Need Among Working-Age Supplemental Security Income Beneficiaries: New York, 1999-2000.
Individuals who reported unmet need for medical care or surgery were asked about the consequences of that unmet need. Approximately 60 percent of those reporting unmet need in both NYC and WC reported negative consequences as a result of that unmet need, sometimes serious (not shown). Negative outcomes included a worsening of the condition, a failure of the condition to improve, or a slower recovery than expected. Between 7 and 8 percent (WC and NYC, respectively) reported needing to go the ER or hospital because of the unmet need (not shown).
Individuals who reported unmet need were asked the main reason for that unmet need. Although the reported reasons varied by type of unmet need and between NYC and WC, there were some common patterns (Table 4). In particular, limited availability of providers was a key factor across all types of unmet need—both in NYC and WC. In WC, from one-third to one-half of those with unmet need for medical care and surgery, doctor care, mental health care, and dental care report problems with the availability of providers as the primary reason for not getting all the care they needed. Likewise, in NYC, between one-quarter to one-third of those with an unmet need reported provider availability as the primary reason for not getting the care they needed. Related to the availability of providers, accessibility of providers (for example, provider location, transportation problems, and language or physical barriers) was also frequently cited as a problem.
Table 4. Reasons for Unmet Need for Adult Supplementary Security Income Beneficiaries: New York, 1999-2000.
| Reason for Unmet Need | Beneficiaries | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| New York City | Westchester County | |||||||
|
|
|
|||||||
| Medical Care or Surgery | Doctor Care | Mental Health Care | Dental Care | Medical Care or Surgery | Doctor Care | Mental Health Care | Dental Care | |
| Sample Size1 | 57 | 108 | 54 | 122 | 127 | 146 | 60 | 201 |
| Percent | ||||||||
| Limited Availability of Providers2 | 27.2 | 28.7 | 34.8 | 25.5 | 35.5 | 46.6 | 43.8 | 50.3 |
| Cost, Coverage, and Administrative Issues3 | 8.6 | 8.2 | 17.7 | 30.7 | 19.8 | 8.9 | 5.4 | 23.3 |
| Problems with Accessibility of Care4 | 16.0 | 27.6 | 13.5 | 16.0 | 13.5 | 11.4 | 7.6 | 6.3 |
| Problems with Quality of Care | 11.5 | 3.2 | 7.9 | 5.9 | 14.0 | 4.5 | 13.7 | 4.8 |
| Health Prevents Treatment | 12.3 | 0.0 | 0.0 | 1.0 | 3.3 | 0.8 | 0.0 | 0.6 |
| Other Reasons5 | 24.4 | 24.8 | 21.5 | 20.8 | 13.8 | 25.9 | 29.5 | 14.6 |
Sample size refers to number of persons reporting an unmet need for specified service.
Includes “providers didn't accept Medicaid,” “trouble finding a provider,” or “couldn't get an appointment.”
Includes “care costs too much” and “Medicaid wouldn't approve care.”
Includes provider location, inconvenient hours, transportation problems, and language or physical barriers.
Includes stigma related to being on Medicaid and fear or avoidance of health care providers.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
Another common reason reported for unmet need was cost, coverage, and administrative issues associated with the Medicaid Program. In particular, those issues were cited as the main reason for unmet need for dental care (31 percent) and mental health care (18 percent) in NYC, and unmet need for dental care (23 percent) and medical care/surgery (20 percent) in WC. Although relatively few SSI enrollees reported quality of care issues as the principal reasons for their unmet need, for some services a substantial minority cited quality as the main reason for their unmet need. For example, more than 10 percent of those with unmet need for medical care and surgery in NYC and WC, and nearly 14 percent of those an unmet need for mental health care in WC cited quality of care issues as the principal reason for their unmet need.
Finally, many with unmet need in NYC and, to a less extent, in WC, reported personal reasons as the main reason for their unmet need. These include stigma, fear, and avoidance of health care providers. In part these reasons likely reflect the personalities of the sample persons. At the same time, they also likely reflect some system problems in that people are reluctant to use the health care system because of how they are treated or the barriers they encounter and the like.
Satisfaction with Care
We measured satisfaction with care across a wide range of measures, including quality of care, and access to certain types of providers. On the whole, SSI beneficiaries reported not being satisfied with the care they receive under FFS Medicaid (Table 5). The majority of SSI enrollees in both NYC (69 percent) and WC (78 percent) rated one or more aspects of their care as fair or poor (as opposed to good, very good, or excellent). In both NYC and WC, the area of greatest dissatisfaction was in the ease of finding a doctor who accepts Medicaid—nearly 30 percent of SSI enrollees in NYC, and 50 percent in WC rated the ease of finding a doctor who accepts Medicaid as fair or poor.
Table 5. Satisfaction with Care Among Adult Supplementary Security Income Beneficiaries: New York, 1999-2000.
| Satisfaction Measure | Beneficiaries | |
|---|---|---|
|
| ||
| New York City | Westchester County | |
| Sample Size | 819 | 903 |
| Percent | ||
| Rated as Being Fair or Poor | ||
| One or More Aspects of Care | 68.6 | 78.4 |
| Overall Quality of Medical Care | 17.8 | 21.5 |
| Ease of Finding a Doctor Who Accepts Medicaid | 28.8 | 49.9 |
| Ease of Getting Specialist Medical Care1 | 25.1 | 39.5 |
| Ease of Getting Emergency Medical Care1 | 33.4 | 29.1 |
| Ease of Getting Mental Health Care1 | 18.2 | 21.7 |
Those indicating they did not need a particular type of care were excluded from calculation.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
Beyond that, the areas with the greatest shares of enrollees reporting ratings of fair or poor in NYC were ease of getting emergency care (33 percent), ease of getting specialist care (25 percent), and ease of getting mental health care (18 percent). The pattern was somewhat different in WC, with ease of getting specialist care (40 percent), ease of getting ER (29 percent), and ease of getting mental health care (22 percent) getting the lowest satisfaction ratings. Beneficiaries appear to be more satisfied with the overall quality of care; nevertheless, approximately one in five of both NYC and WC enrollees rated the overall quality of their health care as fair or poor.
Multivariate Analysis
In an effort to determine whether the experiences of working age SSI Medicaid beneficiaries vary across disability subgroups or whether certain personal characteristics are associated with greater difficulties in obtaining care we conducted mul-tivariate analysis. As shown in Table 6, after controlling for a range of factors, the prevailing pattern was that health care experiences were fairly similar across the disability groups as well as other subgroups.
Table 6. Estimation Results for Adult Working-Age Supplementary Security Income Beneficiaries: New York1, 1999-2000.
| Explanatory Variable | Usual Source of Care | Hospital Stay in Last 12 Months | ER Visit in Last 12 Months | Doctor Visit in Last 3 Months | Unmet Need for Medical Care or Surgery | Rate Overall Quality of Care as Fair or Poor | Rate Ease of Finding a Doctor Who Accepts Medicaid as Fair or Poor |
|---|---|---|---|---|---|---|---|
| Sample Size | 1,785 | 1,784 | 1,763 | 1,774 | 1,776 | 1,740 | 1,425 |
| Predisposing Factors | |||||||
| Age (Continuous) | **0.046 | *-0.020 | *-0.014 | 0.016 | *-0.039 | **-0.029 | **-0.026 |
| Female | 0.543 | 0.187 | *0.346 | 0.402 | -0.153 | -0.414 | *-0.500 |
| Black | 0.468 | 0.050 | 0.329 | 0.009 | -0.109 | -0.095 | **-0.742 |
| Black | 0.468 | 0.050 | 0.329 | 0.009 | -0.109 | -0.095 | **-0.742 |
| Hispanic | 0.806 | 0.249 | 0.007 | 0.271 | 0.171 | -0.409 | **-1.061 |
| High School Graduate | 0.220 | 0.025 | -0.130 | -0.004 | -0.203 | *-0.500 | -0.282 |
| Lives Alone | -0.068 | 0.185 | -0.193 | 0.139 | 0.312 | 0.316 | 0.119 |
| Enabling Factors | |||||||
| Income Less than $10,000 | -0.012 | 0.350 | 0.225 | -0.248 | 0.196 | -0.001 | -0.113 |
| Distance to Closest Hospital | 0.240 | 0.186 | 0.234 | -0.010 | 0.256 | 0.032 | 0.033 |
| Need Factors | |||||||
| Mentally III | **-1.153 | -0.270 | -0.227 | -0.220 | 0.309 | 0.094 | -0.102 |
| MR/DD | -0.459 | **-1.139 | **-0.729 | *0.683 | -0.756 | -0.502 | -0.409 |
| Total Number of ADLs | 0.104 | *0.142 | *0.142 | 0.171 | 0.146 | 0.064 | 0.006 |
| Total Number of IADLs | -0.005 | 0.109 | 0.065 | 0.041 | 0.101 | 0.108 | 0.007 |
| Fair or Poor Health Status | 0.146 | **0.741 | 0.290 | 0.188 | 0.689 | *0.596 | 0.429 |
| Other | |||||||
| Proxy Respondent | 0.977 | -0.021 | -0.381 | 0.141 | -0.011 | -0.465 | -0.483 |
| Westchester County Resident | -0.054 | -0.058 | -0.073 | -0.240 | **0.711 | 0.175 | **0.701 |
| Constant | 0.216 | *-1.465 | -0.142 | 0.377 | *-2.103 | -0.166 | *1.285 |
Significant at the 0.10 level.
Significant at the 0.50 level.
New York City and Westchester County only.
NOTES: ER is emergency room. MR/DD is mentally retarded/developmentally disabled. ADLs is activities of daily living. IADLs is instrumental activities of daily living.
SOURCE: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000.
However, there were some exceptions to this general pattern. Most notably, persons with MR/DD were significantly less likely to have had a hospital stay, gone to the ER, or had a doctor visit than the physically disabled population. Fewer differences were found for persons with mental illness. With the exception of being less likely to report having a usual source of care, the experiences of those with mental illness were not significantly different than those with physical disabilities.
After controlling for other factors, persons in fair to poor health status were more likely to report having had a hospital stay and more likely to rate the ease of finding a doctor who accepts Medicaid as fair or poor. Together, these findings suggest that those in worse health and presumably the most in need are encountering the greatest difficulty in getting care. Level of functional impairment was significant in reported hospital and ER use: Beneficiaries with more ADLs were more likely to report having had a hospital stay and having used the ER compared with the less functionally impaired, IADL impairment level was not significant for any of the measures.
Age seems to affect beneficiaries' health care experiences. With increasing age, beneficiaries were significantly more likely to report having a usual source of care, less likely to have had a hospital stay, and less likely to report an unmet need for medical care or surgery. In addition, older recipients were less likely to rate quality of care or ease of finding a doctor who accepts Medicaid as fair or poor. Collectively, these findings could reflect that, over time, beneficiaries are able to develop a network of providers who offer them continuity of care and provide them with the level of care they feel they need.
After controlling for other factors, beneficiaries' experiences did not significantly vary by racial group. The one exception to this was the likelihood of rating the ease of finding a doctor who accepts Medicaid as fair or poor. Interestingly, black persons and Hispanics were less likely to report the ease of finding a doctor as fair or poor compared with white persons. One possible explanation is that New York, especially NYC, has a history of having providers that serve particular ethnic groups.
A beneficiary's living arrangement, income, or proximity to a hospital had no significant bearing on the measures we examined. Likewise, whether a sample person had a proxy respondent had no significant effect. In general whether the respondent lived in WC or NYC had no significant effect. There were two exceptions to this pattern: WC respondents were significantly more likely to report an unmet need for medical care or surgery and to rate the ease of finding a doctor who accepts Medicaid as fair or poor than their NYC counterparts. These findings on unmet need and ease of finding a doctor for WC support a recent case study report on WC's SSI Medicaid Program where county officials acknowledged that access problems among SSI beneficiaries was perhaps the single strongest motivating factor in wanting to shift to managed care (Coughlin et al., 2000).
Comparison to Other Populations
To provide some context, in this section we compare findings from our survey of SSI beneficiaries with other populations. To do this, we rely on data from the 1997 National Survey of America's Families (NSAF) (Kenney, Scheuren, and Wang, 1999). Specifically, for selected measures, we compare SSI beneficiaries with all non-aged adults nationally and all non-aged Medicaid enrollees nationally.11
As shown in Table 7, New York SSI recipients tend to be older, poorer, and have less formal education compared with the general Medicaid population and the overall adult population. For example, 54 percent of NYC SSI recipients and 42 percent of WC SSI recipients were in the age category 46-64 whereas, for the general Medicaid population and adults nationally, these percentages were 31 and 25 percent, respectively. As to education, 50-60 percent of SSI enrollees have less than a high school education, whereas among the general Medicaid population, approximately 40 percent had less than a high school education. For the general adult population, only 20 percent reported having not completed high school.
Table 7. Comparison of New York Supplementary Security Income (SSI) Enrollees to Nationally Non-Aged Adult Populations, by Selected Measures.
| Measure | New York SSI Enrollees | Non-Aged Adults Nationally | ||
|---|---|---|---|---|
|
|
|
|||
| New York City | Westchester County | All Adults | All Medicaid Adults | |
| Sample Size | 841 | 957 | 55,046 | 4,674 |
| Percent | ||||
| Age | ||||
| 18-30 Years | 17.1 | 28.7 | 30.0 | 40.5 |
| 31-45 Years | 28.3 | 29.3 | 39.3 | 34.9 |
| 46-64 Years | 54.5 | 42.0 | 30.7 | 24.6 |
| School Attainment | ||||
| Less than High School/Ungraded | 59.0 | 49.4 | 16.2 | 42.5 |
| High School Graduate | 25.0 | 31.1 | 30.1 | 28.1 |
| Some College/College Graduate | 16.0 | 19.5 | 53.7 | 29.5 |
| Annual Family Income | ||||
| $0-$4,999 | 10.3 | 18.4 | 26.4 | 23.8 |
| $5,000-$9,999 | 66.7 | 57.3 | 6.6 | 28.4 |
| $10,000-$19,999 | 17.2 | 13.0 | 11.8 | 27.5 |
| $20,000 or More | 5.9 | 11.5 | 55.1 | 20.4 |
| Health Status | ||||
| Very Good/Excellent | 14.7 | 25.6 | 65.3 | 36.0 |
| Good | 23.9 | 25.6 | 22.4 | 28.0 |
| Fair/Poor | 61.4 | 48.7 | 12.2 | 36.1 |
| Service Use Over Past 12 Months | ||||
| Emergency Room Visit | 48.3 | 45.7 | 20.8 | 41.2 |
| Hospital Stay | 26.9 | 23.9 | 7.2 | 18.5 |
| Dental Visit | 69.6 | 68.4 | 68.1 | 51.8 |
| Mental Health Visit | 32.0 | 33.0 | 6.2 | 17.0 |
| Unmet Need | ||||
| Medical Care/Surgery | 7.0 | 13.5 | 7.4 | 10.1 |
| Dental Care | 15.6 | 21.2 | 12.8 | 19.7 |
| Mental Health Care | 6.9 | 6.4 | 1.2 | 3.2 |
| Prescription Drugs | 11.6 | 10.4 | 4.7 | 9.7 |
SOURCES: New York Survey of Working-Age Supplementary Security Income Medicaid Beneficiaries, 1999-2000; and National Survey of America's Families, 1997.
Not surprisingly, SSI enrollees have lower health status compared with the overall adult and Medicaid populations: Between 50 and 60 percent of SSI enrollees reported being in fair or poor health. By contrast, only 12 percent of the general adult population, and 36 percent of the general Medicaid population reported being in fair or poor health.
Reflecting their lower health status, SSI enrollees reported more health care service use (except for dental care) compared with other populations (Table 7). Over the past year, SSI enrollees were more likely to have gone to the ER, to have had a hospital stay, and to have had a mental health visit than either adults overall or the general Medicaid population.
Despite their more frequent use of services, SSI enrollees reported higher levels of unmet need—especially for mental health care—as compared with other populations. For mental health, between 6 and 7 percent of SSI recipients reported an unmet need for mental health care, approximately double the rate for the general Medicaid population and six times the rate for the general adult population.
Summary and Conclusions
This article examines an important subgroup of the Medicaid population—working age SSI Medicaid beneficiaries. Despite being a highly vulnerable and costly population, little is known about this subgroup: What are their characteristics? What is their health and functional status? What are their health care experiences? Answers to these questions become particularly important as many States contemplate implementing managed care programs for persons with disabilities. Indeed, having solid information about the population is an essential starting point for State officials to develop both sound captiation rates and plan contracts. For plans, such information is important to gain insights to a population with which, to date, most plans have had limited experience. Such information is also useful in guiding plans in network development; that is, determining both the type and scope of providers.
In this study, we analyzed data from a 1999-2000 survey of SSI beneficiaries living in NYC and WC, New York. The survey documents how the population was faring under Medicaid FFS system. While SSI beneficiaries and their health care experiences in the two survey locations were not identical, the findings for the samples were very comparable. Among other things, we found a wide diversity in the types of health conditions among the population. Common disabilities and conditions included mental retardation, schizophrenia, paranoia, muscular dystrophy, cerebral palsy, and chronic heart disease. There was also wide variation in functional status, with some reporting no functional limitations while others reported very high impairment levels
Our results on access to care were indeterminate: by some measures, Medicaid beneficiaries had good access to health care services, but by others they did not. For example, while virtually all sample persons reported having a usual source of care, high shares reported long travel time to appointments and long wait times in the office, and a substantial minority reported having communication difficulties with providers. Similarly, while the results show that the SSI recipients are frequent users of health care services, they also reported high levels of unmet need. The principal reasons for their unmet need were limited provider availability and limited provider accessibility. Collectively, these findings suggest that having a usual source of care or being a frequent user of services does not necessarily guarantee that all of a person's needs are fully met. As indicated by SSI beneficiaries' responses to the satisfaction questions, a big issue is provider accessibility, especially access to physicians.
SSI beneficiaries' assessments of their health care under FFS Medicaid were more clear. Nearly 70 percent in NYC and nearly 80 percent in WC rated one or more area of care (such as quality of care, ease of getting specialist care, ease of finding a doctor) as fair or poor. The areas of greatest dissatisfaction were being able to find a doctor who accepts Medicaid, the ease of getting specialist care, and the ease of getting emergency medical care.
The results also highlight how SSI enrollees differ from other segments of the population along several important dimensions. Using data from the NSAF to benchmark the SSI subgroup against other popu-lations—the overall adult population and the general Medicaid population—we found the SSI sample to be older, less formally educated, and poorer. We also found, as anticipated, the SSI were much more likely to report being in fair or poor health: Between 50 and 60 percent of SSI enrollees reported being in fair or poor health while only 12 percent of all adults and 36 percent of all Medicaid enrollees reported fair or poor health.
The multivariate analysis revealed that after controlling for socioeconomics, health status, and geography, health care access, use, and satisfaction did not vary significantly among the three main disability groups. Further, with few exceptions, access, use, and satisfaction did not vary by an individual's personal characteristics, or where they lived.
We acknowledge that our study has some shortcomings, and thus the results should be interpreted with some caution. Our analysis relies on self-reported data which are based on respondents' recall and self-assessment of medical needs. In addition, approximately 20 percent of SSI beneficiaries relied on proxies to respond to the survey. Thus, some of the assessments of access, use, and satisfaction may reflect the experiences and expectations of the proxies rather than those of the beneficiaries. However, our mulitivariate analysis revealed that controlling for other factors, the responses of proxy and self-respondents were not statistically different for key outcome variables. Finally, the study focuses on recipients in two locations within New York State, and thus the results are not generalizable to all of New York or to other States. However, given that New York has the highest spending per disabled Medicaid recipient in the Nation, our results may overstate how SSI beneficiaries are faring under Medicaid.
Implications for Managed Care
Like many other States, New York hopes to shift the majority of its SSI beneficiaries into mandatory managed care in the near future. Indeed, WC has already made this shift, just after we completed our survey. The study results highlight both the challenges and opportunities Federal and State health care policymakers and health plans face as they develop managed care programs for SSI beneficiaries. With respect to challenges, SSI recipients have diverse and complex health care needs, not typically found in other segments of the population. They also are functionally impaired and many possess language and mobility limitations. Further, our data suggest that SSI beneficiaries also have distinct socioe-conomic characteristics—for example, they tend to be older, less formally educated, and poorer—as compared with the general Medicaid population. As such, States and health plans will need to substantially retool their existing managed care programs to accommodate the specialized needs and unique qualities of the SSI population. Such accommodations could include broadening provider networks to include a wide array of providers (medical and otherwise) that can deal with both the medical and non-medical needs of the population. Accommodations could also include providing transportation and language or interpreter services.
States will also need to rethink how they are going to pay health plans to care for SSI recipients. At present most Medicaid managed care programs rely on fairly limited risk adjusters—for example, age, sex, location (Regenstein and Anthony, 1998). However, given the SSI population's wide-ranging health and functional status, it is important that States' capitation rates explicitly account for the population's diversity. Properly and adequately adjusting for risk will be central to the long-term success of a managed care program for the disabled.
With respect to opportunities, the SSI population has much to be gained with a shift to managed care. Under managed care, there is guaranteed access to care with a defined network of providers. Such a guarantee may help those beneficiaries who currently have trouble finding providers that will treat them, a problem reported by significant shares of SSI beneficiaries in our survey. It could also reduce the reported long travel and appointment wait times. With such changes, unmet need levels may decline and, in turn, enrollees' satisfaction with their health care improve.
Our results also suggest that there may be some efficiencies to be gained under managed care. Most prominent is the possible reduction in ER visits and in hospital stays—both very costly and frequently used services. If health plans provide a true medical home for beneficiaries by coordinating care and investing in primary care, inpatient care and ER use could be limited. There also appear to be opportunities to improve preventative care, particularly with respect to Pap smears and flu shots. Together, these efficiencies could potentially afford the New York Medicaid substantial program savings. Given that New York spent nearly $20,000 per SSI beneficiary in 1998 (more than twice the national average) the savings could be substantial.
In conclusion, this study has shown that SSI beneficiaries in New York are a unique population that report facing significant barriers to health care and low levels of satisfaction with their care under the current FFS Medicaid system. While a shift to managed care may improve this situation, it will require careful program design, implementation, and monitoring to ensure success.
Acknowledgments
We would like to acknowledge the help of many officials at New York's Department of Health. We would also like to thank Anne Ciemnecki, Karen Cybulski, and Mike Sinclair in the design and conduct of the survey, Paul Boben, who served as our project officer, and John Holahan for his many helpful comments.
Footnotes
Teresa A. Coughlin, Sharon K. Long, and Stephanie Kendall are with the Urban Institute. The research in this article was funded under HCFA Contract Number 500-95-0040. The views expressed in this article are those of the authors and do not necessarily reflect the views of the Urban Institute or the Centers for Medicare & Medicaid Services (CMS).
There was some—approximately 10 percent—voluntary managed care for Supplementary Security Income (SSI) recipients in NYC at the time of our survey.
Following the shift of disabled Medicaid beneficiaries to managed care, a second survey is scheduled to be fielded by CMS.
For the many disabled individuals who have multiple disabling conditions, we do not have information on those additional disabilities.
Information on primary disabling condition was sought in the interview in order to be able to assign those individuals who were missing SSA data on their disabling condition to the appropriate disability category for the analyses.
For persons without telephones, a toll-free number was provided in the advance letter asking them to call in to complete the survey.
In some cases, a family member would assist in conducting interviews for a Spanish-speaking respondent.
It should be noted that because of multicollinearity issues not all the variables presented in the descriptive analysis are used in the multivariate analysis.
As previously mentioned, the model also includes a variable indicating whether the responses to the survey were obtained from a proxy respondent and thus, may differ from those that would have been reported by the sample member.
Regressions were also run separately for the WC and NYC samples. We found no systematic differences between the results with the combined samples and the separate samples and, for space consideration, present the combined sample results.
The disabled individuals who chose to enroll in Medicaid managed care in NYC were very similar to those in FFS Medicaid in terms of their demographic and socioeconomic characteristics.
We also used the 1997 National Survey of America's Families data for the same set of comparisons using data for New York State residents only. Both the New York-specific data and national data yielded comparable findings.
Reprint Requests: Teresa A. Coughlin, M.P.H., Urban Institute, 2100 M Street, NW., Washington, DC. 20037. E-mail: tcoughli@ui.urban.org
References
- Allen SM, Croke AL. The Faces of Medicaid: The Complexities of Caring for People with Chronic Illnesses and Disabilities. Center for Health Care Strategies; Princeton, NJ.: Oct, 2000. [Google Scholar]
- Andersen R. A Behavioral Model of Families' Use of Health Services. Center for Health Administration Studies. University of Chicago; Chicago, IL.: 1968. [Google Scholar]
- Andersen R. Revisiting the Behavior Model and Access to Care: Does it Matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Andersen R, Aday LA. Access to Medical Care in the U.S.: Realized and Potential. Medical Care. 1978;16(7):533–546. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- Andersen R, Newman JF. Societal and Individual Determinants of Medical Care Utilization in the U.S. Milbank Memorial Fund Quarterly. 1973;51(1):95–124. [PubMed] [Google Scholar]
- Berk ML, Schur CL. Access to Care: How Much Difference Does Medicaid Make? Health Affairs. 1998 May-Jun;17(3):169–180. doi: 10.1377/hlthaff.17.3.169. [DOI] [PubMed] [Google Scholar]
- Bruen B, Holahan J. Medicaid Spending Growth Remained Modest in 1998, But Likely Headed Upward. The Kaiser Commission on Medicaid and the Uninsured. The Henry J. Kaiser Family Foundation; Washington, DC.: Feb, 2001. [Google Scholar]
- Ciemnecki AB, CyBulski KA, Kolln BA, et al. Interviewing Populations with Disabilities by Telephone: Data Quality Measures. Presented at the 55th American Association for Public Opinion Research Annual Conference; Portland, Oregon. May 18-21, 2000. [Google Scholar]
- Cornelius L, Beaureguard K, Cohen J. Usual Source of Medical Care and Their Characteristics. Agency for Health Care Policy and Research; Rockville, MD.: 1991. National Medical Expenditure Survey Research Finding 11. AHCPR No. 91-0042. [Google Scholar]
- Coughlin TA, Long SK, Kasten J, Goldenson S. New York's Partnership Plan: An Early Look at Program Implementation. Urban Institute; Washington, DC.: Feb, 2000. Final Report. [Google Scholar]
- Cybulski KA, Ciemnecki AB. Interviewing Populations with Disabilities by Telephone: Survey Design and Operations. American Statistical Association 2000 Proceedings of the Section on Survey Research Methods; Portland, OR.. 2000. [Google Scholar]
- Davis MH, O'Brien E. Profile of Persons with Disabilities in Medicare and Medicaid. Health Care Financing Review. 1996 Summer;17(4):179–211. [PMC free article] [PubMed] [Google Scholar]
- Ford B. An Overview of Hot Deck Procedures. In: Madow WG, Olkin I, Rubin DB, editors. Incomplete Data in Sample Surveys. Vol. 2. Academic Press; New York, NY.: 1980. [Google Scholar]
- Gold M, Nelson L, Brown R, et al. Disabled Medicare Beneficiaries in HMOs: New Research. Health Affairs. 1997 Sep-Oct;16(5):149–162. doi: 10.1377/hlthaff.16.5.149. [DOI] [PubMed] [Google Scholar]
- Hagglund KJ, Clark M, Conforti K, Shigaki CL. Access to Health Care Services Among People with Disabilities Receiving Medicaid. Missouri Medicine. 1999;96(9):447–453. [PubMed] [Google Scholar]
- Hill S, Wooldridge J. SSI Enrollees in TennCare: Room for Improvement. Mathematica Policy Research, Inc.; Washington, DC.: Mar, 2000. Final Report. [Google Scholar]
- Kenney G, Scheuren F, Wang K. National Survey of America's Families: Survey Method and Data Reliability. The Urban Institute; Washington, DC.: 1999. (NSAF Methodology Series, No. 1). [Google Scholar]
- Mathematica Policy Research Inc. New York Survey of Working-Age Disabled Medicaid Beneficiaries, 1999-2000. Washington, DC.: 2000. [Google Scholar]
- Massey JT, O'Connor D, Krotki K. Response Rates in Random Digit Dial Telephone Surveys. Proceedings of the Survey Research Methods Section of the American Statistical Association; Anaheim, CA.. 1997. [Google Scholar]
- Meyer J, Zeller PJ. Profiles of Disability: Employment and Health Coverage. The Kaiser Commission on Medicaid and the Uninsured. The Henry J. Kaiser Foundation; Washington, DC.: Sep, 1999. [Google Scholar]
- Regenstein M, Anthony SE. Medicaid Managed Care for Persons with Disabilities. No. 11. Urban Institute; Washington, DC.: 1998. Assessing the New Federalism. [Google Scholar]
- Rosenbach ML. Access and Satisfaction Within the Disabled Medicare Population. Health Care Financing Review. 1995 Winter;17(2):147–167. [PMC free article] [PubMed] [Google Scholar]
- Schoen K, Lyons B, Rowland D, et al. Insurance Matters for Low-Income Adults: Results from a Five-State Survey. Health Affairs. 1997 Sep-Oct;16(5):163–171. doi: 10.1377/hlthaff.16.5.163. [DOI] [PubMed] [Google Scholar]
- Sisk J, Gorman SA, Resinger AL, et al. Evaluation of Medicaid Managed Care: Satisfaction, Access, and Use. Journal of the American Medical Association. 1996;276(1):50–55. [PubMed] [Google Scholar]
- Stein REK. Health Care For Children: What's Right, What's Wrong, What's Next. United Hospital Fund; New York, NY.: 1997. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2000. U.S. Department of Health and Human Services; Washington, DC.: 1991. DHHS Pub. No. (PHS) 91-50213. [Google Scholar]
- U.S. General Accounting Office. Medicaid Managed Care: Serving the Disabled Challenges State Programs. U.S. General Accounting Office; Washington, DC.: Jul, 1996. GAO/HEH5-96-136. [Google Scholar]