Abstract
High-risk pools are State programs that were recently brought under Federal review by the Health Insurance Portability and Accountability Act of 1996 (HIPAA). For a subsidized, yet above-standard premium, they provide coverage to individuals lacking access to private health insurance, typically due to pre-existing conditions. Reducing high-risk pool premiums in all States to the level prevailing in the most generous States (at an annual cost of about $105 million) could lead to a modest but significant increase in enrollment, relative to the uninsurable population. In addition, non-premium changes, for example to benefits and marketing, could also have substantial effects on enrollment.
Introduction
The recent economic downturn has reawakened national concern about the problem of the uninsured. While the proportion of the population without health insurance decreased from 1998 (16.3 percent) to 2000 (14 percent) (U.S. Bureau of the Census, 2000; 2001), the recent economic recession and associated loss of jobs has exacerbated the problem. Between March and November of 2001, nearly one million individuals lost their jobs and their health care coverage; one-half of these losses occurred after the terrorist attacks of September 11, 2001 (Families USA, 2001). The increase in the number of uninsured in 2001 was the largest one-year increase in nearly a decade with 2.2 million losing coverage (Families USA, 2002). An additional 2.4 million people lost coverage in 2002 (Mills and Bhandari, 2003). With higher unemployment and lower consumer spending, State tax revenues are down and budget deficits have reappeared. Consequently, Medicaid budgets are tight and some States have cut optional populations from their programs to reduce expenditures (Simon, 2002; Sloane, 2003).
Among the growing number of uninsured is a class of individuals most in need of insurance: the uninsurable. These are individuals with potentially costly health conditions who pose a high risk to any insurance carrier and who cannot obtain health care coverage due to medical underwriting.1 In 29 States (as of July 2002), these high-risk, uninsurable individuals are eligible for coverage under special State programs known as comprehensive health insurance plans for high-risk individuals (high-risk pools). All high-risk pools offer coverage for a subsidized premium that is, nevertheless, above standard rates. Though operations vary by State, subsidy financing is generally provided by assessments on private carriers, general State revenue, other public sources (e.g., tobacco-settlement funds), or a combination of these.
High-risk pools have quietly become an important component in the Nation's public/private patchwork of health care coverage. The number of high-risk pools has been gradually growing along with enrollment since the first pools began operation in Connecticut and Minnesota in 1976. Recently, the 1996 HIPAA has encouraged this growth by requiring States to guarantee health insurance portability (i.e., that health insurance is available) to individuals who meet certain requirements. High-risk pools have been designated as one of the State Alternative Mechanisms (SAMs) for compliance with the portability provisions of HIPAA, although the act does not endorse high-risk pools above all other alternatives. Moreover, HIPAA established a Federal regulatory role over States that do not select an acceptable portability mechanism. CMS is responsible for undertaking periodic reviews to determine which States have SAMs that are in compliance with HIPAA. In addition, CMS directly exercises Federal authority in States that are not in compliance. Since this Federal authority overrides what would otherwise be a State prerogative, HIPAA creates an incentive for States to select an alternative mechanism, thereby strengthening the position of high-risk pool advocates.
In this article, we combine high-risk pool operational data with State demographic and health insurance data to investigate the historical growth in high-risk pools and the affordability of high-risk pool premiums. We also study the potential for enrollment growth if the premium subsidies were increased.
Data
We constructed a database consisting of high-risk pool operational data linked to State demographic data. High-risk pool operational data (number of enrollees, actual premiums charged, statutory premium caps, and other financial and benefits data) for the years 1981-2000 were obtained from Communicating for Agriculture (CFA) (1995-2001/2002).
Most State demographic measures (State population, number of uninsured, number of uninsurable, income statistics) were obtained or constructed from the Current Population Survey March Supplement (CPS) (U.S. Bureau of the Census, 1995-2001). We chose the CPS because the data are relatively current, they are comprehensive on demographics and income, and reasonably so on health insurance. Additionally, by using the standard technique of pooling 3 years of data, we were able to obtain adequate sample sizes for annual State-level descriptive analysis from CPS data.2 Because high-risk pools serve uninsurable individuals, we needed a measure of the number of uninsurable persons in each State. Unfortunately, we are aware of no broadly accepted statistics on this topic, so we developed an approximation, defining the uninsurable population for each State as individuals who were uninsured and who either could not work, were limited in the type of work they could do, or received any disability or worker's compensation income.3 The remaining data items, namely per capita Medicare expenditures, were obtained from the Statistical Abstract of the United States (U.S. Bureau of the Census, 1995-2001).
The resulting data set consists of 335 observations, each representing a high-risk pool in a single State for a single year during the period from 1981-2000. All of these observations include CFA operational data and the 188 State-year observations corresponding to the years 1995-2000 also include statistical abstract and CPS data.
Descriptive Results
Pool Growth
Three high-risk pools were operating by 1981. The Connecticut and Minnesota pools opened in 1976 and Wisconsin's began operation in 1981. From 1981 to 2000, the number of States with high-risk pools increased nearly every year (Table 1). The only year in which the number of pools decreased is 1995, when Tennessee folded its high-risk pool into TennCare.4 Table 1 also shows the number of States that use a high-risk pool as the State alternative mechanism to satisfy the portability requirements of HIPAA. Since the passage of HIPAA in 1996, most States with high-risk pools began offering pool coverage to HIPAA-eligible individuals to satisfy the new portability requirements. Two States created high-risk pools specifically in reaction to the passage of HIPAA (Alabama and Texas) and several new pools have opened more recently (Kentucky, New Hampshire, and Maryland, all too new to be included in this study). Only 4 of the 27 pools operating in 2000 were not HIPAA pools—California, Florida, Missouri, and Washington State.
Table 1. Number of Enrollees and High-Risk Pools: 1981-2000.
| Year | Total Number of Enrollees | Number of Pools | Number of HIPAA Pools |
|---|---|---|---|
| 1981 | 6,668 | 3 | 0 |
| 1982 | 9,199 | 5 | 0 |
| 1983 | 15,448 | 6 | 0 |
| 1984 | 19,602 | 6 | 0 |
| 1985 | 21,536 | 6 | 0 |
| 1986 | 21,833 | 7 | 0 |
| 1987 | 24,231 | 10 | 0 |
| 1988 | 33,301 | 12 | 0 |
| 1989 | 53,458 | 13 | 0 |
| 1990 | 68,263 | 15 | 0 |
| 1991 | 77,683 | 17 | 0 |
| 1992 | 96,245 | 22 | 0 |
| 1993 | 101,623 | 24 | 0 |
| 1994 | 95,536 | 24 | 0 |
| 1995 | 90,405 | 23 | 0 |
| 1996 | 86,723 | 25 | 0 |
| 1997 | 86,555 | 25 | 11 |
| 1998 | 92,101 | 27 | 22 |
| 1999 | 104,918 | 27 | 22 |
| 2000 | 115,688 | 27 | 23 |
NOTE: HIPAA is Health Insurance Portability and Accountability Act of 1996. SOURCE: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002.
Corresponding to the growth in the number of high-risk pools, Table 1 shows nearly steady growth in the number of pool enrollees. The only period of decline was from 1994-1997. During this period, Tennessee folded its pool into TennCare, which accounts for part of the decrease in 1995. The period of declining enrollment also immediately follows or coincides with the passage of small- and non-group insurance reforms in many States (U.S. General Accounting Office, 1995). These reforms may have been associated with reduced financial support for high-risk pools, given the expectation at the time that insurance reform would reduce the need for pool coverage.
The number of individuals with high-risk pool coverage is very small relative to the number of uninsured, as shown in Table 2. However, this number is larger, and in some States substantial, relative to the numbers of medically uninsurable (the target population for the pools).5 Presumably due to its low premiums, Minnesota's pool is the largest in absolute terms (with 25,892 covered in 2000) and relative to the State's uninsured and uninsurable populations (covering 6 and 54 percent, respectively). The figures for Minnesota are far above the national averages; nationally, high-risk pool enrollment is 0.5 percent of the total uninsured population and 8 percent of the uninsurable population.
Table 2. High-Risk Pool Enrollees, by State: 2000.
| State | High-Risk Pool Enrollees | ||
|---|---|---|---|
|
| |||
| Total | Relative to Number Uninsured | Relative to Number Uninsurable | |
|
| |||
| Percent | |||
| Total | 115,688 | 0.45 | 8 |
| Alabama | 2,431 | 0.37 | 5 |
| Alaska | 395 | 0.33 | 4 |
| Arkansas | 2,270 | 0.55 | 7 |
| California | 17,343 | 0.25 | 6 |
| Colorado | 1,536 | 0.25 | 5 |
| Connecticut | 1,719 | 0.51 | 8 |
| Florida | 709 | 0.03 | 1 |
| Illinois | 10,120 | 0.58 | 10 |
| Indiana | 6,475 | 0.89 | 11 |
| Iowa | 271 | 0.11 | 2 |
| Kansas | 1,283 | 0.43 | 6 |
| Louisiana | 1,088 | 0.13 | 2 |
| Minnesota | 25,892 | 6.14 | 54 |
| Mississippi | 2,231 | 0.49 | 7 |
| Missouri | 889 | 0.16 | 3 |
| Montana | 1,687 | 0.99 | 12 |
| Nebraska | 5,023 | 3.03 | 35 |
| New Mexico | 1,063 | 0.25 | 5 |
| North Dakota | 1,307 | 1.68 | 18 |
| Oklahoma | 1,922 | 0.32 | 3 |
| Oregon | 5,833 | 1.22 | 21 |
| South Carolina | 1,451 | 0.25 | 3 |
| Texas | 8,600 | 0.18 | 4 |
| Utah | 1,106 | 0.37 | 5 |
| Washington | 2,333 | 0.29 | 4 |
| Wisconsin | 10,042 | 1.90 | 21 |
| Wyoming | 669 | 0.87 | 11 |
SOURCES: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002. U.S. Census Bureau, Current Population Survey (1999-2001).
Barriers to Enrollment
Of all the possible barriers to high-risk pool enrollment, two stand out as the most significant: enrollment caps or freezes and high premiums.6 California has an enrollment cap and only sells as many policies as it can finance with revenue from a tobacco tax (17,343 in 2000). There is a waiting list of about 4,000 individuals, each expected to wait about a year before being permitted to enroll in California's pool. Florida has an enrollment freeze. In a political settlement with the insurance industry (which protested the size of assessments for pool subsidy funding), Florida's pool has been closed to new enrollment since 1990 and enrollment has declined from a high of 7,500 in that year to 709 in 2000. A pool with an enrollment cap or freeze on HIPAA eligible individuals does not comply with HIPAA regulations, so the pools in Florida and California are not HIPAA pools and could not be unless changes were made to enrollment policy. Note, however, that to comply with HIPAA, a State cannot impose a cap on HIPAA eligibles, but may impose one on enrollees eligible for other reasons (e.g., Louisiana and Illinois).
The most pervasive barrier to enrollment is affordability. In all States, high-risk pool premiums, while subsidized, are above standard rates. Only a small number of States offer additional subsidies for low-income individuals (Wisconsin, Connecticut, New Mexico, Oregon, and Colorado). Consequently, for most people and in most States, high-risk pool premiums are above the already high non-group market rates, rendering high-risk pool coverage unaffordable for many who cannot obtain coverage in any other way.
To provide a sense of the financial burden imposed by pool premiums, Table 3 lists the percents of all individuals, the uninsured, and the uninsurable, for whom the pool premium7 is greater than 25 percent and for whom it is less than 10 percent of family income. Although there is no standard of affordability, the 25 and 10 percent thresholds are intended to serve as rough guides. Table 3 shows, for example, that nationally, high-risk pool premiums are above 25 percent of family income (i.e., are unaffordable) for 10 percent of all individuals, 18 percent of the uninsured, and 29 percent of the uninsurable. By these standards, almost one-third of the uninsurable are unable to afford high-risk pool coverage, although there are large variations by State with Minnesota's premiums being the most affordable to its population and Kansas' among the least. Note that only 22 of the 27 high-risk pool States are listed in Table 3 because premium data were not available for five States (Connecticut, Florida, Indiana, Louisiana, and Nebraska).
Table 3. Percent of Population for Whom Premium was Either Less Than 10 Percent or More Than 25 Percent of Family Income, by Selected States: 2000.
| State | Premium1 | All Individuals | Uninsured | Uninsurable | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| >25% | <10% | >25% | <10% | >25% | <10% | ||
| Alabama | $192 | 9 | 72 | 18 | 54 | 31 | 36 |
| Alaska | 400 | 14 | 57 | 26 | 35 | 36 | 25 |
| Arkansas | 153 | 6 | 77 | 11 | 61 | 14 | 39 |
| California | 280 | 12 | 62 | 19 | 42 | 30 | 36 |
| Colorado | 214 | 6 | 79 | 12 | 56 | 22 | 50 |
| Illinois | 292 | 11 | 67 | 20 | 46 | 33 | 28 |
| Iowa | 273 | 9 | 65 | 18 | 35 | 27 | 27 |
| Kansas | 382 | 18 | 50 | 37 | 24 | 51 | 24 |
| Minnesota | 128 | 2 | 91 | 6 | 82 | 6 | 86 |
| Mississippi | 215 | 11 | 65 | 18 | 46 | 33 | 46 |
| Missouri | 267 | 10 | 69 | 16 | 49 | 21 | 50 |
| Montana | 252 | 14 | 58 | 26 | 36 | 34 | 24 |
| New Mexico | 202 | 10 | 66 | 16 | 49 | 23 | 48 |
| North Dakota | 223 | 9 | 65 | 15 | 46 | 26 | 38 |
| Oklahoma | 224 | 10 | 67 | 15 | 50 | 25 | 40 |
| Oregon | 232 | 10 | 69 | 20 | 45 | 28 | 26 |
| South Carolina | 268 | 10 | 63 | 20 | 45 | 35 | 29 |
| Texas | 237 | 10 | 67 | 17 | 47 | 24 | 38 |
| Utah | 272 | 7 | 73 | 16 | 52 | 25 | 44 |
| Washington | 266 | 10 | 69 | 20 | 49 | 28 | 41 |
| Wisconsin | 196 | 5 | 79 | 16 | 57 | 22 | 55 |
| Wyoming | 179 | 6 | 79 | 13 | 63 | 20 | 57 |
| All of the Above States | — | 10 | 67 | 18 | 46 | 29 | 37 |
Premium in 2001 dollars for a 35-year old, non-smoking male at the lowest deductible, and no optional features as reported by the States to Communicating for Agriculture, Inc. Includes 22 States with high-risk pools and available premium data.
SOURCES: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002. U.S. Census Bureau, Current Population Survey (1999-2001).
Simulating the Implications of Lower Premiums
Given that affordability is a significant barrier to enrollment, it seems likely that lowering premiums would raise enrollment. To evaluate how much enrollment could grow if premiums were reduced, we conducted a simulation of the impact of lowering all premiums to the level seen in the most generous States.8
To conduct the simulation, we first estimated the elasticity of enrollment with respect to premiums using regression methods. The log of enrollment was modeled as a function of the log of high-risk pool premium, the level of benefits, the size and income of the State's uninsured population, and the year. The unit of observation was the State/year. Note that we use measures of the uninsured population as opposed to the uninsurable population because the former is clearly identifiable in the CPS data while the latter is less so due to previously discussed limitations of CPS data.
We began with the specification
| (1) |
where the subscript s indicates State, the subscript t indicates year and all the variables are as defined in Table 4.9 Refer to Technical Note A for the theoretical model that underlies equation 1. Because the actual high-risk pool premium was not available for enough States and years to permit the estimation of equation 1, we used a proxy defined as
Table 4. Definition of Variables.
| Variable1 | Definition/Comment | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| log(enrollments,t) | Log of high-risk pool enrollment. | 7.33 | 1.10 | 5.16 | 10.32 |
| log(premiums,t) | Log of high-risk pool premium. Only available for 58 observations. | 5.39 | 0.31 | 4.75 | 6.05 |
| log(proxy premiums,t)2 | Proxy for high-risk pool premimum. | 8.89 | 0.27 | 8.42 | 9.68 |
| pct. of market premiums,t | High-risk pool premium as percent of market premium. | 1.52 | 0.23 | 1.18 | 2 |
| per capita Medicare expenditures,t | Used as proxy for market premium. | 4,912 | 924.00 | 3,139 | 8,002 |
| lowest deductibles,t | Controls for generosity of benefits.3 | 543.8 | 235.10 | 0 | 1,000 |
| multiple deductibless,t | Binary variable; controls for generosity of benefits.3 | 0.85 | 0.35 | 0 | 1 |
| log(uninsured populations,t) | Controls for demand. | 12.81 | 0.78 | 10.87 | 14.43 |
| log(per capita family income of uninsureds,t) | Controls for demand. | 10.46 | 0.18 | 10.08 | 10.86 |
| yeart | Controls for trends in enrollment and premiums | 1997.58 | 1.70 | 1995 | 2,000 |
| lag log(proxy premiums,t) 2 | Used as an additional instrumental variable for log(proxy premiums,t). | 8.86 | 0.27 | 8.2 | 9.68 |
| lag pct. of market premiums,t2 | Used as an additional instrumental variable for log(proxy premiums,t). | 1.52 | 0.22 | 1.25 | 2 |
| lag per capita Medicare expenditures,t2 | Used as an additional instrumental variable for log(proxy premiums,t). | 4,775 | 992.00 | 2,425 | 8,002 |
Subscript s indexes States (Alabama, Alaska, Arkansas, Colorado, Connecticut, Illinois, Indiana, Iowa, Kansas, Louisiana, Minnesota, Mississippi, Missouri, Montana, Nebraska, New Mexico, North Dakota, Oklahoma, Oregon, South Carolina, Utah, Washington, Wisconsin, and Wyoming). Subscript t indexes years (1995-2000). Not every State has an observation in every year. Three States are excluded: California (enrollment is capped), Florida (pool is closed), and Texas (not in equilibrium).
As described in the text, to remove endogeneity, we instrumented for log(proxy premiums, t). The instruments were lag log(proxy premiums, t), lag pct. of market premiums, t, and lag per capita Medicare expenditures,t.
Benefits vary by State and year and were not consistently provided in our data sources. Deductible levels, however, were consistently provided and serve as a measure of plan generosity.
NOTE: N=137, except where indicated.
SOURCES: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002. U.S. Census Bureau, Current Population Survey (1999-2001).
| (2) |
where per capita Medicare expenditure serves as a proxy for State-to-State/year-to-year variation in the actual market premium. The percent of market premium variable was established through interviews with State high-risk pool administrators and is often, but not always, set at the statutory maximum. In cases where administrators could not supply the percent of market premium, we used the statutory maximum.
One problem with this specification is that plan administrators might adjust premium levels in reaction to unexpected enrollment changes. In particular, if enrollment is higher than budgeted, plan administrators might raise premiums in an effort to keep enrollment and losses in line with legislative expectations. Thus, to the extent that enrollment changes might cause premium changes, the premium variable in equation 1 is endogenous. To address this endogeneity, we estimate equation 1 by instrumental variables using lagged values of the log of proxy premium, the percent of market premium, and per capita Medicare expenditure as instruments for the log of proxy premium.
Table 5 provides the estimated coefficients for equation 1 using the proxy premium of equation 2 and instrumental variables as described. Our estimate of elasticity of enrollment with respect to premium for this specification is -1.9, which is the value used in the simulation that follows. A variety of other specifications were studied and comparable results were obtained.
Table 5. Estimation Results (Dependent Variable Log [enrollments,t])1.
| Variable | Coefficient (Standard Error) |
|---|---|
| log(proxy premiums,t) |
***-1.90 (0.41) |
| lowest deductibles,t | 0.000091 (0.0004) |
| multiple deductibless,t | -0.23 (0.25) |
| log(uninsured populations,t) |
**0.77 (0.12) |
| log(per capita family income of uninsureds,t) |
*1.03 (0.52) |
| yeart | 0.67 (0.051) |
| constant | -129 (100) |
To remove endogeneity, we instrumented for log (proxy premiums, t). The instruments were lag log(proxy premiums, t), lag pct. of market premiums, t, and lag per capita Medicare expenditures, t. Three States are excluded: California (enrollment is capped), Florida (pool is closed), and Texas (not in equilibrium).
Significant at the 5.0 percent level.
Significant at the 0.1 percent level.
NOTE: N = 137, R2 = 0.25.
SOURCES: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002. U.S. Census Bureau, Current Population Survey (1999-2001). U.S. Census Bureau, Statistical Abstract of the United States (1995-2001).
Other researchers have also consistently found that individual insurance purchase responds to price, although magnitudes vary according to the population studied and the source of price variation (Chernew, Frick, and McLaughlin, 1997; Gruber and Poterba, 1994; Ku and Coughlin, 2000; Marquis and Long, 1995; and Stearns and Mroz, 1996). In general, our elasticity is larger in magnitude as compared with those in the literature, which are typically below one in absolute value. However, the market for high-risk pools is unique in that potential enrollees are known to have higher expected health care utilization than the general public as well as being older, having lower incomes, and being less likely to be working. Moreover, high-risk pool enrollees typically pay the entire premium, in contrast to individuals with employer-based group insurance. So, it is reasonable to expect an elasticity larger in magnitude. In a study of disenrollment from eight States' high-risk pools, Stearns and Mroz (1995/1996) observe that severalfold increases in disenrollment rates occurred at the time of selected premium increases, though the degree of response varied across States. Their results are consistent with an elasticity the magnitude of the one we estimate (Technical Note B).
As Table 6 shows, our preferred elasticity estimate of -1.9 implies that if premiums were set to no higher than 125 percent of market rate, enrollment would grow by 33 percent, nationally, reaching 11 percent of the uninsurable (up from 8 percent in 2000—Table 2). Enrollment growth varies by State, depending on how far current pool premiums are from 125 percent of market rate (Technical Note C).
Table 6. Predicted Effect of Reduction in Premiums to 125 Percent of Market Rate, by State: 2000.
| State | Premium as Percent of Market | Year 2000 Enrollment | Simulated Enrollment1 | Simulated Enrollment Relative to | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Actual Enrollment | Uninsured | Uninsurable | ||||
|
| ||||||
| Percent | ||||||
| Total | 115,688 | 153,666 | 133 | 1 | 11 | |
| State | ||||||
| Alabama | 175 | 2,431 | 4,612 | 190 | 1 | 10 |
| Alaska | 200 | 395 | 966 | 245 | 1 | 11 |
| Arkansas | 150 | 2,270 | 3,212 | 141 | 1 | 9 |
| California2,3 | 125 | 17,343 | 17,343 | 100 | 0 | 6 |
| Colorado2 | 118 | 1,536 | 1,536 | 100 | 0 | 5 |
| Connecticut | 150 | 1,719 | 2,432 | 141 | 1 | 12 |
| Florida3 | 250 | 709 | 709 | 100 | 0 | 1 |
| Illinois | 150 | 10,120 | 14,318 | 141 | 1 | 14 |
| Indiana | 150 | 6,475 | 9,161 | 141 | 1 | 16 |
| Iowa | 150 | 271 | 383 | 141 | 0 | 3 |
| Kansas | 150 | 1,283 | 1,815 | 141 | 1 | 8 |
| Louisiana | 200 | 1,088 | 2,662 | 245 | 0 | 5 |
| Minnesota2 | 125 | 25,892 | 25,892 | 100 | 6 | 54 |
| Mississippi | 175 | 2,231 | 4,233 | 190 | 1 | 13 |
| Missouri | 200 | 889 | 2,175 | 245 | 0 | 6 |
| Montana | 150 | 1,687 | 2,387 | 141 | 1 | 16 |
| Nebraska | 135 | 5,023 | 5,815 | 116 | 4 | 41 |
| New Mexico2 | 125 | 1,063 | 1,063 | 100 | 0 | 5 |
| North Dakota | 135 | 1,307 | 1,513 | 116 | 2 | 21 |
| Oklahoma | 140 | 1,922 | 2,385 | 124 | 0 | 4 |
| Oregon2 | 125 | 5,833 | 5,833 | 100 | 1 | 21 |
| South Carolina | 200 | 1,451 | 3,550 | 245 | 1 | 7 |
| Texas3 | 165 | 8,600 | 8,600 | 100 | 0 | 4 |
| Utah | 150 | 1,106 | 1,565 | 141 | 1 | 7 |
| Washington | 150 | 2,333 | 3,301 | 141 | 0 | 6 |
| Wisconsin | 200 | 10,042 | 24,567 | 245 | 5 | 51 |
| Wyoming | 200 | 669 | 1,637 | 245 | 2 | 27 |
Enrollment simulated using Δ log(enrollment) = (-1.9) Δ log(premium).
Premiums in these States are already at or below 125 percent of market rates. Therefore, we did not simulate a change in premium in these States, and thus, there is no change in enrollment.
Three States are excluded: California (enrollment is capped), Florida (pool is closed), and Texas (not in equilibrium).
SOURCES: Communicating for Agriculture, Inc.: Comprehensive Health Insurance for High-Risk Individuals (9th-15th editions). Fargo Falls, MN. 2001/2002. U.S. Bureau of the Census: Statistical Abstract of the United States, 1995-2001. Internet address: http://www.census.gov/prod/www/statistical-abstract-us.html (Accessed 2004.) U.S. Census Bureau, Current Population Survey (1999-2001).
Using premium, claims, and assessment funding figures from CFA, we can calculate a simple approximation of the cost of subsidizing all premiums to 125 percent of market rates. The increase in cost has two components. The first is the change in enrollment multiplied by the difference between the average claim per person and the new premium. The second is the number of current enrollees multiplied by the change in premium.10
An order of magnitude estimate of the annual additional cost of reducing premiums to 125 percent of market rate is about $105 million nationally, or about $2,800 per new enrollee per year (Appendix D). This figure assumes no change in the level of assessment funding currently provided in each State and does not include administrative costs. We acknowledge that a major challenge facing any policymaker wishing to finance high-risk pool expansion is how to do it without displacing current funding (a variant of the crowd-out problem11); however, our purpose here is only to develop a first approximation of what might be possible, postponing such implementation issues.
One additional lesson emerges from this simulation. As Table 6 indicates, even when premiums are fixed at approximately the same level relative to the market, States differ dramatically with respect to the proportion of the uninsurable that would be covered. Six States are projected to cover between 20 and 55 percent, eight States are between 10 and 19 percent, and the remaining States are in the low, single digits. These results underscore the fact that considerations other than premium levels have substantial effects on enrollment. Some of these factors could be circumstantial, such as the relative availability of charity care, and some could reflect characteristics of the high-risk pools, such as the extent of marketing and the attractiveness of benefits.
Although this simulation was intended only as a rough approximation, several cautions still apply. First, the proxy premium used in our preferred specification implicitly assumes that per capita Medicare spending is closely correlated with market rates for individual insurance policies. We acknowledge that this assumption is impossible to verify; nevertheless, some support can be drawn from the fact that elasticity estimates were similar across specifications using actual premiums and proxy premiums. Second, we acknowledge that benefits influence enrollment, but we were only able to include a few covariates to control for differences in benefits due to limitations of sample size and inconsistent reporting of benefits across States and years. The fact that specifications including State-fixed effects produced similar elasticity estimates partially mitigates this concern, provided the most important differences in benefits between States were stable through time. Finally, our definition of uninsurable is by necessity somewhat arbitrary. It is likely that a different definition would produce different results, particularly if the chosen definition included substantially more individuals.
Policy Discussion
Other than encouraging the establishment of high-risk pools, the influence of Federal regulation on access to those pools has been modest to date. Of the two chief barriers to access, enrollment caps or freezes and affordability, HIPAA only addresses the first one, establishing that a high-risk pool must not impose restrictions on the number of HIPAA eligible enrollees in order to be an acceptable portability mechanism (25 of the 27 high-risk pools in operation in 2000 satisfy this criterion, though only 23 are HIPAA pools).
Most States do not provide additional premium subsidization for low-income pool applicants. Therefore, for much of the high-risk target population (the medically uninsurable) high-risk pool coverage is unaffordable. Federal regulation regarding the degree of affordability of high-risk pools could encourage additional enrollment and lead to an increase in coverage for the uninsurable population.
Of course, the benefits of lower premiums come at a cost. For about $105 million in additional premium subsidization, high-risk pool enrollment could be expected to grow by about 33 percent and increase coverage of the uninsurable population from 8 to 11 percent. While this increase may be modest, this is a population most in need of coverage and likely to rely on substantial amounts of high-cost emergency care if uninsured.
The fact that substantial projected enrollment variation remains among States after adjusting for premium differences suggests that significant enrollment growth could be encouraged even without additional premium subsidies. In the course of their regular reviews of State alternative mechanisms under HIPAA, it would be reasonable for regulators to focus their attention on the operations of pools with relatively low enrollment, controlling for premium. In addition to improving understanding of the factors that explain enrollment variations, it is possible that such a ranking by itself would serve as an effective incentive for State policymakers and pool administrators to seek to minimize barriers to access.
For the purposes of this discussion, we have sidestepped several challenging issues associated with an increase in the Federal role. Federal regulation involves questions of Federal versus State authority, funding for the Federal activity, information requirements for monitoring, among other things. Moreover, to be effective, regulators must have strategies to prevent unintended consequences such as the use of Federal money to underwrite current costs, rather than expand coverage. Thus, the results of this article should be interpreted as an example of what is possible under ideal circumstances in which these other issues are resolved.
Given the prevailing fiscal climate and the political challenge of simply maintaining the current level of high-risk pool funding, additional funding is unlikely to come from State sources. Federal action, therefore, appears to be the most feasible instrument of expansion in the near future. This study shows that, building on the foundation established by HIPAA, the combination of new Federal funding and Federal affordability and enrollment guidelines could significantly expand access to health insurance for those currently unable to acquire it.
Epilogue
In December 2003, the U.S. Department of Health and Human Services announced the first round of grants to States with high-risk pools (about $30 million to 16 States). The grants, authorized in the Trade Adjustment Assistance Reform Act of 2002, are available only to States with risk-pool premiums no higher than 150 percent of the market rate. States satisfying this and other criteria can apply for a grant totaling up to 50 percent of the losses incurred in risk-pool operation. While it is too soon to tell what effect the grants will have on high-risk pool enrollment, their intent is to encourage the expansion of access to high-risk pool coverage through reduction in premiums (U.S. Health and Human Services 2003).
Technical Note A
Theoretical Model
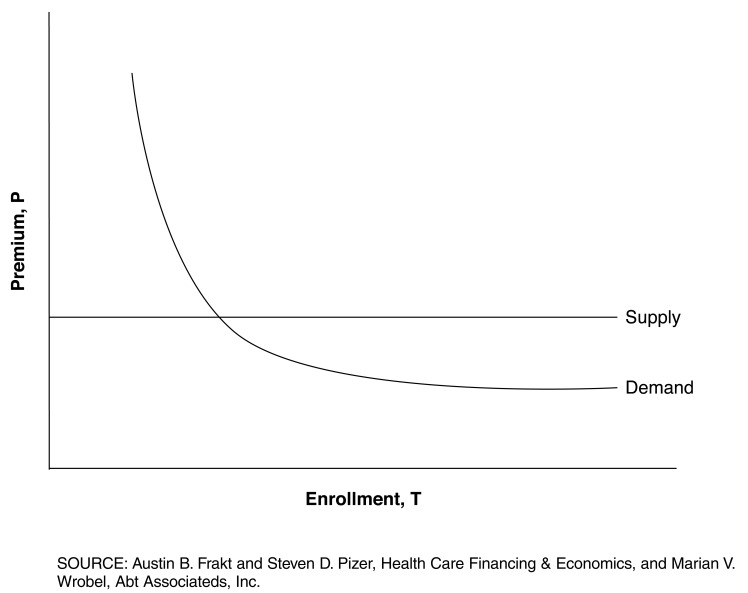
The theoretical model that underlies the empirical work presented in this article begins with the assumption that premiums and benefits are set by high-risk pools prior to enrollment decisions. That is, individuals choose to enroll with full knowledge of the benefits package and cost sharing. We also assume that the elasticity of supply is infinite, i.e., that supply will meet demand, and that elasticity of demand εT, is constant. The infinite supply elasticity assumption justifies the exclusion of pools that impose constraints on enrollment (California and Florida) from our estimation of elasticity of demand. Finally, we assume that total enrollment is a complete measure of demand, i.e., that everyone who wishes to enroll does so. This justifies the exclusion of pools that are too new to have signed up everyone who wishes to enroll (Texas).
Figure 1 illustrates some of our assumptions. The horizontal axis is total enrollment, T, and the vertical axis is premium, P. Since the elasticity of supply is infinite, the supply curve is a horizontal line. Thus, the point of equilibrium, where demand meets supply, is uniquely determined by the demand curve and demand is measured as total enrollment, T.
Figure 1. Theoretical Model.
The equation governing the demand curve takes the form
| (Eq. A.1) |
Demand, T, is a function of premium, P with an elasticity εT, which is expected to be negative. All other things being equal, demand should increase with the generosity of benefits. Demand should be higher in State-years with larger uninsured populations since there would be more individuals in need of high-risk pool coverage. Demand should be higher if the population in need of high-risk pool coverage has higher income. Finally, year controls for secular trends in the health insurance market.
Technical Note B
Comparison of Elasticity Estimate to Stearns and Mroz
Stearns and Mroz (1995/1996) compute an elasticity of disenrollment with respect to premium for high-risk pools in eight States. Using some simple calculus, we convert disenrollment elasticity into an upper bound on elasticity of total enrollment.12 We find that the average upper bound on total enrollment elasticity based on the results of Stearns and Mroz is -1.5, which is consistent with the estimate obtained in this article (because −1.9 is less than the upper-bound of −1.5).
Let Ti, Di, and Ei represent total enrollment, number of disenrollees, and number of enrollees during period i, then
| (Eq. B.1) |
Differentiating Eq. B.1 with respect to premium for period 1, P1, and multiplying by P1/T1 we find an expression for elasticity of total enrollment, εT, in terms of changes in E1 and D1.
| (Eq. B.2) |
We can express εT in terms of elasticity of enrollment, εE, elasticity of disenrollment, εD, enrollment rate, rE, and disenrollment rate, rD:
| (Eq. B.3) |
where
| (Eq. B.4) |
| (Eq. B.5) |
All quantities on the right-hand-side of Eq. B.3 are non-negative except εE, which is non-positive.13 Therefore, the first term on the right-hand-side of Eq. B.3 is negative. Dropping it yields an upper-bound on εT:
| (Eq. B.6) |
Stearns and Mroz study the effect of an upward premium shock on disenrollment in eight States. For each State, they estimate a disenrollment elasticity, εD, and a disenrollment rate, rD. Using these and Eq. B.6, we can estimate an upper-bound on total enrollment elasticity for each State and an average across States. For example, the annualized disenrollment rate for Iowa is rD = 0.2 and the disenrollment elasticity is εD = 10.2. Thus, εT < -2.0. The average upper-bound computed in this way is εT < −1.5. This is strong support that the −1.9 value computed in this article is a reasonable estimate of the elasticity of total enrollment for high-risk pools.14
Technical Note C
Example Simulation Calculation
Below we provide an example calculation of the simulated enrollments provided in Table 6. This example is for the State of Alabama. Let T be total enrollment and P be premium and eT be elasticity of total enrollment with respect to premium. Then, by definition
| (Eq. C.1) |
To simulate a change in T requires use of an approximation to εT. Our approximation is
| (Eq. C.2) |
Using Eq. C.2 and letting T0, T1, P0, and P1 be original enrollment, new (simulated enrollment), original premium, and new (lower) premium, respectively, the equation for simulated enrollment is
| (Eq. C.3) |
Using data for Alabama, the calculation is as follows.
Original Premium (P0)
Per capita Medicare spending (proxy premium) = $5,901.84
Premium as percent of market = 175%
P0 = 1.75 × $5901.84 = $10,328.22
log(P0)= 9.25
Original Enrollment (T0)
T0 = 2,431
log(T0) = 7.80
New, Lower Premium (P1)
Premium as percent of market = 125%
P1 = 1.25 × 5901.84 = $7,377.30
log(P1) = 8.91
New, Simulated Enrollment Calculation (T0)
T1=exp[log(T0)+εT(log(P1)−log(P0))] =exp(7.80−1.9×(8.91- 9.25))=exp(8.45)= 4,656
(small difference from Table 6 due to rounding of intermediate results).
Technical Note D
Confidence Interval of Elasticity Estimate and Range of Enrollment Estimate
Our elasticity estimate is −1.9. The 95 percent confidence interval is −2.7 to −1.1. This implies a range of predicted enrollment of 134,485 to 179,249 and a cost range of $55 to $180 million.
Acknowledgments
The authors wish to thank Jim Fuller for his consistent support for this project. We also wish to thank Sally Stearns, Robert Coulam, and seminar participants at the Academy for Health Services Research and Health Policy and the HIPAA 2001 State-Federal Conference for comments on earlier versions of this research. We would like to express our appreciation to the members of the National Association of State Comprehensive Health Insurance Plans (NASCHIP) for their availability and willingness to help us understand the many nuances of their organizations. Finally, we thank the reviewers for their suggestions that improved readability of this article.
Footnotes
Austin B. Frakt and Steven D. Pizer are with the Department of Veterans Affairs. Marian V. Wrobel is with Abt Associates, Inc. The research in this article was supported by the Centers for Medicare & Medicaid Services (CMS) under Contract Number 500-95-0062(TO#8) and by Abt Associates Inc. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of the Department of Veterans Affairs, Abt Associates Inc., or CMS.
Medical underwriting is the consideration of medical history in the determination of coverage eligibility.
There are also some limitations of CPS data. The survey does not ask about Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage, which is relevant because one must exhaust COBRA coverage to qualify for the protections established by HIPAA. CPS data are not comprehensive with regard to health status which is relevant to determining who might be uninsurable due to underwriting.
Our approach suggests that roughly 1 percent of the total population and 6 percent of the uninsured population is uninsurable; this is slightly higher than results cited by the State of California, namely that 2.5-5.0 percent of California's uninsured are uninsurable due to medical underwriting (Hunt, 2000).
TennCare is Tennessee's health insurance program for the low-income and uninsurable population, including the Medicaid-eligible population. Because the uninsurable population is just a small part of TennCare, it does not operate like a standard high-risk pool and should not be viewed as one.
The target population are those who cannot obtain insurance in the standard (group/individual) market. This includes those estimated as uninsurable from CPS data and high-risk pool enrollees (virtually all high-risk pool enrollees would be uninsurable if not enrolled). Consequently, we calculated percents of uninsurable (target population) as (pool enrollment/[pool enrollment + CPS estimate of uninsurable]) × 100.
Benefits also affect desirability of the product. However, due to inconsistent reporting of benefits across States and years, we were unable to analyze the relationship between benefits and enrollment.
For consistency, we used a single, standard premium (that for a 35-year old, non-smoking male at the lowest deductible and with no optional features).
Four States (California, Minnesota, New Mexico, and Oregon) set their premiums at 125 percent of the market rate. This is the standard used for the simulation. One State, Colorado, sets premiums at 118 percent of the market rate. States conduct market surveys to determine the market rate, but we do not have access to these market surveys.
Three States are excluded when estimating coefficients: California (enrollment is capped), Florida (pool is closed), and Texas (not in equilibrium).
This method is not precise about the level of subsidy spending in each State for two reasons. First, subsidy spending does not track claims on an annual basis—losses in one year are offset by revenues in following years. Second, subsidy spending may occur in forms not easily accounted for, e.g., as low-income premium subsidies.
The term crowd out is typically applied to situations where expanded public services (e.g., Medicaid) cause privately financed services to be reduced (Gruber, 2000).
We distinguish between total enrollees (the number of individuals enrolled at a fixed point in time), enrollees (the number of individuals who enter in a period), and disenrollees (the number of individuals who leave in a period). An elasticity can be associated with each of these: elasticity of total enrollment, elasticity of enrollment, and elasticity of disenrollment, respectively.
That enrollment and disenrollment rates, rE and rD, respectively, are non-negative is obvious. That elasticity of disenrollment, εD, is non-negative is clear from theory (disenrollment increases as price rises) and is demonstrated empirically by Stearns and Mroz (1995/1996). That elasticity of enrollment, eE, is non-positive is clear from theory (enrollment decreases as price rises).
Note that a negative upper-bound (e.g., -1.5) implies that numbers more negative (e.g., -1.9) are consistent.
Reprint Requests: Austin B. Frakt, Ph.D., Health Care Financing & Economics, 150 S. Huntington Avenue, Mail Stop 152H, Boston, MA 02130. E-mail: frakt@bu.edu
References
- Chernew M, Frick K, McLaughlin CG. The Demand for Health Insurance Coverage by Low-Income Workers: Can Reduced Premiums Achieve Full Coverage? Health Services Research. 1997 Oct;32(4):453–470. [PMC free article] [PubMed] [Google Scholar]
- Communicating for Agriculture Inc. Comprehensive Health Insurance for High-Risk Individuals. 9th-15th editions. Fergus Falls, MN.: 1995-2001/2002. [Google Scholar]
- Families USA. Covering the Uninsured: Two Million Americans Lost Their Health Insurance in 2001; Largest One-Year Increase in Nearly a Decade. 2002 Feb 12; Press release. Internet address: http://covertheuninsuredweek.org/media/docs/release021202.php3 (Accessed 2004)
- Families USA. New Unemployment Number Indicates Over 529,000 Laid-Off Workers Lost Health Coverage from September through November. Dec 7, 2001. Press release.
- Gruber J, Poterba J. Tax Incentives and the Decision to Purchase Health Insurance: Evidence from the Self-Employed. The Quarterly Journal of Economics. 1994 Aug;109(3):701–733. [Google Scholar]
- Gruber J. Health Insurance and the Labor Market. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics Vol 1A. Elsevier Science; Amsterdam: 2000. [Google Scholar]
- Hunt S. Individual Health Insurance Options for California. Sep, 2000. Study by Pricewaterhouse Coopers for the California Managed Risk Medical Insurance Board. [Google Scholar]
- Ku L, Coughlin T. Sliding Scale Premium Health Insurance Programs: Four States Experience. Inquiry. 1999-2000 Winter;36(4):471–480. [PubMed] [Google Scholar]
- Marquis MS, Long SH. Worker Demand for Health Insurance in the Non-Group Market. Journal of Health Economics. 1995 May;14(1):47–63. doi: 10.1016/0167-6296(94)00035-3. [DOI] [PubMed] [Google Scholar]
- Mills R, Bhandari S. Health Insurance Coverage in the United States: 2002. Sep, 2003. pp. 60–223. U.S. Census Bureau Current Population Reports. [Google Scholar]
- Simon S. Medicaid Ax Is Falling as Recession Saps States. Los Angeles Times. 2002 Mar 5;:A1. [Google Scholar]
- Sloane T. Medicaid Mahem; State Budget Shortfalls Will Leave Beneficiaries, Providers in Lurch. Modern Healthcare. 2003 Jul 7;33(27):21. [Google Scholar]
- Stearns SC, Mroz TA. Premium Increases and Disenrollment from State Risk Pools. Inquiry. 1995/1996 Winter;32:392–406. [PubMed] [Google Scholar]
- U.S. Bureau of the Census. United States Department of Commerce News. Sep 28, 2000. Chances of Having Health Insurance Increase, Reversing 12-Year Trend, Census Bureau Says. Press release. [Google Scholar]
- U.S. Bureau of the Census. More People Have Health Insurance, Census Bureau Reports. United States Department of Commerce News. 2001 Sep 28; Press release. [Google Scholar]
- U.S. Bureau of the Census. Statistical Abstract of the United States, 1995-2001. Internet address: http://www.census.gov/prod/www/statistical-abstract-us.html (Accessed 2004)
- U.S. Department of Health and Human Services. HHS Awards Nearly $30 Million to States to Offset Costs of Insurance for Residents Too Sick for Conventional Coverage. 2003 Dec 17; Press release. CMS Public Affairs. Internet address: http://www.hhs.gov/news/press/2003pres/20031217a.html (Accessed 2004)
- U.S. General Accounting Office. Health Insurance Regulation: Variation in Recent State Small Employer Health Insurance Reforms. Washington, DC.: Jun, 1995. Fact Sheet for the Chairman, Subcommittee on Employer-Employee Relations, Committee on Economic and Educational Opportunities, House of Representatives. GAO/HEHS-95-161FS. [Google Scholar]