Abstract
Medicaid spending increased dramatically during the 1990s, driven in part by spending for prescription drugs. From 1990 to 2000, Medicaid drug spending increased from $4.4 billion to over $20 billion, an average annual increase of 16.3 percent. Disabled persons experienced an even greater 20 percent average annual increase. By drug category in 1997 (for 29 States), the highest spending amount was for central nervous system (CNS) drugs, accounting for 17 percent of total Medicaid drug spending. These findings provide information on drug spending for dually eligible beneficiaries to policymakers as they seek to target cost-effective coverage and drug therapies.
Introduction
For many years, there has been continued interest by Federal legislators and policymakers concerning health care for the four major Medicaid eligibility groups: aged, disabled (including blind), children, and adults. In the late 1980s, Congress expanded Medicaid coverage to several of these poverty-related groups. Eligibility expansions for older poverty-related children continued through the 1990s. The BBA of 1997 established the SCHIP to provide health insurance coverage for additional groups of children and adults with incomes above the income limits for Medicaid. The Ticket to Work and Work Incentives Improvement Act of 1999 expanded Medicare and Medicaid for some disabled beneficiaries who return to work. There also has been continued concern about the adequacy of Medicare coverage for disabled and aged enrollees. This concern has led to the enactment of legislation for a Federal Medicare prescription drug benefit and a protracted debate about the cost and financing of such a benefit. These interests must be viewed in the context of continued increases in health care spending for Medicaid recipients at a time when fiscal constraint for State budgets has become paramount.
Medicaid payments have now become a significant proportion of every State's budget. In FY 2000, Medicaid was the largest program to provide health care to poor and near poor Americans, covering over 44 million individuals. In that year, Medicaid spent nearly $206 billion, including $21 billion on outpatient drugs—$16.6 billion under FFS programs and an estimated $4.4 billion in prepaid plans (Bruen, 2002). Bruen used CMS-64 data, net of rebates from drug manufacturers, for 50 States, Washington, DC, and other jurisdictions. He also reported that drug spending represented about 10 percent of total Medicaid spending and 14 percent of total national spending on outpatient drugs. Also, most States experienced greater than 50 percent growth in prescription drug spending from 1997-2000. In a recent survey, 36 States identified prescription drugs as the top Medicaid cost driver in 2001 (Smith and Ellis, 2001). Even though Medicaid coverage of outpatient prescription drugs is optional, all States provide prescription drug coverage for categorically needy beneficiaries. An additional 35 States provide some coverage of prescription drugs for medically needy beneficiaries.
In 2000, Medicaid provided health insurance to more than 44 million beneficiaries—16 percent of the U.S. population; $195.5 billion in Medicaid payments—15 percent of total national health care spending; and nearly $21 billion in Medicaid drug payments—17 percent of total national health care spending for drugs (Levit, 2003; U.S. Bureau of the Census, 2003; Klemm, 2003).
Regarding fiscal constraint, the weak economy that has persisted since the September 11, 2001 attacks has created a severe budget crisis for most States (George Washington University, 2003). Many States are considering major cuts to optional Medicaid eligibility and coverage provisions (Kaiser Commission on Medicaid and the Uninsured, 2002a; Toner and Pear, 2003; Desonia, 2002; and Holahan, Weiner, and Lutzky, 2002). Also, most States are using mechanisms and/or limits to contain prescription drug cost increases (Bruen, 2002). These features include copayment, prior authorization, generic substitution, fail-first provisions, multi-tiered formularies, preferred drug lists, and number of prescription limits.
In a previous article, we indicated that Medicaid prescription drug spending increases were a major factor in overall Medicaid spending increases from 1990-1997 (Baugh, Pine, and Blackwell, 1999). This article provides an update to our previous findings by analyzing Medicaid prescription drug spending for the entire decade of the 1990s (1990-2000). Because virtually all Medicaid aged enrollees and nearly one-half of Medicaid disabled enrollees are enrolled in Medicare, the analysis provides important information on Medicaid prescription drug spending for these groups. Additionally, our analysis includes initial data on Medicaid prescription drug spending when drugs are organized by therapeutic use. This latter approach allows us to begin the process of examining Medicaid utilization and payments based on prescription drug mix. Our findings provide additional information to policymakers as the debate over cost and finance continues.
Methodology
Five data sources were used for this article. Medicaid utilization and spending trends were taken from the HCFA-2082, the CMS-64, and Medicaid Statistical Information System (MSIS) tables (Centers for Medicare & Medicaid Services, 2003). Data on national prescription drug spending were taken from the NHE statistics. Data from the MSIS and the State Medicaid Research Files (SMRFs) were used for analyses to: (1) assess the impact of Medicaid managed care enrollment on prescription drug utilization and payments, (2) analyze Medicaid prescription drug utilization and payments by selected beneficiary characteristics, and (3) present Medicaid prescription drug payments by therapeutic use.
HCFA-2082 and MSIS Tables
The HCFA-2082 form “Statistical Reports on Medical Care: Eligibles, Recipients, Payments and Services” is an annual statistical report, by Federal FY, that is based on State Medicaid data reporting to CMS during the years 1990-1998. Some States submitted summary data directly to CMS and others submitted MSIS person-level enrollment and claims data. For these States, CMS prepared the summary statistics from MSIS data. Beginning in FY 1999, all States were required to submit MSIS data to CMS and HCFA-2082 reporting requirements ended. The Medicaid trend data for 1999 and 2000 were prepared from MSIS data.
CMS-64 Data
The CMS-64 is an accounting statement of actual expenditures made by the States for which they are entitled to receive Federal reimbursement under Title XIX. These CMS-64 statistics are Medicaid payment amounts prior to the collection of rebates from the drug manufacturers.
National Health Expenditures
Annually, CMS' Office of the Actuary estimates national health spending in the United States. The NHE estimates health spending by type of service (e.g., hospital care, physician services, nursing home care, and prescription drugs) according to the sources that pay for these services (e.g., Medicare, Medicaid, private health insurance, and out-of-pocket spending). Estimates are based on information collected from public organizations such as the U.S. Bureau of the Census, CMS, the U.S. Bureau of Labor Statistics, and other Federal and State government agencies that fund medical programs and from private organizations such as the American Hospital Association and the Health Insurance Association of America.
Prescription drug expenditures are limited to retail purchases of these products by consumers. They do not include prescription drugs purchased as part of a hospital stay or directly from a physician since these expenditures are included with either hospital or physician services. Prescription drug spending is based most recently on data from IMS Health, which collects data on pharmacy transactions in different retail outlets. Expenditure estimates for earlier years are based on information collected by the U.S. Bureau of the Census in the Census of Retail Trade services called Merchandise Line Sales. This survey collects data on the value of prescription drug sales from retail outlets such as drugstores and grocery stores (Levit, 1999).
MSIS and SMRF Data
For FY 1998, MSIS data files for 35 States were available to develop estimates of prescription drug utilization and spending for dually eligible beneficiaries by selected characteristics: disabled eligibility, aged eligibility by age group, sex, and beneficiary residence. Data on prescription drug utilization and payments for these States were tabulated by therapeutic use using the latest available SMRF data for 1997 from 29 States.
Analytic Measures
Payments
This is total Medicaid payment for prescription drugs during the CY. Payments are gross dollar amounts prior to the receipt of rebates from drug manufacturers. These Medicaid payments represent all prescription drugs provided under FFS (i.e., prescription drugs for which Medicaid paid a pharmacy claim).
Recipients
This is a count of the number of unique Medicaid beneficiaries who received at least one covered drug during the year. Even if a Medicaid beneficiary was covered under a prepaid plan during the year, and the person received at least one FFS drug, the beneficiary is counted as a drug recipient.
Prescriptions
This is the total number of filled prescriptions, original and refills, for Medicaid beneficiaries during the CY.
Rate Measures
The basic statistics, defined earlier, were used to create two rate measures for drugs: payment per prescription, and payment per recipient.
Eligibility Group
This is the program authority whereby a person receives Medicaid eligibility, known as Medicaid “basis of eligibility” (e.g., aged, blind/disabled, children, and adults).
Age
Attained age as of December 31 of the year is aggregated into 5-year age groups for the aged, as follows: 65-69, 70-74, 75-79, 80-84 and 85 or over.
Sex
Statistics are reported for males and females. Data are omitted for persons for whom sex was unknown.
Beneficiary Residence
The county of residence for each beneficiary was identified as either a metropolitan or non-metropolitan county.
Therapeutic Category of Drugs
Drugs have been categorized by therapeutic category using Medi-Span (Wolters Kluwer Health, 2003).
Data Limitations
These Medicaid data do not capture all drugs provided to Medicaid enrollees. Several factors may result in undercounts of numbers of prescriptions and payments.
Encounter records for prescription drugs provided by prepaid plans are omitted from this analysis because reporting of encounter records is currently incomplete and unreliable. Therefore, data on utilization and payments for prescription drugs are missing for services covered by a prepaid plan. The omission of these data is mitigated, in part, because many beneficiaries who are enrolled in prepaid plans receive some or all of their drugs under FFS systems. The impact of this limitation is discussed later.
The analysis omits prescription drugs provided to Medicaid enrollees during hospital stays and, for a small number of States, during nursing home stays. It also omits over-the-counter drugs provided during nursing home stays for most States. In these instances, drugs are included in the facility reimbursement rate and are not separately identifiable.
Medicaid data do not include out-of-pocket payments that Medicaid enrollees may make for their prescription drugs or third-party payments made by other insurers.
Another factor that affects analysis of these data is program variation across the States. Program choices include optional eligibility groups, coverage of selected prescription drugs, restrictions on prescription drug use, and payment methods. Also, States vary greatly in terms of implementing managed care, including full or partially capitated plans under either section 1915(b) or section 1115 provisions. The effects of these variations are not fully measurable.
External factors may also affect study findings. For example, analyses do not account for major Medicaid policy changes such as welfare reform, economic variables that affect an individual's decision to apply for Medicaid enrollment, and changes in the practice of medicine.
Findings
Prescription Drug Payment Trends
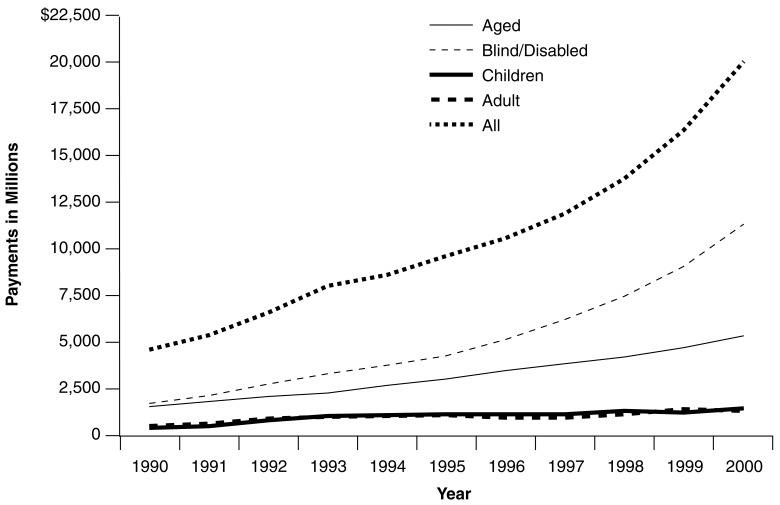
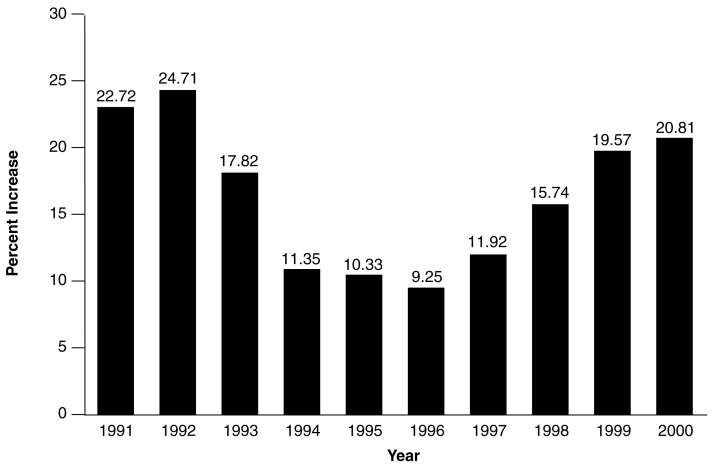
Total Medicaid payments for outpatient prescription drugs grew from $4.4 billion in 1990 to greater than $20 billion in 2000, an average annual increase of 16.3 percent (Figure 1). Large yearly increases were observed in 1991 (22.7 percent) and 1992 (24.7 percent), when the prescription drug rebate program was being implemented (Figure 2). After 1992, annual increases steadily declined through 1996. After 1996, annual increases grew steadily to 20.8 percent by 2000. Data from the CMS-64 confirm that prescription drug spending continued to increase at a high rate in 2001 and 2002 (20.0 and 18.9 percent, respectively).
Figure 1. Medicaid Prescription Drug Payments1, by Eligibility Group2 and Year: Federal FYs 1990-2000.
1 Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers. Medicaid prescription drug payments include all payments for prescription drugs provided under an FFS setting (i.e., prescription drugs for which Medicaid paid a pharmacy claim). Since Medicaid pays a single premium to a prepaid plan for all covered services, it is not possible to identify prescription drug payment when they are covered by a prepaid plan. To this extent, Medicaid prescription drug payments, presented here, may understate total Medicaid payments for prescription drugs. Data are reported for the 50 States and the District of Columbia and exclude other Medicaid jurisdictions. Although Hawaii did not report for 2000, their 1999 data were used as an estimate for 2000.
2 The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
SOURCE: Centers for Medicare & Medicaid Services: Data from CMS Form-2082 and the Medicaid Statistical Information System, 1990-2000.
Figure 2. Medicaid Prescription Drug Payments1, Annual Increase, by Federal FYs: 1991-2000.
1 Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers. Medicaid prescription drug payments include all payments for prescription drugs provided under an FFS setting (i.e., prescription drugs for which Medicaid paid a pharmacy claim). Since Medicaid pays a single premium to a prepaid plan for all covered services, it is not possible to identify prescription drug payment when they are covered by a prepaid plan. To this extent, Medicaid prescription drug payments, presented here, may understate total Medicaid payments for prescription drugs. Data are reported for the 50 States and the District of Columbia and exclude other Medicaid jurisdictions. Although Hawaii did not report for 2000, their 1999 data were used as an estimate for 2000.
SOURCE: Centers for Medicare & Medicaid Services: Data from CMS Form-2082 and the Medicaid Statistical Information System, 1990-2000.
Throughout the decade, disabled persons accounted for the highest Medicaid drug payment amount compared with the other eligibility groups (Figure 1). Drug payments for disabled persons experienced the highest growth over the decade at an average annual rate of 20.1 percent. By 2000, drug spending for the disabled ($11.6 billion) was more than double the amount for the aged ($5.4 billion). In addition, the proportion of total drug spending for the disabled increased from 42 percent in 1990 to 58 percent in 2000.
During the 1990s, Medicaid drug payments for the aged increased from $1.5 billion to $5.4 billion, an annual average increase of 13.5 percent. Together, the aged and disabled represented 85 percent of total Medicaid prescription drug spending in 2000. While Medicaid prescription drug spending levels were much lower for children ($1.6 billion) and adults ($1.4 billion) in 2000, spending for these two groups also increased in the 1990s. The average annual rate of increased Medicaid drug spending during the decade was 13.4 percent for children and 9.7 percent for adults. Between 1999-2000, drug payments increased sharply for each of the eligibility groups: aged (17.5 percent), disabled (23.0 percent), children (19.4 percent), and adults (21.5 percent).
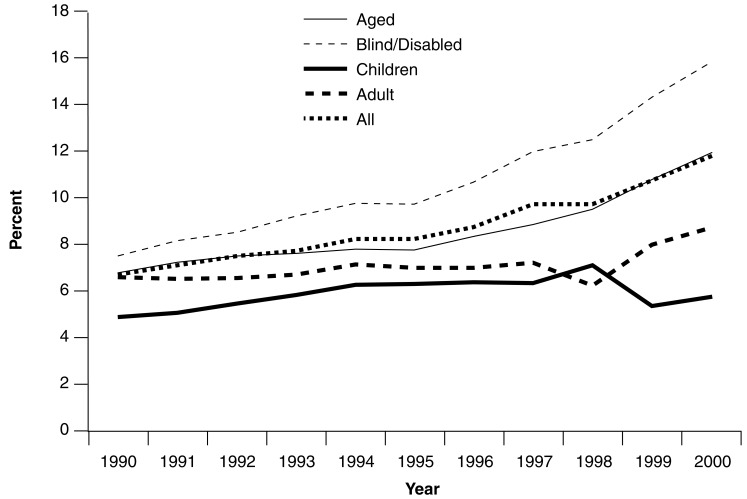
Figure 3 shows Medicaid prescription drug payments as a percent of total Medicaid payments during the decade. For all beneficiaries, prescription drug payments increased from 6.8 percent (1990) to 11.9 percent (2000) of total payments. Similarly, drug payments increased from 7.0 to 12.0 percent of total payments for the aged over these years. Drug payments for the disabled rose from 7.6 percent (1990) to 15.9 percent (2000) of total payments. The increase for adults was less dramatic. In 1990, drug payments represented 6.7 percent of total Medicaid spending for adults and, by 2000, drug payments rose to 8.1 percent of total payments for adults. From 1990 to 1996, prescription drugs were a steadily increasing percent of total Medicaid spending for children. However, there were intermittent increases and decreases after 1996. This finding may reflect the fact that many Medicaid children were being enrolled in prepaid plans in the late 1990s.
Figure 3. Medicaid Prescription Drug Payments1 as a Percent of Total Medicaid Payments, by Eligibility Group2: Federal FYs 1990-2000.
1 Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers. Medicaid prescription drug payments include all payments for prescription drugs provided under an FFS setting (i.e., prescription drugs for which Medicaid paid a pharmacy claim). Since Medicaid pays a single premium to a prepaid plan for all covered services, it is not possible to identify prescription drug payments when they are covered by a prepaid plan. To this extent, Medicaid prescription drug payments, presented here, may understate total Medicaid payments for prescription drugs. Data are reported for the 50 States and the District of Columbia and exclude other Medicaid jurisdictions. Although Hawaii did not report for 2000, their 1999 data were used as an estimate for 2000.
2 The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
SOURCE: Centers for Medicare & Medicaid Services: Data from CMS Form-2082 and the Medicaid Statistical Information System, 1990-2000.
Table 1 presents Medicaid prescription drug payments by State and eligibility group. Together, California ($2.3 billion) and New York ($2.4 billion) represented over 23 percent of total Medicaid drug spending in 2000. In addition, Florida and Texas spent over $1 billion each on Medicaid prescription drugs in 2000. In New York, prescription drugs payments for disabled individuals doubled from $685 million in 1997 to $1.4 billion in 2000.
Table 1. Medicaid Prescription Drug Payment, by State and Eligibility Group1: FY 2000.
| State3 | Medicaid Eligibility Group2 | ||||
|---|---|---|---|---|---|
|
| |||||
| Aged | Blind/Disabled | Children | Adult | All | |
|
| |||||
| Payments (In Millions) | |||||
| Total4 | $5,338.4 | $11,561.2 | $1,562.3 | $1,443.8 | $19,967.0 |
| Alabama | 74.1 | 211.6 | 39.4 | 8.9 | 331.6 |
| Alaska | 9.6 | 28.0 | 5.8 | 7.7 | 51.2 |
| Arizona5 | — | — | — | — | — |
| Arkansas | 59.5 | 115.7 | 25.9 | 8.6 | 209.9 |
| California | 572.1 | 1,506.5 | 91.7 | 140.4 | 2,316.1 |
| Colorado | 54.9 | 80.4 | 11.0 | 6.1 | 152.5 |
| Connecticut | 98.3 | 160.9 | 3.1 | 1.9 | 264.6 |
| Delaware | 10.4 | 29.7 | 6.8 | 19.3 | 66.3 |
| District of Columbia | 7.8 | 42.7 | 2.3 | 2.0 | 55.1 |
| Florida | 310.8 | 902.3 | 84.6 | 66.4 | 1,366.2 |
| Georgia | 138.5 | 326.4 | 68.8 | 38.7 | 580.6 |
| Hawaii5 | — | — | — | — | — |
| Idaho | 20.5 | 49.4 | 7.9 | 5.6 | 83.5 |
| Illinois | 162.7 | 522.1 | 81.5 | 75.5 | 847.0 |
| Indiana | 157.5 | 231.9 | 53.4 | 22.3 | 465.0 |
| Iowa | 63.7 | 99.4 | 18.6 | 13.7 | 193.8 |
| Kansas | 53.8 | 90.7 | 15.4 | 5.6 | 167.2 |
| Kentucky | 101.7 | 299.9 | 38.4 | 25.0 | 465.2 |
| Louisiana | 162.0 | 226.8 | 60.9 | 21.2 | 476.4 |
| Maine | 39.6 | 106.3 | 14.2 | 14.3 | 175.9 |
| Maryland | 77.0 | 221.7 | 44.5 | 26.0 | 374.1 |
| Massachusetts | 132.4 | 437.3 | 36.1 | 75.2 | 682.5 |
| Michigan | 118.4 | 222.4 | 19.4 | 13.7 | 374.3 |
| Minnesota | 37.7 | 166.2 | 10.3 | 7.1 | 221.7 |
| Mississippi | 110.2 | 215.5 | 32.5 | 12.0 | 370.4 |
| Missouri | 195.0 | 334.5 | 43.7 | 26.9 | 600.5 |
| Montana | 15.5 | 31.7 | 4.9 | 6.3 | 58.6 |
| Nebraska | 41.6 | 60.9 | 20.9 | 12.0 | 135.4 |
| Nevada | 15.1 | 31.9 | 3.0 | 1.4 | 51.7 |
| New Hampshire | 24.7 | 37.6 | 10.7 | 7.5 | 80.6 |
| New Jersey | 155.5 | 371.1 | 12.8 | 41.9 | 584.5 |
| New Mexico | 16.9 | 28.6 | 1.5 | 1.6 | 57.5 |
| New York | 417.8 | 1,416.7 | 144.6 | 386.1 | 2,366.9 |
| North Carolina | 287.0 | 380.4 | 71.3 | 54.8 | 794.6 |
| North Dakota | 15.4 | 16.6 | 3.1 | 3.0 | 38.1 |
| Ohio | 272.1 | 519.4 | 52.6 | 38.0 | 882.6 |
| Oklahoma | 77.5 | 73.2 | 21.0 | 5.8 | 178.3 |
| Oregon | 38.9 | 86.1 | 6.4 | 31.7 | 163.3 |
| Pennsylvania | 207.5 | 270.4 | 34.4 | 20.6 | 533.5 |
| Rhode Island | 26.4 | 61.4 | 1.3 | 0.4 | 89.5 |
| South Carolina | 98.5 | 170.9 | 42.5 | 22.6 | 334.7 |
| South Dakota | 14.3 | 22.8 | 5.2 | 2.3 | 44.7 |
| Tennessee5 | — | — | — | — | — |
| Texas | 407.0 | 429.2 | 207.9 | 78.3 | 1,125.2 |
| Utah | 19.4 | 58.0 | 11.8 | 12.7 | 100.8 |
| Vermont | 30.0 | 41.5 | 7.8 | 11.7 | 91.7 |
| Virginia | 130.0 | 198.2 | 37.1 | 16.4 | 382.5 |
| Washington | 109.4 | 253.9 | 9.1 | 12.7 | 387.9 |
| West Virginia | 45.1 | 128.1 | 23.6 | 17.6 | 216.1 |
| Wisconsin | 97.7 | 229.4 | 9.5 | 12.3 | 349.6 |
| Wyoming | 7.0 | 14.5 | 3.6 | 2.1 | 27.2 |
Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers. Medicaid prescription drug payments include all payments for prescription drugs provided under an FFS setting (i.e., prescription drugs for which Medicaid paid a pharmacy claim). Because Medicaid pays a single premium to a prepaid plan for all covered services, it is not possible to identify prescription drug payments when they are covered by a prepaid plan. To this extent, Medicaid prescription drug payments may understate total Medicaid payments for prescription drugs.
The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
Most States had comprehensive prepaid care plans covering at least some State beneficiaries as of June 2000. The States that did not were Alaska, Arkansas, Idaho, Louisiana, Maine, Mississippi, Nebraska, Nevada, North Dakota, South Carolina, South Dakota, West Virginia, and Wyoming.
This is the total for the 47 States and the District of Columbia presented here.
Data are not reported for these States because substantial numbers of State beneficiaries were covered under prepaid plans.
SOURCE: Centers for Medicare & Medicaid Services: Data from the Medicaid Statistical Information System, 2003.
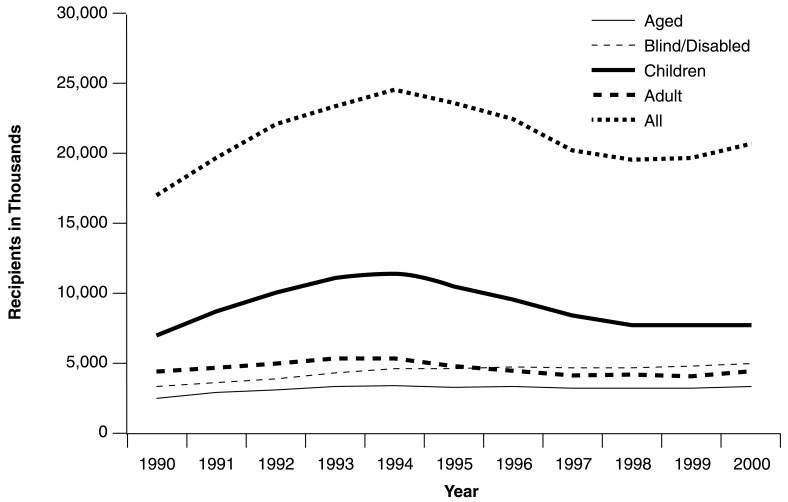
Prescription Drug Recipient Trends
From 1990 to 1994, the number of Medicaid prescription drug recipients increased steadily from 17.3 to 24.4 million (Figure 4). Then, the number decreased to 19.6 million by 1998. After 1998, the numbers began to increase again, reaching 20.5 million in 2000. Recipient trends for aged, adult, and child beneficiaries followed this same pattern during the 1990s. However, the numbers of disabled prescription drug recipients grew more consistently during the decade, with only small declines in 1997 and 1998. As a result, the disabled increased from 17.5 percent (1990) to 24.4 percent (2000) of total drug recipients. Each of the other three groups represented a smaller percent of total drug recipients in 2000 than they did in 1990. Overall, the number of Medicaid drug recipients increased by an annual average of 1.7 percent per year. This statistic ranged from a high of just over 5 percent for the disabled to a 0.2-percent decline for adults. Recipient trends could be affected by many factors, such as health of the economy and enrollment in prepaid plans.
Figure 4. Medicaid Prescription Drug Recipients1, by Eligibility Group2 Federal FYs: 1990-2000.
1 A Medicaid prescription drug recipient is a Medicaid enrollee who received at least one covered prescription drug during the FY. If an enrollee was covered under a prepaid plan, providing either partial or comprehensive coverage during the year, and had at least one FFS claim for a prescription drug during the FY, that enrollee is counted both as a recipient and a prescription drug recipient. Otherwise, enrollees covered under prepaid plans are excluded from recipient counts because it is not possible to identify the plan enrollees who received Medicaid covered services. Therefore, these data may understate the number of recipients and prescription drug recipients. Data are reported for the 50 States and the District of Columbia and exclude other Medicaid jurisdictions. Although Hawaii did not report for 2000, their 1999 data were used as an estimate for 2000.
2 The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
SOURCE: Centers for Medicare & Medicaid Services: Data from CMS Form-2082 and the Medicaid Statistical Information System, 1990-2000.
Medicaid prescription drug recipients, by State, are presented in Table 2 for 2000. The largest number of prescription drug recipients nationally was children (8.3 million), greater than the number of disabled (5.0 million), more than double the number of adults (4.0 million), and nearly three times the number of aged (2.9 million). California had fewer children as drug recipients than adults. Both Texas and New York had larger numbers of children who received prescription drugs than California. This finding could be a result of enrollment of children in prepaid plans in California. In addition, this finding is largely responsible for the observed decline in national totals between 1997-2000. Otherwise, California had the largest number of aged, disabled, and adult prescription drug recipients.
Table 2. Medicaid Prescription Drug Recipient, by State and Eligibility Group1: FY 2000.
| State3 | Medicaid Eligibility Group2 | ||||
|---|---|---|---|---|---|
|
| |||||
| Aged | Blind/Disabled | Children | Adult | All | |
|
| |||||
| Prescription Drug Recipients (in Thousands) | |||||
| Total4 | 2,872.9 | 4,990.8 | 8,314.1 | 3,957.5 | 20,474.2 |
| Alabama | 46.2 | 131.6 | 221.9 | 36.3 | 438.5 |
| Alaska | 5.1 | 8.9 | 29.8 | 16.1 | 60.3 |
| Arizona5 | — | — | — | — | — |
| Arkansas | 35.8 | 75.6 | 140.8 | 37.6 | 290.7 |
| California | 393.6 | 643.0 | 631.6 | 714.6 | 2,487.9 |
| Colorado | 30.5 | 35.1 | 58.8 | 27.7 | 160.3 |
| Connecticut | 46.0 | 48.5 | 9.9 | 6.9 | 113.1 |
| Delaware | 5.2 | 11.8 | 34.3 | 26.6 | 78.2 |
| District of Columbia | 5.1 | 18.7 | 8.4 | 5.6 | 38.1 |
| Florida | 158.6 | 290.0 | 418.6 | 192.8 | 1,072.1 |
| Georgia | 76.5 | 176.1 | 407.6 | 148.3 | 847.7 |
| Hawaii5 | — | — | — | — | — |
| Idaho | 9.0 | 18.6 | 50.0 | 14.4 | 92.8 |
| Illinois | 82.0 | 216.2 | 489.7 | 218.5 | 1,013.3 |
| Indiana | 58.4 | 74.9 | 216.2 | 66.1 | 420.0 |
| Iowa | 32.2 | 44.3 | 91.1 | 42.4 | 212.2 |
| Kansas | 24.2 | 39.0 | 70.4 | 21.2 | 158.3 |
| Kentucky | 42.1 | 139.9 | 185.1 | 56.5 | 427.5 |
| Louisiana | 71.6 | 126.2 | 284.7 | 68.7 | 581.4 |
| Maine | 18.9 | 41.3 | 59.0 | 26.5 | 148.0 |
| Maryland | 40.8 | 85.5 | 204.1 | 63.8 | 409.5 |
| Massachusetts | 83.4 | 187.6 | 220.1 | 171.8 | 666.6 |
| Michigan | 75.4 | 151.4 | 121.1 | 80.0 | 435.7 |
| Minnesota | 26.7 | 68.7 | 51.4 | 30.8 | 180.1 |
| Mississippi | 60.0 | 125.5 | 184.3 | 45.1 | 415.9 |
| Missouri | 81.2 | 111.3 | 167.6 | 82.7 | 447.1 |
| Montana | 8.1 | 13.3 | 25.4 | 11.5 | 58.9 |
| Nebraska | 19.8 | 24.1 | 92.3 | 29.0 | 165.9 |
| Nevada | 9.4 | 16.9 | 15.0 | 7.7 | 51.2 |
| New Hampshire | 11.0 | 11.6 | 39.5 | 10.9 | 73.3 |
| New Jersey | 77.5 | 125.3 | 52.8 | 38.1 | 298.5 |
| New Mexico | 11.6 | 16.2 | 23.2 | 15.8 | 67.2 |
| New York | 237.1 | 533.7 | 844.4 | 549.5 | 2,173.8 |
| North Carolina | 141.9 | 174.8 | 367.6 | 138.1 | 827.0 |
| North Dakota | 7.7 | 7.1 | 16.6 | 7.3 | 39.0 |
| Ohio | 120.3 | 213.9 | 317.1 | 119.2 | 777.6 |
| Oklahoma | 46.0 | 43.5 | 101.0 | 29.9 | 222.0 |
| Oregon | 26.7 | 40.0 | 44.6 | 79.1 | 191.9 |
| Pennsylvania | 92.6 | 112.5 | 161.2 | 47.3 | 416.5 |
| Rhode Island | 15.0 | 26.9 | 4.9 | 2.9 | 49.8 |
| South Carolina | 63.0 | 96.3 | 234.5 | 78.7 | 474.5 |
| South Dakota | 7.1 | 10.1 | 28.4 | 7.8 | 53.7 |
| Tennessee5 | — | — | — | — | — |
| Texas | 244.7 | 259.4 | 1,040.9 | 295.8 | 1,852.8 |
| Vermont | 16.3 | 15.6 | 40.5 | 29.1 | 103.2 |
| Virginia | 62.9 | 78.6 | 153.0 | 48.3 | 347.3 |
| Washington | 58.2 | 101.3 | 86.1 | 77.8 | 339.4 |
| West Virginia | 23.3 | 70.5 | 120.9 | 44.7 | 261.5 |
| Wisconsin | 51.2 | 102.6 | 58.7 | 51.1 | 267.4 |
| Wyoming | 3.2 | 5.9 | 17.5 | 6.5 | 33.3 |
A Medicaid prescription drug recipient is a Medicaid enrollee who received at least one covered prescription drug during the FY. If an enrollee was covered under a prepaid plan, providing either partial or comprehensive coverage during the year, and had at least one FFS claim for a prescription drug during the FY, that enrollee is counted both as a recipient and a prescription drug recipient. Otherwise, enrollees covered under prepaid plans are excluded from recipient counts because it is not possible to identify the plan enrollees who received Medicaid covered services. Therefore, these data may understate the number of recipients and prescription drug recipients.
The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
Most States had comprehensive prepaid care plans covering at least some State beneficiaries as of June 2000.The States that did not were Alaska, Arkansas, Idaho, Louisiana, Maine, Mississippi, Nebraska, Nevada, North Dakota, South Carolina, South Dakota, West Virginia, and Wyoming.
This is the total for the 47 States and the District of Columbia presented here.
Data are not reported for these States because substantial numbers of State beneficiaries were covered under prepaid plans.
SOURCE: Centers for Medicare & Medicaid Services: Data from the Medicaid Statistical Information System, 2003.
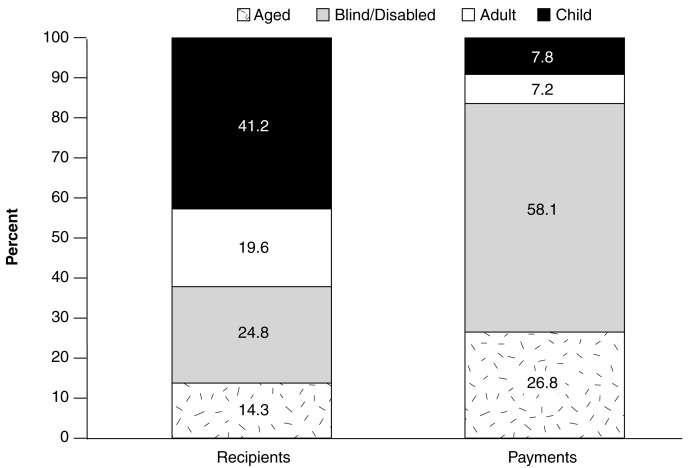
Figure 5 compares the percent of total Medicaid prescription drug recipients with the percent of total Medicaid prescription drug payments for each eligibility group in 2000. Together, children and adults were 60.8 percent of total prescription drug recipients, but they accounted for only 15.0 percent of prescription drug payments. In contrast, the disabled were less than 25 percent of total prescription drug recipients, but they accounted for over 58 percent of prescription drug payments. Similarly, the aged were 14 percent of total prescription drug recipients and represented nearly 27 percent of total prescription drug payments. In comparison to the data we presented for 1997, the percent of total drug recipients and payments for the disabled has increased between 1997-2000. Aged and disabled beneficiaries have higher utilization of inpatient hospital and nursing facility services than adults and children. If it were possible to separate the cost of these drugs from other institutional services, the differences observed would be even larger.
Figure 5. Percent of Total Medicaid Prescription Drug Recipients1 and Payments2 by Eligibility Group3: Federal FY 2000.
1 A Medicaid prescription drug recipient is a Medicaid enrollee who received at least one covered prescription drug during the FY. If an enrollee was covered under a prepaid plan, providing either partial or comprehensive coverage during the year, and had at least one FFS claim for a prescription drug during the FY, that enrollee is counted both as a recipient and a prescription drug recipient. Otherwise, enrollees covered under prepaid plans are excluded from recipient counts because it is not possible to identify the plan enrollees who received Medicaid-covered services. Therefore, these data may understate the number of recipients and prescription drug recipients. Data are reported for the 50 States and the District of Columbia and exclude other Medicaid jurisdictions. Although Hawaii did not report for 2000, their 1999 data were used as an estimate for 2000.
2 Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers. Medicaid prescription drug payments include all payments for prescription drugs provided under an FFS setting (i.e., prescription drugs for which Medicaid paid a pharmacy claim). Since Medicaid pays a single premium to a prepaid plan for all covered services, it is not possible to identify prescription drug payment when they are covered by a prepaid plan. To this extent, Medicaid prescription drug payments presented here may understate total Medicaid payments for prescription drugs.
3 The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. A small number of individuals that are not reported in these four groups have been excluded.
SOURCE: Centers for Medicare & Medicaid Services: Data from CMS Form-2082 and the Medicaid Statistical Information System, 2000.
Prescription Drug Payment Per Recipient Trends
Between 1990-2000, prescription drug payment per recipient grew from $256 to $975 (data not shown), an annual average increase of 14.3 percent. This increase in the payment rate is lower than the 16.3 percent average annual increase in total Medicaid payments during the decade. This is because there was a small average annual increase of 1.7 percent in the number of drug recipients over this time period.
The overall payment per recipient masked wide variations across eligibility groups. Spending per recipient for prescription drugs was higher throughout the decade for the disabled than for the other eligibility groups. In 1990, payment per recipient was only 6 percent higher for the disabled ($617) than for the aged ($582). By 2000, the difference was nearly 25 percent ($2,314 for the disabled versus $1,853 for the aged). In 1990, payment per recipient for the disabled was 10 times the amount for children ($617 for the disabled versus $61 for children). By 2000, spending for the disabled was 12 times the amount for children ($2,314 for the disabled versus $188 for children). Similarly, spending for the disabled increased from 4.4 times the amount for adults in 1990 to 5.8 times the amount for adults in 2000.
The same general patterns in payment per recipient by eligibility group that were observed in the national data for 2000 also persisted in data for individual States (Table 3). However, there were variations across States. Payment per aged recipient ranged from $1,414 in Minnesota to $2,695 in Indiana. For the disabled, the variation was greater, ranging from $1,469 in Michigan to $3,314 in Connecticut. Because payment per recipient was much lower for children and adults, the variation across States in payment for these groups was much smaller. State differences can be attributed to many factors, including enrollment in prepaid plans and controls on drug utilization.
Table 3. Medicaid Prescription Drug Payment Per Recipient, by State and Eligibility Group1: FY 2000.
| State3 | Medicaid Eligibility Group2 | ||||
|---|---|---|---|---|---|
|
| |||||
| Aged | Blind/Disabled | Children | Adult | All | |
|
| |||||
| Payment Per Drug Recipient | |||||
| Total4 | $1,858 | $2,316 | $188 | $365 | $975 |
| Alabama | 1,603 | 1,608 | 177 | 246 | 756 |
| Alaska | 1,869 | 3,139 | 193 | 478 | 849 |
| Arizona5 | — | — | — | — | — |
| Arkansas | 1,661 | 1,531 | 184 | 229 | 722 |
| California | 1,453 | 2,343 | 145 | 196 | 931 |
| Colorado | 1,800 | 2,290 | 186 | 221 | 951 |
| Connecticut | 2,138 | 3,314 | 310 | 275 | 2,340 |
| Delaware | 2,026 | 2,510 | 198 | 724 | 848 |
| District of Columbia | 1,535 | 2,284 | 277 | 359 | 1,445 |
| Florida | 1,960 | 3,111 | 202 | 344 | 1,274 |
| Georgia | 1,811 | 1,853 | 169 | 261 | 685 |
| Hawaii5 | — | — | — | — | — |
| Idaho | 2,285 | 2,649 | 157 | 392 | 900 |
| Illinois | 1,983 | 2,415 | 166 | 346 | 836 |
| Indiana | 2,695 | 3,096 | 247 | 337 | 1,107 |
| Iowa | 1,976 | 2,242 | 204 | 323 | 914 |
| Kansas | 2,218 | 2,326 | 219 | 265 | 1,056 |
| Kentucky | 2,413 | 2,144 | 207 | 442 | 1,088 |
| Louisiana | 2,262 | 1,796 | 214 | 308 | 819 |
| Maine | 2,091 | 2,572 | 240 | 541 | 1,188 |
| Maryland | 1,889 | 2,594 | 218 | 407 | 914 |
| Massachusetts | 1,587 | 2,331 | 164 | 438 | 1,024 |
| Michigan | 1,571 | 1,469 | 160 | 172 | 859 |
| Minnesota | 1,414 | 2,419 | 201 | 230 | 1,231 |
| Mississippi | 1,836 | 1,717 | 176 | 266 | 890 |
| Missouri | 2,401 | 3,005 | 261 | 325 | 1,343 |
| Montana | 1,911 | 2,379 | 193 | 550 | 996 |
| Nebraska | 2,107 | 2,532 | 227 | 414 | 816 |
| Nevada | 1,595 | 1,889 | 197 | 185 | 1,010 |
| New Hampshire | 2,252 | 3,251 | 270 | 692 | 1,099 |
| New Jersey | 2,006 | 2,961 | 243 | 1,100 | 1,959 |
| New Mexico | 1,464 | 1,767 | 63 | 99 | 855 |
| New York | 1,762 | 2,655 | 171 | 703 | 1,089 |
| North Carolina | 2,022 | 2,176 | 194 | 397 | 961 |
| North Dakota | 2,012 | 2,321 | 187 | 403 | 977 |
| Ohio | 2,262 | 2,428 | 166 | 319 | 1,135 |
| Oklahoma | 1,686 | 1,684 | 208 | 195 | 803 |
| Oregon | 1,457 | 2,153 | 143 | 400 | 851 |
| Pennsylvania | 2,240 | 2,404 | 213 | 436 | 1,281 |
| Rhode Island | 1,761 | 2,283 | 256 | 155 | 1,797 |
| South Carolina | 1,564 | 1,775 | 181 | 287 | 706 |
| South Dakota | 2,001 | 2,254 | 183 | 292 | 832 |
| Tennessee5 | — | — | — | — | — |
| Texas | 1,663 | 1,655 | 200 | 265 | 607 |
| Utah | 1,992 | 2,790 | 166 | 419 | 757 |
| Vermont | 1,844 | 2,653 | 193 | 401 | 889 |
| Virginia | 2,065 | 2,520 | 242 | 340 | 1,101 |
| Washington | 1,878 | 2,507 | 105 | 163 | 1,143 |
| West Virginia | 1,940 | 1,817 | 195 | 394 | 826 |
| Wisconsin | 1,908 | 2,237 | 162 | 240 | 1,307 |
| Wyoming | 2,170 | 2,481 | 205 | 321 | 817 |
Medicaid prescription drug payment per recipient is defined to be Medicaid payments for prescription drugs divided by the number of Medicaid enrollees who received at least one covered prescription drug during the FY. A consistent approach has been taken to define the numerator and denominator of this statistic. A Medicaid enrollee is represented in the payment amount (in the numerator) and as a prescription drug recipient (in the denominator) if and only if there was a FFS claim for a prescription drug for that person. Medicaid prescription drug payments are gross amounts prior to the receipt of rebates to the States by prescription drug manufacturers.
The Medicaid eligibility group identifies the basis on which Medicaid eligibility was determined, regardless of cash assistance status. The blind/disabled group includes individuals of any age who were determined to be eligible because of disability. The children's group includes foster care children. The all group includes a small number of individuals that are not reported in the other four groups.
Most States had comprehensive prepaid care plans covering at least some State beneficiaries, as of June 2000.The States that did not were Alaska, Arkansas, Idaho, Louisiana, Maine, Mississippi, Nebraska, Nevada, North Dakota, South Carolina, South Dakota, West Virginia, and Wyoming.
This is the total for the 47 States and the District of Columbia presented here.
Data are not reported for these States because substantial numbers of State beneficiaries were covered under prepaid plans.
SOURCE: Centers for Medicare & Medicaid Services: Data from the Medicaid Statistical Information System, 2003.
In order to gain a better understanding of Medicaid drug spending increases presented here, it is important to develop a knowledge of Medicaid drug spending: (1) variations by selected beneficiary characteristics, (2) levels by therapeutic usage, and (3) in comparison to spending increases for drugs by other payers (e.g., public, private, and beneficiaries out-of-pocket). The next three sections are an introduction to these issues.
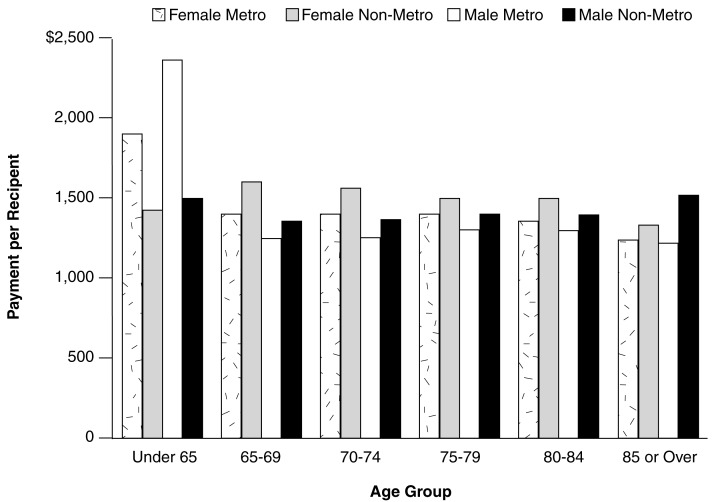
Differences for Dually Eligible Persons
Because of the ongoing interest in the cost of drugs for Medicare beneficiaries, analysis of FY 1998 data for dually eligible beneficiaries was performed. Medicaid prescription drug payments per recipient are presented by selected demographic characteristics for dually aged and disabled beneficiaries (Figure 6). There was no substantial variation in payment amounts among aged beneficiaries, by sex and age group, except that there was a slight decline in payments for persons age 85 or over. Similarly, payment per recipient for dually disabled beneficiaries residing in non-metropolitan areas was comparable to that of aged beneficiaries. However, payment per recipient for both male and female disabled beneficiaries in metropolitan areas was much higher than for that of the other groups.
Figure 6. Medicaid Prescription Drug Payment per Dual Recipient1, by Selected Beneficiary Characteristics2: Federal FY 1998.
1 Medicaid prescription drug payment per recipient is defined to be Medicaid payments for prescription drugs divided by the number of Medicaid enrollees who received at least one covered prescription drug during the FY. A consistent approach has been taken to define the numerator and denominator of this statistic. A Medicaid enrollee is represented in the payment amount (in the numerator) and as a prescription drug recipient (in the denominator) if and only if there was a FFS claim for a prescription drug for that person. Dual recipients are those Medicaid eligibles who were also eligible to receive Medicare benefits.
2 These data are reported for Medicaid beneficiaries who were also enrolled in Medicare (otherwise known as dually eligible enrollees). Beneficiaries were identified as residing in a metropolitan or non-metropolitan area based on their county of residence.
NOTE: For FY 1998, participation in MSIS was voluntary. Of the 38 States that participated, there were consistent data for 35 States to produce these statistics.
SOURCE: Centers for Medicare & Medicaid Services: Data from the Medicaid Statistical Information System, 2003.
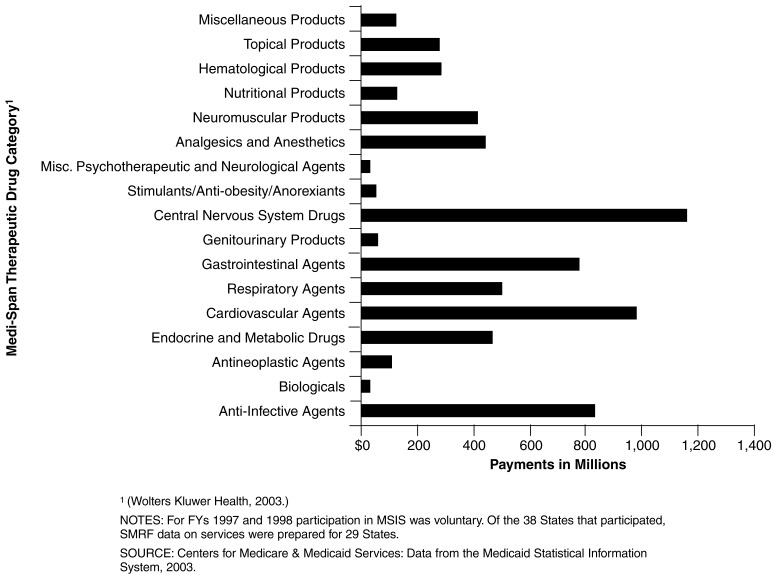
Differences by Drug Therapeutic Category
Because States are faced with the challenge of managing drug expenditures under extreme budget pressure, there is a need to examine variations more closely by therapeutic use.
Figure 7 presents Medicaid prescription drug payments for the SMRF States, by therapeutic category. Among the 17 categories, the highest spending, by category, was for CNS drugs. This category includes anxiolytics, antidepressants, antipsychotics, and hypnotics. In 1997, CNS drugs represented nearly $1.16 billion or greater than 17 percent of total Medicaid spending for prescription drugs in the 29 States. The second highest spending level was for cardiovascular agents (which include calcium channel blockers, beta blockers, and ACE inhibitors) at $982 million (14.7 percent). Cardiovascular agents were followed by anti-infective agents at $835 million (12.5 percent) and gastrointestinal agents at $785 million (11.8 percent). A large proportion of total drug spending (over 56 percent) was concentrated in these four categories. The five categories with the lowest spending levels (miscellaneous psychotherapeutic and neurological agents, stimulants/anti-obesity/anorexiants, genitourinary products, antineoplastic agents, and biologicals) accounted for only 4 percent of total prescription drug spending. However, spending levels differed by eligibility group. The highest spending level for disabled beneficiaries was for CNS drugs. For the aged, cardiovascular agents accounted for the highest amount. For children and adults, the highest spending level was for anti-infective agents (data not shown).
Figure 7. Medicaid Prescription Drug Payments, All Beneficiaries, by Drug Category: CY1997.
There were nearly 197 million prescriptions filled in these States in 1997. The largest number of prescriptions was filled for cardiovascular agents (over 33 million or 17 percent of the total). There were also large numbers of prescriptions filled for CNS drugs, analgesics and anesthetics, anti-infective agents, and respiratory agents. Drugs from these five categories were 63 percent of all filled prescriptions. Five categories (miscellaneous products, miscellaneous psychotherapeutic and neurological agents, stimulants/anti-obesity/anorexiants, antineoplastic agents, and biologicals) had small numbers of filled prescriptions, representing just over 2 percent of total prescriptions. By eligibility group, the most frequently filled prescriptions were: cardiovascular agents for the aged, CNS drugs for the disabled, analgesics and anesthetics for adults, and anti-infective agents for children (data not shown).
Payment per prescription varied between $24 (respiratory agents) and $67 (miscellaneous products). However, payment per prescription was much higher for biologicals ($270) and antineoplastic agents ($172). This same pattern held for the disabled, children, and adults. However, the highest payment per prescription for the aged was for antineoplastic agents ($118) followed by miscellaneous psychotherapeutic and neurological agents ($70) (data not shown).
Differences Among Types of Payers
It is important to note that both private and public payers are experiencing large increases in drug spending. One reason for high spending growth in the late 1990s was a wave of new “blockbuster drugs” entering the market (Levit et al., 2003). Prescription drug payments for all payers increased by nearly 12 percent per year between 1990 and 2000. However, there were major differences for different types of payers. Out-of-pocket payments increased by an annual average of just over 5 percent while third-party payments increased by over 17 percent annually. Among third-party payers, private insurers accounted for an average annual increase of greater than 19 percent while spending in public programs increased by nearly 15 percent per year. Among public programs, the average annual increase for Medicaid, 15.2 percent, exceeded that of other public programs, 13.3 percent (data not shown).
Impact of Medicaid Managed Care Enrollment
An important concern in examining Medicaid utilization and spending trends is the extent of beneficiary enrollment in prepaid plans, either comprehensive plans (e.g., HMOs) or limited plans (e.g., prepaid health plans). This is because a complete and accurate record of services may not be available for these beneficiaries. It should be noted that care delivered through primary care case management is managed care, but services are usually reimbursed on a FFS basis.
Claims data capture FFS prescription drugs provided to Medicaid beneficiaries, including drugs for persons who were in: (1) FFS throughout the year, (2) FFS for part of the year, but who were enrolled in a prepaid plan during their last eligible month in the year, (3) a prepaid health plan, but some or all of their prescription drugs were “carved out” of the plan, and (4) primary care case management. Data from the 29 SMRF States were examined to estimate the impact of managed care on the findings reported here. For these States, the percent of beneficiaries who were enrolled in prepaid plans and received FFS drugs was 67 percent in 1998. There was great variation by State: 9 States above 98 percent, 11 States between 98 and 70 percent, and 9 States below 70 percent, including the lowest State, New Mexico, at 43 percent.
By eligibility group, the percentages in 1998 were much higher for aged and disabled beneficiaries (88 and 83 percent, respectively) compared with children and adults (59 and 64 percent, respectively) (data not shown). Although these study findings are for drugs provided under FFS only, the effect of missing data for services delivered by prepaid plans is much less serious than suggested by other sources (Health Care Financing Administration, 1998).
Summary of Findings
The following findings from this study are highlighted here:
Medicaid prescription drug payments grew from $4.4 billion in 1990 to greater than $20 billion in 2000, with an average annual rate of growth of 16.3 percent. Because drug payment increases after 1997 were larger than those in the mid-1990s, the average annual rate of growth for the decade was larger than the previously reported average annual rate from 1990-1997. During the decade, Medicaid prescription drug payments for disabled beneficiaries grew at an average annual rate of over 20 percent. Two States, California and New York, together, represented 23 percent of national Medicaid prescription drug spending in 2000.
The steady decline in Medicaid prescription drug recipients (excluding persons in comprehensive prepaid plans) reached a low of 19.8 million beneficiaries in 1998. There were slight increases in the number of prescription drug beneficiaries in 1999 and 2000. This pattern was observed for adults, children, and aged beneficiaries. However, the number of disabled prescription drug recipients grew more consistently in the decade, with only small declines in 1997 and 1998. California had the largest number of aged, disabled, and adult prescription drug recipients. While two other States had larger numbers of children who received prescription drugs than California, this finding could be the result of a proportionally larger enrollment of children in prepaid plans in California.
Payment per drug recipient grew during the decade from $256 in 1990 to $975 in 2000. Annual increases were larger beginning in 1994, exceeding 13 percent in each of those years, peaking at nearly 24 percent in 1998 (data not shown). In contrast, annual increases were below 11 percent before 1994. Spending per recipient for prescription drugs was higher throughout the decade for the disabled than for other eligibility groups. However, the difference widened during the 1990s. In 1990, prescription drug spending per recipient for the disabled was 6 percent greater than for the aged. By 2000, spending for the disabled was nearly 25 percent greater. Drug spending for the disabled was also increased from 10 to 12 times the amount for children and from 4.4 to 5.8 times the amount for adults.
In FY 1998, drug payment per recipient for dually aged and disabled beneficiaries did not vary significantly by age or sex, but were much higher for both male and female disabled beneficiaries who lived in metropolitan areas. It is unclear what factor (or factors) led to these large differences.
By therapeutic category, the highest Medicaid prescription drug amount was nearly $1.2 billion for CNS drugs in 29 SMRF States in 1997. Four categories (CNS, gastrointestinal, cardiovascular, and anti-infective drugs) accounted for more than 56 percent of total spending. In contrast, the largest number of prescriptions was reported for cardiovascular agents (over 34 million). Payment per prescription was atypically high for biologicals ($270) and antineoplastic agents ($172).
The average annual increase in drug spending reported from the Medicaid data (16.3 percent) compares favorably with the levels of increase reported for Medicaid in the NHE data (15.2 percent). Medicaid increases were comparable to those experienced by other public payers, but lower than the increase for private payers (over 19 percent) and much higher than out-of-pocket increases (about 5 percent).
Discussion
Spending increases for prescription drugs present a continued challenge to those who shape program policy (Kaiser Commission on Medicaid and the Uninsured, 2002b). The problem is exacerbated by severity of the current budget crisis in many States. The choices are difficult—increased taxation, cuts in other State programs, and cuts in Medicaid (Smith, 2002). States will continue to implement drug utilization controls to gain some savings, but associated savings may not be enough.
The significance of effective drug therapy management assumes an even greater importance as concerns for cost-efficiency continue. Data-driven approaches, such as the use of MSIS data, can assist in effective decisionmaking by monitoring patterns of drug utilization and payments. These data could be combined with clinical analysis of patient outcomes under alternative drug regimens to identify cost effective therapies. Such analyses can help eliminate over utilization and reduce the cost of alternate care resulting from under utilization.
Second, Congress has enacted a Medicare prescription drug benefit. Our results also indicate that spending for prescription drugs for aged and disabled Medicaid enrollees has increased dramatically in the last decade. Unless the trend changes, spending under the Medicare benefit will probably continue to grow rapidly. The Medicaid data provide a base for understanding current prescription drug costs and estimating future spending for both Medicaid and Medicare. Enhanced coding in the data for 1999 and later years will permit analysis of drug spending for various types of dually eligible enrollees (e.g., qualified medicare beneficiaries, qualified disabled working individuals, and other buy-in individuals). Since a Medicare benefit has been enacted, another valuable analytic tool would be a Medicare prescription drug database.
Given the severity of the State budget crisis and ongoing concerns about cost containment by other public and private payers, it is unlikely that these payers will allow growth to continue at these rates. That probably means that beneficiaries may incur greater increases in out-of-pocket payments. This is a particular concern for poor and other low-income groups who can least afford out-of-pocket payment for needed prescription drugs. A better understanding of the factors driving spending increases and variations is needed. As illustrated by the analysis of therapeutic categories, we will expand our knowledge of these factors greatly by analyzing drug spending in the four most expensive categories.
We have avoided undue speculation as to the effects of various factors on observed spending increases. The increases are a result of many factors (and possibly interactions among the factors), including: increasing enrollment (particularly for disabled persons), increased use of drugs, cost inflation, new drug therapies (e.g., blockbuster drugs), the use of single source versus generic drugs and State policies to control drug utilization. A number of factors have been identified here, but the impact and possible interaction of these and other factors should receive appropriate treatment in future research.
Acknowledgments
The authors wish to thank Yifei Hu for her work to prepare the FY 2000 data on Medicaid prescription drug payments and recipients by State.
Footnotes
The authors are with the Centers for Medicare & Medicaid Services (CMS). The views expressed in this article are those of the authors and do not necessarily reflect the views of CMS.
Reprint Requests: David K. Baugh, M.A., Centers for Medicare & Medicaid Services, 7500 Security Boulevard, C3-20-17, Baltimore, MD 21244. E-mail: dbaugh@cms.hhs.gov
References
- Baugh DK, Pine PL, Blackwell S. Trends in Medicaid Prescription Drug Utilization and Payments, 1990-1997. Health Care Financing Review. 1999 Spring;20(3):79–105. [PMC free article] [PubMed] [Google Scholar]
- Bruen B. States Strive to Limit Medicaid Expenditures for Prescribed Drugs. Kaiser Commission on Medicaid and the Uninsured; Washington, DC.: Feb, 2002. [Google Scholar]
- Centers for Medicare & Medicaid Services. Internet address: http://www.cms.gov/medicaid/mcaidsad.asp (Accessed 2004.)
- Desonia R. Running on Empty: The State Budget Crisis Worsens. Sep 25, 2002. The George Washington University, National Health Policy Forum. Issue Brief No. 783. [PubMed]
- George Washington University. Medicaid in 2003: Weathering the Perfect Storm. National Health Policy Forum Session, Meeting Announcement; February 7, 2003. [Google Scholar]
- Health Care Financing Administration. 1998 Medicaid Managed Care Enrollment Report, Summary Statistics as of June 30, 1998. Baltimore, MD.: [Google Scholar]
- Holahan J, Weiner JM, Lutzky AW. Health Policy for Low-Income People: State's Responses to New Challenges. Health Affairs Web Exclusive, May 22, 2002. doi: 10.1377/hlthaff.w2.187. Internet address: http://content.healthaffairs.org/cgi/content/abstract/hlthaff.w2.187v1 (Accessed 2004.) [DOI] [PubMed]
- Kaiser Commission on Medicaid and the Uninsured. State Budgets Under Stress: How are States Planning to Reduce the Growth in Medicaid Costs? The Henry J. Kaiser Foundation; Washington, DC.: Jul 30, 2002a. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Medicaid and the Prescription Drug Benefit, Cost Containment Strategies and State Experiences. The Henry J. Kaiser Foundation; Washington, DC.: Sep, 2002b. [Google Scholar]
- Klemm J. Personal communication. Baltimore, MD.: Oct 7, 2003. [Google Scholar]
- Levit K. Personal communication. Baltimore, MD.: Mar 16, 1999. [Google Scholar]
- Levit K. Personal communication. Baltimore, MD.: May 13, 2003. [Google Scholar]
- Levit K, Smith C, Cowan C, et al. Trends in U.S. Health Care Spending, 2001. Health Affairs. 2003 Jan-Feb;22(1):154–164. doi: 10.1377/hlthaff.22.1.154. [DOI] [PubMed] [Google Scholar]
- Smith V. Making Medicaid Better: Options to Allow States to Continue to Participate and to Bring the Program Up to Date in Today's Health Care Marketplace. 2002 Mar 15; Internet address: http://www.nga.org/cda/files/MAKINGMEDICAIDBETTER.pdf (Accessed 2004.)
- Smith V, Ellis E. Medicaid Budgets Under Stress: Survey Findings for States Fiscal Years 2000, 2001, and 2002. Kaiser Commission on Medicaid and the Uninsured; Washington, DC.: Oct, 2001. [Google Scholar]
- Toner R, Pear R. Cutbacks Imperil Health Coverage for States' Poor. The New York Times. 2003 Apr 28; Section A, p.1. [Google Scholar]
- U.S. Census Bureau. Internet address: http://www.census.gov/main/www/cen2000.html (Accessed 2004.)
- Wolters Kluwer Health. Internet address: http://www.Medi-Span.com/products/product_mddb.asp (Accessed 2004.)