Abstract
Medicare's health care quality improvement program (HCQIP) is a national effort to improve beneficiaries' quality of care. The end stage renal disease (ESRD) HCQIP was implemented in 1994 in response to criticism about the poor quality of care received by ESRD patients. Quality improvement efforts initiated by the ESRD Networks and dialysis providers in response to the HCQIP have demonstrated substantial improvement in care for dialysis patients. This article describes the evolution of the ESRD HCQIP and its successful application in the ESRD program.
Introduction
The adequacy of hemodialysis and the management of anemia in the U.S. ESRD population have improved dramatically in the last decade, partially in response to a program initiated by the Federal Government in collaboration with physicians and allied health professionals to redress substandard care. This alliance was fostered by reports that were critical of the care delivered to dialysis patients. The most influential of these reports was the 1989 morbidity, mortality, and prescription of dialysis symposium, which was convened to discuss the high mortality noted among hemodialysis patients in the U.S. and to consider the possibility that inadequate dialysis might explain the high rates (Parker, 1990). Evidence presented from ESRD registries around the world, including the U.S. renal data system (USRDS), showed that the U.S. mortality was higher than in other ESRD populations, was increasing, and was associated with less intense dialysis (Parker, 1990).
The possibility that care of ESRD patients was inadequate was an important issue for CMS. Since its inception in 1972, the Medicare ESRD program has sought to ensure that beneficiaries received appropriate, high quality care (Rettig and Levinsky, 1991). Initially, Medicare required dialysis treatment centers to be members of regional ESRD Network Organizations (Networks) with local medical review boards (MRBs) that “screened the appropriateness of patients for the proposed treatment procedures” (Rettig and Levinsky, 1991). In 1976, Medicare broadened Network and MRB responsibilities to include oversight and improvement of the quality of patient care, and in 1986 to include facility-specific reporting of poor care and onsite review of facilities and providers (Rettig and Levinsky, 1991). Then in 1988, contracting began with 18 newly configured Networks across the U.S. to oversee the quality of care received by ESRD patients, and to assist providers in quality assurance activities (Frederick et al., 1998).
Concerns were responded to about the poor quality care in 1989 by initiating Medical Case Review (MCR) through its 18 Networks. MCR included retrospective chart audits performed by Network staff against a set of dialysis patient-specific criteria with the results reviewed by the local MRB (Frederick et al., 1998; McClellan et al., 1995a). Cases that failed screening were referred to the Network MRB and if care was judged inadequate, the responsible physician was asked to take corrective action (Rettig and Levinsky, 1991). MCR was not supported by a systematic evaluation and in the absence of evidence for the effectiveness of MCR, a 1991 report from the Institute of Medicine suggested that a more data-driven approach to quality improvement was required to meet the needs of the program (Rettig and Levinsky, 1991). In July 1994, MCR was discontinued when ESRD HCQIP was initiated by Medicare through its Networks (Frederick et al., 1998). This article describes the development and the successful application of the ESRD HCQIP by Medicare in response to these reports.
ESRD Health Care Quality Improvement Program
In September 1993, a meeting was convened with the Networks and the renal community to discuss ideas for redefining the efforts of the ESRD Networks to improve the quality of care for ESRD patients (McClellan et al., 1995b; 1996). Representatives from the American Nephrology Nurses Association, the National Renal Administrators Association, the Renal Physicians Association, the American Association of Kidney Patients, the Forum of ESRD Networks, and Medicare representatives participated in this activity. Medicare's HCQIP concept was applied in the design of the new Network quality program.
The HCQIP was initiated in 1992 through Medicare's peer review organizations to improve care in the general Medicare population (McClellan et al., 1995a; Gagel, 1995; Lohr and Schroeder, 1990; Chassin, 1996; Jencks and Wilensky, 1992). The HCQIP goal is to improve outcomes by providing comparative information and technical support to assist health care providers to improve care (Gagel, 1995). The HCQIP is based on research that shows that variations in the outcomes cannot be entirely explained by differences in disease severity, and thus, are likely due to variations in processes of care. The HCQIP uses clinical practice guidelines to define processes of care that are closely associated with patient outcomes and subject to variation. These variations in process are identified by systems that can collect, manage, and analyze large amounts of data. Finally, the HCQIP model links the evidence about undesirable variations in care to actions by the health care system to improve care (Jencks and Wilensky, 1992). The adequacy of dialysis dose is an example of such a process of care.
The Networks, like the quality improvement organizations (QIOs)—formerly known as peer review organizations—are existing systems that collect and analyze data about processes and outcomes of care, disseminate the resulting information to providers, and assist them in recognizing needed improvements. These systems can also identify patient populations with poor outcomes that can be targeted for interventions. It was natural for Medicare to use its existing Network system to implement HCQIP in the ESRD program (McClellan et al., 1995a). The resulting new Network quality program included the national ESRD core indicators (CI) project as the central focus for assessing and measuring the quality of care for ESRD patients. This CI Project incorporated HCQIP concepts and became the foundation for Medicare's ESRD HCQIP. An ESRD CI Workgroup was formed to develop the project.
Implementation of the CI Project
Development
In 1993, building on the experience of MCR, the CI Workgroup sought input from a wide range of persons with expertise in the treatment of chronic renal disease, in determining the important areas of care for dialysis patients and subsequent indicator identification. The only clinical practice guidelines available at the time were the ones for hemodialysis adequacy developed by the Renal Physicians Association (Hornberger, 1993 a, b; and Renal Physicians Association Working Committee on Clinical Practice Guidelines, 1993). The CI Work group used these guidelines and other literature to select the quality indicators for the national CI Project (McClellan et al., 1995b). The CI Workgroup identified four key indicators to assess and measure important aspects of ESRD care: (1) hematocrit level to measure anemia management, (2) urea reduction ratio (URR) to measure the adequacy of hemodialysis, (3) serum albumin as a marker for nutritional management, and (4) blood pressure level for assessing blood pressure control.
Population
The eligible population for the initial sample and each successive annual sample was comprised of all ESRD patients who were included in the ESRD Network's database. ESRD is unusual within the Medicare system in that all individuals eligible to receive social security benefits, regardless of age, are covered for care. Since the Medicare eligible population exceeds 93 percent of all ESRD patients, the annual samples were representative of the entire ESRD population. In each year, a random sample of adult (age 18 or over) in-center hemodialysis patients, stratified by ESRD Network, were identified by Medicare from Network data systems. Eligible patients had to be receiving dialysis and alive on the last day of the study year. The sample size was originally determined by a desire to be 95 percent confident that network-specific estimates for the selected clinical measures be accurate within plus/minus of 5 percent. This resulted in samples of approximately 350 patients per network on average.
Data Collection
In 1994, the first year of the CI Project, a random sample of adult (age 18 or over) in-center hemodialysis patients, stratified by ESRD Network, was identified by Medicare from Network data systems. A one-page data abstraction form was designed for completion by treatment center staff. The data collection form allowed Medicare to annually obtain the necessary clinical information to calculate the CIs nationally and regionally.
The ESRD Networks distributed the data collection forms to the dialysis facilities with one or more patients in the sample. Facility staff abstracted information for the last 3 months of the study year from the selected patients' medical record. The facilities returned the completed forms to their Networks, where the data were reviewed for acceptability and manually entered into a data entry program. A systematic record re-abstraction of approximately 5 percent of the patients from the initial sample conducted by the Networks assessed the accuracy of information provided by the facilities. The initial validation study following the first year of data collection found that 94 percent of the clinical data reported by the treatment centers agreed with those abstracted by Network staff (Health Care Financing Administration, 1995a). Each year since 1994, a 5-percent sample of patient records is re-abstracted by the Networks to validate the information submitted by the treatment centers.
The data collected in 1994 (for the time period October-December 1993) established a baseline estimate for several important clinical areas of care for adult hemodialysis patients in the U.S. from 1994-1998, Medicare, through its Networks, annually conducted the CI Project. In 1995, collecting clinical data on a national sample of adult peritoneal dialysis patients was added to the project design (Health Care Financing Administration, 1997b). The purposes of these data collections were to determine whether patterns in these clinical measures had changed, and if opportunities to improve care continued to exist.
Network Interventions
In addition to the clinical information collected through the CI Project, the ESRD HCQIP required the Networks to conduct activities to facilitate the translation of Network-specific CIs findings into facility-specific activities to improve care. During the period from 1994-1995, with the initiation of the CI Project, each Network designed its own intervention activities to improve the adequacy of hemodialysis and management of anemia. Interventions included: (1) strategies to select treatment centers needing improvement, (2) dissemination of guidelines and national and Network CIs findings, (3) distribution of algorithms to improve inadequate dialysis and anemia treatment, (4) workshops on adequacy of dialysis, anemia management, and quality improvement, and (5) close supervision of poorly performing treatment centers (McClellan et al., 1998).
Merging the CI and CPM Projects
Development
The Balanced Budget Act of 1997 directed Medicare to develop a method to measure and report the quality of dialysis care provided under the Medicare Program. To respond to this legislation, Medicare funded the development of clinical performance measures (CPMs) based on the National Kidney Foundation's Dialysis Outcome Quality Initiative Clinical Practice Guidelines (PRO-West, 1999). During the 1998 CPM development process, broad participation from the renal community was solicited to ensure the acceptability and utility of the CPMs. The guidelines were prioritized on the strength of supporting evidence, the feasibility of developing CPMs, and the significance of the proposed CPMs to the quality of dialysis care. After prioritization, 16 CPMs pertaining to the adequacy of hemodialysis, vascular access care, and anemia management were developed. In 1999, data abstraction instruments were pilot-tested nationwide to capture the needed information to calculate the CPMs. Also during that year the ESRD CI Project was merged with the CPM development effort, and the project is now known as the ESRD CPM Project. The CPMs are similar to the CIs with the addition of measures for assessing vascular access.
Data Collection and Network Interventions
The ESRD CPM Project, like the CI Project, continues to collect information annually on the hemodialysis and peritoneal dialysis population in order to assess and measure the quality of care of dialysis patients. During the data collection effort in 2001, more than 8,000 hemodialysis patients were sampled, approximately 490 per Network, and completed forms were returned to the Networks by the treatment facilities for 95 percent of those patients selected (Centers for Medicare & Medicaid Services, 2001). The Networks continue to conduct intervention activities or quality improvement projects with treatment centers to improve the quality of care and outcomes of dialysis patients.
CMS and the Networks are collaborating in the development of an electronic data exchange system that will allow the paperless flow of data from treatment centers to the Networks (Krisher and Pastan, 2001). The first phase, connecting CMS and the Networks, was introduced in 1999 and is called the standard information management system. The second phase, which will link treatment centers to Networks, is called the vital information system to improve outcomes in nephrology and is being pilot-tested in three Networks in 2002. The system will allow for the collection and reporting of important clinical information on all patients to measure the quality of their care and outcomes.
Results
Variations in Care
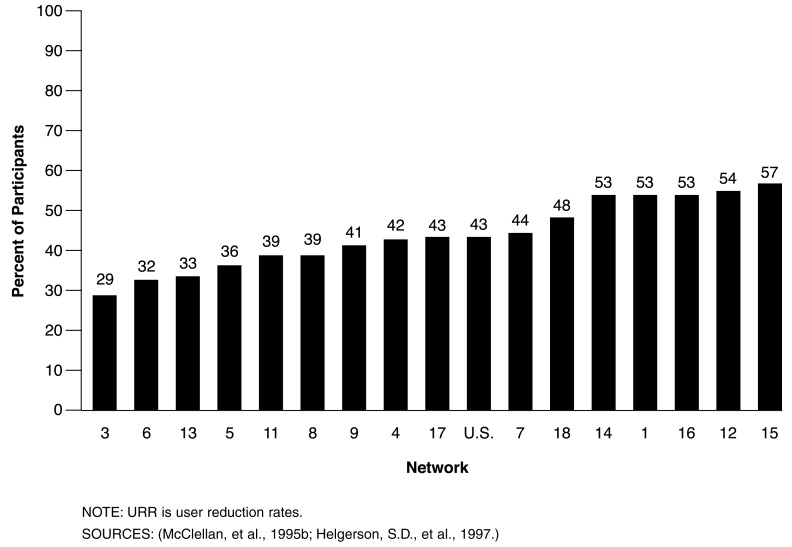
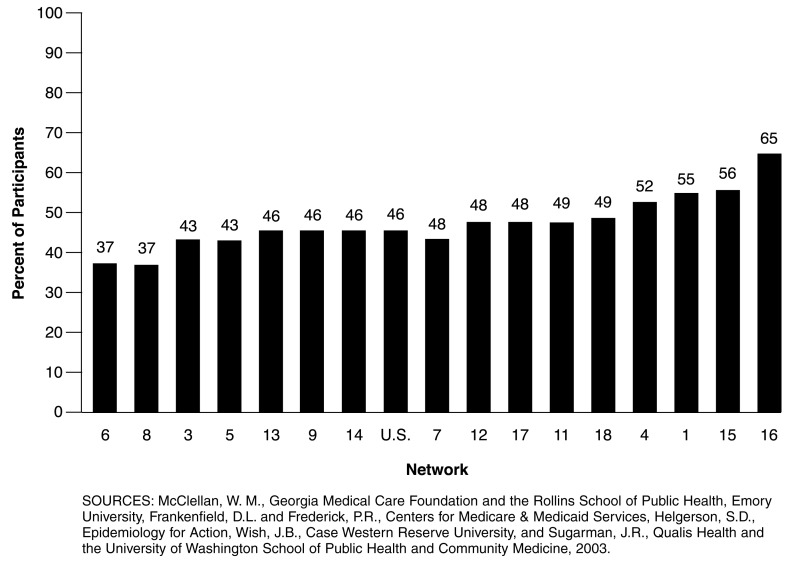
The 1994 CI Project results found substantial variability in the hematocrit level and the URR for hemodialysis patients in the U.S. (Health Care Financing Administration, 1997a). Among adults receiving in-center hemodialysis treatment during the last quarter of 1993, only 43 percent attained a recommended URR of 65 percent or greater, with a mean URR for the national dialysis population of 63 percent (Health Care Financing Administration, 1997a). Figure 1 shows substantial regional variation among the 16 Networks that participated in the first year of the CI Project, with the proportion of adequately dialyzed patients ranging from 29 to 57 percent (Health Care Financing Administration, 1997a). A similar variation was noted in the mean hematocrit achieved by the sampled patients. In late 1993, the percentage of hemodialysis patients, with mean hematocrit 30 percent nationally was 46 percent, ranging from 37 to 65 percent among the 16 ESRD Network regions participating (Figure 2).
Figure 1. Percent of Adult In-Center Hemodialysis Patients with Mean URR 65 Percent or More, by Networks: 1993.
Figure 2. Percent of Adult In-Center Hemodialysis Patients with Mean Hematocrit 30 Percent or More, by Networks: 1993.
Trends in Patterns of Care
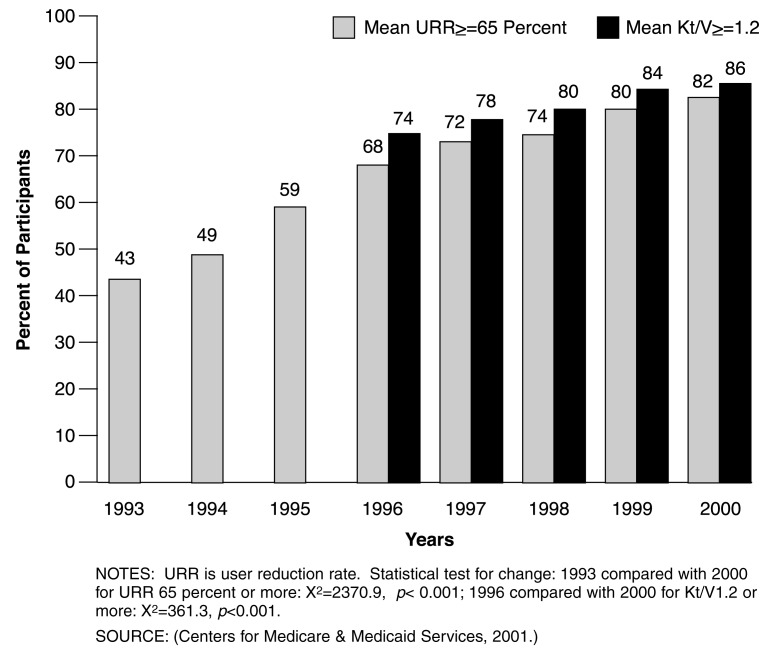
CI/CPM Projects data have been collected annually since 1994 and an annual report describing the findings is available on CMS' Web site (www.cms.hhs.gov/esrd). A steady increase in the proportion of hemodialysis patients receiving adequate treatment has been observed (Centers for Medicare & Medicaid Services, 2001; Helgerson et al., 1997). As shown in Figure 3, nationally, the proportion of individuals with a 3-month mean URR of 65 percent or more increased from 43 percent in late 1993 to 82 percent in late 2000 (Centers for Medicare & Medicaid Services, 2001). Beginning with the 1996 data information was collected to calculate Kt/V values, a measure of dialysis adequacy similar to URR. There has been an increase in the proportion of patients with a mean delivered Kt/V 1.2 or more over time, from 74 percent in late 1996 to 86 percent in late 2000 (Figure 3). These improvements in hemodialysis adequacy over this time period were accompanied by changes in the dialysis prescription. The mean dialysis session length increased from 196 minutes in late 1993 to 215 minutes in late 2000. The proportion of patients dialyzed with a hi-flux dialyzer (KUf 20 or more mL/mmHg/hr) increased from 29 percent in late 1993 to approximately 70 percent in late 2000 (Centers for Medicare & Medicaid Services, 2001).
Figure 3. Percent of Adult In-Center Hemodialysis Patients with Mean URR 65 Percent or More, or Mean Kt/V 1.2 or More: 1993-2000.
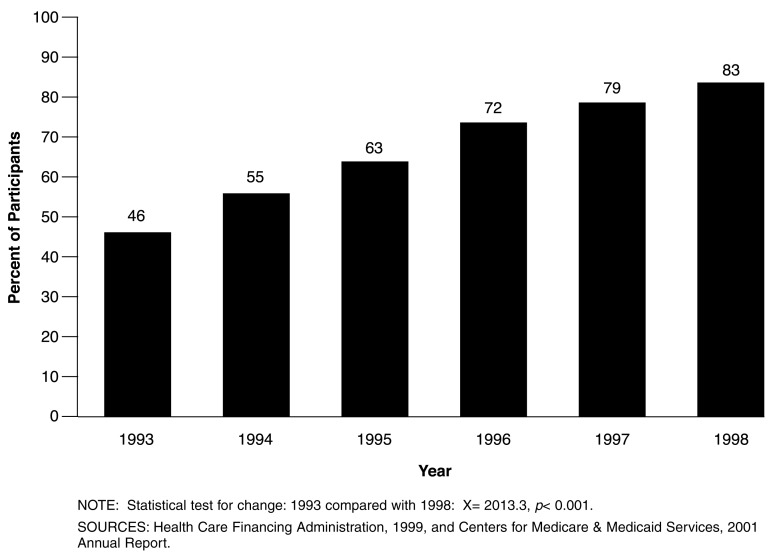
Improvement in anemia management also occurred over the history of the CI/CPM Projects, with the percent of hemodialysis patients achieving a mean hematocrit > 30 percent increasing from 46 percent in late 1993 to 83 percent in late 1998 (Figure 4). The mean hematocrit for sampled patients increased from 30.5 percent in late 1993 to 34.3 percent in late 1998 (Health Care Financing Administration, 1999). Beginning with the data for October-December 1997, hemoglobin values were collected; however, the collection of hematocrit information was discontinued in the 1999 study year. The percent of sampled adult hemodialysis patients achieving mean hemoglobin 11 or more gm/dL increased from 43 percent in late 1997 to 74 percent in late 2000 (Centers for Medicare & Medicaid Services, 2001).
Figure 4. Percent of Adult In-Center Hemodialysis Patients with Mean Hematocrit 30 Percent or More: 1993-1998.
Discussion
During the last decade, physicians and allied health professionals established a voluntary collaboration with CMS to implement Medicare's ESRD HCQIP through the regional ESRD Networks. The resulting CI/CPM Projects were designed to improve ESRD care. The Network system collects, analyzes, and disseminates information about the occurrence and outcomes of ESRD in a defined population. The Networks also assist treatment centers in identifying opportunities to improve care and to implement improvement actions. The renal community continues to be involved in the operation and oversight of the ESRD CPM Project through the multidisciplinary government and non-government ESRD CPM Quality Improvement Committee (Committee).
In 1999, 5 years after the inception of the ESRD HCQIP, Medicare initiated a process to identify information about dialysis facility characteristics and quality of care that could be publicly reported to facilitate consumer choice and to drive quality improvement. An expert workgroup sought input from a broad range of stakeholders to identify a set of measures that could be compiled from existing Medicare data sets and that would be responsive to the interests of dialysis patients as well as professionals (Frederick et al., 2002). In January 2001, CMS released “Dialysis Facility Compare”, a Web site that provides information regarding facility characteristics and quality measures related to dialysis adequacy, anemia management, and patient survival for each Medicare-certified dialysis facility in the U.S. (www.medicare.gov/dialysis/home.asp)
There are two important lessons that professionals in other fields of medicine should examine and consider applying from the ESRD CI/CPM Projects. First, illustrate how an approach based on consensus about a public health problem can be used to mobilize the participation of health care professionals and organizations to design, implement, revise, and maintain a quality improvement initiative. Second, illustrate the role of ongoing data gathering and reporting in evaluating the resulting improvements in care that have been observed since the inception of the projects.
Health care professionals and organizations involved with the care of ESRD patients met with and assisted CMS at each step in the evolution of the CI/CPM Projects. These Workgroup and Committee members assessed the relevance of the data collected, aided in its interpretation within the context of existing clinical practice guidelines for care of ESRD patients, and helped draft timely reports that were disseminated broadly and rapidly to the dialysis community. This collaboration allowed frequent and timely presentation of results from the CI/CPM Projects at national meetings, in relevant medical journals, and in reports listed on CMS' Web site (www.cms.hhs.gov). As described for the transition between the CIs and the CPM phase of this initiative, the active dialogue between CMS and the dialysis community facilitated rapid identification and application of new and revised clinical practice guidelines for ESRD. Finally, the Workgroup and Committee members were active spokes-persons to their respective groups for the CI/CPM Projects, promoting awareness, and support for the goals and programmatic initiatives implemented by CMS to improve ESRD care.
The success of this collaboration and the educational communications that derived from it are largely dependent on the success of the national ESRD surveillance system. First, the CI/CPM Projects demonstrate that it is possible to systematically gather, and report information derived from primary patient records about the quality of health care provided to large populations of ESRD patients. Further, the variations in care we observed were clinically important deviations from standards of care that were, in general, applicable to all ESRD patients. While these variations had been suspected from analyses of smaller, clinical populations, the data from the CI/CPM Projects provide a comprehensive estimate of the magnitude of the problem.
Second, the HCQIP model worked. Serially collected data documented variations in care related to important patient care outcomes. This information was disseminated to providers, and linked to quality improvement activities conducted with individual treatment centers by the Networks. Concurrent with these feedback and facility-specific interventions, care improved as documented by repeated remeasurement.
Third, the HCQIP model is capable of innovation as is illustrated by the incorporation of newly published Dialysis Outcome Quality Initiative Guidelines (National Kidney Foundation, 2001) into CPMs. CMS successfully mobilized and sustained the efforts of clinicians and allied health professionals within the ESRD community beyond the initial implementation of the CI Project in the mid-1990s. When new guidelines became available, these were readily assimilated through a consensus process into performance measures for use in the ESRD HCQIP.
Fourth, this experience illustrates that it is possible to analyze large amounts of data and disseminate the resulting information in a timely manner. During each of the 8 years of data collection, information about the patterns of care of randomly selected samples of ESRD patients alive during the last quarter of the sample year has been reported by CMS within 6 months of receipt of the data.
During the period covered by this article, extensive efforts were made by many groups and organizations to foster improved hemodialysis adequacy and anemia care, and it is reasonable to ask if there is evidence that the changes reported were influenced by the CI/CPM Projects. There is some evidence that the improvements we have reported were associated, in part, with quality improvement activities conducted by the ESRD Networks. McClellan et al.(1998) found that after controlling for case-mix factors and baseline URR, treatment facilities participating in a single Network-sponsored CI/CPM intervention were significantly more likely to improve hemodialysis adequacy compared with non-participants. Further, Network-specific rates of improvement in hemodialysis adequacy were associated with Networks that specific interventions, including targeting poorly performing treatment centers, provision of onsite assistance to help treatment centers identify ways to address poor hemodialysis adequacy and supervising intervention centers until care improved. While observational data like these are not a substitute for a randomized controlled trial, the CI/CPM Projects' impact on patterns of care is consistent with a program effect (Jencks, 1997).
It also is reasonable to ask if the changes in care noted during the last decade have resulted in improvements in patient outcomes. Again, in the absence of appropriate randomized clinical trials, the answer to this question cannot be definitively answered. However, it is encouraging to note that mortality rates for new and established hemodialysis patients have declined 10-15 percent since the inception of the program despite the rising number of older patients with diabetes mellitus accepted for treatment (U.S. Renal Data System, 2001). Thus, although definite evidence is lacking, changes associated with patterns of care within Networks and the current trends in case mix adjusted mortality rates within the national dialysis population are consistent with the expectations that led to the development and implementation of the CI/CPM Projects.
Conclusions
The national ESRD CI/CPM Projects represent a multidisciplinary collaboration with CMS to improve the dialysis care of adult hemodialysis patients that has been sustained over a substantial period of nearly 10 years. Non-government participants have donated their time to the design, implementation, and oversight of the ESRD HCQIP. The ESRD HCQIP was designed to promote adherence to evidence based clinical practice guidelines by trending patterns of care as monitored by the CI/CPM Projects which reflects an increasing adherence to these guidelines. The CI/CPM Projects have been responsive to new guidelines and to developing electronic information transfer technology.
We think that professionals in other fields of medicine should examine the lessons learned from the ESRD CI/CPM Projects, and apply these lessons to improving care for patients with other conditions. There are certainly unique features of ESRD, such as a predominant single payer for care (Medicare), a well-defined and easily recognized patient population, and care that is provided in specialized settings by provider teams that are intensely focused on a single clinical condition. However, Medicare also pays for a substantial portion of care delivered to patients with other chronic conditions. The role played by the ESRD Networks for chronic kidney failure is currently analogous to that played by the Nation's network of State-specific QIOs, contracted by CMS, for certain other diseases. QIOs have evolved from their original quality assurance role in much the same way as have the ESRD Networks. In no other field of medicine have the rapid, sustained, and clinically important process improvements demonstrated for dialysis care been realized. The ESRD program experience supports the utility of the HCQIP model for health care quality assurance and quality improvement in the U.S. population. We recommend that stronger partnerships between professional societies, QIOs, and other stakeholders be forged in order to improve care for patients with other chronic diseases.
Footnotes
William M. McClellan is with the Georgia Medical Care Foundation and the Rollins School of Public Health, Emory University. Diane L. Frankenfield and Pamela R. Frederick are with the Centers for Medicare & Medicaid Services (CMS). Steven D. Helgerson is with Epidemiology for Action. Jay B. Wish is with Case Western Reserve University. Jonathan R. Sugarman is with Qualis Health and the University of Washington School of Public Health and Community Medicine. The views expressed in this article are those of the authors and do not necessarily reflect the views of the Georgia Medical Care Foundation, Rollins School of Public Health, Emory University, CMS, Epidemiology for Action, Case Western Reserve University, Qualis Health, or the University of Washington School of Public Health and Community Medicine.
Reprint Requests: William M. McClellan, M.D., Georgia Medical Care Foundation, 57 Executive Park South, Suite 200, Atlanta, GA 30329. E-mail address: bmcclell@gmcf.org
References
- Centers for Medicare & Medicaid Services. 2001 Annual Report ESRD Clinical Performance Measures Project. 2001 Dec; Internet address: http://www.cms.gov/esrd/1.asp. (Accessed 2003.)
- Centers for Medicare & Medicaid Services. Internet address: http://www.cms.hhs.gov (Accessed 2003.)
- Centers for Medicare & Medicaid Services. Internet address: http://www.cms.hhs.gov/ESRD/asp (Accessed 2003.)
- Centers for Medicare & Medicaid Services. Internet address: http://www.Medicare.gov/dialysis/home.asp (Accessed 2003.)
- Chassin MR. Quality of Health Care, Part 3: Improving the Quality of Care. New England Journal of Medicine. 1996 Oct;335(14):1060–1063. doi: 10.1056/NEJM199610033351413. [DOI] [PubMed] [Google Scholar]
- Frederick PR, Frankenfield DL, Biddle MG, et al. Changes in Dialysis Units' Quality Improvement Practices From 1994 to 1996. American Nephrology Nurses Association Journal. 1998 Oct;25(5):469–478. [PubMed] [Google Scholar]
- Frederick PR, Maxey NL, Clauser SB, Sugarman JR. Developing Dialysis Facility-Specific Performance Measures for Public Reporting. Health Care Financing Review. 2002 Summer;23(4):37–50. [PMC free article] [PubMed] [Google Scholar]
- Gagel BJ. Health Care Quality Improvement Program: A New Approach. Health Care Financing Review. 1995 Summer;16(4):129–140. [PMC free article] [PubMed] [Google Scholar]
- Health Care Financing Administration. 1994 ESRD Core Indicators Project Supplemental Report 1: Results of Validation Study. Office of Clinical Standards and Quality; Baltimore, MD.: Apr, 1995a. [Google Scholar]
- Health Care Financing Administration. 1996 Annual Report, ESRD Core Indicators Project. 1997a Jan; Internet address: http://www.cms.gov/esrd/4.asp. (Accessed 2003.)
- Health Care Financing Administration. 1997 Annual Report, ESRD Core Indicators Project. 1997b Dec; Internet address: http://www.cms.gov/esrd/4.asp. (Accessed 2003.)
- Health Care Financing Administration. 1999 Annual Report, ESRD Core Indicators Project. 1999 Dec; Internet address: http://www.cms.gov/esrd/4.asp. (Accessed 2003.)
- Helgerson SD, McClellan WM, Frederick PR, et al. Improvement in Adequacy of Delivered Dialysis for Adult In-Center Hemodialysis Patients in the United States, 1993 to 1995. American Journal of Kidney Diseases. 1997 Jun;29(6):851–861. doi: 10.1016/s0272-6386(97)90458-3. [DOI] [PubMed] [Google Scholar]
- Hornberger JC. The Hemodialysis Prescription and Quality-Adjusted Life Expectancy. The Journal of the American Society of Nephrology. 1993a Oct;4(4):1004–1020. doi: 10.1681/ASN.V441004. [DOI] [PubMed] [Google Scholar]
- Hornberger JC. The Hemodialysis Prescription and Cost Effectiveness. The Journal of the American Society of Nephrology. 1993b Oct;4(4):1020–1027. doi: 10.1681/ASN.V441021. [DOI] [PubMed] [Google Scholar]
- Jencks SF, Wilensky GR. The Health Care Quality Improvement Initiative: A New Approach to Quality Assurance in Medicare. Journal of the American Medical Association. 1992 Aug;268(7):900–903. [PubMed] [Google Scholar]
- Jencks SF. Can Large-Scale Interventions Improve Care? Journal of the American Medical Association. 1997 Feb;277(5):419–420. [PubMed] [Google Scholar]
- Krisher J, Pastan S. Promoting Quality of Care for ESRD Patients: The Role of the ESRD Networks. Advances in Renal Replacement Therapy. 2001 Apr;8(2):138–143. doi: 10.1053/jarr.2001.23987. [DOI] [PubMed] [Google Scholar]
- Lohr KN, Schroeder SA. A Strategy for Quality Assurance in Medicare. New England Journal of Medicine. 1990 Mar;332(10):707–712. doi: 10.1056/nejm199003083221031. [DOI] [PubMed] [Google Scholar]
- McClellan WM, Helgerson SD, Frederick PR, et al. Implementing the Health Care Quality Improvement Program in the Medicare ESRD Program A New Era of Quality Improvement in ESRD. Advances in Renal Replacement Therapy. 1995a Apr;2(2):89–94. doi: 10.1016/s1073-4449(12)80078-1. [DOI] [PubMed] [Google Scholar]
- McClellan WM, Frederick PR, Helgerson SD, et al. A Data-Driven Approach to Improving the Care of In-Center Hemodialysis Patients. Health Care Financing Review. 1995b Summer;16(4):129–140. [PMC free article] [PubMed] [Google Scholar]
- McClellan WM. Quality of Patient Care in the Medicare End-Stage Renal Disease Program: The Basis and Implementation of the 1994-1997 End-Stage Renal Disease Health Care Quality Improvement Program. Current Opinion in Nephrology and Hypertension. 1996 May;5(3):224–229. doi: 10.1097/00041552-199605000-00007. [DOI] [PubMed] [Google Scholar]
- McClellan WN, Soucie JM, Krisher J, et al. Improving the Care of Patients Treated with Hemodialysis: A Report from the Health Care Financing Administration's ESRD Core Indicators Project. American Journal of Kidney Diseases. 1998 Apr;31(4):584–592. doi: 10.1053/ajkd.1998.v31.pm9531173. [DOI] [PubMed] [Google Scholar]
- National Kidney Foundation. Kidney Disease Outcomes Quality Initiative 2000 Update, Clinical Practice Guidelines. American Journal of Kidney Diseases. 2001 Jan;37(1) Supplement 1:S1–S235. [Google Scholar]
- Parker TF., III Introduction and Summary Proceedings From the Morbidity, Mortality and Prescription of Dialysis Symposium (1989). Dallas, TX. American Journal of Kidney Diseases. 1990 May;15(5):375–83. [PubMed] [Google Scholar]
- PRO-West. ESRD Special Project Developing Clinical Performance Measures for the Care of Patients with ESRD. 1999 Jan; Internet address: http://www.cms.gov/esrd/l.asp. (Accessed 2003.)
- Renal Physicians Association Working Committee on Clinical Practice Guidelines. Clinical Practice Guideline on Adequacy of Hemodialysis Clinical Practice Guideline Number 1. Renal Physicians Association; Washington, DC.: Dec, 1993. [Google Scholar]
- Rettig RA, Levinsky NG. Kidney Failure and the Federal Government. National Academy Press; Washington, DC.: 1991. [PubMed] [Google Scholar]
- U.S. Renal Data System. USRDS 2001 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. 2001 Sep; Internet address: http://www.usrds.org/adr.htm. (Accessed 2003.)