Abstract
Children and adolescents' access to Medicaid-financed behavioral health services was examined over 8 years in Tennessee (managed care) and Mississippi (fee-for-service [FFS]) using logistic regression. Managed care reduced access to behavioral care overall, overnight services (e.g., inpatient), and specialty outpatient services. Managed care also restricted the relative use of overnight and specialty outpatient for children and adolescents. However, managed care had pronounced effects on use of case management services. We also document differences in access and mix of behavioral services used over time by race, sex, age, and Medicaid enrollment category.
Introduction
Since the early 1990s, States have worked at varying speeds to incorporate the principles and practices of managed care for their Medicaid populations. The hope has been that by changing the patterns of service utilization to emphasize preventive care and reduce providers' financial incentives to extend treatment unnecessarily, States would achieve improvements in health at lower cost. The lingering concern in managed care systems is that firms or doctors accrue cost savings for any service withheld, regardless of its benefit to consumers.
Concurrently, the Nation witnessed a great expansion in the volume of health care data collected and a reduction in the cost of data storage and processing. This reduction in research costs has provided hope that statistical analysis of policy changes will protect patient safety and provide a means of evaluating the consequences of system changes like the shift to managed care. Thus, efforts like the Health Plan Employer Data and Information Set (HEDIS®) program by the National Committee on Quality Assurance (NCQA) have emerged as a means of using existing data to monitor health insurance systems.
This article evaluates the effects of a switch to managed behavioral health care in Tennessee's Medicaid Program, focusing on the experiences of children between 4-17 years of age, in contrast to a State which remained FFS, Mississippi. The analyses adjust for other demographic characteristics that might explain variation over time. Our work represents an important contribution for several reasons. First, few State-level data analyses have examined behavioral health services, and fewer still have focused on children and adolescents. Second, the length of the time series for this analysis is 8 years. Prior studies have tended to use at most 3 years, and typically only 1 or 2. This longer time perspective allows investigation of long-term trends in the Medicaid system. Third, our data cover the time period during which managed care started in earnest through Section 1115 waivers from the former Health Care Financing Administration.
Background
Two decades of research on Medicaid have used claims, encounter, and enrollment data to examine the effects of changes in policy on service utilization and costs of treatment. A large portion of this work focused specifically on risk-adjustment and capitation ratesetting, a natural path because managed care was the dominant policy change of the past two decades and developing a budget-neutral yet profit-making set of capitation rates is the fundamental cost problem for States and managed care firms, respectively. Another focus of research with these data has been patterns of utilization among Medicaid enrollees. One branch has followed the economics literature and interest in demand for medical and mental health services (Manning et al., 1987), while another assessed so-called performance indicators or benchmarks for service utilization as a basis for assuring quality of care and contract enforcement. Groups like the NCQA, which produces the HEDIS® measures (National Committee for Quality Assurance, 2003), and the Children's Mental Health Benchmarking Project (Perlman et al., 1999) examine differences in the rates of common services and assess patterns of service use in relation to standards of care (e.g., use of outpatient services following a hospital discharge). Similar efforts are supported through Federal agencies (Mental Health Statistics Improvement Program, 1996; Garnick et al., 2002). While the ultimate research interests differ across these areas, common to them are fundamental questions about the probability of using services among different populations.
Hutchinson and Foster (2002) reviewed the Medicaid managed behavioral health care literature as it pertains to children and concluded, with respect to service use outcomes, that managed care raised overall access (probability of service use), reduced use of inpatient services, increased use of case management care, and had ambiguous effects on the use of outpatient services. Much of the research they identified comes from the Massachusetts Medicaid Program (Dickey et al., 2001; Callahan et al., 1995), with additional results from North Carolina (Burns et al., 1999) and Colorado (Catalano et al., 2000). The General Accounting Office (U.S. General Accounting Office, 1999) found similar results for carve-out programs in four States, while more recent work examining Nebraska's behavioral health carve out (Bouchery and Harwood, 2003) and the Iowa (McCarty and Argeriou, 2003) and Maryland (Ettner, et al., 2003) managed substance abuse programs followed the trends identified by Hutchinson and Foster.
TennCare, Tennessee's statewide managed care Medicaid 1115 waiver program, has received particular scrutiny, predominantly addressing medical care for specific types of diseases or services. However, no studies of TennCare have examined patterns of access and use among children with emotional and behavioral problems using data from the TennCare system. This study goes beyond existing research in the area of managed Medicaid research by examining a longer time series of youth in Medicaid than the studies reviewed by Hutchinson and Foster and the General Accounting Office. As a result we are able to examine longer-term trends in how each State's Medicaid system uses behavioral health services and managed care's effect on those trends.
Methods
Design
Our analysis employs a quasi-experimental interrupted time-series non-equivalent no treatment control group design (Cook, Shadish, and Campbell, 2002) to assess the effect of managed care on measures of access to behavioral health services generally and to inpatient, specialty outpatient, and case management services in particular. We also focus on the effect of managed care on the mix of services children receive. The experimental condition is Medicaid managed care, represented here by Tennessee's TennCare program. Prior to January 1994, Tennessee operated a FFS Medicaid Program. From January 1994 to June 1996, TennCare operated a statewide full-risk capitated managed care program for all medical services under a Section 1115 waiver. Private sector behavioral health service providers were part of the capitation plan, but most behavioral health services in this time period, particularly State mental hospitals and community health centers, remained FFS. Beginning in FY 1997, TennCare carved out behavioral health services on a capitated basis to specialty behavioral health organizations. Because these transitions were universal and without an implementation timelag (e.g., switching a few counties at a time), we used data from Mississippi, which operated a statewide FFS system for its behavioral health care throughout the time period.
The principal benefits of this design are the longitudinal nature of the study and the presence of both pre- and post-intervention measures on the outcomes of interest. However, conclusions drawn from the analysis necessarily must be tempered by the limits of such a design. Use of Mississippi as a comparison group presupposes that the populations of the two States and the operations of their system were similar enough to permit attribution of changes over time to managed care and that no other State-specific interventions affected the program or its enrollees. Mississippi was selected initially because it was the only State in the southeast with a FFS system that could promise timely data access during the observation period. Table 1 shows the behavioral health access rates for both States, and access in the initial year, FY 1994, is comparable in each State. Additional analysis of inpatient admissions shows the States had similar initial lengths of stay: Mississippi averaged 25.3 days with a median of 21; Tennessee averaged 27.4, with a median of 16. Census data for Mississippi and Tennessee show the States have comparable childhood poverty levels (19 versus 18 percent, respectively), childhood Medicaid enrollment (35 versus 38 percent), and percent of children ages 5-15 with disabilities (6 versus 6 percent). Also, survey data on samples from these States show similar rates of serious emotional disturbance in the Medicaid population (22 versus 26 percent) (Heflinger and Saunders, Forthcoming 2005). In addition, our analyses control for observable pre-existing differences in the populations in the analysis. We will note one policy difference between the States in terms of case management in the Discussion section that we treat as part of Tennessee's managed care intervention.
Table 1. Annual Number of Medicaid Enrollees and Behavioral Health Service Users, Age 4-17, by State Fiscal Year: 1994-2001.
| State Fiscal Year (July-June) | Mississippi | Tennessee | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Number of Medicaid Enrollees | Number of Behavioral Service Users | Number of Overnight Users | Number of Specialty Outpatient Users | Number of Case Management Users | Number of Medicaid Enrollees | Number of Behavioral Service Users | Number of Overnight Users | Number of Specialty Outpatient Users | Number of Case Management Users | |
| 1994 | 188,631 | 14,725 | 1,414 | 11,477 | 4,516 | 352,703 | 25,881 | 3,171 | 16,694 | 1,813 |
| 1995 | 190,172 | 16,116 | 1,922 | 12,179 | 5,626 | 398,047 | 28,447 | 3,567 | 17,573 | 1,050 |
| 1996 | 189,298 | 16,801 | 1,945 | 12,486 | 6,236 | 409,270 | 33,989 | 4,120 | 20,941 | 671 |
| 1997 | 185,822 | 16,766 | 1,830 | 12,529 | 6,788 | 423,246 | 32,975 | 2,301 | 18,682 | 2,775 |
| 1998 | 178,038 | 16,537 | 2,053 | 12,567 | 7,559 | 440,411 | 33,877 | 2,100 | 19,026 | 4,245 |
| 1999 | 182,512 | 17,503 | 2,048 | 13,399 | 8,012 | 462,506 | 38,561 | 2,280 | 22,189 | 7,077 |
| 2000 | 205,610 | 18,942 | 2,099 | 13,938 | 8,082 | 469,692 | 41,082 | 2,421 | 23,916 | 9,506 |
| 2001 | 242,162 | 21,103 | 2,521 | 14,796 | 8,314 | 482,466 | 33,681 | 2,014 | 19,625 | 9,960 |
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claims/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
Data
The analysis focuses on youth between age 4-17 years of age with service use and enrollment data between July 1993 and June 2001 (FYs 1994-2001). Enrollment and claims or encounter data come from the Bureau of TennCare and the Mississippi Division of Medicaid. The analysis restricted the claims/encounters used to those with a mental health or sub-stance-related diagnosis (ICD-9-CM code 290 to 315 in the primary or secondary diagnosis). We further excluded records with a primary or secondary diagnosis of developmental delay (ICD-9-CM codes 316 to 319). Both systems use American Hospital Association uniform billing revenue codes, (1992 revision) for hospital-based records and current procedural terminology (CPT) or HCFA common procedure coding system (HCPCS) codes for professional services.
The Bureau of TennCare receives all encounters from participating managed care organizations and behavioral health organizations. A State audit has documented the completeness of the data systems (Division of State Audit, 2002), and further analysis details the completeness and accuracy of those data for behavioral services (Saunders and Heflinger, 2003). The primary limitation in the TennCare data with respect to children and youth with emotional and behavioral problems is a gap in inpatient services reported between April 1995 and June 1996; however, those differences tended to affect lengths of stay rather than the probability of using services. The Mississippi data are nearly identical in structure and layout to the Tennessee data. Other researchers have used Mississippi's data system for analysis (Adams, Bronstein, and Raskind-Booth, 2002).
Lastly, we have excluded services financed through a Medicaid set-aside program for youth in State custody in Tennessee, which affects the presence of their residential and case management services in the TennCare data. Tennessee allowed youth in State custody to be enrolled in managed care firms, but the firms were not responsible for providing residential or case management services for these youth (Comptroller of the Treasury, 2002). The State continued to finance these services on a FFS basis. We believe this exclusion is appropriate because the managed care companies do not determine State custody status for children, inhibiting dumping responses. Also, we allow children in State custody to contribute other services within each year (e.g., a child in State custody who uses outpatient behavioral health services; a child uses inpatient care while still living at home before entering custody). Finally, omitting these services maximizes the contrast between the States on the intervention variable, managed care. We will note the effects of this omission when discussing the results.
Analysis
We identified claims or encounters as relating to a behavioral health service through a combination of diagnostic codes and procedure codes and classified them into research service categories such as inpatient, individual therapy, and case management. These methods are described in detail in Saunders and Heflinger (2003). For this analysis, we focused on overnight settings (inpatient, residential, and inpatient or residential detoxification), specialty outpatient services (individual therapy, partial hospitalization/day treatment, group therapy, family therapy), and case management.1
Our analysis focuses on two key probability measures common to performance measurement and used in econometric estimates of demand for services. The first, access, measures the annual probability of using behavioral health services for individuals in the population.2 This can be thought of as the unconditional probability of behavioral service use and is like the first-part of multi-part models of demand for services (i.e., whether a person receives a service). We also examine the unconditional probability of using each of our three types of services. That is, given that one is enrolled in Medicaid in a year, what is the probability of receiving an overnight service? The effects of covariates on such probabilities would be of actuarial benefit for ratesetting.
Service mix measures refer to the conditional probability of using a particular type of service. That is, given that one receives any behavioral health service, what is the probability of using services of a given type. Just as the multi-part models of demand for services would estimate a probability model for whether a behavioral service user uses inpatient services or not, so we estimate the probability of using an inpatient service, as well as the separate conditional probabilities for specialty outpatient care and case management. We call them mix measures because they give a sense of the relative mix of services used by a person in treatment. If the inpatient mix (the proportion of users who receive inpatient care) rises we know that it is being used as a greater component of treatment for the population.3 This allows examination of how the service system combines resources for patients seeking treatment of behavioral health disorders.
For the overall access analysis, we classified each person enrolled in Medicaid using a dummy variable for whether the person received any behavioral health services in a year for each of the 8 years of data. The unit of analysis is the person-year. We then pooled the person-year records for our two States and estimated a logistic regression for the probability of using any service, adjusting for the additional covariates described later. For the access analyses by type of service, we followed a similar method, classifying individuals as receiving services of a given type (i.e., overnight, specialty outpatient, case management) within the year or not and estimating a logistic regression for each of those probability measures. For the service mix analyses, we restricted the pool of individuals to those who used a behavioral health service within the year. Among these individuals, we created a dummy variable for each type of service, classified the youth according to whether a service of that type was used in that year, and estimated a logistic regression for each of those measures.
Our covariates include a dummy variable equal to 1 for Tennessee youth and 0 for Mississippi youth and a pre-post managed care dummy variable set equal to 1 for the years of managed care in Tennessee and 0 otherwise. Because managed behavioral health care occurs only in Tennessee in this study, we could not interact State with managed care; in essence, the managed care dummy is an interaction with the State dummy. The models use Huber-White adjusted standard errors for significance levels and hypothesis testing about the covariates.
For each outcome measure, we controlled for youths' race, sex, age, and Medicaid enrollment category. Because very few (<1 percent) minority enrollees are other than black enrollees, we dichotomized race as white versus minority, with white as the reference category. Sex has the usual dichotomy with male as the reference. We dropped individuals for whom we did not have a legitimate value for race or sex. We divided youth by age categories into 4-11 year olds and 12-17 year olds with younger children as the reference.
The States share several Medicaid enrollment categories: the disabled (SSI), Aid to Families with Dependent Children/Targeted Assistance for Needy Families (AFDC/TANF), Foster Care, and other poverty-related expansion categories. Prior to TennCare, Tennessee picked up the Medically Needy/Spend Down option and carried that forward under TennCare. As part of TennCare, the State added uninsured children (i.e., youth without private coverage through a parent's employer) and uninsurable children (i.e., youth with preexisting condition exclusions). Each State also had a small number of youth enrolled in State-specific categories that did not fit into the previously mentioned groups; we excluded these youth from the analysis. SSI served as the reference category in the analysis because there is likely more homogeneity across States in terms of their SSI population than in their poverty-related populations due to the heterogeneity in welfare program generosity.
We included a linear time trend (YEAR), coding the first (SFY 1994) as 0 and incrementing subsequent years accordingly (SFY 1995 is YEAR=1, SFY 1996 is YEAR=2, etc.). This variable represents the effect of being enrolled in Medicaid in a particular FY on the probability that a child uses a behavioral health service (or a particular type of behavioral service).
A major concern for the analysis is whether the two States are sufficiently comparable to pool their data and estimate an effect of managed care. If the States have different structural determinants of service use, then we would expect different coefficients for the regressors using only the Tennessee or only the Mississippi data. We assessed the appropriateness of pooling using the Chow test (Greene, 1997). To foreshadow the results, the Chow test rejects the null hypothesis for each analysis, indicating the States are different; however, we present both pooled and separate models by State to look at the magnitude of the managed care effect.
Results
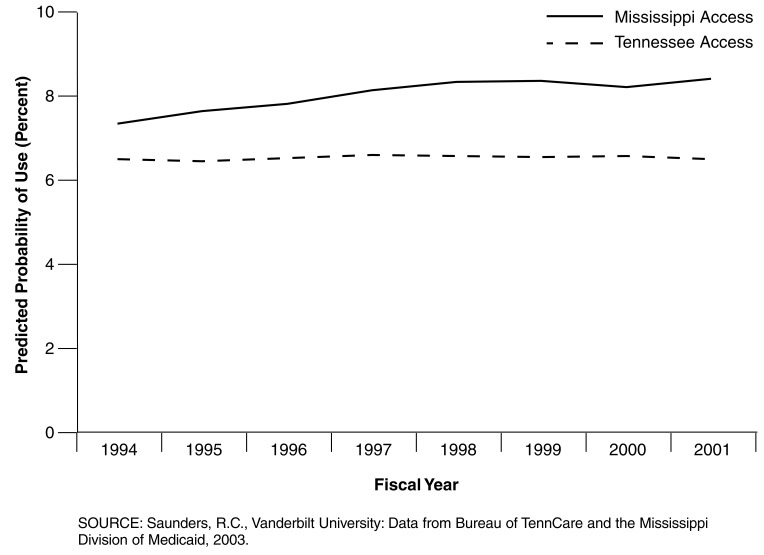
Table 1 presents the size of the cohorts in each State for the study period. Although Tennessee has larger enrolled and treated populations, a greater percentage of Mississippi enrollees use behavioral health services (Figure 1). Table 2 describes the population of enrollees and behavioral health service users in each State in terms of the independent variables for our models for SFY 2000 (the results are similar for all years).
Figure 1. Annual Probability Behavioral Health Services, Access, Age 4-17, by State Fiscal Years: 1994-2001.
Table 2. Demographic Characteristics of Enrollees and Behavioral Service Users, by State Fiscal Year: 2000.
| Category | Mississippi | Tennessee | ||
|---|---|---|---|---|
|
|
|
|||
| Enrollees N=205,610 | Behavioral Health Users N=18,942 | Enrollees N=469,692 | Behavioral Health Users N=205,610 | |
|
| ||||
| Percent | ||||
| Demographic | ||||
| Female | 50.7 | 38.1 | 49.3 | 37.3 |
| Minority | 74.9 | 62.9 | 37.8 | 24.7 |
| Age | ||||
| 4-11Years | 63.0 | 51.8 | 62.4 | 51.9 |
| 12-17 Years | 37.0 | 48.2 | 37.6 | 48.1 |
| Medicaid Enrollment | ||||
| SSI | 8.2 | 24.8 | 4.8 | 14.5 |
| AFDC/TANF | 25.5 | 25.7 | 29.5 | 27.7 |
| Other Poverty | 65.5 | 47.0 | 21.2 | 15.1 |
| Foster Care | 0.5 | 1.8 | 2.3 | 10.4 |
| Medically Needy | N/A | N/A | 7.5 | 5.8 |
| Uninsurable | N/A | N/A | 1.7 | 1.9 |
| Uninsured | N/A | N/A | 33.0 | 24.6 |
NOTES: SSI is supplemental security income. AFDC is Aid to Families with Dependent Children. TANF is Temporary Assistance to Needy Families. NA is not applicable.
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claims/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
In terms of enrollees, the States are comparable in the proportion of youth who are female, teenagers, and enrolled through the AFDC/TANF program. The major differences are in the greater representation of minorities in Mississippi reflecting its greater proportion of black residents (41 versus 19 percent) in Census 2000. The differences in enrollment categories are due to the larger number of options available in Tennessee. Despite these differences, we see similar changes between the enrolled and treated population in the distribution for these variables. In both States, the proportion who are female, minority, or enrolled through other poverty programs declines, while the proportion who are teens, on SSI, or foster care rises.
The rest of this section discusses the managed care effect observed in the overall access probability and then the access and mix probabilities for overnight, specialty outpatient, and case management services. Because the magnitudes and directions of effects for the other covariates are similar across models, we will conclude this section by presenting results for the other covariates together.
Overall Access
The odds of using a behavioral health service within a year under managed care were about 6 percent less than in FFS during the time period of our data (Table 3). Figure 1 shows the predicted probabilities for each State, evaluated at the means of the covariates. In terms of marginal probability, this implies a reduction in the probability of behavioral health service use of 0.004 (Figure 1), or about 4 treated individuals per 1,000 enrollees. However, looking at the Tennessee-only model, managed care led to a slight improvement in the odds of using a service. Thus, managed care may have improved access in Tennessee, but not enough to offset improvements that occurred in Mississippi's FFS system.
Table 3. Logistic Regression Estimates for Access to Behavioral Health Services, Age 4-17, by State Fiscal Years: 1994-2001.
| Access Analysis | Pooled | Mississippi | Tennessee | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
| Access Variable | |||||||||
| Female | 0.653 | 0.002 | 0.000 | 0.665 | 0.004 | 0.000 | 0.647 | 0.003 | 0.000 |
| Minority | 0.505 | 0.002 | 0.000 | 0.568 | 0.003 | 0.000 | 0.469 | 0.002 | 0.000 |
| Age 12-17 | 1.244 | 0.004 | 0.000 | 1.264 | 0.007 | 0.000 | 1.229 | 0.005 | 0.000 |
| Year | 1.039 | 0.001 | 0.000 | 1.048 | 0.001 | 0.000 | 1.021 | 0.002 | 0.000 |
| Managed Care | 0.938 | 0.005 | 0.000 | N/A | N/A | N/A | 1.010 | 0.008 | 0.000 |
| Tennessee | 0.691 | 0.004 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 1.530 | 0.011 | 0.000 | 1.473 | 0.028 | 0.000 | 1.479 | 0.012 | 0.000 |
| AFDC/TANF | 0.352 | 0.002 | 0.000 | 0.374 | 0.003 | 0.000 | 0.335 | 0.002 | 0.000 |
| Other Poverty | 0.235 | 0.001 | 0.000 | 0.257 | 0.002 | 0.000 | 0.214 | 0.002 | 0.000 |
| Uninsurable | 0.313 | 0.005 | 0.000 | N/A | N/A | N/A | 0.294 | 0.005 | 0.000 |
| Uninsured | 0.232 | 0.001 | 0.000 | N/A | N/A | N/A | 0.220 | 0.002 | 0.000 |
| Medically Needy | 0.245 | 0.002 | 0.000 | N/A | N/A | N/A | 0.231 | 0.002 | 0.000 |
Supplemental security income is the reference category.
NOTES: SE is standard error. AFDC is Aid to Families with Dependent Children. TANF is Temporary Assistance to Needy Families. NA is not applicable.
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claim/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
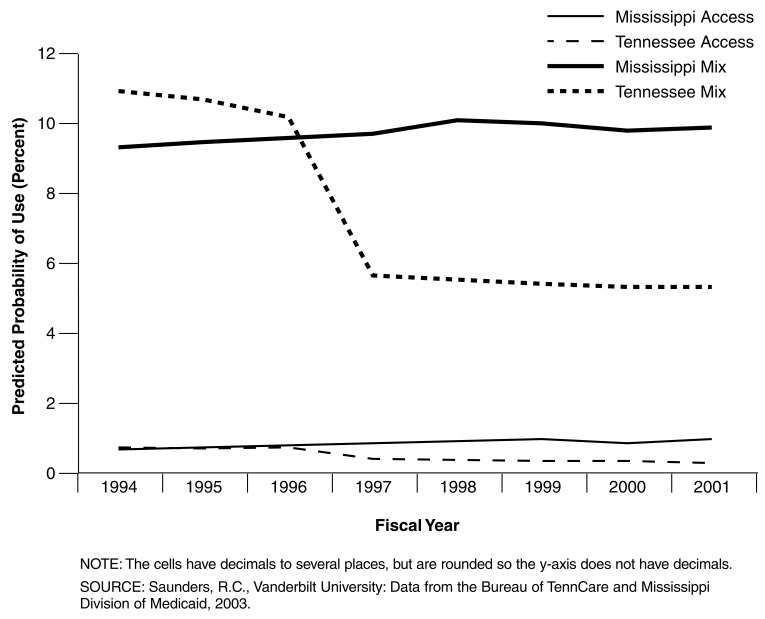
Overnight Services
Managed care reduced the odds of using overnight care such as inpatient or residential treatment by 56 percent (Table 4). The access reduction implied by this ratio is also 0.004 (Figure 2), which, considering the probability of using overnight services is less than 0.01, is fairly large. Figure 2 shows the large reduction in overnight service use concurrent with the implementation of Tennessee's behavioral health carve-out. Among youth in treatment, too, managed care reduced the role of overnight services in treatment by over one-half. The odds of using overnight care conditional on any behavioral service use was 0.47, which corresponds to a probability reduction of 0.046.
Table 4. Logistic Regression Estimates for Access and Mix of Overnight Services, Age 4-17, by State Fiscal Years: 1994-2001.
| Access Analysis | Pooled | Mississippi | Tennessee | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
| Access Variable | |||||||||
| Female | 0.705 | 0.007 | 0.000 | 0.674 | 0.011 | 0.000 | 0.721 | 0.010 | 0.000 |
| Minority | 0.445 | 0.005 | 0.000 | 0.370 | 0.006 | 0.000 | 0.538 | 0.008 | 0.000 |
| Age 12-17 | 2.864 | 0.033 | 0.000 | 3.148 | 0.057 | 0.000 | 2.702 | 0.040 | 0.000 |
| Year | 1.052 | 0.003 | 0.000 | 1.066 | 0.004 | 0.000 | 1.000 | 0.006 | 0.941 |
| Managed Care | 0.438 | 0.008 | 0.000 | N/A | N/A | N/A | 0.537 | 0.014 | 0.000 |
| Tennessee | 0.746 | 0.012 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 1.462 | 0.027 | 0.000 | 2.232 | 0.079 | 0.000 | 1.248 | 0.027 | 0.000 |
| AFDC/TANF | 0.249 | 0.003 | 0.000 | 0.273 | 0.005 | 0.000 | 0.225 | 0.004 | 0.000 |
| Other Poverty | 0.129 | 0.002 | 0.000 | 0.150 | 0.003 | 0.000 | 0.101 | 0.003 | 0.000 |
| Uninsurable | 0.312 | 0.014 | 0.000 | N/A | N/A | N/A | 0.294 | 0.013 | 0.000 |
| Uninsured | 0.139 | 0.003 | 0.000 | N/A | N/A | N/A | 0.131 | 0.003 | 0.000 |
| Medically Needy | 0.183 | 0.005 | 0.000 | N/A | N/A | N/A | 0.172 | 0.005 | 0.000 |
| Mix Analysis | Pooled | Mississippi | Tennessee | ||||||
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
|
| |||||||||
| Access Variable | |||||||||
| Female | 0.960 | 0.011 | 0.000 | 0.907 | 0.016 | 0.000 | 0.995 | 0.014 | 0.724 |
| Minority | 0.788 | 0.010 | 0.000 | 0.601 | 0.010 | 0.000 | 1.032 | 0.017 | 0.049 |
| Age 12-17 | 2.403 | 0.028 | 0.000 | 2.593 | 0.048 | 0.000 | 2.320 | 0.035 | 0.000 |
| Year | 1.006 | 0.003 | 0.041 | 1.015 | 0.004 | 0.000 | 0.974 | 0.006 | 0.000 |
| Managed care | 0.475 | 0.009 | 0.000 | N/A | N/A | N/A | 0.542 | 0.015 | 0.000 |
| Tennessee | 1.015 | 0.018 | 0.394 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 0.913 | 0.018 | 0.000 | 1.468 | 0.055 | 0.000 | 0.798 | 0.018 | 0.000 |
| AFDC/TANF | 0.669 | 0.009 | 0.000 | 0.687 | 0.014 | 0.000 | 0.659 | 0.013 | 0.000 |
| Other Poverty | 0.512 | 0.010 | 0.000 | 0.544 | 0.013 | 0.000 | 0.463 | 0.015 | 0.000 |
| Uninsurable | 0.954 | 0.046 | 0.330 | N/A | N/A | N/A | 0.966 | 0.047 | 0.479 |
| Uninsured | 0.543 | 0.012 | 0.000 | N/A | N/A | N/A | 0.550 | 0.013 | 0.000 |
| Medically Needy | 0.670 | 0.019 | 0.000 | N/A | N/A | N/A | 0.673 | 0.020 | 0.000 |
Supplemental security income is the reference category.
NOTES: SE is standard error. AFDC is Aid to Families with Dependent Children. TANF is Temporary Assistance to Needy Families. NA is not applicable.
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claims/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
Figure 2. Annual Predicted Probability of Overnight Services, Access and Mix, Age 4-17, by State Fiscal Years: 1994-2001.
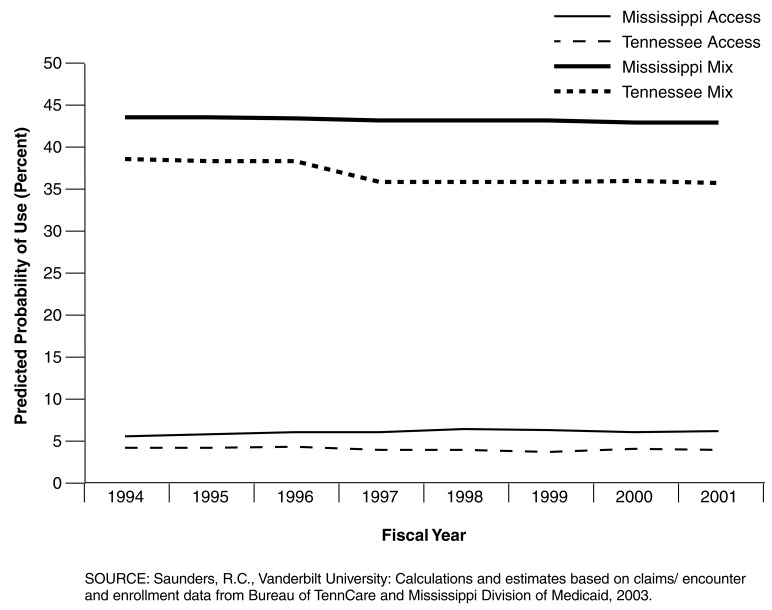
Specialty Outpatient Services
The odds of a child within the Medicaid population using specialty outpatient care are 15 percent less under managed care (Table 5). This corresponds to a reduction in the probability of using specialty outpatient services of 0.008 (Figure 3). Even among youth in treatment, youth in managed care have a reduced likelihood of using these services with an odds ratio of 0.915. In probability terms, this translates to a reduction of 0.022. Within Tennessee, we see a statistically insignificant decrease in access, but significant reduction in the mix of specialty outpatient among youth in treatment. Figure 3 shows the slight dip in both access and mix of this service coinciding with the behavioral health carve-out beginning in FY 1997.
Table 5. Logistic Regression Estimates for Access and Mix of Specialty Outpatient Services, Age 4-17, by State Fiscal Years: 1994-2001.
| Access Analysis | Pooled | Mississippi | Tennessee | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
| Access Variable | |||||||||
| Female | 0.717 | 0.003 | 0.000 | 0.677 | 0.004 | 0.000 | 0.745 | 0.004 | 0 |
| Minority | 0.573 | 0.002 | 0.000 | 0.649 | 0.004 | 0.000 | 0.521 | 0.003 | 0 |
| Age 12-17 | 1.318 | 0.005 | 0.000 | 1.234 | 0.008 | 0.000 | 1.366 | 0.007 | 0 |
| Year | 1.039 | 0.001 | 0.000 | 1.042 | 0.001 | 0.000 | 1.027 | 0.002 | 0 |
| Managed Care | 0.847 | 0.006 | 0.000 | N/A | N/A | N/A | 0.890 | 0.009 | 0.188 |
| Tennessee | 0.593 | 0.004 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 1.867 | 0.015 | 0.000 | 1.571 | 0.033 | 0.000 | 1.764 | 0.017 | 0 |
| AFDC/TANF | 0.355 | 0.002 | 0.000 | 0.386 | 0.003 | 0.000 | 0.324 | 0.003 | 0 |
| Other Poverty | 0.222 | 0.001 | 0.000 | 0.249 | 0.002 | 0.000 | 0.189 | 0.002 | 0 |
| Uninsurable | 0.300 | 0.006 | 0.000 | N/A | N/A | N/A | 0.270 | 0.006 | 0 |
| Uninsured | 0.220 | 0.002 | 0.000 | N/A | N/A | N/A | 0.201 | 0.002 | 0 |
| Medically Needy | 0.236 | 0.003 | 0.000 | N/A | N/A | N/A | 0.213 | 0.002 | 0 |
| Mix Analysis | Pooled | Mississippi | Tennessee | ||||||
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
|
| |||||||||
| Access Variable | |||||||||
| Female | 1.085 | 0.005 | 0.000 | 1.019 | 0.008 | 0.019 | 1.127 | 0.007 | 0.000 |
| Minority | 1.114 | 0.006 | 0.000 | 1.142 | 0.010 | 0.000 | 1.091 | 0.008 | 0.000 |
| Age 12-17 | 1.062 | 0.005 | 0.000 | 0.973 | 0.008 | 0.001 | 1.115 | 0.007 | 0.000 |
| Year | 0.998 | 0.001 | 0.237 | 0.995 | 0.002 | 0.006 | 1.005 | 0.003 | 0.037 |
| Managed Care | 0.915 | 0.008 | 0.000 | N/A | N/A | N/A | 0.891 | 0.010 | 0.000 |
| Tennessee | 0.848 | 0.007 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 1.206 | 0.012 | 0.000 | 1.049 | 0.025 | 0.047 | 1.188 | 0.013 | 0.000 |
| AFDC/TANF | 1.014 | 0.007 | 0.035 | 1.035 | 0.010 | 0.000 | 0.988 | 0.009 | 0.180 |
| Other Poverty | 0.944 | 0.008 | 0.000 | 0.975 | 0.011 | 0.020 | 0.897 | 0.011 | 0.000 |
| Uninsurable | 0.957 | 0.023 | 0.070 | N/A | N/A | N/A | 0.924 | 0.023 | 0.002 |
| Uninsured | 0.945 | 0.009 | 0.000 | N/A | N/A | N/A | 0.914 | 0.010 | 0.000 |
| Medically Needy | 0.956 | 0.013 | 0.001 | N/A | N/A | N/A | 0.921 | 0.013 | 0.000 |
Supplemental security income is the reference category.
NOTES: SE is standard error. AFDC is Aid to Families with Dependent Children. TANF is Temporary Assistance to Needy Families. NA is not applicable.
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claim/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
Figure 3. Annual Predicted Probability of Specialty Outpatient Services, Access and Mix, Age 4-17, by State Fiscal Years: 1994-2001.
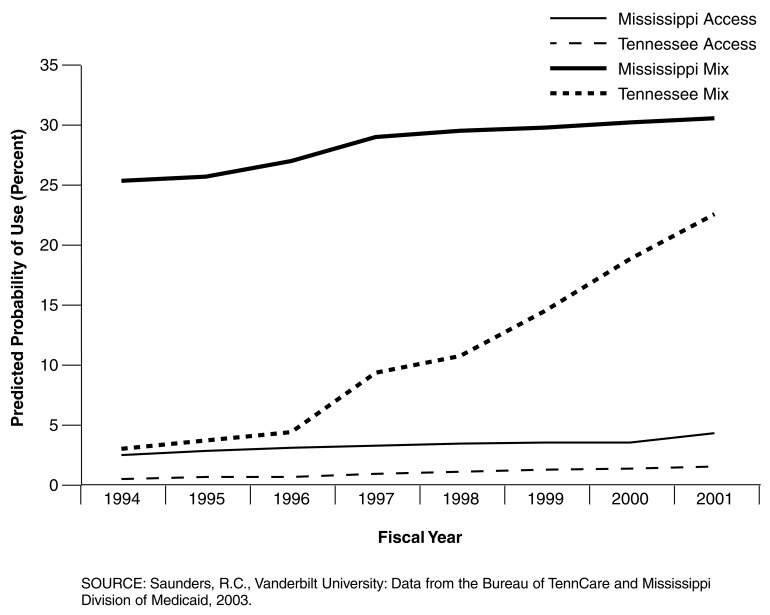
Case Management Services
We see the first positive effect of managed care on access in case management (Table 6). Youth in managed care had a 211-percent greater chance of using this service, an increase in probability of 0.05 (Figure 4). The effect is even larger when looking at those in treatment, where youth had 0.266 greater probability of using case management. In the Tennessee-only model, the effect is smaller than in the pooled results, but still large and positive. Figure 4 shows the large increase in the conditional probability of using this service (mix), and a less pronounced increase in access, beginning in FY 1997.
Table 6. Logistic Regression Estimates for Access and Mix of Case Management Services, Age 4-17, by State Fiscal Years: 1994-2001.
| Access Analysis | Pooled | Mississippi | Tennessee | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds Ratio | Robust | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
| Access Variable | |||||||||
| Female | 0.638 | 0.004 | 0.000 | 0.647 | 0.006 | 0.000 | 0.623 | 0.007 | 0.000 |
| Minority | 0.873 | 0.006 | 0.000 | 0.953 | 0.009 | 0.000 | 0.782 | 0.008 | 0.000 |
| Age 12-17 | 1.346 | 0.009 | 0.000 | 1.234 | 0.011 | 0.000 | 1.543 | 0.016 | 0.000 |
| Year | 1.142 | 0.002 | 0.000 | 1.100 | 0.002 | 0.000 | 1.319 | 0.005 | 0.000 |
| Managed Care | 3.116 | 0.055 | 0.000 | N/A | N/A | N/A | 1.708 | 0.037 | 0.000 |
| Tennessee | 0.117 | 0.002 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 0.558 | 0.011 | 0.000 | 0.970 | 0.032 | 0.356 | 0.361 | 0.009 | 0.000 |
| AFDC/TANF | 0.314 | 0.003 | 0.000 | 0.353 | 0.004 | 0.000 | 0.249 | 0.003 | 0.000 |
| Other Poverty | 0.174 | 0.002 | 0.000 | 0.211 | 0.002 | 0.000 | 0.118 | 0.002 | 0.000 |
| Uninsurable | 0.247 | 0.010 | 0.000 | N/A | N/A | N/A | 0.198 | 0.008 | 0.000 |
| Uninsured | 0.150 | 0.002 | 0.000 | N/A | N/A | N/A | 0.113 | 0.002 | 0.000 |
| Medically Needy | 0.162 | 0.004 | 0.000 | N/A | N/A | N/A | 0.128 | 0.003 | 0.000 |
| Mix Analysis | Pooled | Mississippi | Tennessee | ||||||
|
|
|
|
|||||||
| Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | Odds Ratio | Robust SE | P>|z| | |
|
| |||||||||
| Access Variable | |||||||||
| Female | 0.974 | 0.007 | 0.000 | 0.972 | 0.010 | 0.005 | 0.973 | 0.011 | 0.015 |
| Minority | 1.669 | 0.013 | 0.000 | 1.668 | 0.018 | 0.000 | 1.667 | 0.020 | 0.000 |
| Age 12-17 | 1.083 | 0.008 | 0.000 | 0.965 | 0.010 | 0.000 | 1.277 | 0.014 | 0.000 |
| Year | 1.103 | 0.002 | 0.000 | 1.053 | 0.002 | 0.000 | 1.306 | 0.006 | 0.000 |
| Managed Care | 3.225 | 0.060 | 0.000 | N/A | N/A | N/A | 1.593 | 0.037 | 0.000 |
| Tennessee | 0.171 | 0.003 | 0.000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Enrollment1 | |||||||||
| Foster Care | 0.378 | 0.008 | 0.000 | 0.657 | 0.023 | 0.000 | 0.261 | 0.007 | 0.000 |
| AFDC/TANF | 0.893 | 0.008 | 0.000 | 0.963 | 0.011 | 0.002 | 0.768 | 0.011 | 0.000 |
| Other Poverty | 0.714 | 0.008 | 0.000 | 0.832 | 0.011 | 0.000 | 0.564 | 0.011 | 0.000 |
| Uninsurable | 0.761 | 0.031 | 0.000 | N/A | N/A | N/A | 0.662 | 0.028 | 0.000 |
| Uninsured | 0.656 | 0.010 | 0.000 | N/A | N/A | N/A | 0.536 | 0.009 | 0.000 |
| Medically Needy | 0.688 | 0.017 | 0.000 | N/A | N/A | N/A | 0.601 | 0.016 | 0.000 |
Supplemental security income is the reference category.
NOTES: AFDC is Aid to Families with Dependent Children. TANF is Temporary Assistance to Needy Families. NA is not applicable.
SOURCE: Saunders, R.C., Vanderbilt University: Calculations and estimates based on claim/encounter and enrollment data from Bureau of TennCare and Mississippi Division of Medicaid, 2003.
Figure 4. Annual Predicted Probability of Case Management Services, Access and Mix, Age 4-17, by State Fiscal Years: 1994-2001.
Effects of Other Covariates
In the overall access results (Table 3) as well as the separate estimates by type of service (Table 4-6), female and minority youth were less likely to access behavioral health services overall and by type of service, while teens had a greater likelihood of accessing these services. These results held for both the pooled and separate estimates by State. The same pattern can also be seen in the mix of overnight services. However, the pattern does not hold for the mix of specialty outpatient care, as minority and female youth both have a greater chance of using this service once they are in treatment. Minority youth also have a greater chance of using case management once in treatment. The effects of being a teen on the mix of specialty outpatient and case management move closer to a unitary odds ratio, reflecting differences between the States as Mississippi was more likely to use this service for younger children while Tennessee was more likely to use it with teens.
Looking at the effects of the different enrollment categories, youth in foster care had the greatest chance of accessing services overall and by service type, relative to youth on SSI. However, after entering treatment, children in the foster care category were less likely than children on SSI to use each of these services. One way to think of this is: A random child pulled from the roster of foster care Medicaid enrollees is more likely to use any of these services than one enrolled through SSI, but when we cut the roster to look at only those in treatment, the typical SSI enrollee has a better chance of using each type of service.
Youth in the AFDC/TANF and other poverty categories in both States were less likely than youth on SSI to access services overall and by type of service. This result holds for the separate by-State models. The odds ratios are similar in magnitude across service type, and the most poor youth (AFDC/TANF) have a consistently higher chance of receiving a service than the other poverty category. These results also hold in the mix analyses for outpatient and case management services, though their differences from SSI are of smaller magnitude (i.e., closer to 1.0).
The Tennessee-specific categories are significantly less likely to access services across types of service, and in the access analyses, they are more comparable in magnitude to the poverty categories than SSI or foster care. However, among service users, the uninsured category uses overnight services at a rate comparable to SSI and only slightly less than SSI for specialty outpatient. The pattern of coefficients among these categories matches what one might expect. The uninsurable likely have poor health status, since their health status made them uninsurable in the first place, so they have the smallest difference from the SSI group, which consists of disabled youth. In fact, entry into an overnight facility was sometimes the mechanism for becoming enrolled in TennCare as an uninsurable. The medically needy/spend down group also has identified health problems, but they more closely resemble the poverty categories in service use, perhaps because the reduction in household wealth qualifies one for this category. And, finally, the uninsured most resemble the poverty groups as they simply lack access to employer-sponsored coverage and cannot afford individual coverage. We tested the hypothesis that the coefficients for these three enrollment categories were equal to 1.0; for all the analyses, because of the large sample sizes, we reject the null hypothesis.
Each State experienced positive annual growth in behavioral service access (with the exception of Tennessee's overnight services), all else equal. For the most part Mississippi's FFS system had a faster growth rate in access to these services (i.e., increased odds). In terms of service mix, the annual growth rate is negligible except for case management.
Discussion
The results provide important information about the patterns of service utilization among children in the Medicaid population and the effects of managed care on these patterns. The logistic regressions offer evidence that managed care not only reduces access to behavioral services overall and both access to and mix of inpatient services, where the effect is most pronounced and prior research indicates it should be found (Hutchinson and Foster, 2002), but it also may lead to reductions in specialty outpatient services as well. The decline due to managed care is seen not only in the access rate among enrollees, but also in the role of specialty outpatient services in the mix of services children received. This pattern is consistent with prior work studying this population (Saunders and Heflinger, 2003) and is due in part to large decreases in partial hospitalization, an expensive outpatient alternative to inpatient care, and steady decreases in individual therapy.
Nevertheless, the news is not all bad for managed care. Tennessee experienced significant positive increases in case management services, due in large part to special directives from the Bureau of TennCare to the behavioral health organizations to increase case management and increases in financial incentives to the firms beginning in FY 1998 for this service. Of course, such large increases tend to be more believable when the base rate for this service was so low initially—there was no place to go but up. We attribute this effect to managed care because one of the important aspects of the contracting process is the State's ability to exert market power, in this case by enforcing contractual service obligations.
Looking at the demographic characteristics, there is a consistent pattern of lower behavioral health care access among minority and female youth and greater access for teens across all of the service categories investigated. Disparities in access to behavioral health services for racial/ethnic minorities are of concern nationally (Agency for Healthcare Research and Quality, 2003; U.S. Department of Health and Human Services, 2001). Black and other minority populations have had lower rates of access to health care in general (LaVeist, 2002) and specifically to mental health services (Mayberry, Mili, and Ofili, 2002; Padgett et al., 1994; President's New Freedom Commission, 2003). The greater identification of conduct disorders and other externalizing problems among males may ease entry to treatment for males, although such sex differences are narrowing. Also, male adolescents have been documented to use more overnight services (Halfon, Berkowitz, and Klee, 1992; Hoagwood and Cunningham, 1992) and concerns have been raised that this may be due, in part, to lack of resources to serve them in the community (Heflinger, Simpkins, and Foster, 2002). It is similarly common for the treatment system to serve teens at a greater rate than primary and middle school-aged children (Cuffe et al., 2001).
While disparities between groups largely persist when we look at children in treatment, we notice a few important differences. First, the magnitude of the disparities decreases (i.e., moves closer to an odds-ratio of 1.0), suggesting that much of the disparity in observed use is likely due to barriers to treatment initiation rather than differences in how they are treated after entering the system. However, in some instances we see a reversal in the disparity: for example, minority youth in treatment in both States were more likely to be using case management services than their white counterparts, a pattern that largely holds for specialty outpatient care as well. Some alternative hypotheses might explain these changes with respect to race, particularly for case management. One possibility is minority and white youth who have sought treatment differ in their severity levels. If minorities delay entry to treatment or face greater barriers to treatment, this may exacerbate their illness and require use of more services and require case management. However, if minorities were more functionally impaired once they entered treatment, we might expect higher rates of the overnight services compared with white minorities, and that was not the case. Another possibility is complications in responding to minorities' (or white) cultural patterns of service use. If minorities were more likely to use services in multiple systems, then case management might be reserved to handle these additional complexities. Alternatively, the system may have expectations of parental involvement in treatment such that parents bear the burdens of treatment coordination. Studies on this Medicaid population (Kang, Brannan, and Heflinger, Forthcoming 2005) and other samples of caregivers (Guarnaccia and Parra, 1996; Horwitz and Reinhardt, 1994; Stueve, Vine, and Streuning, 1997) have found that black family members tend to report lower levels of caregiver strain (i.e., burden of care). Perhaps black families are targeted for this type of assistance while white families are expected (by providers or themselves) to be more self-sufficient in their service coordination. Balsa and McGuire (2003) have presented a similar argument with respect to health disparities. However, we cannot rule out (or in) these alternatives completely with the present data because systematic, standardized outcomes data are not routinely collected among this population.
In the Medicaid categories, we saw a consistent pattern of lower access to behavioral health services among youth and greater access of foster care youth relative to youth on SSI. Given the disabilities of youth on SSI and even greater behavioral health issues involved with State custody placements that result in youth being in the foster care eligibility category, this access gradient is not too surprising. We also saw that the magnitude of effect for these variables in the mix analyses brought the odds-ratios closer to 1.0. This likely implies that youth in treatment tend to receive similar services; any financial savings to the firms most likely accrue through reductions in volume of service. The primary exception in these patterns was for foster care youth in overnight settings. This relates to our note in the Methods section about the set-aside program that placed these services outside the management purview of the contractors. The lower rate for foster care youth likely reflects the fact these children can obtain those services through other financing arrangements.
An important observation for Tennessee is the patterns of access and mix in the expansion enrollment categories (i.e., the uninsured and uninsurable) and the medically needy spend down category. In terms of access, children in these three enrollment categories made use of behavioral health services at relatively low rates, comparable to youth in the poverty-related categories. Once in treatment, however, their utilization rates for these services moved closer to the rates of SSI, just like we saw with children in the poverty categories. One of the major concerns in the TennCare program has been the cost of enrollment expansions to cover youth who are otherwise uninsurable or uninsured. This suggests their contribution to costs may not be entirely a matter of adverse selection by enrollees or dumping by employer-sponsored plans, at least with respect to children and behavioral health services. So, if additional capitation requirements were necessary to finance care for these youth, the additional share attributable to behavioral health problems in this subpopulation is likely to be small.
Examination of the time trend variable, which expresses the annual rate of change in access and mix of behavioral services, reveals access to behavioral services generally improved over time in both States, but by a greater amount in Mississippi than in Tennessee. The trend to increased behavioral care is consistent with an increased focus in the mental health field on providing comprehensive, community-based behavioral health services during the 1990s (Fox et al., 1992).
Conclusion
This study has presented important information on the effect that a switch to Medicaid managed care in one Southern State had on patterns of access to behavioral health services and their relative use by youth in treatment. The analyses document important ways in which managed care has shifted the relative use of resources and the services that youth in treatment receive.
An important limitation in most assessments of service utilization patterns and cost analyses is the lack of outcome data. Without outcomes data it is difficult to make population-level inferences about the appropriateness of behavioral service utilization or changes to utilization, financing arrangements, enrollment expansions or other policy interventions. This would be an important improvement to State data systems, monitoring efforts, and so-called report card systems. In addition, State agencies that contract with private managed care companies under 1115 or 1915 waivers are also responsible for monitoring and oversight. Standardized performance measures could be made publicly available and on a regular and timely basis, allowing policymakers, consumers, and health services researchers to evaluate how well the system, whether under a waiver or not, is meeting its goals. Without monitoring, those charged with contract enforcement or treatment responsibilities cannot know whether problems exist within the system. NCQA has advocated a similar position (National Committee for Quality Assurance, 2002), and English and colleagues (1998) emphasized the need for monitoring in managed care.
In the present study, we saw the role that Tennessee's efforts in case management played in increasing this service. In addition to stepping up their own data monitoring efforts, the results of such analysis might provide opportunities to develop targeted 1915 waivers to address the needs of particular subgroups or modify practice patterns for particular services. In Tennessee for example, the clustering of minorities in its major urban areas might afford special opportunities and efficiencies in providing treatment and preventive services to this population. This might also mean placing greater emphasis on recruiting minority providers and increasing cultural-awareness among existing practitioners. Alternatively, both States have large rural populations, and if service utilization differences reflected problems in provider networks (whether managed care or FFS) and travel costs (monetary and timewise) States may find opportunities to address unmet needs for the rural poor.
Regardless of how States respond, whether and how to respond should be informed by data analysis. While Medicaid data are far from perfect for evaluating services, and in many instances state data systems have problems, one way to improve them is to create demand for the by-products of these data.
Acknowledgments
The authors wish to thank Glenn Jennings, formerly of the Bureau of TennCare and Kristi Plotner of the Mississippi Division of Medicaid for their assistance and support in the preparation of this article.
Footnotes
The authors are with Vanderbilt University. The research in this article was funded by the Substance Abuse and Mental Health Administration under contract numbers UR7-TI11304 and IKD1-TI112328 and by the National Institute on Drug Abuse under contract number RO1-DA12982. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of Vanderbilt University, Substance Abuse and Mental Health Administration, National Institute on Drug Abuse, or the Centers for Medicare & Medicaid Services (CMS).
This is only a portion of the types of behavioral services. We have focused on the most common specialty sector treatment services, meaning that we do not count primary care visits for behavioral health purposes, crisis and respite services, or medication management for example.
Access means different things to different researchers. A common alternative is a kind of potential to use services, and those researchers study availability of providers within an area, having a usual source of care or assigned primary care provider, or distance to providers.
However, this increase might reflect severity differences over time, changes in the service system, or both. For our analyses, and nearly all system-level studies, outcomes and severity data are not routinely collected as part of claims and encounter data systems, so this is difficult to assess.
Reprint Requests: Robert C. Saunders, Vanderbilt University, 230 Appleton Place, P.O. Box 90 Peabody College, Nashville, TN 37203. E-mail: robert.c.saunders@vanderbilt.edu
References
- Adams EK, Bronstein JM, Rakind-Hood C. Adjusted Clinical Groups: Predictive Accuracy for Medicaid Enrollees in Three States. Health Care Financing Review. 2002 Fall;24(1):43–61. [PMC free article] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. National Healthcare Disparities Report. Internet address: www.qualitytools.ahrq.gov/. (Accessed 2004.)
- Balsa AI, McGuire TG. Prejudice, Clinical Uncertainty, and Stereotyping as Sources of Health Disparities. Journal of Health Economics. 2003 Jan;22:89–116. doi: 10.1016/s0167-6296(02)00098-x. [DOI] [PubMed] [Google Scholar]
- Bouchery E, Harwood H. The Nebraska Medicaid Managed Behavioral Health Care Initiative: Impacts on Utilization, Expenditures, and Quality of Care for Mental Health. The Journal of Behavioral Health Services & Research. 2003 Jan-Feb;30(1):93–108. doi: 10.1007/BF02287815. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Teagle SE, Schwartz M, et al. Managed Behavioral Health Care: A Medicaid Carve-out for Youth. Health Affairs. 1999 Oct;18(5):214–225. doi: 10.1377/hlthaff.18.5.214. [DOI] [PubMed] [Google Scholar]
- Callahan JJ, Shepard DS, Beinecke RH, et al. Mental Health/Substance Abuse Treatment in Managed Care: The Massachusetts Medicaid Experience. Health Affairs. 1995 Aug;14(3):173–184. doi: 10.1377/hlthaff.14.3.173. [DOI] [PubMed] [Google Scholar]
- Catalano R, Libby A, Snowden L, et al. The Effect of Capitated Financing on Mental Health Services for Children and Youth: The Colorado Experience. American Journal of Public Health. 2000 Dec;90:1861–1865. doi: 10.2105/ajph.90.12.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comptroller of the Treasury, State of Tennessee. Financial and Compliance Audit, Department of Children's Services. 2002 Dec; Internet address: http://www.comptroller.state.tn.us/sa/reports/ag02103.pdf (Accessed 2004.)
- Comptroller of the Treasury, State of Tennessee. Performance Audit: Medicaid Encounter Data: December 2001. Nashville, TN: 2002. [Google Scholar]
- Cook TD, Shadish WR, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Houghton Mifflin Co.; Boston, MA.: 2002. [Google Scholar]
- Cuffe SP, Waller JL, Addy CL, et al. A Longitudinal Study of Adolescent Mental Health Services Use. The Journal of Behavioral Health Services & Research. 2001 Jun;28(1):1–11. doi: 10.1007/BF02287230. [DOI] [PubMed] [Google Scholar]
- Dickey B, Normand SL, Norton EC, et al. Managed Care and Children's Behavioral Health Services: The Massachusetts Experience. Psychiatric Services. 2001 Feb;52:183–188. doi: 10.1176/appi.ps.52.2.183. [DOI] [PubMed] [Google Scholar]
- English A, Kapphahn C, Perkins J, et al. Meeting the Health Care Needs of Adolescents in Managed Care: A Background Paper. Journal of Adolescent Health. 1998 Apr;22:278–292. [PubMed] [Google Scholar]
- Ettner SL, Frank RG, McGuire TG, et al. Risk Adjustment Alternatives in Paying for Behavioral Health Care under Medicaid. Health Services Research. 2001 Aug;36(4):793–811. [PMC free article] [PubMed] [Google Scholar]
- Fox HB, Wicks LN, McManus, et al. Medicaid Financing for Mental Health and Substance Abuse Services for Children and Adolescents. U.S. Department of Health and Human Services; 1993. Publication Number 2794. [Google Scholar]
- Garnick DW, Lee MT, Chalk M, et al. Establishing the Feasibility of Performance Measures for Alcohol and Other Drugs. Journal of Substance Abuse Treatment. 2002 Dec;23(4):375–385. doi: 10.1016/s0740-5472(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Greene WH. Econometric Analysis. Prentice-Hall; Upper Saddle River, NJ.: 1997. [Google Scholar]
- Guarnaccia PJ, Parra P. Ethnicity, Social Status, and Families' Experiences of Caring for a Mentally Ill Family Member. Community Mental Health Journal. 1996 Jun;32(3):243–260. doi: 10.1007/BF02249426. [DOI] [PubMed] [Google Scholar]
- Halfon N, Berkowitz G, Klee L. Children in Foster Care in California: An Examination of Medicaid Reimbursed Health Servics Utilization. Pediatrics. 1992 Jun;89(6):1230–1237. [PubMed] [Google Scholar]
- Heflinger CA, Saunders RC. Physical and Behavioral Health of Medicaid Children in Two Southern States. Southern Medical Journal. doi: 10.1097/01.SMJ.0000149398.02029.5F. Forthcoming 2005. [DOI] [PubMed] [Google Scholar]
- Heflinger CA, Simpkins CG, Foster EM. Modeling Child and Adolescent Psychiatric Hospital Utilization: A Framework for Examining Predictors of Services Use. Children's Services: Social Policy, Research, and Practice. 2002 Jan;5:151–171. [Google Scholar]
- Hoagwood K, Cunningham M. Outcomes of Children with Emotional Disturbance in Residential Treatment for Educational Purposes. Journal of Child and Family Studies. 1992 Jun;1(2):129–140. [Google Scholar]
- Horwitz AV, Reinhard SC. Ethnic Differences in Caregiving Duties and Burdens among Parents and Siblings of Persons with Severe Mental Illnesses. Journal of Health and Social Behavior. 1994 Jun;36:138–150. [PubMed] [Google Scholar]
- Hutchinson AB, Foster EM. The Effect of Medicaid Managed Care on Mental Health Care for Children: A Review of the Literature. Mental Health Services Research. 2002 Mar;5:39–54. doi: 10.1023/a:1021707525105. [DOI] [PubMed] [Google Scholar]
- Kang EJ, Brannan AM, Heflinger CA. Racial Differences in Reports of Strain Among Caregivers of Children with Emotional and Behavioral Disorders. Journal of Child and Family Studies. Forthcoming 2005. [Google Scholar]
- LaVeist TA, editor. Race, Ethnicity, and Health. Jossey-Bass and Company; San Francisco, CA.: 2002. [Google Scholar]
- Manning WG, Newhouse JP, Duan N, et al. Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. The American Economic Review. 1987 Jun;77(3):251–277. [PubMed] [Google Scholar]
- Mayberry RM, Mili F, Ofili E. Racial and Ethnic Differences in Access to Medical Care. In: LaVeist TA, editor. Race, Ethnicity, and Health. Jossey-Bass and Company; San Francisco, CA.: 2002. [DOI] [PubMed] [Google Scholar]
- McCarty D, Argeriou M. The Iowa Managed Substance Abuse Care Plan: Access, Utilization, and Expenditures for Medicaid Recipients. The Journal of Behavioral Health Services & Research. 2003 Jan-Feb;30(1):18–25. doi: 10.1007/BF02287810. [DOI] [PubMed] [Google Scholar]
- Mental Health Statistics Improvement Program. Consumer-Oriented Mental Health Report Card. Center for Mental Health Services; Rockville, MD.: 1996. [Google Scholar]
- National Committee for Quality Assurance. Washington, DC.: 2003. HEDIS® 2004: Volume 1: Narrative, What's In It and Why It Matters. Internet address: http://www.ncqa.org/communications/publications/hedispub.htm. (Accessed 2004.) [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, et al. Ethnic Differences in Use of Inpatient Mental Health Services by Blacks, Whites, and Hispanics in a National Insured Population. Health Services Research. 1994 Jun;29:135–153. [PMC free article] [PubMed] [Google Scholar]
- Perlman SB, Nechasek SL, Dougerty RH. Children's Mental Health Benchmarking: Progress and Potential. Behavioral Healthcare Tomorrow. 1999 Jun;10(3):14, 36–37. [PubMed] [Google Scholar]
- President's New Freedom Commission on Mental Health. Washington, DC.: 2003. Achieving the Promise: Transforming Mental Health Care in America. Internet address: http://www.mentalhealth-commission.gov/reports/FinalReport/toc.html (Accessed 2004.) [Google Scholar]
- Saunders RC, Heflinger CA. Access to and Patterns of Use of Behavioral Health Services Among Children and Adolescents in TennCare. Psychiatric Services. 2003 Oct;54(10):1364–1371. doi: 10.1176/appi.ps.54.10.1364. [DOI] [PubMed] [Google Scholar]
- Stueve A, Vine P, Streuning EL. Perceived Burden among Caregivers of Adults with Serious Metnal Illness: Comparison of Black Hispanic, and White Families. American Journal of Orthopsychiatry. 1997 Apr;67:199–209. doi: 10.1037/h0080223. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. U.S. Government Printing Office; Washington, DC: 2001. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Internet address: http://www.surgeongeneral.gov/library/mental-health/cre/. (Accessed 2004.) [Google Scholar]
- U.S. General Accounting Office. Medicaid Managed Care: Four States' Experiences With Mental Health Carve-out Programs. U.S. Government Printing Office; Washington, DC.: Sep, 1999. GAO/HEHS-99-118. [Google Scholar]